Abstract
OBJECTIVE
Schizophrenia (SZ) and Bipolar Disorder (BD) are associated with multidimensional disability. This study examined differential predictors of functional deficits between the disorders.
METHODS
Community dwelling individuals with SZ (N=161) or BD (N=130) were administered neuropsychological tests, symptom measures, performance-based social and adaptive (i.e., everyday-living skills) functional competence measures, and rated on domains of real-world functioning: 1) Community and Household activities, 2) Work skills, and 3) Interpersonal relationships. We used confirmatory path analysis to find the best fitting models to examine the direct and indirect (as mediated by competence) prediction of the three domains of real-world functioning.
RESULTS
In all models for both groups, neurocognition’s relationship with outcomes was largely mediated by competence. Symptoms were negatively associated with outcomes but unassociated with competence, with the exception of depression, which was a direct and mediated (through social competence) predictor in BD. In both groups, neurocognition was related to Activities directly and through a mediated relationship with adaptive competence. Work Skills were directly and indirectly (through mediation with social competence) predicted by neurocognition in SZ and entirely mediated by adaptive and social competence in BD. Neurocognition was associated with Interpersonal Relationships directly in the SZ group, and mediated by social competence in both groups.
CONCLUSIONS
Although there was greater disability in SZ, neurocognition predicted worse functioning in all outcome domains in both disorders. Our study supports the shared role of neurocognition in BD and SZ in producing disability, with predictive differences between disorders observed in domain-specific effects of symptoms and social and adaptive competence.
Chronic mental disorders such as schizophrenia (SZ) and bipolar disorder (BD) are among the most disabling illnesses worldwide (1-2). Neurocognitive impairment is widely recognized as a primary factor in causing and maintaining disability in SZ (3). Recent work has suggested that the relationship between neurocognition and real world psychosocial outcomes is largely indirect, mediated by variables such as everyday living skills (4), social competence (4), social cognition (6), symptoms (7), intrinsic motivation (8) and metacognition (9). Thus, neurocognitive impairments are important predictors of functional impairments in SZ, but most of the association with real world behaviors flows through their relationship with higher-order adaptive skill sets.
In contrast to the large body of research on the neurocognitive and psychopathological determinants of functional outcomes in SZ, substantially less information is available about the characteristics that contribute to the poor functional outcomes observed in BD (10, 11). Two large prospective studies (12, 13) indicate that depressive symptoms are more frequent and correlated with greater functional impairments than manic symptoms. Psychotic symptoms also contribute to disability, though they are not as prevalent in BD as they are in SZ (14). In recent years, research indicates that impairments in sustained attention, verbal memory, and executive functioning appear to persist in the absence of mood episodes (15) and are related to indices of social and vocational functioning; (16-22). However, the relative and combined contributions of neurocognitive abilities and symptoms to either functional competence or community functioning are unclear.
Additionally, studies of functioning in BD are limited by their reliance on subjective ratings of functioning, such as self-report measures, which have questionable validity in both disorders (23-24) and may be influenced by current mood state (25). Further, reliance on categorical milestones, such as employment, marriage, and independent living, may be limited by socioeconomic status and other contextual influences such as availability of jobs, ethnicity, and disability compensation status (26-27). Further, some cultures provide such significant social support that ability measures have no correlation with outcome (28) Thus, investigators are increasingly relying on more objective measures, such as performance-based assessment of functional capacity and third-party ratings of functional behavior, to provide objective estimates of functional competence and functional outcomes, respectively. To date, results from studies of those with SZ suggest that these competence measures mediate the relationship between neurocognitive impairment and observer-rated functional impairment(29). The few studies that employed performance-based measures of functional competence in BD (30-31), converge to suggest that neurocognition is a stronger predictor of functional competence than symptoms. However, these studies employed samples of middle-aged and elderly adults and did not extend the relationships to real world disability measures.
The present study is the first to extend our previous findings that suggested a relationship between neurocognition and real world behavior that is largely mediated by functional competence to a group of subjects with BD. Further, we have expanded the schizophrenia literature to a more age-diverse sample of outpatients.
METHODS
Participants
Inclusion criteria were DSM-IV diagnosis of Bipolar I Disorder (BD; N=130) or schizophrenia/schizoaffective disorder (SZ; N=161), based on structured interview, and living in the community. All participants were enrolled in a genetic study of schizophrenia and bipolar I disorder conducted by the Epidemiology-Genetics Program in Psychiatry at the Johns Hopkins School of Medicine. Current clinical symptom severity and mood state were not used as an inclusion or exclusion criteria.
The sample was restricted to full or mixed Ashkenazi Jewish background (determined from ancestry of four grandparents) in order to obtain a sample with increased genetic homogeneity. Initial recruitment was conducted nationally via advertisements in newspapers and Jewish publications, talks given at community centers and synagogues, and through the Epidemiology-Genetics Program website (32). Subjects participating in the genetic studies were directly assessed (largely in their own homes) by skilled clinicians (doctoral-level psychologists) using the Diagnostic Interview for Genetic Studies (33). Additional information from medical records, informant reports, and the Family Interview for Genetics Studies (http://zork.wustl.edu/nimh/home/m_interviews.html) was independently reviewed by at least two clinicians (Ph.D. or psychiatrist) prior to forming a consensus DSM-IV diagnosis, as well as consensus on a number of clinical indicators.
Recruitment and data collection methods were identical for both diagnostic groups. Participants from the parent genetics study were recruited via telephone and letter to participate in the current study, and, after providing written informed consent, were assessed in their own homes by members of the original team of clinical examiners. Participants were administered a battery of commonly used neuropsychological tests. The majority of the participants reported taking psychotropic medication (95.7% SZ, 86.9% BD), with expected differences between diagnostic groups in medication class (See Table 1).
Table 1.
Descriptive Statistics and Group Differences
| SZ | BPD | |||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | Range | M | SD | Range | ANOVA | ||
| Demographics | Age at Assessment | 49.9 | 9.6 | 16-78 | 48.4 | 14.3 | 18-80 | F(1,290)=1.0, p=.30 |
| Age at First Mental Health Treatment | 20.3 | 5.8 | 5-41 | 23.3 | 8.9 | 7-54 | F(1,253)=10.5, p=.001 | |
| Years of Education | 14.1 | 5.9 | 4-20 | 14.8 | 8.6 | 8-20 | F(1,290)=0.65, p=.41 | |
| Neurocognition | WRAT Reading Recognition Standard Score | 100.7 | 11.6 | 71-120 | 107.3 | 9.1 | 68-120 | F(1,290)=27.4, p<.001 |
| Rey Auditory Learning Test, Trials I-V | -1.74 | 1.3 | -5.6-2.1 | -0.59 | 1.2 | -3.8-2.1 | F(1,285)=53.7, p<.001 | |
| Trail Making Test, Part A | -2.35 | 1.7 | -5.0-.8 | -1.39 | 1.6 | -5.0-1.4 | F(1,290)=22.6, p<.001 | |
| Trail Making Test, Part B | -1.46 | 2.1 | -5.0-1.5 | -0.27 | 1.5 | -5.0-2.1 | F(1,290)=27.6, p<.001 | |
| WAIS Letter Number Sequencing | -0.59 | 1.1 | -3.0-2.0 | -0.01 | 1.1 | -3.0-3.0 | F(1,285)=20.2, p<.001 | |
| WAIS Digit Symbol | -1.00 | 0.8 | -2.6-1.0 | -0.20 | 1.1 | -2.6-3.0 | F(1,290)=45.4, p<.001 | |
| Semantic Fluency | -0.73 | 1.2 | -3.0-3.4 | -0.08 | 1.2 | -2.8-3.5 | F(1,289)=32.2, p<.001 | |
| Wisconsin Card Sorting Test, Perseverative Errors | -1.05 | 1.0 | -3.1-2.1 | -0.88 | 1.0 | -3.1-3.1 | F(1,278)=1.9, p=.16 | |
| Continuous Performance Test, D-prime | -1.61 | 1.2 | -5.9-1.2 | -0.91 | 1.1 | -3.4-1.5 | F(1,286)=22.4, p<.001 | |
| Neurocognitive Composite | -1.33 | 0.9 | -3.6-.51 | -0.54 | 0.8 | 2.7-1.0 | F(1,290)=54.3, p<.001 | |
| Psychopathology Symptoms | PANSS Negative, Mean Item Score (Range 1-7) | 2.3 | 1.1 | 1.0-6.0 | 1.5 | 0.6 | 1.0-4.3 | F(1,290)=71.8, p<.001 |
| PANSS Positive, Mean Item Score (Range 1-7) | 2.5 | 1.2 | 1.0-5.4 | 1.4 | 0.7 | 1.0-4.0 | F(1,290)=89.3, p<.001 | |
| Beck Depression Inventory (Range 0-63) | 10.9 | 9.4 | 0-41 | 9.8 | 10.2 | 0-45 | F(1,282)=1.1, p=.29 | |
| Profile of Mood States – Bipolar Version (T-Score) | 43.0 | 6.9 | 30-61.3 | 43.6 | 8.5 | 30.6-67.0 | F(1,260)=0.1, p=.72 | |
| Functional and Social Competence | UPSA-B (Range 0-20) | 15.3 | 3.9 | 3-20 | 17.7 | 2.4 | 4.0-20 | F(1,288)=40.3, p<.001 |
| Advanced Finances (Range 0-17) | 8.5 | 4.4 | 0-13 | 11.3 | 2.6 | 0-13 | F(1,282)=38.8, p<.001 | |
| Social Skills Performance Assessment (Range 0-5) | 3.9 | 1.1 | 1.1-5.0 | 4.3 | 0.4 | 3.1-5.0 | F(1,259)=15.8, p<.001 | |
| Real World Behavior | SLOF Interpersonal (Range 0-5) | 4.0 | 0.9 | 1.0-5.0 | 4.4 | 0.6 | 2.1-5.0 | F(1,291)=17.8, p<.001 |
| SLOF Activities (Range 0-5) | 4.3 | 0.7 | 1.6-5.0 | 4.6 | 0.4 | 2.0-5.0 | F(1,291)=25.6, p<.001 | |
| SLOF Work Skills Range (0-5) | 3.7 | 1.0 | 1.0-5.0 | 4.3 | 0.8 | 1.6-5.0 | F(1,291)=35.6, p<.001 | |
| % | N | % | N | Chi-Square | ||
| Demographics | Gender (% Female) | 37.9 | 61 | 49.2 | 64 | X2(1)=3.7, p=.052 |
| Ever Married | 23 | 37 | 54.6 | 71 | X2(1)=32.7, p<.001 | |
| First degree family member with Schizophrenia | 12.4 | 20 | 1.5 | 2 | X2(1)=8.5, p<.001 | |
| First degree family member with Bipolar Disorder | 2.4 | 4 | 32 | 41 | X2(1)=25.4, p<.001 | |
| Medications | Atypical Antipsychotic | 82.6 | 133 | 44.6 | 58 | X2(1)=46.0, p<.001 |
| Typical Antipsychotic | 18.6 | 30 | 4.6 | 6 | X2(1)=13.3, p<.001 | |
| Lithium | 8.7 | 14 | 30.8 | 40 | X2(1)=23.1, p<.001 | |
| Anticonvulsant | 29.2 | 47 | 52.3 | 68 | X2(1)=16.0, p<.001 | |
| Selective Serotonin Reuptake Inhibitor | 39.8 | 64 | 32.2 | 42 | X2(1)=1.7, p=.19 | |
| Tricyclic Antidepressant | 2.5 | 4 | 1.5 | 2 | X2(1)=0.3, p=.57 | |
| Anxiolytic | 18.6 | 30 | 15.4 | 20 | X2(1)=0.5, p=.46 | |
| Anticholinergic | 13 | 21 | 0.8 | 1 | X2(1)=15.5, p<.001 | |
| No Psychotropic Medication | 4.3 | 7 | 13.1 | 17 | X2(1)=7.2, p=.007 |
Note: Neurocognitive scores are represented as z-scores (M=0, SD=1; higher score indicates better performance) transformed relative to age-corrected normative data found in the manuals of each instrument, except WRAT Reading Score (M=100, SD=15; higher score indicates better performance) based on the age-corrected normative data in its manual. For all psychopathology symptom variables, higher scores indicate more severe symptomatology. For Neurocognitive, Competence, and Real World Behavior Scores, higher indicates better performance.
WRAT=Wide Range Achievement Test, 3rd Edition; WAIS=Wechsler Adult Intelligence Scale; PANSS=Positive and Negative Syndrome Scale; BDI; UPSA-B=University of California, San Diego Performance-Based Skills Assessment - Brief; SLOF=Specific Level of Functions Scale.
Measures
Independent Variables
Neurocognitive Composite Score
The neurocognitive battery included commonly used measures of verbal declarative memory, attention, verbal working memory, executive functioning, processing speed, and verbal fluency. We calculated a composite neurocognitive score using equally weighted standardized scores (z-scores; mean=0, standard deviation=1) that were derived from normative data from the manuals for each instrument. The composite neurocognitive score included the following eight variables: total learning from trials 1 through 5 on the Rey Auditory Verbal Learning Test (34), total time to complete Part A and Part B of the Trial Making Test (35), number of correct responses on the Letter Number Span test from the Wechsler Adult Intelligence Scale (WAIS; 36), Perseverative Errors Standard Score on from the 64-Card computerized Wisconsin Card Sorting Test (37), number of correct responses on the WAIS Digit Symbol Coding, total unique correct responses on a Semantic Fluency (38) test, and d-prime (a signal detection measure) from the Continuous Performance Test – Identical Pairs Version, 4-Digit condition (39). The Cronbach’s Alpha of the composite score was 0.84, indicating good internal consistency. We also examined differences between groups in estimated premorbid intelligence using the Wide Range Achievement Test (40) Reading Subtest.
Psychopathology Measures
We assessed depressive symptoms with the Beck Depression Inventory-II (BDI-II; 41), a 21-item questionnaire. A total depressive symptoms score is created by summing the 21 items (range 0 to 84).
The Profile of Mood States – Bipolar Version (42) provided an index of severity of manic symptoms. This self-report of current mood requires the participant to indicate, on a 4-point Likert scale (much unlike this, slightly unlike this, slightly like this, much like this) 72 items. Raw scores were converted to T-scores from normative data found in the manual. The total scale T-score was used as the mania variable, with higher scores indicating more severe manic symptoms (it should be noted that the T-scores are presented relative to the psychiatric outpatient sample, not a healthy comparison sample).
Severity of positive and negative symptoms was assessed using the Positive and Negative Syndrome Scale (43). This 30-item scale contains seven items measuring positive symptoms, seven items measuring negative symptoms, and sixteen items measuring general aspects of psychopathology and was completed after a structured interview by a psychologist and structured interview with an informant. We used the positive and negative domains from the empirically derived 5-factor model of the PANSS (44).
Proposed Mediators
We examined adaptive competence and social competence independently to observe whether they contributed differentially to the prediction of diverse outcomes. These measures had overlap (r2=.37) consistent with the correlation between the UPSA and neurocognitive performance in our previous research (4,5). The magnitude of this correlation suggests that these two ability areas are related, but separable areas of functional skills.
Adaptive Competence
We refer to adaptive competence as those instrumental skills that are important for functioning independently (45). An adaptive functional competence variable was created from an equally weighted composite of the brief version of the UCSD Performance-based Skills Assessment (UPSA-B; 46) and the Advanced Finances Test from the Everyday Functional Battery (EFB; 47); we call this composite measure the UPSA-B/EFB. In the UPSA-B, respondents are asked to role-play tasks in two areas of everyday functioning, communication and finances. The total raw score ranges from 0 to 20. In the Advanced Finances test (47), subjects perform higher level financial management skills than in the UPSA; these include depositing a check, paying three bills (including only a portion of the credit card bill in order to leave money in the account), and balancing a checkbook. Raw scores range from 0 to 17. The composite adaptive functional competence variable had adequate internal consistency (Coefficient alpha = .87). It was converted to a standard score ranging from 0-100 with higher scores indicating better adaptive competence.
Social Competence
Social competence (i.e., paralinguistic and verbal behaviors necessary for communication) was assessed with the Social Skills Performance Assessment (SSPA; 48). After a brief practice, the subjects initiate and maintain a conversation for three minutes in each of two situations: greeting a new neighbor and calling a landlord to request a repair for a leak that has gone unfixed. Affect and grooming are rated in person by the examiner; all other variables, such as interest, fluency, clarity, focus, negotiation ability, submissiveness/persistence, and social appropriateness were rated via audiotape by an offsite trained rater who was unaware of the study design, diagnosis, and all other data. The mean item score on these variables for both scenes was used in this study as the social competence variable, with higher scores indicating better social competence.
Outcome Variables
The Specific Level of Functioning Scale (SLOF, 49) was used to rate real world functional outcome. This 43-item observer-rated scale measures the following domains: Interpersonal Relationships (e.g., initiating, accepting and maintaining social contacts; effectively communicating), Participation in Community and Household Activities (shopping, using telephone, paying bills, use of public transportation), and Work Skills (e.g., employable skills, level of supervision required to complete tasks, ability to stay on task, completes tasks, punctuality). Note that the Work Skills domain comprises behaviors important for vocational performance, but is not a rating of behavior during employment. Ratings by the third-party informant are made on the basis of the amount of assistance required to perform real-world skills, or frequency of the behavior. Raters were selected who were familiar with the participant’s functioning (e.g., family members; friends; case managers). In the case that such individuals were unavailable, the examiner rated this information from their observations of and interactions with the subject. Twelve percent of the SZ group and 13% of the BD group were rated by the examiner on the SLOF. We ran multivariate analyses of variance for each group to determine whether there were differences on the three SLOF variables for those who were rated by an examiner. There were no statistically significant differences for either group on any of the subscales or demographic variables (all p-values>.05).
Statistical Analyses
We tested the direct and indirect predictors of the SLOF real world outcome domains with confirmatory path analyses in the separate diagnostic groups. Based on previous research (8,9), we predicted that neurocognition, the empirically-derived positive and negative symptom domains, and the total scores from the BDI, and POMS-BI as exogenous variables (i.e., variables that are not predicted directly by other variables) would predict each of the real world outcome domains. The two competence measures, the UPSA-B/EFB (adaptive competence) and SSPA (social competence) were hypothesized as mediating neurocognition but not symptom variables.
The final models were developed within each sample through an iterative procedure in which statistically non-significant paths with the smallest contribution to the outcome variable were sequentially eliminated from a saturated model (in which all variables are interrelated) until the best-fitting model was identified, defined by three different goodness of fit statistics, the model chi-square, the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). A good fitting model is reflected by non-significant chi-square tests, a CFI of greater than 0.90, and an RMSEA less than .08. The chi-square test is a comparison of the observed covariance matrix to the covariance matrix of the final model. The CFI compares the final model to an “independence model” and indicates the percent to which covariation in the data are replicable. The independence model is a null model that assumes that all variables are uncorrelated with the dependent variable. The RMSEA is a model fit measure that accounts for model complexity, thus promoting the most parsimonious model by considering degrees of freedom.
Diagnostic comparisons in the strength of neurocognition’s direct and mediated path coefficients for the competence and real world performance measures were performed by testing for the significance of the difference between coefficients. The total causal effects for the real world measures were determined with effects decomposition, where indirect effects are the factor of the coefficient from neurocognition to the competence measure and the competence measure to real world behavior. The total causal effect is the sum of all indirect effects and the direct effect.
RESULTS
The demographic, clinical characteristics, test performance, and functional ratings of the groups are presented in Table 1.
The final models produced adequate fit statistics for both groups across all three real world outcome domains, see Table 2. Neurocognition was associated with both competence variables, but only depressive symptom severity was associated with either competence variable. In both groups, neurocognition was related to Activities (See Figure 1; SZ R2=.53, BD R2=.39) directly and through a mediated relationship with adaptive competence. Negative symptoms and depression severity were negatively associated with Activities in SZ, while positive, negative, and manic symptoms were negatively associated with Activities in BD. Work skills (See Figure 2; SZ R2=.40, BD R2=.30) were directly and indirectly (through mediation with social competence) predicted by neurocognition in SZ, while neurocognition’s association with Work Skills in BD was entirely mediated by adaptive and social competence. Positive and negative symptoms were negatively associated with Work Skills in both groups; depressive symptoms further predicted poor Work Skills in the BD group. Interpersonal relationships (See Figure 3; SZ R2=.53, BD R2=.46) were indirectly (through social competence) predicted by neurocognition in both groups and directly by neurocognition, positive symptoms, and negative symptoms in SZ. In BD, Interpersonal Relationships were predicted by manic symptoms and by depressive symptoms, the latter of which had both a direct and mediated (through social competence) relationship.
Table 2.
Fit Statistics for the Independence and Final Models
| SZ | BPD | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| X2 | (df) | p-value | CFI | RMSEA | (90%CI) | X2 | (df) | p-value | CFI | RMSEA | (90%CI) | ||
| Interpersonal Functioning | Final Model | 11.6 | (8) | .17 | .991 | .03 | (.0-.08) | 16.2 | (13) | .23 | .967 | .04 | (.0-.09) |
| Independence Model | 328.1 | (21) | <.001 | .000 | .22 | (.20-.24) | 161 | (28) | <.001 | .000 | .19 | (.16-.22) | |
| Activities | Final Model | 8.9 | (7) | .25 | 1.000 | .00 | (.0-.12) | 15.7 | (13) | .27 | 1.000 | .00 | (.0-.11) |
| Independence Model | 261.8 | (15) | <.001 | .000 | .32 | (.28-.35) | 159 | (28) | <.001 | .000 | .22 | (.18-.25) | |
| Work Skills | Final Model | 9.5 | (8) | .30 | .976 | .04 | (.0-.09) | 13.4 | (11) | .27 | .994 | .02 | (.0-.11) |
| Independence Model | 169 | (21) | <.001 | .000 | .21 | (.18-.24) | 159 | (28) | <.001 | .000 | .19 | (.16-.21) | |
Figure 1.
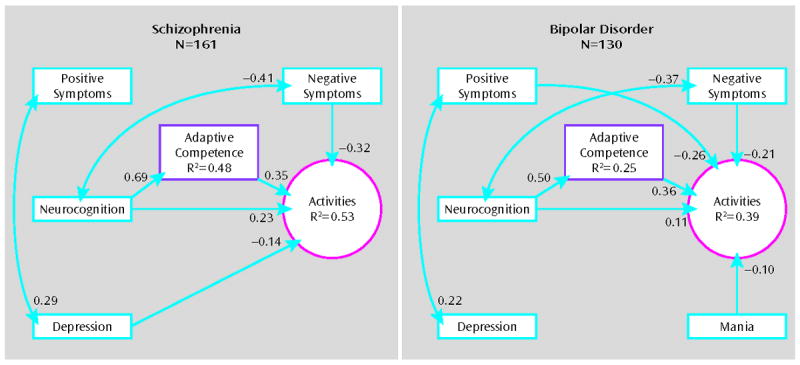
Prediction of Community and Household Activities in Schizophrenia and Bipolar Disorder.
Note: Bidirectional arrows represent correlated exogenous (i.e., variables without direct predictors) variables, represented as correlation coefficients. Unidirectional arrows represent regression beta weights. Variance accounted for is indicated within each the exogenous (i.e., variables with direct predictors) variables.
Figure 2.
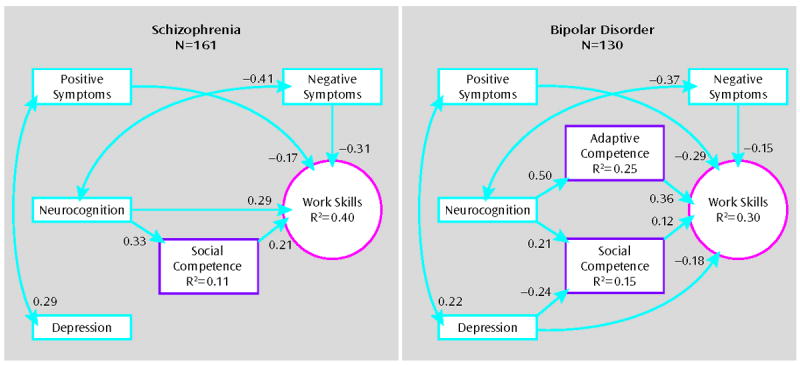
Prediction of Work Skills in Schizophrenia and Bipolar Disorder
Note: Bidirectional arrows represent correlated exogenous (i.e., variables without direct predictors) variables, represented as correlation coefficients. Unidirectional arrows represent regression beta weights. Variance accounted for is indicated within each the exogenous (i.e., variables with direct predictors) variables.
Figure 3.
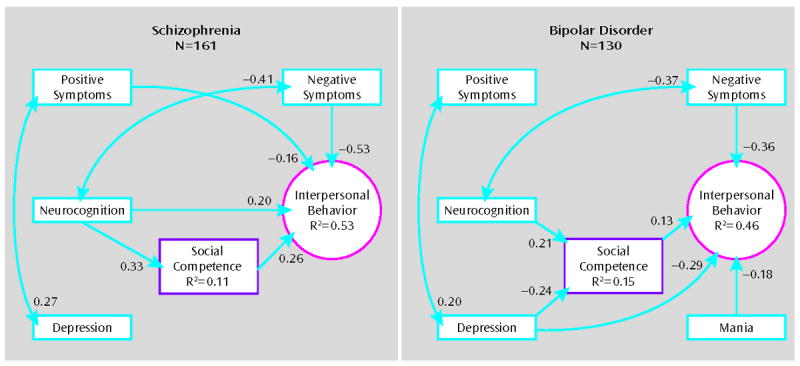
Prediction of Interpersonal Behavior in Schizophrenia and Bipolar Disorder
Note: Bidirectional arrows represent correlated exogenous (i.e., variables without direct predictors) variables, represented as correlation coefficients. Unidirectional arrows represent regression beta weights. Variance accounted for is indicated within each the exogenous (i.e., variables with direct predictors) variables.
The test for significant differences between coefficients revealed significant differences between the two diagnostic groups in the strength of the relationship of neurocognition with competence measures and real world behavior. In the Activities domain, the direct relationship of neurocognition was not significantly different between the groups (p=.15), but the total causal effect (direct + indirect effects) was significantly larger in SZ (.47) compared to BP (.29), p=.038. In this model, the strength of the path from neurocognition to adaptive competence was stronger in SZ, p=.006. Neurocognition was not a direct predictor of Work Skills in BP, and its total causal effect in this group (.20) was lower than SZ (.36), but this difference did not reach statistical significance (p=.07). The relationship of neurocognition with social competence was not significantly different between diagnostic groups (p=.14). Interpersonal behavior was not directly predicted by neurocognition in BP and its total causal effect (.027) was lower than in SZ (.29), p=.01.
DISCUSSION
The present results expand previous findings that modeled the direct and indirect relationships among neurocognitive, symptom, and functional competence measures with everyday outcomes in people with SZ and largely generalize to BD. That is, neurocognition has relationships with functioning that are both direct and mediated by adaptive and social competence. In contrast, clinical symptoms (with the exception of depressive symptoms) were related to functioning in the community but not with competence, suggesting that the effects of positive, negative, and manic symptoms on everyday behaviors might occur at a post-competence level, not affecting the ability to perform skilled acts, yet influencing the likelihood of performing these acts. These findings converge to suggest that we might observe persistent functional disability in schizophrenia and bipolar disorder even after an individual crosses traditional thresholds that would be considered a treatment success (i.e., a percentage reduction in positive symptom severity), as a result of neurocognitive and skill deficits. Conversely, even if an individual acquires certain skills but continues to experience mild levels of core (i.e., positive and negative) and non-specific (i.e., depressed) symptoms, changes in real world behavior might lag or not manifest at all.
The results of this study suggest that the paths from clinical factors to real world disability were consistent in a number of important ways in subjects with SZ versus BD, even with differences between disorders in the severity of these real world deficits. Neurocognition clearly has an important role in functional outcomes across both disorders, though the direct and total effects are larger in SZ. In contrast to a previous study with older SZ (4), the present study found more evidence for direct effects of neurocognition on work skills and interpersonal behavior, perhaps related to the greater age range or larger sample size. To our knowledge, no study had examined whether functional competence measures mediate the link between neurocognition and disability in bipolar disorder; our data suggest that the mediation role of these measures in bipolar disorder may actually be more pronounced than in schizophrenia, with most of the relationship between cognition and real-world outcomes outcome mediated by competence. Thus, the path from neurocognitive deficit to functional disability is stronger and more direct in SZ, but still quite relevant in BD.
The role of symptoms in predicting disability was significant, but generally unmediated by competence measures, and somewhat different in BD compared to SZ. Similar to previous studies and not surprising given their diagnostic importance, depressive and manic symptoms were associated with real world functional performance deficits in bipolar disorder, with manic symptoms having an inverse relationship with activities in the home and community, depression negatively associated with work skills, and both types of mood symptoms associated with poorer interpersonal behavior. Similar to previous reports in BD (12, 13), depressive symptoms were stronger predictors of poor outcomes than manic symptoms. The positive symptom associations with outcomes in this BD sample might indicate that, although less frequent and severe in BD, when present, positive symptoms are more disruptive in this condition with a more cyclical manifestation of psychosis. Negative symptoms are infrequently reported in the BD literature, limiting our interpretation of the present findings. It is unlikely that the relationship is an artifact of measurement overlap with depressive symptoms; depression and negative symptom total scores had a small, non-significant relationship in this sample and previous work has indicated that measurement of depressive symptoms with the BDI does not substantially overlap with negative symptoms (50).
The present findings are supported by other reports that suggest depressive symptoms are important predictors of disability in BD (12, 51). An interesting deviation across the two diagnostic groups was the path from symptoms of depression to real world outcomes. In bipolar disorder, but not schizophrenia, depression was associated with social competence and its relationship with interpersonal behavior and work skills was partially mediated by this relationship. Thus, in BD, depressive symptoms may serve as a potential rate limiter of real world behavior and also a phasic suppressor of social skills. Alternatively, poor social skills may produce a vulnerability to depression. It would be important for future research to investigate the intra-individual trajectories of social skills and depression in BD to understand the direction of causal relationships. Such knowledge would be useful in adapting rehabilitation approaches to bipolar disorder.
There are several limitations to this study. The sample was restricted to a culturally homogenous group. Participants were outpatients and on average experiencing mild symptoms. Therefore, the generalizability of these findings to ethnically diverse populations, or inpatients and/or more acutely ill patients, is limited. Some studies (20) have demonstrated relationships of specific neurocognitive domains to functional deficits that differed by diagnosis; although our sample size was considerable, it was not sufficiently powered to evaluate each neurocognitive test individually in the statistical procedure used. For some individuals with BD, there will be a ceiling effect for the functional competence and outcome domains and future research should determine how sensitive these measures and others are for the more subtle functional deficits. Additionally, it will be important to assess more domains of functioning and to continue to search for optimal methods for assessing disability in chronic mental disorders. Like efforts to refine our assessment of outcomes in SZ (52), our understanding of the severity and predictors of disability in BD would be enhanced by similar endeavors. Finally, this study was cross-sectional; future work examining the sources of intra-individual variability in functional abilities over time is needed to declare causal effects of illness characteristics on long term functioning outcomes.
In summary, our findings generalize multivariate path models linking neurocognitive ability, functional competence and symptoms with real world functional performance to BD and confirm previous models in SZ. Disability is multiply determined, with the effect of neurocognition mediated by functional capacity, and a separable and more direct effect of symptoms. Diagnostic group differences largely concern the strength of the relationships and which symptoms most influence disability, and our study reaffirms the broad debilitating role of bipolar depression in maintaining disability. These results suggest that recent advances in measurement of cognitive and functional abilities in schizophrenia may be quite relevant to measurement of disability and related rehabilitative efforts in BD. As opposed to SZ, there has been little emphasis in pharmacological or non-pharmacological cognitive remediation in BD, and few examples of rehabilitative programs aimed at functional skills targeting bipolar disorder (11). Our results support the suggestion that models for cognitive rehabilitation underway in SZ (53) should be adapted for BD (54).
Acknowledgments
Funding Sources:
Funding for the study presented in this manuscript was provided by the National Institute of Mental Health (NIMH) through award R01MH079784 (to Ann Pulver, ScD). Additional support was provided by NIMH grants RO1MH78775 to Dr. Harvey and NIMH Grant number R01MH078737 to Dr. Patterson.
Dr. Bowie has served on a scientific advisory board and as a consultant for Abbott Pharmaceuticals in the past year. In the past year, Dr. Harvey has served as a consultant to: Eli Lilly and Company, Johnson and Johnson, Merck and Company, Shire Pharma, Dainippon Sumitomo America and he has received grant support from Astra Zeneca.
Footnotes
Disclosures:
All other authors report no financial relationships with commercial interests.
References
- 1.Lopez A, Mathers C, Ezzati M, Murray C. Global burden of disease and risk factors. World bank publications; Washington D.C: 2006. [PubMed] [Google Scholar]
- 2.Ormel J, Petukhova M, Chatterji S, Aguilar-Gaxiola S, Alonso J. Disability and treatment of specific mental and physical disorders. British Journal of Psychiatry. 2008;192:368–375. doi: 10.1192/bjp.bp.107.039107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 4.Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163(3):418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- 5.Bowie CR, Leung WW, Reichenberg A, McClure MM, Patterson TL, Heaton RK, Harvey PD. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008;63(5):505–511. doi: 10.1016/j.biopsych.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sergi MJ, Rassovsky Y, Nuechterlein KH, Green MF. Social perception as a mediator of the influence of early visual processing on functional status in schizophrenia. Am J Psychiatry. 2006;163(3):448–454. doi: 10.1176/appi.ajp.163.3.448. [DOI] [PubMed] [Google Scholar]
- 7.Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113(2-3):189–199. doi: 10.1016/j.schres.2009.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: testing mediator and moderator effects. Schizophr Res. 2008;105(1-3):95–104. doi: 10.1016/j.schres.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Koren D, Seidman LJ, Goldsmith M, Harvey PD. Real-world cognitive--and metacognitive--dysfunction in schizophrenia: a new approach for measuring (and remediating) more “right stuff”. Schizophr Bull. 2006;32(2):310–326. doi: 10.1093/schbul/sbj035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green MF. Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry. 2006;67:e12. [PubMed] [Google Scholar]
- 11.Wingo AP, Harvey PD, Baldessarini RJ. Neurocognitive impairment in bipolar disorder patients: functional implications. Bipolar Disord. 2009;11:113–125. doi: 10.1111/j.1399-5618.2009.00665.x. [DOI] [PubMed] [Google Scholar]
- 12.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, Coryell W, Maser JD, Keller MB. Psychosocial disability in the course of bipolar I and II disorders: a prospective, comparative, longitudinal study. Arch Gen Psychiatry. 2005;62:1322–1330. doi: 10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- 13.Post R, Leverich GS, Altshuler LL, Frye MA, Suppes TM, Keck PE, Jr, McElroy SL, Kupka R, Nolen WA, Grunze H, Walden J. An overview of recent findings of the Stanley Foundation Bipolar Network (Part I) Bipolar Disord. 2003;5:310–319. doi: 10.1034/j.1399-5618.2003.00051.x. [DOI] [PubMed] [Google Scholar]
- 14.Huxley N, Baldessarini RJ. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9:183–196. doi: 10.1111/j.1399-5618.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- 15.Bearden CE, Hoffman KM, Cannon TD. The neuropsychology and neuroanatomy of bipolar affective disorder: a critical review. Bipolar Disord. 2001;3:106–150. doi: 10.1034/j.1399-5618.2001.030302.x. discussion 151-103. [DOI] [PubMed] [Google Scholar]
- 16.Altshuler L, Tekell J, Biswas K, Kilbourne AM, Evans D, Tang D, Bauer MS. Executive function and employment status among veterans with bipolar disorder. Psychiatr Serv. 2007;58:1441–1447. doi: 10.1176/ps.2007.58.11.1441. [DOI] [PubMed] [Google Scholar]
- 17.Altshuler LL, Bearden CE, Green MF, van Gorp W, Mintz J. A relationship between neurocognitive impairment and functional impairment in bipolar disorder: a pilot study. Psychiatry Res. 2008;157:289–293. doi: 10.1016/j.psychres.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 18.Dickerson FB, Boronow JJ, Stallings CR, Origoni AE, Cole S, Yolken RH. Association between cognitive functioning and employment status of persons with bipolar disorder. Psychiatr Serv. 2004;55:54–58. doi: 10.1176/appi.ps.55.1.54. [DOI] [PubMed] [Google Scholar]
- 19.Jaeger J, Vieta E. Functional outcome and disability in bipolar disorders: ongoing research and future directions. Bipolar Disord. 2007;9(1-2):1–2. doi: 10.1111/j.1399-5618.2007.00441.x. [DOI] [PubMed] [Google Scholar]
- 20.Laes JR, Sponheim SR. Does cognition predict community function only in schizophrenia?: a study of schizophrenia patients, bipolar affective disorder patients, and community control subjects. Schizophr Res. 2006;84(1):121–131. doi: 10.1016/j.schres.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 21.Martinez-Aran A, Vieta E, Torrent C, Sanchez-Moreno J, Goikolea JM, Salamero M, Malhi GS, Gonzalez-Pinto A, Daban C, Alvarez-Grandi S, Fountoulakis K, Kaprinis G, Tabares-Seisdedos R, Ayuso-Mateos JL. Functional outcome in bipolar disorder: the role of clinical and cognitive factors. Bipolar Disord. 2007;9:103–113. doi: 10.1111/j.1399-5618.2007.00327.x. [DOI] [PubMed] [Google Scholar]
- 22.Tabarés-Seisdedos R, Balanzá-Martínez V, Sánchez-Moreno J, Martinez-Aran A, Salazar-Fraile J, Selva-Vera G, Rubio C, Mata I, Gomez-Beneyto M, Vieta E. Neurocognitive and clinical predictors of functional outcome in patients with schizophrenia and bipolar I disorder at one-year follow-up. J Affect Disord. 2008;109:286–299. doi: 10.1016/j.jad.2007.12.234. [DOI] [PubMed] [Google Scholar]
- 23.Bowie CR, Twamley EW, Anderson H, Halpern B, Patterson TL, Harvey PD. Self-assessment of functional status in schizophrenia. J Psychiatr Res. 2007;41(12):1012–1018. doi: 10.1016/j.jpsychires.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burdick KE, Endick CJ, Goldberg JF. Assessing cognitive deficits in bipolar disorder: are self-reports valid? Psychiatry Res. 2005;136(1):43–50. doi: 10.1016/j.psychres.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Dean BB, Gerner D, Gerner RH. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in bipolar disorder. Curr Med Res Opin. 2004;20(2):139–154. doi: 10.1185/030079903125002801. [DOI] [PubMed] [Google Scholar]
- 26.Drake RE, Fox TS, Leather PK, Becker DR, Musumeci JS, Ingram WF, McHugo GJ. Regional variation in competitive employment for persons with severe mental illness. Adm Policy Ment Health. 1998;25(5):493–504. [Google Scholar]
- 27.Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, Stroup S, Hsiao JK, Lieberman J CATIE Study Investigators Group. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163(3):411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- 28.Harvey PD, Helldin L, Bowie CR, Heaton RK, Olsson AK, Hjarthag F, Norlander T, Patterson TL. Performance-based measurement of functional disability in schizophrenia: a cross-national study in the United States and Sweden. Am J Psychiatry. 2009;166(7):821–827. doi: 10.1176/appi.ajp.2009.09010106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Twamley EW, Doshi RR, Nayak GV, Palmer BW, Golshan S, Heaton RK, Patterson TL, Jeste DV. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am J Psychiatry. 2002;159:2013–2020. doi: 10.1176/appi.ajp.159.12.2013. [DOI] [PubMed] [Google Scholar]
- 30.Gildengers AG, Butters MA, Chisholm D, Rogers JC, Holm MB, Bhalla RK, Seligman K, Dew MA, Reynolds CF, Kupfer DJ, Mulsant BH. Cognitive functioning and instrumental activities of daily living in late-life bipolar disorder. Am J Geriatr Psychiatry. 2007;15:174–179. doi: 10.1097/JGP.0b013e31802dd367. [DOI] [PubMed] [Google Scholar]
- 31.Depp CA, Cain AE, Palmer BW, Moore DJ, Eyler LT, Lebowitz BD, Patterson TL, Jeste DV. Assessment of medication management ability in middle-aged and older adults with bipolar disorder. J Clin Psychopharmacol. 2008;28:225–229. doi: 10.1097/JCP.0b013e318166dfed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fallin MD, Lasseter VK, Avramopoulos D, Nicodemus KK, Wolyniec PS, McGrath JA, Steel G, Nestadt G, Liang KY, Huganir RL, Valle D, Pulver AE. Bipolar I disorder and schizophrenia: a 440-single-nucleotide polymorphism screen of 64 candidate genes among ashkenazi jewish case-parent trios. Am J Hum Genet. 2005;77:918–936. doi: 10.1086/497703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nurnberger JI, Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, Reich T. Diagnostic interview for genetic studies. Rationale, unique features, and training NIMH Genetics Initiative. Arch Gen Psychiatry. 1994;51:849–859. doi: 10.1001/archpsyc.1994.03950110009002. [DOI] [PubMed] [Google Scholar]
- 34.Schmidt M. Rey Auditory and Verbal Learning Test: A handbook. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- 35.Reitan RM, Wolfson D. The Halstead-Reitan neuropsychological test battery: Theory and clinical interpretation. 2. Tucson, AZ: Neuropsychology Press; 1993. [Google Scholar]
- 36.Wechsler D. WAIS-IV: Technical and Scoring Manual. San Antonio, TX: Pearson; 2008. [Google Scholar]
- 37.Heaton RK, Chellune CJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test Manual-Revised and expanded. Odessa, FL: Psychological Assessment Resources; 1993. [Google Scholar]
- 38.Spreen O, Strauss E. A compendium of neuropsychological tests and norms. 2. New York, NY: Oxford University Press; 1998. [Google Scholar]
- 39.Cornblatt BA, Risch NJ, Faris G, Friedman D, Erlenmeyer-Kimling L. The Continuous Performance Test, identical pairs version (CPT-IP): I. New findings about sustained attention in normal families. Psychiatry Res. 1988;26(2):223–238. doi: 10.1016/0165-1781(88)90076-5. [DOI] [PubMed] [Google Scholar]
- 40.Jastak S. Wide range achievement test. 3. San Antonio, TX: Wide Range Inc; 1993. [Google Scholar]
- 41.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory: II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 42.Lorr M, McNair DM. Manual. Profile of Mood States. Bipolar Form. San Diego, CA: Educational and Industrial Testing Service; 1968. [Google Scholar]
- 43.Kay SR, Fiszbein A, Opler LA. The Positive And Negative Syndrome Scale (PANSS) for schizophrenia. Schiz Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 44.White L, Harvey PD, Opler L, Lindenmayer JP. Empirical assessment of the factorial structure of clinical symptoms in schizophrenia. A multisite, multimodel evaluation of the factorial structure of the Positive and Negative Syndrome Scale. The PANSS Study Group. Psychopathology. 1997;30(5):263–74. doi: 10.1159/000285058. [DOI] [PubMed] [Google Scholar]
- 45.Mausbach BT, Bowie CR, Harvey PD, Twamley EW, Goldman SR, Jeste DV, Patterson TL. Usefulness of the UCSD Performance-based Skills Assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. Journal of Psychiatric Research. 2008;42:320–327. doi: 10.1016/j.jpsychires.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- 47.Heaton RK, Marcotte TD, Mindt MR, Sadek J, Moore DJ, Bentley H, McCutchan JA, Reicks C, Grant I HNRC Group. The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychological Soc. 2004;10:317–331. doi: 10.1017/S1355617704102130. [DOI] [PubMed] [Google Scholar]
- 48.Patterson TL, Moscona S, McKibbin CL, Davidson K, Jeste DV. Social skills performance assessment among older patients with schizophrenia. Schizophr Res. 2001;48:351–360. doi: 10.1016/s0920-9964(00)00109-2. [DOI] [PubMed] [Google Scholar]
- 49.Schneider LC, Streuening EL. SLOF: A behavioral rating scale for assessing the mentally ill. Social Work Research and Abstracts. 1983;6:9–21. doi: 10.1093/swra/19.3.9. [DOI] [PubMed] [Google Scholar]
- 50.Chemerinski E, Bowie C, Anderson H, Harvey PD. Depression in schizophrenia: methodological artifact or distinct feature of the illness? J Neuropsychiatry Clin Neurosci. 2008;20(4):431–440. doi: 10.1176/appi.neuropsych.20.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Simon GE, Bauer MS, Ludman EJ, Operskalski BH, Unutzer J. Mood symptoms, functional impairment, and disability in people with bipolar disorder: specific effects of mania and depression. J Clin Psychiatry. 2007;68:1237–1245. doi: 10.4088/jcp.v68n0811. [DOI] [PubMed] [Google Scholar]
- 52.Leifker FR, Patterson TL, Heaton RK, Harvey PD. Validating Measures of Real-World Outcome: The Results of the VALERO Expert Survey and RAND Panel. Schizophr Bull. doi: 10.1093/schbul/sbp044. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Green MF, Nuechterlein KH. The MATRICS initiative: developing a consensus cognitive battery for clinical trials. Schizophr Res. 2004;72(1):1–3. doi: 10.1016/j.schres.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 54.Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sachs GS, Thase ME, Calabrese JR, Marangell LB, Ostacher MJ, Patel J, Thomas MR, Araga M, Gonzalez JM, Wisniewski SR. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: results from a 9-month randomized controlled trial. Am J Psychiatry. 2007;164(9):1340–1347. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]


