Abstract
Background
Flail chest (FC) results in paradoxical chest wall movement, altered respiratory mechanics, and frequently respiratory failure. Despite advances in ventilatory management, FC remains associated with significant morbidity and mortality. Operative fixation of the flail segment has been advocated as an adjunct to supportive care, but no definitive clinical trial exists to delineate the role of surgery.
Objective
To perform a systematic review and meta-analysis of studies comparing operative to nonoperative therapy in adult FC patients. Outcomes were duration of mechanical ventilation (DMV), intensive care unit length of stay (ICULOS), hospital length of stay (HLOS), mortality, incidence of pneumonia, and tracheostomy.
Methods
A comprehensive search of 5 electronic databases was performed to identify randomized controlled trials and observational studies (cohort or case-control). Pooled effect size (ES) or relative risk (RR) was calculated using a fixed or random effects model, as appropriate.
Results
Nine studies with a total of 538 patients met inclusion criteria. Compared to control treatment, operative management of FC was associated with shorter DMV (pooled ES −4.52; days, 95% confidence interval [CI] −5.54, −3.50), ICULOS (−3.40 days; 95% CI −6.01,−0.79), HLOS (−3.82 days; 95% CI −7.12,−0.54), and decreased mortality (pooled RR 0.44; 95% CI 0.28, 0.69), pneumonia (0.45; 95% CI 0.30, 0.69), and tracheostomy (0.25; 95% CI 0.13, 0.47).
Conclusions
As compared to nonoperative therapy, operative fixation of FC is associated with reductions in DMV, LOS, mortality, and complications associated with prolonged MV. These findings support the need for an adequately powered clinical study to further define the role of this intervention.
Introduction
Flail chest (FC), defined as fracture of 3 or more sequential ribs at multiple sites, results in paradoxical chest wall movement, altered respiratory mechanics, and frequently respiratory failure.1 Despite advances in ventilatory management, patients with FC typically require prolonged ventilatory support and lengthy ICU and hospital stays. Although present in a minority of patients who sustain blunt trauma,2-4 FC is associated with significant morbidity, mortality, and resource expenditure.
Standard treatment of FC includes aggressive pulmonary toilet, pain control, and ventilatory support.1 Operative fixation of the flail segment has been advocated as an adjunct to these supportive measures, allowing for early restoration of chest wall integrity and respiratory mechanics.1 Numerous studies examining a variety of clinical endpoints, trial designs, and patient populations have been reported.5-14 This heterogeneous body of literature has produced conflicting results as to the benefits and risks of operative management in the setting of FC. Despite continued interest by the surgical community, no definitive clinical trial exists to delineate the role of surgery in patients with FC. As a result, approaches to patient management vary widely.15
We undertook this meta-analysis to synthesize relevant studies comparing operative and non-operative management of FC. Understanding whether operative rib fixation is beneficial, ascertaining the magnitude of the benefit, and determining the patient populations most appropriate for this procedure will provide critical components for the design of an informative phase III study.
Methods
This analysis was performed consistent with recommendations from the Cochrane Collaboration and Meta-analysis of Observational Studies in Epidemiology guidelines.16, 17 A priori, we developed a protocol outlining our research question, outcome measures, search strategy, study inclusion/exclusion criteria, and methods of data extraction and analysis.
Study Identification
We searched MEDLINE (1966-2012), Embase (1947-2012), Scopus (all years), Cochrane Databases and ClinicalTrials.gov (all limited to English, Human Studies) using MeSH terms and key words associated with 3 primary categories: flail chest, operative management, and study design (Table 1). The latest search was performed in February 2012. Citation lists were independently reviewed by two authors (J.A.L., L.E.) to identify relevant studies. Titles and abstracts were screened, and articles were retrieved if potentially relevant. The reference lists of retrieved papers were also screened to identify additional studies.
Table 1.
MeSH Terms and Keywords in Search Strategy
| Category | Search Strategy |
|---|---|
| Flail Chest | “Rib Fractures”[Mesh] OR
“Flail Chest”[Mesh] OR “Rib Fracture” OR
“Rib Fractures” OR “costal fracture” OR
“flail thorax” OR “thorax flail” OR “Flail Chest” OR “Stove in Chest” OR “Stove-in Chest” |
| Operative Management | “General Surgery”[Mesh] OR
“Surgical Procedures, Operative”[Mesh] OR
“surgery”[Subheading] OR “surgery” OR
“operative” OR “operating” OR “operation” OR operate* OR “invasive procedures” OR “invasive procedure” OR “surgical” OR “resection” |
| Study Design | “Controlled Clinical
Trial”[Publication Type] OR “Randomized Controlled
Trial”[Publication Type] OR Groups[tiab] OR trial[tiab] OR randomly[tiab] OR randomized[tiab] OR grouped[tiab] OR group[tiab] OR “Case-Control Studies”[Mesh] OR “Retrospective Studies”[Mesh] OR “Retrospective Studies” OR “Case-Control Studies” OR “Case-Control Study” OR “Case-Comparison Studies” OR “Case Comparison Studies” OR “Case-Comparison Study” OR “Case-Compeer Studies” OR “Case Compeer Studies” OR “Case- Compeer Study” OR “Case-Referrent Studies” OR “Case Referrent Studies” OR “Case-Referrent Study” OR “Case-Referent Studies” OR “Case Referent Studies” OR “Case-Referent Study” OR “Case-Base Studies” OR “Case Base Studies” OR “Case-Base Study” OR “Case Control Studies” OR “Case Control Study” OR “Retrospective Study” OR “matched case control” OR “ex post facto design” OR “retrospective design” OR “retrospective panel studies” OR “retrospective panel study” |
Study Selection and Outcomes
All randomized controlled trials (RCTs), cohort, and case-control trials involving adult patients with predominantly FC comparing operative (any method) to non-operative therapy were eligible for inclusion. Flail Chest was defined as ≥ 3 consecutive ribs fractured in ≥ 2 places. Primary outcome was duration of mechanical ventilation (DMV); secondary outcomes were intensive care unit length of stay (ICULOS), hospital length of stay (HLOS), mortality, incidence of pneumonia, and rate of tracheostomy. Studies were included if they reported data on the primary outcome of interest. Case series were included if they were reported as all sequential patients with FC and if both operative and nonoperative patient groups were described, as these studies also fit the definition of a retrospective cohort. We excluded case reports, case series which did not fit the criteria for retrospective cohort design, review articles, editorials, or studies which did not report data on our outcomes of interest. Studies were considered for inclusion by two authors (J.A.L, L.E.), with any disagreements resolved by senior authors (B.D.F, G.A.C).
Data Extraction and Quality Assessment
Articles which met inclusion/exclusion criteria underwent quality assessment and data extraction using a standardized data collection form. The following data was extracted: authors, journal, year of publication, country of origin, and type of study design. The following data regarding each arm was also recorded: number of patients, average age, average Injury Severity Score (ISS), number of events (deaths, pneumonia, tracheostomy), average DMV, average ICU LOS, and average HLOS. When reported, standard deviations and p-values were recorded for continuous variables.
We assessed study quality based on a 27-point metric created for quality assessment of both randomized and nonrandomized studies.18 Aspects of study design assessed were data reporting, internal and external validity, and statistical analysis. The cutoffs for quality were determined by dividing the possible 27 points into quartiles. A score of 22 or above was designated as high quality, 15-21 indicated moderate quality, 7-14 indicated fair quality, and 6 or below was categorized as a low quality study. Two authors (J.A.L, L.E) assessed the studies and high inter-rater reliability was observed.
Statistical Analysis
While a number of approaches to operative management for FC have been described, small numbers of patients treated by a given method precluded us from assessing for differences among techniques. Patients undergoing operative management of any type were pooled. Endpoints of interest were not uniformly reported by all studies. Analysis for each outcome was conducted using only studies which reported data for that outcome.
Inconsistencies in data reporting necessitated conversion of the continuous outcomes into the difference between the means of the operative group and nonoperative group, or effect size (ES), and standard error of the effect size (SE[ES]).19 The SE[ES] was calculated through the identification of the t-score from a t-table using the degrees of freedom of the study based upon the sample size and the p-value. The ES was divided by the obtained t-score to determine the standard error of the effect size. The formula is summarized as follows:
.
For studies without exact p-values, but which stated results that were non-significant (p>0.05), we used the t-value associated with a p = 0.1 for our calculation. For studies reporting significant results (p<0.05), we used the t-value associated with a p=0.05 for our calculation. Studies reporting outcomes where neither p-values nor standard errors were described were excluded from analysis.
Heterogeneity was assessed using χ2 (Cochran Q statistic) and quantified using I2. I2 values <25% were considered low heterogeneity; I2 values between 25% and 50% were considered moderate heterogeneity; I2 values >50% were considered high heterogeneity.20 In the absence of significant heterogeneity (p<0.05), a fixed effects model (Mantel-Haenszel method) was used to calculate pooled ES with 95% confidence interval (CI) for continuous outcomes or log relative risk (RR) with 95% CI for categorical outcomes.21 If significant heterogeneity was present, a random effects model (DerSimonian and Laird method) was used.22 Outcomes with significant heterogeneity as determined by χ2 and high heterogeneity as quantified by I2 were explored for possible sources of heterogeneity by random-effects meta-regression.23 Potential sources of heterogeneity explored included study quality (continuous quality score), patient age, and ISS. We assessed publication bias using funnel plots and Egger test.24,25 Sensitivity analyses were performed to evaluate the robustness of pooled estimates. Individual studies were removed in an iterative fashion and the meta-analysis was repeated to determine the influence of each study on the pooled estimate and 95% CI. All analyses were performed using STATA 10.1 (Stata, College Station, TX).
Results
Study Identification, Selection, and Quality Assessment
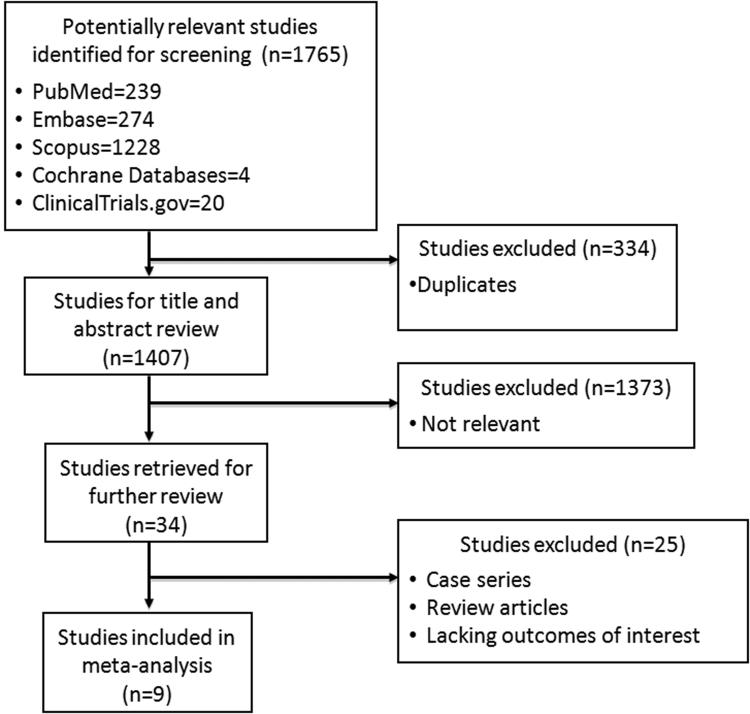
A total of 1,407 articles were retrieved (Figure 1). Reasons for study exclusion were lack of relevance (n=1373), ineligible study design (n=21), and failure to report outcomes of interest (n=4). Nine studies (2 RCTs, 4 cohort studies, 3 case-control studies) met inclusion criteria.5-13 These studies, which enrolled 538 patients receiving either operative fixation (n=219) or nonoperative treatment (n=319) of FC, were of moderate quality (mean (±STD) quality score 19 (±2.8)). Common quality deficiencies included selection bias and incomplete reporting of important confounders, data, patient follow-up, or statistical methods. Characteristics of studies included in our analysis are summarized in Table 2.
Figure 1.
Flow diagram of study selection for meta-analysis.
Table 2.
Characteristics of Studies Comparing Operative to Nonoperative Management of Flail Chest
| Author (Year) | Location | Study Design | n: Operative Patients |
n: Nonoperative Patients |
Outcomes Reported | Timing of Operative Intervention |
Quality Rating* |
|---|---|---|---|---|---|---|---|
| Ahmed et al (1995) | UAE | Cohort | 26 | 38 | DMV, ICULOS, mortality, TRCH |
12-24 hrs after ICU admission |
Fair |
| Karev (1997) | Ukraine | Cohort | 40 | 93 | DMV, PNA mortality | Within 24 hrs of
hospital admission |
Moderate |
| Voggenreiter et al (1998) | Germany | Cohort | 20 | 22 | DMV, PNA, mortality | Not specified | Moderate |
| Tanaka et al (2002) | Japan | RCT | 18 | 19 | DMV, ICULOS, PNA, TRCH |
Mean 8.2 ± 4.1 days
after admission; randomized d 5 |
Moderate |
| Balci et al (2004) | Turkey | Cohort | 27 | 37 | DMV, HLOS, mortality, TRCH |
All but 2 patients within 48 hrs of hospital admission |
Moderate |
| Granetzny et al (2005) | Egypt | RCT | 20 | 20 | DMV, ICULOS, HLOS, mortality |
24-36 hrs after ICU admission; randomized 24 hrs after admission |
High |
| Nirula et al (2006) | USA | Case-control | 30 | 30 | DMV, ICULOS, HLOS | Mean 3 d after hospital admission |
Moderate |
| Althausen et al (2011) | USA | Case-control | 22 | 28 | DMV, ICULOS, HLOS, PNA, TRCH |
Mean 2.3 d after
hospital admission |
Moderate |
| de Moya et al (2011) | USA | Case-control | 16 | 32 | DMV, ICULOS, HLOS, PNA |
Mean 5 d after hospital admission |
Moderate |
RCT, randomized control trial; DMV, duration of mechanical ventilation; ICULOS, intensive care unit length of stay; HLOS, hospital length of stay; PNA, pneumonia; TRCH, tracheostomy; hrs, hours; d, days
see Methods section, Data Extraction and Quality Assessment, for detail on determination of Quality Rating
Clinical Outcomes
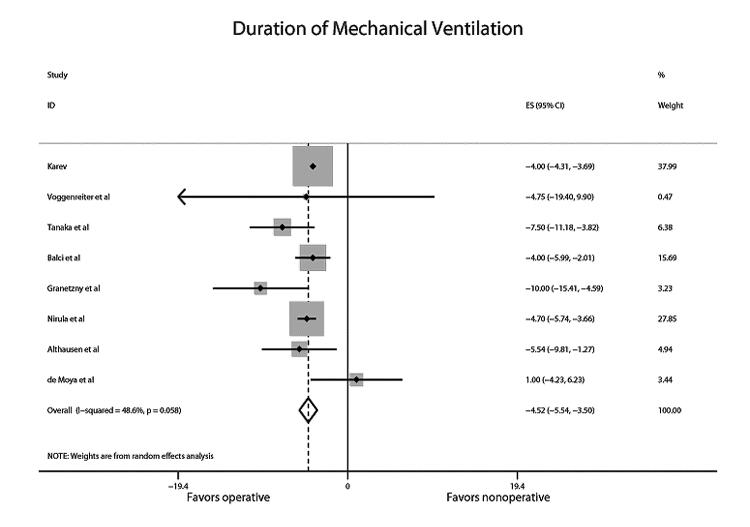
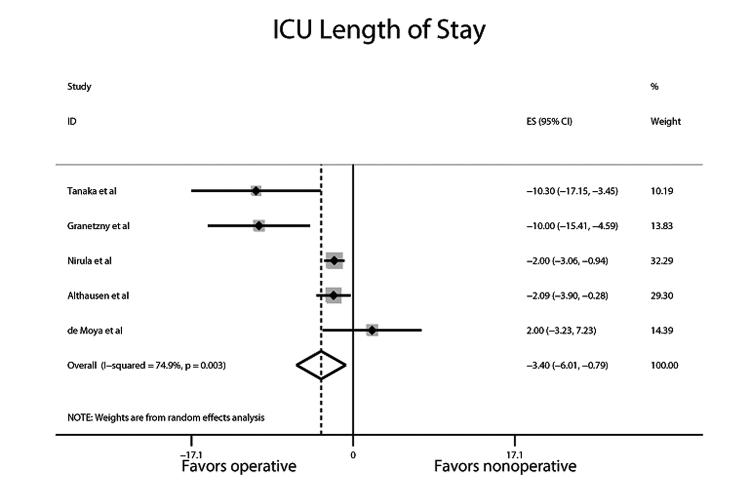
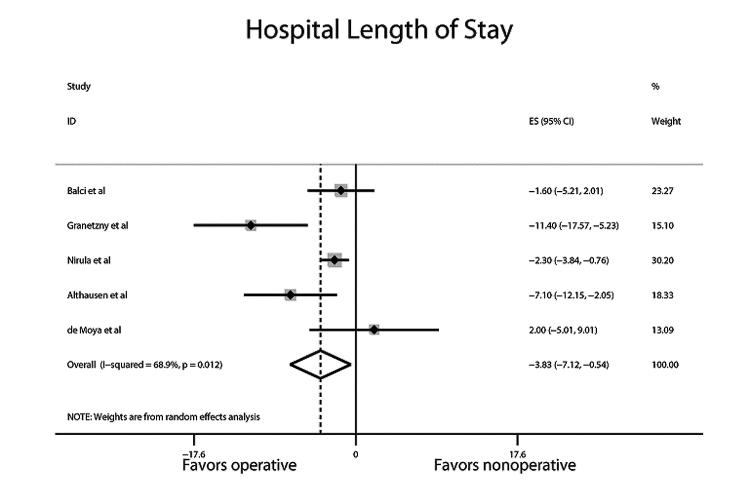
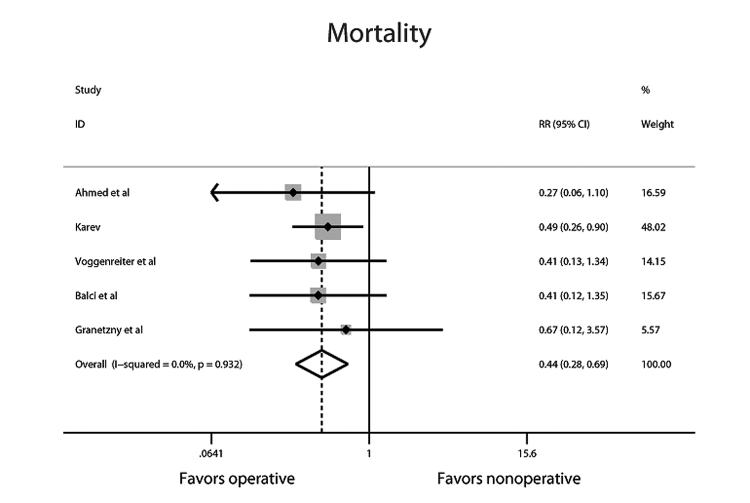
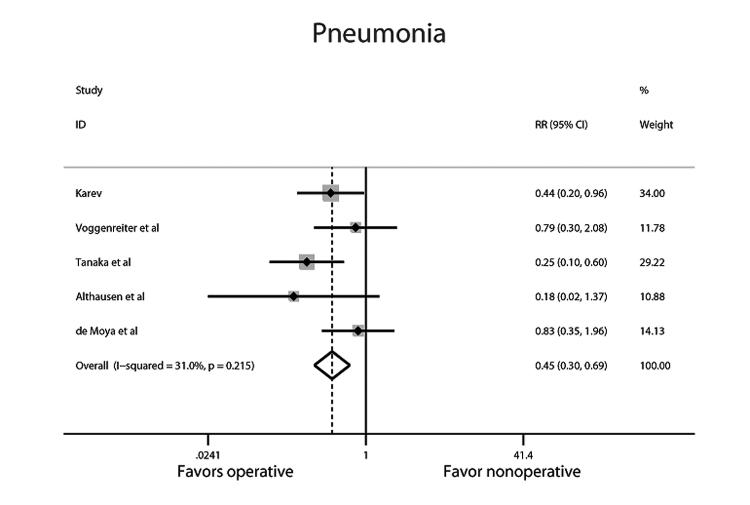
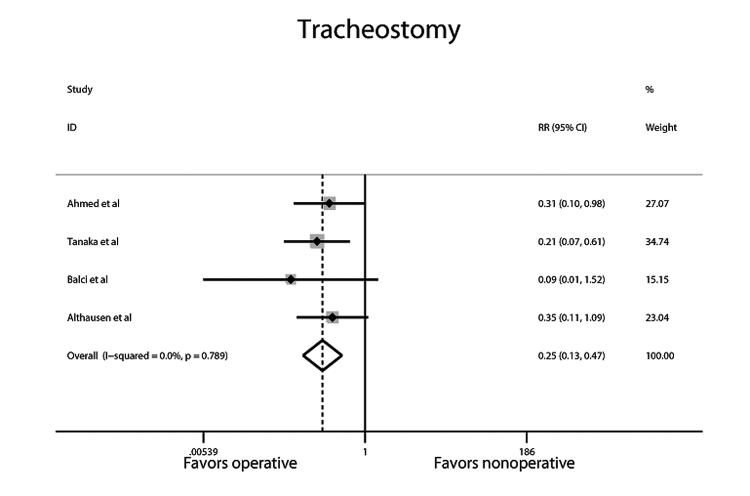
Compared with non-operative treatment, operative management of FC was associated with reductions in DMV (pooled ES −4.52; 95% CI −5.54, −3.50; Figure 2), ICU LOS (pooled ES − 3.40, 95% CI −6.01, −0.80; Figure 3), HLOS (pooled ES −3.83 days, 95% CI −7.12, −0.54; Figure 4), mortality (pooled RR 0.43, 95% CI 0.28-0.69; Figure 5), pneumonia (pooled RR 0.45, 95% CI 0.29-0.67; Figure 6), and use of tracheostomy (pooled RR 0.25, 95% CI 0.13-0.47; Figure 7). Although statistically significant heterogeneity was not present for the outcome of DMV (χ2=13.62, p=0.058; I2=48.6), a random effects model was used due to a p-value approaching significance. Heterogeneity was not statistically significant among studies in the analyses for mortality (χ2=0.85, p=0.932; I2=0), pneumonia (χ2=5.79, p=0.215; I2=31) or tracheostomy (χ2=1.05, p=0.789; I2=0). Significant heterogeneity was present among studies in the analysis for both ICU LOS (χ2=15.96, p=0.003; I2=74.9) and HLOS (χ2=12.87, p=0.012; I2=68.9). A summary of clinical outcomes is provided in Table 3.
Figure 2.
Forest plot of the pooled effect size (ES) in days for the outcome duration of mechanical ventilation (DMV). Pooled ES is −4.52 days; 95% confidence interval −5.54, −3.50. χ2 for heterogeneity=13.62, p=0.058, I2=48.6.
Figure 3.
Forest plot of the pooled effect size (ES) in days for the outcome ICU length of stay (ICULOS). Pooled ES is −3.4 days; 95% confidence interval −6.01, −0.80. χ2 for heterogeneity=15.96, p=0.003; I2=74.9.
Figure 4.
Forest plot of the pooled effect size (ES) in days for the outcome hospital length of stay (HLOS). Pooled ES is −3.83 days, 95% confidence interval −7.12, −0.54. χ2 for heterogeneity=12.87, p=0.012; I2=68.9.
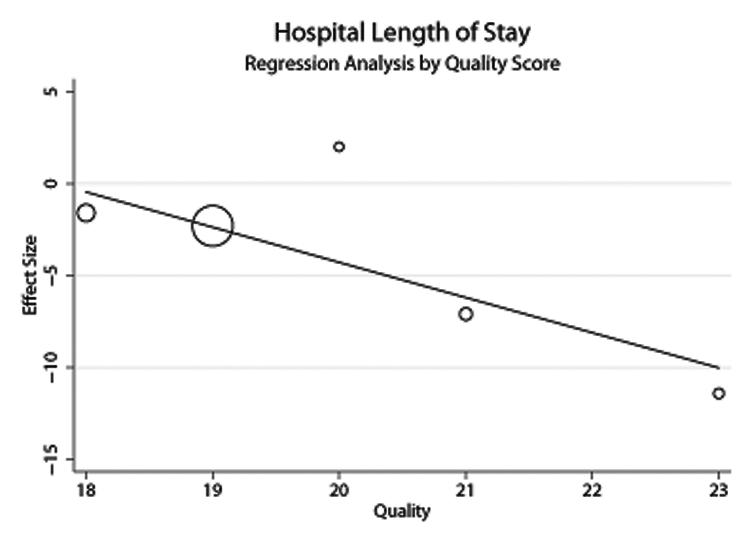
Figure 5.
Random effects regression model of the impact of total quality score on hospital length of stay (HLOS). Residual I2 after adjusting for total quality score=20.98
Figure 6.
Forest plot of the pooled relative risk (RR) for the outcome of mortality. Pooled RR is 0.43, 95% confidence interval 0.28-0.69. χ2 for heterogeneity=0.85, p=0.932; I2=0.
Figure 7.
Forest plot of the pooled relative risk (RR) for the outcome of pneumonia. Pooled RR is 0.45, 95% confidence interval 0.29-0.67. χ2 for heterogeneity=5.79, p=0.215; I2=31.
Table 3.
Pooled Estimates of Average Benefit of Operative vs. Nonoperative Management of Flail Chest
| Outcome | Risk Estimates Pooled Estimate |
95% CI | Tests of Heterogeneity | ||
|---|---|---|---|---|---|
| Χ2 value | p value* | I2 value | |||
| Duration of Mechanical
Ventilation (DMV) |
−4.52 days | −5.54, −3.50 | 13.62 | 0.058 | 48.6 |
| Intensive Care Unit Length of
Stay (ICULOS) |
−3.40 days | −6.01, −0.79 | 15.96 | 0.003 | 74.9 |
| Hospital Length of Stay (HLOS) |
−3.82 days | −7.12, −0.54 | 12.87 | 0.012 | 68.9 |
| Mortality | RR 0.44 | 0.28, 0.69 | 0.85 | 0.932 | 0.0 |
| Pneumonia | RR 0.45 | 0.30, 0.69 | 5.79 | 0.215 | 31.0 |
| Tracheostomy | RR 0.25 | 0.13, 0.47 | 1.05 | 0.789 | 0.0 |
p value for Χ2 test of heterogeneity
To explore possible sources of this heterogeneity, regression analyses were performed using age, ISS and quality score as covariates. Heterogeneity present for ICU LOS was not explained by age, ISS or quality score. However for HLOS, 48% of the heterogeneity was explained by the continuous quality score (Residual I2=20.98, Figure 8), indicating studies with higher quality were more likely to report a larger effect size.
Figure 8.
Forest plot of the pooled relative risk (RR) for the outcome of tracheostomy. Pooled RR is 0.25, 95% confidence interval 0.13-0.47. χ2 for heterogeneity=1.05, p=0.789; I2=0.
We were also able to calculate overall rates for the outcomes of mortality, pneumonia, and tracheostomy. For all patients with FC, overall rates were 27% for mortality, 31% for pneumonia, and 26% for tracheostomy. When stratified by operative versus nonoperative therapy, rates for mortality were 14% and 36%, rates for pneumonia were 18% and 39%, and rates for tracheostomy were 10% and 39%, respectively.
Publication Bias
Presence of publication bias was evaluated separately for each outcome. No evidence of publication bias was present for any outcome as assessed by visual inspection of funnel plots or Egger test (data not shown).
Sensitivity Analysis
Sensitivity analyses were performed separately for each outcome. Analyses for the outcomes of DMV, mortality, pneumonia, and tracheostomy demonstrated no significant change to the overall estimate with sequential removal of studies. However, sensitivity analyses for both ICU LOS and HLOS demonstrated significant changes in the combined estimate with serial removal of studies (data not shown).
Discussion
In 2009, Mayberry et al14 published a survey targeting trauma, orthopedic, and thoracic surgeons in the US on their opinions regarding indications for operative repair of rib and sternal fractures. One-third of respondents reported that operative management of FC was warranted after failure to wean from mechanical ventilation at 7 days, and an additional 29% felt that operative management was indicated for failure to wean at 14 days. Only 8% of surgeons felt operative management was indicated for patients with FC who did not require mechanical ventilation. Given this lack of consensus, we undertook this meta-analysis to determine if there was a net favorable or detrimental effect for this procedure. Our findings suggest that operative management in this context has beneficial effects on morbidity, mortality, and resource expenditure. We found that operative management was associated with 4.5 fewer days of mechanical ventilation, 3.4 fewer days in the ICU, and almost 4 fewer days in the hospital relative to patients managed nonoperatively. Additionally, operative stabilization was associated with >50% reductions in mortality, incidence of pneumonia, and use of tracheostomy. There are several important factors that our study was not designed to address, principal among these is timing of the intervention. In theory, ‘early’ surgical intervention—within 24-72 hours of injury—would provide the most benefit to patients with FC in terms of avoidance of prolonged mechanical ventilation and associated complications. In contrast, use of surgical intervention later in the time course of disease might result in marginal benefit while exposing patients to procedural risks. Time to surgical stabilization varied in the studies included our analysis from ≤24 hours to >8 days after admission. Determining optimal timing of intervention will be a critical element in design of a phase III study.
We were unable to assess the potential role of operative management of FC in the subset of patients with concurrent pulmonary contusion. Patients with FC complicated by pulmonary contusion may require mechanical ventilation due to a combination of pulmonary dysfunction and altered respiratory mechanics, such that potential improvement in respiratory mechanics with operative fixation is not sufficient to significantly affect ventilator weaning. Voggenreiter et al found that patients with pulmonary contusion who underwent operative fixation had similar DMV to patients with pulmonary contusions managed non-operatively.7 Althausen et al reported similar findings.12 Due to limited data reporting and small sample sizes, we were unable to perform subset analysis in patients with pulmonary contusion.
We targeted patients with 3 or more rib fractures producing a flail segment; patients with fewer rib fractures may not benefit from operative intervention. One study in our analysis, by de Moya et al, produced point estimates that favored non-operative management, although the difference between the operative and nonoperative groups was not significant.13 The lack of benefit seen for DMV and LOS outcomes in the study by de Moya et al may have resulted from the inclusion of patients with less severe chest wall injuries—only 75% of the operative group was classified by the authors as having FC or severe chest wall deformity. Additionally, the authors found no difference in narcotics usage between the 2 groups, indicating that operative management may not be beneficial for the sole indication of pain management.
We were unable to determine the optimal approach for rib fracture fixation. Multiple techniques have been described, including use of metal plates7, 12, 13, 26-34, absorbable plates35-42, intramedullary fixation5, 6, 10, 43, Judet struts7, 8, 44-46, and U-plates47. The studies included in our analyses represent a wide range of surgical techniques, and individual studies often employed more than one surgical technique. These surgical approaches may differ greatly in terms of their efficacy and safety. As with any surgical procedure, operative fixation of rib fractures is associated with the risk of complications such as wound infection, hardware failure or migration, and malunion/ nonunion of the fracture site. We were unable to assess the magnitude or frequency of potential harms associated with operative management of FC; only 3 of our included studies reported complications. Both efficacy and potential harms must be considered when determining the optimal technique for rib fracture fixation. Additionally, the small number of patients in our analyses treated with each technique necessitated pooling of all patients who received operative therapy into one group. We were therefore unable to assess superiority of any one technique.
We detected significant heterogeneity for two of the outcomes in our analysis, ICULOS and HLOS. We explored this heterogeneity by examining the contribution of age, ISS, and study quality. For ICULOS, observed heterogeneity could not be explained by any of these factors. In contrast, for HLOS, nearly one-half of study variability was attributable to study quality. An inherent limitation of meta-analyses is that the strength of the findings is dependent on the quality of the underlying studies. The studies included in our analyses were of moderate to lower quality. However, the slope of our meta-regression was favorable: higher quality studies were more likely to report a greater benefit associated with operative management, relative to lower quality studies. Based on the results of our meta-regression, it is reasonable to estimate that a future high quality study would demonstrate a significant difference in HLOS comparing operative and non-operative patients.
Conclusion
Meta-analyses are often exploratory and hypothesis-generating, and not intended to guide clinical practice. While our findings suggest that operative management in the setting of FC is associated with significant effects on morbidity, mortality, and resource expenditure, they require prospective validation in a thoughtfully designed and appropriately powered clinical investigation. In addition to examining patient selection, timing, and technique, a future study should standardize other facets of care that may similarly impact outcomes (e.g., protocols to guide ventilator weaning and sedation).49, 50 If our findings are confirmed in such a fashion, operative fixation in the setting of FC may become a standard approach to managing a problematic clinical entity.
Acknowledgments
We would like to thank Susan Fowler for her expertise and assistance with our literature search.
Foundation: This work was supported by NIH 5T32GM00879510
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Simon B, Ebert J, Bokhari F, et al. [6/12/12];Practice Management Guideline for Pulmonary Contusion-Flail Chest. EAST Practice Management Workgroup for Pulmonary Contusion-Flail Chest. 2006 Jun; Accessed online www.east.org.
- 2.Champion HR, Copes WS, Sacco WJ, et al. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990 Nov;30(11):1356–65. [PubMed] [Google Scholar]
- 3.Borman JB, Aharonson-Daniel L, Savitsky B, Peleg K. Unilateral flail chest is seldom a lethal injury. Emerg Med J. 2006 Dec;23(12):903–5. doi: 10.1136/emj.2006.037945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lafferty PM, Anavian J, Will RE, et al. Operative Treatment of Chest Wall Injuries: Indications, Technique, and Outcomes. J Bone Joint Surg Am. 2011;93(1):97–110. doi: 10.2106/JBJS.I.00696. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed Z, Mohyuddin Z. Management of Flail chest injury: internal fixation vs endotracheal intubation and ventilation. J Thorac Cardiovasc Surg. 1995;110:1676–80. doi: 10.1016/S0022-5223(95)70030-7. [DOI] [PubMed] [Google Scholar]
- 6.Karev DV. Operative Management of the Flail Chest. Wiad Lek. 1997;50(Suppl 1 Pt 2):205–8. [PubMed] [Google Scholar]
- 7.Voggenreiter G, Neudeck F, Aufmkolk M, et al. Operative chest wall stabilization in flail chest - Outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998;187:130–8. doi: 10.1016/s1072-7515(98)00142-2. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization or internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–32. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Balci AE, Eren S, Cakir O, et al. Open fixation in flail chest. Asian Cardiovasc Thorac Ann. 2004;12:11–15. doi: 10.1177/021849230401200104. [DOI] [PubMed] [Google Scholar]
- 10.Granetzny A, El-Aal MA, Emam E, et al. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4:583–87. doi: 10.1510/icvts.2005.111807. [DOI] [PubMed] [Google Scholar]
- 11.Nirula R, Allen B, Layman R, et al. Rib fracture stabilization in patients sustaining blunt chest injury. Am Surg. 2006;72:307–9. doi: 10.1177/000313480607200405. [DOI] [PubMed] [Google Scholar]
- 12.Althausen PL, Shannon S, Watts C, et al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma. 2011;25:641–7. doi: 10.1097/BOT.0b013e318234d479. [DOI] [PubMed] [Google Scholar]
- 13.de Moya M, Bramos T, Agarwal S, et al. Pain as an indication for rib fixation: a bi-institutional pilot study. J Trauma. 2011;71:1750–54. doi: 10.1097/TA.0b013e31823c85e9. [DOI] [PubMed] [Google Scholar]
- 14.Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am. 2011;93(1):97–110. doi: 10.2106/JBJS.I.00696. [DOI] [PubMed] [Google Scholar]
- 15.Mayberry JC, Ham LB, Schipper PH, et al. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J Trauma. 2009;66:875–879. doi: 10.1097/TA.0b013e318190c3d3. [DOI] [PubMed] [Google Scholar]
- 16.Clarke M, Horton R. Bringing it all together: Lancet-Cochrane collaborate on systematic reviews. Lancet. 2001;357:1728. doi: 10.1016/S0140-6736(00)04934-5. [DOI] [PubMed] [Google Scholar]
- 17.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 18.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of healthcare interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman D, editors. Systematic reviews in Health Care: Meta-analysis in Context. 2nd eds BMJ Books; London: 2011. pp. 285–312. [Google Scholar]
- 20.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48. [PubMed] [Google Scholar]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Berkey CS, Hoaglin DC, Mosteller F, Colditz GA. A random-effects regression model for meta-analysis. Stat Med. 1995;14(4):395–411. doi: 10.1002/sim.4780140406. [DOI] [PubMed] [Google Scholar]
- 24.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–5. doi: 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lardinois D, Krueger T, Dusmet M, et al. Pulmonary function testing after operative stabilization of the chest wall for flail chest. Eur J Cardiothorac Surg. 2001;20:496–501. doi: 10.1016/s1010-7940(01)00818-1. [DOI] [PubMed] [Google Scholar]
- 27.Oyarzun JR, Bush AP, McCormick JR, et al. Use of 3.5-mm acetabular reconstruction plates for internal fixation of flail chest injuries. Ann Thorac Surg. 1998;65:1471–4. doi: 10.1016/s0003-4975(98)00090-3. [DOI] [PubMed] [Google Scholar]
- 28.Hellberg K, de Vivie ER, Fuchs K, et al. Stabilization of flail chest by compression osteosynthesis—experimental and clinical results. Thorac Cardiovasc Surg. 1981;29:275–81. doi: 10.1055/s-2007-1023495. [DOI] [PubMed] [Google Scholar]
- 29.Engle C, Krieg JC, Madey SM, et al. Operative chest wall fixation with osteosynthesis plates. J Trauma. 2005;58:181–6. doi: 10.1097/01.ta.0000063612.25756.60. [DOI] [PubMed] [Google Scholar]
- 30.Richardson JD, Franklin GA, Heffley S, et al. Operative fixation of chest wall fractures: an underused procedure? Am Surg. 2007;67:660–4. [PubMed] [Google Scholar]
- 31.Paris F, Tarazona V, Blasco E, et al. Surgical Stabilization of traumatic flail chest. Thorax. 1975;30:521–7. doi: 10.1136/thx.30.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anavian J, Guthrie ST, Cole PA. Surgical management of multiple painful rib nonunions in a patient with a history of severe shoulder girdle trauma: a case report and literature review. J Orthop Trauma. 2009;23:600–4. doi: 10.1097/BOT.0b013e3181a15e90. [DOI] [PubMed] [Google Scholar]
- 33.Mohr M, Abrams E, Engle C, et al. Geometry of human ribs pertinent to orthopedic chest-wall reconstruction. J Biomech. 2007;40:1310–7. doi: 10.1016/j.jbiomech.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 34.Beelen R, Rumbaut J, De Geest R. Surgical Stabilization of a rib fracture using an angle stable plate. J Trauma. 2007;63:1159–60. doi: 10.1097/01.ta.0000222536.91745.b4. [DOI] [PubMed] [Google Scholar]
- 35.Mayberry JC, Terhes JT, Ellis TJ, et al. Absorbable plates for rib fracture repair: preliminary experience. J Trauma. 2003;55:835–9. doi: 10.1097/01.TA.0000090037.72142.33. [DOI] [PubMed] [Google Scholar]
- 36.Vu KC, Skourtis ME, Gong X, et al. Reduction of rib fractures with a bioresorbable plating system: preliminary observations. J Trauma. 2008;64:1264–9. doi: 10.1097/TA.0b013e3180340e31. [DOI] [PubMed] [Google Scholar]
- 37.Iwasaki A, Hamatake D, Shirakusa T. Bioabsorbable poly-L-lactide rib-connecting pins may reduce acute pain after thoracotomy. Thorac Cardiovasc Surg. 2004;52:49–53. doi: 10.1055/s-2004-815802. [DOI] [PubMed] [Google Scholar]
- 38.Ambrose GC, Clanton TO. Bioabsorbable implants: review of clinical experience in orthopedic surgery. Ann Biomed Eng. 2004;32:171–7. doi: 10.1023/b:abme.0000007802.59936.fc. [DOI] [PubMed] [Google Scholar]
- 39.Matsui T, Kitano M, Nakamura T, et al. Bioabsorbable struts made from poly-L-lactide and their application for treatment of chest deformity. J Thorac Cardiovasc Surg. 1994;108:162–8. [PubMed] [Google Scholar]
- 40.Tatsumi A, Kanemitsu N, Nakamura T, et al. Bioabsorbable poly-L-lactide costal coaptation pins and their clinical application in thoracotomy. Ann Thorac Surg. 1999;67:765–8. doi: 10.1016/s0003-4975(98)01264-8. [DOI] [PubMed] [Google Scholar]
- 41.Campbell N, Conagien P, Martin K, et al. Surgical stabilization of rib fractures using Inion OTPS wraps—techniques and quality of life follow-up. J Trauma. 2009;67:596–691. doi: 10.1097/TA.0b013e3181ad8cb7. [DOI] [PubMed] [Google Scholar]
- 42.Puma F, Ragusa M, Santoprete S, et al. Chest wall stabilization with synthetic reabsorbable material. Ann Thorac Surg. 1999;67:1823–4. doi: 10.1016/s0003-4975(99)00379-3. [DOI] [PubMed] [Google Scholar]
- 43.Moore BP. Operative stabilization of non-penetrating chest injuries. J Thorac Cardiovasc Surg. 1975;70:619–30. [PubMed] [Google Scholar]
- 44.Judet R. Osteosytheses costale. Rev Chir Orthop Reparatrice Appar Mot. 1973;59(Suppl 1):334–5. [PubMed] [Google Scholar]
- 45.Menard A, Testart J, Philippe JM, et al. Treatment of flail chest with Judet’s struts. J Thorac Cardiovasc Surg. 1983;86:300–5. [PubMed] [Google Scholar]
- 46.Landreneau RJ, Hinson JM, Jr, Hazelrigg SR, et al. Strut fixation of an extensive flail chest. Ann Thorac Surg. 1991;51:473–5. doi: 10.1016/0003-4975(91)90871-m. [DOI] [PubMed] [Google Scholar]
- 47.Sales JR, Ellis TJ, Gillard J, et al. Biomechanical testing of a novel, minimally invasive rib fracture plating system. J Trauma. 2008;64:1270–4. doi: 10.1097/TA.0b013e31804a7fd5. [DOI] [PubMed] [Google Scholar]
- 48.LeLorier J, Gregoire G, Benhaddad A, et al. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997;337:536–42. doi: 10.1056/NEJM199708213370806. [DOI] [PubMed] [Google Scholar]
- 49.Esteban A, Frutos F, Tobin MJ, et al. A comparison of four methods of weaning patients from mechanical ventilation. N Engl J Med. 1995;332:345–350. doi: 10.1056/NEJM199502093320601. [DOI] [PubMed] [Google Scholar]
- 50.Kress JP, Pohlman AS, O’Connor MF, et al. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–1477. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]