Abstract
Despite negative outcomes for depressed mothers and their children, no treatment specifically designed to address maternal depression in the context of home visitation has emerged. In-Home Cognitive Behavioral Therapy (IH-CBT) is an adapted treatment that is delivered in the home, focuses on the needs of new mothers, and leverages ongoing home visiting to optimize engagement and outcomes. This study examined the efficacy of IH-CBT using a randomized clinical trial. Subjects were 93 new mothers in a home visiting program. Mothers with major depressive disorder identified at 3 months postpartum were randomized into IH-CBT and ongoing home visitation (n=47) or standard home visitation (SHV; n=46) in which they received home visitation alone and could obtain treatment in the community. Depression was measured at pre- and posttreatment, and 3-month follow-up using interviews, clinician ratings, and self-report. Mothers receiving IH-CBT showed improvements in all indicators of depression relative to the SHV condition and these gains were maintained at follow-up. For example, 70.7% of mothers receiving IH-CBT were no longer depressed at posttreatment in terms of meeting criteria for major depressive disorder compared to 30.2% in the SHV group. These findings suggest that IH-CBT is an efficacious treatment for depressed mothers in home visitation programs.
Keywords: home visitation, maternal depression, cognitive behavioral therapy, adapted treatment
Home visitation is a promising prevention strategy for young children and their mothers (Sweet & Appelbaum, 2004). Originally designed to prevent child abuse and neglect, home visitation programs have broadened to encompass multiple approaches to optimize child health and development (Boller & Strong, 2010). Although there is significant variability in the formats and strategies used by home visitation models, they typically share common elements: (a) enrollment early in the child's life (or prenatally), (b) engagement of mothers early in their roles as parents, (c) strengthening of individual and family protective factors and mitigating risk factors to promote normative development, (d) frequent contact between home visitors and families, and (e) extended program duration (up to 3 years) to ensure that home visitors are present during developmental transitions in which new needs of children and families emerge.
There are up to 500,000 children and their mothers served by home visiting programs in the USA (Astuto & Allen, 2009). Mothers served by home visitation are typically socially isolated, impoverished, and underemployed. As a result, home visitation programs spend considerable time working directly with mothers to address such issues as stress and coping, health, social functioning, and educational advancement. By strengthening functioning in these domains, mothers are more available to their children, better able to meet child needs, and are amenable to the psychoeducational approaches used by home visitors. Maternal depression negatively impacts these areas, and is recognized as a major public health problem. Indeed, research shows that between 28% and 61% of mothers in home visitation report clinically elevated levels of depression during the course of service (Ammerman et al., 2010). Several studies have found that depression is linked with poorer outcomes in home visitation (Ammerman et al., 2012; Duggan et al., 2009). Furthermore, home visitors report being unprepared to work with depressed mothers (Tandon, Parillo, Jenkins, & Duggan, 2005), that depressed mothers are harder to engage during home visits and are less able to benefit from services (Stevens et al., 2005), and that depression makes it more difficult to implement program curricula (Administration on Children Youth and Families, 2002).
Clinical trials suggest that home visitation alone provides little to no benefit in reducing maternal depressive symptoms (Duggan, Fuddy, Burrell, et al., 2004), or that symptom reduction is short-lived (Landsverk et al., 2002) or occurs only after services have ended (Chazan-Cohen et al., 2007). Thus, during the important first years of the child's life these mothers and their offspring are at risk to experience the negative effects of depression and less able to take advantage of the services provided by home visitors. One of the goals of home visitation is to link mothers to other needed resources in the community, including mental health treatment. Yet, home visitors often fail to identify depression (Duggan, Fuddy, McFarlane, et al., 2004). Even though depression screening has become standard in home visitation programs, mothers infrequently obtain mental health treatment even when the need is recognized (Tandon et al., 2008). When mothers obtain treatment, the competing time demands in complex health systems preclude adequate collaboration between clinicians and home visitors, which in turn potentially undermines treatment effectiveness. No effective interventions have been developed that address this problem in home visitation.
In order to be effective, treatment for depressed mothers in home visitation needs to accommodate the unique features of the setting (e.g., the home), population (e.g., low income, new mothers), and context (e.g., concurrent services provided by home visitors). In fact, it is widely acknowledged that the attenuated effectiveness observed when evidence-based treatments are applied in real-world settings is attributable in part to the failure to attend to such accommodations (Conner-Smith & Weisz, 2003; Weisz et al., 2012). In response, Ammerman et al. (2007) systematically adapted cognitive behavioral therapy (CBT) in order to optimize its effectiveness for depressed mothers receiving home visitation. Although there are several treatments that have been found to be effective for depressed mothers (Cohen et al., 2010), and there have been successful efforts to provide intervention in the home setting (Leis, Mendelson, Tandon, & Perry, 2009), CBT was selected because (a) it is theoretically and practically compatible with home visiting and different home visiting models, (b) it has a strong foundation of evidence for efficacy, and (c) it is widely trained and as a result an adapted version could be more readily disseminated and adopted by home visiting programs. In-Home Cognitive Behavioral Therapy (IH-CBT) is implemented by therapists who provide treatment concurrently with ongoing home visitation. IH-CBT combines the core principles and techniques of CBT (J. Beck, 2011) with a set of procedures and strategies that promote engagement, make content relevant to the needs of mothers in home visitation, facilitate delivery in the home, and explicitly foster a collaborative relationship between the therapist and home visitor in order to smoothly coordinate services. Adaptations include procedures for identifying suitable areas for conducting therapy in homes that are often small, crowded, and unkempt; addressing the unique issues of socially isolated, low-income mothers in raising a newborn; and building close working relationships between home visitors and therapists. IH-CBT is an enhancement to standard home visitation that emphasizes the reduction of maternal depressive symptoms and recovery from major depressive disorder (MDD).
Preliminary empirical support for IH-CBT was obtained in an open trial (Ammerman et al., 2011) with 64 mothers aged 18 years and older who were participating in home visitation and who obtained scores of ≥20 on the Beck Depression Inventory-II (BDI-II) and met criteria for MDD using the PRIME-MD. Pre-post comparisons revealed that 46.9% of mothers were partially remitted in terms of MDD diagnosis and 32.8% were fully remitted at the end of treatment. Mothers also reported decreased self-reported depressive symptoms and improvements in social support, relationships, coping, and satisfaction with motherhood. A comparison of mothers treated with IH-CBT to 241 untreated mothers who had similarly elevated BDI-II scores at enrollment in home visitation showed a substantial reduction (p<.01) in the treatment group (18.4 points) relative to untreated mothers (10.6 points). Group comparisons were not moderated by maternal age, race, education, or home visitation model. While promising, these findings are limited by the fact that a more rigorous randomized clinical trial design was not used, there was no follow-up, younger mothers were not included, and clinical moderators were not considered.
The purpose of this study was to test the efficacy of IH-CBT using a randomized clinical trial. Specifically, new mothers enrolled in a community-based home visitation program were identified using a two-step process comprised of a screen and subsequent confirmation of MDD diagnosis. Mothers were 16 years of age or older and were identified at 3 months postpartum. Mothers were randomly assigned to IH-CBT+home visiting or standard home visiting (in which mothers were permitted to obtain treatment in the community). Multiple measures of depression including clinical interviews and self-report methods were administered at pretreatment, posttreatment, and 3-month follow-up. It was hypothesized that mothers receiving IH-CBT would report lower levels of depressive symptoms, would no longer meet diagnostic criteria for MDD, and have lower levels of depressive severity than controls. It was further expected that improvements in the IH-CBT group would be sustained over the 3-month follow-up.
Method
PARTICIPANTS
Subjects consisted of 93 new mothers aged 16 or older who participated in a home visitation program, and were diagnosed with MDD. Mothers were enrolled in Every Child Succeeds, a community--based home visitation program serving Southwestern Ohio and Northern Kentucky (USA). The geographic area covered by the program included urban, suburban, and rural areas. Two models of home visitation were utilized in this program: Nurse-Family Partnership (NFP; Olds, 2010) and Healthy Families America (HFA; Holton & Harding, 2007). Participating mothers had at least one of the following demographic risk characteristics needed for eligibility: unmarried, low income, ≤18 years, inadequate prenatal care. Mothers were enrolled in home visiting prior to 28 weeks gestation in NFP as per model parameters and from 20 weeks gestation through the child reaching 3 months of age for HFA. Mothers were referred from prenatal clinics, hospitals, social service agencies, and community physicians. In the NFP home visits were provided by nurses, while in HFA home visits were provided by social workers, related professionals, and paraprofessionals. The goals of the home visitation program were to (a) improve pregnancy outcomes through nutrition education and substance use reduction; (b) support parents in providing children with a safe, nurturing, and stimulating home environment; (c) optimize child health and development; (d) link families to health care and other needed services; and (e) promote economic self-sufficiency.
Mothers were young (range was 16 to 37 years, M = 21.9, SD = 4.8), predominantly Caucasian (62.4%) and African-American (32.2%), unmarried (87.1%), and low income (76.3%<$20,000 annual household income). The breakdown of MDD severity was mild=28.0%, moderate=48.4%, and severe=23.6%. Onset of the presenting episode during postpartum (within 4 weeks after birth) was found in 29.0% of participants. Recurrent depression was reported by 74.2% of mothers: mean number of episodes=2.6 (SD = 1.6), mean age of first episode=15.2 years (SD = 5.1). Comorbidity was high, with 76.1% of participants meeting criteria for other psychiatric disorders. Representation of the five most frequent diagnoses was as follows: PTSD = 40.9%, generalized anxiety disorder = 36.6%, social phobia = 30.1%, obsessive-compulsive disorder = 26.9%, panic disorder = 25.8%.
DESIGN
A randomized clinical trial design was used with assessments at pretreatment, posttreatment, and 3-month follow-up. Participants were randomized to IH-CBT (IH-CBT+home visiting) or standard home visitation (SHV; home visiting alone) groups following the pretreatment assessment. Randomization was stratified by race and home visiting model (HFA, NFP). Within the IH-CBT group a further randomization was done to assign individuals to therapists (n=2). The randomization schedule was prepared prior to the start of the study and assignments were placed in separate envelopes that were opened sequentially.
During recruitment, 1,768 mothers were enrolled in the home visiting program and eligible to be screened for depression. Of these, 1,240 (70.1%) were screened using the Edinburgh Postnatal Depression Scale (Cox, Holden, & Sagovsky, 1987). Of those screened, 306 (24.7%) had scores of ≥11, which suggested potential MDD (Gibson et al., 2009). Among mothers with scores at or above the screening cutoff, 151 (49.3%) were referred to the study. Reasons for not being referred included already receiving treatment in the community, disinterest, and not having time to participate. No differences were found between screened and unscreened mothers, those with scores above or below the cutoff, and those referred or not referred on mother age, mother race, household income, baby age, or home visiting model (all p>.05). Mothers with scores at or above the cutoff who were referred to the study had higher EPDS scores at screening relative to those not referred, M=15.9 (SD=5.2) vs. M=14.5 (SD=3.4), t=2.8, p<.01.
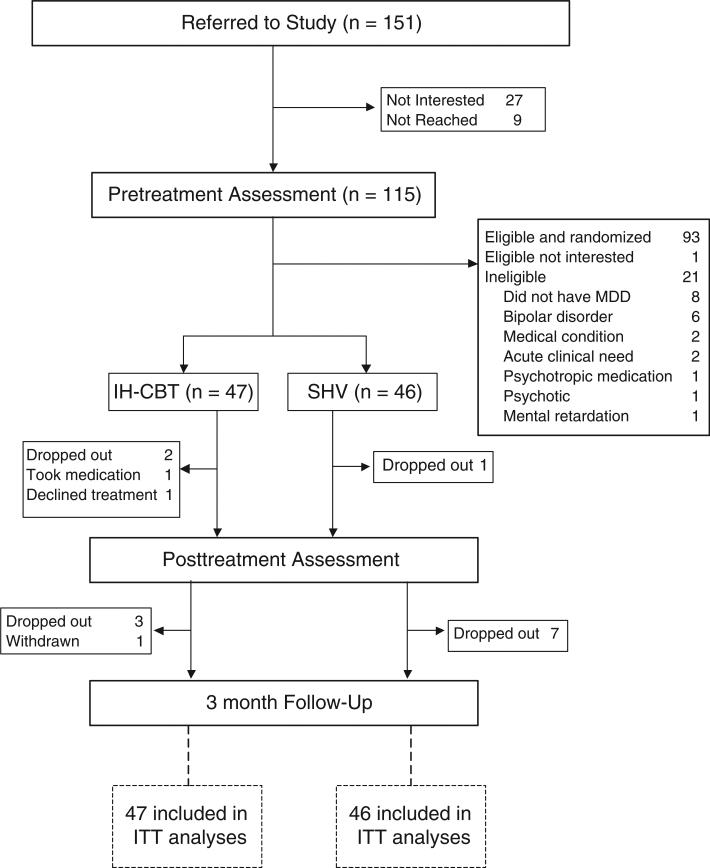
Figure 1 shows the Consort diagram through the study starting at referral. Of the 151 referred mothers (who were referred by 48 home visitors), 115 subsequently received a pretreatment assessment. Twenty-seven referred mothers were not interested in participating, and 9 were unable to be reached. There were no differences between assessed and nonassessed participants on mother age, mother race, household income, baby age, or home visiting model (all p>.05). Ninety-four of 115 participants were found to be eligible. Reasons for ineligibility were not having MDD (8), having bipolar disorder (6), medical condition contributing to psychiatric presentation (2), acute clinical need (2), taking psychotropic medication (1), psychotic (1), and mental retardation (1). One mother was disinterested in participating following the assessment but prior to randomization. The remaining 93 mothers were randomized to IH-CBT (n=47) or SVH (n=46) and comprised the intent-to-treat sample. Between pretreatment and posttreatment assessments, 1 mother in IH-CBT started medication following the 1st treatment session and another declined treatment after randomization. Three mothers dropped out of the study between pretreatment and posttreatment, and an additional 10 dropped out between posttreatment and follow-up. There were no differences in dropout rate between conditions, and dropout was unrelated to initial MDD severity, recurrent vs. single episode MDD, or psychiatric comorbidity (p>.05). One mother in IH-CBT did not receive the follow-up assessment as it coincided with the death of her child. Overall, 93.5% of participants received at least one of the posttreatment and follow-up assessments.
FIGURE 1.
Flow of participants through study. Randomization was stratified by race, home visiting model, and therapist.
PROCEDURES
Mothers were recruited in a two-step process. First, home visitors in both home visiting models administered the EPDS to mothers at 3 months postpartum. Mothers who screened positive were approached to participate in the study. Following presentation of the consent form, interested mothers received a pretreatment and eligibility assessment. Inclusion criteria were ≥16 years of age and current diagnosis of MDD. Exclusion criteria were bipolar disorder, current substance dependence, psychosis, mental retardation, suicidality, or homicidality requiring acute intervention, or current use of psychotropic medications or psychotherapy. Mothers with a history of receiving medication and/or psychotherapy but who had not received treatment in the 6 months prior to enrollment in the study were included. Assessments were conducted at pretreatment, posttreatment (about 5 months later), and 3-month follow-up. Each assessment was conducted in the home over one or two sessions. Clinical ratings and diagnoses were obtained by independent evaluators at posttreatment and follow-up assessments. Independent evaluators were third-year graduate students in clinical psychology who were trained to criterion. They were blinded to time and condition and conducted interviews with mothers separately in the home. Participants received $35 at posttreatment assessment and $45 at follow-up.
Mothers assigned to IH-CBT were not permitted to receive additional treatment during the treatment phase of the trial. Receipt of mental health treatment was documented in the SHV group at posttreatment and in both the IH-CBT and SHV groups at follow-up assessments. Mothers in the SHV group were permitted to obtain treatment in the community. Both receipt and adequacy of treatment was documented and explored in secondary analyses. Those who still met diagnostic criteria for MDD using the SCID at posttreatment had the option of receiving IH-CBT. Of the 25 SHV mothers who still had MDD and were not receiving community treatment, 13 accepted this option and received partial IH-CBT treatment between posttreatment and follow-up. The study was approved by our hospital's Institutional Review Board.
EXPERIMENTAL CONDITIONS
IH-CBT
Mothers in the IH-CBT condition received IH-CBT+home visiting (see SHV condition for description). IH-CBT was delivered in the home by two licensed master's-level social workers. Treatment consisted of 15 sessions that were scheduled weekly and lasted 60 minutes plus a booster session 1 month posttreatment. The focus and content of treatment followed the directives of CBT (J. Beck, 2011). The primary target of treatment was depression reduction. Treatment components included behavioral activation, identification of automatic thoughts and schemas, thought restructuring, and relapse prevention (Hollon & Dimidjian, 2009). Significant adaptations to CBT were made to address setting, population, and context in order to maximize engagement and outcomes (Goodheart, Kazdin, & Sternberg, 2006). These adaptations were made based upon a review of the literature, consultation with home visitors, and input from mothers in home visitation. First, IH-CBT was delivered in the home. Although CBT has been provided in the home before, there are unique challenges in administering treatment in the homes of young, low-income mothers. These require creative solutions and accommodations to ensure effective treatment delivery in environments where privacy was often difficult to guarantee, the child was present, and unexpected interruptions occurred. However, providing treatment in the home offered advantages in that many of the clinical issues that were addressed in treatment occurred in the home setting, and the therapist was able to observe elements of the home that may have been contributory to the clinical presentation. The second adaptation involved addressing the primary concerns of young, low-income, new mothers who were socially isolated (Levy & O'Hara, 2010). Treatment content focused on issues relevant to this population, such as transition to adult roles, stress management, parenting challenges, and family relationships. For the youngest mothers, additional contextual and developmental issues were incorporated into treatment (e.g., school attendance, living with parents). The third adaptation sought to facilitate close collaboration with home visitors. Collaboration occurred through written communication between therapist and home visitor utilizing a shared web-based system and telephone contact as needed. In addition, the home visitor attended the 15th session with the mother and therapist. Weekly supervision was provided by doctoral-level clinicians and included review of audiotaped sessions. Therapists completed a self-reported fidelity checklist indicating adherence to elements of CBT (e.g., use of CBT tools) and IH-CBT (e.g., contacted home visitor).
SHV
In SHV, mothers received services from home visitors as per the HFA and NFP model directives. Both models call for regular home visits during the intervals covered during the trial, and home visitors are given discretion to increase frequency of visits if needed. Curricula for both models are distinct but emphasize child health and development, nurturing mother-child relationship, maternal health and self-sufficiency, and linkage to other community services. Consistent with standard of care, mothers in the SHV condition were permitted to receive treatment for depression in the community.
INSTRUMENTS
Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I, January 2007 version; Spitzer, Williams, Gibbon, & First, 1992)
The SCID is a semistructured psychiatric interview that is widely used in research and clinical practice. It is used to diagnose 14 common psychiatric disorders, including MDD. Interviews were audio-recorded and 25% were rated by a second rater, yielding a kappa coefficient=.89. The full SCID was administered at pretreatment and the MDD portion was administered by independent evaluators at posttreatment and follow-up.
Hamilton Depression Rating Scale (HDRS; Hamilton, 1960)
The first 17 items of the HDRS were used as part of the psychiatric interview. The HDRS is a clinician rating that consists of depressive symptoms that are recorded using 5- or 3-point scales reflecting presence and severity over the past week. Interviews were audio-recorded and 25% were rated by a second rater, yielding an intraclass correlation coefficient of .93. The HDRS was administered at pretreatment and by independent evaluators at posttreatment and follow-up.
Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987)
The EPDS is a 10-item self-report measure of depressive symptoms. Items consist of depressive symptoms that are endorsed on a 4-point scale indicating occurrence and severity over the past week, yielding a total score. The EPDS was used to screen mothers for eligibility for the full assessment using a cutoff of ≥11. The EPDS was also administered at pretreatment, posttreatment, and follow-up.
Beck Depression Inventory-II (BDI-II; A. Beck, Steer, & Brown, 1996)
The BDI-II is one of the most widely used self-report screens of depressive symptomatology, with strong reliability and validity properties. It consists of 21 items indicating presence of symptoms over the past 2 weeks by endorsing one of four statements reflecting severity, yielding a total score. The BDI-II was administered at pretreatment, posttreatment, and follow-up.
Global Assessment of Functioning Scale (GAF; American Psychiatric Association, 1994)
The GAF is a 100-point scale divided into 10 categories reflecting degree of adaptive functioning. This widely used index is frequently applied in conjunction with standardized psychiatric interviews, and has demonstrated acceptable psychometrics (Jones, Thornicroft, Coffey, & Dunn, 1995). Twenty-five percent of audio-recorded interviews were rated by a second rater, yielding an intraclass correlation coefficient of .84. The GAF was administered at the pretreatment assessment and by independent evaluators at posttreatment and follow-up.
Outside Treatment Tracking Form (OTTF)
The OTTF was developed to track the receipt of mental health treatment obtained in the community. At pretreatment, it was used to confirm that mothers were not already receiving psychiatric treatment. At posttreatment and follow-up, it was used to document receipt of psychological or medical treatments, including type, dosage, and length of treatment. These data were used to create a categorical variable describing receipt and adequacy of treatment between pre- and posttreatment and posttreatment and follow-up. For medication, adequate treatment was defined as receiving an approved antidepressant and maintenance for at least 2 months, and for psychological treatment as receiving psychotherapy for at least 4 sessions over 2 months.
Consumer Satisfaction
Mothers in the IH-CBT condition and their home visitors completed surveys to ascertain their satisfaction with treatment. Each item consisted of a statement about the treatment that was endorsed using a 5-point scale of agreement (1 = strongly agree, 5 = strongly disagree). The survey addressed general features of treatment (“therapist answered my questions”), specific elements of IH-CBT (“therapist and home visitor worked together”), and other benefits of treatment (“I am more confident about caring about my child”).
Results
OVERVIEW OF ANALYSES
An intent-to-treat approach was used such that all randomized subjects were included in analyses. As groups did not differ on demographics and baseline clinical features, these were not included as covariates. Therapist, single episode vs. recurrent MDD, and comorbidity were examined as moderators of treatment outcomes. Primary analyses used linear mixed effect regression with restricted maximum likelihood estimation. This approach accounts for missing data and uses all data in estimating effects (Verbeke & Molenberghs, 2000). The basic model included terms for group assignment (IH-CBT or SHV), time (pretreatment, posttreatment, and follow-up) and the interaction between group and time. Different correlation structures for the repeated measurements were explored and compared using a goodness of fit test. When a significant Time×Group interaction term was observed, we conducted follow-up analyses by dividing the data on the level of the interaction variables and reporting the corresponding least square means, which are the predicted means derived from the fitted model. Effect size measures were generated using the least square means and corresponding standard errors along the respective sample size for each group that resulted from fitting the mixed model based on the intent-to-treat sample. Following these, the magnitude of effect sizes for those who completed the treatment and those who did not were also described. Since we are investigating multiple outcomes, the reported p-values for the main analysis were adjusted using a false discovery rate methodology (Benjamini & Hochberg, 2000). PROC MIXED was used for the continuous data and PROC GENMOD with a logit link function and generalized estimating equations was used to analyze the dichotomous MDD variable (SAS version 9.3). Finally, consumer satisfaction in the IH-CBT group and receipt of community treatment in the SHV group were examined descriptively.
SAMPLE CHARACTERISTICS
Table 1 shows the demographics of the two groups. No differences were found between treatment and control groups on these variables. There were no differences between groups on the risk variables (unmarried, low income, ≤18 years, inadequate prenatal care) used to determine eligibility for the home visiting program. In terms of home visitation model, 81 mothers were in the HFA model and 12 in the NFP model. Eighty-five mothers were primiparous and 8 had more than one child (all of these were in the HFA model). Mothers received a mean of 13.9 (SD = 9.2) home visits prior to assessment. No differences were found on one vs. multiple children, χ2 (1)=0.0, p>.05, or number of home visits received, t(91)=1.2, p>.05. Groups were equivalent on home visitor training and education.
Table 1.
Demographic Characteristics of IH-CBT (n=47) and SHV (n=46) Participants
| Variable | IH-CBT Condition |
SHV Condition |
t or x2 | p-value |
|---|---|---|---|---|
| Mean (SD) or N (%) | Mean (SD) or N (%) | |||
| Mother Age (years) | 22.4 (5.2) | 21.5 (3.9) | 0.9 | ns |
| Mother Race | ||||
| White | 30 (63.8%) | 28 (60.8%) | 1.2 | ns |
| African American | 14 (29.9%) | 16 (34.8%) | ||
| Native American | 1 (2.1%) | 0 (0.0%) | ||
| Native Hawaiian or other Pacific Islander | 1 (2.1%) | 1 (2.2%) | ||
| Bi-racial | 1 (2.1%) | 1 (2.2%) | ||
| Mother Ethnicity | ||||
| Latina | 3 (6.4%) | 4 (8.7%) | 0.5 | ns |
| None | 44 (93.6%) | 42 (91.3%) | ||
| Marital Status | ||||
| Single, Never Married | 41 (87.2%) | 39 (84.8%) | 1.0 | ns |
| Married | 6 (12.8%) | 6 (13.0%) | ||
| Separated | 0 (0.0%) | 1 (2.2%) | ||
| Education (years) | 11.6 (2.0) | 11.3 (1.7) | 1.0 | ns |
| Income | ||||
| $0-9,999 | 27 (57.4%) | 25 (54.3%) | 6.8 | ns |
| $10,000-19,999 | 7 (14.9%) | 13 (28.3%) | ||
| $20,000-29,999 | 10 (21.3%) | 4 (8.7%) | ||
| $30,000-39,999 | 2 (4.3%) | 1 (2.2%) | ||
| $40,000-49,999 | 0 (0.0%) | 2 (4.3%) | ||
| >$50, 000 | 1 (2.1%) | 1 (2.2%) | ||
| Child's age (days) | 159.8 (73.7) | 146.1 (74.4) | 0.9 | ns |
MODERATING VARIABLES
Recurrent depression (single episode vs. recurrent MDD), initial MDD severity, presence of a comorbid psychiatric disorder, home visiting model, and home visitor were examined as moderating variables by including them in the mixed model as main effects and in all two- and three-way interactions. These variables were found to be nonsignificant on all outcome variables (p>.05). In the IH-CBT condition, no significant differences were found between therapists on baseline subject demographic and clinical characteristics and on all outcome variables.
GROUP COMPARISONS
Groups were compared on the two self-report measures of depression (BDI-II and EPDS), clinician ratings of depression severity (HDRS), diagnosis of MDD, and GAF scores of functioning. Table 2 presents the means, SDs, numbers/percentages, t-values, and χ2 value (for MDD diagnosis) for IH-CBT and SHV groups across the three time points (pretreatment, posttreatment, follow-up). The result of the test of interaction between group and time is also given by F- or χ2 values. All measures except MDD diagnosis were analyzed using a linear mixed effect model where time (pretreatment, posttreatment, follow-up), treatment group (IH-CBT, SHV) and the Time×Group interaction were predictor variables. MDD diagnosis was analyzed using generalized linear model with logit link function and estimating equation approach. For all outcomes except MDD diagnosis, the interaction term was statistically significant, indicating that the change between the two groups differed depending on the particular time. Specifically, mothers receiving IH-CBT reported lower levels of self-reported depression, received lower clinician ratings of depressive severity, and demonstrated increased overall functioning over time relative to those in the SHV group. Subsequently, t-tests and X2 analyses were conducted to compare groups at each time point and to compare scores and proportions between each time point within groups. Results indicated that the two groups did not differ at baseline on all measures, but IH-CBT and SHV mothers were statistically different (p<.01) at posttreatment and follow-up. For both groups, there were statistically significant (p<.01) reductions in depression measures and improved overall functioning from pretreatment to posttreatment and pretreatment to follow-up, although no changes from posttreatment to follow-up. Thus, the impact of IH-CBT was realized from pretreatment to posttreatment and maintained over 3-month follow-up. For MDD diagnosis, a significant effect for group was found (p<.01) such that, relative to those in SHV, mothers in the IH-CBT were less likely to receive a diagnosis at posttreatment (29.3% vs. 69.8%) and follow-up (20.5% vs. 52.6%).
Table 2.
Comparisons Between IH-CBT (N=47) and SHV (N=46) Groups on Depression Measures and Overall Functioning at Each Time Point
| Group |
t or χ2 | F or χ2 |
|||||
|---|---|---|---|---|---|---|---|
| Measure | Assessment | IH-CBT |
SHV |
Group × Time | |||
| Mean/N | SD/% | Mean/N | SD/% | ||||
| BDI-II | Pre | 33.11 | 9.90 | 34.54 | 10.04 | -0.70 | 7.87** |
| Post | 12.70 | 15.44 | 26.51 | 13.49 | -4.35*** | ||
| Follow-up | 12.31 | 13.71 | 21.74 | 14.91 | -2.89** | ||
| EPDS | Pre | 18.77 | 3.96 | 19.22 | 4.07 | -0.54 | 7.39** |
| Post | 9.49 | 7.35 | 15.26 | 5.47 | -4.09*** | ||
| Follow-up | 8.59 | 7.22 | 13.24 | 8.20 | -2.64* | ||
| HDRS | Pre | 21.87 | 4.37 | 21.96 | 4.40 | -0.09 | 9.23** |
| Post | 8.71 | 7.86 | 15.05 | 8.24 | -3.61** | ||
| Follow-up | 7.28 | 6.47 | 12.21 | 8.32 | -2.91** | ||
| GAF | Pre | 55.51 | 6.29 | 56.11 | 6.44 | -0.45 | 7.40** |
| Post | 72.22 | 13.88 | 63.23 | 12.18 | 3.16** | ||
| Follow-up | 73.41 | 13.48 | 65.39 | 12.98 | 2.66* | ||
| MDD | Pre | 47 | 100.0% | 46 | 100.0% | 0.44 | |
| Post | 12 | 29.3% | 30 | 69.8% | 13.8*** | ||
| Follow-up | 8 | 20.5% | 20 | 52.6% | 8.6** | ||
Note. BDI-II=Beck Depression Inventory-II; EPDS=Edinburgh Postnatal Depression Scale; HDRS=Hamilton Depression Rating Scale; GAF=Global Assessment of Functioning Scale; MDD=Major Depressive Disorder diagnosis from SCID-I.
p<0.05
p<0.01
p<0.001 (p-values are FDR adjusted). χ2 test is for MDD diagnosis.
Table 3 shows the effect sizes based on least-squared means (for BDI-II, EPDS, HDRS, GAF and adjusted odds-ratios; MDD diagnosis) between groups at pretreatment, posttreatment and follow-up. At posttreatment, effect sizes range from 0.65 to 0.90 indicating medium to large effects. ORs for MDD diagnosis were 0.18 at posttreatment and 0.23 at follow-up, reflecting a substantial reduction in MDD diagnosis in IH-CBT relative to SHV mothers.
Table 3.
Effect Size Estimates for Comparison between IH-CBT and SHV for All Subjects (N=93), and for Those with Complete (n=23) and Partially Complete (n=24) Sessions of IH-CBT
| All subjects | Completers | Partial Completers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time |
Time |
|||||||||
| Post |
Follow-up |
Post |
Follow- up |
Post |
Follow- up |
|||||
| Mean difference | SD | ES | Mean difference | SD | ES | ES | ES | ES | ES | |
| BDI-II | -13.81 | 3.18 | 0.90 | -9.43 | 3.26 | 0.60 | 1.51 | 0.92 | 0.44 | 0.30 |
| EPDS | -5.77 | 1.41 | 0.84 | -4.65 | 1.76 | 0.55 | 1.27 | 0.75 | 0.54 | 0.32 |
| HDRS | -6.34 | 1.76 | 0.75 | -4.93 | 1.70 | 0.60 | 1.02 | 0.78 | 0.46 | 0.38 |
| GAF | 8.99 | 2.85 | 0.65 | 8.02 | 3.02 | 0.55 | 0.89 | 0.77 | 0.46 | 0.34 |
| MDD* | -1.72 | 0.48 | 0.18 | -1.46 | 0.51 | 0.23 | 0.12 | 0.09 | 0.28 | 0.45 |
Note. BDI-II=Beck Depression Inventory-II; EPDS=Edinburgh Postnatal Depression Scale; HDRS=Hamilton Depression Rating Scale; GAF=Global Assessment of Functioning Scale; MDD=Major Depressive Disorder diagnosis from SCID-I.
values are the coefficient for the main effect of group and the ES is the odds ratio.
TREATMENT COMPLETION AND EFFECT SIZES
Overall, mothers receiving IH-CBT had a mean of 11.2 (SD=5.5) sessions. In order to examine the impacts of treatment based on completion status, mothers in the IH-CBT group were divided into those who received 15 sessions and booster (completers, n=23) and those who received 14 or fewer sessions (partial completers, n=24). The small numbers of subjects in the partial completers subgroup precluded examination of treatment effects based on number of sessions. Partial completers received a mean of 7.3 (SD=5.5) sessions. Effect sizes were determined for completers and partial completers at posttreatment and follow-up; these are presented in Table 3, in addition to effect sizes for the sample as a whole. Effect sizes for continuous variables were based on least-square means, and for the binary variable of MDD diagnosis the adjusted odds ratio is shown. Comparisons of completers and partial completers indicates substantially larger effect sizes for all variables at each time point for mothers who received the full allotment of sessions in contrast to those who received fewer sessions than intended. However, partial completers had effect sizes in the small to moderate ranges, indicating that incomplete receipt of IH-CBT imparted benefits relative to untreated controls.
CONSUMER SATISFACTION
Results of the surveys given to mothers in the IH-CBT condition and their home visitors indicated broad endorsement of satisfaction with program elements. Mothers were particularly pleased (strongly agree or agree) with the site of treatment (100.0%) and the flexibility in scheduling (100.0%) that it entailed. Both mothers and home visitors were satisfied with unique elements of IH-CBT, including therapist-home visitor collaboration (87.5%, 86.7%) and maintenance of confidentiality (95.8%, 93.3%). In terms of secondary benefits from their perspectives, mothers stated that they were more confident in caring for their child (85.5%), more effective as parents (85.4%), and felt emotionally closer to their child (83.3%).
RECEIPT OF TREATMENT IN THE SHV CONDITION
Results indicated that 34.9% of SHV mothers utilized treatment in the community between pretreatment and posttreatment— 20.9% received medication and 16.3% received psychotherapy. Using predetermined criteria for adequacy, only 7.0% of all SHV mothers received appropriate and sufficient treatment during this interval. Between posttreatment and follow-up, 44.7% received treatment (18.4% received medication and 36.8% received psychotherapy). Using the same predetermined criteria for adequacy and taking into account mothers who began treatment during the prior interval and continued through the follow-up phase, 15.8% of mothers received treatment that was deemed appropriate and sufficient during this interval.
Discussion
This is the first study documenting the efficacy of an adapted and augmented treatment specifically designed for postpartum depression in mothers participating in home visitation prevention programs. Given that mothers in home visitation typically exhibit numerous risk factors for MDD, and studies have documented high rates of clinically significant depression in this population that otherwise go untreated, development of an efficacious treatment is noteworthy. This study found that depressed mothers receiving IH-CBT and concurrent home visiting had substantial improvements relative to home visiting alone in diagnosed MDD, self-reported depressive symptoms, and clinician ratings of depressive symptoms and overall functioning. Moreover, these improvements were sustained at 3 months follow-up. The convergence of findings from multiple sources and measures establishes the strong impact of IH-CBT. Indeed, effect sizes are comparable to those found in trials of CBT with other populations (Hollon, Stewart, & Strunk, 2006) and with antidepressant medications (Kirsch et al., 2008). The fact that SHV mothers had a higher rate of accessing mental health care than what is typically observed in home visiting, and some crossed over to IH-CBT at posttreatment, this control condition represents a more stringent comparison for IH-CBT and underscores the impact of the intervention. Additionally, treatment outcomes were not moderated by therapist, maternal age, race, number of children, home visitation model, other comorbidities, or type of MDD (single episode vs. recurrent). These findings suggest that IH-CBT is broadly applicable and generalizable to other programs.
Also encouraging was the relatively high rate of treatment completion (48.9%). Indeed, mothers receiving IH-CBT had an average of 11.2 sessions (SD=5.5), a substantially higher dose of treatment relative to the average of 4.3 sessions (SD=3.5) in adult outpatient settings (Hansen, Lambert, & Forman, 2002). Taken together, efforts to address the mental health needs of depressed mothers in home visitation are likely to be more successful if treatment is provided in the home under the aegis of home visitation programs in contrast to overhauling complex and often unwieldy community mental health systems.
Examination of effect sizes for mothers who completed or partially completed IH-CBT suggests that receiving the full allotment of sessions was beneficial in terms of reduction in depressive symptoms and decreased likelihood of receiving an MDD diagnosis at posttreatment and follow-up. While this pattern has been documented in prior research with CBT for depression (Saatsi, Hardy, & Cahill, 2007) these comparisons must be interpreted cautiously as it is possible that differences between completers and partial completers may be due to variables other than treatment dose, such as motivation or other non-specific influences. Although partial completers showed some improvement relative to controls, effect sizes were one third to one half as large as those found for completers. This is consistent with the theoretical foundation of CBT and IH-CBT in particular, which states that sufficient time in treatment is required to learn, apply, and master new skills in mood management. This may be especially true with new mothers who have demographic and clinical risks and may require more intensive treatment to yield substantial changes in depression (Forman et al., 2007; Nanni, Uher, & Danese, 2012).
A number of authors have called for adapting treatments to specific populations and settings to enhance engagement and effectiveness (Barrera et al., 2012). In addition, home-based treatments for postpartum depression have been found to be less effective for low-income mothers (Leis et al., 2009), which may be attributable in part to inadequate adaptation to the unique needs of this population. Feedback from mothers and home visitors indicates that the novel adaptations to treatment that were made in IH-CBT were well-received. Both mothers and home visitors were satisfied with the explicit collaborative relationship between home visitors and therapists, and mothers clearly valued the delivery of treatment in the home setting. It is probable that the efficacy of the treatment was related to the focus on content that was especially relevant to young, low-income new mothers in home visitation. By having trained therapists provide treatment concurrent with home visitation, the home visitor was not required to reduce or alter home visitation curricula. In addition, there were no differences between conditions on number of home visits received during the treatment and follow-up intervals, indicating that the addition of a therapist in IH-CBT did not interfere with fully participating in home visitation.
Research has consistently demonstrated that depressed mothers in home visitation infrequently obtain mental health care in the community, despite the efforts of home visitors to link them to such services (Ammerman et al., 2010). Only 34.9% of mothers in the SHV condition obtained mental health treatment in the community between pretreatment and posttreatment, and of these just 18.8% met predetermined criteria for adequacy. Yet this is higher than the 14.4% of depressed mothers in home visiting who received mental health treatment during a 9-month interval in a naturalistic study (Ammerman et al., 2009). The greater access to care may be due to home visitors being more aware of the clinical condition of mothers, or of mothers being more motivated to seek treatment in the context of participating in a clinical trial. Regardless, the rate of accessing care is still small, and it rarely led to receipt of effective and sufficient treatment. The low levels further underscore the need for providing treatment in the home. The barriers faced by mothers in obtaining treatment in the community are many. Inconsistent transportation, lack of insurance, delays in care (particularly among mothers receiving Medicaid), limited provider options, and decreasing number of care providers impedes access to effective treatment (Bao et al., 2011; Miranda et al., 2003).
The study had a number of strengths. First, the design provided a rigorous framework within which to examine IH-CBT. Given that many home visitation programs have made investments in approaches that are untested and may be ineffective, this study offers evidence for a treatment approach that benefits depressed women in this type of program. Findings are generalizable to low-income, socially isolated mothers, who in turn reflect the largest population enrolled in home visiting programs. Second, the use of multiple measures and data collection methods allows examination of the convergence of findings. This is in contrast to the sole reliance on single self-report measures that characterizes much of the research on maternal depression in home visitation. In addition, this measurement strategy facilitates comparison of findings from this study to the numerous other investigations of treatment of maternal depression that rely on diverse measures. Third, diagnostic interviews and HDRS assessments were blinded at posttreatment and follow-up. Fourth, an intent-to-treat strategy was used and retention of the sample was good, particularly for this high-risk population. Fifth, two widely disseminated models of home visitation were represented in the sample. IH-CBT was designed to fit seamlessly with different home visiting models, and the fact that model did not moderate response to treatment provides support that IH-CBT is efficacious across multiple approaches and is generalizable to other home visiting programs. Sixth, feedback about treatment was obtained from both mothers and home visitors. Querying both types of consumer, particularly about unique features of the treatment that constitute important new adaptations (e.g., privacy, confidentiality, setting), provides important information about social validity in the context of a complex, multiprovider social service program.
The study also has several limitations that warrant caution in interpreting findings. First, the sample size was relatively small, limiting power particularly for moderating analyses. However, effect sizes for moderating variables were small and statistically non-significant. Second, no observational measures were used, precluding examination of changes in specific skills or behaviors. Third, there was no long-term follow-up. It is not known if gains were sustainable beyond the 3-month follow-up time point, a period in which risk for relapse is high (Hollon & Dimidjian, 2009). However, confirming maintenance of gains at 3 months following treatment is an important step in establishing treatment efficacy and provides justification for future research on longer term impacts. Fourth, although comparing IH-CBT to a “treatment as usual” condition such as SHV is informative, it is possible that the addition of a second person in the form of therapist may have accounted for some of the benefits of IH-CBT relative to controls. Yet, while we did not control for additional contact in the design, it is unlikely that this factor explains the findings. There is little evidence that nonspecific social interaction imparts much benefit to adults with MDD and research has consistently found that interactions with a home visitor alone lead to little or no improvement in depression. Fifth, some mothers in the SHV condition received treatment in the intervals between pretreatment, posttreatment, and follow-up. This was by design in that the SHV condition reflected “home visiting as usual” in which mothers were permitted to obtain community treatment. As noted, only a small minority received adequate treatment. Likewise, some SHV mothers crossed over to IH-CBT at posttreatment. To the extent that community treatment or crossing over may have benefited some mothers in the SHV condition, this provides a more conservative test of the efficacy of IH-CBT. Sixth, because some home visitors had mothers in both IH-CBT and SHV conditions, there is a risk of contamination. Such a confound would mitigate effect sizes and it is unlikely that this was a significant concern given the robustness of the superiority of IH-CBT to home visiting alone. Moreover, none of the home visitors were taught CBT strategies, and it is improbable that they would acquire such skills simply by having mothers in treatment. And seventh, findings may not be generalizable to mothers with higher levels of social resources.
CONCLUSIONS
Results from this study add to the growing body of literature demonstrating that systematic adaptations to evidence-based treatments have the potential to yield clinically meaningful and efficacious treatment for high-risk populations. IH-CBT provides a compelling option for new mothers enrolled in home visitation. Modifications to treatment implementation break down barriers to access, take advantage of other care providers already in the home to foster strong working relationships, and address salient needs in this population. IH-CBT is feasible and lends itself to adoption by other home visitation programs. Use of master's-level therapists is cost-effective and provides a growing pool of professionals from which home visitation programs can draw. CBT is among the most widely trained evidence-based treatments (Norcross, Hedges, & Prochaska, 2002), further contributing to a sufficient source of potential therapists. Integrated doctoral-level supervision supports therapists in addressing the complex needs of depressed mothers with comorbidities and significant trauma histories. IH-CBT has the potential to expand access to effective treatment to mothers with MDD who otherwise face overwhelming barriers to care.
Acknowledgments
Supported by Grant R34MH073867 from the National Institute of Mental Health. The authors acknowledge the participation and support of The Health Foundation of Greater Cincinnati, United Way of Greater Cincinnati, Kentucky H.A.N.D.S., Ohio Help Me Grow, and www.OhioCanDo4Kids.org. The authors thank Drs. Neil M. Richtand, Lawson R. Wulsin, and Floyd R. Sallee for their assistance to the study.
Contributor Information
Robert T. Ammerman, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine
Frank W. Putnam, University of North Carolina School of Medicine and Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine
Mekibib Altaye, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine.
Jack Stevens, Nationwide Children's Hospital, Ohio State University College of Medicine.
Angelique R. Teeters, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine
Judith B. Van Ginkel, Cincinnati Children's Hospital Medical Center, University of Cincinnati College of Medicine
References
- Administration on Children Youth and Families . Making a difference in the lives of children and families: The impacts of Early Head Start Programs on infants and toddlers and their families. U.S. Department of Health and Human Services; Washington, DC: 2002. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Ammerman RT, Bodley AL, Putnam FW, Lopez WL, Holleb LJ, Stevens J, Van Ginkel JB. In-Home Cognitive Behavior Therapy for a depressed mother in a home visitation program. Clinical Case Studies. 2007;6(2):161–180. http://dx.doi.org/10.1177/1534650106286533. [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Chen L, Holleb LJ, Stevens J, Van Ginkel JB. Changes in depressive symptoms in first time mothers in home visitation. Child Abuse & Neglect. 2009;33(3):127–138. doi: 10.1016/j.chiabu.2008.09.005. http://dx.doi.org/10.1016/j.chiabu.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Bosse NR, Teeters AR, Van Ginkel JB. Maternal depression in home visitation: A systematic review. Aggression and Violent Behavior. 2010;15(3):191–200. doi: 10.1016/j.avb.2009.12.002. http://dx.doi.org/10.1016/j.avb.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Chard KM, Stevens J, Van Ginkel JB. PTSD in depressed mothers in home visitation. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(2):186–195. doi: 10.1037/a0023062. http://dx.doi.org/10.1037/a0023062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Stevens J, Bosse NR, Short JA, Bodley AL, Van Ginkel JB. An open trial of In-Home CBT for depressed mothers in home visitation. Maternal and Child Health Journal. 2011;15(8):1333–1341. doi: 10.1007/s10995-010-0691-7. http://dx.doi.org/10.1007/s10995-010-0691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astuto J, Allen L. Home visitation and young children: An approach worth investing in? Society for Research in Child Development, Social Policy Report. 2009;23:3–22. [Google Scholar]
- Bao Y, Alexopoulos GS, Casalino LP, Ten Have TR, Donohue JM, Post EP, Bruce ML. Collaborative depression care management and disparities in depression treatment and outcomes. Archives of General Psychiatry. 2011;68(6):627–636. doi: 10.1001/archgenpsychiatry.2011.55. http://dx.doi.org/10.1001/archgenpsychiatry.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera M, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: A progress report. Journal of Consulting and Clinical Psychology. 2012 doi: 10.1037/a0027085. [Online publication January 30, 2012]. http://dx.doi.org/10.1037/a0027085. [DOI] [PMC free article] [PubMed]
- Beck AT, Steer RA, Brown GK. BDI-II Manual. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Beck JS. Cognitive behavior therapy: Basics and beyond. 2nd ed. Guilford; New York, NY: 2011. [Google Scholar]
- Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics. 2000;25:60–83. [Google Scholar]
- Boller K, Strong DA. Home visiting: Looking back and moving forward. Zero to Three. 2010;30(6):4–9. [Google Scholar]
- Chazan-Cohen R, Ayoub C, Pan BA, Roggman L, Raikes H, McKelvey L, Hart A. It takes time: Impacts of Early Head Start that lead to reductions in maternal depression two years later. Infant Mental Health Journal. 2007;28:151–170. doi: 10.1002/imhj.20127. http://dx.doi.org/10.1002/imhj.20127. [DOI] [PubMed] [Google Scholar]
- Cohen LS, Wang B, Nonacs R, Viguera AC, Lemon EL, Freeman MP. Treatment of mood disorders during pregnancy and postpartum. Psychiatric Clinics of North America. 2010;33:273–293. doi: 10.1016/j.psc.2010.02.001. http://dx.doi.org/10.1016/j.psc.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Conner-Smith JK, Weisz JR. Applying treatment outcome research in clinical practice: Techniques for adapting interventions to the real world. Child and Adolescent Mental Health. 2003;8:3–10. doi: 10.1111/1475-3588.00038. http://dx.doi.org/10.1111/1475-3588.00038. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Duggan AK, Berlin LJ, Cassidy J, Burrell L, Tandon SD. Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at-risk mothers and infants. Journal of Consulting and Clinical Psychology. 2009;77:788–799. doi: 10.1037/a0015709. http://dx.doi.org/10.1037/a0015709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan A, Fuddy L, Burrell L, Higman SM, McFarlane E, Windham A, Sia C. Randomized trial of a statewide home visiting program to prevent child abuse: Impact in reducing parental risk factors. Child Abuse & Neglect. 2004;28:623–643. doi: 10.1016/j.chiabu.2003.08.008. http://dx.doi.org/10.1016/j.chiabu.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Duggan A, Fuddy L, McFarlane E, Burrell L, Windham A, Higman S, Sia C. Evaluating a statewide home visiting program to prevent child abuse in at-risk families of newborns: Fathers’ participation and outcomes. Child Maltreatment. 2004;9(1):3–17. doi: 10.1177/1077559503261336. http://dx.doi.org/10.1177/1077559503261336. [DOI] [PubMed] [Google Scholar]
- Forman DR, O'Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19:585–602. doi: 10.1017/S0954579407070289. http://dx.doi.org/10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica. 2009;119(5):350–364. doi: 10.1111/j.1600-0447.2009.01363.x. http://dx.doi.org/10.1111/j.1600-0447.2009.01363.x. [DOI] [PubMed] [Google Scholar]
- Goodheart CD, Kazdin AE, Sternberg RJ, editors. Evidence-based psychotherapy: Where practice and research meet. American Psychological Association; Washington, DC: 2006. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen NB, Lambert MJ, Forman EM. The psychotherapy dose-response effect and its implications for treatment delivery services. Clinical Psychology: Science and Practice. 2002;9:329–343. http://dx.doi.org/10.1093/clipsy.9.3.329. [Google Scholar]
- Hollon SD, Dimidjian S. Cognitive and behavioral treatment of depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2nd ed. Guilford; New York, NY: 2009. pp. 586–603. [Google Scholar]
- Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Psychology. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. http://dx.doi.org/10.1146/annurev.psych.57.102904.190044. [DOI] [PubMed] [Google Scholar]
- Holton JK, Harding K. Healthy Families America: Ruminations on implementing a home visitation program to prevent child maltreatment. Journal of Prevention and Intervention in the Community. 2007;34(1–2):13–38. doi: 10.1300/J005v34n01_02. http://dx.doi.org/10.1300/J005v34n01_02. [DOI] [PubMed] [Google Scholar]
- Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). British Journal of Psychiatry. 1995;166(5):654–659. doi: 10.1192/bjp.166.5.654. [DOI] [PubMed] [Google Scholar]
- Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: A meta-analysis of data submitted to the Food and Drug Administration. PLoS Medicine. 2008;5(2):e45. doi: 10.1371/journal.pmed.0050045. http://dx.doi.org/10.1371/journal.pmed.0050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsverk J, Carrilio T, Connelly CD, Granger WC, Slymen DJ, Newton RR, Jones C. Healthy Familes San Diego clinical trial: Technical report. San Diego Children's Hospital and Health Center; San Diego: 2002. [Google Scholar]
- Leis JA, Mendelson T, Tandon DS, Perry DF. A systematic review of home-based interventions to prevent and treat postpartum depression. Archives of Women's Mental Health. 2009;12:3–13. doi: 10.1007/s00737-008-0039-0. http://dx.doi.org/10.1007/s00737-008-0039-0. [DOI] [PubMed] [Google Scholar]
- Levy LB, O'Hara MW. Psychotherapeutic interventions for depressed, low-income women: A review of the literature. Clinical Psychology Review. 2010;30(8):934–950. doi: 10.1016/j.cpr.2010.06.006. http://dx.doi.org/10.1016/j.cpr.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: A randomized control trial. Journal of the American Medical Association. 2003;290:57–65. doi: 10.1001/jama.290.1.57. http://dx.doi.org/10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. American Journal of Psychiatry. 2012;169(2):141–151. doi: 10.1176/appi.ajp.2011.11020335. http://dx.doi.org/10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- Norcross JC, Hedges M, Prochaska JO. The Face of 2010:A Delphi Poll on the future of psychotherapy. Professional Psychology: Research and Practice. 2002;23(3):316–322. http://dx.doi.org/10.103//0735-7028.33.3.316. [Google Scholar]
- Olds DL. The Nurse-Family Partnership: From trials to practice. In: Reynolds AJ, Rolnick AJ, Englund MM, Temple JA, editors. Childhood programs and practices in the first decade of life: A human capital integration. Cambridge University Press; New York, NY: 2010. pp. 49–75. [Google Scholar]
- Saatsi S, Hardy G, Cahill J. Predictors of outcome and completion status in cognitive therapy for depression. Psychotherapy Research. 2007;2(17):189–200. [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Stevens J, Ammerman RT, Putnam FW, Gannon TA, Van Ginkel JB. Facilitators and barriers to engagement in home visitation: A qualitative analysis of maternal, provider, and supervisor data. Journal of Aggression, Maltreatment, and Trauma. 2005;11(4):75–93. [Google Scholar]
- Sweet MA, Appelbaum MI. Is home visiting an effective strategy? A meta-analytic review of home visiting programs for families with young children. Child Development. 2004;75(5):1435–1456. doi: 10.1111/j.1467-8624.2004.00750.x. http://dx.doi.org/10.1111/j.1467-8624.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- Tandon SD, Parillo K, Mercer C, Keefer M, Duggan AK. Engagement in paraprofessional home visitation: Families’ reasons for enrollment and program response to identified reasons. Womens Health Issues. 2008;18(2):118–129. doi: 10.1016/j.whi.2007.10.005. http://dx.doi.org/10.1016/j.whi.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Tandon SD, Parillo KM, Jenkins C, Duggan AK. Formative evaluation of home visitors’ role in addressing poor mental health, domestic violence, and substance abuse among low-income pregnant and parenting women. Maternal and Child Health Journal. 2005;9:273–283. doi: 10.1007/s10995-005-0012-8. http://dx.doi.org/10.1007/s10995-005-0012-8. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. Springer; New York, NY: 2000. [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, Research Network on Youth Mental Health Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry. 2012;69(3):274–282. doi: 10.1001/archgenpsychiatry.2011.147. http://dx.doi.org/10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]