INTRODUCTION
Osteoarticular tuberculosis, especially in the foot is uncommon.1 It makes up less than 3% of cases of extra-pulmonary tuberculosis. As such, it has remained a diagnostic enigma despite improvements in investigative technology.1–4 It is an aggressive disease. Any significant delay in diagnosis may lead to spread of the infection from bone into adjacent joints and surrounding soft tissue. This leads to significant functional disability.1,4
CASE REPORT
A 36-year-old South Indian priest attended the orthopaedic department with a 1-year history of spontaneous onset right foot pain. There was no history of trauma or any systemic symptoms that may indicate infection. By the time of presentation he had been living in the UK for over 5 years. His symptoms were affecting his work as a priest as footwear was not permitted in his temple.
On examination there was mild smooth swelling over the dorsal aspect of the midfoot and also diffuse hindfoot swelling. Initial radiographs showed non-specific changes in the right second tarsometatarsal joint with mild cystic change and osteopaenia. (Figure 1).
Figure 1.
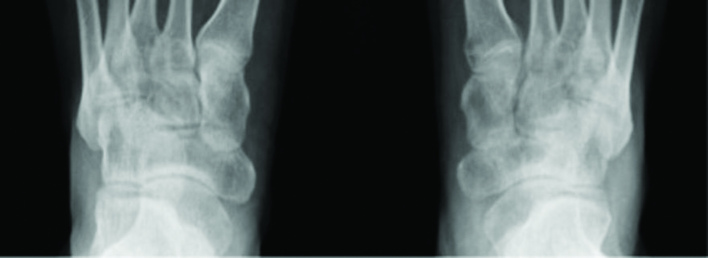
Plain antero-posterior radiograph. Loss of definition of cortices in the tarsometatarsal joint of the right foot compared to the left. Mild osteopaenia and cystic changes.
Magnetic resonance imaging (MRI) demonstrated a soft tissue mass arising from the second and third tarsometatarsal joints with associated bone destruction and soft tissue expansion. (Figure 2).
Figure 2.
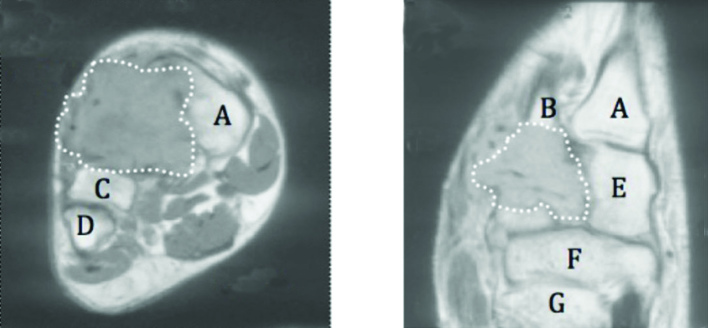
Magnetic resonance imaging. a) coronal and b) axial sections through right mid foot demonstrating soft tissue mass obliterating second and third tarsometatarsal joints (delineated by dotted line). Key: A: first metatarsal, B: second metatarsal, C: third metatarsal, D: fourth metatarsal, E: medial cuneifrom, F: navicular, G: talus.
The lack of significant inflammatory change suggested a locally aggressive lesion of possible neoplastic origin.
Due to lack of diagnostic clarity, further tissue diagnosis was sought with appropriately planned biopsy for histology and culture to include atypical organisms.
Initial acid-fast bacilli (AFB) result was negative. Histology revealed multiple compact granulomata with necrotic centres containing multinucleated giant cells consistent with a mycobacterium infection. This was discussed with the histologists and respiratory physicians and the decision was made to commence treatment for tuberculosis. Subsequent culture confirmed mycobacterium tuberculosis that was sensitive to routine antimicrobials.
On completion of a 6-month antimicrobial treatment regimen had become clinically asymptomatic with regards to his foot. He was able to continue his work as a priest with no reported functional limitation. Radiographically the architecture of the midfoot was preserved with only mild second and third tarsometatarsal degenerative change.
DISCUSSION
Tuberculosis is sometimes referred to colloquially as ‘the great mimicker’,1 and as a result many cases of foot tuberculosis do not present in a classical manner. To further complicate the issue, radiological findings are often atypical1,5 and serological markers of infection are often equivocal. In the case of this patient, his symptoms had been present for over a year, and yet there were no clear clinical or radiological signs of infection to help guide diagnosis. However the suspicious appearance of the lesion on MRI was enough to warrant biopsy, which led to the final diagnosis within 6 weeks of initial presentation.
The prevalence of tuberculosis is increasing in developed countries. In the UK the Health Protection Agency’s annual tuberculosis report demonstrates significantly greater incidence in 2012 than 2010.6 This is widely attributed to migrant population, increasing rates of immunosuppressive disease (especially the current HIV epidemic), multidrug resistant strains of the mycobacterium, and increasing healthcare worker exposure.7,8
Pulmonary disease is the most contributory to this increase but relative increasing incidence of osteoarticular tuberculosis is also reported.9 The spine and weight-bearing joints are most commonly affected but the mycobacterium can infect any bone, joint, tendon, or bursa.10 As a result all clinical practitioners must have a very low index of suspicion for this condition especially in patients from high-risk demographics. Chemotheraputic treatment of this disease has a good prognosis. Early diagnosis and initiation of appropriate treatment is desirable to minimise extent of local disease and potential increased functional disability.
Patient consent
The patient has provided written consent for this article to be published.
Provenance
Freely submitted; externally peer reviewed.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Cheung JP, Ho KW, Lam YL, Shek TW. Unusual presentations of osteoarticular tuberculosis in two paediatric patients. BMJ Case Rep 2012. 2012;pii:bcr2012006714. doi: 10.1136/bcr-2012-006714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhillon MS, Sharma S, Gill SS, Nagi ON. Tuberculosis of bones and joints of the foot. Foot Ankle Int. 1993;14(9):505–513. doi: 10.1177/107110079301400904. [DOI] [PubMed] [Google Scholar]
- 3.Dhillon MS, Nagi ON. Tuberculosis of the foot and ankle. Clin Orthop. 2002;398:107–113. doi: 10.1097/00003086-200205000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Dhillon MS, Tuli SM. Osteoarticular tuberculosis of the foot and ankle. Foot Ankle Int. 2001;22(8):679–686. doi: 10.1177/107110070102200812. [DOI] [PubMed] [Google Scholar]
- 5.Mittal R, Gupta V, Rastogi S. Tuberculosis of the foot. J Bone Joint Surg. 1999;81:997–1000. doi: 10.1302/0301-620x.81b6.9925. [DOI] [PubMed] [Google Scholar]
- 6.Health Protection Agency. Tuberculosis in the UK: 2012 report. London: HPA; 2012. http://www.hpa.org.uk/webw/HPAweb&HPAwebStandard/HPAweb_C/1317134916916 (accessed 17 May 2013). [Google Scholar]
- 7.Pigrau-Serrallach C, Rodríguez-Pardo D. Bone and joint tuberculosis. Eur Spine J. 2012. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 8.Talbot JC, Bismil Q, Saralaya D, et al. Musculoskeletal tuberculosis in Bradford—a 6-year review. Ann R Coll Surg Engl. 2007;89(4):405–409. doi: 10.1308/003588407X183328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah BA, Splain S. Multifocal osteoarticular tuberculosis. Orthopaedics. 2005;28(3):329–332. doi: 10.3928/0147-7447-20050301-22. [DOI] [PubMed] [Google Scholar]
- 10.Zychowicz ME. Osteoarticular manifestations of mycobacterium tuberculosis infection. Orthop Nurs. 2010;29(6):400–406. doi: 10.1097/NOR.0b013e3181fb9a92. [DOI] [PubMed] [Google Scholar]


