Abstract
Premature infants are at increased risk for poor health, feeding difficulties, and impaired mother-infant interaction leading to developmental delay. Social-environmental risks, such as poverty or minority status, compound these biologic risks, placing premature infants in double jeopardy. Guided by an ecological model, the Hospital-Home Transition: Optimizing Prematures’ Environment (H-HOPE) intervention combines the Auditory, Tactile, Visual, and Vestibular intervention with participatory guidance provided by a nurse and community advocate to address the impact of multiple risk factors on premature infants’ development.
Keywords: Ecologic model, Premature infant development, Developmental intervention, Health disparities, Multiple social-environmental risks, Home visitors
The biologic risk of prematurity (34 weeks or less gestation at birth) is associated with feeding and mother-infant interaction difficulties, higher rates of chronic and acute morbidities, developmental delays, and behavioral problems. These ongoing health problems contribute to lower childhood IQ, limited academic achievement, longer hospitalizations, and increased health care costs (Bhutta, Cleves, Casey, Cradock, & Anand, 2002; Davis, Edwards, & Mohay, 2003; de Kleine et al., 2003; McGrath & Sullivan, 2002; Muller-Nix et al., 2004; O’Brien et al., 2004; Parker, Greer, & Zuckerman, 1988; Saigal et al., 2003; Stoelhorst et al., 2003; Talmi & Harmon, 2003). Premature infants born into families with multiple social-environmental risks face double jeopardy (Parker et al., 1988). When biological risks are combined with social-environmental risk factors, premature infants experience lower quality parenting (e.g., less maternal responsiveness), less optimal early health and development, greater behavioral problems, and lower achievement during later childhood (Bendersky & Lewis, 1994; Bradley et al., 1994; Burchinal, Roberts, Zeisel, Hennon, & Hooper, 2006; Duncan, Huston, & McLoyd, 1998; Malat, Oh, & Hamilton, 2005; Saigal et al., 2003; Sameroff, Seifer, Baldwin, & Baldwin, 1993). Premature infants appear to be especially vulnerable to social-environmental risks such as poverty, minority status, or low education (Bradley et al; Parker, Zahr, Cole, & Brecht, 1992), and these risks compound the biologic risks of prematurity, further compromising premature infant health and development. Developing effective interventions that focus on mother-premature infant dyads at high social-environmental risk has the potential to ameliorate the detrimental effects of these multiple risk factors. The challenge of transitioning premature infants to oral feeding and ensuring that their mothers are prepared for the specific needs of these infants has not been comprehensively addressed. Few interventions have focused on improving both infant feeding and mother-infant interaction for this at-risk population.
CALLOUT 1
This article summarizes previous research on premature infants at social-environmental risk and describes the ecologic model of infant development, which provides a conceptual framework for intervening to meet the needs of mother-premature infant dyads. A unique new intervention is presented that is currently being tested and offers an integrated approach to address needs identified in previous research.
Biologic Risk of Prematurity Affects Behavioral Organization and Feeding
An infant’s behavioral organization is a reflection of central nervous system integrity and defines the brain’s potential to develop normally (Als et al., 2004; Medoff-Cooper, McGrath, & Bilker, 2000). Well established indicators of behavioral organization include infant behavioral state, behavioral cues (pre-feeding, engagement, and disengagement cues), and sucking organization (Als et al.; Medoff-Cooper & Ratcliffe, 2005). Alterations in behavioral organization include a lower capacity for self-regulation, less behavioral alertness, hypersensitivity to stimulation (Als et al.; Feldman & Eidelman, 2006; White-Traut, Nelson, Silvestri, Cunningham, & Patel, 1997), and poorer oral feeding. Inefficient oral feeding in turn demands substantial energy expenditure from the infant, delays hospital progression, and increases health care costs. It is not until 32-34 weeks that the breathing, sucking, and swallowing mechanisms become functionally coordinated (Medoff-Cooper, 2006); prior to this point the infant is predisposed to to apneic events, bradycardia, oxygen desaturation and fatigue during feeding (Lau, Smith, & Schanler, 2003; McGrath & Medoff-Cooper, 2001).
A premature infant’s level of arousal is related to sucking characteristics (Crook, 1979), and it has been hypothesized that successful oral feeding is preceded by an alert behavioral state (White-Traut, Berbaum, Lessen, McFarlin, & Cardenas, 2005). A relationship between alert behavioral states and nipple feeding success in premature infants has been reported (White-Traut et al., 2002a), and slight arousal encourages the infant to enter an alert, awake state. However, conflicting evidence of this relationship has also been reported (Medoff-Cooper et al., 2000). These differences in results reveal the challenges of measuring premature infants’ behavioral state during feedings.
Additional factors are known to affect oral feeding success. An infant’s biologic health, central nervous system maturation, behavioral state and feeding experience have all been shown to affect the quality of nutritive sucking (McCain, 1997; Medoff-Cooper et al., 2000; Pickler, Best, Reyna, Gutcher, & Wetzel, 2006). Pickler and colleagues (2006) found a premature infant’s previous oral feeding experience to have the most significant effect on the features of sucking.
Feeding is critically important because it involves mother-infant interaction and is a primary factor affecting infant growth (Pridham, Saxe, & Limbo, 2004). As such, it is a major concern for both clinicians and parents during the transition to full oral feeding through discharge to home (Pridham et al., 2006). Premature infants’ behavioral cues are subtle, less differentiated, and difficult for caregivers unfamiliar with premature infant behaviors to perceive correctly (White-Traut et al., 2002b). Most early mother-infant interactions occur in the context of feeding and infant feeding difficulties make these early interactions highly stressful with potentially negative consequences for the infant and the mother (Barnard, 1997; Barnard et al., 1988; Davis et al., 2003; Feldman, Keren, Gross-Rozval, & Tyano, 2004).
Needs of Mothers of Premature Infants
Emotional Challenges
Mothers may experience high stress, anxiety, and depression related to their infants’ prematurity and the alteration of their early mothering experience (Feldman & Eidelman, 2006; Holditch-Davis, Bartlett, Blickman, & Miles, 2003; Holditch-Davis & Miles, 2000; Lucarelli, Ambruzzi, Cimino, D’Olimpio, & Finistrella, 2003; Mew, Holditch-Davis, Belyea, Miles, & Fishel, 2003). Postpartum depression, which peaks at 6 weeks post delivery, can occur in up to 10% of new mothers of premature infants (Martins & Gaffan, 2000), and almost half of all mothers of premature infants report depressive symptoms (Mew et al.). Mothers also express a high need for education and support for infant care and feeding during hospitalization and the transition to home (Holditch-Davis et al., 2003; Mew et al.; Pridham et al., 2004).
One source of maternal stress is the premature infant’s immature behavioral organization and unclear behavioral cues which may reduce the mother’s ability to recognize and respond to the infant’s behaviors. This may lead to decreased confidence in her ability to provide infant care, and as a result the mother’s perceptions of her infant may be negatively altered, increasing the risk of anxiety and maladaptive mother-infant interaction. High anxiety also decreases the mother’s capacity for learning and performance, exacerbating difficulties in learning to respond appropriately to the infant (Holditch-Davis et al., 2003; Pridham et al., 2004).
Parenting difficulties
High maternal anxiety and/or depression are related to difficulty in parenting, negative mother-infant interaction, and poor child health and development (Carter, Garrity-Rokous, Chazan-Cohen, Little, & Briggs-Gowan, 2001; Crittenden, Kim, Watanabe, & Norr, 2002; Feldman & Eidelman, 2006; Petterson & Albers, 2001; Pridham, Lin, & Brown, 2001; Singer et al., 2003). Repeated negative perceptions of the infant can further limit a mother’s capacity to respond appropriately, thus disrupting the development of appropriate mother-infant interactions (Coyl, Roggman, & Newland, 2002; Pridham et al.). Over time, lack of responsivity, sensitivity, maternal growth fostering, and contingency behaviors during interactions lead to poorer infant growth and development (Feldman & Eidelman, 2006; Feldman et al., 2004) and continued perception of child vulnerability (Miles & Holditch-Davis, 1997).
Contingency behavior is the ability of the mother and the infant to change their behavior based on the partner’s response during an interaction. Contingency allows the infant to learn about his/her environment and how to interact with it and to learn about predictability and the relationship of environmental stimuli to their behavior (Blackburn, 1983). Contingency behaviors during intervention is a favorable approach because it provides opportunities for infants to interact with their environment, learn about predictability and the relationship of environmental stimuli to their behavior. If the infant shows signs of distress or irritability, the intervention is modulated to optimize individual behavioral response.
Mother-Premature Infant Interaction Difficulties
Positive mother-infant interactions help establish social competency and secure attachment essential for later social, language, and cognitive development (Barnard, 1997). Positive interactions are characterized by maternal sensitivity to cues, responsiveness, social-emotional and cognitive growth fostering infant clarity of cues, responsiveness to caregiver, and greater mother-infant contingency. Contingent behaviors are critical to optimal patterns of interaction, providing opportunities for infants to learn about the predictability and responsiveness of their early relationships (Barnard, 1997; Cusson, 2003).
CALLOUT 2
Mothers of premature infants often respond inappropriately to their infants’ behaviors, have less positive mother-infant interaction scores and less contingency (Barnard, Bee, & Hammond, 1984; Magill-Evans & Harrison, 2001; Miles & Holditch-Davis, 1997; Singer et al., 2003). Initially mothers respond by overstimulating their infants, resulting in a negative response from the infants and leading to maladaptive patterns of behavior in which the mother either continues her non-contingent overstimulation or decreases her stimulation in spite of infant readiness cues (Barnard et al.; Holditch-Davis, Miles, & Belyea, 2000). Mother-infant interaction can be improved by addressing the mother’s emotional stress, modifying behavioral dynamics during interaction, and improving the mother’s understanding of her infant’s immature behavioral organization.
Multiple Social-Environmental Risks Compound the Need for Intervention
A strong body of research has linked maternal, familial, and neighborhood social-environmental risk factors with less optimal early health and development, more behavioral problems and lower achievement. The impact of these risk factors on infant development is magnified in premature infants (Bendersky & Lewis, 1994; Bradley et al., 1994; Burchinal et al., 2006; Malat et al., 2005; McGauhey, Starfield, Alexander, & Ensminger, 1991; Murry et al., 2004). For example, premature infants reared in poverty have three times the rate of school failure than children from high income families, while full term infants reared in poverty have only twice the rate of school failure (McGauhey et al., 1991). Bradley and colleagues’ (1994) classic study examined performance in growth, health, and cognitive and social development and found only 26 (11%) of 243 three year olds born prematurely and living in poverty functioned in the normal range for all four of these outcomes.
Maternal, Family, and Neighborhood Risk Factors
Maternal minority status is associated with socio-economic disadvantage, health disparities, racism, anti-immigrant sentiments, and language barriers (Bradley et al., 2001; Brousseau, Hoffmann, Yauck, Nattinger, & Flores, 2005; Malat et al., 2005; Murry et al., 2004; Shi & Stevens, 2005; Simpson et al., 2005). Younger maternal age and less education are often associated with more negative parenting behaviors and poorer child outcomes (Barnard et al., 1988; Booth, Mitchell, Barnard, & Spieker, 1989). Mothers with multiple environmental stressors experience mental health problems including anxiety and postpartum and chronic depressive symptoms, all associated with lower quality parenting and child behavior problems (Brooten et al., 1988; Carter et al., 2001; Coyl et al., 2002; Petterson & Albers, 2001). Lack of social support has had a consistent negative impact on parenting leading to less favorable maternal and infant outcomes (Caldwell, Antonucci, Jackson, Wolford, & Osofsky, 1997; Hess, Papas, & Black, 2002; Zahr, 1991).
Family poverty, income loss, or continuing financial strains are associated with negative emotions, greater interpersonal stress, and harsher parenting (Chase-Lansdale, Gordon, Brooks-Gunn, & Klebanov, 1997). Poverty is widely recognized as one of the most potent risk factors (Bugental & Happaney, 2004; National Institute of Child Health and Human Development Early Child Care Research Network, 2005; Slack, Holl, McDaniel, Yoo, & Bolger, 2004), and neighborhoods with high levels of poverty, stress, violence and lack of supportive services also negatively affect mothers and families, which indirectly affects infants (Chase-Lansdale et al.; Duncan et al., 1998).
Family factors may have both positive and negative affects. More children in the household or a child younger than two reduces the amount of time and attention available for the infant. Larger households have more activity and noise in the home, which can be especially stressful for the premature infant (Bradley et al., 1994; Sameroff & Fiese, 2000). However, other family factors may have a positive, protective effect. For example, in many Latino and African American families, other adults, especially a co-resident grandmother, may play a significant role in both direct infant care and guidance to the mother, thus augmenting the resources available to both mother and infant (Caldwell et al., 1997; Chase-Lansdale et al., 1997).
Total Social-Environmental Risks
Premature infants’ risk for poorer health, development, and behavioral problems increases significantly when two or more social-environmental risk factors are present (Bradley et al., 1994; Sameroff & Fiese, 2000). In the classic Rochester Longitudinal Study by Sameroff, Seifer, Zax and Barocas (1987), the percentage of children with below average intelligence and social competency scores did not differ for children with 0-1 risk factors but substantially increased at each risk level from 2-5 factors and continued to increase at a slower rate for children with 6-8 factors.
Risk Factors are Mediated by Parenting
Many negative effects of social-environmental risk factors are compounded by less maternal responsiveness, lower quality of parenting, and the home environment (Bradley et al., 2001; Bradley et al., 1994; Brooks-Gunn, Klebanov, & Liaw, 1995; Carter et al., 2001; Duncan et al., 1998; Poehlmann & Fiese, 2001; Pridham et al., 2006; Pridham et al., 2004; Schiffman, Omar, & McKelvey, 2003). For premature infants, less positive social environments are associated with a higher incidence of failure to thrive (Herrenkohl, Herrenkohl, Rupert, Egolf, & Lutz, 1995). The mediating role of parenting is important for intervention, since parenting is easier to change than the larger environment.
Sameroff’s Ecologic Model of Infant Development
The challenges faced by mother-premature infant dyads at both biologic and social-environmental risk can be addressed using Sameroff’s Transactional Model (Sameroff & Fiese, 2000; Sameroff & Mackenzie, 2003). In the Transactional Model, child development is a product of continuous, dynamic and bi-directional interactions between the child, mother, family, and neighborhood. For infants, the most direct influences occur in the immediate parenting environment, especially during interactions with the mother (Nursing Child Assessment Satellite Training Program, 1990). Early transactions set the stage for later relationships so that early disturbances in infant behaviors, maternal perceptions, and mother-infant interactions can have lasting consequences (Sameroff & Fiese, 2000; Sameroff & Mackenzie, 2003).
To improve outcomes for mother-infant dyads, Sameroff and Feise recommended that interventions include one or more of three basic strategies: remediation, redefinition, and re-education (2000). The authors incorporated these three strategies in this intervention to improve premature infants’ feeding. Remediation focuses on changing the infant’s behavioral capacity including behavior toward the parent prior to and immediately after feeding. Redefinition focuses on changing the parent’s attitudes and interpretations about the child’s behaviors. Re-education focuses on changing the parent’s behaviors toward the infant. Previous research on premature infants and mothers has either focused on infant remediation during hospitalization or maternal redefinition and re-education post-discharge.
Interventions for premature infants have concentrated on supporting the continuing development of the nervous system, presumably by facilitating the development of the primary sensory pathways that first develop in the fetus (Als et al., 2004; Burns, Cunningham, White-Traut, Silvestri, & Nelson, 1994; Lekskulchai & Cole, 2001; White-Traut & Nelson, 1988; White-Traut et al., 1997; White-Traut et al., 2002a; White-Traut et al., 2002b). In contrast to tactile stimulation only, multi-sensory intervention for premature infants consistently demonstrates significant improvement in behavioral organization (more alert behavioral states and pre-feeding behaviors), more rapid progression from full gavage to full oral feedings, greater weight gain, improved development, and shortened hospital stay, making it superior to single modality stimulation for promotion of self-regulation (White-Traut & Nelson, 1988; White-Traut et al., 1997).
Previous interventions for mothers have generally combined redefinition and re-education. Short-term, in-hospital interventions with mothers have reduced maternal anxiety, lowered parenting stress, and improved parent-infant interactions and related parenting outcomes (Davis et al., 2003; Kaaresen, Ronning, Ulvund, & Dahl, 2006; Parker et al., 1992). Another hospital-based intervention demonstrated to mothers how to modulate their premature infant’s state (e.g., to alertness before feeding) and was effective for mothers with a high level of education. However, only the in-hospital component followed by participatory guidance at home was effective in improving interaction for less educated mothers (Kang et al., 1995). Other research has demonstrated home visits by a nurse allows safe and cost-effective, early hospital discharge of full term and premature infants (Brooten et al., 1986; Nacion, 1988; Norr, Nacion, & Abramson, 1989).
Maternal redefinition and re-education through extended home visits has been shown to improve full-term infant health and developmental outcomes, including infants in families at high social-environmental risk (Barnard et al., 1988; Olds et al., 1999; Ramey & Ramey, 1998). A nurse home-visiting program focusing on first-time mothers with multiple social-environmental risks, replicated in three different cities, has had remarkable success in improving maternal life course (economic achievement and subsequent pregnancy reduction), parental care (fewer injuries and ingestions), and child outcomes (better emotional and language development, and more positive behaviors) (Olds, 2006; Olds, Henderson, Kitzman, Eckenrode, & Tatelbaum, 1998; Olds et al., 2004). A less intensive program of home visits by a nurse-community health advocate team improved infant mental development for African-Americans only and increased maternal life skills for Latinas only (Norr et al., 2003). Two recent meta-analyses have found that early interventions for parents were effective in increasing maternal sensitivity (Bakermans-Kranenburg, van IJzendoorn, & Juffer, 2003) and in improving the home environment for the young child (Bakermans-Kranenburg, van IJzendoorn, & Bradley, 2005). Importantly, home based intervention with a limited number of sessions was more effective (Bakermans-Kranenburg et al., 2005).
Home visits for maternal redefinition and re-education have also improved premature infant health and developmental outcomes (Barnard, 1997; Barrera, Kitching, Cunningham, Doucet, & Rosenbaum, 1990; Casiro et al., 1993; Kang et al., 1995; McCormick et al., 2006; Olds, 2006; Parker et al., 1992). However, the results have been less consistent for premature infants, and several studies have failed to document improved outcomes for premature infants from mixed racial-ethnic populations with multiple social-environmental risks (Barkauskas, 1983; Bryant & Maxwell, 1997; Siegel, Bauman, Schaefer, Saunders, & Ingram, 1980; Zahr, 2000). The largest intervention for premature infants, the Infant Health and Development Project, begun 20 years ago, included both early home visits and developmentally based center care through age 3. The impact of the intervention differed by birth weight. Compared to a control group, heavier infants (greater than 2000 gms) had higher cognitive achievement and fewer behavioral problems from age 3 – 18 (McCormick et al., 2006). Infants who weighed more than2000 gms showed gains at age 3 but not after age 5 (McCormick et al., 2006).
In addition to home visiting, using adult learning and behavioral change theory to improve techniques for maternal redefinition and re-education is a major conceptual advance. Participatory guidance (Rogoff, Mistry, Goncu, & Mosier, 1993) or interactional coaching models of instruction (Stern-Bruschweiler & Stern, 1989) have been shown to improve health care management and interactional skills for adolescent mothers, mothers of premature infants, and mothers who are depressed (Horowitz et al., 2001; Kang et al., 1995; Lawhon, 2002; Limbo, Petersen, & Pridham, 2003; Pridham et al., 2006; Rogoff et al., 1993). Pridham found that poverty negatively affects the development of positive maternal affect and behavior while contributing to an increase in negative maternal affect and behavior (Pridham et al., 2005). In contrast, guided participation positively contributed to premature infants’ and mothers’ feeding competencies and the regulation of their negative affect and behavior (Pridham et al., 2005).
H-HOPE Intervention
To address the issues identified in previous research, the authors developed the Hospital-Home Transition: Optimizing Prematures’ Environment H-HOPE) Intervention for mother-premature infant dyads. This intervention is unique because it provides an integrated approach that addresses three gaps identified in previous research. The target group for the intervention is mother-premature infant dyads at high risk of suboptimal outcomes who seldom receive intervention. The time of the intervention focuses on a critical transition period for the mother-premature infant dyad. The content of the intervention simultaneously addresses both the infant’s and mother’s needs.
CALLOUT 3
Target Group
The target group for the H-HOPE Intervention is mother-premature infant dyads where the infant is born between 29-34 weeks gestation without serious complications. These mother-infant dyads also have two or more social-environmental risk factors identified in previous research as being associated with negative outcomes (Sameroff, Seifer, Zax, & Barocas, 1987). While otherwise healthy premature infants born at these gestational ages are capable of normal development, when multiple social-environmental risk factors are present, premature infants are at high risk for suboptimal growth and developmental problems (Bradley et al., 1994; McGauhey et al., 1991; Sameroff et al., 1987). This group is especially likely to benefit from early intervention, but currently few interventions are tailored to their specific needs.
Timing
The H-HOPE intervention is provided from 32-34 weeks gestational age through 4 weeks corrected age. This critical period encompasses infant transition from gavage to oral feeding, mother-infant transition to home, and change from hospital to outpatient providers. The transition to oral feeding challenges the premature infant to maintain more alert states while coordinating breathing, sucking, and swallowing. The infant’s degree of success during this time also influences the mother, as the infant’s ability to interact with her is also developing. This is a period that mothers of premature infants have consistently identified as a time when they would benefit from ongoing support (Holditch-Davis & Miles, 2000; Holditch-Davis et al., 2000; Kang et al., 1995; Pridham et al., 2005).
Content
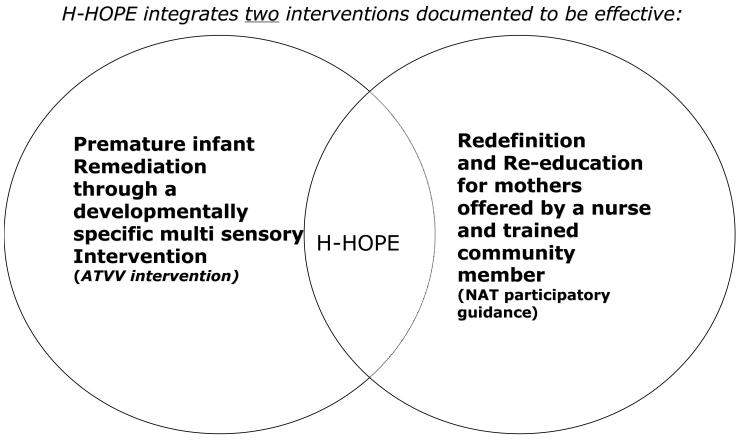
The content of the H-HOPE Intervention, based on Sameroff’s Transactional Model, integrates two different, early interventions into one to provide remediation for the infant and redefinition and re-education for the mother using visits by a Nurse-Community Advocate Team (NAT) (a registered nurse). Both interventions have been documented to be effective in previous research. A developmentally-specific multi-sensory intervention, the Auditory, Tactile, Visual and Vestibular Intervention (ATVV) provides infant remediation (Burns et al., 1994; Nelson et al., 2001; White-Traut & Nelson, 1988; White-Traut et al., 1997; White-Traut et al., 2002a; White-Traut & Pate, 1987) and is easily learned by mothers and nurses. The ATVV was developed over the last 20 years by the first author. Participatory guidance offered by the NAT provides redefinition and re-education for the mother (Barnes-Boyd, Norr, & Nacion, 1996; Barnes-Boyd, Norr, & Nacion, 2001; Nacion, Norr, Burnett, & Boyd, 2000; Norr et al., 2003).
Infant remediation
The ATVV intervention is a 15-minute, multi-sensory intervention that incorporates the interactive behaviors of mothers and infants. The first part of the ATVV intervention consists of auditory stimulation. A soothing, female voice is presented to the infant for a minimum of 30 seconds, using infant directed speech to alert the infant to the presence of the caregiver. The infant directed speech continues throughout the 15-minute intervention. The tactile component of the intervention is then added for 10 minutes. The infant is first placed in a supine position, and the head, chest, abdomen, legs, and arms are massaged with moderate pressure. The infant is then repositioned prone, and the head and back are massaged. Following 10 minutes of talking and massage, the infant is swaddled and held with the limbs in flexion. For the last 5 minutes, the infant is horizontally rocked. Throughout the intervention, eye contact is attempted with the infant (Burns et al., 1994). The infant receives the ATVV intervention by the mother or the nurse twice a day, from 32 weeks gestation while hospitalized and by the mother after hospital discharge through one month corrected age. The ATVV is offered prior to feeding and in an environment with reduced sound and light. In the hospital, nurses will dim lights and minimize noise, while mothers at home are instructed to turn off the TV and radio.
Maternal redefinition and re-education
The maternal redefinition and re-education components of the intervention are participatory guidance offered by the NAT. The nurse provides professional expertise while the community advocate offers lived experience with the environmental stressors facing the mother. The mother is taught to recognize her infant’s behavioral states and pre-feeding, engagement and disengagement behavioral cues (redefinition). The mother is also taught to modify her behavior in response to her baby’s behavioral cues, techniques to soothe a fussy baby and to promote social interaction during feeding (re-education). The NAT teaches the mother the ATVV intervention and explores with her how to create a quiet home environment (re-education). In addition, the NAT asks about and responds to the mother’s concerns, weighs the infant, discusses safety, and assesses the mother’s stressors, supports, and signs of depression. At each home visit, the nurse observes administration of the ATVV and a feeding and gives participatory guidance regarding the contribution of mother and infant to the interaction, infant behavioral state and cues, and the mother’s use of soothing behaviors (redefinition and re-education) (Sumner & Spietz, 1994). Each mother receives two in-hospital visits and two home visits, one within the first two days after infant discharge to home and the second after the infant has been home for two weeks. A telephone contact is made after each home visit.
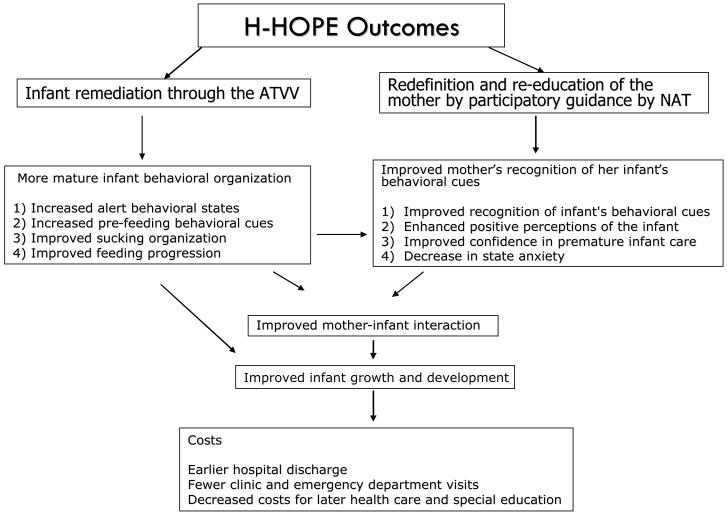
Anticipated Impact of the H-HOPE Intervention
The H-HOPE intervention should have positive impact on the infant, the mother, mother-infant interaction, and infant growth and development leading to reduced health care costs (Figure 2). The intervention is currently being tested in a five-year, randomized clinical trial of 252 mother-premature infant dyads at two clinical sites. Infant remediation through the ATVV is expected to lead to increasingly mature behavioral organization, which will result in improved feeding progression and growth. Consequently, the premature infant will be discharged earlier, reducing the cost of the hospitalization. Increasingly mature behavioral organization will also improve the mother’s ability to understand and interpret her infant’s behaviors, the quality of their interactions, and infant growth and development.
Figure 2.
Anticipated Outcomes of the H-HOPE Intervention
Redefinition and re-education of the mother by participatory guidance will improve the mother’s recognition of her infant’s behavioral cues, enhancing positive perceptions of the infant and increasing her confidence in premature infant care. As a mother’s ability to understand and interpret her premature infant’s behavior increases, her level of state anxiety will decrease and mother-infant interaction will improve. As mothers become more confident in their ability to care for their infants, unnecessary clinic and emergency department visits should decline, and health care costs should decrease. Thus, the H-HOPE intervention will work synergistically to improve infant feeding progression, the quality of mother-infant interaction, and infant growth and development, thus reducing health care and special education costs.
Implications
Prematurity extracts a high cost on infants, families, and the nation. Approximately half a million premature infants are born each year in the United States, and the national prematurity rate of 12.5% has not declined over the last 20 years (Martin et al., 2006). Moreover, there are significant racial health disparities associated with prematurity. The rate of premature birth among African Americans is 17.9%, while the rate of premature birth among Whites is 11.5% (Martin et al., 2006). Most premature infants require an expensive and lengthy hospital stay, presenting significant economic costs to their families and society.
Since the H-HOPE intervention intercedes in the crucial early period when the foundation for positive interaction between mother and infant is being built, this intervention has the potential to significantly impact the economic, medical, and social costs of prematurity. Reducing hospital stay by as little as three days could save over $2 billion annually. If the H-HOPE intervention is successful, it has the potential to significantly reduce national expenditure for health care and special education, and these findings can serve as a national model to address the unique social and health care needs of this vulnerable group of mothers and premature infants.
Callouts.
Mother-premature infant dyads at high social-environmental risk are a group in need of early interventions that address feeding and mother-infant interaction.
Mothers of premature infants often respond inappropriately to their infants’ behaviors and have less positive mother-infant interaction scores and less contingency.
The Hospital-Home Transition: Optimizing Prematures’ Environment intervention is unique because it provides an integrated approach that addresses gaps identified in previous research.
Figure 1.
The H-HOPE Intervention
Acknowledgements
Funded by the National Institute of Child Health and Development and the National Institute of Nursing Research, Grant 1 R01 HD050738-01A2 and the Harris Foundation.
Footnotes
The authors and planners for this activity report no conflict of interest or relevant financial relationships. The article includes no discussion of off-label drug or devise use.
Contributor Information
Rosemary White-Traut, professor and the head of the Department of Women Children and Family Health Science, the University of Illinois at Chicago, College of Nursing, Chicago, IL.
Kathleen Norr, professor in the Department of Women Children and Family Health Science, the University of Illinois at Chicago, College of Nursing, Chicago, IL.
Reference List
- Als H, Duffy FH, McAnulty GB, Rivkin MJ, Vajapeyam S, Mulkern RV, et al. Early experience alters brain function and structure. Pediatrics. 2004;113:846–857. doi: 10.1542/peds.113.4.846. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van IJzendoorn MH, Bradley RH. Those who have, receive: The Matthew effect in early childhood intervention in the home environment. Review of Educational Research. 2005;75:1–26. [Google Scholar]
- Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- Barkauskas VH. Effectiveness of public health nurse home visits to primarous mothers and their infants. American Journal of Public Health. 1983;73:573–580. doi: 10.2105/ajph.73.5.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard KE. Influencing parent-child interactions for children at-risk. In: Guralnick MJ, editor. The effectiveness of early intervention. P. H. Brookes; Baltimore, MD: 1997. pp. 249–268. [Google Scholar]
- Barnard KE, Bee HL, Hammond MA. Developmental changes in maternal interactions with term and preterm infants. Infant Behavior & Development. 1984;7:101–113. [Google Scholar]
- Barnard KE, Magyary D, Sumner G, Booth CL, Mitchell SK, Spieker S. Prevention of parenting alterations for women with low social support. Psychiatry. 1988;51:248–253. doi: 10.1080/00332747.1988.11024399. [DOI] [PubMed] [Google Scholar]
- Barnes-Boyd C, Norr KF, Nacion KW. Evaluation of an interagency home visiting program to reduce postneonatal mortality in disadvantaged communities. Public Health Nursing. 1996;13:201–208. doi: 10.1111/j.1525-1446.1996.tb00241.x. [DOI] [PubMed] [Google Scholar]
- Barnes-Boyd C, Norr KF, Nacion KW. Promoting infant health through home visiting by a nurse-managed community worker team. Public Health Nursing. 2001;18:225–235. doi: 10.1046/j.1525-1446.2001.00225.x. [DOI] [PubMed] [Google Scholar]
- Barrera ME, Kitching KJ, Cunningham CE, Doucet D, Rosenbaum PL. A 3-year early home intervention follow-up with low birthweight infants and their parents. Topics in Early Childhood Special Education. 1990;10:14–28. [Google Scholar]
- Bendersky M, Lewis M. Environmental risk, biological risk, and developmental outcome. Developmental Psychology. 1994;30:484–494. [Google Scholar]
- Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: A meta-analysis. JAMA. 2002;288:728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- Blackburn S. Fostering behavioral development of high-risk infants. Journal of Obstetric, Gynecologic and Neonatal Nursing. 1983;3(Supplement):76S–86S. doi: 10.1111/j.1552-6909.1983.tb01104.x. [DOI] [PubMed] [Google Scholar]
- Booth CL, Mitchell SK, Barnard KE, Spieker S. Development of maternal social skills in multiproblem families: Effects on the mother-child relationship. Developmental Psychology. 1989;25:403–409. [Google Scholar]
- Bradley RH, Corwyn RF, McAdoo HP, Coll CG. The home environments of children in the United States part I: Variations by age, ethnicity, and poverty status. Child Development. 2001;72:1844–1867. doi: 10.1111/1467-8624.t01-1-00382. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Whiteside L, Mundfrom DJ, Casey PH, Kelleher KJ, Pope SK. Early indications of resilience and their relation to experiences in the home environments of low birthweight, premature children living in poverty. Child Development. 1994;65:346–360. [PubMed] [Google Scholar]
- Brooks-Gunn J, Klebanov PK, Liaw F. The learning, physical, and emotional environment of the home in the context of poverty: The Infant Health and Development Program. Children and Youth Services Review. 1995;17:251–276. [Google Scholar]
- Brooten D, Gennaro S, Brown LP, Butts P, Gibbons AL, Bakewell-Sachs S, et al. Anxiety, depression and hostility in mothers of preterm infants. Nursing Research. 1988;37:213–216. [PubMed] [Google Scholar]
- Brooten D, Kumar S, Brown LP, Butts P, Finkler SA, Bakewell-Sachs S, et al. A randomized clinical trial of every hospital discharge and home follow-up of very-low-birth-weight infants. New England Journal of Medicine. 1986;315:934–939. doi: 10.1056/NEJM198610093151505. [DOI] [PubMed] [Google Scholar]
- Brousseau DC, Hoffmann RG, Yauck J, Nattinger AB, Flores G. Disparities for Latino children in the timely receipt of medical care. Ambulatory Pediatrics. 2005;5:319–325. doi: 10.1367/A04-203R1.1. [DOI] [PubMed] [Google Scholar]
- Bryant D, Maxwell K. The effectiveness of early intervention for disadvantaged children. In: Guralnick M, editor. The effectiveness of early intervention. Pauly Books; Baltimore: 1997. pp. 23–46. [Google Scholar]
- Bugental DB, Happaney K. Predicting infant maltreatment in low-income families: The interactive effects of maternal attributions and child status at birth. Developmental Psychology. 2004;40:234–243. doi: 10.1037/0012-1649.40.2.234. [DOI] [PubMed] [Google Scholar]
- Burchinal M, Roberts JE, Zeisel SA, Hennon EA, Hooper S. Social risk and protective child, parenting, and child care factors in early elementary school years. Parenting: Science and Practice. 2006;6:79–113. [Google Scholar]
- Burns K, Cunningham N, White-Traut RC, Silvestri JM, Nelson MN. Infant stimulation: Modification of an intervention based on physiological and behavioral cues. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1994;23:581–589. doi: 10.1111/j.1552-6909.1994.tb01924.x. [DOI] [PubMed] [Google Scholar]
- Caldwell CH, Antonucci TC, Jackson JS, Wolford ML, Osofsky JD. Perceptions of parental support and depressive symptomatology among Black and White adolescent mothers. Journal of Emotional & Behavioral Disorders. 1997;5:173–183. [Google Scholar]
- Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, Briggs-Gowan MJ. Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:18–26. doi: 10.1097/00004583-200101000-00012. [DOI] [PubMed] [Google Scholar]
- Casiro OG, McKenzie ME, McFadyen L, Shapiro C, Seshia MM, MacDonald N, et al. Earlier discharge with community-based intervention for low birth weight infants: A randomized trial. Pediatrics. 1993;92:128–134. [PubMed] [Google Scholar]
- Chase-Lansdale PL, Gordon RA, Brooks-Gunn J, Klebanov PK. Neighborhood and family influences on the intellectual and behavioral competence of preschool and early school-age children. In: Brooks-Gunn J, Duncan GJ, Aber JLE, editors. Neighborhood poverty: Context and consequences for children. Russell Sage Foundation; New York: 1997. pp. 79–118. [Google Scholar]
- Coyl DD, Roggman LA, Newland LA. Stress, maternal depression, and negative mother-infant interactions in relation to infant attachment. Infant Mental Health Journal. 2002;23:145–163. [Google Scholar]
- Crittenden KS, Kim S, Watanabe K, Norr KF. Welfare, work and well-being among inner-city mothers. Journal of Prevention & Intervention in the Community. 2002;23:41–64. [Google Scholar]
- Crook CK. The organization and control of infant sucking. Advances in Child Development. 1979;14:209–252. doi: 10.1016/s0065-2407(08)60115-9. [DOI] [PubMed] [Google Scholar]
- Cusson RM. Factors influencing language development in preterm infants. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN / NAACOG. 2003;32:402–409. doi: 10.1177/0884217503253530. [DOI] [PubMed] [Google Scholar]
- Davis L, Edwards H, Mohay H. Mother-infant interaction in premature infants at three months after nursery discharge. International Journal of Nursing Practice. 2003;9:374–381. doi: 10.1046/j.1440-172x.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- de Kleine MJ, den Ouden AL, Kollee LA, Nijhuis-van der Sanden MW, Sondaar M, Kessel-Feddema BJ, et al. Development and evaluation of a follow up assessment of preterm infants at 5 years of age. Archives of Disease in Childhood. 2003;88:870–875. doi: 10.1136/adc.88.10.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Huston A, McLoyd VC. Growing up poor: The effects on achievement, parenting and child care. Consortium of Social Science Associations; Washington, D.C.: 1998. [Google Scholar]
- Feldman R, Eidelman AI. Neonatal state organization, neuromaturation, mother-infant interaction, and cognitive development in small-for-gestational-age premature infants. Pediatrics. 2006;118:e869–e878. doi: 10.1542/peds.2005-2040. [DOI] [PubMed] [Google Scholar]
- Feldman R, Keren M, Gross-Rozval O, Tyano S. Mother-child touch patterns in infant feeding disorders: Relation to maternal, child, and environmental factors. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1089–1097. doi: 10.1097/01.chi.0000132810.98922.83. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelman AI. Direct and indirect effects of breast milk on neurobehavioral and cognitive development of premature infants. Developmental Psychobiology. 2003;43:109–119. doi: 10.1002/dev.10126. [DOI] [PubMed] [Google Scholar]
- Herrenkohl EC, Herrenkohl RC, Rupert LJ, Egolf BP, Lutz JG. Risk factors for behavioral dysfunction: The relative impact of maltreatment, SES, physical health problems, cognitive ability, and quality of parent-child interaction. Child Abuse & Neglect. 1995;19:191–203. doi: 10.1016/0145-2134(94)00116-c. [DOI] [PubMed] [Google Scholar]
- Hess CR, Papas MA, Black MM. Resilience among African American adolescent mothers: Predictors of positive parenting in early infancy. Journal of Pediatric Psychology. 2002;27:619–629. doi: 10.1093/jpepsy/27.7.619. [DOI] [PubMed] [Google Scholar]
- Holditch-Davis D, Bartlett TR, Blickman AL, Miles MS. Posttraumatic stress symptoms in mothers of premature infants. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN / NAACOG. 2003;32:161–171. doi: 10.1177/0884217503252035. [DOI] [PubMed] [Google Scholar]
- Holditch-Davis D, Miles MS. Mothers’ stories about their experiences in the neonatal intensive care unit. Neonatal Network: NN. 2000;19:13–21. doi: 10.1891/0730-0832.19.3.13. [DOI] [PubMed] [Google Scholar]
- Holditch-Davis D, Miles MS, Belyea M. Feeding and nonfeeding interactions of mothers and prematures. Western Journal of Nursing Research. 2000;22:320–334. doi: 10.1177/01939450022044449. [DOI] [PubMed] [Google Scholar]
- Horowitz JA, Bell M, Trybulski J, Munro BH, Moser D, Hartz SA, et al. Promoting responsiveness between mothers with depressive symptoms and their infants. Journal of Nursing Scholarship. 2001;33:323–329. doi: 10.1111/j.1547-5069.2001.00323.x. [DOI] [PubMed] [Google Scholar]
- Kaaresen PI, Ronning JA, Ulvund SE, Dahl LB. A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics. 2006;118:e9–e19. doi: 10.1542/peds.2005-1491. [DOI] [PubMed] [Google Scholar]
- Kang R, Barnard K, Hammond M, Oshio S, Spencer C, Thibodeaux B, et al. Preterm infant follow-up project: A multi-site field experiment of hospital and home intervention programs for mothers and preterm infants. Public Health Nursing. 1995;12:171–180. doi: 10.1111/j.1525-1446.1995.tb00006.x. [DOI] [PubMed] [Google Scholar]
- Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatrica. 2003;92:721–727. [PubMed] [Google Scholar]
- Lawhon G. Facilitation of parenting the premature infant within the newborn intensive care unit. Journal of Perinatal & Neonatal Nursing. 2002;16:71–82. doi: 10.1097/00005237-200206000-00008. [DOI] [PubMed] [Google Scholar]
- Lekskulchai R, Cole J. Effect of a developmental program on motor performance in infants born preterm. The Australian Journal of Physiotherapy. 2001;47:169–176. doi: 10.1016/s0004-9514(14)60264-6. [DOI] [PubMed] [Google Scholar]
- Limbo R, Petersen W, Pridham K. Promoting safety of young children with guided participation processes. Journal of Pediatric Health Care. 2003;17:245–251. doi: 10.1016/s0891-5245(02)88335-3. [DOI] [PubMed] [Google Scholar]
- Lucarelli L, Ambruzzi AM, Cimino S, D’Olimpio F, Finistrella V. Feeding disorders in infancy: An empirical study on mother-infant interactions. Minerva Pediatrica. 2003;55:243–253. [PubMed] [Google Scholar]
- Magill-Evans J, Harrison MJ. Parent-child interactions, parenting stress, and developmental outcomes at 4 years. Children’s Health Care: Journal of the Association for the Care of Children’s Health. 2001;30:135–150. [Google Scholar]
- Malat J, Oh HJ, Hamilton MA. Poverty experience, race, and child health. Public Health Reports. 2005;120:442–447. doi: 10.1177/003335490512000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: Final data for 2004. National Center for Health Statistics; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant-mother attachment: A meta-analytic investigation. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41:737–746. [PubMed] [Google Scholar]
- McCain GC. Behavioral state activity during nipple feedings for preterm infants. Neonatal Network: NN. 1997;16:43–47. [PubMed] [Google Scholar]
- McCormick MC, Brooks-Gunn J, Buka SL, Goldman J, Yu J, Salganik M, et al. Early intervention in low birth weight premature infants: Results at 18 years of age for the Infant Health and Development Program. Pediatrics. 2006;117:771–780. doi: 10.1542/peds.2005-1316. [DOI] [PubMed] [Google Scholar]
- McGauhey PJ, Starfield B, Alexander C, Ensminger ME. Social environment and vulnerability of low birth weight children: A social-epidemiological perspective. Pediatrics. 1991;88:943–953. [PubMed] [Google Scholar]
- McGrath JM, Medoff-Cooper B. Apnea and periodic breathing during bottle feeding of premature infants. Communicating Nursing Research. 2001;34:220. [Google Scholar]
- McGrath M, Sullivan M. Birth weight, neonatal morbidities, and school age outcomes in full-term and preterm infants. Issues in Comprehensive Pediatric Nursing. 2002;25:231–254. doi: 10.1080/01460860290042611. [DOI] [PubMed] [Google Scholar]
- Medoff-Cooper B. Nutritive sucking. In: Salkind NJ, editor. Encyclopedia of human development. Sage Publications; Thousand Oaks, CA: 2006. [Google Scholar]
- Medoff-Cooper B, McGrath JM, Bilker W. Nutritive sucking and neurobehavioral development in preterm infants from 34 weeks PCA to term. MCN: The American Journal of Maternal Child Nursing. 2000;25:64–70. doi: 10.1097/00005721-200003000-00004. [DOI] [PubMed] [Google Scholar]
- Medoff-Cooper B, Ratcliffe SJ. Development of preterm infants: Feeding behaviors and Brazelton Neonatal Behavioral Assessment Scale at 40 and 44 weeks’ postconceptional age. Advances in Nursing Science. 2005;28:356–363. doi: 10.1097/00012272-200510000-00007. [DOI] [PubMed] [Google Scholar]
- Mew AM, Holditch-Davis D, Belyea M, Miles MS, Fishel A. Correlates of depressive symptoms in mothers of preterm infants. Neonatal Network: NN. 2003;22:51–60. doi: 10.1891/0730-0832.22.5.51. [DOI] [PubMed] [Google Scholar]
- Miles MS, Holditch-Davis D. Parenting the prematurely born child: Pathways of influence. Seminars in Perinatology. 1997;21:254–266. doi: 10.1016/s0146-0005(97)80067-5. [DOI] [PubMed] [Google Scholar]
- Muller-Nix C, Forcada-Guex M, Pierrehumbert B, Jaunin L, Borghini A, Ansermet F. Prematurity, maternal stress and mother-child interactions. Early Human Development. 2004;79:145–158. doi: 10.1016/j.earlhumdev.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Murry VM, Kotchick BA, Wallace S, Ketchen B, Eddings K, Heller L, et al. Race, culture, and ethnicity: Implications for a community intervention. Journal of Child and Family Studies. 2004;13:81–99. [Google Scholar]
- Nacion KW. Postpartum maternal concerns of low-income women experiencing early and conventional discharge (Doctoral dissertation, University of Illinois at Chicago, 1988) Dissertation Abstracts International. 1988;49(09):3678. [Google Scholar]
- Nacion KW, Norr KF, Burnett GM, Boyd CB. Validating the safety of nurse-health advocate services. Public Health Nursing. 2000;17:32–42. doi: 10.1046/j.1525-1446.2000.00032.x. [DOI] [PubMed] [Google Scholar]
- National Institute of Child Health and Human Development Early Child Care Research Network Duration and developmental timing of poverty and children’s cognitive and social development from birth through third grade. Child Development. 2005;76:795–810. doi: 10.1111/j.1467-8624.2005.00878.x. [DOI] [PubMed] [Google Scholar]
- Nelson MN, White-Traut RC, Vasan U, Silvestri JM, Comiskey E, Meleedy-Rey P, et al. One-year outcome of Auditory-Tactile-Visual-Vestibular intervention in the Neonatal Intensive Care Unit: Effects of severe prematurity and central nervous system injury. Journal of Child Neurology. 2001;16:493–498. doi: 10.1177/088307380101600706. [DOI] [PubMed] [Google Scholar]
- Norr KF, Crittenden KS, Lehrer EL, Reyes O, Boyd CB, Nacion KW, et al. Maternal and infant outcomes at one year for a nurse-health advocate home visiting program serving African Americans and Mexican Americans. Public Health Nursing. 2003;20:190–203. doi: 10.1046/j.0737-1209.2003.20306.x. [DOI] [PubMed] [Google Scholar]
- Norr KF, Nacion KW, Abramson R. Early discharge with home follow-up: Impacts on low-income mothers and infants. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN / NAACOG. 1989;18:133–141. doi: 10.1111/j.1552-6909.1989.tb00476.x. [DOI] [PubMed] [Google Scholar]
- Nursing Child Assessment Satellite Training Program . Keys to caregiving: Study guide. NCAST Publications, University of Washington; Seattle, WA: 1990. [Google Scholar]
- O’Brien F, Roth S, Stewart A, Rifkin L, Rushe T, Wyatt J. The neurodevelopmental progress of infants less than 33 weeks into adolescence. Archives of Disease in Childhood. 2004;89:207–211. doi: 10.1136/adc.2002.006676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds D, Henderson CR, Jr., Kitzman H, Eckenrode J, Tatelbaum R. The promise of home visitation: Results of two randomized trials. Journal of Community Psychology. 1998;26:5–21. [Google Scholar]
- Olds DL. The nurse-family partnership: An evidence-based preventive intervention. Infant Mental Health Journal. 2006;27:5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr., Kitzman HJ, Eckenrode JJ, Cole RE, Tatelbaum RC. Prenatal and infancy home visitation by nurses: Recent findings. The Future of Children. 1999;9:44–65. [PubMed] [Google Scholar]
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: Age 4 follow-up results of a randomized trial. Pediatrics. 2004;114:1560–1568. doi: 10.1542/peds.2004-0961. [DOI] [PubMed] [Google Scholar]
- Parker S, Greer S, Zuckerman B. Double jeopardy: The impact of poverty on early child development. Pediatric Clinics of North America. 1988;35:1227–1240. doi: 10.1016/s0031-3955(16)36580-4. [DOI] [PubMed] [Google Scholar]
- Parker SJ, Zahr LK, Cole JG, Brecht ML. Outcome after developmental intervention in the neonatal intensive care unit for mothers of preterm infants with low socioeconomic status. The Journal of Pediatrics. 1992;120:780–785. doi: 10.1016/s0022-3476(05)80248-3. [DOI] [PubMed] [Google Scholar]
- Petterson SM, Albers AB. Effects of poverty and maternal depression on early child development. Child Development. 2001;72:1794–1813. doi: 10.1111/1467-8624.00379. [DOI] [PubMed] [Google Scholar]
- Pickler RH, Best AM, Reyna BA, Gutcher GR, Wetzel PA. Predictors of nutritive sucking in preterm infants. Journal of Perinatology. 2006;26:693–699. doi: 10.1038/sj.jp.7211590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poehlmann J, Fiese BH. Parent-infant interaction as a mediator of the relation between neonatal risk status and 12-month cognitive development. Infant Behavior & Development. 2001;24:171–188. [Google Scholar]
- Pridham K, Brown R, Clark R, Limbo RK, Schroeder M, Henriques J, et al. Effect of guided participation on feeding competencies of mothers and their premature infants. Research in Nursing & Health. 2005;28:252–267. doi: 10.1002/nur.20073. [DOI] [PubMed] [Google Scholar]
- Pridham K, Lin CY, Brown R. Mothers’ evaluation of their caregiving for premature and full-term infants through the first year: Contributing factors. Research in Nursing & Health. 2001;24:157–169. doi: 10.1002/nur.1019. [DOI] [PubMed] [Google Scholar]
- Pridham K, Saxe R, Limbo R. Feeding issues for mothers of very low-birth-weight, premature infants through the first year. Journal of Perinatal & Neonatal Nursing. 2004;18:161–169. doi: 10.1097/00005237-200404000-00010. [DOI] [PubMed] [Google Scholar]
- Pridham KA, Krolikowski MM, Limbo RK, Paradowski J, Rudd N, Meurer JR, et al. Guiding mothers’ management of health problems of very low birth-weight infants. Public Health Nursing. 2006;23:205–215. doi: 10.1111/j.1525-1446.2006.230302.x. [DOI] [PubMed] [Google Scholar]
- Ramey CT, Ramey SL. Prevention of intellectual disabilities: Early interventions to improve cognitive development. Preventive Medicine. 1998;27:224–232. doi: 10.1006/pmed.1998.0279. [DOI] [PubMed] [Google Scholar]
- Rogoff B, Mistry J, Goncu A, Mosier C. Guided participation in cultural activity by toddlers and caregivers. Monographs of the Society for Research in Child Development. 1993;58:1–179. [PubMed] [Google Scholar]
- Saigal S, Den Ouden L, Wolke D, Hoult L, Paneth N, Streiner DL, et al. School-age outcomes in children who were extremely low birth weight from four international population-based cohorts. Pediatrics. 2003;112:943–950. doi: 10.1542/peds.112.4.943. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Fiese BH. Transactional regulation: The developmental ecology of early intervention. In: Shonkoff JP, Meisels SJ, editors. Handbook of early childhood intervention. Cambridge University Press; New York: 2000. pp. 135–159. [Google Scholar]
- Sameroff AJ, Mackenzie MJ. Research strategies for capturing transactional models of development: The limits of the possible. Development and Psychopathology. 2003;15:613–640. doi: 10.1017/s0954579403000312. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Zax M, Barocas R. Early indicators of developmental risk: Rochester longitudinal study. Schizophrenia Bulletin. 1987;13:383–394. doi: 10.1093/schbul/13.3.383. [DOI] [PubMed] [Google Scholar]
- Schiffman RF, Omar MA, McKelvey LM. Mother-infant interaction in low-income families. MCN: The American Journal of Maternal Child Nursing. 2003;28:246–251. doi: 10.1097/00005721-200307000-00008. [DOI] [PubMed] [Google Scholar]
- Shi L, Stevens GD. Disparities in access to care and satisfaction among U.S. children: The roles of race/ethnicity and poverty status. Public Health Reports. 2005;120:431–441. doi: 10.1177/003335490512000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel E, Bauman KE, Schaefer ES, Saunders MM, Ingram DD. Hospital and home support during infancy: Impact on maternal attachment, child abuse and neglect, and health care utilization. Pediatrics. 1980;66:183–190. [PubMed] [Google Scholar]
- Simpson L, Owens PL, Zodet MW, Chevarley FM, Dougherty D, Elixhauser A, et al. Health care for children and youth in the United States: Annual report on patterns of coverage, utilization, quality, and expenditures by income. Ambulatory Pediatrics. 2005;5:6–44. doi: 10.1367/A04-119R.1. [DOI] [PubMed] [Google Scholar]
- Singer LT, Fulton S, Davillier M, Koshy D, Salvator A, Baley JE. Effects of infant risk status and maternal psychological distress on maternal-infant interactions during the first year of life. Journal of Developmental and Behavioral Pediatrics. 2003;24:233–241. doi: 10.1097/00004703-200308000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slack KS, Holl JL, McDaniel M, Yoo J, Bolger K. Understanding the risks of child neglect: An exploration of poverty and parenting characteristics. Child Maltreatment. 2004;9:395–408. doi: 10.1177/1077559504269193. [DOI] [PubMed] [Google Scholar]
- Stern-Bruschweiler N, Stern DN. A model for conceptualizing the role of the mother’s representational world in various mother-infant therapies. Infant Mental Health Journal. 1989;10:142–156. [Google Scholar]
- Stoelhorst GM, Rijken M, Martens SE, van Zwieten PH, Feenstra J, Zwinderman AH, et al. Developmental outcome at 18 and 24 months of age in very preterm children: A cohort study from 1996-1997. Early Human Development. 2003;72:83–95. doi: 10.1016/s0378-3782(03)00011-2. [DOI] [PubMed] [Google Scholar]
- Sumner G, Spietz A. NCAST-Caregiver/parent-child interaction feeding manual. NCATS Publications; Seattle, WA: 1994. [Google Scholar]
- Talmi A, Harmon RJ. Relationships between preterm infants and their parents: Disruption and development. Zero to Three. 2003;24:13–20. [Google Scholar]
- White-Traut RC, Berbaum ML, Lessen B, McFarlin B, Cardenas L. Feeding readiness in preterm infants: The relationship between preterm behavioral state and feeding readiness behaviors and efficiency during transition from gavage to oral feeding. MCN: The American Journal of Maternal Child Nursing. 2005;30:52–59. [PubMed] [Google Scholar]
- White-Traut RC, Nelson MN. Maternally administered tactile, auditory, visual, and vestibular stimulation: Relationship to later interactions between mothers and premature infants. Research in Nursing & Health. 1988;11:31–39. doi: 10.1002/nur.4770110106. [DOI] [PubMed] [Google Scholar]
- White-Traut RC, Nelson MN, Silvestri JM, Cunningham N, Patel M. Responses of preterm infants to unimodal and multimodal sensory intervention. Pediatric Nursing. 1997;23:169–175. [PubMed] [Google Scholar]
- White-Traut RC, Nelson MN, Silvestri JM, Vasan U, Littau S, Meleedy-Rey P, et al. Effect of auditory, tactile, visual, and vestibular intervention on length of stay, alertness, and feeding progression in preterm infants. Developmental Medicine and Child Neurology. 2002a;44:91–97. doi: 10.1017/s0012162201001736. [DOI] [PubMed] [Google Scholar]
- White-Traut RC, Nelson MN, Silvestri JM, Vasan U, Patel M, Cardenas L. Feeding readiness behaviors and feeding efficiency in response to ATVV intervention. Newborn and Infant Nursing Reviews. 2002b;2:166–173. [Google Scholar]
- White-Traut RC, Pate CMH. Modulating infant state in premature infants. Journal of Pediatric Nursing. 1987;2:96–101. [PubMed] [Google Scholar]
- Zahr L. Correlates of mother-infant interaction in premature infants from low socioeconomic backgrounds. Pediatric Nursing. 1991;17:259–264. [PubMed] [Google Scholar]
- Zahr LK. Home-based intervention after discharge for Latino families of low-birth-weight infants. Infant Mental Health Journal. 2000;21:448–463. [Google Scholar]