Abstract
Coronary heart disease (CHD) mortality is one of the major contributors to racial disparities in health in the United States (US). We examined spatial heterogeneity in black–white differences in CHD mortality across the US and assessed the contributions of poverty and segregation. We used county-level, age-adjusted CHD mortality rates for blacks and whites in the continental US between 1996 and 2006. Geographically weighted regression was employed to assess spatial heterogeneity. There was significant spatial heterogeneity in black–white differences in CHD mortality (median black–white difference 17.7 per 100,000, 25th–75th percentile (IQR): 4.0, 34.0, P value for spatial non-stationarity < 0.0001) before controlling for poverty and segregation. This heterogeneity was no longer present after accounting for county differences in race-specific poverty and segregation and interactions of these variables with race (median black–white difference −13.5 per 100,000, IQR: −41.3, 15.7, P value for spatial non-stationarity = 0.4346). The results demonstrate the importance of spatial heterogeneity in understanding and eliminating racial disparities in CHD mortality. Additional research to identify the individual and contextual factors that explain the local variations in racial disparities is warranted.
Keywords: Racial disparities, CHD mortality, Poverty, Segregation, Spatial heterogeneity, Geographically weighted regression, United States
1. Introduction
Coronary heart disease (CHD) is the leading cause of mortality and morbidity in the United States (US) and is one of the most important contributors to black–white disparities in life expectancy (Wong et al., 2002; Harper et al., 2007). Despite downward trends (Cooper et al., 2000), CHD mortality in blacks remains significantly higher than in whites (Lloyd-Jones et al., 2010). In 2006, CHD death rates per 100,000 populations were 161.6 for blacks and 134.2 for whites in the US (Keenan and Shaw, 2011).
Previous studies have documented substantial geographic variations in CHD mortality for both blacks and whites across the US (Wing et al., 1990; Pickle and Gillum, 1999; Barnett and Halverson, 2000; Casper et al., 2000; Barnett et al., 2001; Halverson et al., 2002). The highest rates of CHD mortality are generally observed in rural south (Barnett and Halverson, 2000) and in Oklahoma, the Appalachian region, and along the Ohio–Mississippi River Basin (Pickle and Gillum, 1999). These studies also highlight that geographic patterns sometimes vary by race. For example, among adult blacks, the highest rates are observed in the rural south, and in major metropolitan areas outside south. The highest rates among adult whites are also primarily in the rural south but high rates are also observed along the southeast coastal plain, and in the economically distressed Appalachian region (Pickle and Gillum, 1999; Barnett and Halverson, 2000; Halverson et al., 2002).
Although studies of geographic variations in rates have made important contributions to our understanding of how geography and race jointly shape the distribution of CHD mortality, relatively few studies have explicitly investigated spatial heterogeneity in race differences. Tassone et al. (2009) used Bayesian spatial hierarchical modeling to examine racial disparity in stroke mortality in the southeastern US and found important evidence of geographic heterogeneity. Holt and Lo (2008) used geographically weighed regression to demonstrate spatial heterogeneity in the relationship between all cause mortality and census tract-level socioeconomic/race composition in the Atlanta metropolitan area. Chen et al. (2010) examined spatial variation in the effects of social disadvantage, lack of economic opportunity, and residential stability on cardiovascular mortality in Taiwan, and found evidence that the effects of these factors varied over space. To our knowledge, no studies have quantified spatial heterogeneity in CHD mortality disparities across the US or systematically investigated the contributors to this spatial heterogeneity.
Two spatially linked factors that may contribute to black–white differences in CHD mortality, and to spatial heterogeneity in black white differences, are poverty and residential segregation. Multiple studies have consistently shown that measures of area deprivation (including poverty) are associated with cardiovascular diseases for both larger and smaller area sizes (Diez Roux et al., 1997; Smith et al., 1998; Armstrong et al. 1998; Diez Roux et al., 2001; Cubbin et al., 2001; Cooper et al., 2001; Sundquist et al., 2004). Poverty may affect racial disparities in CHD mortality by shaping differential access to resources and physical and social environments that may in turn affect behavioral and psychosocial risks factors for coronary heart disease (Ellaway and Macintyre, 1996; Sampson et al., 1997; Ross, 2000; Silver et al., 2002; Morland et al., 2002; Diez Roux, 2003). Thus, area poverty, and specifically geographic variability in differences in poverty levels between blacks and whites, could be an important contributor to spatial heterogeneity in black–white CHD disparities.
A growing body of research has also shown that residential segregation is related to adverse health outcomes among some race or ethnic groups (Williams and Collins, 2001; Acevedo-Garcia et al., 2003; White and Borrell, 2011). Several ecological studies have shown that segregation is positively associated with adult black mortality rates (Bird, 1995; Collins and Williams, 1999; Hart et al., 1998; Shihadeh and Flynn, 1996) and black infant mortality (LaVeist, 1993; Polednak, 1996b). Other work has shown that more segregated areas also tend to have larger differences in mortality rates between blacks and whites (Polednak, 1993; 1996a). Recent work has also shown smaller black–white disparities in several CVD risks factors in more racially integrated neighborhoods (LaVeist et al., 2011). For example, the authors found that disparities in hypertension, diabetes, and obesity among women narrowed or vanished in racially integrated southwest Baltimore.
The degree of racial residential segregation may be linked to differential distribution of health relevant resources, inequalities in economic, occupational, and educational opportunities, and levels of racism (including institutional racism) as well as other stressors, all of which may contribute to race differences in CHD risk. For example, residential segregation can modify or magnify racial disparities in CHD by isolating blacks in concentrated poverty and creating vastly different economic, physical, and social neighborhood environments for blacks and whites (Williams and Collins, 2001; Schulz et al., 2002; Schulz et al., 2005; Mays et al., 2007; Kramer and Hogue, 2009). These differential exposures to physical and social environments in turn shape health behaviors and psychosocial factors which are risk factors for CHD. In addition, residential segregation may influence CHD mortality by acting synergistically with other race spatially-patterned factors (e.g., stress linked to discrimination interacting with differential access to healthy foods).
Despite abundant research on the impact of poverty and residential segregation on health, little work has directly examined the contribution of poverty and segregation to geographic variability in black–white differences in health. Identifying important geographic sources of spatial heterogeneity in black–white differences could yield important clues on the etiology of these differences and could point to important social and/or environmental factors. A better understanding of the magnitude and determinants of spatial heterogeneity in racial disparities in CHD mortality is important to the formulation of policies to eliminate disparities.
We used county-level data on CHD mortality for the continental US for the period 1999–2006 and geographically weighted regression (Fotheringham et al., 2002) (a novel method in public health and epidemiology) to investigate the spatial heterogeneity in racial disparities and the factors associated with this spatial heterogeneity. Our objectives were twofold. First, we assessed the spatial heterogeneity in racial disparities in CHD mortality. Next, we examined the contributions of county and race-specific poverty and residential segregation to the spatial heterogeneity in racial disparities.
2. Materials and methods
2.1. Data and data sources
The study population consisted of whites and blacks of all ages who resided in the continental US during the years 1999–2006. Data on CHD mortality for the study period at the county level were extracted from the Centers for Disease Control and Prevention’s (CDC) WONDER database (Centers for Disease Control and Prevention (CDC) 2010). CHD mortality data included all deaths coded as I20–I25 using the International Cause of Death (ICD-10) classification.
The data sets retrieved were race-specific (black and white) CHD death counts, population at risk, and age-adjusted CHD mortality rates for each county in the continental US (N = 3108) over 8 years (1999–2006). The CHD mortality rates were age-adjusted to the 2000 US Standard Population and were reported as deaths per 100,000. CDC identifies counties having cumulative deaths of 20 or fewer as “unreliable” mortality rates because of small number of population (Hoyert et al., 2005). To avoid excessive random variation, counties with morality rates based on < = 20 deaths were not included in our analyses. Of the total counties in the US, 3049 counties had reliable mortality rates for whites and 1162 counties had reliable mortality rates for blacks (the difference is attributable to counties with a very small Black population which makes rates unreliable). In order to take advantage of all available data, analyses used all CHD rates available for a total of 4211 data points. This included 1162 counties with available mortality for both blacks and whites and 1887 counties with available mortality for Whites only. Because even counties with rates for whites only contribute information on spatial patterning of White mortality rates, counties with White only mortality rates were included in main analyses. An assumption implicit in this approach is that racial differences observed in counties with rates for both race groups are generalizable to all counties. In sensitivity analyses we restricted analyses to counties that had data on both blacks and whites and found “qualitatively” similar results.
We structured the data using a repeat measures format in which some counties had one mortality rate (e.g., when only a white rate was available) but others had two (when both black and white rates available). An indicator of whether the rate was for black or white residents was included. In addition each observation (i.e., each county and race-specific rate) was linked to data on county and race-specific measures of poverty and segregation as described below.
Data on the percentage of persons with income below poverty line separately for blacks and whites at the county level were extracted from US census bureau for the year 2000. This measure was used to characterize race differences in socioeconomic circumstances within each county. In addition, data on county-level residential segregation, as measured by the isolation index, separately for blacks and whites for the year 2000 at the county level were abstracted from GeoDa Center for Geospatial Analysis and Computation (2010). The isolation index measures the probability that a randomly chosen member of one group will meet another member of the same group (Massey and Denton, 1988). It ranges in value from 0 to 1, with higher values representing greater isolation/segregation.
2.2. Geographical weighted regression
Ordinary least squares (OLS) regression has been commonly used in epidemiology to quantify relationships between exposures and health outcomes. OLS generates “global” regression coefficients, which assumes that the relationships are constant over space. This approach may mask spatial variability in the relationships. Moreover, it ignores the spatial dependencies between variables (Huang and Leung, 2002), which may sometimes result in biased estimates and can result in overstated statistical significance of associations. The OLS regression model applied to our data can be expressed as
| (1) |
where yi is the county and race-specific CHD mortality rate for observation i (observations are all available county and race-specific mortality rates, n = 4211), xik is the value of the kth independent variable for observation i (i.e., race, county and race-specific poverty and segregation), β0 is the intercept parameter, βk is the regression coefficient for kth independent variable, and εi is a random error term for observation i.
A local regression technique called geographically weighted regression (GWR) has been developed for exploring spatial heterogeneity in spatial data (Brunsdon et al., 1996; Fotheringham et al., 2002). GWR extends traditional regression models such as OLS by allowing regression coefficients to vary spatially within a study area. Unlike OLS, GWR assumes that relationships between exposures and health outcomes may vary over space; consequently it generates a set of local regression coefficients for each observation point in the study area. The GWR model can be written as
| (2) |
where βi0(ui,vi) is the intercept parameter at point i, βik(ui,vi) is the local regression coefficient for the kth independent variable at point i, and (ui,vi) is the coordinate of the ith point in the study area, which is the ith county and race-specific CHD mortality rate. In our study, the x and y coordinates were given in meters through Albers Equal Area Conic projection system. GWR requires assigning a specific x and y coordinate to each observation i. A common approach with county-level data is to assign the coordinate for the centroid of each county to the rate. However, since our data sometimes had two observations for each county (one for blacks and one for whites) assigning the centroid coordinate to both results in convergence problems. To address this problem, we assigned each mortality rate to a randomly generated location within the county. Sensitivity analyses were performed to check whether the selection of the random locations has any influences on the results, our analyses indicated that the random locations did not change the magnitude and direction of the results.
In GWR, the local regression coefficients for all points i are estimated using the locally weighted least square procedure by weighting all observations according to their spatial proximity to the regression point i. It is assumed that the observed data in closer proximity to the regression point i carry more weight than data located farther away, and so have a greater influence in the estimation of βik(ui,vi). The parameters can be estimated by solving the following matrix equation:
| (3) |
where β̂(u,v) represents the unbiased estimate of β, and W(u,v) is the weighting matrix that ensures observations near to the regression point i have a greater weight and is calculated from a kernel function. In this study, we used the following Gaussian weighting kernel function form:
| (4) |
where dij is the Euclidean distance between observations i and j, and h is the kernel bandwidth beyond which the weights are zero. Either a fixed or adaptive kernel bandwidth can be used to define the weights. The fixed kernel uses a constant bandwidth over space, while adaptive kernel allows the bandwidth to vary over space so that bandwidths are smaller in areas where data are denser and larger where data are sparse. Because of greatly varying density of mortality rates over space (due to varying geographic coverage of counties) in our data, we chose an adaptive kernel and the optimal kernel bandwidth for our study was determined using the cross-validation calibration method (Fotheringham et al., 2002).
2.3. Statistical analyses
In our implementation of OLS and GWR models, CHD mortality rates were modeled as a function of a race indicator as well as measure of county and race-specific poverty and segregation. The coefficient associated with the race indicator can be interpreted as the mean difference in CHD mortality between blacks and whites after adjustment for other variables in the model. In order to investigate spatial heterogeneity in disparities in CHD mortality rates between blacks and whites, we fitted a series of sequential models to the county and race-specific age adjusted CHD mortality rates. We first fitted an OLS model (model 1) to quantify the overall unadjusted absolute black–white disparity in CHD rates. We then fitted the same model using GWR and quantified the spatial heterogeneity in the unadjusted race difference (model 2).
To investigate the contribution of spatially varying factors to the race difference (and the spatial heterogeneity in the race difference), we fitted a series of sequential GWR models that incorporated county and race-specific poverty and segregation measures as main effects and in interaction with race: Model 3, added county and race-specific poverty to model 2; Model 4 incorporated county and race-specific segregation variables in addition to race and poverty, and Model 5 incorporated interaction terms between race and poverty and race and segregation. The interaction terms allow assessment of whether the magnitude of black–white differences in CHD mortality varies by level of race specific poverty or segregation. Models 3–5 were fitted in order to investigate the contributions of the variables to (1) overall black–white differences in CHD mortality rates (reflected in the regression coefficient associated with race) and (2) to spatial heterogeneity in black–white differences (reflected in measures of the spatial heterogeneity of the coefficient). These models were fitted using GWR in order to allow the effects of all variables (not just race) to vary over space. For comparison purposes, we also fitted the full model using OLS (model 6). In additional analyses the full OLS model was refitted to account for repeat observations within each county using the General Estimating Equations approach (model 7). This approach was used to test the sensitivity of OLS results to non-independence of observations within each county (Liang and Zeger, 1986).
While OLS provides global estimates of the relationships between CHD mortality and race, poverty and segregation variables, the GWR model generates local regression coefficients, local standard error, and local R2 values at each geographic location. Local values of t-statistics can be calculated by dividing each local regression coefficients by the corresponding local standard error. Although these t-values cannot be interpreted in a formal statistical sense (Waller et al., 2007), they are often used as exploratory tools to highlight local areas where interesting relationships appear to be occurring. In this study, and following the approach used in other work employing GWR (Brunsdon et al., 2002; Ali et al., 2007; Graif and Sampson, 2009; Gilbert and Chakraborty, 2011), we compared the global OLS coefficients for each parameter to the median (as well as to the 25th and 75th percentiles) of the GWR local coefficients in order to assess the impact on the estimated associations of allowing coefficients to vary over space. We also mapped the GWR local coefficients and t-values to highlight the spatial variability in the relationships between CHD mortality and race, poverty, and residential segregation. Since some of the spatial variability in the relationships can be due to sampling variation, we used the Leung’s F3 test to determine the statistical significance of the spatial non stationarity (Leung et al., 2000a).
We also conducted ANOVA F tests to determine whether the GWR model is a significant improvement over the corresponding OLS model (Brunsdon et al., 1999, Fotheringham et al., 2002). In addition, we also used R2 and Akaike Information Criterion (AIC) to assess if GWR provides a better fit to our data than OLS model while adjusting for the different degrees of freedom in the two models (Fotheringham et al., 2002). The R2 of OLS was compared with the median of the GWR local R2. Finally, we tested for the presence of residual spatial autocorrelation in the OLS and GWR residuals using Moran’s I statistic (Moran, 1950) to determine whether GWR accounts for the spatial autocorrelation in the data (Huang and Leung, 2002). All analyses were implemented in R statistical software (R Development Core Team, 2010). All maps were made using ArcGIS 9.3.
3. Results
The analysis included 1162 and 3049 counties with valid CHD mortality rates for blacks and whites respectively (Table 1). On average, blacks had higher CHD death rates (186 per 100,000) compared to whites (161 per 100,000). The median county-specific percent below the poverty line for blacks was substantially higher (28.1%) than for whites (10.9%). The county-specific segregation was higher in whites than in blacks (median segregation for whites was 0.90 (0.76, 0.96) versus 0.29 (0.15, 0.45) for blacks).
Table 1.
Selected characteristics of the counties included in the analyses (median, 25th, 75th percentile).
| Characteristics | Counties with Black mortality rates N = 1162 | Counties with White mortality rates N = 3049 | Total N = 4211 |
|---|---|---|---|
| Population* | 68,045 (31,524, 169,017) | 181,900 (78,987, 465,095) | 140,178 (59,509, 370,074) |
| CHD Deaths | 88 (46, 207) | 367 (173, 833) | 266 (103, 670) |
| CHD mortality rates (per 100,000) | 185.99 (156.08, 221.71) | 161.31 (135.70, 190.29) | 167.57 (139.38, 199.37) |
| *Poverty, % | 28.12 (22.33, 35.18) | 10.86 (8.19, 13.85) | 12.76 (9.18, 21.20) |
| *Segregation | 0.29 (0.15, 0.45) | 0.90 (0.76, 0.96) | 0.81 (0.48, 0.94) |
Poverty and segregation are county and race-specific.
Table 2 displays mean differences in CHD mortality rates associated with race and other covariates in OLS and sequential GWR models. The OLS estimates for model 1 indicated the presence of significant black–white differences in CHD mortality. On average for the whole US, CHD mortality was significantly higher in blacks than in whites (mean difference = 27.8, P < 0.0001). Model 2 shows the GWR estimates analogous to the OLS model 1. The median value of the GWR race coefficient was of a magnitude comparable to the OLS coefficient although somewhat smaller (17.7 vs. 27.8). However, the interquartile range (IQR) for the GWR race coefficients was from 4.0 to 34.0, suggesting the existence of significant spatial non-stationarity in black–white differences in CHD mortality across the US (Leung’s F3 test < 0.0001).
Table 2.
Mean Differences in age-adjusted CHD mortality associated with race and covariates in OLSa, GEEa and GWRa Models (N = 4211).
| OLS Model 1 | GWR Model 2 | GWR Model 3 | GWR Model 4 | GWR Model 5 | OLS Model 6 | GEE Model 7 | |
|---|---|---|---|---|---|---|---|
| Race | 27.84††† (1.64) | 17.71*** (4.0, 34.0) | −10.75*** (−37.66, 18.02) | −19.25*** (−52.39, 12.63) | −13.52 (−41.34, 15.68) | −28.24 ††† (4.23) | −21.93 ††† (4.12) |
| Povertyb | 17.53*** (5.71, 31.63) | 18.16*** (7.29, 29.64) | 22.81*** (12.05, 35.61) | 26.03 ††† (1.66) | 20.59 ††† (1.70) | ||
| Segregationb | −5.64*** (−16.03, 4.78) | −0.38*** (−14.93, 14.68) | 0.17 (1.52) | −1.91 (1.41) | |||
| Race*poverty | −8.75 (−24.53, 6.64) | −7.23 †† (2.23) | −7.50ccc (1.87) | ||||
| Race*segregation | −3.22* (−29.78, 19.90) | −16.12 ††† (2.61) | −9.9 ††† (2.76) | ||||
| R2 (%) | 6.4 | 27.9 (19.9, 38.1) | 35.6 (25.4, 46.3) | 32.2 (23.6, 41.5) | 31.8 (22.8, 39.9) | 14.9 | |
| AIC | 44491.15 | 41860.74 | 41582.81 | 41952.97 | 42180.61 | 44027.97 | |
| Moran’s I test | N/A | N/A | N/A | N/A | 0.025††† | 0.30††† | |
| ANOVA F test | 5.03† | 4.49† | 4.73††† | 5.31††† |
P < 0.05;
P < 0.001;
P < 0.0001 are significance levels of the OLS and GEE models indicate whether the coefficients are significantly different from zero.
P < 0.05;
P < 0.001;
P < 0.0001 are significance levels of GWR models indicate whether there is significant spatial variation in the relationships between CHD mortality and race, poverty, segregation, and interaction terms, as determined by the Leung’s F 3 test (Leung et al., 2000a).
For the OSL and GEE models estimates correspond to the coefficient and the SE in parentheses. For GWR models estimates correspond to the median coefficients and the 25th and 75th percentiles in parentheses.
Poverty and segregation were Z-scored and mean centered.
Comparison of the OLS model 1 with the analogous GWR model 2 based on the ANOVA F-test (F = 5.03; P < 0.05) revealed the GWR model was a statistically significant improvement over the OLS model. The GWR model also produced higher local median R2 (GWR 28% vs. OLS 6%), indicating a large improvement in explained variance. Furthermore, the AIC for the GWR model 2 was approximately 6.0% lower than the analogous OLS model 2 (41861 for GWR vs. 44491 for OLS), suggesting the GWR model fit the data better than the OLS model.
Subsequent models 3–5 were fitted to examine the contribution of county and race-specific poverty and segregation to the race differences and to spatial heterogeneity in the race differences. The median coefficients from the GWR revealed that higher poverty was associated with higher CHD mortality, and adjustment for county-specific poverty changed the direction of the median coefficient for the black–white difference (model 3). The addition of race-specific segregation (model 4) did not substantially modify the association of race or poverty with CHD. After adjustment for race-specific poverty, higher segregation was associated with lower CHD mortality overall (model 4). However, there was evidence that the inverse association of segregation with CHD mortality was substantially stronger in blacks than in whites (model 5, −0.38 in whites and −3.60 in blacks). In contrast, the association of higher poverty with higher CHD mortality appeared to be weaker in blacks than in whites (GWR model 5, median difference 22.8 in whites and 14.1 in blacks).
The GWR results revealed substantial spatial heterogeneity in the coefficients for the main effects of poverty and segregation (Leung’s F3 test < 0.0001 for poverty and segregation in model 5). The interquartile range (IQR) for the main effects of poverty includes only positive values (12.1 to 35.6). In contrast, the IQR for the main effects of segregation includes both negative and positive values (IQR −14.9 to 14.7). The interaction between race and poverty did not exhibit significant spatial non-stationarity (P = 0.3508) but the interaction between race and segregation was statistically non-stationary (P = 0.0016) (see Table 2). The addition of additive interactions between race and poverty and race and segregation eliminated the statistically significant spatial heterogeneity in the effect of race observed in models 2–4 (Leung’s F3 test for the main effect of race P = 0.4346 in model 5). The adjusted R2 and the AIC comparisons also showed better fit for the GWR model than the analogous OLS model (model 6). In addition, the OLS residuals were significantly spatially autocorrelated (Moran’s I = 0.30, P < 0.0001), whereas the GWR model substantially reduced the magnitude of spatial autocorrelation in the residuals (Moran’s I = 0.025, P < 0.0001). Table 2 also shows the full model fitted with GEE (model 7). This model is directly analogous to the OLS model but improves on this model because it accounts for the repeat observations within counties. Inspection of the coefficients from this model shows that the directionality and magnitudes of the associations were generally consistent with those observed in the GWR model, although some differences were observed when estimates from this model were compared to median coefficients estimated by GWR.
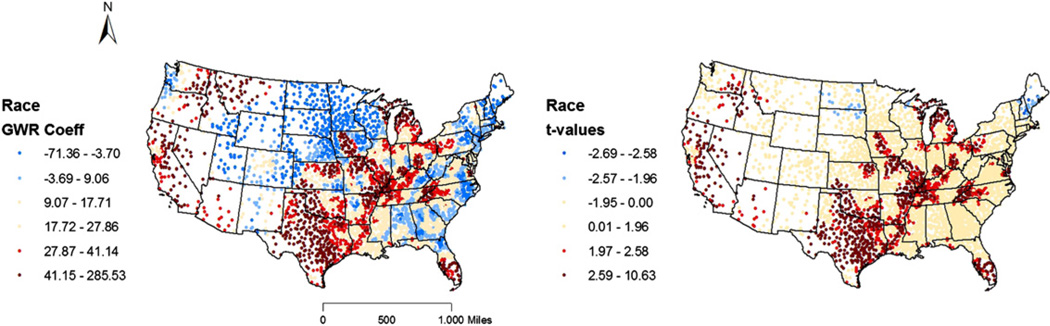
Maps of GWR coefficients and t-values for model 2 (Fig. 1) and model 5 (Fig. 2A–D) allow the visualization of the spatial heterogeneity in racial disparities in CHD mortality before and after adjustment for poverty and segregation. Fig. 1 shows that both the magnitude and direction of racial disparities in CHD mortality as estimated in model 2 (unadjusted GWR model) varies across the US. The t-map reveals significant and positive race effects around West South Central (Arkansas, Texas, Oklahoma, and Louisiana), along the Mississippi–Ohio River, and some counties in the West Coast and South Florida, indicating higher rates of CHD mortality for blacks than whites in these counties. A few counties in the New England and the Dakotas exhibit higher rates of CHD mortality for whites than for blacks. A number of counties in the Southeast coastal plain, Rocky Mountain States, and Great Plain States showed no significant racial disparities in CHD mortality.
Fig. 1.
Depicts maps of the GWR coefficients (left) and t-values (right) from the unadjusted GWR model 2 for the main effect of race variable (or spatial heterogeneity in racial disparities in CHD mortality before adjusting for poverty and segregation). The t-map displays absolute t-values greater than 1.96 and 2.58 which correspond to the 95% and 99% significant levels respectively. In all the t-maps, the red colors indicate locations with a positive t-statistic greater than or equal to 1.96, the blue colors indicate locations with a negative t-statistic smaller than or equal to −1.96 and light yellow color represent locations with a t-statistic between −1.96 and +1.96.
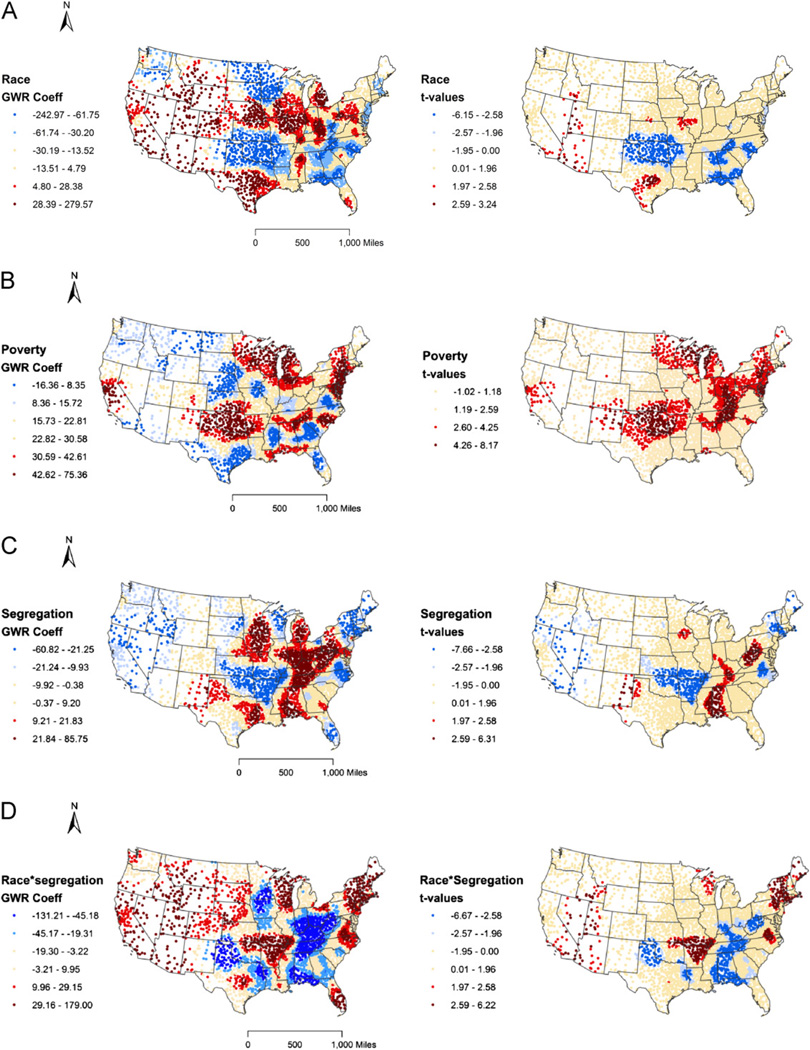
Fig. 2.
(A) Depicts maps of GWR coefficients (left) and t-values (right) from the fully adjusted GWR model 5 for the main effect of race variable (or spatial heterogeneity in racial disparities in CHD mortality after adjusting for poverty and segregation). (B) Depicts maps of GWR coefficients (left) and t-values (right) from the fully adjusted GWR model 5 for the main effect of poverty variable. (C) Depicts maps of GWR coefficients (left) and t-values (right) from the fully adjusted GWR model 5 for the main effect of segregation (or the effect of segregation in whites). (D) Depicts maps of GWR coefficients (left) and t-values (right) from the fully adjusted GWR model 5 for the interaction between race and segregation.
Fig. 2 displays the maps of GWR coefficients and t-values for the main effect of race variable after adjusting for poverty and segregation (fully adjusted model 5). Because the model includes interactions between race and mean-centered measures of poverty and segregation, the estimates can be interpreted as race differences at the mean values of poverty and segregation. The t-map shows that the high rates of CHD mortality for blacks around the West South Central, South Florida, and California was eliminated, suggesting that poverty and segregation completely explain the black–white differences in CHD mortality in these counties. Similarly, among whites the high mortality rates in counties around New England and the Dakotas also disappeared after controlling for poverty and segregation. However, scattered counties in the Rocky Mountain States, and some counties in Texas, Illinois, and Missouri still have unexplained high rates of CHD mortality in blacks.
Fig. 2B shows the maps of GWR coefficients and t-values for the main effect of the poverty variable (which can also be interpreted as the effect of the poverty variable among whites). The t-map shows an overall positive relationship between poverty and CHD mortality, mirroring the global estimates. Positive and statistically significant effects of poverty appear across most of the counties in the US. Interaction terms suggested weaker effects of poverty in blacks than in whites (models 5 and 6) but since these effects did not vary spatially they are not shown in a figure.
Fig. 2C and D show the maps of GWR coefficients and t-values for the main effect of segregation (or the effect of segregation in whites) and the interaction between segregation and race, both of which were found to vary spatially. Maps show generally stronger inverse associations between segregation and CHD in blacks (as indicated by a median coefficient with a negative sign, Fig. 2D) although there is substantial spatial variation in this effect. For example, positive estimates of the interaction effect (indicating a positive association of segregation with CHD mortality, i.e., greater CHD mortality in areas of greater segregation) were obtained for the Northeast, portions of counties bordering Kansas, Arkansas, Missouri, and Oklahoma, and some counties in the Rocky Mountain States (Fig. 2D).
4. Discussion
Ordinary least squares results showed that for the whole US, the difference in CHD mortality between blacks and whites was 28 per 100,000 before controlling for county poverty and segregation. Greater poverty was associated with higher CHD mortality (although this association was weaker in blacks than in whites) and greater segregation was not associated with CHD mortality in whites but was associated with lower CHD mortality in blacks. After adjustment for poverty, segregation, and their differential effects by race CHD rates in blacks were 28 per 100,000 lower than for whites. Accounting for repeat observations within counties using GEE did not substantially alter these results.
The results from the OLS model were useful in providing an average picture of racial disparities but they masked important local variations in the relationships. Furthermore, the OLS model explained only 15% of the variance in the CHD mortality and did not account for the spatial autocorrelation in the data. On the other hand, the GWR model showed improvements of model performance over the corresponding OLS model. It produced a large improvement in explained variance (32%) without adding new variables to the model and reduced spatial autocorrelations in the residuals as examined by Moran’s I statistics. These findings suggest the spatial variation in coefficients captured by the GWR is an important feature in the underlying relationships in the data.
The GWR results revealed that both the magnitude and direction of race differences in CHD mortality vary significantly across the US. In the unadjusted model, 50% of the counties in the US had black–white mean differences in CHD mortality that ranged from as low as 4 to as high as 34 CHD deaths per 100,000. Counties with higher rates of CHD mortality in blacks were predominantly located around West South Central, along Mississippi–Ohio River, and some counties in the West Coast and South Florida. These results are similar in patterns to those previously reported (Pickle and Gillum, 1999; Barnett and Halverson, 2000; Halverson et al., 2002). Only very few counties in Dakotas and New England had higher CHD rates in whites than in blacks, while a number of counties did not display significant black–white differences in CHD mortality.
Once we controlled for county and race-specific poverty and segregation race differences in CHD mortality did not show significant geographic variations, suggesting that the spatial patterning of these factors may contribute in part to spatial heterogeneity in disparities. Notably, the high rates of CHD mortality in blacks around the West South Central, along Mississippi–Ohio River, and some counties in the West Coast and South Florida disappeared after adjustment.
We found that higher poverty was associated with higher CHD mortality in both blacks and whites across the US, although some spatial heterogeneity in the effect of poverty was observed. This finding is consistent with prior work (Smith et al., 1998; Armstrong et al., 1998; Cooper et al., 2001). Poverty may contribute to high CHD mortality for both blacks and whites through both material and psychosocial processes (Silver et al., 2002; Diez Roux, 2003; van Jaarsveld et al., 2007) linked to poverty itself and to area poverty. Although higher county-level poverty rate was associated with increased CHD mortality rates in both blacks and whites, similar to other studies (Tassone et al., 2009) the effect of poverty was weaker in blacks than in whites. Other work has also shown weaker socioeconomic patterning of some CVD risk factors in blacks than in whites, especially in the case of men (Diez Roux et al., 1997; Boykin et al., 2011). Our data do not allow us to determine the reason for the weaker poverty effects in blacks. However, it is important to note that the distributions of poverty were quite different by race, and thus the weaker effect observed in blacks (at higher levels of poverty) could reflect a non-linear relation between poverty and CHD mortality such that the relation becomes weaker as poverty increases.
In the fully adjusted OLS model greater segregation was not associated with CHD mortality in whites but was associated with lower CHD mortality in blacks. However, a closer look at the GWR results indicated that segregation was positively associated with CHD mortality in some counties while negatively associated in other counties (Fig. 2d). For example, among blacks three clusters showed significant positive associations of segregation with CHD mortality (the Northeast states, counties bordering Arkansas, Oklahoma, Missouri, and Kansas; and scattered counties in the Rocky Mountain States). Conversely, segregation was negatively associated with CHD mortality among blacks in counties of south central states (Mississippi, Alabama, Tenseness, and West Virginia). Our results support previous mixed findings where some studies have reported that residential segregation is associated with higher risk for mortality among blacks (Collins and Williams, 1999, Williams and Collins, 2001, Acevedo-Garcia et al., 2003) but at least one study in New York City has reported protective effects (Fang et al., 1998). The variable associations of segregation with health among blacks are also consistent with various types of processes through which segregation has been hypothesized to relate to health. Greater segregation may result in worse environmental conditions in segregated groups with consequent adverse health effects (Williams and Collins, 2001). However, some beneficial effects of living in areas where one is not in the minority (such as increased social support and reduced exposure to discrimination) have also been hypothesized (Halpern and Nazroo, 2000; Henderson et al., 2005). Additional work is needed to determine why segregation is adversely related to CHD mortality in some areas but not in others.
A limitation of our study is that we investigated only a small set of county level variables. In addition, the number of counties with valid rates for blacks was substantially smaller than the ones with data for whites. Nevertheless, we found “qualitatively” similar patterns when we restricted analyses to counties with valid data for both blacks and whites (results not shown). In order to obtain reliable rates, we pooled across various calendar years which could have masked important temporal variations. In addition, counties may not be the most optimal geographic level to investigate because county-level measures may obscure important heterogeneity. The ecological nature of these analyses also limits the types of inferences that can be drawn. Studies that incorporate both individual and contextual factors are needed to better understand the causes of heterogeneity in racial disparities.
While the GWR method is useful for describing spatial heterogeneity it presents several challenges (Cho et al., 2010). First, it provides estimates of the median value and distribution of the coefficients over space but does not allow statistical testing of the average effect as OLS does. In addition the OLS coefficients and the median GWR are not directly comparable as they reflect different measures of association, with one being a global estimate and another being a median of spatially varying local estimates. Second, GWR is susceptible to multicollinearity among local estimates in the model (Wheeler and Tiefelsdorf, 2005). Third the GWR method tends to generate extreme local coefficients and may overstate spatial heterogeneity (Farber, Páez 2007). For example, if one considers all the GWR coefficients for race in the fully adjusted model, the coefficients for race range from −243.0 to 279.6. These extreme coefficients are difficult to interpret and might be due to over-fitting of the model. By definition, GWR will always fit the data better than OLS and may generate these extreme values. Fourth, although GWR method substantially mitigates spatial autocorrelation in the model residuals, it does not always adequately address it (Leung et al., 2000b; Wheeler and Tiefelsdorf, 2005).
Our study indicates significant spatial heterogeneity in black-white differences in CHD mortality across the US. Poverty and segregation appear to explain at least some of this spatial heterogeneity. However, we note that the GWR results are intended to be more exploratory and hypothesis generating rather than hypothesis testing. Thus our results suggest that spatial heterogeneity in health disparities is present and suggest that further investigations of the reasons of this heterogeneity are needed.
The presence of substantial heterogeneity in black white differences in CHD mortality is consistent with recent work highlighting the context-dependence of black–white disparities in cardiovascular risks (Kershaw et al., 2011; Laveist et al., 2011). The fact that disparities are heterogeneous across space highlights these differences are not “natural” or biologically determined, but are malleable and context dependent. Additional research to identify the contextual and individual-level factors that explain the underlying local variations in racial disparities in health is warranted.
Acknowledgments
Funding
This work was supported by Center for Integrative Approaches to Health Disparities, University of Michigan, which is funded by the National Center on Minority Health and Health Disparities (P60MD002249).
References
- Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. American Journal of Public Health. 2003;93:215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali K, Partridge MD, Olfert MR. Can geographically weighted regressions improve regional analysis and policy making? International Regional Science Review. 2007;30:300–329. [Google Scholar]
- Armstrong D, Barnett E, Casper ML, Wing S. Community occupational structure, medical and economic resources, and coronary mortality among US blacks and whites, 1980–1988. Annals of Epidemiology. 1998;8:184–191. doi: 10.1016/s1047-2797(97)00202-0. [DOI] [PubMed] [Google Scholar]
- Barnett E, Casper ML, Halverson JA, Elmes GA, Braham VE, Majeed Z, Bloom A, Stanley S. Men and heart disease: an atlas of racial and ethnic disparities in mortality Morgantown. WV: Office for Social Environment and Health Research, West Virginia University; 2001. [Google Scholar]
- Barnett E, Halverson JA. Disparities in premature coronary heart disease mortality by region and urbanicity among black and white adults ages 35–64, 1985–1995. Public Health Reports. 2000;115:52–64. [PMC free article] [PubMed] [Google Scholar]
- Bird ST. Separate black and white infant mortality models: differences in the importance of structural variables. Social Science & Medicine. 1995;41:1507–1512. doi: 10.1016/0277-9536(95)00029-7. [DOI] [PubMed] [Google Scholar]
- Boykin S, Diez-Roux AV, Carnethon M, Shrager S, Ni H, Whitt-Glover M. Racial/ethnic heterogeneity in the socioeconomic patterning of CVD risk factors: in the United States: the multi-ethnic study of atherosclerosis. Journal of Health Care for the Poor and Underserved. 2011;22(1):111–127. doi: 10.1353/hpu.2011.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunsdon C, Fotheringham AS, Charlton ME. Geographically weighted regression: a method for exploring spatial nonstationarity. Geographical Analysis. 1996;28:281–298. [Google Scholar]
- Brunsdon C, Fotheringham AS, Charlton ME. Some notes on parametric significance tests for geographically weighted regression. Journal of Regional Science. 1999;39:497–524. [Google Scholar]
- Brunsdon C, Fotheringham AS, Charlton ME. Geographically weighted summary statistics: a framework for localized exploratory data analysis. Computers Environment and Urban Systems. 2002;26:501–524. [Google Scholar]
- Casper ML, Barnett E, Halverson JA, Elmes GA, Braham VE, Majeed Z, Bloom A, Stanley S. Women and heart disease: an atlas of racial and ethnic disparities in mortality Morgantown. WV: Office for Social Environment and Health Research. West Virginia University; 2000. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) [Accessed 10 June, 2010)];WONDER database. ( http://wonder.cdc.gov/mortSQL.html)
- Chen VY, Wu PC, Yang TC, Su HJ. Examining non-stationary effects of social determinants on cardiovascular mortality after cold surges in Taiwan. Science of the Total Environment. 2010;408:2042–2049. doi: 10.1016/j.scitotenv.2009.11.044. [DOI] [PubMed] [Google Scholar]
- Cho SH, Lambert DM, Chen Z. Geographically weighted regression bandwidth selection and spatial autocorrelation: an empirical example using Chinese agriculture data. Applied Economics Letters. 2010;17(8):767–772. [Google Scholar]
- Collins CA, Williams DR. Segregation and mortality: the deadly effects of racism? Sociological Forum. 1999;14:495–523. [Google Scholar]
- Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, Hogelin G, Marler J, McGovern P, Morosco G, Mosca L, Pearson T, Stamler J, Stryer D, Thom T. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- Cooper RS, Kennelly JF, Durazo-Arvizu R, Oh HJ, Kaplan G, Lynch J. Relationship between prematuremortality and socioeconomic factors in black and white populations of US metropolitan areas. Public Health Report. 2001;116:464–473. doi: 10.1093/phr/116.5.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cubbin C, Hadden WC, Winkleby MA. Neighborhood context and cardiovascular disease risk factors: the contribution of material deprivation. Ethnicity and Disease. 2001;11:687–700. [PubMed] [Google Scholar]
- Diez Roux AV, Nieto FJ, Muntaner C, Tyroler HA, Comstock GW, Shahar E, Cooper LS, Watson RL, Szklo M. Neighborhood environments and coronary heart disease: a multilevel analysis. American Journal of Epidemiology. 1997;46:48–63. doi: 10.1093/oxfordjournals.aje.a009191. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disease. The New England Journal of Medicine. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV. Residential environments and cardiovascular risk. Journal of Urban Health. 2003;80(4):569–589. doi: 10.1093/jurban/jtg065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellaway A, Macintyre S. Does where you live predict related behaviours? A case study in Glasgow. Health Bulletin. 1996;54(6):443–446. [PubMed] [Google Scholar]
- Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Social Science & Medicine. 1998;47:469–476. doi: 10.1016/s0277-9536(98)00128-2. [DOI] [PubMed] [Google Scholar]
- Farber S, Paéz A. A systematic investigation of cross-validation in GWR model estimation: empirical analysis and Monte Carlo simulations. Journal of Geographical Systems. 2007;9:371–396. [Google Scholar]
- Fotheringham AS, Brunsdon C, Charlton ME. Geographically weighted regression: the analysis of spatially varying relationships. Chichester Hoboken N.J: Wiley; 2002. [Google Scholar]
- GeoDa Center for Geospatial Analysis and Computation. Arizona State University; [(Accessed June 10, 2010)]. ( http://geodacenter.asu.edu/geodata) [Google Scholar]
- Gilbert A, Chakraborty J. Using geographically weighted regression for environmental justice analysis: cumulative cancer risks from air toxics in Florida. Social Science Research. 2011;40(1):273–286. [Google Scholar]
- Graif C, Sampson RJ. Spatial heterogeneity in the effects of immigration and diversity on neighborhood homicide rates. Homicide Studies. 2009;13:242–260. doi: 10.1177/1088767909336728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. The International Journal of Social Psychiatry. 2000;46(1):34–46. doi: 10.1177/002076400004600105. [DOI] [PubMed] [Google Scholar]
- Halverson JA, Barnett E, Casper M. Geographic disparities in heart disease and stroke mortality among black and white populations in the Appalachia region. Ethnicity and Disease. 2002;12:S3-82–S3-91. [PubMed] [Google Scholar]
- Harper S, Lynch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983–2003. JAMA. 2007;297:1224–1232. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- Hart KD, Kunitz SJ, Sell RR, Mukamel DB. Metropolitan governance, residential segregation, and mortality among African Americans. American Journal of Public Health. 1998;88:434–438. doi: 10.2105/ajph.88.3.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C, Diez Roux AV, Jacobs DR, Jr, et al. Neighborhood characteristics, individual level socioeconomic factors, and depressive symptoms in young adults: the CARDIA study. Journal of Epidemiology and Community Health. 2005;59:322–328. doi: 10.1136/jech.2003.018846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt JB, Lo CP. The geography of mortality in the Atlanta metropolitan area. Computers, Environment and Urban Systems. 2008;32:149–164. [Google Scholar]
- Hoyert DL, Kung HC, Smith BL. Deaths: preliminary data for 2003. National Vital Statistics Reports. 2005;53:1–48. [PubMed] [Google Scholar]
- Huang Y, Leung Y. Analyzing regional industrialization in Jiangsu province using geographically weighted regression. Journal of Geographical Systems. 2002;4:233–249. [Google Scholar]
- Keenan NL, Shaw KM. Coronary heart disease and stroke deaths—United States. Morbidity and Mortality Weekly Report. 2011;60(suppl.):62–66. [PubMed] [Google Scholar]
- Kershaw KN, Diez Roux A, Burgard S, Lisabeth L, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and Black–White disparities in hypertension. American Journal of Epidemiology. 2011 doi: 10.1093/aje/kwr116. http://dx.doi.org/10.1093/aje/kwr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiologic Reviews. 2009 doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA. Separation, poverty, and empowerment: health consequences for African Americans. Millbank Quarterly. 1993;73(1):41–64. [PubMed] [Google Scholar]
- Laveist T, Pollack K, Thorpe R, Jr, Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Affairs. 2011;30(10):1880–1887. doi: 10.1377/hlthaff.2011.0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung Y, Mei C, Zhang W. Statistical tests for spatial nonstationary based on the geographically weighted regression model. Environment and Planning A. 2000a;32:9–32. [Google Scholar]
- Leung Y, Mei C, Zhang W. Testing for spatial autocorrelation among the residuals of the geographically weighted regression. Environment and Planning A. 2000b;32:871–890. [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalised linear models. Biometrika. 1986;73:12–22. [Google Scholar]
- Lloyd-Jones D, Adams RJ, Brown TM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- Massey DS, Denton NA. The dimensions of residential segregation. Social Forces. 1988;67:281–315. [Google Scholar]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran PAP. Notes on continuous stochastic phenomena. Biometrika. 1950;37:17–23. [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux AV, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Pickle LW, Gillum RF. Geographic variation in cardiovascular disease mortality in US blacks and whites. Journal of National Medical Association. 1999;91:545–556. [PMC free article] [PubMed] [Google Scholar]
- Polednak AP. Poverty, residential segregation, and black/white mortality ratios in urban areas. Journal of Health Care for the Poor and Underserved. 1993;4:363–373. doi: 10.1353/hpu.2010.0094. [DOI] [PubMed] [Google Scholar]
- Polednak AP. Segregation, discrimination and mortality in U.S. blacks. Ethnicity & Disease. 1996a;6:99–108. [PubMed] [Google Scholar]
- Polednak AP. Trends in US urban black infant mortality, by degree of residential segregation. American Journal of Public Health. 1996b;86:723–726. doi: 10.2105/ajph.86.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team. R Foundation for Statistical Computing. Vienna, Austria: 2010. R: A language and environment for statistical computing. ISBN 3-900051-07-0, URL < http://www.R-project.org>. [Google Scholar]
- Ross CE. Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior. 2000;41(2):177–187. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Kannan S, Dvonch JT, Israel BA, Allen 3rd A, James SA, House JS, Lepkowski J. Social and physical environments and disparities in risk for cardiovascular disease: the healthy environments partnership conceptual model. Environmental Health Perspectives. 2005;113:1817–1825. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Williams DR, Israel BA, Lempert LB. Racial and spatial relations as fundamental determinants of health in Detroit. Milbank Quarterly. 2002;80:677–707. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shihadeh ES, Flynn N. Segregation and crime: the effect of black social isolation on the rates of black urban violence. Social Forces. 1996;74:1325–1352. [Google Scholar]
- Silver E, Mulvey EP, Swanson JW. Neighborhood structural characteristics and mental disorder: Faris and Dunham revisited. Social Science & Medicine. 2002;55:1457–1470. doi: 10.1016/s0277-9536(01)00266-0. [DOI] [PubMed] [Google Scholar]
- Smith GD, Hart C, Watt G, Hole D, Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley study. Journal of Epidemiology and Community Health. 1998;52(6):399–405. doi: 10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundquist K, Malmstrom M, Johansson SE. Neighborhood deprivation and incidence of coronary heart disease: a multilevel study of 2.6 million women and men in Sweden. Journal of Epidemiology and Community Health. 2004;58:71–77. doi: 10.1136/jech.58.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassone EC, Waller LA, Casper MA. Small-area racial disparity in stroke mortality: an application of Bayesian spatial hierarchical modeling. Epidemiology. 2009;20:234–241. doi: 10.1097/EDE.0b013e3181935aee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller L, Zhu L, Gotway C, Gorman D, Gruenewald P. Quantifying geographic variations in associations between alcohol distribution and violence: a comparison of geographically weighted regression and spatially varying coefficient models. Stochastic Environmental Research and Risk Assessment (SERRA) 2007;21(5):573–588. [Google Scholar]
- Wheeler D, Tiefelsdorf M. Multicollinearity and correlation among local regression coefficients in geographically weighted regression. Journal of Geographical Systems. 2005;7:161–187. [Google Scholar]
- White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health & Place. 2011;17:438–448. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Report. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing S, Casper M, Davis W, Hayes C, Riggan W, Tyroler HA. Trends in the geographic inequality of cardiovascular disease mortality in the United States, 1962–1982. Social Science & Medicine. 1990;30:261–266. doi: 10.1016/0277-9536(90)90181-q. [DOI] [PubMed] [Google Scholar]
- Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. New England Journal of Medicine. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- van Jaarsveld CH, Miles A, Wardle J. Pathways from deprivation to health differed between individual and neighborhood-based indices. Journal of Clinical Epidemiology. 2007;60:712–719. doi: 10.1016/j.jclinepi.2006.10.005. [DOI] [PubMed] [Google Scholar]