Abstract
Cardiac conduction is mediated by gap junction channels that are formed by connexin (Cx) protein subunits. The connexin family of proteins consists of more than 20 members varying in their biophysical properties and ability to combine with other connexins into heteromeric gap junction channels. The mammalian heart shows regional differences both in connexin expression profile and in degree of electrical coupling. The latter reflects functional requirements for conduction velocity which needs to be low in the sinoatrial and atrioventricular nodes and high in the ventricular conduction system. Over the past 20 years knowledge of the biology of gap junction channels and their role in the genesis of cardiac arrhythmias has increased enormously. This review focuses on the insights gained from transgenic mouse models. The mouse heart expresses Cx30, 30.2, 37, 40, 43, 45, and 46. For these connexins a variety of knock-outs, heart-specific knock-outs, conditional knock-outs, double knock-outs, knock-ins and overexpressors has been studied. We discuss the cardiac phenotype in these models and compare Cx expression between mice and men. Mouse models have enhanced our understanding of (patho)-physiological implications of Cx diversity in the heart. In principle connexin-specific modulation of electrical coupling in the heart represents an interesting treatment strategy for cardiac arrhythmias and conduction disorders.
Keywords: gap junctions, connexins, mouse models, conduction, arrhythmias, cardiac
Introduction
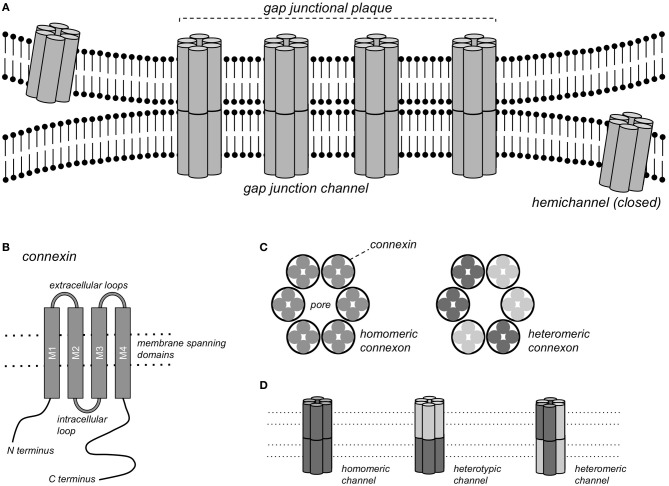
Gap junction channels form continuous pores between the cytoplasms of closely apposed cells that are permeable to ions and molecules <1 kDa, thereby conferring electrical and metabolic coupling between neighboring cells. Gap junction channels consist of connexin (Cx) protein subunits. More than 20 Cx isoforms have been described in both humans and mice and mutations in Cx genes have been implicated in various inheritable diseases (Sohl and Willecke, 2004; Dobrowolski and Willecke, 2009). Complete gap junction channels are formed by the docking of two hemichannels, or connexons, contributed by closely apposed cells (Figure 1). Each connexon consists of 6 connexin subunits, and a homomeric gap junction channel consists of 12 Cx proteins of the same isoform. When two homomeric connexons consisting of different connexins are apposed, a heterotypic channel may form if those connexins are compatible. In heteromeric connexons, different isoforms are mixed, and a heteromeric channel may form. Some Cxs also form functional hemichannels, i.e., connexons that can open under certain conditions, causing depolarization of the plasma membrane (John et al., 1999; Bukauskas et al., 2006).
Figure 1.
Gap junction channels. (A) Schematic representation of a gap junctional plaque, with each of the neighboring cells contributing one hemichannel to form the complete gap junction channel. (B) Structure of the pattern of a single connexin subunit with 4 domains traversing the membrane. (C) A hemichannel or connexon consists of a hexagonal arrangement of 6 Cx subunits, either of the same Cx isoform (homomeric connexon) or of different isoforms (heteromeric connexon). (D) Gap junction channels formed by homomeric connexons of the same isoform (homomeric channel), by homomeric connexons of different isoforms (heterotypic channel) or by heteromeric connexons (heteromeric channels).
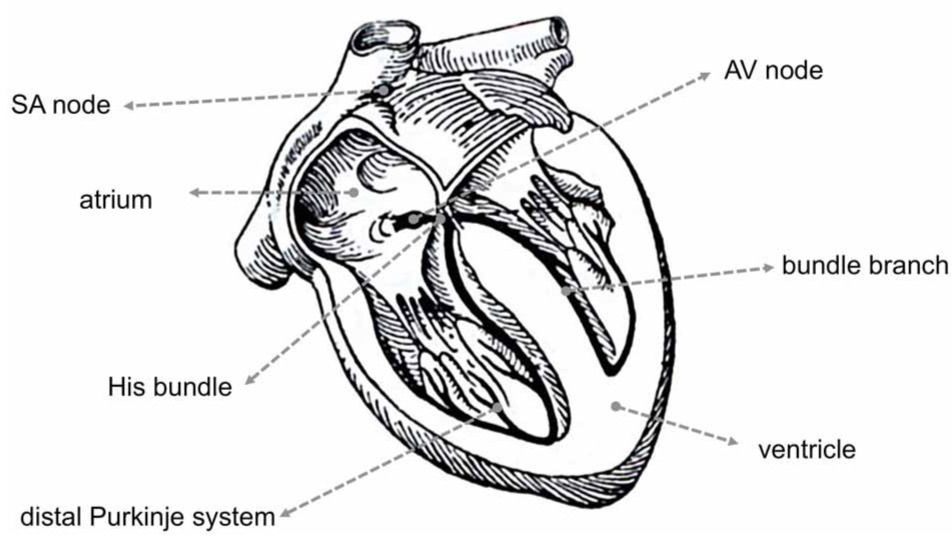
Different regions of the heart show specific profiles of Cx expression, which in mouse and human hearts show many similarities, but also some important differences (Table 1). Different parts of the heart also have varying requirements for the degree of electrical coupling. To spread the activation wave rapidly over the ventricles, the large Purkinje myocytes of the specialized ventricular conduction system need to be strongly coupled. To create a delay between the atrial and ventricular contraction, a very low degree of coupling is required in the atrioventricular (AV) node. Similarly, to allow pacemaker function, pacemaker myocytes in the sinoatrial (SA) node need to be weakly coupled, otherwise the pacemaker (or ectopic focus) would in effect be silenced by the surrounding working myocardium (Joyner and van Capelle, 1986; Joyner et al., 2000).
Table 1.
Comparison of Cx regional expression in the mouse and human heart.
 | ||||
|---|---|---|---|---|
| Mouse | References | Human | References | |
| SA node | Cx45, Cx30.2, (Cx30, Cx46) | Verheijck et al., 2001; Kreuzberg et al., 2005; Chi et al., 2010; Gros et al., 2010 | Cx45, Cx40 | Davis et al., 1995; Chandler et al., 2009; Kreuzberg et al., 2009 |
| Atria | Cx40, Cx43, ((Cx45)) | Delorme et al., 1995, 1997; Alcoléa et al., 2004; Miquerol et al., 2004 | Cx40, Cx43, (Cx45) | Davis et al., 1995; Vozzi et al., 1999; Kanagaratnam et al., 2002; Kreuzberg et al., 2009; Greener et al., 2011 |
| AV node (compact) | Cx45, Cx30.2 | Coppen et al., 2001; Miquerol et al., 2004; Kreuzberg et al., 2006 | Cx40, Cx45 | Davis et al., 1995; Kreuzberg et al., 2009; Greener et al., 2011 |
| His bundle | Cx40, Cx45, (Cx30.2, Cx46) | Simon et al., 1998; Coppen et al., 1999, 2001; Kreuzberg et al., 2006; Chi et al., 2010 | Cx40, Cx43 | Hucker et al., 2008; Greener et al., 2011 |
| Bundle branches | Cx40, Cx45, (Cx46) | Simon et al., 1998; Coppen et al., 1999, 2001; van Rijen et al., 2001; Chi et al., 2010 | Cx45 | Davis et al., 1995; Coppen et al., 2003; Kreuzberg et al., 2009; Greener et al., 2011 |
| Distal Purkinje system | Cx40, Cx43, Cx45, (Cx46) | Coppen et al., 1999; Miquerol et al., 2003; Chi et al., 2010 | Cx40, Cx43, (Cx45) | van Kempen et al., 1995; Coppen et al., 2003; Kreuzberg et al., 2009 |
| Ventricles | Cx43, ((Cx45)) | Delorme et al., 1997; Stein et al., 2009; Bao et al., 2011 | Cx43, (Cx45) | Davis et al., 1995; Vozzi et al., 1999; Dupont et al., 2001; Kreuzberg et al., 2009; Greener et al., 2011 |
(Cx) and ((Cx)) signify relatively small and trace amounts.
Cardiac gap junctions are highly dynamic structures, with a Cx43 protein half-life of a few hours and a comparably rapid redistribution in response to e.g., ischemia (Beardslee et al., 1998; Smyth et al., 2012). Connexins interact directly with numerous other cellular proteins, e.g., cytoskeletal components (Herve et al., 2007). Apart from their well-established roles in electrical and metabolic coupling, a number of other functions of Cx proteins are emerging, for example in mechanical adhesion and interactions with voltage-gated membrane channels (Agullo-Pascual and Delmar, 2012) and, in the case of Cx43, in mitochondrial metabolism (Ruiz-Meana et al., 2008). Conversely, electrical coupling may be mediated not only by gap junction channels, but also to some degree by ephaptic coupling, i.e., by electric field effects (Sperelakis, 2002; Lin and Keener, 2010).
Connexins differ in various biophysical properties, such as single channel conductance, permeability to larger (dye) molecules and sensitivity to the cytoplasmic pH and transjunctional potential difference, (see e.g., Elfgang et al., 1995; Gonzalez et al., 2007; Rackauskas et al., 2010). Concerning the latter, gap junction channels may close during prolonged, large voltage differences between cells, for example when one myocyte fires an action potential while its direct neighbor remains at rest (Lin and Veenstra, 2004; Lin et al., 2005). While such large voltage gradients can be imposed in voltage clamp experiments, they are unlikely to occur in the heart. Even in regions with a relatively low degree of electrical coupling, such as the SA node, transjunctional potential differences >10 mV last only a few milliseconds (Verheule et al., 2001), which would be too short for the slow process of voltage-dependent inactivation of gap junction channels.
Cx trafficking, degradation, channel gating and permeability can be regulated by phosphorylation of serine and tyrosine residues (Solan and Lampe, 2009). During ischemia, intracellular acidification, release of lipids and channel phosphorylation cause channel closure and redistribution (Dhein, 2006). This response to ischemia allows the confinement of diseased from healthy myocardium, thus enabling the myocardium to “heal-over” (de Mello et al., 1969). On the other hand, redistribution of connexins under pathological conditions has been implicated in arrhythmogenesis (Salameh and Dhein, 2011; Duffy, 2012).
Much of our current knowledge of cardiac connexins stems from studies on mouse models (Table 2). There are numerous similarities, but also some important differences between the hearts of mice and humans (Kaese and Verheule, 2012). In this review, we will discuss evidence from genetically engineered mouse models on the properties and roles of the various cardiac connexins, highlighting both their role during cardiac development and in the adult heart.
Table 2.
Overview of genetically engineered mouse models.
| Type | Model | Initial description |
|---|---|---|
| Knock-out | Cx30−/− | Gros et al., 2010 |
| Cx30.2−/− | Kreuzberg et al., 2006 | |
| Cx37−/− | Simon et al., 1997; Munger et al., 2013 | |
| Cx40−/− | Kirchhoff et al., 1998; Simon et al., 1998 | |
| Cx43−/− | Reaume et al., 1995 | |
| Cx45−/− | Kumai et al., 2000 | |
| Cx46−/− | Chi et al., 2010 | |
| Conditional Knockout | Cx43 inducible | Eckardt et al., 2004 |
| Cx43 heart-specific | Gutstein et al., 2001a | |
| Cx43 chimera | Gutstein et al., 2001b | |
| Cx45 heart-specific | Frank et al., 2012 | |
| Overexpression | Cx43 | Ewart et al., 1997 |
| Cx45 | Betsuyaku et al., 2006 | |
| Double knock-outs | Cx30.2−/−–Cx40−/− | Schrickel et al., 2009 |
| Cx30.2−/−–Cx45inducible | Frank et al., 2012 | |
| Cx32−/−–Cx43−/− | Houghton et al., 1999 | |
| Cx37−/−–Cx40−/− | Simon et al., 2004 | |
| Cx40−/−–Cx43−/− and +/− | Kirchhoff et al., 2000; Simon et al., 2004 | |
| Cx40−/−–Cx45+/− | Kruger et al., 2006 | |
| Knock-ins | Cx40 KI Cx45 | Alcoléa et al., 2004 |
| Cx43 KI Cx26 | Winterhager et al., 2007 | |
| Cx43 KI Cx31 | Zheng-Fischhofer et al., 2006 | |
| Cx43 KI Cx32 | Plum et al., 2000 | |
| Cx43 KI Cx40 | Plum et al., 2000 | |
| Cx45 KI Cx36 | Frank et al., 2010 | |
| Mutants | Cx43 K258stop | Maass et al., 2004, 2007 |
| Cx43 S325/328/330 E or A | Remo et al., 2011 | |
| Cx43 I130T | Kalcheva et al., 2007 | |
| Cx43 G138R | Dobrowolski et al., 2008 | |
| Cx43 G60S | Flenniken et al., 2005; Manias et al., 2008 |
Connexin 30
Cx30 forms channels with a large single channel conductance (γj) of 179 pS (in K-aspartate), a potential of half-maximal inactivation (V1/2) of 27 mV and a voltage-independent fraction (Gj, min) of 0.15 (Valiunas et al., 1999). Cx30 is expressed at low abundance in the murine SA node (Gros et al., 2010). Interestingly, Cx30-deficient mice have a 9% higher heart rate than wild type (Wt) mice and a lower beat-to-beat variability (Gros et al., 2010). This increased rate was still present under autonomic blockade, indicating that Cx30 affects the intrinsic pacemaker frequency. The presence of Cx30 could conceivably enhance electrical coupling between the SA node and the surrounding atrium and thereby decelerate impulse formation within the SA node (Dhein, 2010; Gros et al., 2010). However, it is not known whether Cx30 in the SA node forms heteromeric gap junction channels with the other connexins present (Cx30.2 and Cx45), and whether this would increase or decrease cell-to-cell electrical coupling.
Connexin 30.2
Cx30.2, the murine ortholog of human Cx31.9 (Belluardo et al., 2001), forms small conductance, weakly voltage-dependent channels [γj = 9 pS, V1/2 > 60 mV (Kreuzberg et al., 2005)]. Cx30.2 is expressed in the murine SA node, AV node and His bundle (Kreuzberg et al., 2005). In transfected HeLa cells, Cx30.2 can form both heterotypic (Kreuzberg et al., 2005) and heteromeric (Gemel et al., 2008) channels with Cx40, Cx43, and Cx45, the major myocardial connexins. Cx30.2 was colocalized with Cx45 in the SA and AV nodes, but not with Cx40 and Cx43 (Kreuzberg et al., 2005). Surprisingly, Cx30.2 deficient mice display accelerated AV nodal conduction, a decrease in AV Wenckebach period and a higher ventricular rate during atrial fibrillation (Kreuzberg et al., 2006). In addition, whereas deletion of Cx40 slows AV conduction, it is normal in mice deficient for both Cx30.2 and Cx40 (Schrickel et al., 2009), suggesting that the balance between Cx40 and Cx30.2 is an important determinant of AV conduction in mice. Cx30.2 is able to form functional hemichannels (Bukauskas et al., 2006), which in the open state would decrease the membrane resistance and thereby slow conduction, but the role of these hemichannels in the adult heart is uncertain at present. During development, Cx30.2 expression and proper development of the AV conduction system is determined by an enhancer region under the control of Tbx5 and GATA4. Accordingly, the PR interval is shortened in GATA4+/− mice (Munshi et al., 2009). Moreover, inhibition of Notch signaling during development leads to a loss of Cx30.2 expressing cells, hypoplasia of the AV node and accelerated AV conduction (Rentschler et al., 2011). It is important to note that Cx31.9, the human ortholog of murine Cx30.2, is not expressed in the human SA and AV nodes, ventricular conduction system or working myocardium (Kreuzberg et al., 2009). This indicates that the presence of Cx30.2 may reflect an adaptation in the small mouse heart to allow high activation frequencies and optimize A-V timing. In addition to this difference, AV conduction system in the mouse is also electrically connected to the ventricles at the basal part of the septum, leading to a baso-apical activation pattern within the septum (van Rijen et al., 2001).
Connexin 37
Cx37 forms large conductance channels that are moderately voltage sensitive [γj = 200–250 pS in K-glutamate, V1/2 = 28 mV, Gj, min = 0.27 (Reed et al., 1993)]. In the adult heart, Cx37 is expressed by endothelial cells in blood vessels and the endocardial lining of the chambers, although expression has also been observed in parts of the ventricular myocardium during embryonic development (Haefliger et al., 2000). Cx37−/− mice do not develop venous and lymphatic valves (Munger et al., 2013). In addition, mice lacking both Cx37 and Cx40 show a high incidence of atrial and ventricular septal defects at birth (Simon et al., 2004).
Connexin 40
Properties and expression
Cx40 forms channels with a large single channel conductance and moderate voltage-sensitivity [γj = 150 pS in KCl, V1/2 = 44 mV, Gj, min = 0.5 (Traub et al., 1994)]. In the developing mouse heart, Cx40 is widely expressed in the ventricles and atria at embryonic day 11. From day 14 onwards, Cx40 becomes restricted to the conduction system in the ventricles, but it remains present in the atrial working myocardium (Delorme et al., 1995). The transcription factors Tbx2 and Tbx3 repress Cx40 expression (Hoogaars et al., 2004; Aanhaanen et al., 2011). Inactivation of Tbx2 leads to the formation of Cx40-expressing accessory pathways and ventricular preexcitation (Aanhaanen et al., 2011). On the other hand, Cx40 expression is increased by Nkx2-5 (Harris et al., 2006) and Tbx5 (Pizard et al., 2005; Arnolds et al., 2012) that delineate the conduction system. In fact, normal development of the ventricular conduction system requires the expression of Cx40 (Sankova et al., 2012).
In the adult mouse heart, Cx40 is expressed by atrial myocytes and ventricular conduction system (His bundle, left and right bundle branches and Purkinje network) (Simon et al., 1998; Miquerol et al., 2004; van Veen et al., 2005b). The selective expression of Cx40 by the conduction system within the ventricle has allowed sophisticated functional studies on conduction within the Purkinje network (Miquerol et al., 2004; Tallini et al., 2007).
Atria
Information on the effect of Cx40-deficiency on atrial conduction is somewhat contradictory. In the first studies, the P wave duration was significantly prolonged (Kirchhoff et al., 1998; Simon et al., 1998; Hagendorff et al., 1999; Verheule et al., 1999; Bagwe et al., 2005). Some other studies have not reproduced this observation (Bevilacqua et al., 2000; Tamaddon et al., 2000; Vanderbrink et al., 2000). Measurement of P-wave duration in mice is not straightforward, requiring different leads to accurately determine the end of the biphasic P-wave. In two studies that measured atrial conduction directly using direct contact mapping or optical mapping, a reduction in conduction velocity was observed (Verheule et al., 1999; Bagwe et al., 2005). However, a later study used optical mapping to show that deletion of Cx40 did not affect conduction velocity, but did abolish the difference in conduction velocity between the left and right atria (Leaf et al., 2008).
Atrial myocytes express both Cx40 and 43. Based on expression studies in Xenopus oocytes, Cx40 and 43 were originally thought to be incompatible (White and Bruzzone, 1996). However, later studies presented compelling evidence that Cx40 and 43 can form both heterotypic (Valiunas et al., 2000) and heteromeric (He et al., 1999; Cottrell and Burt, 2001) gap junction channels in mammalian cells, including adult atrial myocytes (Elenes et al., 1999). In cultured neonatal mouse atrial myocytes, Cx40 and 43 appear to make equal contributions to total gap junctional conductance (Lin et al., 2010). Intriguingly, a study on cultured strands of atrial myocytes that the Cx40/Cx43 ratio was an important determinant of propagation, with Cx43 increasing and Cx40 decreasing conduction velocity (Beauchamp et al., 2006).
In intact Cx40−/− mice, episodes of atrial tachyarrythmias/atrial fibrillation could be induced by transesophageal pacing (Hagendorff et al., 1999) and direct atrial pacing (Verheule et al., 1999; Bevilacqua et al., 2000). In perfused Cx40−/− mouse hearts studied with optical mapping, atrial ectopic beats and intraatrial conduction block during pacing at high rates were reported (Bagwe et al., 2005).
Sinoatrial node
In contrast to larger species, such as rabbits (Verheule et al., 2001), pacemaker myocytes in the central SA node do not express Cx40 (Verheijck et al., 2001; Wiese et al., 2009) However, Cx40-deficiency does cause a modest increase in sinus cycle length (Hagendorff et al., 1999; Verheule et al., 1999; Bevilacqua et al., 2000; de Wit et al., 2003), and an increase in (corrected) SA node recovery time (Hagendorff et al., 1999; Verheule et al., 1999). The effects of Cx40-deficiency on SA node function may be caused either by altered conduction from the SA node to the atrium and/or by the phenomenon that the “atrial pacemaking complex” may be much larger than the area that is classically considered to be the sinus node (Glukhov et al., 2010).
Atrioventricular conduction
AV conduction is also affected in Cx40−/− mice, reflected in a prolonged PR interval, increased QRS duration and a QRS morphology reminiscent of right bundle branch block in humans (Kirchhoff et al., 1998; Simon et al., 1998; Verheule et al., 1999; Bevilacqua et al., 2000; Vanderbrink et al., 2000). In addition, episodes of 2nd and 3rd degree AV block were observed in Cx40−/− mice (Kirchhoff et al., 1998; Hagendorff et al., 1999). With minor differences between studies, Cx40-deficiency prolongs the AV effective refractory period (ERP), the cycle lengths of A to V Wenckebach and 2:1 block, while the atrial ERP, ventricular ERP, cycle lengths of V to A Wenckebach and 2:1 block are not affected (Hagendorff et al., 1999; Verheule et al., 1999; Bevilacqua et al., 2000; Vanderbrink et al., 2000). Although Cx40 is not expressed in the central AV node (Delorme et al., 1995; Simon et al., 1998; Coppen et al., 1999), the AH interval is prolonged in intact mice (Bevilacqua et al., 2000; Vanderbrink et al., 2000), AV nodal conduction curves are shifted (Vanderbrink et al., 2000) and AV nodal facilitation is reversed (Zhu et al., 2005), indicative of an effect on the AV node itself. However, AV nodal conduction curves recorded in perfused hearts did not differ between Wt and Cx40−/− mice (van Rijen et al., 2001), suggesting a possible role of autonomic activity in the observations in intact mice.
Both the left and right bundle branch normally express high levels of Cx40 (Simon et al., 1998; van Rijen et al., 2001). High resolution mapping has revealed that deletion of Cx40 leads to slower conduction in the left bundle branch and conduction block in the thinner right bundle branch, causing a delayed activation of the right ventricle (Tamaddon et al., 2000; van Rijen et al., 2001). Interestingly, in mice the common bundle (expressing Cx40 and 45) is electrically connected to the base of the interventricular septum (expressing Cx43) through a small transitional zone expressing Cx43 and 45 (van Rijen et al., 2001; van Veen et al., 2005b) This arrangement results in an activation pattern within the septum from base to apex that is quite different from the pattern in humans (Durrer et al., 1970).
Ventricles
In the ventricular myocardium, which expresses Cx43 but not Cx40, conduction velocity is unaffected by Cx40-deficiency and the inducibility of ventricular arrhythmias under normal conditions was not increased (Verheule et al., 1999; Bevilacqua et al., 2000; Tamaddon et al., 2000), although one study reported an increased inducibility of ventricular tachycardia (VT) in Cx40−/− mice during infusion of isoproterenol (Bevilacqua et al., 2000), possibly involving the Purkinje system.
In none of the studies mentioned above did heterozygous Cx40+/− mice display a electrophysiological phenotype that differed from Cx40+/+ mice, indicating that even a substantial reduction in Cx40 protein does not greatly affect cardiac conduction in mice. Moreover, although it differs considerably in its biophysical properties, Cx45 can replace Cx40 almost completely, because cardiac activation in Cx40KICx45 mice is normal, except for a slower conduction velocity in the left atrium and right bundle branch (Alcoléa et al., 2004).
Two factors complicate the interpretation of electrophysiological data from Cx40−/− mice. First, although this was not noted in the earliest studies, Cx40 deficient mice display a high incidence of a variety of cardiac malformations, including ventricular septal defects, tetralogy of Fallot, double-outlet right ventricles, endocardial cushion and aortic arch defects (Kirchhoff et al., 2000; Gu et al., 2003). The occurrence of cardiac malformations is exacerbated in mice in which a homozygous deletion of Cx40 is combined with a heterozygous deletion of either Cx43 (Kirchhoff et al., 2000) or Cx45 (Kruger et al., 2006), leading to neonatal lethality in the former and additional atrial defects and further delayed AV conduction in the latter. Mice that are homozygously deficient for both Cx40 and 43 die much earlier than Cx43−/− mice, around embryonic day 12, with an abnormal rotation of the ventricles (Simon et al., 2004). Second, apart from expression by atrial myocytes and Purkinje cells, Cx40 is also expressed by endothelial cells (Dahl et al., 1995), together with Cx37. Interestingly, de Wit et al have reported that in Cx40−/− mice, arterioles show spontaneous, irregular vasomotion and that blood pressure is greatly increased from 90 to 120 mmHg (de Wit et al., 2003). To what extent hypertension in Cx40−/− mice is responsible for secondary changes in cardiac pump function, autonomic regulation and electrophysiology (e.g., decreased heart rate and slower AV nodal conduction) is uncertain at present.
Connexin 43
Properties and expression
Cx43 forms channels with a single channel conductance of 120 pS (in CsCl) and a modest voltage dependence (V1/2 = 60 mV and Gj, min = 0.4) (Elenes et al., 2001).
In the developing mouse heart, Cx43 is specifically present in the trabeculated parts of the ventricle at embryonic day 12.5, but is abundantly expressed by the entire working myocardium later on (Coppen et al., 2003; Miquerol et al., 2003). Cx43 expression is suppressed by the transcription factors Tbx18 (specifying the SA node), Tbx2 and Tbx3 (specifying the AV conduction system) (Christoffels et al., 2004; Bakker et al., 2008; Kapoor et al., 2011; Sizarov et al., 2011).
Cx43−/− mice die shortly after birth from respiratory failure caused by a right ventricular outflow tract obstruction (Reaume et al., 1995). Abnormal cardiac development is already visible during the looping phase at embryonic day 10 (Ya et al., 1998). The outflow tract defect can be traced back to the neural crest, where abnormal p53 activation in Cx43−/− mice causes apoptosis of primordial germ cells that would otherwise have migrated to the heart (Lo et al., 1997; Francis and Lo, 2006). Both a deficiency and an excess of Cx43 can derail this process (Ewart et al., 1997; Huang et al., 1998), although it does not necessarily depend on Cx43 expression in the neural crest itself (Kretz et al., 2006). In addition to this defect, Cx43−/− (and Cx43+/−) mice also show abnormal patterning of the main coronary arteries (Li et al., 2002; Walker et al., 2005; Liu et al., 2006).
Ventricular conduction
Using optical mapping in Cx43−/− mouse embryos, Vaidya et al reported that ventricular conduction velocity was unaffected at embryonic day 12.5, when Cx40 is still present abundantly in the ventricle. At embryonic day 17.5 however, ventricular conduction velocity was greatly reduced and ventricular arrhythmias were frequently observed (Vaidya et al., 2001). Accordingly, gap junctional coupling and conduction velocity are dramatically reduced in cultured neonatal myocytes from Cx43−/− mice, which do not show a compensatory increase in Cx40 and 45 (Beauchamp et al., 2004; Vink et al., 2004).
In adult mice, Cx43 is expressed in the atrial and ventricular working myocardium and in the distal Purkinje system (Gourdie et al., 1991; Gros and Jongsma, 1996; van Veen et al., 2005b). Within the ventricular wall, Cx43 expression is lower in the epicardium than in deeper regions (Yamada et al., 2004). Unlike Cx43−/− mice, Cx43+/− mice survive and age normally (Betsuyaku et al., 2002), although ventricular and atrial level of Cx43 protein are reduced by approximately 50% (Guerrero et al., 1997; Thomas et al., 1998). There has been a debate about to what extent this reduction in expression affects conduction, with one group reporting a 50% reduction in ventricular conduction velocity (Guerrero et al., 1997; Eloff et al., 2001), and another group reporting no change (Morley et al., 2000). The latter result is in better agreement with studies using mathematical models, which predict a weaker dependence of conduction velocity on gap junctional coupling (Shaw and Rudy, 1997; Wiegerinck et al., 2006) and a study on strands of cultured myocytes from Cx43+/+ and Cx43+/− mice, which did not show a difference in conduction velocity (Thomas et al., 2003). Moreover, two later studies in adult mice with conditional deletion of Cx43 showed a reduction of conduction velocity by approximately 40% while Cx43 protein level was decreased by 90% (Gutstein et al., 2001a; van Rijen et al., 2004). Conduction anisotropy and heterogeneity were increased, especially in the RV. VT was readily induced by pacing, often with a stable reentrant circuit in the RV and fibrillatory conduction in the LV (van Rijen et al., 2004). Telemetric recordings revealed that most mice die from arrhythmic sudden death within weeks of the start of Cx elimination (Gutstein et al., 2001a). By contrast, in a conditional knock-out strain with a 50% reduction in Cx43, no change in conduction velocity was observed and no arrhythmias were inducible (van Rijen et al., 2004).
Similar findings were reported in mice with a cardiac-specific deletion with a gradual postnatal decline in Cx43 expression. At birth, cardiac structure in these mice is normal (Eckardt et al., 2006), but Cx43 protein decreases to 59% of control level at 25 days (without a change in conduction velocity) and 18% at 45 days (with a 50% decrease in conduction velocity). At the latter stage, lethal VTs could be induced in 80% of the mice (Danik et al., 2004). Interestingly, optical mapping during sinus rhythm in this model revealed ectopic sites of ventricular activation caused by a paradoxical increase in conduction across Purkinje-ventricular junctions (Morley et al., 2005). In another approach, chimeric mice were produced with a patchy Cx43 expression pattern in the ventricles. In addition to a depressed pump function, these mice showed heterogeneous ventricular conduction and spontaneous non-sustained VT (Gutstein et al., 2001b, 2005).
Replacement of Cx43
Several studies have assessed whether the role of Cx43 can be taken over by other Cxs, using knock-in mouse models in which Cx43 was replaced by Cx40, 32, 31, or 26. Anatomically, Cx43KI40 hearts showed no abnormalities at birth (apart from mild hypertrophy in some mice), whereas Cx43KI32 hearts showed a mild form of the RV outflow tract abnormalities seen in Cx43−/− mice (Plum et al., 2000). ECG intervals in adult Cx43KI32 and Cx43KI40 mice did not differ from those in control mice. However, spontaneous ventricular extrasystoles were observed more frequently in Cx43KI40 mice than in Cx43KI32 and control mice. In Cx43KI31 mice, the RV outflow tract obstruction is severe, cardiac conduction is markedly slow and mice die within days after birth (Zheng-Fischhofer et al., 2006). In this context it is worth noting that Cx31 is highly restricted in its ability to form channels with other Cxs (Elfgang et al., 1995). Neonatal Cx43KI26 mice do not have structurally abnormal hearts, have only slightly decelerated cardiac conduction, but died within weeks because of deficient lactation of their heterozygous mothers (Winterhager et al., 2007). Adult Cx43KI26 mice (reared by foster mothers) showed a small prolongation in His-to-ventricle conduction time and QRS duration. Thus, several connexins are able to replace Cx43 in the developing and heatlhy adult heart to a large degree. However, the consequences of replacing Cx43 may be more pronounced under pathological conditions (see below for an example in Cx43KI32 mice).
Response to ischemia
In the ventricles, the closing of gap junction channels in response to ischemia enables the myocardium to “heal-over” (de Mello et al., 1969), but it is also associated with (phase 1b) arrhythmias occurring 15–60 min after the onset of ischemia (De Groot and Coronel, 2004; Wit and Peters, 2012). During acute ischemia, spontaneous and induced VT occurred more frequently in Cx43+/− than in Cx43+/+ mice (Lerner et al., 2000). However, infarct size in the weeks after coronary occlusion was smaller in Cx43+/− mice (Kanno et al., 2003). At those later time points, the incidence of spontaneous and induced VT did not differ between Cx43+/− and Cx43+/+ mice, suggesting that effect of reduced coupling is offset by the smaller infarct size (Betsuyaku et al., 2004).
Cx43 hemichannels are present in the plasma membrane and can open as a non-selective pore in response to metabolic inhibition, which would accelerate cell death (John et al., 1999; Kondo et al., 2000). Gap 19, a peptide that prevents hemichannel opening, without affecting gap junction channels, reduces ischemia/reperfusion damage (Wang et al., 2013).
In addition, Cx43 is located in the nuclear membrane and in subsarcolemmal mitochondria (Rodriguez-Sinovas et al., 2007; Boengler et al., 2009). Ischemic preconditioning increases the levels of mitochondrial Cx43 (Boengler et al., 2005) and accordingly, ischemic preconditioning is lost in Cx43+/− mice (Schwanke et al., 2002; Li et al., 2004). Cx43 is involved in mitochondrial K+ uptake (Miro-Casas et al., 2009) and respiration (Boengler et al., 2012), forming hemichannels in the mitochondrial inner membrane that interact with other proteins (Rodriguez-Sinovas et al., 2007).
The carboxy terminus of the Cx43 protein is an important regulatory domain, involved in e.g., the response to intracellular acidification (Duffy et al., 2004). A mutant with a C terminal truncation shows a redistribution of Cx43 to the periphery of larger, sparser gap junctions (Maass et al., 2007). After ischemia/reperfusion, this mutant has larger infarcts and a higher incidence of induced VT (Maass et al., 2009). Similarly, increased gap junctional coupling by adenoviral transfection of the less pH-sensitive Cx32 increases infarct size in mice with a coronary occlusion (Prestia et al., 2011). Replacement of Cx43 with Cx32 has more complex effects (Rodriguez-Sinovas et al., 2010). Under normal conditions, ATP levels were decreased and lactate levels were increased in the myocardium of these Cx43KI32 mice. Although infarct size following ischemia/reperfusion was smaller, protection by preconditioning was lost, indicating that Cx32 cannot replace Cx43 in its role in mitochondrial metabolism and preconditioning.
Cx43 mutations
Several models of mutations in Cx genes have been developed that correspond to inherited diseases in humans, as reviewed in (Dobrowolski and Willecke, 2009) and (Delmar and Makita, 2012). The G60S missense mutation in Cx43 acts in a dominant negative way to cause oculodentodigital dysplasia, including various cardiac manifestations (patent foramen ovale, reduced cardiac function, a large decrease in Cx43 due to impaired trafficking to the intercalated disc, a small decrease in ventricular conduction velocity and a variety of ECG abnormalities, both brady- and tachyarrhythmias) (Flenniken et al., 2005; Kalcheva et al., 2007; Manias et al., 2008; Tuomi et al., 2011). The G138R (Dobrowolski et al., 2008) and I130T (Kalcheva et al., 2007) mutants show a similar phenotype of oculodentodigital dysplasia, including similar alterations in cardiac structure and function. However, in the case of G138R, Cx43 trafficking seems to be normal, but Cx43 (hemichannel) function is reduced due to a loss of phosphorylation. The importance of Cx43 phosphorylation is also underscored by a study on mice with “phosphatase resistant” Cx43, in which serine residues 325, 328, and 330 are replaced by either phosphomimetic glutamine (S3E) or non-phosphorylatable alanine (S3A) (Remo et al., 2011). S3E mice were resistant to gap junctional remodeling in response to transverse aortic constriction and showed a lower inducibility of VT than wildtype mice. Conversely, in S3A mice Cx43 was lost from the intercalated disc in response to transverse aortic constriction and inducibility of VT was higher than in wildtype mice.
Interactions with other proteins
Cx43 interacts with a number of other proteins. Whereas the organizations of adherens junctions is not disrupted in the absence of Cx43 (Gutstein et al., 2003), conversely a loss of E-cadherin, N-cadherin, desmin or desmoplakin does greatly decrease Cx43 in intercalated discs (Ferreira-Cornwell et al., 2002; Gard et al., 2005; Kostetskii et al., 2005; Li et al., 2005; Gomes et al., 2012). Among the many changes in gene expression (directly or indirectly) caused by the absence of Cx43 (Iacobas et al., 2005), potassium current also show regional alterations in Cx43−/− mice, leading to proarrhythmic shortening of the action potential duration (Danik et al., 2008), whereas sodium channel function may (Desplantez et al., 2012; Jansen et al., 2012a) or may not (Johnson et al., 1999) be affected. Short term (6 h) ventricular pacing causes a decrease in Cx43 gene expression (Kontogeorgis et al., 2008a), while the shift in potassium channel expression in response to pacing was altered in Cx43+/− mice (Kontogeorgis et al., 2008b).
Interestingly, inducible deletion of Cx43 leads to increased fibrosis during aging and pressure overload because of enhanced fibroblast activity, with a concomitant increase in conduction heterogeneity and vulnerability to VT (Jansen et al., 2012b). On the other hand, TGFβ—dependent profibrotic signaling in response to myocardial infarction is blunted in Cx43+/− mice compared to Cx43+/+ mice, leading to a decrease in post-infarct fibrosis (Zhang et al., 2010b), probably because of the difference in Cx43 expression in fibroblasts (Zhang et al., 2010a). With respect to arrhythmogenesis, these and some other studies highlight the clinically relevant conjunction of changes in excitability, electrical coupling and structural remodeling (van Veen et al., 2005a; Stein et al., 2009) that is poorly captured by monogenic alterations in transgenic mouse models.
Connexin 45
Properties and expression
Cx45 forms channels with small conductance of 30 pS that are the most sensitive to transjunctional voltage of all cardiac Cxs (V1/2 = 13 mV, Gj, min = 0.12) (Moreno et al., 1995). Cx45 is the connexin expressed earliest in the developing heart, and the only one present before embryonic day 9. Cx45-deficient mice develop conduction block and a cushion defect caused by impairment of the epithelial-mesenchymal transformation of the cardiac endothelium (Kumai et al., 2000). Mice with cardiac myocyte-specific deletion of Cx45 do not have the cushion defect, but still develop conduction block and also die at around embryonic day 10 from pump failure (Nishii et al., 2003). The function of Cx45 in early cardiac development cannot be replaced by the neuronal connexin Cx36 (Frank et al., 2010).
Pacemaker and conduction system
During later embryonic development, Cx45 becomes increasingly localized to pacemaker and conduction system Alcolea et al., 1999; Coppen et al., 1999. In adult mice, Cx45 is the main connexin in the central SA node, a region apposed by protrusions of Cx40 and 43 positive atrial cells (Verheijck et al., 2001). Nevertheless, the heart rate is unaffected in mice with a heart-specific inducible Cx45 deletion (Frank et al., 2012). Furthermore, Cx45 is expressed along the entire AV conduction system, including the AV node, His bundle, proximal bundle branches and Purkinje system (Coppen et al., 1999; van Veen et al., 2005b). In adult mice, the dependence of AV conduction on the 3 Cxs expressed in the AV node region is complex. As noted above, mice deficient in Cx30.2 and 40 show accelerated and decelerated AV conduction, respectively (Schrickel et al., 2009). Apparently, Cx45 is sufficient for AV conduction, because mice deficient in both Cx30.2 and 40 show normal AV conduction (Schrickel et al., 2009). In mice with a heart-specific, inducible deficiency in Cx45, AV nodal conduction is slower than normal (Frank et al., 2012), whereas atrial and ventricular conduction was not affected (Bao et al., 2011). Interestingly, these mice also displayed a posttranslational reduction of Cx30.2 expression in the conduction system. Combining the inducible deficiency in Cx45 with a deficiency in Cx30.2 further slowed AV nodal conduction (Frank et al., 2012). Although a heterozygous deletion of Cx45 does not prolong the PR interval by itself, it does further increase the observed PR prolongation in Cx40-deficient mice (Kruger et al., 2006).
Working myocardium
Cx45 was initially thought to be widely expressed in the mammalian working myocardium (Davis et al., 1994; Verheule et al., 1997). Coppen et al later showed that this observation was mainly caused by cross-reactivity of a Cx45 antibody with Cx43 (Coppen et al., 1998). Low levels of Cx45 are expressed in the mouse ventricular working myocardium, amounting to 0.3% of total gap junction protein (Bao et al., 2011). Cx45 can form both heterotypic (Elenes et al., 2001) and heteromeric (Desplantez et al., 2004) channels with Cx43. However, co-expression of Cx45 with Cx43 appears to decrease the size of gap junctions (Grikscheit et al., 2008). This phenomenon could be more important under conditions with a higher Cx45/Cx43 ratio, for example in the ventricular epicardium, where Cx43 levels are relatively low (Yamada et al., 2004), or during heart failure, where the expression of Cx45 increases and Cx43 decreases (Yamada et al., 2003). Indeed, mice overexpressing Cx45 in the heart showed a reduction in gap junctional coupling and an increased inducibility of VT (Betsuyaku et al., 2006).
Connexin 46
Along with Cx50, Cx46 is the main connexin expressed in the lens, forming channels with a γj = 140 pS in CsCl, V1/2 = 48 mV, Gj, min = 0.11 (Hopperstad et al., 2000). mRNA for Cx46 (and Cx50) has been detected in the adult canine heart (Davis et al., 1994). The localization of Cx46 (and Cx50) protein in the dog heart is unknown, although one study detected minimal Cx46 immunoreactivity between some atrial and ventricular myocytes (Davis et al., 1995). However, in neonatal mice Cx46-positive myocytes were detected in the cardiac conduction system (or more precisely in the atrium, AV canal, intraventricular septum and ventricular subendocardium) (Chi et al., 2010). Cx46-deficient mice displayed a slightly lower heart rate, a prolonged QRS and QT duration and a QRS morphology consistent with bundle branch block (Chi et al., 2010). Cx46 has a propensity to form functional hemichannels (Trexler et al., 1996; Pfahnl and Dahl, 1999), but their role in the heart is unknown.
Conclusions
The diversity of connexins in the heart allows fine-tuning of electrical coupling depending on the region and on conditions. As therapeutic strategies, both increasing and decreasing gap junctional coupling could in theory be beneficial under certain circumstances. However, a non-specific treatment targeting gap junctions may have beneficial effects in one part of the heart but cause deleterious side effects in another. Several compounds have been developed that can modulate gap junctions (Herve and Dhein, 2010; De Vuyst et al., 2011). Some of these have been successfully tested in animal models. For example, in canine model of heart failure, enhancing gap junctional coupling with rotigaptide can reduce the vulnerability to atrial fibrillation (Guerra et al., 2006). For more selective pharmacological manipulation of gap junction coupling, it is desirable for a treatment to be (1) specific to the heart and/or (2) specific for a particular connexin. In this respect, gap junction blocking “peptidomimetics,” a class of small peptide molecules that have some Cx selectivity, are especially promising (Evans et al., 2012). An enormous amount of knowledge on cardiac connexins has been gathered from genetically engineered mouse models, as described above. There are some important differences in cardiac electrophysiology in general and connexin distribution in particular between murine and human hearts (Kaese and Verheule, 2012). Nevertheless, for the development of connexin-specific treatment strategies, knowledge derived from transgenic mouse models provides a wealth of valuable insights.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Sven Kaese received a scholarship from the Peter-Osypka-Foundation. Also supported by the European Union (FP7 Collaborative project EUTRAF, 261057) to Sander Verheule.
References
- Aanhaanen W. T., Boukens B. J., Sizarov A., Wakker V., De Gier-De Vries C., Van Ginneken A. C., et al. (2011). Defective Tbx2-dependent patterning of the atrioventricular canal myocardium causes accessory pathway formation in mice. J. Clin. Invest. 121, 534–544 10.1172/JCI44350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agullo-Pascual E., Delmar M. (2012). The noncanonical functions of Cx43 in the heart. J. Membr. Biol. 245, 477–482 10.1007/s00232-012-9466-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcoléa S., Jarry-Guichard T., De Bakker J., Gonzalez D., Lamers W., Coppen S., et al. (2004). Replacement of connexin40 by connexin45 in the mouse: impact on cardiac electrical conduction. Circ. Res. 94, 100–109 10.1161/01.RES.0000108261.67979.2A [DOI] [PubMed] [Google Scholar]
- Alcolea S., Theveniau-Ruissy M., Jarry-Guichard T., Marics I., Tzouanacou E., Chauvin J. P., et al. (1999). Downregulation of connexin 45 gene products during mouse heart development. Circ. Res. 84, 1365–1379 10.1161/01.RES.84.12.1365 [DOI] [PubMed] [Google Scholar]
- Arnolds D. E., Liu F., Fahrenbach J. P., Kim G. H., Schillinger K. J., Smemo S., et al. (2012). TBX5 drives Scn5a expression to regulate cardiac conduction system function. J. Clin. Invest. 122, 2509–2518 10.1172/JCI62617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagwe S., Berenfeld O., Vaidya D., Morley G. E., Jalife J. (2005). Altered right atrial excitation and propagation in connexin40 knockout mice. Circulation 112, 2245–2253 10.1161/CIRCULATIONAHA.104.527325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker M. L., Boukens B. J., Mommersteeg M. T., Brons J. F., Wakker V., Moorman A. F., et al. (2008). Transcription factor Tbx3 is required for the specification of the atrioventricular conduction system. Circ. Res. 102, 1340–1349 10.1161/CIRCRESAHA.107.169565 [DOI] [PubMed] [Google Scholar]
- Bao M., Kanter E. M., Huang R. Y., Maxeiner S., Frank M., Zhang Y., et al. (2011). Residual Cx45 and its relationship to Cx43 in murine ventricular myocardium. Channels (Austin) 5, 489–499 10.4161/chan.5.6.18523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee M. A., Laing J. G., Beyer E. C., Saffitz J. E. (1998). Rapid turnover of connexin43 in the adult rat heart. Circ. Res. 83, 629–635 10.1161/01.RES.83.6.629 [DOI] [PubMed] [Google Scholar]
- Beauchamp P., Choby C., Desplantez T., De Peyer K., Green K., Yamada K. A., et al. (2004). Electrical propagation in synthetic ventricular myocyte strands from germline connexin43 knockout mice. Circ. Res. 95, 170–178 10.1161/01.RES.0000134923.05174.2f [DOI] [PubMed] [Google Scholar]
- Beauchamp P., Yamada K. A., Baertschi A. J., Green K., Kanter E. M., Saffitz J. E., et al. (2006). Relative contributions of connexins 40 and 43 to atrial impulse propagation in synthetic strands of neonatal and fetal murine cardiomyocytes. Circ. Res. 99, 1216–1224 10.1161/01.RES.0000250607.34498.b4 [DOI] [PubMed] [Google Scholar]
- Belluardo N., White T. W., Srinivas M., Trovato-Salinaro A., Ripps H., Mudo G., et al. (2001). Identification and functional expression of HCx31.9, a novel gap junction gene. Cell Commun. Adhes. 8, 173–178 10.3109/15419060109080719 [DOI] [PubMed] [Google Scholar]
- Betsuyaku T., Kanno S., Lerner D. L., Schuessler R. B., Saffitz J. E., Yamada K. A. (2004). Spontaneous and inducible ventricular arrhythmias after myocardial infarction in mice. Cardiovasc. Pathol. 13, 156–164 10.1016/S1054-8807(03)00152-2 [DOI] [PubMed] [Google Scholar]
- Betsuyaku T., Kovacs A., Saffitz J. E., Yamada K. A. (2002). Cardiac structure and function in young and senescent mice heterozygous for a connexin43 null mutation. J. Mol. Cell. Cardiol. 34, 175–184 10.1006/jmcc.2001.1499 [DOI] [PubMed] [Google Scholar]
- Betsuyaku T., Nnebe N. S., Sundset R., Patibandla S., Krueger C. M., Yamada K. A. (2006). Overexpression of cardiac connexin45 increases susceptibility to ventricular tachyarrhythmias in vivo. Am. J. Physiol. Heart Circ. Physiol. 290, H163–H171 10.1152/ajpheart.01308.2004 [DOI] [PubMed] [Google Scholar]
- Bevilacqua L. M., Simon A. M., Maguire C. T., Gehrmann J., Wakimoto H., Paul D. L., et al. (2000). A targeted disruption in connexin40 leads to distinct atrioventricular conduction defects. J. Interv. Card. Electrophysiol. 4, 459–467 10.1023/A:1009800328836 [DOI] [PubMed] [Google Scholar]
- Boengler K., Dodoni G., Rodriguez-Sinovas A., Cabestrero A., Ruiz-Meana M., Gres P., et al. (2005). Connexin 43 in cardiomyocyte mitochondria and its increase by ischemic preconditioning. Cardiovasc. Res. 67, 234–244 10.1016/j.cardiores.2005.04.014 [DOI] [PubMed] [Google Scholar]
- Boengler K., Ruiz-Meana M., Gent S., Ungefug E., Soetkamp D., Miro-Casas E., et al. (2012). Mitochondrial connexin 43 impacts on respiratory complex I activity and mitochondrial oxygen consumption. J. Cell. Mol. Med. 16, 1649–1655 10.1111/j.1582-4934.2011.01516.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boengler K., Stahlhofen S., Van De Sand A., Gres P., Ruiz-Meana M., Garcia-Dorado D., et al. (2009). Presence of connexin 43 in subsarcolemmal, but not in interfibrillar cardiomyocyte mitochondria. Basic Res. Cardiol. 104, 141–147 10.1007/s00395-009-0007-5 [DOI] [PubMed] [Google Scholar]
- Bukauskas F. F., Kreuzberg M. M., Rackauskas M., Bukauskiene A., Bennett M. V., Verselis V. K., et al. (2006). Properties of mouse connexin 30.2 and human connexin 31.9 hemichannels: implications for atrioventricular conduction in the heart. Proc. Natl. Acad. Sci. U.S.A. 103, 9726–9731 10.1073/pnas.0603372103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler N. J., Greener I. D., Tellez J. O., Inada S., Musa H., Molenaar P., et al. (2009). Molecular architecture of the human sinus node: insights into the function of the cardiac pacemaker. Circulation 119, 1562–1575 10.1161/CIRCULATIONAHA.108.804369 [DOI] [PubMed] [Google Scholar]
- Chi N. C., Bussen M., Brand-Arzamendi K., Ding C., Olgin J. E., Shaw R. M., et al. (2010). Cardiac conduction is required to preserve cardiac chamber morphology. Proc. Natl. Acad. Sci. U.S.A. 107, 14662–14667 10.1073/pnas.0909432107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christoffels V. M., Hoogaars W. M., Tessari A., Clout D. E., Moorman A. F., Campione M. (2004). T-box transcription factor Tbx2 represses differentiation and formation of the cardiac chambers. Dev. Dyn. 229, 763–770 10.1002/dvdy.10487 [DOI] [PubMed] [Google Scholar]
- Coppen S. R., Dupont E., Rothery S., Severs N. J. (1998). Connexin45 expression is preferentially associated with the ventricular conduction system in mouse and rat heart. Circ. Res. 82, 232–243 10.1161/01.RES.82.2.232 [DOI] [PubMed] [Google Scholar]
- Coppen S. R., Gourdie R. G., Severs N. J. (2001). Connexin45 is the first connexin to be expressed in the central conduction system of the mouse heart. Exp. Clin. Cardiol. 6, 17–23 [PMC free article] [PubMed] [Google Scholar]
- Coppen S. R., Kaba R. A., Halliday D., Dupont E., Skepper J. N., Elneil S., et al. (2003). Comparison of connexin expression patterns in the developing mouse heart and human foetal heart. Mol. Cell. Biochem. 242, 121–127 10.1023/A:1021150014764 [DOI] [PubMed] [Google Scholar]
- Coppen S. R., Severs N. J., Gourdie R. G. (1999). Connexin45 (alpha 6) expression delineates an extended conduction system in the embryonic and mature rodent heart. Dev. Genet. 24, 82–90 [DOI] [PubMed] [Google Scholar]
- Cottrell G. T., Burt J. M. (2001). Heterotypic gap junction channel formation between heteromeric and homomeric Cx40 and Cx43 connexons. Am. J. Physiol. Cell Physiol. 281, C1559–C1567 [DOI] [PubMed] [Google Scholar]
- Dahl E., Winterhager E., Traub O., Willecke K. (1995). Expression of gap junction genes, connexin40 and connexin43, during fetal mouse development. Anat. Embryol. 191, 267–278 10.1007/BF00187825 [DOI] [PubMed] [Google Scholar]
- Danik S. B., Liu F., Zhang J., Suk H. J., Morley G. E., Fishman G. I., et al. (2004). Modulation of cardiac gap junction expression and arrhythmic susceptibility. Circ. Res. 95, 1035–1041 10.1161/01.RES.0000148664.33695.2a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danik S. B., Rosner G., Lader J., Gutstein D. E., Fishman G. I., Morley G. E. (2008). Electrical remodeling contributes to complex tachyarrhythmias in connexin43-deficient mouse hearts. FASEB J. 22, 1204–1212 10.1096/fj.07-8974com [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis L. M., Kanter H. L., Beyer E. C., Saffitz J. E. (1994). Distinct gap junction protein phenotypes in cardiac tissues with disparate conduction properties. J. Am. Coll. Cardiol. 24, 1124–1132 10.1016/0735-1097(94)90879-6 [DOI] [PubMed] [Google Scholar]
- Davis L. M., Rodefeld M. E., Green K., Beyer E. C., Saffitz J. E. (1995). Gap junction protein phenotypes of the human heart and conduction system. J. Cardiovasc. Electrophysiol. 6, 813–822 10.1111/j.1540-8167.1995.tb00357.x [DOI] [PubMed] [Google Scholar]
- De Groot J. R., Coronel R. (2004). Acute ischemia-induced gap junctional uncoupling and arrhythmogenesis. Cardiovasc. Res. 62, 323–334 10.1016/j.cardiores.2004.01.033 [DOI] [PubMed] [Google Scholar]
- Delorme B., Dahl E., Jarry-Guichard T., Briand J. P., Willecke K., Gros D., et al. (1997). Expression pattern of connexin gene products at the early developmental stages of the mouse cardiovascular system. Circ. Res. 81, 423–437 10.1161/01.RES.81.3.423 [DOI] [PubMed] [Google Scholar]
- Delorme B., Dahl E., Jarry-Guichard T., Marics I., Briand J. P., Willecke K., et al. (1995). Developmental regulation of connexin 40 gene expression in mouse heart correlates with the differentiation of the conduction system. Dev. Dyn. 204, 358–371 10.1002/aja.1002040403 [DOI] [PubMed] [Google Scholar]
- Delmar M., Makita N. (2012). Cardiac connexins, mutations and arrhythmias. Curr. Opin. Cardiol. 27, 236–241 10.1097/HCO.0b013e328352220e [DOI] [PubMed] [Google Scholar]
- de Mello W. C., Motta G. E., Chapeau M. (1969). A study on the healing-over of myocardial cells of toads. Circ. Res. 24, 475–487 10.1161/01.RES.24.3.475 [DOI] [PubMed] [Google Scholar]
- Desplantez T., Halliday D., Dupont E., Weingart R. (2004). Cardiac connexins Cx43 and Cx45: formation of diverse gap junction channels with diverse electrical properties. Pflugers Arch. 448, 363–375 10.1007/s00424-004-1250-0 [DOI] [PubMed] [Google Scholar]
- Desplantez T., McCain M. L., Beauchamp P., Rigoli G., Rothen-Rutishauser B., Parker K. K., et al. (2012). Connexin43 ablation in foetal atrial myocytes decreases electrical coupling, partner connexins, and sodium current. Cardiovasc. Res. 94, 58–65 10.1093/cvr/cvs025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vuyst E., Boengler K., Antoons G., Sipido K. R., Schulz R., Leybaert L. (2011). Pharmacological modulation of connexin-formed channels in cardiac pathophysiology. Br. J. Pharmacol. 163, 469–483 10.1111/j.1476-5381.2011.01244.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit C., Roos F., Bolz S. S., Pohl U. (2003). Lack of vascular connexin 40 is associated with hypertension and irregular arteriolar vasomotion. Physiol. Genomics 13, 169–177 [DOI] [PubMed] [Google Scholar]
- Dhein S. (2006). Cardiac ischemia and uncoupling: gap junctions in ischemia and infarction. Adv. Cardiol. 42, 198–212 10.1159/000092570 [DOI] [PubMed] [Google Scholar]
- Dhein S. (2010). Cx30 in the sinus node of murine heart: just one connexin more, or more. Evidence for a construction principle? Cardiovasc. Res. 85, 7–8 10.1093/cvr/cvp351 [DOI] [PubMed] [Google Scholar]
- Dobrowolski R., Sasse P., Schrickel J. W., Watkins M., Kim J. S., Rackauskas M., et al. (2008). The conditional connexin43G138R mouse mutant represents a new model of hereditary oculodentodigital dysplasia in humans. Hum. Mol. Genet. 17, 539–554 10.1093/hmg/ddm329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobrowolski R., Willecke K. (2009). Connexin-caused genetic diseases and corresponding mouse models. Antioxid. Redox Signal. 11, 283–295 10.1089/ars.2008.2128 [DOI] [PubMed] [Google Scholar]
- Duffy H. S. (2012). The molecular mechanisms of gap junction remodeling. Heart Rhythm 9, 1331–1334 10.1016/j.hrthm.2011.11.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy H. S., Ashton A. W., O'donnell P., Coombs W., Taffet S. M., Delmar M., et al. (2004). Regulation of connexin43 protein complexes by intracellular acidification. Circ. Res. 94, 215–222 10.1161/01.RES.0000113924.06926.11 [DOI] [PubMed] [Google Scholar]
- Dupont E., Matsushita T., Kaba R. A., Vozzi C., Coppen S. R., Khan N., et al. (2001). Altered connexin expression in human congestive heart failure. J. Mol. Cell. Cardiol. 33, 359–371 10.1006/jmcc.2000.1308 [DOI] [PubMed] [Google Scholar]
- Durrer D., Van Dam R. T., Freud G. E., Janse M. J., Meijler F. L., Arzbaecher R. C. (1970). Total excitation of the isolated human heart. Circulation 41, 899–912 10.1161/01.CIR.41.6.899 [DOI] [PubMed] [Google Scholar]
- Eckardt D., Kirchhoff S., Kim J. S., Degen J., Theis M., Ott T., et al. (2006). Cardiomyocyte-restricted deletion of connexin43 during mouse development. J. Mol. Cell. Cardiol. 41, 963–971 10.1016/j.yjmcc.2006.07.017 [DOI] [PubMed] [Google Scholar]
- Eckardt D., Theis M., Degen J., Ott T., van Rijen H. V., Kirchhoff S., et al. (2004). Functional role of connexin43 gap junction channels in adult mouse heart assessed by inducible gene deletion. J. Mol. Cell. Cardiol. 36, 101–110 10.1016/j.yjmcc.2003.10.006 [DOI] [PubMed] [Google Scholar]
- Elenes S., Martinez A. D., Delmar M., Beyer E. C., Moreno A. P. (2001). Heterotypic docking of Cx43 and Cx45 connexons blocks fast voltage gating of Cx43. Biophys. J. 81, 1406–1418 10.1016/S0006-3495(01)75796-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elenes S., Rubart M., Moreno A. P. (1999). Junctional communication between isolated pairs of canine atrial cells is mediated by homogeneous and heterogeneous gap junction channels. J. Cardiovasc. Electrophysiol. 10, 990–1004 10.1111/j.1540-8167.1999.tb01270.x [DOI] [PubMed] [Google Scholar]
- Elfgang C., Eckert R., Lichtenberg-Frate H., Butterweck A., Traub O., Klein R. A., et al. (1995). Specific permeability and selective formation of gap junction channels in connexin-transfected HeLa cells. J. Cell Biol. 129, 805–817 10.1083/jcb.129.3.805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eloff B. C., Lerner D. L., Yamada K. A., Schuessler R. B., Saffitz J. E., Rosenbaum D. S. (2001). High resolution optical mapping reveals conduction slowing in connexin43 deficient mice. Cardiovasc. Res. 51, 681–690 10.1016/S0008-6363(01)00341-8 [DOI] [PubMed] [Google Scholar]
- Evans W. H., Bultynck G., Leybaert L. (2012). Manipulating connexin communication channels: use of peptidomimetics and the translational outputs. J. Membr. Biol. 245, 437–449 10.1007/s00232-012-9488-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewart J. L., Cohen M. F., Meyer R. A., Huang G. Y., Wessels A., Gourdie R. G., et al. (1997). Heart and neural tube defects in transgenic mice overexpressing the Cx43 gap junction gene. Development 124, 1281–1292 [DOI] [PubMed] [Google Scholar]
- Ferreira-Cornwell M. C., Luo Y., Narula N., Lenox J. M., Lieberman M., Radice G. L. (2002). Remodeling the intercalated disc leads to cardiomyopathy in mice misexpressing cadherins in the heart. J. Cell. Sci. 115, 1623–1634 [DOI] [PubMed] [Google Scholar]
- Flenniken A. M., Osborne L. R., Anderson N., Ciliberti N., Fleming C., Gittens J. E., et al. (2005). A Gja1 missense mutation in a mouse model of oculodentodigital dysplasia. Development 132, 4375–4386 10.1242/dev.02011 [DOI] [PubMed] [Google Scholar]
- Francis R. J., Lo C. W. (2006). Primordial germ cell deficiency in the connexin 43 knockout mouse arises from apoptosis associated with abnormal p53 activation. Development 133, 3451–3460 10.1242/dev.02506 [DOI] [PubMed] [Google Scholar]
- Frank M., Eiberger B., Janssen-Bienhold U., De Sevilla Muller L. P., Tjarks A., Kim J. S., et al. (2010). Neuronal connexin-36 can functionally replace connexin-45 in mouse retina but not in the developing heart. J. Cell Sci. 123, 3605–3615 10.1242/jcs.068668 [DOI] [PubMed] [Google Scholar]
- Frank M., Wirth A., Andrie R. P., Kreuzberg M. M., Dobrowolski R., Seifert G., et al. (2012). Connexin45 provides optimal atrioventricular nodal conduction in the adult mouse heart. Circ. Res. 111, 1528–1538 10.1161/CIRCRESAHA.112.270561 [DOI] [PubMed] [Google Scholar]
- Gard J. J., Yamada K., Green K. G., Eloff B. C., Rosenbaum D. S., Wang X., et al. (2005). Remodeling of gap junctions and slow conduction in a mouse model of desmin-related cardiomyopathy. Cardiovasc. Res. 67, 539–547 10.1016/j.cardiores.2005.04.004 [DOI] [PubMed] [Google Scholar]
- Gemel J., Lin X., Collins R., Veenstra R. D., Beyer E. C. (2008). Cx30.2 can form heteromeric gap junction channels with other cardiac connexins. Biochem. Biophys. Res. Commun. 369, 388–394 10.1016/j.bbrc.2008.02.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glukhov A. V., Fedorov V. V., Anderson M. E., Mohler P. J., Efimov I. R. (2010). Functional anatomy of the murine sinus node: high-resolution optical mapping of ankyrin-B heterozygous mice. Am. J. Physiol. Heart Circ. Physiol. 299, H482–H491 10.1152/ajpheart.00756.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes J., Finlay M., Ahmed A. K., Ciaccio E. J., Asimaki A., Saffitz J. E., et al. (2012). Electrophysiological abnormalities precede overt structural changes in arrhythmogenic right ventricular cardiomyopathy due to mutations in desmoplakin-A combined murine and human study. Eur. Heart J. 33, 1942–1953 10.1093/eurheartj/ehr472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez D., Gomez-Hernandez J. M., Barrio L. C. (2007). Molecular basis of voltage dependence of connexin channels: an integrative appraisal. Prog. Biophys. Mol. Biol. 94, 66–106 10.1016/j.pbiomolbio.2007.03.007 [DOI] [PubMed] [Google Scholar]
- Gourdie R. G., Green C. R., Severs N. J. (1991). Gap junction distribution in adult mammalian myocardium revealed by an anti-peptide antibody and laser scanning confocal microscopy. J. Cell Sci. 99, 41–55 [DOI] [PubMed] [Google Scholar]
- Greener I. D., Monfredi O., Inada S., Chandler N. J., Tellez J. O., Atkinson A., et al. (2011). Molecular architecture of the human specialised atrioventricular conduction axis. J. Mol. Cell. Cardiol. 50, 642–651 10.1016/j.yjmcc.2010.12.017 [DOI] [PubMed] [Google Scholar]
- Grikscheit K., Thomas N., Bruce A. F., Rothery S., Chan J., Severs N. J., et al. (2008). Coexpression of connexin 45 with connexin 43 decreases gap junction size. Cell Commun. Adhes. 15, 185–193 10.1080/15419060802013943 [DOI] [PubMed] [Google Scholar]
- Gros D., Theveniau-Ruissy M., Bernard M., Calmels T., Kober F., Sohl G., et al. (2010). Connexin 30 is expressed in the mouse sino-atrial node and modulates heart rate. Cardiovasc. Res. 85, 45–55 10.1093/cvr/cvp280 [DOI] [PubMed] [Google Scholar]
- Gros D. B., Jongsma H. J. (1996). Connexins in mammalian heart function. Bioessays 18, 719–730 10.1002/bies.950180907 [DOI] [PubMed] [Google Scholar]
- Gu H., Smith F. C., Taffet S. M., Delmar M. (2003). High incidence of cardiac malformations in connexin40-deficient mice. Circ. Res. 93, 201–206 10.1161/01.RES.0000084852.65396.70 [DOI] [PubMed] [Google Scholar]
- Guerra J. M., Everett T. H. T., Lee K. W., Wilson E., Olgin J. E. (2006). Effects of the gap junction modifier rotigaptide (ZP123) on atrial conduction and vulnerability to atrial fibrillation. Circulation 114, 110–118 10.1161/CIRCULATIONAHA.105.606251 [DOI] [PubMed] [Google Scholar]
- Guerrero P. A., Schuessler R. B., Davis L. M., Beyer E. C., Johnson C. M., Yamada K. A., et al. (1997). Slow ventricular conduction in mice heterozygous for a connexin43 null mutation. J. Clin. Invest. 99, 1991–1998 10.1172/JCI119367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutstein D. E., Danik S. B., Lewitton S., France D., Liu F., Chen F. L., et al. (2005). Focal gap junction uncoupling and spontaneous ventricular ectopy. Am. J. Physiol. Heart Circ. Physiol. 289, H1091–H1098 10.1152/ajpheart.00095.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutstein D. E., Liu F. Y., Meyers M. B., Choo A., Fishman G. I. (2003). The organization of adherens junctions and desmosomes at the cardiac intercalated disc is independent of gap junctions. J. Cell. Sci. 116, 875–885 10.1242/jcs.00258 [DOI] [PubMed] [Google Scholar]
- Gutstein D. E., Morley G. E., Tamaddon H., Vaidya D., Schneider M. D., Chen J., et al. (2001a). Conduction slowing and sudden arrhythmic death in mice with cardiac-restricted inactivation of connexin43. Circ. Res. 88, 333–339 10.1161/01.RES.88.3.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutstein D. E., Morley G. E., Vaidya D., Liu F., Chen F. L., Stuhlmann H., et al. (2001b). Heterogeneous expression of gap junction channels in the heart leads to conduction defects and ventricular dysfunction. Circulation 104, 1194–1199 10.1161/hc3601.093990 [DOI] [PubMed] [Google Scholar]
- Haefliger J. A., Polikar R., Schnyder G., Burdet M., Sutter E., Pexieder T., et al. (2000). Connexin37 in normal and pathological development of mouse heart and great arteries. Dev. Dyn. 218, 331–344 [DOI] [PubMed] [Google Scholar]
- Hagendorff A., Schumacher B., Kirchhoff S., Luderitz B., Willecke K. (1999). Conduction disturbances and increased atrial vulnerability in Connexin40-deficient mice analyzed by transesophageal stimulation. Circulation 99, 1508–1515 10.1161/01.CIR.99.11.1508 [DOI] [PubMed] [Google Scholar]
- Harris B. S., Spruill L., Edmonson A. M., Rackley M. S., Benson D. W., O'brien T. X., et al. (2006). Differentiation of cardiac Purkinje fibers requires precise spatiotemporal regulation of Nkx2-5 expression. Dev. Dyn. 235, 38–49 10.1002/dvdy.20580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He D. S., Jiang J. X., Taffet S. M., Burt J. M. (1999). Formation of heteromeric gap junction channels by connexins 40 and 43 in vascular smooth muscle cells. Proc. Natl. Acad. Sci. U.S.A. 96, 6495–6500 10.1073/pnas.96.11.6495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herve J. C., Bourmeyster N., Sarrouilhe D., Duffy H. S. (2007). Gap junctional complexes: from partners to functions. Prog. Biophys. Mol. Biol. 94, 29–65 10.1016/j.pbiomolbio.2007.03.010 [DOI] [PubMed] [Google Scholar]
- Herve J. C., Dhein S. (2010). Peptides targeting gap junctional structures. Curr. Pharm. Des. 16, 3056–3070 10.2174/138161210793292528 [DOI] [PubMed] [Google Scholar]
- Hoogaars W. M., Tessari A., Moorman A. F., De Boer P. A., Hagoort J., Soufan A. T., et al. (2004). The transcriptional repressor Tbx3 delineates the developing central conduction system of the heart. Cardiovasc. Res. 62, 489–499 10.1016/j.cardiores.2004.01.030 [DOI] [PubMed] [Google Scholar]
- Hopperstad M. G., Srinivas M., Spray D. C. (2000). Properties of gap junction channels formed by Cx46 alone and in combination with Cx50. Biophys. J. 79, 1954–1966 10.1016/S0006-3495(00)76444-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houghton F. D., Thonnissen E., Kidder G. M., Naus C. C., Willecke K., Winterhager E. (1999). Doubly mutant mice, deficient in connexin32 and -43, show normal prenatal development of organs where the two gap junction proteins are expressed in the same cells. Dev. Genet. 24, 5–12 [DOI] [PubMed] [Google Scholar]
- Huang G. Y., Wessels A., Smith B. R., Linask K. K., Ewart J. L., Lo C. W. (1998). Alteration in connexin 43 gap junction gene dosage impairs conotruncal heart development. Dev. Biol. 198, 32–44 10.1016/S0012-1606(98)80027-4 [DOI] [PubMed] [Google Scholar]
- Hucker W. J., McCain M. L., Laughner J. I., Iaizzo P. A., Efimov I. R. (2008). Connexin 43 expression delineates two discrete pathways in the human atrioventricular junction. Anat. Rec. (Hoboken) 291, 204–215 10.1002/ar.20631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobas D. A., Iacobas S., Li W. E., Zoidl G., Dermietzel R., Spray D. C. (2005). Genes controlling multiple functional pathways are transcriptionally regulated in connexin43 null mouse heart. Physiol. Genomics 20, 211–223 10.1152/physiolgenomics.00229.2003 [DOI] [PubMed] [Google Scholar]
- Jansen J. A., Noorman M., Musa H., Stein M., De Jong S., van Der Nagel R., et al. (2012a). Reduced heterogeneous expression of Cx43 results in decreased Nav1.5 expression and reduced sodium current that accounts for arrhythmia vulnerability in conditional Cx43 knockout mice. Heart Rhythm 9, 600–607 10.1016/j.hrthm.2011.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen J. A., van Veen T. A., De Jong S., van Der Nagel R., van Stuijvenberg L., Driessen H., et al. (2012b). Reduced Cx43 expression triggers increased fibrosis due to enhanced fibroblast activity. Circ. Arrhythm. Electrophysiol. 5, 380–390 10.1161/CIRCEP.111.966580 [DOI] [PubMed] [Google Scholar]
- John S. A., Kondo R., Wang S. Y., Goldhaber J. I., Weiss J. N. (1999). Connexin-43 hemichannels opened by metabolic inhibition. J. Biol. Chem. 274, 236–240 10.1074/jbc.274.1.236 [DOI] [PubMed] [Google Scholar]
- Johnson C. M., Green K. G., Kanter E. M., Bou-Abboud E., Saffitz J. E., Yamada K. A. (1999). Voltage-gated Na+ channel activity and connexin expression in Cx43-deficient cardiac myocytes. J. Cardiovasc. Electrophysiol. 10, 1390–1401 10.1111/j.1540-8167.1999.tb00195.x [DOI] [PubMed] [Google Scholar]
- Joyner R. W., van Capelle F. J. (1986). Propagation through electrically coupled cells. How a small SA node drives a large atrium. Biophys. J. 50, 1157–1164 10.1016/S0006-3495(86)83559-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyner R. W., Wang Y. G., Wilders R., Golod D. A., Wagner M. B., Kumar R., et al. (2000). A spontaneously active focus drives a model atrial sheet more easily than a model ventricular sheet. Am. J. Physiol. Heart Circ. Physiol. 279, H752–H763 [DOI] [PubMed] [Google Scholar]
- Kaese S., Verheule S. (2012). Cardiac electrophysiology in mice: a matter of size. Front. Physiol. 3:345 10.3389/fphys.2012.00345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalcheva N., Qu J., Sandeep N., Garcia L., Zhang J., Wang Z., et al. (2007). Gap junction remodeling and cardiac arrhythmogenesis in a murine model of oculodentodigital dysplasia. Proc. Natl. Acad. Sci. U.S.A. 104, 20512–20516 10.1073/pnas.0705472105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanagaratnam P., Rothery S., Patel P., Severs N. J., Peters N. S. (2002). Relative expression of immunolocalized connexins 40 and 43 correlates with human atrial conduction properties. J. Am. Coll. Cardiol. 39, 116–123 10.1016/S0735-1097(01)01710-7 [DOI] [PubMed] [Google Scholar]
- Kanno S., Kovacs A., Yamada K. A., Saffitz J. E. (2003). Connexin43 as a determinant of myocardial infarct size following coronary occlusion in mice. J. Am. Coll. Cardiol. 41, 681–686 10.1016/S0735-1097(02)02893-0 [DOI] [PubMed] [Google Scholar]
- Kapoor N., Galang G., Marban E., Cho H. C. (2011). Transcriptional suppression of connexin43 by TBX18 undermines cell-cell electrical coupling in postnatal cardiomyocytes. J. Biol. Chem. 286, 14073–14079 10.1074/jbc.M110.185298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchhoff S., Kim J. S., Hagendorff A., Thonnissen E., Kruger O., Lamers W. H., et al. (2000). Abnormal cardiac conduction and morphogenesis in connexin40 and connexin43 double-deficient mice. Circ. Res. 87, 399–405 10.1161/01.RES.87.5.399 [DOI] [PubMed] [Google Scholar]
- Kirchhoff S., Nelles E., Hagendorff A., Kruger O., Traub O., Willecke K. (1998). Reduced cardiac conduction velocity and predisposition to arrhythmias in connexin40-deficient mice. Curr. Biol. 8, 299–302 10.1016/S0960-9822(98)70114-9 [DOI] [PubMed] [Google Scholar]
- Kondo R. P., Wang S. Y., John S. A., Weiss J. N., Goldhaber J. I. (2000). Metabolic inhibition activates a non-selective current through connexin hemichannels in isolated ventricular myocytes. J. Mol. Cell. Cardiol. 32, 1859–1872 10.1006/jmcc.2000.1220 [DOI] [PubMed] [Google Scholar]
- Kontogeorgis A., Kaba R. A., Kang E., Feig J. E., Gupta P. P., Ponzio M., et al. (2008a). Short-term pacing in the mouse alters cardiac expression of connexin43. BMC Physiol. 8:8 10.1186/1472-6793-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontogeorgis A., Li X., Kang E. Y., Feig J. E., Ponzio M., Kang G., et al. (2008b). Decreased connexin43 expression in the mouse heart potentiates pacing-induced remodeling of repolarizing currents. Am. J. Physiol. Heart Circ. Physiol. 295, H1905–H1916 10.1152/ajpheart.590.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostetskii I., Li J., Xiong Y., Zhou R., Ferrari V. A., Patel V. V., et al. (2005). Induced deletion of the N-cadherin gene in the heart leads to dissolution of the intercalated disc structure. Circ. Res. 96, 346–354 10.1161/01.RES.0000156274.72390.2c [DOI] [PubMed] [Google Scholar]
- Kretz M., Eckardt D., Kruger O., Kim J. S., Maurer J., Theis M., et al. (2006). Normal embryonic development and cardiac morphogenesis in mice with Wnt1-Cre-mediated deletion of connexin43. Genesis 44, 269–276 10.1002/dvg.20204 [DOI] [PubMed] [Google Scholar]
- Kreuzberg M. M., Liebermann M., Segschneider S., Dobrowolski R., Dobrzynski H., Kaba R., et al. (2009). Human connexin31.9, unlike its orthologous protein connexin30.2 in the mouse, is not detectable in the human cardiac conduction system. J. Mol. Cell. Cardiol. 46, 553–559 10.1016/j.yjmcc.2008.12.007 [DOI] [PubMed] [Google Scholar]
- Kreuzberg M. M., Schrickel J. W., Ghanem A., Kim J. S., Degen J., Janssen-Bienhold U., et al. (2006). Connexin30.2 containing gap junction channels decelerate impulse propagation through the atrioventricular node. Proc. Natl. Acad. Sci. U.S.A. 103, 5959–5964 10.1073/pnas.0508512103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreuzberg M. M., Sohl G., Kim J. S., Verselis V. K., Willecke K., Bukauskas F. F. (2005). Functional properties of mouse connexin30.2 expressed in the conduction system of the heart. Circ. Res. 96, 1169–1177 10.1161/01.RES.0000169271.33675.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger O., Maxeiner S., Kim J. S., van Rijen H. V., De Bakker J. M., Eckardt D., et al. (2006). Cardiac morphogenetic defects and conduction abnormalities in mice homozygously deficient for connexin40 and heterozygously deficient for connexin45. J. Mol. Cell. Cardiol. 41, 787–797 10.1016/j.yjmcc.2006.07.005 [DOI] [PubMed] [Google Scholar]
- Kumai M., Nishii K., Nakamura K., Takeda N., Suzuki M., Shibata Y. (2000). Loss of connexin45 causes a cushion defect in early cardiogenesis. Development 127, 3501–3512 [DOI] [PubMed] [Google Scholar]
- Leaf D. E., Feig J. E., Vasquez C., Riva P. L., Yu C., Lader J. M., et al. (2008). Connexin40 imparts conduction heterogeneity to atrial tissue. Circ. Res. 103, 1001–1008 10.1161/CIRCRESAHA.107.168997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner D. L., Yamada K. A., Schuessler R. B., Saffitz J. E. (2000). Accelerated onset and increased incidence of ventricular arrhythmias induced by ischemia in Cx43-deficient mice. Circulation 101, 547–552 10.1161/01.CIR.101.5.547 [DOI] [PubMed] [Google Scholar]
- Li J., Patel V. V., Kostetskii I., Xiong Y., Chu A. F., Jacobson J. T., et al. (2005). Cardiac-specific loss of N-cadherin leads to alteration in connexins with conduction slowing and arrhythmogenesis. Circ. Res. 97, 474–481 10.1161/01.RES.0000181132.11393.18 [DOI] [PubMed] [Google Scholar]
- Li W. E., Waldo K., Linask K. L., Chen T., Wessels A., Parmacek M. S., et al. (2002). An essential role for connexin43 gap junctions in mouse coronary artery development. Development 129, 2031–2042 [DOI] [PubMed] [Google Scholar]
- Li X., Heinzel F. R., Boengler K., Schulz R., Heusch G. (2004). Role of connexin 43 in ischemic preconditioning does not involve intercellular communication through gap junctions. J. Mol. Cell. Cardiol. 36, 161–163 10.1016/j.yjmcc.2003.10.019 [DOI] [PubMed] [Google Scholar]
- Lin J., Keener J. P. (2010). Modeling electrical activity of myocardial cells incorporating the effects of ephaptic coupling. Proc. Natl. Acad. Sci. U.S.A. 107, 20935–20940 10.1073/pnas.1010154107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X., Gemel J., Beyer E. C., Veenstra R. D. (2005). Dynamic model for ventricular junctional conductance during the cardiac action potential. Am. J. Physiol. Heart Circ. Physiol. 288, H1113–H1123 10.1152/ajpheart.00882.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X., Gemel J., Glass A., Zemlin C. W., Beyer E. C., Veenstra R. D. (2010). Connexin40 and connexin43 determine gating properties of atrial gap junction channels. J. Mol. Cell. Cardiol. 48, 238–245 10.1016/j.yjmcc.2009.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin X., Veenstra R. D. (2004). Action potential modulation of connexin40 gap junctional conductance. Am. J. Physiol. Heart Circ. Physiol. 286, H1726–H1735 10.1152/ajpheart.00943.2003 [DOI] [PubMed] [Google Scholar]
- Liu S., Liu F., Schneider A. E., St Amand T., Epstein J. A., Gutstein D. E. (2006). Distinct cardiac malformations caused by absence of connexin 43 in the neural crest and in the non-crest neural tube. Development 133, 2063–2073 10.1242/dev.02374 [DOI] [PubMed] [Google Scholar]
- Lo C. W., Cohen M. F., Huang G. Y., Lazatin B. O., Patel N., Sullivan R., et al. (1997). Cx43 gap junction gene expression and gap junctional communication in mouse neural crest cells. Dev. Genet. 20, 119–132 [DOI] [PubMed] [Google Scholar]
- Maass K., Chase S. E., Lin X., Delmar M. (2009). Cx43 CT domain influences infarct size and susceptibility to ventricular tachyarrhythmias in acute myocardial infarction. Cardiovasc. Res. 84, 361–367 10.1093/cvr/cvp250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maass K., Ghanem A., Kim J. S., Saathoff M., Urschel S., Kirfel G., et al. (2004). Defective epidermal barrier in neonatal mice lacking the C-terminal region of connexin43. Mol. Biol. Cell 15, 4597–4608 10.1091/mbc.E04-04-0324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maass K., Shibayama J., Chase S. E., Willecke K., Delmar M. (2007). C-terminal truncation of connexin43 changes number, size, and localization of cardiac gap junction plaques. Circ. Res. 101, 1283–1291 10.1161/CIRCRESAHA.107.162818 [DOI] [PubMed] [Google Scholar]
- Manias J. L., Plante I., Gong X. Q., Shao Q., Churko J., Bai D., et al. (2008). Fate of connexin43 in cardiac tissue harbouring a disease-linked connexin43 mutant. Cardiovasc. Res. 80, 385–395 10.1093/cvr/cvn203 [DOI] [PubMed] [Google Scholar]
- Miquerol L., Dupays L., Theveniau-Ruissy M., Alcolea S., Jarry-Guichard T., Abran P., et al. (2003). Gap junctional connexins in the developing mouse cardiac conduction system. Novartis Found. Symp. 250, 80–98 discussion 98–109, 276–279. [DOI] [PubMed] [Google Scholar]
- Miquerol L., Meysen S., Mangoni M., Bois P., van Rijen H. V., Abran P., et al. (2004). Architectural and functional asymmetry of the His-Purkinje system of the murine heart. Cardiovasc. Res. 63, 77–86 10.1016/j.cardiores.2004.03.007 [DOI] [PubMed] [Google Scholar]
- Miro-Casas E., Ruiz-Meana M., Agullo E., Stahlhofen S., Rodriguez-Sinovas A., Cabestrero A., et al. (2009). Connexin43 in cardiomyocyte mitochondria contributes to mitochondrial potassium uptake. Cardiovasc. Res. 83, 747–756 10.1093/cvr/cvp157 [DOI] [PubMed] [Google Scholar]
- Moreno A. P., Laing J. G., Beyer E. C., Spray D. C. (1995). Properties of gap junction channels formed of connexin 45 endogenously expressed in human hepatoma (SKHep1) cells. Am. J. Physiol. 268, C356–C365 [DOI] [PubMed] [Google Scholar]
- Morley G. E., Danik S. B., Bernstein S., Sun Y., Rosner G., Gutstein D. E., et al. (2005). Reduced intercellular coupling leads to paradoxical propagation across the Purkinje-ventricular junction and aberrant myocardial activation. Proc. Natl. Acad. Sci. U.S.A. 102, 4126–4129 10.1073/pnas.0500881102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley G. E., Vaidya D., Jalife J. (2000). Characterization of conduction in the ventricles of normal and heterozygous Cx43 knockout mice using optical mapping. J. Cardiovasc. Electrophysiol. 11, 375–377 10.1111/j.1540-8167.2000.tb01811.x [DOI] [PubMed] [Google Scholar]
- Munger S. J., Kanady J. D., Simon A. M. (2013). Absence of venous valves in mice lacking Connexin37. Dev. Biol. 373, 338–348 10.1016/j.ydbio.2012.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munshi N. V., McAnally J., Bezprozvannaya S., Berry J. M., Richardson J. A., Hill J. A., et al. (2009). Cx30.2 enhancer analysis identifies Gata4 as a novel regulator of atrioventricular delay. Development 136, 2665–2674 10.1242/dev.038562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishii K., Kumai M., Egashira K., Miwa T., Hashizume K., Miyano Y., et al. (2003). Mice lacking connexin45 conditionally in cardiac myocytes display embryonic lethality similar to that of germline knockout mice without endocardial cushion defect. Cell Commun. Adhes. 10, 365–369 [DOI] [PubMed] [Google Scholar]
- Pfahnl A., Dahl G. (1999). Gating of cx46 gap junction hemichannels by calcium and voltage. Pflugers Arch. 437, 345–353 10.1007/s004240050788 [DOI] [PubMed] [Google Scholar]
- Pizard A., Burgon P. G., Paul D. L., Bruneau B. G., Seidman C. E., Seidman J. G. (2005). Connexin 40, a target of transcription factor Tbx5, patterns wrist, digits, and sternum. Mol. Cell. Biol. 25, 5073–5083 10.1128/MCB.25.12.5073-5083.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plum A., Hallas G., Magin T., Dombrowski F., Hagendorff A., Schumacher B., et al. (2000). Unique and shared functions of different connexins in mice. Curr. Biol. 10, 1083–1091 10.1016/S0960-9822(00)00690-4 [DOI] [PubMed] [Google Scholar]
- Prestia K. A., Sosunov E. A., Anyukhovsky E. P., Dolmatova E., Kelly C. W., Brink P. R., et al. (2011). Increased cell-cell coupling increases infarct size and does not decrease incidence of ventricular tachycardia in mice. Front. Physiol. 2:1 10.3389/fphys.2011.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rackauskas M., Neverauskas V., Skeberdis V. A. (2010). Diversity and properties of connexin gap junction channels. Medicina (Kaunas) 46, 1–12 [PubMed] [Google Scholar]
- Reaume A. G., De Sousa P. A., Kulkarni S., Langille B. L., Zhu D., Davies T. C., et al. (1995). Cardiac malformation in neonatal mice lacking connexin43. Science 267, 1831–1834 10.1126/science.7892609 [DOI] [PubMed] [Google Scholar]
- Reed K. E., Westphale E. M., Larson D. M., Wang H. Z., Veenstra R. D., Beyer E. C. (1993). Molecular cloning and functional expression of human connexin37, an endothelial cell gap junction protein. J. Clin. Invest. 91, 997–1004 10.1172/JCI116321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remo B. F., Qu J., Volpicelli F. M., Giovannone S., Shin D., Lader J., et al. (2011). Phosphatase-resistant gap junctions inhibit pathological remodeling and prevent arrhythmias. Circ. Res. 108, 1459–1466 10.1161/CIRCRESAHA.111.244046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentschler S., Harris B. S., Kuznekoff L., Jain R., Manderfield L., Lu M. M., et al. (2011). Notch signaling regulates murine atrioventricular conduction and the formation of accessory pathways. J. Clin. Invest. 121, 525–533 10.1172/JCI44470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Sinovas A., Cabestrero A., Lopez D., Torre I., Morente M., Abellan A., et al. (2007). The modulatory effects of connexin 43 on cell death/survival beyond cell coupling. Prog. Biophys. Mol. Biol. 94, 219–232 10.1016/j.pbiomolbio.2007.03.003 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Sinovas A., Sanchez J. A., Gonzalez-Loyola A., Barba I., Morente M., Aguilar R., et al. (2010). Effects of substitution of Cx43 by Cx32 on myocardial energy metabolism, tolerance to ischaemia and preconditioning protection. J. Physiol. 588, 1139–1151 10.1113/jphysiol.2009.186577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Meana M., Rodriguez-Sinovas A., Cabestrero A., Boengler K., Heusch G., Garcia-Dorado D. (2008). Mitochondrial connexin43 as a new player in the pathophysiology of myocardial ischaemia-reperfusion injury. Cardiovasc. Res. 77, 325–333 10.1093/cvr/cvm062 [DOI] [PubMed] [Google Scholar]
- Salameh A., Dhein S. (2011). Adrenergic control of cardiac gap junction function and expression. Naunyn Schmiedebergs Arch. Pharmacol. 383, 331–346 10.1007/s00210-011-0603-4 [DOI] [PubMed] [Google Scholar]
- Sankova B., Benes J. Jr., Krejci E., Dupays L., Theveniau-Ruissy M., Miquerol L., et al. (2012). The effect of connexin40 deficiency on ventricular conduction system function during development. Cardiovasc. Res. 95, 469–479 10.1093/cvr/cvs210 [DOI] [PubMed] [Google Scholar]
- Schrickel J. W., Kreuzberg M. M., Ghanem A., Kim J. S., Linhart M., Andrie R., et al. (2009). Normal impulse propagation in the atrioventricular conduction system of Cx30.2/Cx40 double deficient mice. J. Mol. Cell. Cardiol. 46, 644–652 10.1016/j.yjmcc.2009.02.012 [DOI] [PubMed] [Google Scholar]
- Schwanke U., Konietzka I., Duschin A., Li X., Schulz R., Heusch G. (2002). No ischemic preconditioning in heterozygous connexin43-deficient mice. Am. J. Physiol. Heart Circ. Physiol. 283, H1740–H1742 [DOI] [PubMed] [Google Scholar]
- Shaw R. M., Rudy Y. (1997). Ionic mechanisms of propagation in cardiac tissue. Roles of the sodium and L-type calcium currents during reduced excitability and decreased gap junction coupling. Circ. Res. 81, 727–741 10.1161/01.RES.81.5.727 [DOI] [PubMed] [Google Scholar]
- Simon A. M., Goodenough D. A., Li E., Paul D. L. (1997). Female infertility in mice lacking connexin 37. Nature 385, 525–529 10.1038/385525a0 [DOI] [PubMed] [Google Scholar]
- Simon A. M., Goodenough D. A., Paul D. L. (1998). Mice lacking connexin40 have cardiac conduction abnormalities characteristic of atrioventricular block and bundle branch block. Curr. Biol. 8, 295–298 10.1016/S0960-9822(98)70113-7 [DOI] [PubMed] [Google Scholar]
- Simon A. M., McWhorter A. R., Dones J. A., Jackson C. L., Chen H. (2004). Heart and head defects in mice lacking pairs of connexins. Dev. Biol. 265, 369–383 10.1016/j.ydbio.2003.09.036 [DOI] [PubMed] [Google Scholar]
- Sizarov A., Devalla H. D., Anderson R. H., Passier R., Christoffels V. M., Moorman A. F. (2011). Molecular analysis of patterning of conduction tissues in the developing human heart. Circ. Arrhythm. Electrophysiol. 4, 532–542 10.1161/CIRCEP.111.963421 [DOI] [PubMed] [Google Scholar]
- Smyth J. W., Vogan J. M., Buch P. J., Zhang S. S., Fong T. S., Hong T. T., et al. (2012). Actin cytoskeleton rest stops regulate anterograde traffic of connexin 43 vesicles to the plasma membrane. Circ. Res. 110, 978–989 10.1161/CIRCRESAHA.111.257964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohl G., Willecke K. (2004). Gap junctions and the connexin protein family. Cardiovasc. Res. 62, 228–232 10.1016/j.cardiores.2003.11.013 [DOI] [PubMed] [Google Scholar]
- Solan J. L., Lampe P. D. (2009). Connexin43 phosphorylation: structural changes and biological effects. Biochem. J. 419, 261–272 10.1042/BJ20082319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperelakis N. (2002). An electric field mechanism for transmission of excitation between myocardial cells. Circ. Res. 91, 985–987 10.1161/01.RES.0000045656.34731.6D [DOI] [PubMed] [Google Scholar]
- Stein M., van Veen T. A., Remme C. A., Boulaksil M., Noorman M., van Stuijvenberg L., et al. (2009). Combined reduction of intercellular coupling and membrane excitability differentially affects transverse and longitudinal cardiac conduction. Cardiovasc. Res. 83, 52–60 10.1093/cvr/cvp124 [DOI] [PubMed] [Google Scholar]
- Tallini Y. N., Brekke J. F., Shui B., Doran R., Hwang S. M., Nakai J., et al. (2007). Propagated endothelial Ca2+ waves and arteriolar dilation in vivo: measurements in Cx40BAC GCaMP2 transgenic mice. Circ. Res. 101, 1300–1309 10.1161/CIRCRESAHA.107.149484 [DOI] [PubMed] [Google Scholar]
- Tamaddon H. S., Vaidya D., Simon A. M., Paul D. L., Jalife J., Morley G. E. (2000). High-resolution optical mapping of the right bundle branch in connexin40 knockout mice reveals slow conduction in the specialized conduction system. Circ. Res. 87, 929–936 10.1161/01.RES.87.10.929 [DOI] [PubMed] [Google Scholar]
- Thomas S. A., Schuessler R. B., Berul C. I., Beardslee M. A., Beyer E. C., Mendelsohn M. E., et al. (1998). Disparate effects of deficient expression of connexin43 on atrial and ventricular conduction: evidence for chamber-specific molecular determinants of conduction. Circulation 97, 686–691 10.1161/01.CIR.97.7.686 [DOI] [PubMed] [Google Scholar]
- Thomas S. P., Kucera J. P., Bircher-Lehmann L., Rudy Y., Saffitz J. E., Kleber A. G. (2003). Impulse propagation in synthetic strands of neonatal cardiac myocytes with genetically reduced levels of connexin43. Circ. Res. 92, 1209–1216 10.1161/01.RES.0000074916.41221.EA [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traub O., Eckert R., Lichtenberg-Frate H., Elfgang C., Bastide B., Scheidtmann K. H., et al. (1994). Immunochemical and electrophysiological characterization of murine connexin40 and -43 in mouse tissues and transfected human cells. Eur. J. Cell Biol. 64, 101–112 [PubMed] [Google Scholar]
- Trexler E. B., Bennett M. V., Bargiello T. A., Verselis V. K. (1996). Voltage gating and permeation in a gap junction hemichannel. Proc. Natl. Acad. Sci. U.S.A. 93, 5836–5841 10.1073/pnas.93.12.5836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuomi J. M., Tyml K., Jones D. L. (2011). Atrial tachycardia/fibrillation in the connexin 43 G60S mutant (Oculodentodigital dysplasia) mouse. Am. J. Physiol. Heart Circ. Physiol. 300, H1402–H1411 10.1152/ajpheart.01094.2010 [DOI] [PubMed] [Google Scholar]
- Vaidya D., Tamaddon H. S., Lo C. W., Taffet S. M., Delmar M., Morley G. E., et al. (2001). Null mutation of connexin43 causes slow propagation of ventricular activation in the late stages of mouse embryonic development. Circ. Res. 88, 1196–1202 10.1161/hh1101.091107 [DOI] [PubMed] [Google Scholar]
- Valiunas V., Manthey D., Vogel R., Willecke K., Weingart R. (1999). Biophysical properties of mouse connexin30 gap junction channels studied in transfected human HeLa cells. J. Physiol. 3, 631–644 10.1111/j.1469-7793.1999.0631n.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valiunas V., Weingart R., Brink P. R. (2000). Formation of heterotypic gap junction channels by connexins 40 and 43. Circ. Res. 86, E42–E49 10.1161/01.RES.86.2.e42 [DOI] [PubMed] [Google Scholar]
- Vanderbrink B. A., Sellitto C., Saba S., Link M. S., Zhu W., Homoud M. K., et al. (2000). Connexin40-deficient mice exhibit atrioventricular nodal and infra-Hisian conduction abnormalities. J. Cardiovasc. Electrophysiol. 11, 1270–1276 10.1046/j.1540-8167.2000.01270.x [DOI] [PubMed] [Google Scholar]
- van Kempen M. J., Ten Velde I., Wessels A., Oosthoek P. W., Gros D., Jongsma H. J., et al. (1995). Differential connexin distribution accommodates cardiac function in different species. Microsc. Res. Tech. 31, 420–436 10.1002/jemt.1070310511 [DOI] [PubMed] [Google Scholar]
- van Rijen H. V., Eckardt D., Degen J., Theis M., Ott T., Willecke K., et al. (2004). Slow conduction and enhanced anisotropy increase the propensity for ventricular tachyarrhythmias in adult mice with induced deletion of connexin43. Circulation 109, 1048–1055 10.1161/01.CIR.0000117402.70689.75 [DOI] [PubMed] [Google Scholar]
- van Rijen H. V., van Veen T. A., Van Kempen M. J., Wilms-Schopman F. J., Potse M., Krueger O., et al. (2001). Impaired conduction in the bundle branches of mouse hearts lacking the gap junction protein connexin40. Circulation 103, 1591–1598 10.1161/01.CIR.103.11.1591 [DOI] [PubMed] [Google Scholar]
- van Veen T. A., Stein M., Royer A., Le Quang K., Charpentier F., Colledge W. H., et al. (2005a). Impaired impulse propagation in Scn5a-knockout mice: combined contribution of excitability, connexin expression, and tissue architecture in relation to aging. Circulation 112, 1927–1935 [DOI] [PubMed] [Google Scholar]
- van Veen T. A., van Rijen H. V., Van Kempen M. J., Miquerol L., Opthof T., Gros D., et al. (2005b). Discontinuous conduction in mouse bundle branches is caused by bundle-branch architecture. Circulation 112, 2235–2244 [DOI] [PubMed] [Google Scholar]
- Verheijck E. E., van Kempen M. J., Veereschild M., Lurvink J., Jongsma H. J., Bouman L. N. (2001). Electrophysiological features of the mouse sinoatrial node in relation to connexin distribution. Cardiovasc. Res. 52, 40–50 10.1016/S0008-6363(01)00364-9 [DOI] [PubMed] [Google Scholar]
- Verheule S., van Batenburg C. A., Coenjaerts F. E., Kirchhoff S., Willecke K., Jongsma H. J. (1999). Cardiac conduction abnormalities in mice lacking the gap junction protein connexin40. J. Cardiovasc. Electrophysiol. 10, 1380–1389 10.1111/j.1540-8167.1999.tb00194.x [DOI] [PubMed] [Google Scholar]
- Verheule S., van Kempen M. J., Postma S., Rook M. B., Jongsma H. J. (2001). Gap junctions in the rabbit sinoatrial node. Am. J. Physiol. Heart Circ. Physiol. 280, H2103–H2115 [DOI] [PubMed] [Google Scholar]
- Verheule S., van Kempen M. J., Te Welscher P. H., Kwak B. R., Jongsma H. J. (1997). Characterization of gap junction channels in adult rabbit atrial and ventricular myocardium. Circ. Res. 80, 673–681 10.1161/01.RES.80.5.673 [DOI] [PubMed] [Google Scholar]
- Vink M. J., Suadicani S. O., Vieira D. M., Urban-Maldonado M., Gao Y., Fishman G. I., et al. (2004). Alterations of intercellular communication in neonatal cardiac myocytes from connexin43 null mice. Cardiovasc. Res. 62, 397–406 10.1016/j.cardiores.2004.01.015 [DOI] [PubMed] [Google Scholar]
- Vozzi C., Dupont E., Coppen S. R., Yeh H. I., Severs N. J. (1999). Chamber-related differences in connexin expression in the human heart. J. Mol. Cell. Cardiol. 31, 991–1003 10.1006/jmcc.1999.0937 [DOI] [PubMed] [Google Scholar]
- Walker D. L., Vacha S. J., Kirby M. L., Lo C. W. (2005). Connexin43 deficiency causes dysregulation of coronary vasculogenesis. Dev. Biol. 284, 479–498 10.1016/j.ydbio.2005.06.004 [DOI] [PubMed] [Google Scholar]
- Wang N., De Vuyst E., Ponsaerts R., Boengler K., Palacios-Prado N., Wauman J., et al. (2013). Selective inhibition of Cx43 hemichannels by Gap19 and its impact on myocardial ischemia/reperfusion injury. Basic Res. Cardiol. 108, 309 10.1007/s00395-012-0309-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White T. W., Bruzzone R. (1996). Multiple connexin proteins in single intercellular channels: connexin compatibility and functional consequences. J. Bioenerg. Biomembr. 28, 339–350 10.1007/BF02110110 [DOI] [PubMed] [Google Scholar]
- Wiegerinck R. F., Verkerk A. O., Belterman C. N., van Veen T. A., Baartscheer A., Opthof T., et al. (2006). Larger cell size in rabbits with heart failure increases myocardial conduction velocity and QRS duration. Circulation 113, 806–813 10.1161/CIRCULATIONAHA.105.565804 [DOI] [PubMed] [Google Scholar]
- Wiese C., Grieskamp T., Airik R., Mommersteeg M. T., Gardiwal A., De Gier-De Vries C., et al. (2009). Formation of the sinus node head and differentiation of sinus node myocardium are independently regulated by Tbx18 and Tbx3. Circ. Res. 104, 388–397 10.1161/CIRCRESAHA.108.187062 [DOI] [PubMed] [Google Scholar]
- Winterhager E., Pielensticker N., Freyer J., Ghanem A., Schrickel J. W., Kim J. S., et al. (2007). Replacement of connexin43 by connexin26 in transgenic mice leads to dysfunctional reproductive organs and slowed ventricular conduction in the heart. BMC Dev. Biol. 7:26 10.1186/1471-213X-7-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wit A. L., Peters N. S. (2012). The role of gap junctions in the arrhythmias of ischemia and infarction. Heart Rhythm 9, 308–311 10.1016/j.hrthm.2011.09.056 [DOI] [PubMed] [Google Scholar]
- Ya J., Erdtsieck-Ernste E. B., De Boer P. A., van Kempen M. J., Jongsma H., Gros D., et al. (1998). Heart defects in connexin43-deficient mice. Circ. Res. 82, 360–366 10.1161/01.RES.82.3.360 [DOI] [PubMed] [Google Scholar]
- Yamada K. A., Kanter E. M., Green K. G., Saffitz J. E. (2004). Transmural distribution of connexins in rodent hearts. J. Cardiovasc. Electrophysiol. 15, 710–715 10.1046/j.1540-8167.2004.03514.x [DOI] [PubMed] [Google Scholar]
- Yamada K. A., Rogers J. G., Sundset R., Steinberg T. H., Saffitz J. (2003). Up-regulation of connexin45 in heart failure. J. Cardiovasc. Electrophysiol. 14, 1205–1212 10.1046/j.1540-8167.2003.03276.x [DOI] [PubMed] [Google Scholar]
- Zhang Y., Kanter E. M., Yamada K. A. (2010a). Remodeling of cardiac fibroblasts following myocardial infarction results in increased gap junction intercellular communication. Cardiovasc. Pathol. 19, e233–e240 10.1016/j.carpath.2009.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Wang H., Kovacs A., Kanter E. M., Yamada K. A. (2010b). Reduced expression of Cx43 attenuates ventricular remodeling after myocardial infarction via impaired TGF-beta signaling. Am. J. Physiol. Heart Circ. Physiol. 298, H477–H487 10.1152/ajpheart.00806.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng-Fischhofer Q., Ghanem A., Kim J. S., Kibschull M., Schwarz G., Schwab J. O., et al. (2006). Connexin31 cannot functionally replace connexin43 during cardiac morphogenesis in mice. J. Cell. Sci. 119, 693–701 10.1242/jcs.02800 [DOI] [PubMed] [Google Scholar]
- Zhu W., Saba S., Link M. S., Bak E., Homoud M. K., Estes N. A., et al. (2005). Atrioventricular nodal reverse facilitation in connexin40-deficient mice. Heart Rhythm 2, 1231–1237 10.1016/j.hrthm.2005.07.022 [DOI] [PubMed] [Google Scholar]