Abstract
We report a case of acute postoperative endophthalmitis caused by vancomycin-resistant Staphylococcus hominis, treated at our hospital. An 80-year-old male presented 2 days after uncomplicated phacoemulsification and posterior chamber intraocular lens implantation, with a 24-hour history of progressive visual loss and redness in the operated (right) eye. On examination, best corrected visual acuity was counting fingers. Anterior segment examination revealed conjunctival injection, chemosis, corneal edema, and hypopyon. B-scan ultrasonography showed vitreous opacification, but no retinal detachment. Acute postoperative endophthalmitis was diagnosed. We performed vitrectomy with vancomycin in the irrigating solution, intraocular lens removal, and silicone oil tamponade. Culture of the vitreous grew Staphylococcus hominis. Antibiotic susceptibility testing showed the isolate was sensitive to trimethoprim/sulfamethoxazole and teicoplanin but resistant to ciprofloxacin, moxifloxacin, levofloxacin, cefazolin, and vancomycin. At 3 months, the visual acuity of the silicone oil-treated eye was 20/400.
Keywords: endophthalmitis, Staphylococcus hominis, vancomycin
Introduction
The incidence of infectious endophthalmitis after cataract surgery has been estimated to range from 0.07% to 0.13%.1 To our knowledge, there are no reports of vancomycin resistance to Staphylococcus hominis following endophthalmitis. We report a case of acute postoperative endophthalmitis caused by vancomycin-resistant S. hominis treated at our hospital.
Case report
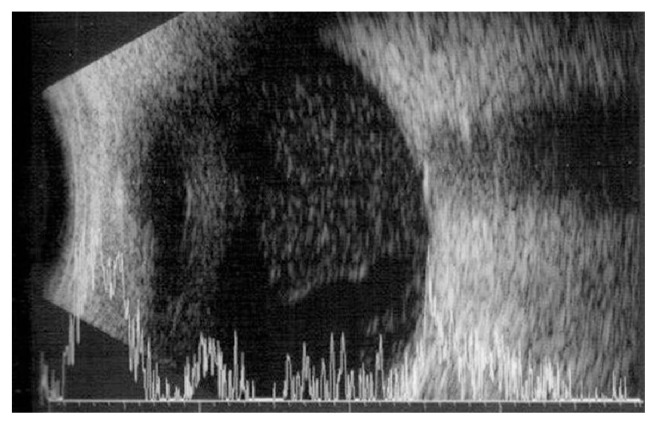
An 80-year-old male presented 2 days after an uncomplicated phacoemulsification and implantation of a posterior chamber intraocular lens (IOL) (C-flex®; Rayner, Hove, UK), with a 24-hour history of progressive visual loss and redness in the operated (right) eye. Preoperative best-corrected visual acuity (BCVA) was 20/200 in the right eye. Past medical history was significant for hypertension, atrial fibrillation, and prostate cancer. On examination, the BCVA was counting fingers. Anterior segment examination revealed conjunctival injection, chemosis, corneal edema, and hypopyon (2 mm size). B-scan ultrasonography showed vitreous opacification but no retinal detachment (Figure 1). Acute postoperative endophthalmitis was diagnosed.
Figure 1.
B-scan ultrasonography demonstrated vitreous opacities but no retinal detachment.
A vitreous biopsy was performed immediately, with an intravitreal injection of vancomycin 1.0 mg/0.1 mL and ceftazidime 2.25 mg/0.1 mL. Approximately 3 hours after the vitreous biopsy and intravitreal injection of antibiotics, an operating room became available, and we performed 23-gauge pars plana vitrectomy (PPV), using vancomycin in the irrigating solution, and IOL removal with the capsular bag. During the vitrectomy, we saw severe vitreous opacification and a thick exudative membrane that covered the entire retina. After delicate vitrectomy-like shaving, we could see the disc and major vessel arcade faintly. The vitreous humor obtained during the vitrectomy and IOL were sent to the laboratory for smear and culture test. Finally, we finished surgery after fluid−air exchange and silicone oil tamponade.
Culture of the vitreous grew S. hominis. Antibiotic susceptibility testing (microbroth dilution MIC test) showed that the isolate was sensitive to trimethoprim/sulfamethoxazole (MIC sensitive [S] ≤2/38) and teicoplanin (S ≤4) but resistant to ciprofloxacin (MIC resistant [R] >2), moxifloxacin (R >4), levofloxacin (R >4), cefazolin (R >8), and vancomycin (R = 8~16). Postoperatively, the patient was treated with 2% teicoplanin eye drops, topical fortified vancomycin, and prednisolone acetate eye drops.
At 3 months, the visual acuity of the silicone oil-treated eye was 20/400.
Discussion
S. hominis is normally found on human skin and is usually harmless but can sometimes cause infections in people with abnormally weak immune systems. Most, if not all, strains are susceptible to penicillin, erythromycin, and novobiocin, but a divergent strain, S. hominis subsp. novobiosepticus (SHN), was found recently.2 This strain was named so because of its unique resistance to novobiocin and its failure to produce acid aerobically, from trehalose and glucosamine. The S. hominis strains are also somewhat resistant to methicillin and gentamicin, and most strains are resistant to erythromycin, clindamycin, chloramphenicol, trimethoprim/sulfamethoxazole, and ciprofloxacin as well. The SHN strain seems to have thickened cell walls, and this tendency may be the result of a genetic background that also allows for vancomycin resistance.3
The SHN is so similar to the original S. hominis that a MicroScan system (Dade Behring, West Sacramento, CA, USA) is needed to differentiate the S. hominis and SHN in the clinical microbiology laboratory.4 However, unfortunately, our hospital did not have this equipment.
Another point must be considered. Previously, Iyer et al reported that patients with S. hominis endophthalmitis have a subacute onset and are asymptomatic.5 However, the present case had an acute-onset postoperative endophthalmitis. In our case, a high-virulence organism and S. hominis may have presented as a mixed infection, and thus, it is possible that only S. hominis was cultured instead of the high-virulence organism.
Asaoka studied the role of coagulase-negative staphylococci (CNS) in outer eye infections.6 Their results indicated that of 57 strains of CNS, only three (5.3%) strains belonged to S. hominis. Furthermore, these CNS were resistant to aminoglycoside and macrolide antibiotics, which are commonly used as eye drops for ocular infectious diseases. However, Asaoka suggested that ocular CNS infections can occur in immunologically compromised host patients.
At 3 months, the visual acuity of the silicone oil-treated eye was 20/400. Although rare, we report that acute-onset, postoperative S. hominis endophthalmitis can occur in an immunocompetent patient.
Conclusion
We present a case of acute-onset, postoperative vancomycin-resistant S. hominis endophthalmitis managed with intravitreal antibiotics injection, PPV, IOL removal and silicone oil tamponade.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Jager RD, Aiello LP, Patel SC, Cunningham ET., Jr Risks of intravitreous injection: a comprehensive review. Retina. 2004;24(5):676–698. doi: 10.1097/00006982-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Kloos WE, George CG, Olgiate JS, et al. Staphylococcus hominis subsp. novobiosepticus subsp. nov, a novel trehalose- and N-acetyl-D-glucosamine-negative, novobiocin- and multiple-antibiotic-resistant subspecies isolated from human blood cultures. Int J Syst Bacteriol. 1998;48(Pt 3):799–812. doi: 10.1099/00207713-48-3-799. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgibbon JE, Nahvi MD, Dubin DT, John JF., Jr A sequence variant of Staphylococcus hominis with a high prevalence of oxacillin and fluoroquinolone resistance. Res Microbiol. 2001;152(9):805–810. doi: 10.1016/s0923-2508(01)01264-5. [DOI] [PubMed] [Google Scholar]
- 4.Palazzo IC, d’Azevedo PA, Secchi C, Pignatari AC, Darini AL. Staphylococcus hominis subsp. novobiosepticus strains causing nosocomial bloodstream infection in Brazil. J Antimicrob Chemother. 2008;62(6):1222–1226. doi: 10.1093/jac/dkn375. [DOI] [PubMed] [Google Scholar]
- 5.Iyer MN, Wirostko WJ, Kim SH, Simons KB. Staphylococcus hominis endophthalmitis associated with a capsular hypopyon. Am J Ophthalmol. 2005;139(5):930–932. doi: 10.1016/j.ajo.2004.10.060. [DOI] [PubMed] [Google Scholar]
- 6.Asaoka I. Role of Staphylococcus epidermidis in outer eye infections. Nihon Ganka Gakkai Zasshi. 1989;93(3):351–357. Japanese. [PubMed] [Google Scholar]