Abstract
Objective
To understand home-care nurses‘ perceptions of the post-hospitalization information needs and communication problems of elderly patients, and how these factors might contribute to undesirable outcomes including poor patient reintegration into prior living environments and unplanned hospital readmissions.
Design
A ranked list of information needs experienced by patients was developed by two Nominal Group Technique (NGT) sessions from the perspective of home-care nurses. The list was combined with results from previously published work to develop a web-based survey administered to home care nurses‘ to elicit perceptions of patients‘ post-hospitalization information needs.
Results
Seventeen nurses participated in the NGT sessions, producing a list of 28 challenges grouped into five themes: medications, disease/condition, discharge, non-medication care, and functional limitations, and communication problems. The survey was sent to 220 home-care nurses, with a 54.1% (119/220) response rate. Respondents identified several frequent, high-impact information and communication needs that have received little attention in readmission literature, including information about medication regimens; the severity of their condition; hospital discharge management process; non-medication care regimens such as wound care, use of durable medical equipment and home safety; the extent of care needed, and which providers are best suited to provide that care. Responses also identified several communication difficulties that may play a role in readmissions.
Conclusions
Information needs and communication problems identified by home-care nurses expanded upon and reinforced results from prior studies. These results might be used to develop interventions that may improve information sharing among clinicians, patients, and caregivers during care transitions to ensure patient reintegration into prior living environments, potentially preventing unplanned hospital readmissions.
Keywords: Patient readmission, information literacy, community health nursing, geriatric nursing
INTRODUCTION
When patients move or are discharged from one care setting to another, such as from the hospital to the home, they experience care transitions[1]. Difficulties in these transitions frequently play an important role in readmissions, with up to 25% of hospital discharges resulting in the patient being readmitted within 30 days[2]. Studies have found that between 5% and 77% of these readmissions might be avoidable[3] and some can be predicted based on factors such as length of stay, acuity, comorbidity, and emergency department use[4]. Increased attention to the difficulties that arise during complicated care transitions illustrate the need for further research and process improvements[5].
Home-care nurses have a unique perspective on care transitions, working with patients immediately following discharge from hospital stays for conditions that require continued monitoring[6], and providing in-home health care nursing practice and education to approximately 10 million patients in the US annually[7]. The use of home health care has been shown to reduce use of inpatient hospital care[8], and to decrease both mortality and admission to long term institutional care[9]. Home-care nurses also support optimal health outcomes by keeping patients in their homes; increasing their ability to care for themselves; reducing their use of hospital, rehabilitation and long-term care facility resources; and reducing hospital readmissions[10–15]. As clinicians who enter the home, home-care nurses have insight into the experiences and needs of patients, which provides them with a unique and potentially useful perspective regarding patient perceptions of information needs. Despite all the research that has been completed to date on unmet information needs following transfer from hospital to home, to the best of our knowledge, none has formally evaluated home care nurses‘ perceptions of patients‘ post-hospitalization information needs.
Information transfer is a critical component of care transitions. As unmet information needs factor prominently in analyses of both Greenwald‘s factors contributing to readmission in high-risk discharges[2] and Coleman‘s model of care transitions[1], understanding these needs may be the first step in developing interventions aimed at reducing readmissions. Greenwald‘s readmission risks include lapse of communication, inadequate patient education, medication errors, lack of timely follow-up, lapse in home services, new medical problems, worsening old problems, addiction issues, language/cultural barriers, medication adherence, missed follow-up appointments, test errors, inappropriate discharge, inappropriate medications, and inadequate home services[2]. Coleman‘s model of effective care transitions includes communication of care plan, care summary, health problems, medications; communication of expectations at next site to patient; medication reconciliation; clinical follow-up information; information about medical status changes, symptoms of worsening condition, and who to contact[1]. All of these could be related to information needs, and form the basis for this study.
The conceptual model of transitions of care developed by the National Transitions of Care Coalition (NTOCC), suggests a one-way transformation of information from a sender (the hospital) to receivers, including the patient, caregivers, and home care nurses, if applicable[16]. However, this model lacks both a definition of the information that needs to be shared with different clinicians including home care nurses and a description of how that information should be shared. This study seeks to build upon the NTOCC conceptual model and these prior efforts to more precisely identify both the information that the patients, caregivers and nurses need for a safe, effective care transition to the home, and barriers that might impede the communication of that information.
Our goal is to formulate a model of information needs and communication difficulties that contribute to hospital readmissions involving elderly patients. We conducted a two-phase inquiry with the goal of understanding home-care nurses‘ perceptions of the information needs and communication problems that their elderly patients experience in the post-hospitalization period, and how those needs might be related to hospital readmissions (Figure 1). Results from this study will inform the development of informatics tools and interventions designed to support home-care nurses and patients in care transitions, potentially reducing readmissions and improving reintegration into prior living environments.
Figure 1.
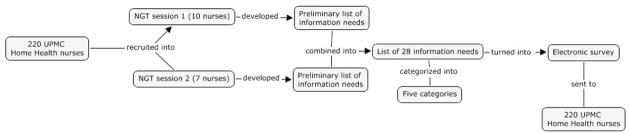
Study Methods Flowchart
RESEARCH QUESTIONS
Phase I: What unmet information needs and communication difficulties do home-care nurses perceive that their elderly patients experience in the first 30 days after they return home from the hospital?
Phase II: As perceived by home-care nurses, how frequently do their elderly patients experience the information needs and communication difficulties identified in Phase I, and when they do occur, how frequently do they result in the patient returning to the hospital?
METHODS
Study Design
We used a combination of Nominal Group Technique (NGT)[17] sessions and a web-based survey to identify and rank unmet information needs and communication difficulties that impact hospital readmissions of elderly patients during the immediate post-hospitalization period. We recruited home-care nurses due to their broad experience with large numbers of elderly patients and their ability to influence the information provided to the patients.
Study Participants and Setting
Participants for both the NGT and survey were home-care nurses, also known as visiting nurses, employed by University of Pittsburgh Medical Center (UPMC) Home Health, a division of UPMC, a large healthcare provider in southwestern Pennsylvania. They were recruited by email to participate in both the NGT sessions and the survey. All participants were registered nurses, fluent in both verbal and written English, and employed at least part time as home-care nurses by UPMC Home Health. All registered nurses employed by UPMC Home Health were invited to participate in both the NGT sessions and the survey. All participants consented to participate in writing.
Nominal Group Technique
We used the Nominal Group Technique[17], a methodology for developing a ranked list of responses to a focused question. Our question was: “In your experience, what information-related problems have your elderly patients experienced that contributed to hospital readmissions?” The NGT uses an iterative process to generate a priority-ordered list of answers. Participants are asked to identify ideas in response to the question of interest; to share their responses with the group; to develop a consensus list of candidate responses; and finally to individually choose the five most important responses (on a scale of one to five, five being most important). The responses are aggregated using the points assigned by the participants. Any information need selected by at least one participant was included in the final list of unmet information needs. Two authors (KMR and FML) combined the lists developed by the two NGT sessions to eliminate redundant entries, forming a consensus list of information needs. Two authors (KMR and HH) performed a thematic analysis using structural coding on the list of information needs without any initial categories, considering common aspects such as the subject of the information need, the timing of the information need, and the location of the information need[18]. Disagreements and confusions were iteratively discussed until consensus occurred.
Survey Development and Administration
The list of information needs resulting from the NGT sessions was used to develop a survey (supplemental appendix) about home-care nurses‘ perceptions of the information needs that their patients experience after leaving the hospital. Participants were asked to rate each information need on its frequency and impact on hospital readmission. Impact was defined as the frequency of rehospitalization associated with occurrences of a given need – in other words, when the need was present, how often did it lead to readmission? Both frequency and impact were rated on 5-point scales (1=rarely, 5=almost always). The survey was administered to home-care nurses via an online survey tool (www.surveygizmo.com), and those that completed the survey were eligible to enter a drawing for one of five $20 gift cards as a participation incentive.
The complete survey is given in the supplementary appendix (available online only). This study was approved by the University of Pittsburgh Institutional Review Board.
Analysis
Descriptive statistics were used to summarize demographic data for participants in both phases of the study. KMR and HH grouped the information needs into themes. We calculated descriptive statistics for survey responses. These included percentages of the participants that described an information need as “often” or “almost always” occurring (frequency) and those that described an information need as “often” or “almost always” resulting in a patient‘s readmission to the hospital (impact).
RESULTS
NGT sessions
A total of 17 nurses participated in the two NGT sessions (Table 1). The sessions consisted of predominantly Caucasian, middle-aged, well-educated, highly experienced, and female nurses.
Table 1.
Demographics
| Focus Groups | Survey | |
|---|---|---|
|
| ||
| Number of participants | 17 | 119 |
| Age (years) | ||
| 20–35 | 2 (11.8%) | 15 (12.6%) |
| 36–50 | 7 (41.2%) | 40 (33.6%) |
| 51–65 | 8 (47.0%) | 56 (47.1%) |
| > 65 | 0 (0%) | 8 (6.7%) |
| Highest Degree Earned | ||
| Diploma | 1 (5.9%) | 21 (17.7%) |
| Associate’s | 5 (29.4%) | 43 (36.1%) |
| Bachelor’s | 10 (58.8%) | 49 (41.2%) |
| Master’s | 1 (5.9%) | 5 (4.2%) |
| Other | 0 (0%) | 1 (0.8%) |
| Years as nurse | ||
| <5 | 2 (11.8%) | 7 (5.9%) |
| 5–15 | 2 (11.8%) | 23 (19.3%) |
| 16–25 | 7 (41.1%) | 28 (23.5%) |
| 26–35 | 5 (29.4%) | 35 (29.4%) |
| >35 | 1 (5.9%) | 26 (21.9%) |
| Years as home-care nurse | ||
| <5 | 4 (23.5%) | 29 (24.4%) |
| 5–15 | 7 (41.2%) | 49 (41.1%) |
| 16–25 | 4 (23.5%) | 29 (24.4%) |
| 26–35 | 2 (11.8%) | 12 (10.1%) |
| >35 | 0 (0%) | 0 (0%) |
| Hours per week | ||
| <20 | 2 (11.7%) | 9 (7.6%) |
| 20–30 | 0 (0%) | 21 (17.6%) |
| 31–40 | 7 (41.2%) | 40 (33.6%) |
| >40 | 8 (47.1%) | 49 (41.2%) |
The NGT sessions developed a list of 28 distinct responses. Categorization of these responses identified five topical themes: medications; disease/condition; non-medication care/treatment/safety; functional limitations; and communication problems (Table 2).
Table 2.
Information Needs and Communication Problems Identified by Home-Care Nurses in Two NGT sessions
Information needs and communication problems identified by home care nurses, grouped into five themes, with frequency and impact scores. The scores are the percentage of respondents (total = 119) who rated each information need as either “often” or “almost always” occurring (frequency) and when it occurs, as “often” or “almost always” resulting in a readmission (impact).
| Theme | Information Needs and Communication Problems | Frequency (%) | Impact (%) |
|---|---|---|---|
|
| |||
| Medications | 1. Post-discharge changes/medication reconciliation (new drugs, dose/schedule changes, discontinuation of prior drugs) | 50.4 | 23.5 |
| 2. Reason for taking | 51.3 | 17.7 | |
| 3. Side effects | 49.6 | 18.5 | |
| 4. Costs | 67.2 | 36.1 | |
| 5. When to contact doctor regarding abnormal reactions | 42.9 | 26.9 | |
| 6. Confusion regarding brand vs. generic | 55.5 | 32.8 | |
| 7. How to take medications | 30.2 | 19.3 | |
| 8. When to take medications | 28.6 | 14.3 | |
| 9. Which medications to take | 30.3 | 21.9 | |
| 10. Risks of noncompliance | 47.1 | 41.2 | |
|
| |||
| Disease/condition | 11. Diagnosed diseases/conditions | 27.7 | 23.5 |
| 12. Disease/condition progression | 51.3 | 39.5 | |
| 13. Symptoms of worsening condition | 29.4 | 39.5 | |
| 14. Disease severity | 50.4 | 31.9 | |
|
| |||
| Non-medication Care/Treatment/Safety | 15. How to use/manage home medical equipment | 40.3 | 18.5 |
| 16. Wound care | 41.2 | 16 | |
| 17. Home safety | 44.5 | 15.1 | |
| 18. Prescribed diet | 32.8 | 19.3 | |
|
| |||
| Functional Limitations | 19. Understanding of functional limitations | 22.6 | 17.7 |
| 20. Underestimation of need for caregiver/nursing care | 30.3 | 20.2 | |
| 21. Understanding home care nurses‘ role | 63 | 24.4 | |
|
| |||
| Communication Problems | 22. Understanding doctors (accents, hearing difficulty, literacy, health literacy) | 31.9 | 11.8 |
| 23. Miscommunication between clinicians | 17.7 | 6.7 | |
| 24. Miscommunication between patient and clinicians | 19.3 | 10.1 | |
| 25. Incorrect/misunderstood discharge instructions (rushed, skipped, confusing, health literacy problems) | 47.9 | 31.9 | |
| 26. Follow-up instructions (labs, testing, specialists, check-ups) | 24.4 | 15.1 | |
| 27. Conflicting information from clinicians | 26.9 | 12.6 | |
| 28. Information overload | 48.7 | 31.1 | |
Participants in the NGTs shared numerous anecdotes that underscored the potential impact of unmet information needs. One described a situation where a patient was instructed at hospital discharge to wait for a home care nurse before doing anything to a decubitus ulcer that the patient developed while in the hospital. The patient took these instructions literally and did not examine, clean, or change the dressings. When the home care nurse arrived at the patient‘s residence 48 hours post-discharge (the standard maximum time between discharge and the nurse‘s first visit), the wound had already become infected necessitating a hospital readmission. Based on this discussion, the issue of incorrect/misunderstood discharge instructions (rushed, skipped, confusing, health literacy problems) was included as a communication problem, and wound care instruction was included as an information need. Another nurse described a disagreement with a patient about the severity of his diabetes. Specifically, the patient did not understand how severe his diabetes was, and thus did not recognize the importance of adherence to a diabetic diet and the prescribed medication regimen. For this patient, one information need resulted in multiple other information needs.
Survey
The survey response rate was 54% (119/220, demographic data given in Table 1). Respondents appeared to be very familiar with readmissions, with 44% (52/119) reporting that more than 10% of their patients experienced a hospital readmission in the prior 30 days.
Table 3 contains the top 10 information needs and communication difficulties, as scored by the nurses, in terms of frequency of occurrence of the information need and perceived impact on hospital readmissions. Seven information needs appear in both the top 10 lists of frequency scores and of impact scores.
Table 3.
Top 10 Frequency Scores vs. Impact Scores of Information Needs and Communication Problems*
Percentages of respondents (total = 119) who rated each information need or communication problem as either “often” or “almost always” occurring (frequency) and when it occurs, as “often” or “almost always” resulting in a readmission (impact). Bold denotes an information need that is in the top 10 for both frequency and impact.
| Information Need | Frequency | Information Need | Impact |
|---|---|---|---|
| Cost of drugs | 67.2% | Risks of non-compliance | 41.2% |
| Understanding home care nurses’ role | 63.0% | Disease/condition progression | 39.5% |
| Brand vs. generic confusion | 55.5% | Symptoms of worsening condition | 39.5% |
| Reason for taking drug | 51.3% | Cost of drugs | 36.1% |
| Disease/condition progression | 51.3% | Brand vs. generic confusion | 32.8% |
| Medication reconciliation | 50.4% | Severity of diagnosis | 31.9% |
| Severity of diagnosis | 50.4% | Incorrect/misunderstood discharge information | 31.9% |
| Drug side effects | 49.6% | Information overload | 31.1% |
| Information overload | 48.7% | When to contact doctor about abnormal reaction | 26.9% |
| Incorrect/misunderstood discharge information | 47.9% | Understanding home care nurses’ role | 24.4% |
DISCUSSION
This is the first study that uses the perspective of home-care nurses to examine the post-hospitalization unmet information needs of elderly patients. These nurses present an important opportunity to help with patient integration and reduction of unplanned hospitalization. Our research results provide a unique and potentially useful perspective regarding patient perceptions of information needs.
Novel Information Needs
Our respondents identified several frequent, high impact information and communication needs including information about medication regimens (reason for taking, side effects, costs, brand vs. generic names, and risks of non-compliance); the severity of their condition; hospital discharge management process; non-medication care regimens such as wound care, use of durable medical equipment and home safety; the extent of care needed, and which providers are best suited to provide that care (Figure 2).
Information needs previously discussed in the literature[1,2] were identified, and often ranked highly, by the respondents. Five of the top information needs in the lists of high-frequency and high-impact needs appear in earlier work[1,2], whereas all of the needs identified by these authors appear in the total list of 28 information needs and communication problems identified in our NGT sessions.
Information Need Themes
Medications
The emergence of medication concerns as a major theme is consistent with previous reports[19–34]. Our respondents indicated that a lack of understanding of the consequences of medication non-adherence may be more of a problem than gaps in the information necessary for compliance. This is consistent with research showing that negative beliefs about medicines and treatments predict medication non-adherence[35,36]. Respondents identified several information needs that have not received much attention in prior literature. Lack of information about medication costs presents challenges, as patients are surprised with unaffordable prescriptions, and may leave some unfilled, thus increasing non-adherence and potentially increasing the likelihood of readmission. Similarly, misunderstanding the relationship between generic and brand-name drugs may cause some patients to take both, doubling their dosage.
Other studies address the significant information difficulties related to medication adherence challenges that elderly patients experience during transitional care. Specific problems include the reliability of medication information, concerns about polypharmacy, discrepancies in medication information, and the sharing of medical information among clinicians[19–25]. Information at discharge, including information such as medication lists and general expectations for the transition back to the home, can lead to discharges that patients perceive to be less confusing[26,27]. However, interventions aimed at meeting the information needs of discharged patients[28–34] have generally not been informed by formal prior inquiries into these needs, nor do they detail what information is provided to patients in those studies.
Disease/Condition and Non-Medication Care
Nurses indicated that patients often do not understand the severity of their diagnoses, particularly with respect to the importance of medications, treatments, lifestyle changes, and identifying changes in symptoms that may require additional medical intervention. They also do not know how to operate home medical equipment such as oxygen tanks and insulin pumps, how to care for wounds, how to follow prescribed diets, or how to make their homes safe. These problems may be related to low health literacy levels of patients, a pervasive barrier to effective health care[37,38].
Functional Limitations
Greater understanding of clinicians‘ roles was a frequently cited need. The nurses indicated that patients and families often treated nurses as home aides, expecting that nurses would help with duties such as bathing and feeding. As these tasks are not normally considered to be the responsibility of the nurses, mismatched expectations could lead to poor outcomes if feeding or hygiene is neglected.
Communication
Although our original intent was to identify specific types of information that may be lacking, the phrasing of our initial inquiry question - “In your experience, what information-related problems have your elderly patients experienced that contributed to hospital readmissions?”-implicitly invited participants to discuss communication problems as well as specific information topics. The identification and resolution of communication breakdowns will certainly be necessary components of any interventions that will address these information needs. Specific difficulties identified by respondents include miscommunication between clinicians, and between patients and clinicians. Nurses also felt that difficulties with accents, hearing, and literacy often prevented patients from understanding physicians. Problems with discharge instructions include incorrect or misunderstood discharge information, concerns about follow-up instructions, and conflicting information from different clinicians. The nurses stated that their patients frequently do not understand their doctors for those reasons, nor do they ask for clarification. Consequently, they lack important information.
Respondents identified patient information overload as a potential source of difficulties, despite patients‘ lack of knowledge about many aspects of their conditions and treatments. To effectively help older patients, improved information resources will have to strike a balance between emphasizing vital information about conditions and consequences, and consideration for patients‘ health literacy and cognitive function. Information overload creates an information need by making pertinent information inaccessible.
Care Transitions and Information Continuity
Information sharing generally features prominently in home care transition models. A review of conceptual models and frameworks of care transitions[39] discussed six approaches to care transitions[29–31,40–43], four of which involve hospital to home transitions. The Transitional Care Model (TCM)[40] incorporates planning at discharge and home follow-up care, with an emphasis on engaging the patient and family in the care. The Care Transitions Program (CTI)[41,42], based on Coleman‘s model of effective care transitions[1], involves home visits and phone calls, and encourages self-management by the patient and communication with the primary care provider. Project BOOST attempts to improve the discharge process comprehensively using evidence-based methods[43]. ProjectRED combines a virtual patient advocate who provides information to the patient at discharge with a comprehensive information packet given to the patient, caregivers, and primary care provider[29–31]. Watkins and Kring describe an intervention for frail older adults using home care visits, education, and a comprehensive set of support services to reduce hospital readmissions by 61% and save over $600000 per year[44].
These models have all been shown to reduce hospital readmissions, and some have been shown to reduce costs[29–31,40–42,44]. They all emphasize communication of information between patients, caregivers, and clinicians as a central aspect of an effective care transition. This is reflected in the NTOCC‘s model of effective care transitions, in which information is relayed from one care location to another[16]. Although these models all involve sharing information with patients, they differ in what is shared and how it is shared. However, no minimum required information necessary for an effective care transition has been identified, nor do the creators of these models provide justification for the information given to patients in their interventions. Our study attempts to address this void in the NTOCC model by identifying the information home-care nurses consider important for a safe transition home from the hospital. This novel perspective has led to the identification of information needs that have not been previously discussed.
Our work suggests that greater information sharing, and therefore information continuity, might be extended to home-care nurses in order to have an even greater impact on reducing readmissions. Research has shown that information continuity is important for avoiding readmissions[45,46]. A study of the perspectives of stakeholders in handovers between hospital staff and general practitioners found that one of the major reasons for ineffective handovers was inadequate information sharing between hospital and community clinicians[47]. The discharge report has been cited as the information source that home care nurses‘ find most lacking[48]. Although the ProjectRED protocol explicitly includes information sharing between patients and clinicians, by providing participants‘ information packets to their primary care provider[29,30], home-care nurses are not included. Sharing information with home care nurses, not just physicians, might alleviate some of the concerns raised by participants in our study.
A survey of 18 home-care nurses about their perceptions of transitions from hospital to home[49], identified a list of gaps in transition, including information needs consistent with our results, such as wound care and home medical equipment information. This work provides further support for our observations.
Nurses in our NGT sessions noted that they frequently lack information necessary for providing effective home care. They rely on the patients and caregivers to provide relevant information, which is often wrong, misunderstood, or lacking. The nurses felt that simply providing additional information to patients would not be sufficient, as many patients might have difficulty with comprehension and would need explanations from a home-care nurse or other clinician.
Although many of these information needs may be addressed separately by current practices, combining these details in a customized, comprehensive resource may help reduce confusion and information overload. The integration of such a resource into post-discharge home-care practice would provide nurses with opportunities to review issues with their patients and their patients‘ physicians, potentially improving the immediate post-hospitalization period. Ideally, this would effectively provide the key information‘ in the NTOCC conceptual framework for care transitions[16].
Policy and Recommendations
Since hospital readmissions have multiple underlying causes, it is unlikely that a single solution can address all potential problems. Studies implementing interventions to improve patient handovers have not yet clearly identified which interventions are most effective at improving patient care[50]. The framework developed by the NTOCC, which emphasizes a patient-centered approach and a shared accountability of information exchange[16], has the possibility of improving the current situation. Hospital systems need to develop protocols for sharing key information between clinicians, patients and their caregivers at each and every care transition. Multiple effective models have been developed, but have not been widely implemented. Our results suggest that home care nurses have a valuable role to play in the development and implementation of these protocols.
This study suggests information that should be considered for inclusion in the information exchange with home care nurses, as well as identifies communication problems that hinder the sharing of information. Addressing both the key information and the most effective ways of transmitting that information to the people who need it is important for improving the process of care transitions to the home, and to potentially reduce hospital readmissions.
Limitations
Further investigation amongst a larger and more diverse set of home-care nurses in terms of geography and types of patients followed is needed to rigorously determine the relative importance of the various needs. Moreover, as we do not know if patients would return the same results, surveys targeting patients directly could further substantiate these findings. We did not ask the nurses to delve into health and cognitive differences across patient populations, so we do not know whether and how different information needs were important for different types of patients with varying underlying comorbid illnesses, cognitive function or functional status. Better understanding of patient and home-care nurse perspectives of information continuity during care transitions will be another step towards a broader and more systemic solution to improve care transitions and reduce hospital readmissions.
CONCLUSION
Home-care nurses identified a variety of unmet information needs during the first 30 days in the immediate post-hospitalization period that can result in readmission of their patients. Several of these needs were not previously discussed in the literature, including the need for more detailed information about medication regimens, the severity of the patient‘s condition, post-discharge procedures, non-medication care regimens unrelated to medications, and the need for ongoing care with appropriate providers. These results provide insight into the types of information needs that home care nurses perceive as contributing to sub-optimal outcomes, including readmissions. Future research is needed to determine how and when to provide this information to patients and home care nurses, and how the impact of such interventions might best be measured. Meeting these information needs may prevent hospital readmissions, improve health outcomes, and keep patients safer at home.
Supplementary Material
Box 1. Novel Information Needs and Communication Problems.
Reason for taking medications
Side effects of medications
Costs of medications
Confusion regarding brand vs. generic medications
Risks of noncompliance of medications
Disease severity
Conflicting information from clinicians
Information overload
How to use/manage home medical equipment
Wound care
Home safety
Understanding of functional limitations
Underestimation of need for caregiver/nursing care
Understanding home care nurses’ role
Acknowledgments
The authors also wish to thank the UPMC Home Health Agency. Christa Bartos provided valuable feedback on drafts of this manuscript.
FUNDING
This study was supported by the NLM Fellowship 5 T15 LM007059-24, Agency for Healthcare Research and Quality (R01HS018721) and National Institute of Aging grants (R01AG027017; P30AG024827; K07AG033174).
Footnotes
COMPETING INTERESTS
There are no competing interests to report.
Contributorship Statement
Katrina Romagnoli developed and executed the study, analyzed the data, and wrote the paper. Steven Handler oversaw the development and execution of the study, and helped write and edit the paper. Frank Ligons assisted in data collection and provided feedback on the paper. Harry Hochheiser oversaw the development and execution of the study, assisted in analyzing the data, and helped write and edit the paper.
Data Sharing Statement
Data is available upon request from corresponding author.
References
- 1.Coleman EA. Falling Through the Cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs. J Am Geriatr Soc. 2003;51:549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 2.Greenwald JL, Denham CR, Jack BW. The hospital discharge: A review of a high risk care transition with highlights of a reengineered discharge process. J Patient Saf. 2007;3:97–106. [Google Scholar]
- 3.Van Walraven C, Bennett C, Jennings A, et al. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183:E391–402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Walraven C, Dhalla IA, Etchells E, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182:551–557. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.AARP Public Policy Institute. Taking the Long View: Investing in Medicaid Home and Community-based Services is Cost-Effective. 2009. [Google Scholar]
- 6.Swan BA. A nurse learns firsthand that you may fend for yourself after a hospital stay. Health Aff (Millwood) 2012;31:2579–82. doi: 10.1377/hlthaff.2012.0516. [DOI] [PubMed] [Google Scholar]
- 7.Home Health Nurses Association. [Accessed 1/31, 2012]; Available at: http://www.hhna.org.
- 8.Hughes S, Ulasevich A, Weaver F, et al. Impact of home care on hospital days: a meta analysis. Health Serv Res. 1997;32:415–432. [PMC free article] [PubMed] [Google Scholar]
- 9.Elkan R, Kendrick D, Dewey M, et al. Effectiveness of home based support for older people: Systematic review and meta-analysis. BMJ. 2001;323:719–24. doi: 10.1136/bmj.323.7315.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Joint Commission. Home—The Best Place for Health Care. 2011. [Google Scholar]
- 11.Barrett D, Secic M, Borowske D. The Gatekeeper Program: proactive identification and case management of at-risk older adults prevents nursing home placement, saving healthcare dollars program evaluation. Home Healthc Nurse. 2010;28:191–197. doi: 10.1097/01.NHH.0000369772.41656.4e. [DOI] [PubMed] [Google Scholar]
- 12.Beales JL, Edes T. Veteran‘s Affairs home based primary care. Clin Geriatr Med. 2009;25:149–154. doi: 10.1016/j.cger.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Leff B, Burton L, Mader SL, et al. Comparison of Functional Outcomes Associated with Hospital at Home Care and Traditional Acute Hospital Care. J Am Geriatr Soc. 2009;57:273–278. doi: 10.1111/j.1532-5415.2008.02103.x. [DOI] [PubMed] [Google Scholar]
- 14.Counsell SR, Callahan CM, Clark DO, et al. Geriatric Care Management for Low-Income Seniors. JAMA. 2007;298:2623–2633. doi: 10.1001/jama.298.22.2623. [DOI] [PubMed] [Google Scholar]
- 15.Mamolen NL, Brenner PS. The impact of a burn wound education program and implementation of a clinical pathway on patient outcomes. The Journal of Burn Care & Rehabilitation. 2000;21:440–445. doi: 10.1097/00004630-200021050-00010. [DOI] [PubMed] [Google Scholar]
- 16.National Transitions of Care Coalition. [Accessed 9/24, 2012];Improving Transitions of Care: The Vision of the National Transitions of Care Coalition. 2008 Available at: http://www.ntocc.org/Portals/0/PDF/Resources/PolicyPaper.pdf.
- 17.Carney O, McIntosh J, Worth A. The use of the Nominal Group Technique in research with community nurses. J Adv Nurs. 1996;23:1024–1029. doi: 10.1046/j.1365-2648.1996.09623.x. [DOI] [PubMed] [Google Scholar]
- 18.Saldana J. The Coding Manual for Qualitative Researchers. Thousand Oaks, Calif: Sage; 2009. [Google Scholar]
- 19.Marcusen C. Information and communication needs of individuals living with advanced cancer. Semin Oncol Nurs. 2010;26:151–156. doi: 10.1016/j.soncn.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Beaudoin CE, Hong T. Health information seeking, diet and physical activity: An empirical assessment by medium and critical demographics. Int J Med Inform. 2010;80:586–595. doi: 10.1016/j.ijmedinf.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Lithner M, Zilling T. Pre- and postoperative information needs. Patient Educ Couns. 2000;40:29–37. doi: 10.1016/s0738-3991(99)00043-9. [DOI] [PubMed] [Google Scholar]
- 22.Haverhals L, Lee C, Siek K, et al. Older adults with multi-morbidity: medication management processes and design implications for personal health applications. J Med Internet Res. 2011;13:e44. doi: 10.2196/jmir.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Madden JM, Graves AJ, Zhang F, et al. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA. 2008;299:1922–1928. doi: 10.1001/jama.299.16.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marcum Z, Gellad W. Medication adherence to multi-drug regimens. Clin Geriatr Med. 2012 doi: 10.1016/j.cger.2012.01.008. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Handler SM, Perera S, Olshansky EF, et al. Identifying Modifiable Barriers to Medication Error Reporting in the Nursing Home Setting. J Am Med Dir Assoc. 2007;8:568–574. doi: 10.1016/j.jamda.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fagermoen MS, Hamilton G. Patient information at discharge—A study of a combined approach. Patient Educ Couns. 2006;63:169–176. doi: 10.1016/j.pec.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 27.Sheard C, Garrud P. Evaluation of generic patient information: Effects on health outcomes, knowledge and satisfaction. Patient Educ Couns. 2006;4(61):43–47. doi: 10.1016/j.pec.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Siek KA, Ross SE, Khan DU, et al. Colorado Care Tablet: The design of an interoperable Personal Health Application to help older adults with multimorbidity manage their medications. J Biomed Inform. 2010;43:S22–S26. doi: 10.1016/j.jbi.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clancy CM. Reengineering Hospital Discharge: A Protocol to Improve Patient Safety, Reduce Costs, and Boost Patient Satisfaction. Am J Med Qual. 2009;24:344–346. doi: 10.1177/1062860609338131. [DOI] [PubMed] [Google Scholar]
- 31.Bickmore TW, Pfeifer LM, Paasche-Orlow MK. Using computer agents to explain medical documents to patients with low health literacy. Patient Educ Couns. 2009;75:315–320. doi: 10.1016/j.pec.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4:211–218. doi: 10.1002/jhm.427. [DOI] [PubMed] [Google Scholar]
- 33.Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 34.Shu CC, Hsu NC, Lin YF, et al. Integrated postdischarge transitional care in a hospitalist system to improve discharge outcome: an experimental study. BMC Med. 2011;9:96. doi: 10.1186/1741-7015-9-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wileman V, Chilcot J, Norton S, et al. Choosing not to take phosphate binders: the role of dialysis patients’ medication beliefs. Nephron Clin Pract. 2011;119:205–213. doi: 10.1159/000329106. [DOI] [PubMed] [Google Scholar]
- 36.Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;12(47):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 37.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15:259–267. [Google Scholar]
- 38.Williams MV, Baker DW, Parker RM, et al. Relationship of Functional Health Literacy to Patients’ Knowledge of Their Chronic Disease: A Study of Patients With Hypertension and Diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 39.Enderlin CA, McLeskey N, Rooker JL, et al. Review of current conceptual models and frameworks to guide transitions of care in older adults. Geriatr Nurs. 2012 doi: 10.1016/j.gerinurse.2012.08.003. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 40.Naylor MD, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 41.The Care Transitions Program. Health Care Services for Improving Quality and Safety during Hand-Offs. Eric Coleman Model (CTI) Available at: http://www.caretransitions.org. Cited November 28, 2012.
- 42.Parrish MM, O‘Malley K, Adams RI, et al. Implementation of the care transitions intervention: sustainability and lessons learned. Prof Case Manag. 2009;14:282–93. doi: 10.1097/NCM.0b013e3181c3d380. [DOI] [PubMed] [Google Scholar]
- 43.BOOST (Better Outcomes for Older Adults through Safe Transitions) Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home&TEMPLATE=/CM/HTMLDisplay.cfm&CONTENTID=27659. Cited November 28, 2012.
- 44.Watkins L, hall C, Kring D. Hospital to home: a transition program for frail older adults. Prof Case Manag. 2012;17:117–123. doi: 10.1097/NCM.0b013e318243d6a7. [DOI] [PubMed] [Google Scholar]
- 45.Van Walraven C, Taljaard M, Etchells E, et al. The independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists. J Hosp Med. 2010;5:398–405. doi: 10.1002/jhm.716. [DOI] [PubMed] [Google Scholar]
- 46.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 47.Göbel B, Zwart D, Hesselink G, et al. Stakeholder perspectives on handovers between hospital staff and general practitioners: an evaluation through the microsystem lens. BMJ Qual Saf. 2012;21 (Suppl 1):i106–i113. doi: 10.1136/bmjqs-2012-001192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vaidya SR, Shapiro JS, Papa AV, et al. Perceptions of health information exchange in home healthcare. Comput Inform Nurs. 2012 doi: 10.1097/NXN.0b013e3182573a91. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 49.Smith SB, Alexander JW. Nursing perception of patient transitions from hospitals to home with home health. Prof Case Manag. 2012;17:175–185. doi: 10.1097/NCM.0b013e31825297e8. [DOI] [PubMed] [Google Scholar]
- 50.Hesselink G, Schoonhoven L, Barach P, et al. Improving Patient Handovers from Hospital to Primary Care: A Systematic Review. Ann Intern Med. 2012;157:417–428. doi: 10.7326/0003-4819-157-6-201209180-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


