Abstract
Background
Glaucoma and dry eye disorders (DEDs) are frequent comorbidities. The antioxidant and anti-inflammatory properties of essential polyunsaturated fatty acids have been extensively studied in relation to eye diseases.
Objective
Our objective was to determine the effects of oral supplementation with a combined formulation of antioxidants and essential polyunsaturated fatty acids on expression of cytokines and chemokines in tears from patients with DEDs or primary open-angle glaucoma (POAG).
Methods
Participants (n = 97) were distributed into three groups: (1) individuals with nonsevere DEDs (DEDG), (2) individuals with nonadvanced POAG (POAGG), and (3) healthy controls. These groups were randomized into two subgroups: one received a daily antioxidant and essential polyunsaturated fatty acid supplement (two pills) for 3 months (+S), and the other did not (−NS). Participants were interviewed and ophthalmologically examined. Concentrations of specific cytokines and chemokines in reflex tears were determined by multiplexed particle-based flow cytometry. The data were analyzed statistically (SPSS version 15.0).
Results
Comparison of the results from the DEDG and POAGG patients showed significant differences in tear expression of granulocyte-macrophage colony-stimulating factor (P = 0.008), tumor necrosis factor α (P = 0.005), vascular endothelial growth factor (P = 0.038), interleukin-4 (P = 0.030), and interleukin-6 (P = 0.044). The main signs and symptoms of dry eyes such as dryness, burning, photophobia, eye heaviness, and blurred vision, as well as positive changes in eyelashes, hair, nails and skin, were significantly improved in DEDG +S and POAGG +S patients relative to unsupplemented patients.
Conclusion
Inflammation biomarkers were differentially expressed in glaucomatous tears, but the differences changed upon antioxidant/essential polyunsaturated fatty acid supplementation. Chronic instillation of antihypertensive eye drops must be considered for integrating protocols to glaucoma standards of care.
Keywords: glaucoma, dry eye disorders, tears, cytokines, antioxidants, essential fatty acids
Introduction
Owing to advances in disease prevention, detection, and treatment, life expectancy1 has increased in most countries. From 2005 to 2010, the worldwide average life expectancy at birth was 67.88 years (70.14 years for females and 65.71 years for males).2 As a result, biomedical research on the diseases of aging is especially relevant. Age is an important risk factor for ocular diseases such as glaucoma, dry eye disorders (DEDs), cataracts, and age-related macular degeneration, and in elderly people, such diseases can occur together, significantly impairing visual acuity and thus reducing quality of life.
DEDs are complex pathological conditions involving the eyelids, lacrimal glands, tear film, and ocular surface tissues.3 There are two major forms of DEDs – the deficient aqueous tear production form (due to lacrimal gland dysfunction) and the increased evaporative loss form (due to meibomian gland disorder) – but combinations of the two forms are usually seen in clinical practice.4,5 DEDs are also classified according to severity, ranging from normal to mild-to-moderate to severe. Dry eyes usually affect people aged above 60 years old. Significant reduction in body water associated with aging may play a role in the onset or progression of DEDs. Meibomian gland dropout, reduced goblet cells, and laxity of the eyelids may also be contributing factors. In addition, diverse pathologic manifestations on the ocular surface may be triggered by external or internal injury, as well as by menopause, topical or systemic medications, light, computer use, environmental pollutants, and air conditioning.3–5
Glaucoma is a group of diseases characterized by increased intraocular pressure as the main risk factor, leading to progressive visual field defects and visual impairment secondary to loss of retinal ganglion cells and optic nerve fibers.6 People with a glaucomatous family history, diabetes, hypertension, or myopia; African-Americans, Hispanics, and Asians; and people over forty years are at increased risk of glaucoma. Among the various types of glaucoma, the most prevalent is primary open-angle glaucoma (POAG), which accounts for almost 80% of all glaucomas.7,8 The prevalence of POAG has been estimated as 1.1%–3.0% of Western populations aged 40 years or more. Glaucoma remains the second leading cause of blindness worldwide.8
Therefore, both glaucoma and DEDs are highly correlated with age. It is not atypical to see patients chronically treated with antihypertensive eye drops who also exhibit the clinical DED manifestations, from a lesser to a greater degree of severity categories. Recent studies have indicated that 66% of patients with severe DEDs also have glaucoma,9 and approximately 60% of glaucomatous individuals undergoing topical antiglaucoma therapy report DED symptoms.10 However, most cases of glaucoma and DED comorbidity remain undiagnosed, or misclassified as chronic eye irritation, and this is the most important point to be addressed in the present work.
Oxidative stress (OS) plays a significant role in a wide spectrum of ocular conditions.11 OS, an imbalance between pro-oxidant and antioxidant species, can result from the accumulation or uncontrolled generation of reactive oxygen species, partially reduced byproducts of molecular oxygen,11 which may trigger damage to lipids, proteins, and nucleic acids, resulting in cell lesions and death. A significant increase in oxidative activity and a decrease in antioxidant defenses in ocular fluids and tissues as well as in plasma samples have been associated with DEDs,5 POAG,12,13 cataracts,14 diabetic retinopathy,15,16 and age-related macular degeneration.17 However, the pathogenesis of OS and the contribution of this condition to the initial stages or progression of DEDs in patients with POAG remain unclear.
The eyes are continuously exposed to environmental irritants, which stimulate inflammation and immune response (IIR) processes intended to prevent and heal external and internal injuries. The main mediators of IIR processes include leukocytes and other cells involved in the innate immunity system, as well as T, B, and natural killer (NK) lymphocytes (the major components of the adaptive immune system); and the interactions between these cells are modulated by cytokines, chemokines and other molecules.18 Uncontrolled acute or chronic inflammation can lead to tissue damage. For example, altered levels of a wide spectrum of IIR mediators in blood, the aqueous humor, the vitreous body, and eye tissues support the idea that abnormal activity of the immune system is involved in both anterior and posterior ocular segment disorders.19–22 Moreover, altered immune response regulation may shift the physiological equilibrium over a chronic-cumulative period, leading to a low-grade inflammatory degenerative process, known as para-inflammation, with the oxidative stress acting as a local trigger for retinal para-inflammatory responses.23
Advances in biotechnology, such as multiplexed flow cytometry assays, may improve our understanding of the pathogenesis and progression of eye diseases.24,25
Antioxidants (AOXs) and anti-inflammatory compounds, such as essential polyunsaturated fatty acids (EPUFAs), may have potential for the treatment of eye diseases. EPUFAs, such as omega-3 (ω-3) and omega-6 (ω-6) fatty acids have important effects in the body. Omega fatty acids provide energy and perform important functions in the body; enhance appropriate prenatal and postnatal development (mainly of the central and peripheral nervous systems), lower cholesterol and triglyceride levels, reduce acute and chronic inflammation, help in the management of emotional distress and depression, benefit patients with neurodegenerative disorders, reduce respiratory and asthma-like symptoms, regulate the blood pressure, and reduce the odds of developing cancer, heart disease, and stroke.26–32 The ω-3-derived eicosanoids exert anti-inflammatory effects, whereas the ω-6-derived eicosanoids are pro-inflammatory.28,30 The regulation of the biochemical mechanisms of acute inflammation, which is at least in part performed by endogenous EPUFA-derived autacoids (including pro-resolving mediators such as lipoxins, resolvins, protectins, and maresins), has recently been the subject of diverse studies.31–38 EPUFAs are expected to be useful molecules for studies of ocular health and disease, including DEDs and POAG.
In this study, our main goals were the following: (1) to assess the expression of IIR molecules in tears of patients diagnosed with DEDs or POAG and (2) to evaluate the effect of oral supplementation with a combined formulation of AOXs and EPUFAs on the signs and symptoms of dry eyes in patients diagnosed with nonsevere DEDs or POAG, by comparing the supplemented DED or POAG groups with the corresponding unsupplemented groups, as well as with healthy controls.
Materials and methods
This prospective, open-label, randomized study was approved by the Institutional Review Board of the University Hospital (Valencia, Spain), as a nonsignificant risk investigational device study (Ethics Committee approved reference 59/10), and all tenets of the Declaration of Helsinki for the protection of human subjects in medical research were strictly observed.
Study design
Using the main inclusion and exclusion criteria (Table 1), we enrolled a total of 97 participants of both sexes, aged 25–80 years, during ophthalmologic appointments at the study centers University and Polytechnic Hospital La Fe (Valencia, Spain), Ophthalmic Research Unit Santiago Grisolia (Valencia, Spain), and Hospital of Jerez (Jerez de la Frontera, Cadiz, Spain), between March 2012 and November 2012.
Table 1.
Main inclusion and exclusion criteria among the study participants
| Inclusion criteria | Exclusion criteria |
|---|---|
| Aged 25–80 years | Aged <20 years, or >80 years |
| Diagnosed of mild-to-moderate | Athopy, allergic disorders |
| DED (DEDG) | Wearing contact lenses |
| Diagnosed of nonsevere POAG (POAGG) | History of refractive surgery |
| Healthy subjects (CG) | Ophthalmic laser treatment (less than 3 months) |
| To be able to participate in the study | Systemic diseases and General Treatments |
| Informed consent | Eyelid anomalies, severe blepharitis or meibomitis, punctal occlusion |
| Ocular disorders and eyedrops other than artificial tears | |
| Not able to participate in the study |
Abbreviations: DED, dry eye disorder; POAG, primary open-angle glaucoma; CG, control group; G, group.
Prior to the baseline visit, participants were required to discontinue, for at least 1 month, use of nutritional supplements, systemic antihistamines, and treatments related to dry eyes (or meibomian gland disorder) such as antibiotics, nonsteroidal and anti-inflammatory drugs, and corticosteroids, as well as artificial tears containing vitamins. In addition, participants were asked to strictly follow the recommendations of the ophthalmologists throughout the duration of study. Ocular lubricants without nutraceuticals were permitted and their use or nonuse was recorded. Antihypertensive eye drops were also allowed and their use or nonuse was also recorded. Patients with obvious infection or significant eyelid inflammation were excluded from the study, as were patients with advanced glaucoma and patients with a previous diagnosis of coexisting POAG and DEDs. We wanted to analyze the ocular surface characteristics and the expression of IIR molecules in tears for two specific groups of patients: those with a diagnosis of a nonsevere DED and those with a diagnosis of nonadvanced POAG.
Suitable participants (97 participants, 194 eyes) were assigned to one of the following groups: (1) patients diagnosed with nonsevere DEDs (DEDG; n = 30), (2) patients diagnosed of nonadvanced POAG (POAGG; n = 31), and (3) a control group of healthy participants (CG; n = 36). Two homogeneous subgroups were selected: one group was prescribed an oral supplement containing AOXs and EPUFAs (AOX/EPUFA, two capsules per day, +S) and the other received no supplement (−NS). The oral supplement was Brudysec 1.5® (Brudy Laboratories, Barcelona, Spain), each capsule of which contains the following components in a combined nutraceutical formulation: docosahexaenoic acid (350 mg), eicosapentaenoic acid (42.5 mg), docosapentaenoic acid (30 mg), vitamin A (133 μg), vitamin C (26.7 mg), vitamin E (4 mg), tyrosine (10.8 mg), cysteine (5.83 mg), glutathione (2 mg), zinc (1.6 mg), copper (0.16 mg), manganese (0.33 mg), selenium (9.17 μg).
Ophthalmologists were instructed to emphasize, during an initial personal interview with each participant, compliance with the oral supplementation regimen, to maximize the effectiveness of the supplements and in turn, the reliability of the study data. After the initial visit, all participants were followed every 4 weeks for a total follow-up period of 3 months.
Participant management
At the beginning of the study, all participants underwent an interview during which information about their personal and familial background and the characteristics of their eye disease (DED or POAG) was collected; emphasis was placed on the signs and symptoms of dry eyes and the participants’ subjective sensations. For each group of participants, the effectiveness of AOX/EPUFA supplementation was evaluated in terms of clinical and molecular changes from baseline to 3 months.
A systematized ophthalmologic examination was conducted on all participants: the examination included measurement of the best corrected visual acuity in each eye, the Schirmer’s test, slit lamp examination of the eye adnexa and anterior eye segment, measurement of tear breakup time (BUT) with fluorescein, and examination of corneal surface details with fluorescein. All of the ophthalmologists were instructed to fill a specifically designed a fullsheath to enclose all data and were advised to strictly follow the study protocol. The primary outcome ophthalmologic measures of the effectiveness of the oral nutraceutical formulation were the Schirmer’s test and fluorescein tear BUT, and the secondary outcome measures were dry eye symptoms and subjective sensations.
Tear sampling
We used the gentle rubbing method to obtain reflex tears from all participants, and we assayed the expression of a specific set of cytokines and chemokines in the tear samples by means of the Luminex® R-200 multiplex system (Luminex, Austin, TX, USA). Polystyrene beads coupled covalently to specifically directed antibodies (human cytokine/chemokine panel) were allowed to react with 30–40 μL of each tear sample containing unknown amounts of cytokines and chemokines, or with a standard solution containing known amounts of cytokines and chemokines, at room temperature for 1 hour, as previously described.39 The specific set of IIR molecules that were determined by means of this assay, as standardized by the manufacturers, were interleukin (IL)-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, and IL-12; tumor necrosis factor alpha (TNF-α); vascular endothelial growth factor (VEGF); granulocyte-macrophage colony-stimulating factor (GM-CSF); and interferon gamma. Briefly, a series of washes were carried out to remove unbound protein. Then a biotinylated detection antibody specific for a different epitope on the cytokine was added to the beads and incubated at room temperature for 30 minutes. Streptavidin-phycoerythrin, which binds to the biotinylated detection antibodies, was used to detect the reaction mixture. We used a flow-based Bio-Plex® suspension array system (Bio-Rad Laboratories, Hercules, CA, USA) to identify and quantify each particular antigen–antibody reaction. Identification of the assayed molecules was based on bead color and fluorescence, using fluorescently labeled reporter molecules associated with each target protein. Unknown cytokine and chemokine concentrations were calculated automatically by the Bio-Plex Manager software using a standard curve derived from a recombinant cytokine standard. Cytokine and chemokine concentrations were corrected for the initial total protein concentration of each human tear sample during analysis.
All the results are shown as means ± standard deviations for two or three determinations and are expressed in picograms per milliliters per milligram.
Statistical procedures
Demographic, clinical, and biochemical data were recorded in a previously designed Excel sheet (Microsoft Corporation, Redmond, WA, USA). A nonparametric Mann–Whitney U-test was selected for comparing two independent sample groups by means of the SPSS software (version 15.0, SPSS Inc, Chicago, IL, USA). All results were statistically analyzed to detect differences between groups. For our purposes, P < 0.05 was established as statistically significant.
Results
The median ages of the participant groups were 52 ± 15 years (DEDG), 64 ± 17 years (POAGG), and 50 ± 12 years (CG). When the participants were aged over 40 years (pivotal risk factor for both the DEDs and POAG) the percentages attending each group were 64% (DEDG), 67% (POAGG), and 60% (CG). Regarding sex, the percentages of men and women in all groups were 28% and 72% (DEDG), 29% and 71% (POAGG), and 32% and 68% (CG) respectively. Patient characteristics and risk factors for DEDs are reflected in the Table 2.
Table 2.
Patient characteristics
| Duration years | MENOP % | DM % | HBP % | CVD % | SEDENT % | SMKING % | DRNKING % | AIR C % | POLLT % | PCU % | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| POAGG | 3 ± 3 | 40 | 28 | 33 | 14 | 40 | 9 | 19 | 29 | 29 | 28 |
| DEDG | 3 + 1 | 56 | 19 | 26 | 11 | 33 | 15 | 11 | 89 | 85 | 86 |
| CG | – | 43 | – | 3 | 3 | 24 | 15 | 11 | 85 | 80 | 23 |
Abbreviations: AIR C, air conditioning exposure; CG, control group; CVD, cardiovascular disorders; DEDG, dry eye disorder group; DM, Diabetes Mellitus; DRNKING, drinking habits; HBP, high blood pressure; MENOP, menopause; PCU, personal computer use; POAGG, primary open-angle glaucoma group; POLLT, pollutants exposure; SEDENT, sedentary lifestyle; SMKING, smoking habits.
All the DEDG patients reported a history of dry eyes before the start of the study; they suffered from at least one of the following signs and symptoms: scratchy sensation, soreness, itchiness, grittiness, foreign body sensation, dryness, burning, photophobia, eye fatigue and/or blurred vision, and redness. Most of the DEDG patients (89%) used eye drops regularly for treating their ocular surface alteration. None of the DEDG patients suffered from severe dryness or Sjögren’s syndrome.
None of the POAGG patients had a previous diagnosis of a DED or used tear substitutes. Of the POAGG patients who were under treatment with antihypertensive drops treatment, 52% reported at least one of the dry eye signs and symptoms listed above for the DEDG patients. The POAGG patients mainly presented with a burning, dryness, photophobia, and/or conjunctival hyperemia, usually in both eyes.
The three groups of participants were examined under a slit lamp in relation to their anterior eye segment, and almost every DEDG patient displayed ocular surface disorder morphological alterations such as marginal blepharitis and stinging of the cornea. Most of the POAGG patients showed DED-related morphological changes (38%). However, neither the interviews nor the ocular surface examination revealed significant DED-related manifestations in the healthy participants.
The Schirmer’s test scores were significantly lower in the DEDG (4.26 ± 0.59 mm) than in the POAGG (7.82 ± 1.92 mm) or the CG (13.25 ± 2.46 mm; P = 0.0002), reflecting the altered tear secretion in both the DEDG and POAGG patients. DEDG and POAGG patients who were younger than 40 normally moistened 7–12 mm of each paper strip with 5 minutes of contacting the paper strip, whereas patients older than 40 usually moistened about 4–9 mm of each strip.
The fluorescein tear BUT was much shorter in the DEDG patients (4.35 ± 1.23 seconds) than in the POAGG and CG patients (6.14 ± 2.32 seconds and 14.24 ± 3.22 seconds, respectively), which strongly reflects the altered tear film stability in the DEDG and the POAGG patients as compared to that in the CG patients (P = 0.0001).
None of the three groups showed significant differences in best corrected visual acuity from baseline to 3 months, and no changes in this parameter was also noticed in the oral supplementation subgroups from pre- to postsupplementation.
Results from the tear-sampling procedure were calculated by subtracting background cytokine and chemokine concentrations from cytokine concentrations in the tear samples. The standard curves for both the kit assay and extraction buffers were similar for the 12 analyzed molecules. The set of assayed molecules showed a wide variety of expression levels in the tear samples, and the precision of the values as measured by the Luminex multianalyte profiling bioassay system was acceptable. The amounts of tear samples obtained from the study participants permitted detection in up to 92% of the samples.
Noticeable increases in the collected amount of tears (30% or more) were observed in the DEDG and POAGG subgroups taking the AOX/EPUFA supplement with respect to the amounts in the same groups not taking the supplement.
Comparison of the results from the DEDG and POAGG patients showed significant differences in tear levels of GM-CSF (P = 0.008), TNF-α (P = 0.005), VEGF (P = 0.038), IL-4 (P = 0.030), and IL-6 (P = 0.044). These results are shown in Figure 1.
Figure 1.
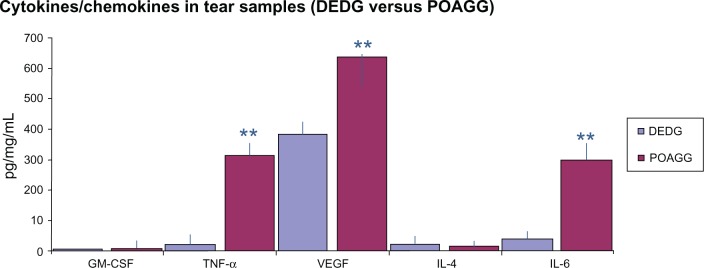
Comparison of the expression of cytokines/chemokines in tears from the DEDG and POAGG patients.
Notes: Data are mean ± standard deviation for three assays. **Indicates a P value < 0.001.
Abbreviations: DEDG, dry eye disorder group; GM-CSF, granulocyte-macrophage colony-stimulating factor; IL-4, interleukin-4; IL-6, interleukin-6; POAGG, primary open-angle glaucoma group; TNF-α, tumor necrosis factor alpha; VEGF, vascular endothelial growth factor.
Comparison of the data for the POAGG and CG patients demonstrated significant differences in the tear levels of IL-6 (P = 0.014) (Figure 2).
Figure 2.
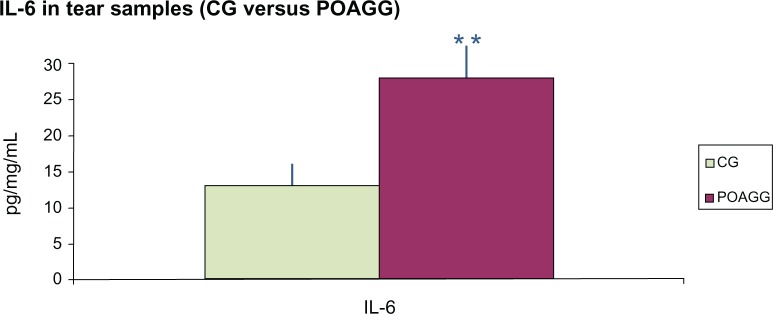
Comparison of the expression of IL-6 in tears from the CG and POAGG patients.
Notes: Data are mean ± standard deviation for three assays. **Indicates a P value < 0.001.
Abbreviations: CG, control group; IL-6, interleukin-6; POAGG, primary open-angle glaucoma group.
The POAGG +S patients showed a significant reduction in the tear concentrations of IL-6 (P = 0.44) and TNF-α (P = 0.00001) compared to the POAGG −NS patients (Figure 3).
Figure 3.
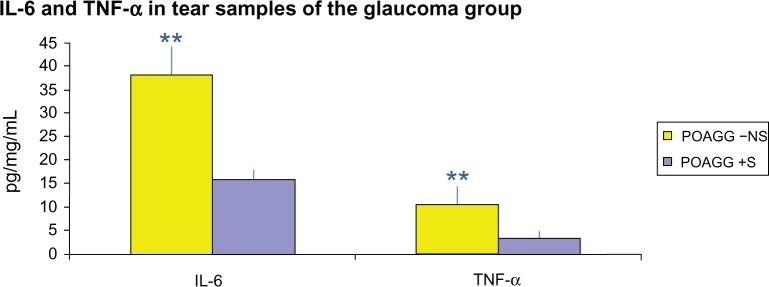
Comparison of the expression of IL-6 and TnF-α in tears from the POAGG +S compared to the POAGG −NS patients.
Notes: Data are mean ± standard deviation for three assays. **Indicates a P value < 0.001.
Abbreviations: IL-6, interleukin-6; POAGG −NS, primary open-angle glaucoma group without oral supplements; POAGG +S, primary open-angle glaucoma group with oral supplements; TNF-α, tumor necrosis factor alpha.
The main signs and symptoms of dry eyes were significantly improved in the DEDG +S and POAGG +S patients compared to the corresponding patients who did not receive the supplement. At 3 months, an overall improvement in both the objective and the subjective manifestations was observed in the DEDG +S patients as compared to the DEDG −NS patients, and in the POAGG +S patients as compared to the POAGG −NS patients. Patients reported amelioration of at least 68% of ocular signs such as dryness, burning, photophobia, eye heaviness, and blurred vision, as well as noticeable improvements in eyelashes, hair, nails and skin.
Discussion
Dry eyes are usually due to environmental irritants and topical or systemic medications.3–5,39,40 Because most patients with glaucoma are not aware of suffering any type of ocular surface disorder, special attention has to be paid to patients with chronic glaucoma who may develop DED signs and symptoms during the course of their treatment. The main goal of this study was to determine whether there were any differences in tear expression of IIR mediators in patients with nonsevere DEDs and patients with POAG as compared to expression in healthy controls. We used the Luminex multianalyte profiling assay system, a new technique that allows simultaneous measurement of various molecules in a single microplate well.41 We also evaluated the effect on patients with POAG or DED of oral supplementation with AOX/EPUFA over the course of 3 months for each group of participants.
Human tears contain a wide spectrum of cytokines and chemokines, the main function of which is to maintain the morphologic and physiologic properties of the ocular surface.41–46 We found that tears collected from patients with DEDG and POAG showed differential expression of the assayed cytokines and chemokines compared to the tears of healthy controls. Specifically, the concentrations of IL-6 and TNF-α were significantly higher in the DEDG and POAGG than in the CG. Other investigators have also detected higher IL-6 and TNF-α levels in the conjunctival epithelium and in tear samples of patients with DEDs.43,47,48 However, it has also been reported that the concentration of IL-6 is not higher in tear samples from patients with moderately dry eyes.49 Because inflammatory processes mediated by cytokines and chemokines are commonly associated with ocular surface disorders, independently of their etiology, our data strongly suggest that the augmented expression of IL-6 and TNF-α in tears is worth noting, because these proinflammatory cytokines are most probably the underlying cause of most clinical manifestations of the ocular surface alterations in both the DEDG and POAGG patients.
Aging is a relevant factor in both DEDs and POAG. When all the participants were assembled as being aged over 40 years, each group (DEDG, POAGG and CG) and subgroup (patients taking or not taking oral supplements) was homogeneous in their percentages.
Percentages of men and women in all groups were 28% and 72% (DEDG), 29% and 71% (POAGG), and 32% and 68% (CG) respectively, reflecting the differences in gender of both diseases in the general population.
Daily dietary intake of EPUFAs (ω-3 and ω-6) is necessary so that they can exert their effects in the body (eg, on the immune system) at both the cellular and the humoral levels.30,31 Furthermore, the ω-3 EPUFA intake and the ω-3 EPUFA/ω-6 EPUFA intake ratio affect the expression of inflammatory biomarkers.50 Therefore, it has been shown that ω-3 EPUFA supplementation can protect the ocular surface in patients at risk of DEDs.33,51–53 In the present work, we determined whether the oral supplementation of a combined formulation of AOXs and EPUFAs (Brudysec 1.5®) influenced the progression of DED, and our data suggest that supplement intake significantly changed the expression patterns of various cytokines and chemokines in tears collected from patients with DEDs or POAG compared to the patterns in the corresponding unsupplemented patients. Other investigators previously reported similar results for AOX and EPUFA supplementation in patients with dry eyes.51–53
Patients with POAG are generally not aware of having ocular surface dysfunction, probably because they do not recognize some of the ocular signs and symptoms. As reported by Gilbard54 other possible causes (and their symptoms) have to be considered for a patient’s chronic eye irritation, as follows: iatrogenic, non-specific ocular irritation, tarsal foreign body, anterior blepharitis, obstruction of the lacrimal drainage system, meibomian gland dysfunction, allergic conjunctivitis, nocturnal lagophthalmos, superior limbic keratoconjunctivitis, superficial punctate Thygenson’s keratitis, dry eyelid skin, normal eyes responding to abnormal environment, and blepharospasm. In these cases, careful questioning and specific clinical examination may reveal that patients are experiencing DED signs and symptoms rather than eye irritation.
All of the DED patients in our study reported a history of dry eyes before starting the study, whereas only half of the patients with POAG suffered symptoms related to dry eyes, mainly dryness, photophobia, burning, or conjunctival hyperemia. Furthermore, examination of the POAG patients revealed significant reductions in Schirmer’s test scores and fluorescein tear BUT compared to those of the controls. In agreement with our data, other authors have also reported that around 60% of patients with POAG have dry eye signs and symptoms.9,10 We speculate that POAG patients needing long-term treatment with antihypertensive eye drops are at risk of developing a DED (or exacerbating a latent DED). The significant role of aging in both DEDs and POAG may increase the probability of POAG and DED comorbidity.55–57 Therefore, we strongly recommend that patients with POAG be carefully evaluated for dry eye symptoms prior to starting any topical antiglaucomatous therapy. Our results suggest that in addition to the use of eye drops to protect the ocular surface, oral supplementation with a combination of AOXs and EPUFAs, such as in the present study (Brudysec 1.5®), should be considered for elderly glaucomatous patients at risk for DEDs.
Footnotes
Disclosure
The authors report no conflicts of interest in this work. Part of this work was presented to the Meeting of the Society of Research in Retina and Visual Sciences (SIRCOVA) in Valencia, Spain (2013).
References
- 1.Caspari R, Lee SH. Is human longevity a consequence of cultural change or modern biology? Am J Phys Anthropol. 2006;129:512–517. doi: 10.1002/ajpa.20360. [DOI] [PubMed] [Google Scholar]
- 2.United Nations, Department of Economic and Social Affairs, Population Division . CD-ROM Edition – Extended Dataset in Excel and ASCII Formats. United Nations publication; World Population Prospects: The 2010 Revision. sales no 11.XIII.7. [Google Scholar]
- 3.Perry HD. Dry eye disease: pathophysiology, classification, and diagnosis. Am J Manag Care. 2008;14(Suppl 3):S79–S87. [PubMed] [Google Scholar]
- 4.Tavares F de P, Fernandes RS, Bernardes TF, et al. Dry eye disease. Semin Ophthalmol. 2010;25:84–93. doi: 10.3109/08820538.2010.488568. [DOI] [PubMed] [Google Scholar]
- 5.Labbé A, Brignole-Baudouin F, Baudouin C. Ocular surface investigations in dry eye. J Fr Ophthalmol. 2007;30:76–97. doi: 10.1016/s0181-5512(07)89557-x. [DOI] [PubMed] [Google Scholar]
- 6.Kwon YH, Fingert JH, Kuehn MH, Alward WL. Primary open-angle glaucoma. N Engl J Med. 2009;360(11):1113–1124. doi: 10.1056/NEJMra0804630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munoz B, West SK, Rubin GS, et al. Causes of blindness and visual impairment in a population of older Americans: The Salisbury Eye Evaluation Study. Arch Ophthalmol. 2000;118:819–825. doi: 10.1001/archopht.118.6.819. [DOI] [PubMed] [Google Scholar]
- 8.Friedman DS, Wolfs RC, O’Colmain BJ, et al. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122(4):532–538. doi: 10.1001/archopht.122.4.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai JH, Derby E, Holland EJ, Khatana AK. Incidence and prevalence of glaucoma in severe ocular surface disease. Cornea. 2006;25(5):530–532. doi: 10.1097/01.ico.0000220776.93852.d9. [DOI] [PubMed] [Google Scholar]
- 10.Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350–355. doi: 10.1097/IJG.0b013e31815c5f4f. [DOI] [PubMed] [Google Scholar]
- 11.Halliwell B. Free radicals and antioxidants: Updating a personal view. Nutr Rev. 2012;70:257–265. doi: 10.1111/j.1753-4887.2012.00476.x. [DOI] [PubMed] [Google Scholar]
- 12.Zanon-Moreno V, Marco-Ventura P, Lleó-Perez AV, et al. Oxidative stress in primary open-angle glaucoma. J Glaucoma. 2008;17:263–268. doi: 10.1097/IJG.0b013e31815c3a7f. [DOI] [PubMed] [Google Scholar]
- 13.Pinazo-Durán MD, Zanon-Moreno V, Garcia-Medina JJ, Gallego-Pinazo R. Evaluation of presumptive biomarkers of oxidative stress, immune response and apoptosis in primary open-angle glaucoma. Current Opin Pharmacol. 2013;13(1):98–107. doi: 10.1016/j.coph.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Berthoud VM, Beyer EC. Oxidative stress, lens gap junctions, and cataracts. Antioxid Redox Signal. 2009;11:339–353. doi: 10.1089/ars.2008.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia-Medina JJ, Pinazo-Durán MD, Garcia-Medina M, et al. Antioxidant supplementation on diabetic retinopathy over a 5-year follow-up period. Eur J Ophthalmol. 2011;21:637–643. doi: 10.5301/EJO.2010.6212. [DOI] [PubMed] [Google Scholar]
- 16.Mancino R, Di Pierro D, Varesi C, et al. Lipid peroxidation and total antioxidant capacity in vitreous, aqueous humor, and blood samples from patients with diabetic retinopathy. Mol Vis. 2011;17:1298–1304. [PMC free article] [PubMed] [Google Scholar]
- 17.Suzuki M, Tsujikawa M, Itabe H, et al. Chronic photo-oxidative stress and subsequent MCP-1 activation as causative factors for age-related macular degeneration. J Cell Sci. 2012;125:2407–2415. doi: 10.1242/jcs.097683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medzhitov R, Janeway C., Jr Innate immunity. N Engl J Med. 2000;343:338–344. doi: 10.1056/NEJM200008033430506. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki M, Tsujikawa M, Itabe H, et al. Chronic photo-oxidative stress and subsequent MCP-1 activation as causative factors for age-related macular degeneration. J Cell Sci. 2012;125:2407–2415. doi: 10.1242/jcs.097683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zoukhri D. Effect of inflammation on lacrimal gland function. Exp Eye Res. 2006;82:885–898. doi: 10.1016/j.exer.2005.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krabbe KS, Pedersen M, Bruunsgaard H. Inflammatory mediators in the elderly. Exp Gerontol. 2004;39:687–699. doi: 10.1016/j.exger.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 22.Stevenson W, Chauhan SK, Dana R. An immune-mediated ocular surface disorder. Arch Ophthalmol. 2012;130:90–100. doi: 10.1001/archophthalmol.2011.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu H, Chen M, Forrester JV. Para-inflammation in the aging retina. Prog Retin Eye Res. 2009;28:348–368. doi: 10.1016/j.preteyeres.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Yoshida N, Ikeda Y, Notomi S, et al. Laboratory evidence of sustained chronic inflammatory reaction in retinitis pigmentosa. Ophthalmology. 2013;120(1):e5–e12. doi: 10.1016/j.ophtha.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 25.Gallego-Pinazo R, Marsiglia M, Mrejen S, et al. Outer retinal tubulations in chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2012 doi: 10.1007/s00417-012-2151-0. [DOI] [PubMed] [Google Scholar]
- 26.Swenor BK, Bressler S, Caulfield L, et al. The impact of fish and shellfish consumption on age-related macular degeneration. Ophthalmology. 2010;117:2395–2401. doi: 10.1016/j.ophtha.2010.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chong EWT, Kreis AJ, Wong JY, et al. Dietary ω-3 fatty acid and fish intake in the primary prevention of age-related macular degeneration: a systematic review and meta-analysis. Arch Ophthalmol. 2008;126:826–833. doi: 10.1001/archopht.126.6.826. [DOI] [PubMed] [Google Scholar]
- 28.Licinio J, Wong ML. The role of inflammatory mediators in the biology of major depression: Central nervous system cytokines modulate the biological substrate of depressive symptoms, regulate stress-responsive systems, and contribute to neurotoxicity and neuroprotection. Mol Psychiatry. 1999;4:317–327. doi: 10.1038/sj.mp.4000586. [DOI] [PubMed] [Google Scholar]
- 29.Ren H, Magulike N, Ghebremeskel K, et al. Primary open-angle glaucoma patients have reduced levels of blood docosahexaenoic and eicosapentaenoic acids. Prostaglandins Leukot Essent Fatty Acids. 2006;74:157–163. doi: 10.1016/j.plefa.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Pinazo-Durán MD, Boscá-Gomar L. Anti-inflammatory properties of essential fatty acids. Editorial. Arch Soc Esp Oftalmol. 2012;87:203–205. doi: 10.1016/j.oftal.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 31.Sapieha P, Stahl A, Chen J, et al. 5-Lipoxygenase metabolite 4-HDHA is a mediator of the antiangiogenic effect of ω-3 polyunsaturated fatty acids. Sci Transl Med. 2011;3:69ra12. doi: 10.1126/scitranslmed.3001571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenberg ES, Asbell PA. Essential fatty acids in the treatment of dry eye. Ocul Surf. 2010;8:18–28. doi: 10.1016/s1542-0124(12)70214-8. [DOI] [PubMed] [Google Scholar]
- 33.Pinazo-Durán MD, Galbis-Estrada C, Cantu-Dibildox J, Pons-Vazquez S, Benítez-del-Castillo J. Effects of a nutraceutical formulation based on the combination of antioxidants and ω-3 essential fatty acids in the expression of inflammation and immune response mediators in tears from patients with dry eye disorders. Clin Int Aging. 2013;8:1–10. doi: 10.2147/CIA.S40640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roncone M, Bartlett H, Eperjesi F. Essential fatty acids for dry eye: a review. Cont Lens Anterior Eye. 2010;33:49–54. doi: 10.1016/j.clae.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 35.Brignole-Baudouin F, Baudouin C, Aragona P, et al. A multicentre, double-masked, randomized, controlled trial assessing the effect of oral supplementation of omega-3 and omega-6 fatty acids on a conjunctival inflammatory marker in dry eye patients. Acta Ophthalmol. 2011;89:e591–e597. doi: 10.1111/j.1755-3768.2011.02196.x. [DOI] [PubMed] [Google Scholar]
- 36.Rand AL, Asbell PA. Nutritional supplements for dry eye syndrome. Curr Opin Ophthalmol. 2011;22:279–282. doi: 10.1097/ICU.0b013e3283477d23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cortina MS, Bazan HE. Docosahexaenoic acid, protectins and dry eye. Curr Opin Clin Nutr Metab Care. 2011;14:132–137. doi: 10.1097/MCO.0b013e328342bb1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li N, He J, Schwartz CE, et al. Resolvin E1 improves tear production and decreases inflammation in a dry eye mouse model. J Ocul Pharmacol Ther. 2010;26:431–439. doi: 10.1089/jop.2010.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264–1268. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 40.Baudouin C. A new approach for better comprehension of diseases of the ocular surface. J Fr Ophthalmol. 2007;30:239–246. doi: 10.1016/s0181-5512(07)89584-2. [DOI] [PubMed] [Google Scholar]
- 41.VanDerMeid KR, Su SP, Krenzer KL, et al. A method to extract cytokines and matrix metalloproteinases from Schirmer strips and analyse using Luminex. Mol Vis. 2011;17:1056–1063. [PMC free article] [PubMed] [Google Scholar]
- 42.Enríquez-de-Salamanca A, Castellanos E, Stern ME, et al. Tear cytokine and chemokine analysis and clinical correlations in evaporative-type dry eye disease. Mol Vis. 2010;16:862–873. [PMC free article] [PubMed] [Google Scholar]
- 43.Baudouin C, Brignole F, Becquet F, et al. Flow cytometry in impression cytology specimens: a new method for evaluation of conjunctival inflammation. Invest Ophthalmol Vis Sci. 1997;8:1458–1464. [PubMed] [Google Scholar]
- 44.Vignali DA. Multiplexed particle-based flow cytometric assays. J Immunol Methods. 2000;243:243–255. doi: 10.1016/s0022-1759(00)00238-6. [DOI] [PubMed] [Google Scholar]
- 45.Massingale ML, Li X, Vallabhajosyula M, et al. Analysis of inflammatory cytokines in the tears of dry eye patients. Cornea. 2009;28:1023–1027. doi: 10.1097/ICO.0b013e3181a16578. [DOI] [PubMed] [Google Scholar]
- 46.Brignole F, Pisella PH, Goldschild M, et al. Flow cytometric analysis of inflammatory markers in conjunctival epithelial cells of patients with dry eyes. Invest Ophthalmol Vis Sci. 2001;4:1356–1363. [PubMed] [Google Scholar]
- 47.Higuchi A, Kawakita T, Tsubota K. IL-6 induction in desiccated corneal epithelium in vitro and in vivo. Mol Vis. 2011;17:2400–2406. [PMC free article] [PubMed] [Google Scholar]
- 48.Boehm N, Riechardt AI, Wiegand M, Pfeiffer N, Grus FH. Proinflammatory cytokine profiling of tears from dry eye patients by means of antibody microarrays. Invest Ophthalmol Vis Sci. 2011;52:7725–7730. doi: 10.1167/iovs.11-7266. [DOI] [PubMed] [Google Scholar]
- 49.Narayanan S, Miller WL, McDermott AM. Conjunctival cytokine expression in symptomatic moderate dry eye subjects. Invest Ophthalmol Vis Sci. 2006;47:2445–2450. doi: 10.1167/iovs.05-1364. [DOI] [PubMed] [Google Scholar]
- 50.Hibbeln JR, Nieminen LRG, Blasbalg TL, Riggs JA, Lands WEM. Healthy intakes of n-3 and n-6 fatty acids: estimations considering worldwide diversity. Am J Clin Nutrition. 2006;83:1483S–1493S. doi: 10.1093/ajcn/83.6.1483S. [DOI] [PubMed] [Google Scholar]
- 51.Sullivan BD, Cermak JM, Sullivan RM, et al. Correlations between nutrient intake and the polar lipid profiles of meibomian gland secretions in women with Sjogrens syndrome. In: Sullivan D, et al., editors. Lacrimal Gland, Tear Film, and Dry Eye Syndrome. Kluwer Academic/Plenum Publishers; 2002. pp. 441–447. [DOI] [PubMed] [Google Scholar]
- 52.Chia EM, Mitchell P, Rochtchina E, et al. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Experiment Ophthalmol (Australia) 2003;31:229–232. doi: 10.1046/j.1442-9071.2003.00634.x. [DOI] [PubMed] [Google Scholar]
- 53.Miljanović B, Trivedi KA, Dana MR, Gilbard JP, Buring JE, Schaumberg DA. Relation between dietary n-3 and n-6 fatty acids and clinically diagnosed dry eye syndrome in women. Am J Clin Nutr. 2005;82:887–893. doi: 10.1093/ajcn/82.4.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gilbard J P.Dry Eye Disorders Albert DM, Jakobiec FA.Principles and Practice of Ophthalmology Philadelphia: WB Saunders Company; 1994257–276. [Google Scholar]; Schein OD, Munoz B, Tielsch JM, et al. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124:723–728. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- 55.Rossi GC, Tinelli C, Pasinetti GM, et al. Dry eye syndrome-related quality of life in glaucoma patients. Eur J Ophthalmol. 2009;19:572–579. doi: 10.1177/112067210901900409. [DOI] [PubMed] [Google Scholar]
- 56.Rüfer F, Erb C. Influence of dry eye syndrome on glaucoma diagnostic procedures. Ophthalmologe. 2012;109:1082–1086. doi: 10.1007/s00347-012-2640-x. [DOI] [PubMed] [Google Scholar]
- 57.Labbé A, Terry O, Brasnu E, Van Went C, Baudouin C. Tear film osmolarity in patients treated for glaucoma or ocular hypertension. Cornea. 2012;31:994–999. doi: 10.1097/ICO.0b013e31823f8cb6. [DOI] [PubMed] [Google Scholar]


