Abstract
Developing interprofessional education (IPE) curricula that improve collaborative practice across professions has proven challenging. A theoretical basis for understanding collaborative practice in health care settings is needed to guide the education and evaluation of health professions trainees and practitioners and support the team-based delivery of care. IPE should incorporate theory-driven, evidence-based methods and build competency toward effective collaboration.
In this article, the authors review several concepts from the organizational science literature and propose using these as a framework for understanding how health care teams function. Specifically, they outline the team process model of action and planning phases in collaborative work; discuss leadership and followership, including how locus (a leader’s integration into a team’s usual work) and formality (a leader’s responsibility conferred by the traditional hierarchy) affect team functions; and describe dynamic delegation, an approach to conceptualizing escalation and delegation within health care teams. For each concept, they identify competencies for knowledge, attitudes, and behaviors to aid in the development of innovative curricula to improve collaborative practice. They suggest that gaining an understanding of these principles will prepare health care trainees, whether team leaders or members, to analyze team performance, adapt behaviors that improve collaboration, and create team-based health care delivery processes that lead to improved clinical outcomes.
Despite decades of interest in interprofessional education (IPE) as a means to promote more “efficient, effective, comprehensive, and personalized” health care,1–3 few IPE programs have demonstrated sustained benefits for trainees or patients.4 In Canada5 and the United States,6 expert panels have defined interprofessional competencies to support overarching goals for educating health professions trainees (that is, learners at any stage of professional education in health care including continuing professional development). Yet even as these competencies specify desired outcomes for IPE, how best to achieve these goals within the educational and clinical systems of team-based health care remains unclear.
A team’s success on a given task depends upon at least four conditions: The task must be suitable for teamwork, the team must include the right group of people to perform the task, the team members must combine their resources effectively to complete the task, and the organization must provide a supportive context for the team.7,8 Meeting these conditions in health care settings is a challenge as the nature of care delivery is complex.9–12 Health care is delivered in dynamic environments where providers care for many patients, each of whom may be served by several teams with different members. Further, each team’s approach to interprofessional collaboration may vary according to contextual factors (e.g., patient acuity, team composition, resource availability).13 Health care professionals—whether team leaders or team members—must adjust their approaches based on contextual factors to meet the needs of patients and communities.14 Leaders, in particular, influence teams’ effectiveness by facilitating action and making sure the resources necessary for optimal performance are available.15 Team members, however, may have conflicting perceptions of leadership structures and responsibilities,16 decreasing the team’s effectiveness.
Recognizing that health care teams have varied structures and engage in diverse processes, educators should strive to develop curricula that help trainees gain a deeper understanding of collaborative work.2 To aid in the construction of educational programs with targeted IPE objectives, we sought to identify theoretical bases that support competencies for collaborative practice. We turned to the literature of organizational science, specifically the field of industrial and organizational psychology. In this field,
psychologists study the behavior of people at work. [They] derive principles of individual, group, and organization behavior through research. They develop scientific knowledge and apply it to the solution of problems in work settings. The applications are science- and research-based … integrating science and practice so that activities in one domain inform activities in the other domain.17
In this article, we present select concepts to create a foundation for understanding teams, leadership, and collaboration in health care. The four concepts described--team process, leadership and followership, locus and formality of leadership, and dynamic delegation--apply to teams across health care settings. Health care workers at all stages of training who learn about these concepts will gain a deeper understanding of collaborative work and become better equipped to participate in and lead teams. We also propose knowledge, attitudinal, and behavioral competencies related to each concept that we believe should inform the efforts of educators, practitioners, and clinical and administrative leaders as they strive to improve collaborative practice and patient care.
A Framework for Collaborative Practice in Health Care
Team process
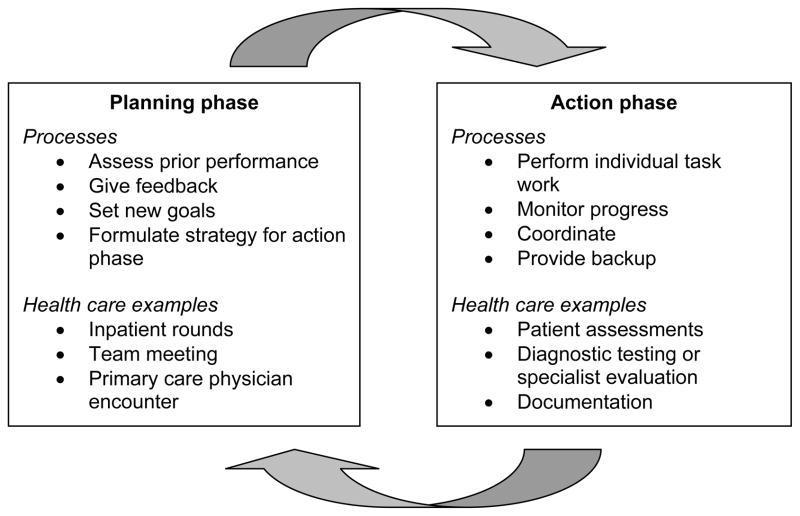
As Figure 1 illustrates, the work of teams is cyclical in nature and may be divided into two general phases: planning and action.18 Planning phase activities are usually conducted as a team and include assessing prior performance and formulating strategies for future actions. Action phase activities include individual task work and monitoring progress toward achieving goals decided upon in the action phase. Before accomplishing an overall goal, a team often cycles through the planning and action phases multiple times.
Figure 1.
Team process cycles: Examples of planning and action phases in health care.
One example of a planning phase activity is daily inpatient rounds, during which teams review plans of care for patients and make decisions regarding the action phase--the work/care to be provided for the remainder of the day. Similarly, teams in long-term care settings hold weekly or monthly team meetings (the planning phase) where they review the clinical status of patients and establish plans of care (the resulting action phase).
Inadequacies in the planning phase can lead to action phase failures that cause patient harm, especially in high-risk situations like transitions of care.19 For example, during the transition of care between inpatient and outpatient settings, failing to properly compile the discharge medication list (planning phase) can lead to errors in hospital discharge processes (action phase) and deleterious patient outcomes in the post-acute care setting.20,21 The planning phase process of compiling the discharge medication list may require input from many different professionals including nurses, pharmacists, physicians, and care coordinators. While the physician is responsible for prescribing the medications, other critical contributions can include the pharmacist’s advice on safety issues (e.g., medication interactions), the bedside nurse’s opinion on administration concerns, and the care coordinator’s guidance related to insurance formularies. The related action phase activities, including writing prescriptions and teaching the patient/family about the medications, require a solid basis of interprofessional collaboration during the planning phase. Without a collaborative setting for discharge planning, such as interprofessional rounds, planning phase activities may not be accomplished properly and action phase activities may be prone to error.
The action and planning phases require different approaches to work and training.22 While the profession-specific work of the action phase is the focus of most health professions training, the interprofessional work of the planning phase requires each team member to possess knowledge, attitudes, and behaviors that enable effective collaboration.23 During the planning phase, team members as a group should engage in reflection and feedback activities that review past team performance, assess progress toward overall goals, develop interval goals, and create an implementation plan for the next action phase. Planning phase activities in health care settings, however, often fall short of performance expectations24 for reasons such as excluding key team members from other health professions, failing to review prior team performance broadly, and setting interval goals that do not take into account the expertise and perspectives of all team members. These missed opportunities lead to poor team cohesion and coordination as well as suboptimal outcomes in the action phase.25,26 Additionally, the expanding scope of practice for many health professions has increased the overlap of practice capabilities.27 Health care teams should therefore use the planning phase to determine which team member is best suited to complete a specific task based on contextual factors (e.g., resource availability, competing work demands) and expertise.
Recognizing the differing functions of the phases of the team process and understanding how the planning phase affects performance in the action phase should lead to a better appreciation of these functions and improved patient care.18 Building on this attitudinal foundation, practitioners, especially individuals in leadership roles, should demonstrate the ability during the planning phase to (a) guide teams through reflection and feedback about preceding action phases and (b) develop team goals for succeeding action phases. Because the planning phase requires the collaborative attitudes and skills central to interprofessional care, we recommend that educators develop curricula to teach these concepts of team process as an underlying framework for collaborative practice (Table 1).
Table 1.
Concepts and Competencies Drawn From the Organizational Science Literature: A Framework to Inform Curriculum Planning for Collaborative Practice in Health Care
| Concept (source) | Competencies | ||
|---|---|---|---|
| Knowledge | Attitudes | Behaviors | |
| Team process (Marks et al, 200118) |
|
|
|
| Leadership and followership (Day et al, 200432; Carsten & Uhl-Bien, 201329) |
|
|
|
| Locus and formality of leadership (Morgeson et al, 201030) |
|
|
|
| Dynamic delegation (Klein et al, 200634) |
|
|
|
Leadership and followership
Leadership in the dynamic environments of health care should not be viewed as fixed, but rather as “coproduced.”28,29 In other words, it should involve leaders and followers working together to achieve outcomes, with each team member leading and following at times, and each influencing and enhancing the collaborative process. To be effective in a leadership capacity, individuals should provide team members with the resources and support they need to be successful in their roles.30 Some leadership responsibilities, such as establishing goals and providing feedback, are critical in the planning phase, while others, like providing organizational structure and managing internal and external resources, are more critical during the action phase.30 If leaders fulfill these responsibilities, team members can complete their duties and meet their individual goals, and the team, in turn, can meet the team’s goals.31 In health care, team leaders must therefore appreciate the range of expertise and understand the abilities of all professionals on the team, recognize what each team member requires to succeed, and ensure individuals’ needs are met. In addition, they must be able to engage team members who are separated by geographic and hierarchical barriers and realize when another team member is better equipped to lead the team.
The desired leadership behaviors may not always be demonstrated in clinical settings, however. In an inpatient environment, team members from the same discipline often work in partnership—that is, physicians assist physicians and nurses help nurses. These collaborative, consultative relationships employ sound leadership practices that encourage a free exchange of information and expertise to ensure patient care needs are met. In contrast, collaboration across professions may be hindered by barriers including hierarchy (e.g., the very experienced nurse is called by a first name but the new intern is called “doctor”) or geography (e.g., doctors cluster in the physician work room while nurses gather at the nurses’ station). Leaders, especially those who are organizationally and culturally empowered such as physicians, should strive to overcome these obstacles in order to assess and meet the needs of all team members. Certain safety processes, like surgical timeouts, offer opportunities to confront barriers directly and emphasize team members’ obligations to each other and to the patient. It is up to leaders to use these processes to create an inclusive, open environment that facilitates collaboration.
To lead teams successfully, trainees should develop knowledge, attitudes, and behaviors in the domain of leadership32 (Table 1). They need foundational knowledge about the range of professionals on health care teams and what each profession requires to accomplish its work (Table 1). Trainees should also learn to recognize barriers to collaborative practice. Individuals who are often in leadership capacities in the health care environment should demonstrate that they can assess and meet the resource needs of team members and overcome barriers to collaboration.33 All health care professionals should recognize that leadership and followership are complementary roles, and they should be empowered and willing to move between these roles as situations dictate.33
Locus and formality of leadership
The capabilities of a leader are shaped by situational factors, including locus and formality.30,32 Locus describes a leader’s relationship to the team: leaders can be internal (engaged in the team’s ongoing work) or external (not directly engaged in the team’s day-to-day work). Internal leaders are often more familiar with team members and better at functions such as team problem-solving and planning, whereas external leaders may have a better perspective for developing and training team members or managing the team’s boundaries.30
As an example, consider a patient with an acute change in clinical status. An internal leader, in this case a nurse or physician, with knowledge of the patient’s clinical course and team members’ individual abilities is able to adapt to the patient’s changing needs in a critical situation, using context-specific information. In contrast, an external leader, such as a cross-covering house officer or float nurse, would need to dedicate more effort to tasks like assessing the abilities of other team members and understanding typical unit practices. External leaders may be more effective in other situations. For instance, a medical consultant can provide a fresh perspective on a patient’s clinical care and, based on his or her expertise and the patient’s needs, may even assume a leadership role temporarily (e.g., an advanced practice nurse directing wound care) or more permanently (e.g., a physician transferring care to a service that is more suited to the patient’s condition). External leaders also are better than internal leaders at assessing team performance, which should be considered when planning assessments.30
Formality, or an organization’s recognition of the leader’s responsibility for team performance, is another situational factor that shapes leadership in health care settings.30 Formal leaders are embedded in the organizational hierarchy and control the pathways to escalate concerns and to access resources. Informal leaders have less explicit responsibilities and less clear mechanisms to attain resources, maintain organizational structure, and accomplish team goals efficiently and effectively. To escalate medical care, informal leaders must engage formal leaders.
As an illustration, consider the different processes of care during an acute event for two types of teams: a cardiac bypass surgical team with formal, internal leaders, and a resuscitation team, with both informal, internal and formal, external leaders. On the cardiac bypass surgical team, the attending surgeon and anesthesiologist typically share leadership responsibilities. Both of these leaders are internal to the team and their leadership capacity is formally established. Because they are internal leaders, they are knowledgeable about the patient case and other team members’ capabilities. They work with the team to anticipate problems and take preemptive action to avoid them. If unexpected events occur, these internal leaders have the capability to make quick corrective actions via existing organizational structures. No inefficient and potentially hazardous transfers of leadership are necessary.
The leaders of an early stage resuscitation team have different locus and formality. A floor nurse (an internal, informal leader) may discover a patient in cardiac arrest and initially lead the team. While the nurse has the insight of an internal leader about the patient, he or she has limited access to the resources available to formal leaders. The code team is activated to bring in an external, formal leader to assume team leadership. Although this individual provides expertise and expanded access to resources, these benefits are challenged by the inefficient and potentially hazardous period of clinical and team reassessment required by the transition of leadership from an internal leader to an external leader.
In less acute settings (e.g. ambulatory), there is often less structured authority,13 and leadership formality may not be defined by traditional hierarchy. For example, a case manager may be the formal, internal leader of a team managing the care of a patient with complex biopsychosocial needs. The physicians, nurse clinicians, and pharmacists who provide input should recognize the central nature of the case manager in the patient’s care.
Health care professionals therefore need to be trained to be sensitive to how locus and formality modulate leadership capabilities32 and, based on these concepts, adopt the leadership behaviors appropriate for the situation (Table 1). Trainees should learn that (a) external leaders need to value the team knowledge of and lead collaboratively with internal leaders and (b) internal leaders need to seek external leaders’ insights on both clinical care and team performance. When in formal leadership capacities, health care practitioners should be taught to create structures and a climate that empowers informal leaders to escalate concerns and access resources.
Dynamic delegation
Dynamic delegation is a team leadership theory developed by organizational scientists studying health care teams in a trauma resuscitation unit at an academic medical center.34 In this theory, team structures are described as shared, hierarchical, and de-individualized. Shared means that leadership responsibility is held by several people—in this example, the resident, fellow, and attending physician. Hierarchical refers to the presence of a formal leadership structure based on expertise that defines the power relationship between individuals. In other words, the fellow has more power and expertise than the resident and, if necessary, can assume control from the resident without conflict; likewise, the attending can smoothly assume control from the fellow. Corresponding formal structures exist for other health professions and settings. De-individualized indicates that capabilities are specific to roles rather than to people. Capabilities are often formally proscribed by licensure or certification. For example, physicians of a specific level of certification and licensure are expected to demonstrate certain capabilities. While individual performance may fluctuate within a range, all individuals holding the same role are expected to possess minimum competency in profession-specific areas. Within a shared, hierarchical, and de-individualized structure, the process of dynamic delegation can operate, with leadership authority transferred up and down the hierarchy in response to specific clinical events.34
This dynamism results in two desirable outcomes. First, dynamic delegation improves efficiency by allocating the most advanced expertise to only the most challenging or critical situations.34 For example, a home health nurse visiting a homebound outpatient monitors the patient for signs of clinical deterioration and escalates any concerns to the physician overseeing the case. That physician, meanwhile, attends to diagnosing undefined medical problems. Second, and of particular importance in academic health centers, dynamic delegation trains the next generation of experts.34 Novices are granted early leadership responsibilities that increase as they demonstrate competencies, but they receive assistance from experts if they encounter difficulty. For example, an intern may cover 20 patients at night with little need for expert assistance. However, if one of those patients has a clinical status change, the intern may call the supervising resident, who is responsible for several interns and all of their patients. The resident provides additional expertise as well as experiential training for the intern, but if the resident is uncertain how to proceed with the patient or determines the patient is critically ill, he or she will engage the attending physician to lend additional expertise. When the situation has stabilized, the expert transitions leadership back to the novice.
Dynamic delegation also describes other team processes in health care. Both a bedside nurse making an inpatient assessment and a pharmacist reviewing an outpatient medication plan are, for that moment, leading the team. If the clinical situation warrants, they can access formal leadership to increase the available expertise.
Dynamic delegation provides an organizing framework that educators can use to teach health professions trainees about the complex interactions between members of interprofessional teams.34 Trainees should understand that leadership is often shared, hierarchical, and de-individualized and that individuals have specific responsibilities to the team at different levels in the hierarchy. All health care professionals should demonstrate the ability to deliver care as dictated by a clinical situation, accepting responsibility for effective delegation and escalation within the hierarchy as necessary (Table 1).
Implications for Health Care Teams and Education
Comparing medical education today with the Flexnerian model, Berwick and Finkelstein note that “the new social context requires preparation of physicians to thrive in systems of inescapable interdependence; and their comfort in that interdependence is now a precondition to providing high-quality care.”35 To accomplish this aim, health professions trainees must acquire a fundamental understanding of the team processes undergirding clinical care. Concepts drawn from organizational science can provide educators with a framework to support interprofessional and discipline-specific curricula that teach the basics of team function and collaborative care (Table 1).
Currently, most education about teams occurs through two approaches. The traditional approach relies on less-structured educational experiences comprising clinical education24,36,37; this has led to a gap between what is taught in the classroom and what occurs during the delivery of care.38 More recently, team training programs that make use of simulation39,40 (e.g., TeamSTEPPS41), have been implemented in many settings to train health care workers in communication and teamwork skills and to develop new care processes that support teamwork.
Health professions trainees who are taught the theoretical foundations we have outlined in this article will gain an understanding of team function that will help them both facilitate collaboration in existing care processes and create new approaches to care that are more supportive of teamwork. They will also be able to contextualize clinical experiences, differentiate effective and ineffective teams, and lead efforts to improve team function and overall practice.
We suggest that team behaviors are best taught through a sequence of learning activities, including foundational instruction in the classroom, reinforcement in simulation-based settings, and development of proficiency through feedback and reflection in clinical settings.42,43 If health professions trainees are imbued with an understanding of team function that is reinforced through practice-based activities, they will be positioned to act as agents of change,44 leading and creating health care structures that stimulate a more collaborative culture and reshape health care delivery to improve patient outcomes.
Acknowledgments
The authors would like to thank Roberta Waite, EdD, APRN, CNS-BC, associate professor at Drexel University, for her insights about nursing leadership.
Funding/Support: Dr. Dow is supported by a faculty fellowship grant from the Josiah H. Macy Jr. Foundation and by a grant from the Donald W. Reynolds Foundation. Dr. DiazGranados and Dr. Mazmanian are funded by a grant award (UL1TR000058) from the National Institutes of Health (NIH). The contents of this article are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences, the Josiah H. Macy Jr. Foundation, the Donald W. Reynolds Foundation, or the NIH.
Footnotes
Other disclosures: None.
Ethical approval: Not applicable.
Previous presentations: A portion of this work was presented at the Association of American Medical Colleges Integrating Quality meeting, June 2012, Rosemont, Illinois.
Contributor Information
Dr. Alan W. Dow, Assistant vice president of health sciences for interprofessional education and collaborative care, assistant dean of medical education, and associate professor of medicine, Department of Internal Medicine, Virginia Commonwealth University, Richmond, Virginia.
Dr. Deborah DiazGranados, Assistant professor, Office of Assessment and Evaluation Studies, School of Medicine, and program evaluator, VCU Center for Clinical and Translational Research, Virginia Commonwealth University, Richmond, Virginia.
Dr. Paul E. Mazmanian, Associate dean for assessment and evaluation studies, School of Medicine, and director of evaluation, VCU Center for Clinical and Translational Research, Virginia Commonwealth University, Richmond, Virginia.
Dr. Sheldon M. Retchin, Senior vice president of health sciences, Virginia Commonwealth University, and chief executive officer, VCU Health System, Richmond, Virginia.
References
- 1.Institute of Medicine. Educating for the Health Team. Washington, DC: National Academy of Sciences; 1972. [Google Scholar]
- 2.Institute of Medicine. Health Professions Education: A Bridge to Quality. Washington, DC: National Academy of Sciences; 2003. [Google Scholar]
- 3.World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 4.Reeves S, Zwarenstein M, Goldman J, et al. The effectiveness of interprofessional education: Key findings from a new systematic review. Journal of Interprofessional Care. 2010;24(3):230–241. doi: 10.3109/13561820903163405. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Interprofessional Health Collaborative. A National Interprofessional Competency Framework. Vancouver, Canada: Canadian Interprofessional Health Collaborative; 2010. [Google Scholar]
- 6.Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative; 2011. [Google Scholar]
- 7.Levi DJ. Group Dynamics for Teams. 3. Thousand Oaks, CA: SAGE; 2011. [Google Scholar]
- 8.Guzzo RA, Dickson MW. Teams in organizations: Recent research on performance and effectiveness. Annual Review of Psychology. 1996;47:307–338. doi: 10.1146/annurev.psych.47.1.307. [DOI] [PubMed] [Google Scholar]
- 9.Ramanujam R, Rousseau DM. The challenges are organizational not just clinical. Journal of Organizational Behavior. 2006;27(7):811–827. [Google Scholar]
- 10.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 11.Nelson EC, Batalden PB, Godfrey MM. Quality by Design: A Clinical Microsystems Approach. San Francisco, CA: Jossey-Bass; 2007. [Google Scholar]
- 12.Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 13.Retchin SM. A conceptual framework for interprofessional and co-managed care. Academic Medicine. 2008;27(7):929–933. doi: 10.1097/ACM.0b013e3181850b4b. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell PM, Wynia R, Golden B, et al. Discussion Paper. Washington, DC: Institute of Medicine; 2012. Core Priniciples and Values of Effective Team-Based Health Care. [Google Scholar]
- 15.Alonso A, Dunleavy DM. Building teamwork skills in healthcare: The case for communication and coordination competencies. In: Salas E, Frush K, editors. Improving Patient Safety Through Teamwork and Team Training. New York: Oxford University Press; 2013. pp. 41–58. [Google Scholar]
- 16.Lingard L, Vanstone M, Durrant M, et al. Conflicting messages: Examining the dynamics of leadership in interprofessional teams. Academic Medicine. 2012;87(12):1762–1767. doi: 10.1097/ACM.0b013e318271fc82. [DOI] [PubMed] [Google Scholar]
- 17.Zedeck S. APA Handbook of Industrial and Organizational Psychology. Washington, DC: American Psychological Association; 2011. Introduction; p. xxiv. [Google Scholar]
- 18.Marks MA, Mathieu JE, Zaccaro SJ. A temporally based framework and taxonomy of team processes. The Academy of Management Review. 2001;26(3):356–376. [Google Scholar]
- 19.Coleman EA, Berenson RA. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Annals of Internal Medicine. 2004;141(7):533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 20.Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306(8):840–847. doi: 10.1001/jama.2011.1206. [DOI] [PubMed] [Google Scholar]
- 21.Boockvar K, Fishman E, Kyriacou CK, Monias A, Gavi S, Cortes T. Adverse events due to discontinuation in drug use and dose changes in patients transferred between acute and long-term care facilities. Archives of Internal Medicine. 2004;164(5):545–550. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- 22.Bowers CA, Braun CC, Morgan BB. Team workload: Its meaning and measurement. In: Brannick M, Salas E, Prince C, editors. Team Performance Assessment and Measurement: Theory, Research, and Applications. New York: Lawrence Erlbaum; 1997. pp. 85–110. [Google Scholar]
- 23.Bedwell W, Wildman J, DiazGranados D, Salazar M, Kramer W, Salas E. Collaboration at work: An integrative multilevel conceptualization. Human Resource Management Review. 2012;22(2):128–145. [Google Scholar]
- 24.Bharwani AM, Harris GC, Southwick FS. Perspective: A business school view of medical interprofessional rounds: Transforming rounding groups into rounding teams. Academic Medicine. 2012;87(12):1768–1771. doi: 10.1097/ACM.0b013e318271f8da. [DOI] [PubMed] [Google Scholar]
- 25.Larson E. The impact of physician-nurse interaction on patient care. Holistic Nursing Practice. 1999;13(2):38–46. doi: 10.1097/00004650-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Mathieu JE, Buttons SB. An examination of the relative impact of normative information and self efficacy on personal goals and performance over time. Journal of Applied Social Psychology. 1992;22:1758–1775. [Google Scholar]
- 27.Fairman JA, Rowe JW, Hassmiller S, Shalala DE. Broadening the scope of nursing practice. New England Journal of Medicine. 2011;364(3):193–196. doi: 10.1056/NEJMp1012121. [DOI] [PubMed] [Google Scholar]
- 28.Shamir B. Introduction: From passive recipients to active co-producers—The roles of followers in the leadership process. In: Shamir B, Pillai R, Bligh M, Uhl-Bien M, editors. Follower-Centered Perspectives on Leadership: A Tribute to J R Meindl. Stamford, CT: Information Age Publishing; 2007. [Google Scholar]
- 29.Carsten MK, Uhl-Bien M. Ethical followership: An examination of followership beliefs and crimes of obedience. Journal of Leadership and Organizational Studies. 2013;20(1):49–61. [Google Scholar]
- 30.Morgeson FP, DeRue DS, Karam EP. Leadership in teams: A functional approach to understanding leadership structures and processes. Journal of Management. 2010;36(1):5–39. [Google Scholar]
- 31.Burke CS, Stagl KC, Klein C, Goodwin GF, Salas E, Haplin SM. What type of leadership behaviors are functional in teams? A meta-analysis. Leadership Quarterly. 2006;17(3):288–307. [Google Scholar]
- 32.Day DV, Gronn P, Salas E. Leadership capacity in teams. Leadership Quarterly. 2004;15(6):857–880. [Google Scholar]
- 33.McGrath J. Leadership Behavior: Some Requirements for Leadership Training. Washington, DC: U.S. Civil Service Commission, Office of Career Development; 1962. [Google Scholar]
- 34.Klein KJ, Ziegert JC, Knight AP, Xiao Y. Dynamic delegation: Shared, hierarchical, and deindividualized leadership in extreme action teams. Administrative Science Quarterly. 2006;51(4):590–621. [Google Scholar]
- 35.Berwick DM, Finkelstein JA. Preparing medical students for the continual improvement of health and health care: Abraham Flexner and the new “public interest”. Academic Medicine. 2010;85(9):S56–S65. doi: 10.1097/ACM.0b013e3181ead779. [DOI] [PubMed] [Google Scholar]
- 36.Hafferty F. Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine. 1998;73(4):403–407. doi: 10.1097/00001888-199804000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Blumenthal DM, Bernard K, Bohnen J, Bohmer R. Addressing the leadership gap in medicine: Residents’ need for systematic leadership development training. Academic Medicine. 2012;87(4):513–522. doi: 10.1097/ACM.0b013e31824a0c47. [DOI] [PubMed] [Google Scholar]
- 38.Ferguson KE, Jinks AM. Integrating what is taught with what is practiced in the nursing curriculum: A multi-dimensional model. Journal of Advanced Nursing. 1994;20(4):687–695. doi: 10.1046/j.1365-2648.1994.20040687.x. [DOI] [PubMed] [Google Scholar]
- 39.Rosen M, Hunt E, Pronovost P, Federowicz M, Weaver S. In situ simulation in continuing education for the health care professions: A systematic review. Journal of Continuing Education in the Health Professions. 2012;32(4):243–54. doi: 10.1002/chp.21152. [DOI] [PubMed] [Google Scholar]
- 40.Baker DP, Salas E, King H, Battles J, Barach P. The role of teamwork in the professional education of physicians: Current status and assessment recommendations. Joint Commission Journal on Quality and Patient Safety. 2005;31(4):185–202. doi: 10.1016/s1553-7250(05)31025-7. [DOI] [PubMed] [Google Scholar]
- 41.Clancy CM, Tornberg DN. TeamSTEPPS: Assuring optimal teamwork in clinical settings. American Journal of Medical Quality. 2007;22(3):214–217. doi: 10.1177/1062860607300616. [DOI] [PubMed] [Google Scholar]
- 42.Kern DE, Thomas PA, Howard DM, Bass EB. Curriculum Development for Medical Education: A Six-Step Approach. Baltimore, MD: Johns Hopkins University Press; 1998. [Google Scholar]
- 43.Salas E, Tannenbaum SI, Kriager K, Smith-Jentsch KA. The science of training and development in organizations: What matters in practice. Psychological Science in the Public Interest. 2012;13(2):74–101. doi: 10.1177/1529100612436661. [DOI] [PubMed] [Google Scholar]
- 44.Havelock R, Havelock M. Training for Change Agents: A Guide to the Design of Training Programs in Education and Other Fields. Ann Arbor, MI: The University of Michigan; 1973. [Google Scholar]