Abstract
Background
Current evidence-based guidelines for low back pain (LBP) recommend multiple diverse approaches to treatment and suggest considering patient preferences when formulating a treatment plan.
Aim
To explore patient preferences and to identify patients’ beliefs about LBP treatments.
Design and setting
Qualitative study using focus groups in primary care in South-West England.
Method
Thirteen focus groups were organised with a purposive sample of 75 adults with LBP. Group discussions of LBP treatments were facilitated, audiorecorded, and the verbatim transcripts thematically analysed.
Results
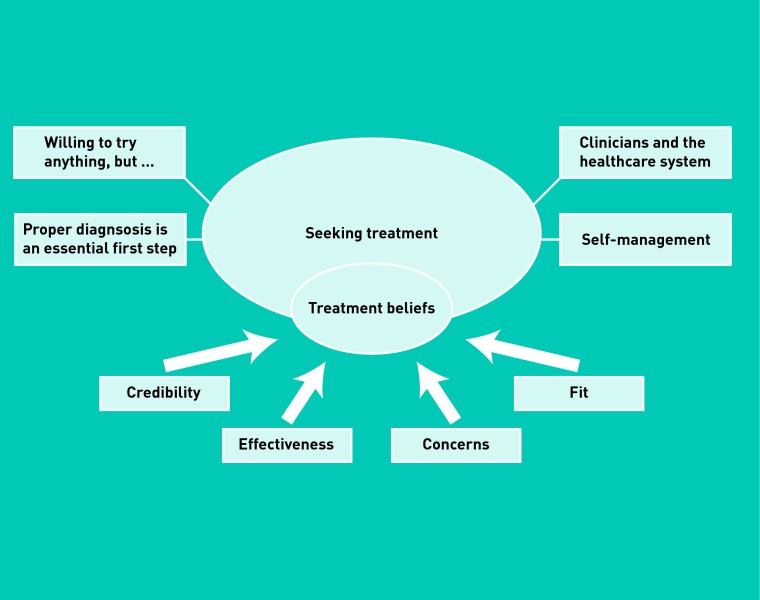
Eight themes were identified, four related to treatment beliefs and four to seeking treatment. Treatment beliefs comprised participants’ expectations and appraisals of specific treatments, which were underpinned by four distinct dimensions: credibility, effectiveness, concerns and individual fit. Treatment beliefs were expressed in the broader context of treatment seeking: participants’ primary concern was to obtain a clear explanation of their LBP which went beyond a diagnostic label and provided an understanding of the cause(s) of their LBP. They described engaging in self-management activities and claimed they were willing to try anything if it might help them. Participants wanted an empathic and expert practitioner who could deliver a suitable treatment (or refer them on to someone else) and help them to negotiate the challenges of the healthcare system.
Conclusion
These findings highlight the importance of helping patients develop coherent illness representations about their LBP before trying to engage them in treatment-decisions, uptake, or adherence. Addressing patients’ illness and treatment perceptions in clinical practice could improve shared decision making and patient outcomes.
Keywords: back pain; health knowledge, attitudes, practice; illness behaviour; patient preference; primary health care; qualitative research
INTRODUCTION
Low back pain (LBP) is experienced by up to 84% of the population and is often accompanied by substantial personal, social, and economic consequences.1–3 No single treatment is universally effective; the challenge for patients and clinicians is to identify the optimum treatment for the individual. This is reflected in current evidence-based recommendations for LBP management which incorporate not only medical and psychological approaches but also physical treatments, exercise, and complementary and alternative medicines (CAMs).4–7
Recent models of stratified primary care based on risk of poor prognosis offer new approaches to matching patients to suitable treatments.8 Another approach is to consider patient preferences, in line with increasing awareness of the need to promote shared decision making in health care.9 Qualitative methods are ideally suited to patients’ perspectives in an open and non-directive manner.10 Prior qualitative research in LBP has focused on patients’ lived experiences, including desires for clear diagnosis, adequate explanations, instructions and pain relief, access to a range of diagnostic and treatment services, and partnerships with clinicians.11–15 Others have highlighted the psychological burden of LBP and struggles for understanding and legitimisation.16–20 Few have focused on patients’ perspectives on treatment. A qualitative study was conducted to explore patients’ beliefs about LBP treatments.
METHOD
Design
Focus groups were used to collect qualitative data because they: efficiently elicit qualitative data from multiple participants; produce data that reflect socially acceptable experiences, beliefs, and language; allow researchers to observe interactions between participants and thus reflect participants’ own understandings.21,22
The topic guide (Appendix 1) elicited discussion of multiple LBP treatments, with a focus on those named in the current UK clinical guidelines (medication, exercise, manual therapy, acupuncture, combined psychological and physical treatment programmes, and spinal surgery4); these overlap with other international guidelines.5–7
Participants
The inclusion criteria were: adult (≥ 18 years), conversant in English, history of LBP at least 6 weeks, not caused by fracture, infection, inflammatory disorder, cancer, or nerve root compression. Participants best placed to help explore beliefs about and experiences of LBP treatments were purposively sampled.23 As there was interest in how patients go about evaluating different treatments (not whether a treatment is evaluated positively or negatively), some participants who had and some who had not experienced each treatment, and some who had and had not found each treatment helpful were sampled. Diversity was also ensured in sex, age, and location.
How this fits in
Low back pain is prevalent in primary care where current evidence-based guidelines recommend taking into account patients’ preferences when choosing between medical approaches, psychological approaches, physical treatments, exercise, and complementary and alternative therapies. Previous qualitative studies have illustrated the psychosocial impact of low back pain and the challenges faced by sufferers. This study shows that patients’ beliefs about diverse treatments for low back pain are organised around four key dimensions (credibility, effectiveness, concerns, and individual fit). Clinicians should help patients to develop a coherent understanding of their back pain as a prerequisite to engaging them in treatment-related decision making.
Potential participants across South-West England were identified from a) lists of patients who had recently consulted their family doctor or CAM practitioner because of LBP and b) members of a chronic pain patient support group. They were informed about the study and invited to participate. Seventy-five responders participated in 13 focus groups. Participants were between 29 and 85 years old (median = 62 years), 64% were female, and approximately two-thirds had pain for more than 3 years (Table 1). Each focus group included 4–10 participants (median = 6) and lasted 70–90 minutes (mean/median 80). Groups were held during 2011 at doctors’ premises and were audiorecorded (with prior written informed consent), transcribed verbatim, and anonymised. Data analysis and collection proceeded iteratively; focus groups were stopped when participants with diverse experiences and characteristics had been sampled, when no new themes were apparent, and when existing themes were well-elaborated.24
Table 1.
Participants’ characteristics (N = 75)
| Characteristic | N(%) |
|---|---|
| Age | 29–85 years (median 62 years) |
|
| |
| Females | 48 (64) |
|
| |
| Location | |
| Hampshire | 55 (73) |
| Dorset | 8 (11) |
| Wiltshire | 6 (8) |
| Isle of Wight | 6 (8) |
|
| |
| Recruitment source | |
| Family doctor | 66 (88) |
| CAM practitioner | 5 (7) |
| Chronic pain patient support group | 4 (5) |
|
| |
| Pain duration | |
| Persistent LBP (6wks–12 months) | 16 (21) |
| Chronic/recurrent LBP (12 months–3 years) | 9 (12) |
| Chronic/recurrent LBP (>3years) | 50 (67) |
|
| |
| Treatments experienced | |
| Self-management advice | 10 (13) |
| Pain medication | 67 (89) |
| Manual therapy | 63 (84) |
| Exercise | 46 (61) |
| Acupuncture | 18 (24) |
| Psychological and physical programme | 6 (8) |
| Referral for spinal fusion | 5 (7) |
CAM = complementary and alternative medicine. LBP = low back pain.
Data analysis
Thematic analysis25 was conducted and NVivo (version 9) was used for data management and coding. After repeated reading of transcripts and listening to audiorecordings, participants’ talk was analysed at the level of meaning unit (a statement that expresses a single meaning). First, talk was deductively categorised as related to a recommended treatment (medication, exercise, manual therapy, acupuncture, combined psychological and physical treatment programmes, or spinal surgery), to other treatments, or to clinical management of LBP. Then, an inductive approach was taken to identify dimensions underlying participants’ perceptions of particular treatments (treatment beliefs) and themes related to the clinical management of LBP (collectively labelled treatment seeking). Strategies to enhance analytic rigour included constant comparison of categories, themes, and talk between and within focus groups and about the same and different treatments,24 coding led by one researcher reviewed by a second, and discussion of the emerging analysis by the research team (Appendix 2). Illustrative quotes presented below were selected from the coded transcripts for typicality and eloquence in illustrating the themes.
RESULTS
Figure 1 illustrates the main themes and their inter-relations.
Figure 1.
Thematic map showing themes related to treatment beliefs and seeking treatment.
Treatment beliefs
Participants evaluated treatments holistically across four dimensions of credibility, effectiveness, concerns, and individual fit; they balanced different considerations but prioritised effectiveness. Treatments moved in and out of favour contingent on factors such as personal experience and the other treatment options considered. Each dimension of treatment beliefs is described briefly; Table 2 summarises how these dimensions were expressed for each recommended treatment.
Table 2.
How treatment beliefs were expressed in relation to specific treatments
| Credibility — perceived mechanisms | Effectiveness and effects | Concerns | |
|---|---|---|---|
| Medications | Relaxes muscles; enables detachment; reduces inflammation: ‘I use ibuprofen when I’ve got a problem and ibuprofen’s like a miracle drug because it relaxes the muscles and takes away the pain.’ (Female, FG4) |
Temporary relief; prevents worsening; enables activity; last resort: ‘I don’t think it’s a way of getting over, you know, it’s not going to fix your back, but it’s a way of helping just make it a little bit easier for yourself.’ (Male, FG12) |
Side effects; poly-pharmacy; addiction and desensitisation; masks pain and could lead to further damage: ‘You take one tablet but then you have to take two or three tablets to counteract that one tablet that you’re taking.’ (Male, FG13) |
| Exercise | Strengthens muscles; reduces stiffness; improves mental state; weight loss: ‘The only thing I found useful there in a more permanent place is exercise [...] to strengthen the muscles so that they hold the spine in a more useful position.’ (Male, FG7) |
Temporary relief; maintenance; enables activity; cure: ‘There’s not a cure, because there is no reversing it and that’s what they told me so the only way to do it is to maintain it and to do that is to have exercise.’ (Male, FG2) |
Injuring the back; difficulties maintaining motivation: ‘If you start to feel a little bit of an improvement, it’s an encouragement to keep on at it, but then you get a bad day and you just don’t you — just can’t face doing any exercise so you just give up on it in the end.’ (Female, FG11) |
| Manual therapy | Realigns the spine; releases the nerves; strengthens muscles: ‘If you’re misaligned, it’s putting additional pressure on nerves, cartilage, all sorts of things and when you realign that into the correct position that releases that pressure which reduces the pain.’ (Female, FG10) |
Temporary relief; maintenance; prevents worsening; cure: ‘[The practitioner] slowed down the rate at which it got worse but he didn’t improve it.’ (Male, FG10) |
Feeling sore after manipulation; causing further damage; ‘cracking’ bones: ‘You lie on this bed and the first thing he does is crack your back so one part’s up there and one part’s down and all of a sudden he pulls this lever and you think, my god my back’s broken.’ (Female, FG5) |
| Acupuncture | Stimulates nerves; relaxes muscles: ‘The energy lines generally follow the major nerve roots as well [...] by stimulating the nerve passage ways, and stimulating the nerve roots, you can get them to switch on, switch off, or reset effectively.’ (Female, FG10) |
Temporary relief; cure: ‘Lasted about 4 months, three sessions and it lasted about 4 months and that was you know.’ (Male, FG8) |
Fear of needles; needling painful: ‘You haven’t got to look at the needles, they are gonna be in your back, so that doesn’t phase me, it’s not the thought of it, it’s actually seeing them go in to your skin.’ (Male, FG12) |
| Combined psychological and physical approach | Teaches self-management; improves posture; releases tension: ‘When you go to a course like that, everybody’s in the same situation and you know, and it was you know, and you learn you learn a lot about you know how to look after your own back.’ (Female, FG11) |
Last resort: ‘I think it’s basically telling you that you’ve got your bad back and you’re going to have to look after it for you, you keep yourself fit by doing gentle exercise.’ (Female, FG11) |
Being diagnosed (stigmatised) with a psychological disorder; controlling pain is difficult to learn: ‘At first I found it very hard to get my head around what he was saying and even now, I try to do it if I’m in a really bad day, my back or my knees of whatever’s hurting, I can lay there and really try it but I find it very, very hard to think that mind over matter is …’ (Male, FG13) |
| Spinal fusion | Not discussed. | Last resort; medium-term solution: ‘Surgery is a last resort, you know, you try, like you say, all of that on there, then you know, you come to the end of the road and that’s the only option they got, they ain’t going to operate just for the sake of operating.’ (Male, FG9) |
Inherent risks of surgery; implications of permanent changes to the spine: ‘It’s a loss almost, it’s to me it’s almost a sadness because you’ve already embarked on having limitations and obviously as you get older, the limitations may increase.’ (Female, FG8) |
Credibility
According to participants, a treatment should be credible (a ‘proper treatment’), should ‘make sense’ (have a believable mechanism of action), and should be delivered by ‘the right practitioner’. Some participants argued that a treatment should match the perceived location and cause of their condition, for example, massage was credible for muscle problems. Table 3 illustrates strategies participants used for assessing credibility in the absence of personal experience. Credibility was often evaluated by comparing treatments, and a treatment perceived as lacking credibility could be considered for a trial period to assess its effectiveness and safety, or could become a preferred option if more credible treatments were tried and found ineffective.
Table 3.
Strategies participants used for assessing treatment and practitioner credibility in the absence of personal experience
| Strategy/source of information to assess credibility | Illustrative quote |
|---|---|
| Recommendations from trusted sources, personal, or professional | ‘If it was recommended by somebody I had confidence in. […] if it’s somebody who’s either had it done or it’s recommended by a GP.’ Male, FG10 |
| Mass media | ‘Definitely would consider it yeah, it actually sounds interesting, you see enough of it on the television.’ Female, FG8 |
| Practitioner’s training and qualifications | ‘I went to see a properly qualified acupuncturist who spent 4 years training to become a proper acupuncturist, I didn’t just go and put myself into the hands of a physiotherapist who’d had half an hour’s training.’ Female, FG10 |
Effectiveness
There was clear consensus that treatments should have proven effectiveness for LBP. Three treatments were discussed as potential cures which might enable a patient to regain prior good health (exercise, acupuncture, and manual therapy) but these treatments were also described by other participants as providing only temporary relief or preventing symptoms worsening. Medications were perceived as providing temporary relief, an ‘easy fix’ to avoid but not address the underlying problem. However, temporary relief could itself be a valued outcome if it enabled participants to retain or regain valued life activities or enable self-management. Some participants acknowledged that hoping for a permanent cure was unrealistic.
Concerns
Participants expressed concerns about the treatment costs (such as financial, time, and travel) and safety (such as longer-term side effects, risk of damage, and painful treatments). The specific content varied across treatments (Table 2), but generally concerns deterred participants from trying or led them to adjust or discontinue recommended treatments. For example, participants were deterred from trying acupuncture because of concerns over needles. They adjusted or stopped medication because of concerns about addiction, drug desensitisation, and the potential to cause further damage by masking pain.
When perceived effectiveness was high this could help participants overcome concerns:
‘You’ve got no chance of stopping it if it’s going to go wrong, so I think that the chiro[practor] from my own personal viewpoint would be I’ve got to see some positive results from others before I go for it myself‘.
(Male, FG11)
Individual fit
Participants discussed how, ideally, a treatment should fit the patient’s individual circumstances and characteristics (such as age, injury, and lifestyle) and get to the root cause of their LBP. An appropriate exercise programme would provide individualised recommendations (not standardised exercise print-outs) and supervision to ensure correct, safe, and effective exercise. While a good fit for the individual was seen as an important precursor for effective individual treatment, this was assessed independently of general treatment effectiveness:
‘Whenever they were doing any kind of massage or anything into my back, they were never hitting the spots ever, but I don’t think it’s down to them I think it’s whatever they do isn’t right for me’.
(Female, FG7)
Seeking treatment
Participants’ treatment beliefs were expressed and should be understood in the context of their broader treatment-seeking experiences.
‘Proper’ diagnosis is an essential first step
Receiving a diagnosis came as a relief for some participants, particularly those with concerns about possible sinister causes of LBP. However, diagnosis in its various forms was also experienced as insufficient, confusing, worrying, or dismissive. ‘Low back pain’ and similar labels were deemed insufficient generic diagnoses. Instead, participants wanted individualised explanations of the causal factors responsible for their pain:
‘We’ve all got pain and got different reasons for causing it I should think’ (Male, FG12).
Typically, physiological or anatomical explanations were sought and valued:
‘What helped me a lot […] was trying to understand what’s going on, you know, how the back works and what it looks like and what the muscles are and, you know, where the nerves are’
(Male, FG4).
Consistent with this perspective, participants argued that accurate diagnosis could only be achieved through detailed examination (assessment through physical touch) and/or tests (X-rays and MRI scans), although some limitations and risks of tests were acknowledged.
Without a clear diagnosis (identifying the cause of pain), participants did not see how an appropriate treatment could be selected (to resolve the cause of pain); treatment decisions in these circumstances were seen as unsystematic ‘hit-and-miss’ or ‘trial-and-error’, and treatments themselves were seen as potentially harmful, unlikely to help, and a waste of time and resources:
‘Certainly, at the moment, I don’t believe anything that I’ve been told is going to cure whatever I’ve got because I don’t know what I’ve got. So it’s a bit up in the air but can you see where I’m coming from; I need to know, so that I know what they are doing to me is going to help me.’
(Female, FG1)
Willing to try anything, but ..
Participants expressed willingness to experience different treatments (‘I’ll try anything’; Female, FG8), but usually qualified this by considering effectiveness (‘anything that would actually help and you know would help’; Male, FG12), or credibility (‘if a doctor said to me you need this done’; Female, FG8). Willingness to try different treatments was also contingent on their emerging effectiveness; participants talked about assessing effectiveness during ‘trial periods’. Opinions differed regarding the length of trial periods:
‘You know if it didn’t work the first time for me I would probably think that’s not for me, but you did try it three times so you know’
(Female, FG8).
Participants valued a systematic active approach to monitoring and evaluating initial effectiveness of individualised treatment within the context of an on-going therapeutic relationship:
‘I’d like an action plan so that after a certain time — so if he said to me, you know, let’s give it 3 months, I’ll give you all these exercises, I’ll give you this to do, I’ll give you that to do, come back in 3 months and let’s see where you are in 3 months’ time.’
(Female, FG2)
Clinicians and the healthcare system
Participants wanted clinicians to be knowledgeable, conscientious, empathic, respectful, and trustworthy; to acknowledge and believe individual’s experiences of pain; and to provide adequate treatment (according to the above dimensions). Participants were concerned not to be seen as malingerers or hypochondriacs; some described this as a reason for avoiding seeking care despite wanting treatment. Those who sought care found it distressing to feel disrespected or disbelieved by a practitioner. They discussed feeling ‘fobbed off’, ‘dumped’ and ‘dismissed’ when told to live with pain and that it had no physical cause or was a natural consequence of aging:
‘When you’re told ‘live with it’, it’s the most awful feeling, you know and sometimes you’re just reduced to tears because you think if they won’t help, what can you do?’
(Male, FG2).
Using the healthcare system was described as a challenging process of negotiating referrals, tests and treatments. Participants were concerned to maximise their chances of obtaining good quality care and to minimise demands on their personal resources (such as private sector financial costs, travel costs, timing of appointments, and waiting lists). Some participants greatly valued the advocacy role that family doctors can play in helping them to negotiate the system. As participants shared their experiences with each other during the focus groups a collaborative process of trying to understand how the system operates was observed. This encompassed discussions of procedures for obtaining appointments and referrals, allocation of resources, key decision-makers, and local availability of treatments (Table 4).
Table 4.
Excerpts from focus groups to illustrate participants sharing experiences about treatment seeking
| Topic | Illustrative excerpt |
|---|---|
| The impact of clinicians and the healthcare system | FP: ‘A friend of mine … went down to [town] hospital and… she’s been on a pain management course — |
| MP: ‘They run one in [town 2].’ | |
| FP ‘Oh do they?’ | |
| FP ‘Ask your doctor. ‘ | |
| MP ‘Ask your GP to be referred.’ | |
| FP ‘Yeah to the pain clinic.’ | |
| MP ‘Ask to be referred to the pain clinic in [town 2] and they will refer you on a pain management program, but you have to go through the pain clinic … to go on it.’ | |
| FP ‘No one’s offered me a pain clinic.’ (FG13) | |
|
| |
| Self-management | FP1:‘it is doing your homework about who you need to see and why you need to see them but I’m sure —’ |
| FP2:‘That’s the doctor’s job isn’t it?’ | |
| FP1:‘Not always, not always.’ | |
| FP3:‘I think you have to take some responsibility for —’ | |
| FP2:‘But I’m nowhere near a doctor, so if I’ve got a certain pain I wouldn’t know who to go to, I would have no idea.’ (FG8) | |
FP = female participant. MP = male participant.
Self-management
Recommended treatments were considered and used alongside self-management techniques, such as: changing postural habits and ergonomics; goal-setting and pacing; sleep behaviours and postures; emotion regulation and distraction. Techniques were seen as prohibitively difficult; as strategies that complement and/or supplement clinician-delivered treatment; and as valuable ways to take personal control of LBP. Participants who were unwilling to change their habits or lifestyle typically were not confident in their ability to self-manage or to make decisions; they preferred doctors to choose treatments for them (Table 4). Participants who primarily self-managed their LBP typically preferred to choose for themselves which clinicians to consult and/or which treatments to trial to supplement their daily self-management (for example, during flare-ups).
DISCUSSION
Summary
Four core dimensions underpinned patients’ beliefs about LBP therapies: credibility, effectiveness, concerns and individual fit. These beliefs were expressed in the broader context of self-management, clinicians, and health care systems. The participants’ primary concern was to obtain a clear explanation of their LBP that went beyond a diagnostic label to help them to understand the cause(s) of their pain. This appears to be an essential prerequisite for meaningful engagement with treatment decision making.
Strengths and limitations
Not all patients’ views of all LBP treatments were considered but many commonly recommended treatments have been covered. Participants had persistent, chronic, or recurrent LBP; they might have better-elaborated and more entrenched views about treatments than patients with acute LBP. Participants were recruited from South-West England; the findings will reflect local health services. Focus groups allowed the study to observe patients learning from each other, but participants who had experienced a particular treatment tended to contribute more to discussions of that treatment than those with less experience.
Comparison with existing literature
This study’s findings can be interpreted in relation to Leventhal’s commonsense model of illness behaviour, according to which patients form illness representations26 and treatment beliefs27 which inform the iterative selection and appraisal of coping strategies including healthcare utilisation.28–30 In the current study, patients wanted a clear explanation of their pain which provided not only a diagnostic label but, more importantly, an individualised causal understanding; that is, they were striving to develop a realistic illness representation. This was an essential prerequisite for engaging with treatment decisions: uncertain and poorly elaborated understandings of LBP appeared to have a dramatic impact, driving reluctance to engage with decision making and/or recommended treatments. Others have similarly described the impact of illness uncertainty (and lack of legitimisation) on psychosocial adjustment15,18,19,31 and patients’ often-frustrated desires for clear explanations for pain.11,12,14,16 The current study extends this literature by demonstrating the potential consequences of illness uncertainty for treatment beliefs and decisions in patients with chronic LBP.
Four core dimensions underpinning treatment beliefs about diverse therapeutic approaches were identified: a treatment should have a credible mechanism of action and be delivered by a credible clinician, should have proven effectiveness in attaining a relevant short- or long-term goal, should prompt few concerns about safety and accessibility, and should be a good individual fit for the person’s diagnosis and life circumstances. These constructs partially overlap with dimensions underpinning beliefs about medicines (necessity and concerns)32,33 and constructs from psychotherapy (credibility and expectancy).34 Patients’ beliefs about LBP treatments cannot fully be understood with these existing constructs, as individualised fit is essential in this context.
Implications for practice and research
Quantitative studies are needed to test hypotheses concerning the correlates and impact of patients’ treatment beliefs. A questionnaire to measure the range of LBP treatment beliefs identified here is being validated; this will enable future studies to compare treatment beliefs between different groups of patients (for example acute/chronic LBP; males/females; treatment experienced/naive) and to test the impact of treatment beliefs on treatment-related decisions, behaviours, and outcomes.
Many clinicians struggle with communicating a clear explanation or specific diagnosis for patients with LBP35–37 and guidelines consistently recommend a focused history and physical examination but no routine imaging.4–7 Indeed achieving reliable and valid, specific, diagnoses for most patients with LBP is neither possible nor desirable.38 This study’s participants’ desire for causal explanations suggests greater educational efforts are needed to explain to the general public why diagnostic tests such as X-rays are not routinely recommended. This would usefully assist clinicians’ efforts in addressing diagnostic expectations of individual patients.
Offering information about treatments in a standardised, non-interactive, format (such as a leaflet) is likely to be of limited value, since LBP patients tend to prefer an individualised approach and differ in their information needs. Stiggelbout and colleagues9 recommend a strategy to achieve patient-centred decision making in consultations; this study suggests adjustments to this process for patients with LBP. These are summarised in Table 5. This approach could be further developed to support clinicians in helping their patients to develop illness representations that are coherent and pragmatic (that is, perceived as useful for guiding action). Clinicians could use the common-sense model to guide discussion around the core dimensions of illness perception: identity (symptoms and diagnostic label), causal factors (heavily emphasised by this study’s participants), timeline, consequences, and controllability (probing the specific dimensions of treatment beliefs identified above).39 Developing and testing such a theory-driven, consultation-based, communication strategy to improve proximal (such as treatment uptake, adherence) and distal (such as function) health outcomes may be helpful.
Table 5.
Patient-centred decision making processes
| Process to achieve patient-centred decision making in primary care5 | Suggested modifications for patients with LBP |
|---|---|
| Create awareness of equipoise | Create awareness of equipoise and help patient to develop a realistic illness representation. Elicit and address patients’ concerns regarding diagnosis, for example by clearly explaining why further tests are not being ordered and findings from the clinical history and assessment can confirm the diagnosis. |
| Discuss the potential benefits and harms of available treatments and their associated probabilities | Elicit and discuss patients’ goals for treatment in general as well as their perceptions of and preferences for available treatments, not only in terms of potential benefits and harms, but also likely mechanisms of action, practitioner credentials, and individual fit for their own particular back problem. |
| Elicit the patient’s views regarding the options | Provide guidance and support in negotiating the healthcare system and empower the patient to access their preferred treatment where possible within local constraints. |
LBP = low back pain.
Acknowledgments
We thank the participants for sharing their experiences and the Primary Care Research Network and all the clinicians who helped to recruit the participants.
Appendix 1. Focus group topic guide
- Generate a list of treatments that participants:
- ○ Have tried in the past
- ○ Would like to try
- ○ Do not want to try
- Open discussion of each treatment, including:
- ○ Personal experiences
- ○ Advantages
- ○ Disadvantages
- ○ Reasons for use/not use
Open discussion of experiences of seeking care for low back pain
Generate a wish-list of desired approach and treatments for low back pain in primary care
Appendix 2. The influence of the researchers on the qualitative analysis
A critical realist approach to this work was taken. The ontological assumption is that while participants’ experiences cannot be objectively observed by attending to their accounts, their accounts can be treated as a representation of their experiences. Epistemologically, it can be assumed that the act of research (in this case the focus group) has an unavoidable role in shaping the participants’ talk and that the analyst similarly brings existing theories and knowledge to bear when interpreting the data. It is possible to reduce the inappropriate influences of the researchers in the production of what is necessarily culturally-bound knowledge. By describing the background here it is hoped to render transparent the theories and knowledge that were drew on when interpreting the data.
The analysis was led by Alexandra Dima, who also organised the focus groups. She is a post-doctoral researcher in health psychology interested in how patients manage chronic conditions, including their perceptions of illness and treatments, their health behaviours and their communication with the healthcare providers. Her doctoral thesis focused on patient’s adjustment to chronic pain conditions, including low back pain. She is familiar with various theoretical models of heath behaviour and pain perception and coping. Felicity L Bishop had detailed input into the coding and interpretation. She is lecturer in health psychology at the University of Southampton with particular research interests in how and why patients use complementary and alternative medicines and prior familiarity with Leventhal’s common sense model as well as other health psychological models and frameworks related to illness behaviour.
All other authors contributed to data interpretation.
Nadine E Foster is a physiotherapist whose research involves testing treatments and services for patients with common musculoskeletal problems, including low back pain, in primary care. Her research has identified that patients perceptions about their back pain at the time of consultation predict their clinical outcome in the short and long term, and that using a range of key predictors of outcome, in one brief index of risk, to match back pain patients to treatments, provides clinical and cost benefits for patients and health services. Rona Moss-Morris has carried out research in LBP including studies investigating 1) cognitive processes of change across a multidisciplinary pain management programme and 2) Patients’ expectations of a pain management programme. She has just started a new study investigating pain in MS. George T Lewith is professor of health research at the University of Southampton and leader of the Integrated Medicine research group; he has a long-standing research interest in acupuncture and has used it in his own clinical practice. Paul Little is professor of primary care research at the University of Southampton who has research interests in low back pain (in particular the Alexander technique) and doctor–patient communication in primary care.
Overall, working in a multidisciplinary team enabled us to avoid drawing premature conclusions and helped sensitise us to diverse interpretations of the data.
Funding
This article presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. This study was funded by the NIHR School for Primary Care Research (Project Number 75). Felicity L Bishop’s post was funded by Arthritis Research UK (Career Development Fellowship 18099). George T Lewith’s post is supported by a grant from the Rufford Maurice Laing Foundation. Nadine E Foster’s post is supported by a NIHR Research Professorship.
Ethical approval
Obtained ethics approval from Southampton and South West Hampshire REC B (10/H0504/78).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482–491. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 2.Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84(1):95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 4.Savigny P, Kuntze S, Watson P, et al. Low back pain Early management of persistent non-specific low back pain. London: NICE; 2009. NICE clinical guideline 88. http://www.nice.org.uk/nicemedia/live/11887/44343/44343.pdf (accessed 23 May 2013). [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 6.Airaksinen O, Brox J, Cedraschi C, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(0):s192–s300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Tulder M, Becker A, Bekkering T, et al. Chapter 3 European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15(0):s169–s191. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill JC, Whitehurst DG, Lewis M, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378(9802):1560–1571. doi: 10.1016/S0140-6736(11)60937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stiggelbout AM, der Weijden TV, De Wit PT, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256. doi: 10.1136/bmj.e256. [DOI] [PubMed] [Google Scholar]
- 10.Holloway I. Basic concepts for qualitative reserach. Oxford: Blackwell; 1997. [Google Scholar]
- 11.Verbeek J, Sengers M-J, Riemans L, Haafkens J. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine. 2004;29(20):2309–2318. doi: 10.1097/01.brs.0000142007.38256.7f. [DOI] [PubMed] [Google Scholar]
- 12.Laerum E, Indahl A, Skouen JS. What is ‘the good back-consultation’? A combined qualitative and quantitative study of chronic low back pain patients’ interaction with and perceptions of consultations with specialists. J Rehabil Med. 2006;38(4):255–262. doi: 10.1080/16501970600613461. [DOI] [PubMed] [Google Scholar]
- 13.Slade SC, Molloy E, Keating JL. ‘Listen to me, tell me’: a qualitative study of partnership in care for people with non-specific chronic low back pain. Clin Rehabil. 2009;23(3):270–280. doi: 10.1177/0269215508100468. [DOI] [PubMed] [Google Scholar]
- 14.McIntosh A, Shaw CFM. Barriers to patient information provision in primary care: patients’ and general practitioners’ experiences and expectations of information for low back pain. Health Expect. 2003;6(1):19–29. doi: 10.1046/j.1369-6513.2003.00197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corbett M, Foster NE, Ong BN. Living with low back pain — Stories of hope and despair. Soc Sci Med. 2007;65(8):1584–1594. doi: 10.1016/j.socscimed.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 16.Osborn M, Smith JA. The personal experience of chronic benign lower back pain: An interpretative phenomenological analysis. Br J Health Psychol. 1998;3(1):65–83. [Google Scholar]
- 17.Snelgrove S, Liossi C. An interpretative phenomenological analysis of living with chronic low back pain. Br J Health Psychol. 2009;14(Pt 4):735–749. doi: 10.1348/135910709X402612. [DOI] [PubMed] [Google Scholar]
- 18.Walker J, Holloway I, Sofaer B. In the system: the lived experience of chronic back pain from the perspectives of those seeking help from pain clinics. Pain. 1999;80(3):621–628. doi: 10.1016/S0304-3959(98)00254-1. [DOI] [PubMed] [Google Scholar]
- 19.May CR, Rose MJ, Johnstone FCW. Dealing with doubt; How patients account for non-specific chronic low back pain. J Psychosom Res. 2000;49(4):223–225. doi: 10.1016/s0022-3999(00)00168-9. [DOI] [PubMed] [Google Scholar]
- 20.Glenton C. Chronic back pain sufferers — striving for the sick role. Soc Sci Med. 2003;57(11):2243–2252. doi: 10.1016/s0277-9536(03)00130-8. [DOI] [PubMed] [Google Scholar]
- 21.Morgan DL, Krueger RA. When to use focus groups and why. In: Morgan DL, editor. Successful focus groups. London: Sage; 1993. pp. 3–19. [Google Scholar]
- 22.Wilkinson S. Focus groups in health research. J Health Psychol. 1998;3(3):329–348. doi: 10.1177/135910539800300304. [DOI] [PubMed] [Google Scholar]
- 23.Patton MQ. Qualitative research and evaluation methods. 3rd edn. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 24.Glaser BG, Strauss A. The discovery of grounded theory. In: Glaser BG, Strauss A, editors. The discovery of grounded theory. London: Weidenfeld and Nicolson; 1967. pp. 1–18. [Google Scholar]
- 25.Joffe H, Yardley L. Content and thematic analysis. In: Marks DF, editor. Research methods for clinical and health psychology. London: Sage; 2004. pp. 56–68. [Google Scholar]
- 26.Leventhal HA, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. London: Routledge; 2003. pp. 42–65. [Google Scholar]
- 27.Horne R. Representations of medication and treatment: advances in theory and measurement. In: Petrie KJ, Weinman JA, editors. Perceptions of health and illness. Amsterdam: Harwood Academic Publishers; 1997. pp. 155–188. [Google Scholar]
- 28.Glattacker M, Heyduck K, Meffert C. Illness beliefs, treatment beliefs and information needs as starting points for patient information — Evaluation of an intervention for patients with chronic back pain. Patient Educ Couns. 2012;86(3):378–389. doi: 10.1016/j.pec.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 29.Foster NE, Thomas E, Bishop A, et al. Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain. 2010;148(3):398–406. doi: 10.1016/j.pain.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foster NE, Bishop A, Thomas E, et al. Illness perceptions of low back pain patients in primary care: what are they, do they change and are they associated with outcome? Pain. 2008;136(1–2):177–187. doi: 10.1016/j.pain.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Ong BN, Hooper H, Dunn K, Croft P. Establishing self and meaning in low back pain narratives. Sociol Rev. 2004;52(4):532–549. [Google Scholar]
- 32.Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 33.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. [Google Scholar]
- 34.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 35.Slade SC, Molloy E, Keating JL. The dilemma of diagnostic uncertainty when treating people with chronic low back pain: a qualitative study. Clin Rehabil. 2012;26(6):558–569. doi: 10.1177/0269215511420179. [DOI] [PubMed] [Google Scholar]
- 36.Jeffrey J, Foster N. A qualitative investigation of physical therapists’ experiences and feelings of managing patients with nonspecific low back pain. Phys Ther. 2012;92(2):266–278. doi: 10.2522/ptj.20100416. [DOI] [PubMed] [Google Scholar]
- 37.Sanders T, Foster N, Ong B. Perceptions of general practitioners towards the use of a new system for treating back pain: a qualitative interview study. BMC Med. 2011;9(1):49. doi: 10.1186/1741-7015-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deyo RA. Diagnostic evaluation of lbp: reaching a specific diagnosis is often impossible. Arch Intern Med. 2002;162(13):1444–1447. doi: 10.1001/archinte.162.13.1444. [DOI] [PubMed] [Google Scholar]
- 39.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health. 1998;13:717–733. [Google Scholar]