Abstract
Background
Most unintentional childhood poisonings and firearm injuries occur in residential environments. Therefore, a preventive strategy includes limiting children’s access to poisons and firearms through safe storage. This study examines storage of poisons and firearms among households with older adults, and households where young children reside compared to those where they visit only.
Methods
Sample is from a 2002 national random-digit-dial survey of 1003 households. Analyses were weighted to reflect the national population.
Results
There were 637 households with children residents or visitors aged <6 years. Seventy-five percent of the households (n =480) had children aged <6 as visitors only, and 15% had older adult residents (aged ≥70 years). Poisons and firearms were stored less securely in homes with young children as visitors as compared to those homes with resident young children. In 55% of homes where young children lived, and 74% of homes where young children were only visitors, household chemicals were reportedly stored unlocked. Although firearm ownership was comparable between the two categories of households (33% vs 34%), homes in which children were only visitors were more likely to store firearms unlocked (56%), than homes in which children resided (33%). Homes with older adult residents had more firearms present.
Conclusions
Children are at risk from improperly stored poisonous substances and firearms in their own homes and homes they visit. Strategies are needed to improve the storage practices of both poisons and firearms to minimize in-home hazards to young children, particularly raising awareness of these hazards to young visitors.
Introduction
Unintentional injuries are the leading cause of death for young children aged 1 to 9 years in the United States.1 Each year, about one fourth of U.S. children seek medical attention for an injury.2 Poisoning and firearm injuries represent some of the most common unintentional injuries to children. Among those aged <6 years, there were 93,703 unintentional poisonings, and approximately 233 unintentional firearm injuries in the United States in 2001. During this same time period there were 49 unintentional poisoning deaths and 17 unintentional firearm deaths in this age group.1
Firearms are present in approximately one third of all U.S. households.3 In these households, nearly one half of all firearms are stored unlocked4; and approximately one fifth of households have guns stored both loaded and unlocked.5 Although households with children tend to have safer firearm storage practices than those without children, the proportions of household firearm ownership in homes with versus without children are comparable.6,7
Unintentional poisonings and firearm injuries are similar in that both commonly take place in a home environment. About 90% of poison exposures and 69% of unintentional firearm injuries to children occur in a residence.8,9 Thus, a primary strategy to prevent both types of injuries is to limit home access to poisonous substances and firearms through safe storage.
Recommendations for the safe storage of poisonous substances and firearms have been put forth by many professional organizations10–17 based on evidence of the risk of injuries from access to firearms18,19 and poisons20 in the home. Through policy statements and The Injury Prevention Program, the American Academy of Pediatrics (AAP) recommends that poisonous substances be kept out of children’s sight and reach, that medicine and household products be purchased in childproof packages, and that safety caps always be replaced immediately after use. AAP also recommends that all medicines, household products, and personal care products be stored in locked cabinets and that caregivers be aware of medicines and potentially poisonous substances that visitors to a child’s home may introduce.10,11 Similarly, AAP recommends that firearms be removed from homes with children. For families choosing to keep firearms in the home, AAP recommends that guns be stored unloaded, in a locked place, and separate from the ammunition.10 While these recommendations are logical and likely to limit youth access to these agents, currently there are no published studies documenting the effectiveness of safe storage of poisons or firearms. However, there have been studies documenting that unsecured firearms have been a key factor in firearm injuries among children.9,21 Safe storage of firearms also includes the use of safety devices. Two recent publications suggest that safety devices could reduce unintentional fatalities by 31% to 37%.21,22 Despite safety devices for storage and safety recommendations, many households do not store their poisons and firearms safely.
Several studies have documented storage practices of poisonous substances in households with children, including medication,23–30 cleaning products,24,26–28 pesticides,24,31 and chemicals.25,27,29,32 These studies show that parents report storing poisonous substances out of children’s reach in 18% to >90% of households.23–32 The percentage of households in which poisons were reportedly kept locked also varied widely, ranging from 9% to 89%.26,27 The variations in reported poison storage practices are likely explained by the regional, economic, and cultural differences of the populations studied as well as by variations across studies in self-report versus observed storage. There generally is less variation among reported firearm storage practices across studies.33
The primary aim of this study was to examine how poisonous substances and firearms are stored in U.S. households where young children reside compared with households where young children only visit. Children are exposed to poisons and firearms in homes they visit as well as where they live. It was hypothesized that the storage practices of firearms and poisons would be safer in homes where children live compared to homes in which children only visit. Because children often visit homes of older adults (e.g., babysitters, grandparents) where attention to child safety may be different and exposure to poisons such as medications greater, a secondary aim was to examine the poison and firearm storage practices in these homes compared to other homes children visit. The hypothesis was that storage practices would be safer or more consistent with AAP recommendations in homes without older adult residents.
Methods
Data were collected on 1003 respondents through telephone interviews over a period of 11 weeks (March to June 2002) using computer-assisted telephone interviewing (CATI). The sample was selected by the University of North Carolina Survey Research Unit. The sampling frame consisted of a database of active residential telephone numbers in the continental United States (i.e., excluding Alaska and Hawaii). A simple random sample of households was obtained through random digit dialing. Calls were made at different times of the day and on different days of the week; a maximum of 20 calls were made to selected numbers. Adults who answered the phone were interviewed, provided they met other study criteria, including age ≥18 years and English speakers, and having some role in making safety decisions for the household. Those living in group facilities where decisions about safety practices are often not made at the individual level were excluded (i.e., prisons, nursing homes, assisted living facilities, barracks, and dormitories).
Trained interviewers administered the 92-item questionnaire in an average of 10 minutes. Topics on the questionnaire related to safety issues and injury prevention practices in the home, sociodemographic characteristics of the household, and characteristics and location of the home. Respondents were asked whether they had any children aged 0 to 6 years living in the home. In a separate question, they were asked whether there were any children aged <6 years who lived in or visited the home at least once a year. This study was approved by the Institutional Review Board of the School of Public Health, at the University of North Carolina at Chapel Hill. Interviewers verbally obtained informed consent at the beginning of each call.
The sample for these analyses was restricted to households in which at least one child aged <6 years lived or visited at least once a year. Frequency distributions describe storage practices of firearms and poisonous substances. Cross-tabulations compare storage practices across characteristics of the respondents’ households. Household-level variables included presence of older adults, location of residence, home ownership status, gross household income, type of dwelling, region, and urbanicity. “Older adults” were defined as aged ≥70 years. “Urban/suburban” residence location was defined as in a metropolitan statistical area (MSA) or in a county containing a center city, whereas “not urban/suburban” meant being outside an MSA. “Don’t know” responses and refusals were coded as missing, and were excluded from the analyses. Results are reported as crude odds ratios with 95% confidence intervals.
Estimates were weighted to adjust for characteristics expected to be related to home safety practices, including: (1) the number of telephone lines per household, (2) the presence of children aged ≤6 years who lived in the home, (3) the presence of older adults, and (4) home ownership status. The weights allow the estimates to reflect the overall population of households in the continental United States. Data were analyzed using SAS software, version 8.2 (SAS Institute, Cary NC, 2002).
Results
A total of 1539 eligible individuals were invited to participate in the study, and interviews were completed with 1003 of these. There were 498 refusals; 38 incomplete interviews; 1144 unanswered calls for which eligibility could not be determined (e.g., no reply, line busy, answering machine response only after repeated callbacks); and 1942 ineligible numbers (e.g., number no longer in service, dedicated fax line, unable to communicate coherently and in English) for which calls were attempted. Under the assumption that the calls for which eligibility could not be determined had an eligibility proportion identical to the calls for which eligibility could be determined, the response rate was 50%.34
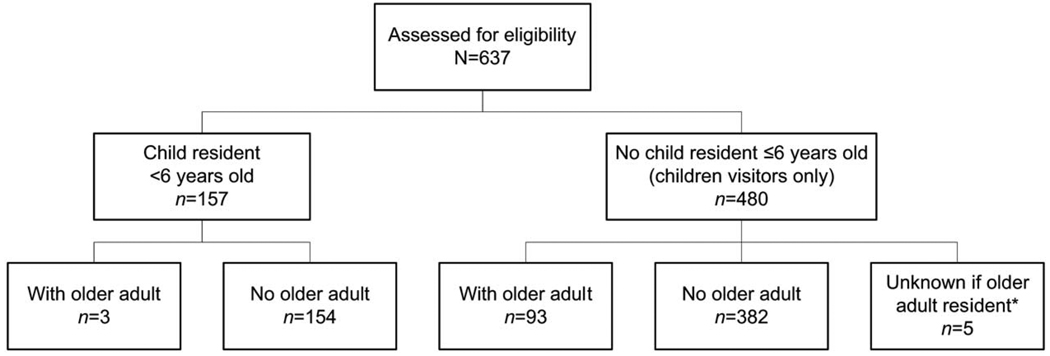
Of the 1003 households included in the original study, these analyses were restricted to the 637 in which children aged <6 years were residents or visitors (64%). There were older adults living in about 20% of homes in which children aged <6 were only visitors (93/480). In contrast, there were very few (n = 3) households with both older adults and young children living there. As shown in Figure 1, 480 (75%) of the households had children aged <6 who were visitors only, and about one fourth of households (n = 157) had residents aged <6. Fifteen percent of the 637 households had older adults (n =96).
Figure 1.
Sample size of study population overall and by subgroups, based on weighted data. *Missing data due to “don’t know” or “refused” responses.
The majority of respondents reported that they own the home in which they live, have a gross household income of ≥$35,000 per year, live in an urban or suburban area, and live in a house. Slightly more than one third of respondents reside in the South. Differences in household characteristics among households in which young children lived as compared to those homes where young children were visitors were minimal (Table 1).
Table 1.
Characteristics of respondents’ households, by presence of young children and older adults, United States, 2002a
| Characteristic | Children aged <6 live in homeb (n = 157) |
Children aged <6 visit home at least once a year | ||
|---|---|---|---|---|
| Total (n =480) |
Adults aged ≥70 (n =93) |
No adults aged ≥70 (n =382) |
||
| Home ownership | ||||
| Own | 64 | 73 | 79 | 73 |
| Rent | 36 | 27 | 21 | 27 |
| Region | ||||
| Northeast | 18 | 21 | 21 | 21 |
| West | 22 | 19 | 18 | 19 |
| Midwest | 24 | 28 | 25 | 28 |
| South | 36 | 32 | 36 | 32 |
| Household income | ||||
| ≥$35,000 | 67 | 66 | 50 | 69 |
| <$35,000 | 34 | 34 | 50 | 31 |
| Type of dwelling | ||||
| House | 68 | 70 | 71 | 70 |
| Other type of structurec | 32 | 30 | 29 | 30 |
| Urbanicity | ||||
| Urban/suburban | 83 | 72 | 67 | 72 |
| Rural/small town | 17 | 28 | 33 | 28 |
Values are percentages unless otherwise indicated. Percentages do not include missing data. Frequencies and percentages are based on weighted data.
Households where children live may or may not have children visiting.
Other types of household structures included apartments and apartment-type buildings, townhouses, duplexes, trailers, and manufactured or mobile homes.
Storage Behaviors
Poisonous substances and firearms were reportedly stored less securely in homes with children as visitors than in homes with resident children. Compared to respondents from homes with children residents, those in homes with children as visitors only had approximately two times higher odds of reporting medicines kept out in the open (38% vs 18%), stored in a purse (46% vs 33%), or unlocked (83% vs 78%). However, the difference between the two groups for storing medicines unlocked was not statistically significant. Similarly, households with child visitors only were more likely than homes with child residents to report storing household, shop, and garden chemicals unsafely (Table 2). Likewise, although reported firearm ownership was comparable between the two categories of households (33% vs 34%), homes in which children are only visitors were more likely to store firearms unlocked (56%) than homes in which children resided (33%) (OR = 2.57, confidence interval [CI] = 1.32–5.03) (Table 2). Among households without older adult residents in which children were visitors only, the odds of reported unsafe storage practices for poisonous substances or guns were two to three times higher than in homes without older adult residents where children resided (Table 3).
Table 2.
Household storage of poisonous substances and firearms, by whether young children live in or only visit the home, United States, 2002
| Storage practice | Children aged <6 live in homea n (%)b |
Children aged <6 only visit home n (%)b |
OR (95% CI)c |
|---|---|---|---|
| Total | 157/157 (100) | 480/480 (100) | |
| Poisons | |||
| Medicines in the open | 27/157 (18) | 183/480 (38) | 2.89 (1.84–4.54) |
| Medicines unlocked | 122/157 (78) | 400/479 (83) | 1.40 (0.89–2.19) |
| Medicines in a purse/pocketbook | 50/153 (33) | 218/476 (46) | 1.74 (1.18–2.54) |
| Household chemicals unlocked | 85/157 (55) | 354/480 (74) | 2.33 (1.60–3.39) |
| Shop or garden chemicals | |||
| Present | 76/156 (49) | 252/480 (52) | 1/16 (0.81–1.66) |
| Present and unlockedd | 43/75 (58) | 144/244 (59) | 1.04 (0.62–1.76) |
| Firearms | |||
| Present | 50/153 (33) | 159/469 (34) | 1.06 (0.72–1.57) |
| Present and not all locked upe | 16/50 (33) | 88/157 (56) | 2.57 (1.32–5.03) |
Households where children live may or may not have children visiting.
Denominators in certain cells may vary due to missing data. Frequencies and percentages are based on weighted data.
Odds of the storage practice in households with children aged <6 visiting versus living in home.
This question was restricted to households where shop/garden chemicals were present.
This question was restricted to households where firearms were present.
CI, confidence interval; OR, odds ratio.
Table 3.
Risk of unsafe storage of poisons and firearms by whether young children live in or only visit in homes without older adults, United States, 2002a
| Storage practice | Odds ratio (95% confidence interval) |
p valueb |
|---|---|---|
| Poisons | ||
| Medicines in the open | 2.82 (1.76–4.50) | <0.0001** |
| Medicines unlocked | 1.63 (1.02–2.62) | 0.0414* |
| Medicines in a purse/pocketbook | 1.91 (1.28–2.84) | 0.0014* |
| Household chemicals unlocked | 2.64 (1.78–3.92) | <0.0001** |
| Shop or garden chemicals unlocked | 1.04 (0.60–1.79) | 0.8945 |
| Firearms | ||
| Present | 0.96 (0.64–1.44) | 0.8556 |
| Not all locked up | 2.14 (1.21–4.82) | 0.0114** |
Results are based on weighted data.
Value based on Pearson’s chi-square test.
p<0.05 (bolded).
p<0.0001 (bolded).
It was expected that homes with older adults would have less safe storage practices than homes without older adults; however, this was not always the case and the differences were not statistically significant (Table 4). The majority of homes, regardless of the presence of older adults, reported medication and storage practices in which medications or household chemicals were not locked up, although fewer than half of each group indicated that medications are kept in the open. Interestingly, firearm ownership was higher in households containing older adults (42%) than those without older adults (32%), and this approached statistical significance. Proportionally more households with older adults reported storing their firearms unlocked compared to homes without older adults (61% vs 54%) (Table 4).
Table 4.
Storage of poisons and firearms in homes with young children as visitors only: comparison by presence or absence of older adults, United States, 2002a
| Storage practice | Older adults n (%) | No older adults n (%) | OR (95% CI) |
|---|---|---|---|
| Total | 93/93 (100) | 382/382 (100) | |
| Poisons | |||
| Medicines in the open | 40/93 (43) | 141/382 (37) | 1.30 (0.82–2.07) |
| Medicines unlocked | 70/92 (77) | 326/382 (85) | 0.58 (0.33–1.01) |
| Medicines in a purse/pocketbook | 37/92 (40) | 178/380 (47) | 0.75 (0.47–1.19) |
| Household chemicals unlocked | 62/93 (67) | 288/382 (75) | 0.65 (0.40–1.06) |
| Shop or garden chemicals | |||
| Present | 42/93 (45) | 209/382 (55) | 0.68 (0.43–1.06) |
| Present and unlockedb | 25/40 (63) | 117/202 (58) | 1.21 (0.61–2.44) |
| Firearms | |||
| Present | 38/90 (42) | 121/375 (32) | 1.50 (0.94–2.40) |
| Present and not all locked upc | 22/36 (61) | 66/121 (54) | 1.32 (0.62–2.82) |
Denominators in certain cells may vary due to missing data. Frequencies and percentages are based on weighted data.
This question was restricted to households where shop/garden chemicals were present.
This question was restricted to households where firearms were present.
CI, confidence interval; OR, odds ratio.
Discussion
These data demonstrate that children are at substantial potential risk from improperly stored poisonous substances and firearms in their own homes, yet may be at even greater risk in the homes they visit. Clearly, strategies are needed to improve the storage practices of both poisons and firearms to minimize in-home hazards to young children, and to eliminate the barriers to safe storage. Barriers that have been demonstrated to hinder injury prevention practices such as storage of poisons are living in substandard housing, limited financial resources, and inconvenience.26,29 Language and culture have also been demonstrated to be barriers. A study of Hispanic mothers revealed that they did not store their poisons safely because they did not have these hazardous substances in Mexico and did not recognize the agents as poisonous.29 Studies have demonstrated that individuals do not store their firearms safely because it is inconvenient and may hinder quick access to a firearm in case of an emergency.35,36 Firearm ownership for protection has been associated with unsafe firearm storage.30,37
The finding that high proportions of children may encounter potentially dangerous access to poisons and firearms in the homes they visit is important. This points to the need to encourage parents to investigate the safety practices in homes in which their children visit, whether other children live there or not. This message should be included when pediatricians and others provide guidance to parents, just as parents are encouraged to investigate practices of surrogate caretakers with respect to child passenger safety, dietary restrictions, or potential allergens. Recent campaigns organized by the American Academy of Pediatrics in collaboration with PAX:Real Solutions to Gun Violence stress the importance of asking about the presence and storage practices of guns in places where children play and visit.38 According to the data, this is particularly important, especially in homes where children do not reside but visit, which could include the homes of relatives (e.g., grandparents), babysitters, and friends. Likewise, the general public needs to be more attentive to storage issues of both poisons and firearms so as to prepare their homes for young visitors.
The presence of older adults in a household may affect the presence of household firearms. Homes with older adults in which children were visitors proportionally had more firearms present and poorer storage practices of firearms than homes without older adults. While these differences may not be statistically significant, they may be clinically relevant and represent a risk to children. These homes should not be ignored when recommendations are promoted to protect the safety of children in homes. In fact, the lack of familiarity with the behaviors of specific children who may visit only occasionally may be a particular issue in some of these homes.
Although not the focus of the investigation, the results also raise questions about the hazards for older children and adolescents who may engage in exploratory or suicidal behaviors, deliberately gaining access to either poisonous substances or to firearms in homes they visit. Firearms are the most common means of suicides, and in 2000 resulted in 55% of deaths among 10- to 24-year-olds (n = 2377), with poisonings resulting in 7% of deaths (n = 319).1 Although suicide by poisoning is generally more common among young females; the majority of female suicides are committed with firearms and the prevalence of firearm use among females in suicides has remained relatively constant in recent years.39
This study is limited due to the response rate, and self-reported information obtained by telephone without the opportunity to validate responses. Consequently, the reported storage habits are likely underestimates and the risks to children are potentially greater. In addition, the information obtained does not differentiate between loaded and unloaded firearms, nor does it identify homes in which injuries have occurred and in which there may be increased sensitivity to poison or firearm storage issues. Furthermore, questions were only asked of homes in which English was spoken and young children live or visit, and relatively few minorities or rural residents were interviewed. Thus, these results may not be generalizable to these populations. The risk of unsafe firearm storage is often greater for children aged 10 to 17 than for children <6. Also, the 0-to-6 age group has heterogeneous risks for some exposures. For example, medicines left on a counter top may be beyond the reach for many children aged <2, but not for 5- and 6-year-old children. Despite these limitations, this study may be the first to examine practices in homes that children visit, and to compare homes with and without older adult residents.
Many unanswered questions remain. For example, we cannot examine what could be substantial differences among households with respect to the frequency, duration, or nature of visits made by child visitors (e.g., staying overnight vs coming to play vs being supervised by parents while visiting). Also, more detailed queries about both poison storage practices and firearm storage would be illuminating to help determine if practices vary with respect to different age configurations in the home (e.g., children aged <3 years) or family size, or if homes that have experienced ingestions by children typically alter their practices. Likewise, more information about the storage of bullets or use of different methods of firearm storage that differentiate loaded from unloaded guns of varying types might help target intervention approaches for families with firearms. It would also be helpful to have more information about how storage practices evolve, and what types of psychosocial factors or educational messages have been influential in decision making about storage practices of both poisons and firearms.
Finally, although BB and pellet guns are not considered firearms and are not discussed here, there is increasing evidence that they can cause serious injuries that presumably could be amenable to the same types of storage interventions as firearms. Further investigation about safe storage as it relates to these guns may be warranted.
Because of the demonstrated risks of firearms and poisons, two common elements of the home environment, it is important that information about storage practices be understood and used to shape efforts aimed at improving safety for children both in the homes where they reside as well as in those where they are only visitors. Further research is needed to assess the magnitude of exposure and risk of firearm injury and poisoning to child visitors.
Acknowledgments
This work was funded by a contract from the Home Safety Council (HSC) to the University of North Carolina Injury Prevention Research Center, with additional support from the National Center for Injury Prevention and Control (R49/CCR402444). Additional support was provided in part by the William T. Grant Faculty Scholars Program and the Robert Wood Johnson Harold Amos Faculty Development Program (TCB), and the National Institute of Child Health and Human Development (RMJ). We wish to thank Anna Waller, ScD, Stephen W. Marshall, PhD, Carla Black, MPH, Daniel Macklin, MD, MPH, Jingzhen Yang, MPH, Ashley Bowers, MS, and Briana Webster for their work on the study. We also wish to thank David Oliver of the HSC and HSC consultants Deborah Girasek, MD, Guohua Li, MD, and Murray Katcher, MD, for their assistance in reviewing drafts of the survey instrument.
Footnotes
No financial conflict of interest was reported by the authors of this paper.
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based injury statistics query and reporting system. [Accessed April 2003]; Available at: www.cdc.gov/ncipc/wisqars.
- 2.Scheidt PC, Harel Y, Trumble AC, et al. The epidemiology of nonfatal injuries among U.S. children and youth. Am J Public Health. 1995;85:932–938. doi: 10.2105/ajph.85.7.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weil DS, Hemenway D. Loaded guns in the home: analysis of a national random survey of gun owners. JAMA. 1992;267:3033–3037. [PubMed] [Google Scholar]
- 4.Senturia YD, Christoffel KK, Donavan M. Children’s household exposure to guns: a pediatric practice-based survey. Pediatrics. 1994;93:469–475. [PubMed] [Google Scholar]
- 5.Stennies G, Ikeda R, Ledbetter S, et al. Firearm storage practices and children in the home, United States, 1994. Arch Pediatr Adolesc Med. 1999;153:586–590. doi: 10.1001/archpedi.153.6.586. [DOI] [PubMed] [Google Scholar]
- 6.Schuster M, Franke T, Bastian A, et al. Firearm storage patterns in U.S. homes with children. Am J Public Health. 2000;90:588–594. doi: 10.2105/ajph.90.4.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson RM, Coyne-Beasley T, Runyan CW. Firearm ownership and storage practices in the United States: a systematic review. Am J Prev Med. 2004;27:173–182. doi: 10.1016/j.amepre.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Litovitz TL, Klein-Schwartz W, White S, et al. 2000 Annual report of the American Association of Poison Control Centers Toxic Exposures Surveillance System. Am J Emerg Med. 2001;19:337–396. doi: 10.1053/ajem.2001.25272. [DOI] [PubMed] [Google Scholar]
- 9.Grossman DC, Reay DT, Baker SA. Self-inflicted and unintentional firearm injuries among children and adolescents: the source of the firearm. Arch Pediatr Adolesc Med. 1999;153:875–878. doi: 10.1001/archpedi.153.8.875. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics, Committee on Injury and Poison Prevention. Firearm related injuries affecting the pediatric population. Pediatrics. 2000;105:888–895. [PubMed] [Google Scholar]
- 11.American Academy of Pediatrics, Committee on Injury and Poison Prevention. Firearms and adolescents (RE9233) Pediatrics. 1992;89:784–787. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Fact sheet: “Poisoning prevention: safety tips for you and your family.”. [Accessed January 2003];Available at: www.cdc.gov/ncipc/factsheets/poisons_prevention.htm.
- 13.American College of Preventive Medicine. Preventing handgun injury: American College of Preventive Medicine position statement. Am J Prev Med. 2002;23:314–316. doi: 10.1016/s0749-3797(02)00520-2. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Family Physicians. AAFP selected policies on health issues: firearms/handguns. [Accessed August 10, 2002]; Available at: www.aafp.org/policy/49.html. [Google Scholar]
- 15.American College of Physicians. Firearm injury prevention: position paper. Ann Intern Med. 1998;128:236–241. [PubMed] [Google Scholar]
- 16.American College of Surgeons. Statement on firearm injuries. Bull Am Coll Surg. 2000;85:24. [PubMed] [Google Scholar]
- 17.Borowsky JW, Resnick MD. Adolescents and firearms: position paper of the society for adolescent medicine. J Adolesc Health. 1998;23:117–118. doi: 10.1016/s1054-139x(98)00072-x. [DOI] [PubMed] [Google Scholar]
- 18.Kellermann AL, Rivara FP, Rushforth NB, et al. Gun ownership as a risk factor for homicide in the home. N Engl J Med. 1993;329:1084–1091. doi: 10.1056/NEJM199310073291506. [DOI] [PubMed] [Google Scholar]
- 19.Kellermann AL, Reay D. Protection of peril? An analysis of firearm-related deaths in the home. N Engl J Med. 1986;314:1557–1560. doi: 10.1056/NEJM198606123142406. [DOI] [PubMed] [Google Scholar]
- 20.Brayden RM, MacLean WE, Jr, Bonfiglio JF, et al. Behavioral antecedents of pediatric poisonings. Clin Pediatr (Phila) 1993;32:30–35. doi: 10.1177/000992289303200106. [DOI] [PubMed] [Google Scholar]
- 21.U.S. General Accounting Office. Washington DC: General Accounting Office; 1991. Mar, Accidental shootings: many deaths and injuries caused by firearms could be prevented. [Google Scholar]
- 22.Vernick JS, O’Brien M, Hepburn LM, et al. Unintentional and underdetermined firearm related deaths: a preventable death analysis for three safety devices. Inj Prev. 2003;9:307–311. doi: 10.1136/ip.9.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwarz DF, Grisso JA, Miles C, et al. An injury prevention program in an urban African-American community. Am J Public Health. 1993;83:675–680. doi: 10.2105/ajph.83.5.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santer LJ, Stocking CB. Safety practices and living conditions of low-income urban families. Pediatrics. 1991;88:1112–1118. [PubMed] [Google Scholar]
- 25.Johnston BD, Britt J, D’Ambrosio L, et al. A preschool program for safety and injury prevention delivered by home visitors. Inj Prev. 2000;6:305–309. doi: 10.1136/ip.6.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gielen AC, Wilson MEH, Faden RR, et al. In-home injury prevention practices for infants and toddlers: the role of parental beliefs, barriers, and housing quality. Health Educ Q. 1995;22:85–95. doi: 10.1177/109019819502200108. [DOI] [PubMed] [Google Scholar]
- 27.Gielen AC, Wilson MEH, McDonald EM, et al. Randomized trial of enhanced anticipatory guidance for injury prevention. Arch Pediatr Adolesc Med. 2001;155:42–49. doi: 10.1001/archpedi.155.1.42. [DOI] [PubMed] [Google Scholar]
- 28.Coffman S, Martin V, Prill N, et al. Perceptions, safety behaviors, and learning needs of parents of children brought to an emergency department. J Emerg Nurs. 1998;24:133–139. doi: 10.1016/s0099-1767(98)90015-0. [DOI] [PubMed] [Google Scholar]
- 29.Mull DS, Agran PF, Winn DG, et al. Household poisoning exposure among children of Mexican-born mothers: an ethnographic study. Womens J Med. 1999;171:16–19. [PMC free article] [PubMed] [Google Scholar]
- 30.Coyne-Beasley T, McGee K, Johnson RM, et al. The association of handgun ownership and storage practices with safety consciousness. Arch Pediatr Adolesc Med. 2002;156:763–768. doi: 10.1001/archpedi.156.8.763. [DOI] [PubMed] [Google Scholar]
- 31.Bass JK, Ortega L, Rosales C, et al. What’s being used at home? A household pesticide survey. Pan Am J Public Health. 2001;9:138–144. doi: 10.1590/s1020-49892001000300002. [DOI] [PubMed] [Google Scholar]
- 32.Liller KD, Craig J, Crane N, et al. Evaluation of a poison prevention lesson for kindergarten and third grade students. Inj Prev. 1998;4:218–221. doi: 10.1136/ip.4.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith T. Chicago: National Opinion Research Center, University of Chicago; 2001. Dec, National gun policy survey of the National Opinion Research Center: research findings. 2001. [Google Scholar]
- 34.American Association for Public Opinion Research. 3rd ed. Lenexa KS: American Association for Public Opinion Research; 2004. Standard definitions: final dispositions of case codes and outcome rates for surveys. [Google Scholar]
- 35.Coyne-Beasley T, Johnson RM. Law enforcement officers’ opinions about gun locks: anchors on life jackets? Inj Prev. 2001;7:200–204. doi: 10.1136/ip.7.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coyne-Beasley T, Johnson RM, Charles LE, et al. Firearm storage practice of officers in a law enforcement agency in the south. Am J Prev Med. 2001;21:118–123. doi: 10.1016/s0749-3797(01)00327-0. [DOI] [PubMed] [Google Scholar]
- 37.Coyne-Beasley T, Schoenbach V, Johnson R. Love our kids, lock your guns. A community-based firearm safety counseling and gun lock distribution program. Arch Pediatr Adolesc Med. 2001;155:659–664. doi: 10.1001/archpedi.155.6.659. [DOI] [PubMed] [Google Scholar]
- 38.American Academy of Pediatrics. PAX and AAP team up again to send a critical summer message to parents: ask if there are guns where your children play. [Accessed April 16, 2003]; Available at: www.aap.org/advocacy/releasese/junepax.htm.
- 39.Romero MP, Wintemute GJ. The epidemiology of firearm suicide in the United States. J Urban Health. 2002;79:39–48. doi: 10.1093/jurban/79.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]