Abstract
Background
Influenza vaccination decisions may be influenced by perceived risk reduction related to herd immunity.
Purpose
This paper examines how free riding or protective benefits to the community affect vaccination decisions.
Methods
A survey of a nationally representative panel of U.S. adults (N=442 respondents; data collected and analyzed during 2012) asked about how respondents made vaccination decisions, including whether and how vaccination among the members of respondents’ social networks influenced their own vaccination decisions.
Results
Most individuals (61%) reported that vaccination in the social network would not influence their decision. Among those perceiving being influenced by vaccination in their social network, most stated that an increase in network vaccination coverage would make them more likely to get vaccinated, rather than less. Overall, only 6% (28 out of 442) gave a response consistent with the reduced-risk logic of herd immunity, which was more common among those stating that they would be less likely to get vaccinated (emphasizing free riding) than among those more likely to get vaccinated (emphasizing social protection; 33% vs. 11%, two-sided p = .0005). The reduced-risk logic of herd immunity, and more specifically free riding, is consciously considered by relatively few individuals. Far more common are social influences bolstering personal vaccination, such as peer pressure and social learning (6% vs. 11%, two-sided p = .015).
Conclusions
Interventionists may be better off capitalizing on existing social-influence considerations than combating the conscious lure of free riding.
Introduction
Influenza vaccination is universally recommended, but uptake is dismal among adults at 46%.1 The decision to be vaccinated depends largely upon the perceived risks and benefits,2 potentially including the perceived risk or protection provided by an individuals’ social networks. If people associate transmission risk with the infectiousness of their social networks, increasing vaccination, resulting in “herd immunity,” should reduce the expected benefits of personal vaccination because individuals perceive lower likelihood of contact with infection.3 Such reduced risk perceptions related to herd immunity may lead individuals to act in their own interest and forgo vaccination – the so-called “free rider” problem.4,5
Other influences arising from social networks such as social learning and peer pressure could lead to increased or decreased vaccination rates. In particular, the flip side to free riding is the “indirect protection” of others by one’s own vaccination. Individuals electing to vaccinate not only protect themselves, but also contribute to herd immunity, protecting those in their social networks.6
This report extends our understanding of social influences on vaccination decisions, which has been based largely on experimental studies,6,7 small-sample qualitative research,8,9 and limited populations such as college students. It is hypothesized that herd immunity, and specifically free riding, will play a relatively minor conscious role in vaccination decisions. The paper presents open-ended reporting of a national sample’s perceptions related to (a) the risk-reduction logic of herd immunity, (b) the two logical extensions of the herd immunity concept – free riding and protection of others – and (c) how these perceptions relate to the likelihood of influenza vaccination.
Methods
From April to June of 2012, a web-based survey was fielded to a nationally representative sample of U.S. adults age 18 and older participating in RAND’s American Life Panel (https://mmicdata.rand.org/alp/). The study protocol was approved by the institutional review board of the RAND Corporation, and analyses were conducted in 2012.
As part of a larger survey, respondents were asked, “If enough people that you have regular, face-to-face contact with get vaccinated, would you be more or less likely to get vaccinated yourself?” Response options were “much more likely,” “somewhat more likely,” “neither more nor less likely,” “somewhat less likely,” and “much less likely.” Respondents were then asked the open-ended question “Why do you think you would be more [less] likely to get vaccinated?” (excluding those neither more nor less likely to be vaccinated). Respondents also reported on influenza vaccination during the prior year.
The coding scheme for the open-text responses incorporated reasons for being more or less likely to get vaccinated, with codes based on initial review of responses and existing literature (see Table 1 for coding scheme). Two researchers coded responses, achieving agreement on 86% of passages and resolving discrepancies by consensus.
Table 1.
Coding scheme classifying open-text reasons for being more or less likely to get vaccinated
| Code | Example |
|---|---|
| Codes for respondents who agreed that vaccination in their social network would make them more likely to get vaccinated | |
| Social Influence Specifically Herd Immunity (Protecting Others) |
“Because the people I surround myself with are responsible enough to take care of themselves and others, so why shouldn’t I?” “Because none of us would be able to pass on the flu to each other.” |
| Risk of Getting Sick | “I believe getting vaccinated prevents me from getting the flu and less colds.” |
| Past Behavior | “I get vaccinated for the flu every year” |
| Reduced Barriers | “I am likely to get vaccinated when it is easily available to me.” |
| Codes for respondents who agreed that vaccination in their social network would make them less likely to get vaccinated | |
| Herd Immunity (Free Riding) | “If everyone else is vaccinated I wouldn’t need to be because the people around me aren’t sick and therefore I won’t get sick.” |
| Don’t Need the Vaccine | “I just don’t think I need it, I have never been sick with anything like it.” |
| Vaccine Not Effective/Safe | “They do not work, they are filled with things that should not be injected into the human body.” |
| Past Behavior | “I have NEVER had a flu shot.” |
| Barriers to Vaccination | “Because it cost money to get the shot.” |
| Low Trust in Authorities | “I do not trust the government.“ |
Frequency distributions summarize responses. Chi-squared tests of independence compare relationships between two categorical variables, z-tests compare proportions in independent samples, and McNemar tests compare proportions among dependent samples.
Results
The overall response rate was 85.5% (N=442). Mean age was 49.7 years, 47.1% male, 86.4% white, and 44.1% had a Bachelor’s degree or higher. Half (44.8%) reported influenza vaccination in the prior year – consistent with CDC’s 46% estimated vaccination rate.1
Most (61%) reported that vaccination in their social network would not influence their decision to receive influenza vaccine. Of the 39% of respondents who did report that the rate of vaccination in their network influenced their decision, most (132 of 174) agreed that it would make them more likely to get vaccinated. Self-reported vaccination rates were highest for this group (64.1%), followed by those reporting no influence (39.7%) or negative influence (19.0%, p<.001).
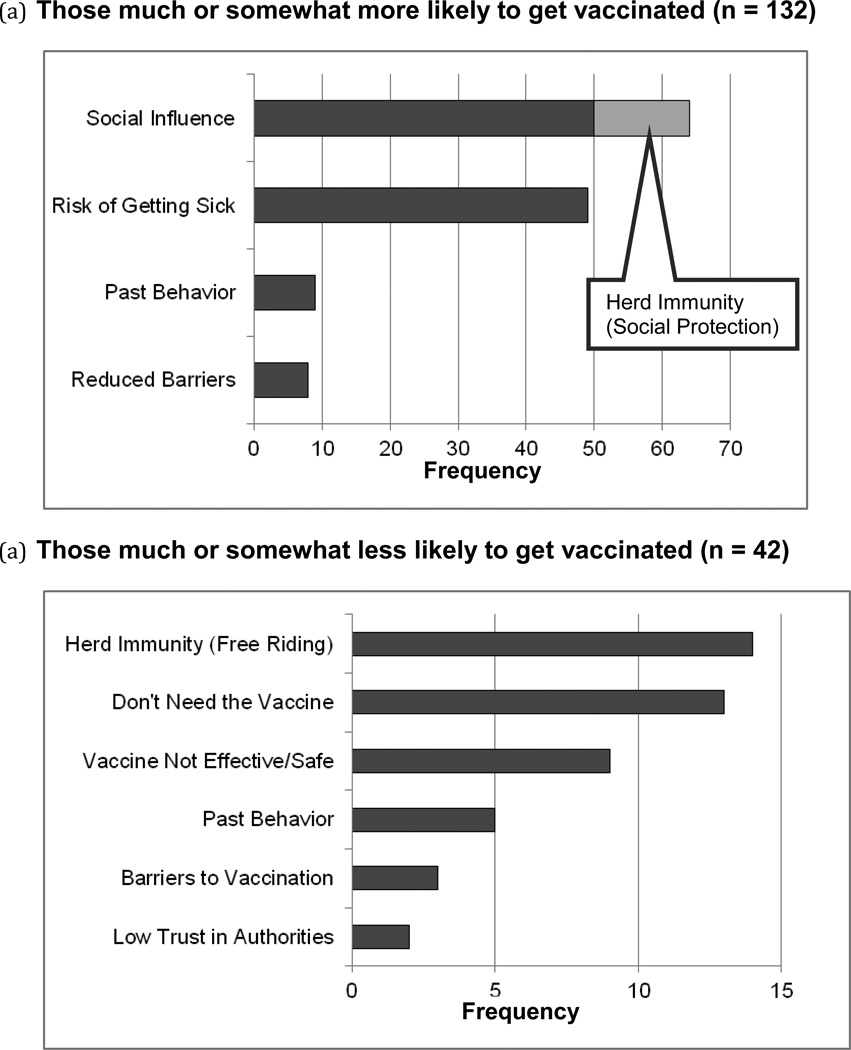
Of 132 respondents stating that vaccination in their social network would make them more likely to get vaccinated, 126 (95%) gave open-ended explanations, and 64 (51%) were socially-related (top bar, Figure 1a). Fourteen of those 64 (22%) reflected the social-protection logic behind herd immunity (“less people will get sick”). However, most of the social reasons (50 of 64) related to social influence, either through information obtained from the social network (“if many around me are getting vaccinated, it must be a good idea”) or social pressure (“peer pressure”). With regards to actual vaccination, those giving any socially-related reason were somewhat more likely to report getting vaccinated than the rest of the sample (63% vs. 44%, p=.05), but those giving social-protection reasons were substantially more likely to get vaccinated (92% vs. 44%, p=.0005).
Figure 1.
Reasons for (top) or against (bottom) getting vaccinated if enough of those around you were.
Of the 42 who stated that vaccination in their network would make them less likely to get vaccinated, 40 (95%) gave text responses (Figure 1b). Fourteen of those 40 (35%) mentioned socially-related factors, all consistent with herd immunity and free riding (“less likely those around me will get the flu and pass it on to me”). This rate of herd-immunity-related responses was significantly higher than among those saying that they would be more likely to get vaccinated if enough people in their social network got vaccinated (p=.0005). Compared to the rest of the sample, those giving free-riding-related reasons were no more or less likely to self-report actually getting vaccinated (36% vs. 45%, ns.).
Overall, only 6% (28 of 442) gave a response consistent with the reduced-risk logic of herd immunity (either free riding or social protection).
Discussion
This study examines whether the reduced-risk logic of herd immunity is consciously considered in vaccination decisions. Most people asserted that vaccination by those around them is irrelevant to their personal vaccination decisions, but those seeing an influence were more likely to increase willingness to get vaccinated than decrease. Even among those claiming to be influenced by their social network, most did not express thoughts about herd immunity specifically. Many gave non-social reasons even though the preceding question asked specifically about social influences, highlighting the rarity of herd immunity as a prominent conscious consideration. Proportionally, the logic of herd immunity was more likely among those who stated that if enough people around them got vaccinated, that they would be less likely to get vaccinated (consistent with free riding) than among those stated that they would be more likely to get vaccinated (consistent with protecting others). Overall, these results support the main hypothesis.
The data are self-reports (prompted by specific question wording), thus limited to cognitions of which people are aware and willing to report.10 Given that free riding is a rational extension of recognizing herd immunity,4,5 it is appropriate to consider conscious rationales. Although the number of respondents providing open-ended responses limits the ability to cross-tabulate with other factors, the diverse national sample provides evidence on the prevalence and influence of herd immunity considerations and complements past research using small interview samples8,9 and detailed scenarios.6,7
Although free riding was not consciously considered by most of our sample, some may subconsciously take advantage of herd immunity. That said, models of vaccination behavior11,12 often focus on herd immunity, neglecting the potentially greater effects of social learning and social pressure.13
In summary, the reduced-risk logic of herd immunity is consciously considered by few, and these considerations are as likely to relate to social protection as to free riding. Far more common are social influences bolstering vaccination, such as peer pressure and social learning. Instead of trying to combat the conscious lure of free riding, interventionists may be better off capitalizing on existing social-influence considerations.
Acknowledgements
Financial support for the data collection underlying this study was provided by the National Cancer Institute (NCI) under grant 5R21CA157571-02 (PI: Vardavas). Dr. Marcum was supported by the National Institute on Aging under grant T32AG000244. This work would not have been possible without the insights of our colleagues, Kayla de la Haye, Daniela Golinelli, Amber Jaycocks, and Sarah Nowak.
Footnotes
Conflict of interest statement:
Drs. Parker, Vardavas, Marcum, and Gidengil have no other financial disclosures.
References
- 1.Centers for Disease Control and Prevention. March Flu Vaccination Coverage. United States, 2011– 12 Influenza Season. [Accessed July 12, 2012];2012 http://www.cdc.gov/flu/professionals/vaccination/nfs-survey-march2012.htm.
- 2.Gidengil CA, Parker AM, Zikmund-Fisher BJ. Trends in risk perceptions and vaccination intentions: a longitudinal study of the first year of the H1N1 pandemic. Am J Public Health. 2012 Apr;102(4):672–679. doi: 10.2105/AJPH.2011.300407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fine PE. Herd immunity: history, theory, practice. Epidemiol Rev. 1993;15(2):265–302. doi: 10.1093/oxfordjournals.epirev.a036121. [DOI] [PubMed] [Google Scholar]
- 4.Funk S, Salathe M, Jansen VA. Modelling the influence of human behaviour on the spread of infectious diseases: a review. J R Soc Interface. 2010 Sep 6;7(50):1247–1256. doi: 10.1098/rsif.2010.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vardavas R, Breban R, Blower S. Can influenza epidemics be prevented by voluntary vaccination? PLoS Comput Biol. 2007 May;3(5):e85. doi: 10.1371/journal.pcbi.0030085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hershey JC, Asch DA, Thumasathit T, Meszaros J, Waters VV. The roles of altruism, free riding, and bandwagoning in vaccination decisions. Organization Behavior and Human Decision Processes. 1994;59(2):177–187. [Google Scholar]
- 7.Vietri JT, Li M, Galvani AP, Chapman GB. Vaccinating to help ourselves and others. Med Decis Making. 2012 May-Jun;32(3):447–458. doi: 10.1177/0272989X11427762. [DOI] [PubMed] [Google Scholar]
- 8.Downs JS, de Bruin WB, Fischhoff B. Parents' vaccination comprehension and decisions. Vaccine. 2008 Mar 17;26(12):1595–1607. doi: 10.1016/j.vaccine.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006 May;117(5):1532–1541. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 10.Ericsson KA, Simon HA. Verbal reports as data. Psychological Review. 1980;87(3):215–251. [Google Scholar]
- 11.Galvani AP, Reluga TC, Chapman GB. Long-standing influenza vaccination policy is in accord with individual self-interest but not with the utilitarian optimum. Proc Natl Acad Sci U S A. 2007 Mar 27;104(13):5692–5697. doi: 10.1073/pnas.0606774104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhattacharyya S, Bauch CT. "Wait and see" vaccinating behaviour during a pandemic: a game theoretic analysis. Vaccine. 2011 Jul 26;29(33):5519–5525. doi: 10.1016/j.vaccine.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 13.Vardavas R, Marcum CS. Modeling influenza vaccination behavior via inductive reasoning games. In: Manfredi P, d'Onofrio A, editors. Modeling the Interplay Between Human Behavior and the Spread of Infectious Diseases. New York: Springer; 2012. [Google Scholar]