Abstract
Human parainfluenza virus type 1 (HPIV1) is a significant cause of respiratory tract disease in infants and young children for which a vaccine is needed. In the present study, we sought to attenuate HPIV1 by the importation of one or more known attenuating point mutations from heterologous paramyxoviruses into homologous sites in HPIV1. The introduced mutations were derived from three attenuated paramyxoviruses: (i) HPIV3cp45, a live-attenuated HPIV3 vaccine candidate containing multiple attenuating mutations; (ii) the respiratory syncytial virus cpts530 with an attenuating mutation in the L polymerase protein; and (iii) a murine PIV1 (MPIV1) attenuated by a mutation in the accessory C protein. Recombinant HPIV1 (rHPIV1) mutants bearing a single imported mutation in C, any of three different mutations in L, or a pair of mutations in F exhibited a 100-fold or greater reduction in replication in the upper or lower respiratory tract of hamsters. Both temperature-sensitive (ts) (mutations in the L and F proteins) and non-ts (the mutation in the C protein) attenuating mutations were identified. rHPIV1 mutants containing a combination of mutations in L were generated that were more attenuated than viruses bearing the individual mutations, showing that the systematic accretion of mutations can yield progressive increases in attenuation. Hamsters immunized with rHPIV1 mutants bearing one or two mutations developed neutralizing antibodies and were resistant to challenge with wild-type HPIV1. Thus, importation of attenuating mutations from heterologous viruses is an effective means for rapidly identifying mutations that attenuate HPIV1 and for generating live-attenuated HPIV1 vaccine candidates.
Human parainfluenza virus type 1 (HPIV1) is a member of the Paramyxovirinae subfamily of the Paramyxoviridae family of the single-stranded negative-sense RNA viruses that also includes HPIV2, HPIV3, HPIV4A, and HPIV4B (3). HPIV1, Sendai virus (a murine PIV1 [MPIV1]), and HPIV3 are classified in the Respirovirus genus. HPIV4 and HPIV2 are members of the Rubulavirus genus. The Paramyxoviridae family also contains a second subfamily of viruses, Pneumovirinae, that consists of the Pneumovirus and Metapneumovirus genera, including, respectively, human respiratory syncytial virus (RSV) and the recently identified human metapneumovirus (54).
HPIV1 causes severe respiratory tract illness that can lead to the hospitalization of infants and young children. HPIV1 is the principal etiologic agent of croup and, less frequently, can cause pneumonia and bronchiolitis (3). Infection with parainfluenza viruses is commonly accompanied by the secondary complication of otitis media (23). RSV, HPIV1, HPIV2, and HPIV3 have been identified as the principal etiologic agents responsible, respectively, for 23.3, 6.0, 3.2 and 11.5% of pediatric hospitalizations for respiratory tract diseases (3, 7, 23, 24, 33, 41). Together, they account for up to half of all hospitalizations of infants and young children for respiratory disease. RSV and the HPIVs are also receiving increasing recognition as important causes of respiratory tract disease in adults (1, 6, 14, 26, 31, 32). Thus, there is a need to produce vaccines against these viruses that can prevent the serious lower respiratory tract disease and the otitis media that accompanies their infections. The present study focuses on the development of mutations that would be useful in a live-attenuated HPIV1 vaccine.
The genome of the Washington/20993/1964 strain of HPIV1 (HPIV1/Wash/64) is 15,600 nucleotides in length and has an organization similar to that of the other members of the Respirovirus genus (39). The ribonucleocapsid-associated proteins include the nucleocapsid protein (N), the phosphoprotein (P), and the large polymerase (L) that carry out transcription and replication. The organization of the HPIV1 P gene is most closely related to that of MPIV1 (34, 39, 40, 42). Similar to that of MPIV1, the P gene of HPIV1 contains an alternative open reading frame (ORF) with several alternative translational start sites encoding a set of up to four C-terminal nested proteins, the C′, C, Y1, and Y2 proteins that appear to be interferon antagonists (17). The P gene of MPIV1 encodes another protein, called V, by yet another alternative ORF that is accessed by cotranscriptional editing, which is represented in HPIV1 by a relic ORF that is interrupted by stop codons, is not accessed by RNA editing, and thus does not appear to be expressed (3). The internal matrix protein (M) and the major protective antigens, the fusion protein (F) and the hemagglutinin-neuraminidase glycoprotein (HN), are the envelope-associated proteins. The gene order from the 3′ end is N, P/C, M, F, HN, and L.
Wild-type recombinant HPIV1 (rHPIV1) has recently been recovered from a full-length antigenomic HPIV1 cDNA (39), providing a starting point for developing attenuated vaccine candidates by reverse genetics. One method for rapidly developing attenuated mutations via reverse genetics is importing one or more known attenuating mutations identified in a heterologous virus into the homologous positions of the virus of interest, in this case HPIV1, using sequence alignments as a guide. For example, we recently showed that attenuating mutations identified in RSV or MPIV1 could be imported into HPIV3 to yield attenuated HPIV3 derivatives (12, 49). Since attenuating mutations were not known or available for HPIV1, we attempted to similarly attenuate HPIV1 by the importation of a number of previously identified attenuating mutations of both the ts and non-ts varieties from several other heterologous paramyxoviruses representing both subfamilies.
The mutations for importation into HPIV1 were chosen from three diverse paramyxoviruses: (i) the HPIV3 candidate vaccine HPIV3cp45 (2, 30, 46), (ii) the attenuated cpts530 RSV mutant, (5), and (iii) an attenuated strain of MPIV1 (16, 25). The HPIV3cp45 mutant was chosen as a donor of mutations since it is a promising HPIV3 candidate vaccine currently in phase II clinical trials that is attenuated in both the upper and lower respiratory tract of experimental animals and susceptible humans and for which the attenuating mutations have been identified (29, 45, 46). These mutations include three temperature-sensitive (ts) attenuating point mutations in the L polymerase gene, one non-ts attenuating point mutation in the C gene, and a set of two mutations in the F gene that together confer the non-ts attenuation phenotype (46). As described in the present paper, importation of the complete set of HPIV3cp45 mutations into HPIV1 did not yield viable virus, and thus, the cp45 mutations were introduced into HPIV1 individually or as small subsets. The ts attenuating F521L mutation in the L protein of the RSVcpts530 mutant was also chosen for importation into HPIV1, since the wild-type amino acid assignment at the homologous position of the L protein is conserved in over 14 other paramyxoviruses, including viruses from each paramyxovirus genus (49). Importation of this RSV mutation into the homologous position of the L protein of wild-type HPIV3 specified ts and attenuation (att) phenotypes, and it also augmented the level of attenuation and temperature sensitivity of HPIV3cp45 (49). The attenuating point mutation in the C protein of MPIV1 (F170S) was also chosen for importation into HPIV1, since this mutation was previously shown to specify a non-ts attenuation phenotype when introduced into a heterologous HPIV3 backbone (12). We specifically sought to import both ts and non-ts attenuating mutations into rHPIV1, since live-attenuated vaccine viruses containing both ts and non-ts attenuating mutations are phenotypically more stable following in vitro and in vivo replication than those containing only ts mutations (22, 37). In the present study, both ts and non-ts mutations in the C, L, or F protein were identified that attenuated HPIV1 for hamsters. Thus, the importation of attenuating mutations previously characterized in heterologous paramyxoviruses into HPIV1 can be used to rapidly identify mutations that attenuate HPIV1 and to generate potential live-attenuated HPIV1 vaccine viruses.
MATERIALS AND METHODS
Viruses and cells.
LLC-MK2 cells (ATCC CCL 7.1) and HEp-2 cells (ATCC CCL 23) were maintained in Opti-MEM I (Gibco-Invitrogen, Inc., Grand Island, N.Y.) supplemented with 5% fetal bovine serum (FBS) and gentamicin sulfate (50 μg/ml) or in Dulbecco minimal essential medium (Quality Biological, Inc., Gaithersburg, Md.) supplemented with 10% FBS, gentamicin sulfate (50 μg/ml), and 2 mM glutamine (Gibco-Invitrogen, Inc.). The recombinant HPIV3 wild-type strain JS (rHPIV3) (11), the recombinant JS-derived HPIV3cp45 vaccine candidate (rHPIV3 cp45) (46), and an rHPIV3 containing cp45-derived mutations in the F protein (46) were grown in LLC-MK2 cells as previously described (11, 22, 46). The biologically derived HPIV1 wild-type strain HPIV1 Wash/64 (HPIV1 wild type) (38), a wild-type rHPIV1 (39), and rHPIV1 mutants were grown in LLC-MK2 cells in the presence of added trypsin as described elsewhere (39).
Sequence comparison to identify ts and non-ts attenuating mutations from MPIV1, RSV, and HPIV3 to be imported into rHPIV1.
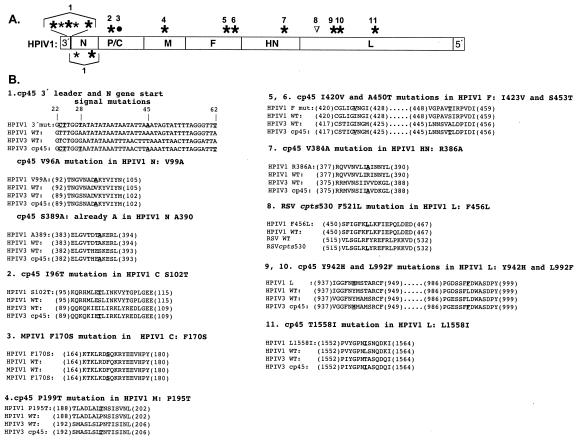
Regions of HPIV1 and other paramyxoviruses were aligned using Clustal W alignment (53) with the MacVector program (Accelrys, San Diego, Calif.) and the GAP program of the Wisconsin Package, version 10.2 (Accelrys). The nucleotide and protein sequences of HPIV1 (GenBank accession no. AF457102) was compared to that of HPIV3 (GenBank accession no. X57559) in order to identify which of the 15 mutations could be imported from HPIV3cp45 (GenBank accession no. U5116). To identify the homologous region in the HPIV1 C protein in order to introduce the non-ts attenuating F170S point mutation from the C protein of MPIV1 strain MVC11 (16, 25), the C protein sequence was aligned with those of the MPIV1 Z strain (GenBank accession no. M30202) and HPIV3. The attenuating F521S ts point mutation in the L protein of RSV (28) was identified in HPIV1 by sequence comparison among HPIV3, HPIV1, and other paramyxoviruses (49). The specific changes made to the nucleotide or amino acid sequence in rHPIV1 to import the mutations from HPIV3, MPIV1, and RSV are indicated in Fig. 1 and Table 1.
FIG. 1.
Diagram of the locations of the mutations identified in heterologous viruses that were imported into rHPIV1. (A) Map of HPIV1 genomic RNA. Twelve mutations that were imported from HPIV3cp45 (see B, below, for descriptions) are represented by large asterisks. Three additional mutations in HPIV3cp45 (panel B) that could not be imported into HPIV1 since the two viruses possess the same nucleotide or amino acid assignment at those positions are indicated by small asterisks. The F170S mutation imported from the MVC11 strain of MPIV1 (16, 25) is represented by a • symbol, and the F456L mutation imported from the RSV cpts530 mutant (27) is represented by a ▿ symbol. The individual mutations or sets of mutations that were imported into HPIV1 are indicated by the numbers 1 through 11 and correspond to the numbered sequence alignments in panel B below. (B) Sequence alignments are provided among HPIV1 wild-type, HPIV3 wild-type, and HPIV3 cp45 for all alignments except for mutations no. 3 and no. 8, for which the parents of the mutations were MPIV1 MVC11 and RSVcpts530, respectively. For mutations in the 3′ leader region, the sequence is presented as positive-sense cDNA, and nucleotide numbering is shown at the top relative to the 3′ end of the genome. For the other mutations, alignment of the appropriate protein sequences is shown. The number in parentheses flanking each amino acid sequence segment indicates the position of the residue at the beginning and end of the segment, respectively, in the complete amino acid sequence. The top sequence in each alignment indicates the change(s) that were made to rHPIV1, the next sequence is that of wild-type rHPIV1, the next is of the wild-type heterologous virus (e.g., HPIV3cp45, MPIV1, or RSV), and the last is of the mutant heterologous virus. Each rHPIV1 residue shown in bold type was altered to match the corresponding residue in the mutant heterologous virus. WT, wild-type; mut, mutation.
TABLE 1.
Importation of mutations previously characterized in attenuated MPIV1, RSV, and HPIV3 into the homologous positions of the HPIV1 antigenomic cDNA
| Mutation no.a | Region of HPIV1 genome or protein with mutation | Location of the aa substitution in the rHPIV1 proteinb | Nucleotide positionc in rHPIV1 | Sequence change(s)d | Viral origin of mutatione | Conservedf |
|---|---|---|---|---|---|---|
| 1 | 3′ leader | Noncoding | 23 | AACTTGTTTGGAATATA | HPIV3cp45 leader 23 | Yes |
| AACTTGCTTGGAATATA | ||||||
| 1 | 3′ leader | Noncoding | 28 | AACTTGTTTGGAATATA | HPIV3cp45 leader 28 | No |
| AACTTGTTTGGTATATA | ||||||
| 1 | N gene start | Noncoding | 62 | TTTTAGGGTTAAAGTAA TTTTAGGGTTTAAGTAA | HPIV3cp45 N gene start signal | Yes |
| 1 | N | V99A | 415-416 | GTC AAT GCT GAT GTC AA | HPIV3cp45/V96A | Yes |
| GTT AAC GCT GAT GCG AA | ||||||
| 2 | C | S102T | 2157 | ATG CTA GAA TCC TTG | HPIV3cp45/I96T | No |
| ATG CTA GAA ACC TTG | ||||||
| 3 | C | F170S | 2362 | GGG ATT TCC AGA AGA | MPIV1/F170S | Yes |
| GGG ATT CCC AGA AGA | ||||||
| 4 | M | P195T | 4251, 4253 | CTT GCA TTA CCG AAC | HPIV3cp45/P199T | Yes |
| CTA GCGCTA ACT AAC | ||||||
| 5 | F | I423V | 6354, 6356 | GGT TTA ATA GGT ATA | HPIV3cp45/I420V | Yes |
| GGT CTCGTG GGT ATA | ||||||
| 6 | F | S453T | 6444, 6446 | CCA GCA GTC TCC ATT | HPIV3cp45/A450T | No |
| CCC GCG GTC ACA ATT | ||||||
| 7 | HN | R386A | 8055-8057 | AAT GTC TTA ATT CGT | HPIV3cp45/V384A | No |
| AAC GTT TTA ATT GCG | ||||||
| 8 | L | F456L | 10137, 10139 | A TTT AAA TTT TTA AAA | RSVcpts530/F521L | Yes |
| T TTT AAA CTG TTA AAA | ||||||
| 9 | L | Y942H | 115595, 11597 | AAC TAT ATG TCT AC | HPIV3cp45/Y942H | Yes |
| AAC CAC ATG TCG AC | ||||||
| 10 | L | L992F | 11747 | C TCA AGC TTC TTA GAT | HPIV3cp45/L992F | Yes |
| C TCG AGC TTC TTT GAT | ||||||
| 11 | L | L15581 | 13443, 13445 | GGA CCT AAC TTG TCC | HPIV3cp45/T1558I | No |
| GGG CCC AAC ATC TCC |
See Fig. 1.
Homologous regions in HPIV1 versus the original heterologous viruses (MPIV1, RSV, and HPIV3) were identified using either Clustal W alignment or GAP alignment with the Wisconsin Package, version 10.2, software package.
Nucleotide change(s) made to introduce the putative attenuating mutation(s) into HPIV1, numbered starting from the 3′ end of the wild-type HPIV1 viral genome.
The sequence shown is in the positive sense, and the wild-type sequence is shown above the mutated sequence. Nucleotide substitutions are in bold type. Underlined residues indicate the codon involved in amino acid coding changes. Restriction sites are italicized.
The virus in which the original mutation was found is indicated, and the location of the nucleotide or amino acid changed in the original virus is also indicated. The amino acid carried by wild-type virus is indicated first, followed by its position in the protein and the mutant amino acid residue.
Indicates whether the nucleotide or amino acid assignment in question was conserved between wild-type HPIV1 and wild-type MPIV1, RSV, or HPIV3.
Construction of point mutations in the HPIV1 antigenomic cDNA.
Subgenomic clones of rHPIV1 (39) were used to introduce mutations from the HPIV3 cp45 vaccine candidate (21, 22, 30, 46), the MVC11 mutant of MPIV1 (16, 25), and the RSV mutant, cpts530 (9, 28). The mutations were introduced into the appropriate subgenomic clone (39) using a modified PCR mutagenesis protocol described elsewhere (35) with the Advantage-HF PCR kit (Clontech Laboratories, Palo Alto, Calif.). The subgenomic clone containing the mutation was then sequenced for the entirety of the region that had been PCR amplified by using a Perkin-Elmer ABI 3100 sequencer with the BigDye sequencing kit (Perkin-Elmer Applied Biosystems, Warrington, United Kingdom) to confirm that the subclone did not contain any extraneous mutations introduced during PCR amplification. Full-length HPIV1 cDNAs containing the mutations were assembled using standard molecular cloning techniques, and the appropriate region was sequenced again as described above to ensure that the full-length HPIV1 cDNAs contained the engineered mutation.
Construction of HPIV3 antigenomic cDNA bearing individual HPIV3cp45 F gene mutations.
The two mutations in the F gene of HPIV3cp45 (Table 1) were introduced individually into the complete HPIV3 antigenomic cDNA by site-directed mutagenesis. Point mutations were introduced into a subgenomic HPIV3 fragment using mutagenic oligonucleotides with the Transformer Mutagenesis kit (Clontech), and a full-length antigenomic cDNA bearing either the F protein I420V or the A450T codon substitution was assembled as described previously (45, 46). When possible, each cp45 change was engineered to be accompanied by a proximal, transcriptionally silent nucleotide substitution that introduced a restriction enzyme recognition site, which served as a marker to confirm the presence of the mutation in the cDNA and in the recovered virus.
Recovery of rHPIV1 and rHPIV3 mutant viruses.
Recovery of each mutant rHPIV1 virus and mutant rHPIV3 virus containing one or both of the mutations imported from the HPIV3cp45 F protein was performed at the permissive temperature of 32°C as described previously for rHPIV1 and rHPIV3 (39, 46). To confirm that recovered recombinant viruses containing the appropriate mutations were rescued from cDNA, viral RNA (vRNA) was isolated as described previously (39) and was amplified by reverse transcription (RT)-PCR by using either the SuperScript First-Strand Synthesis system or the Thermoscript RT-PCR system (Invitrogen, Inc.) for the RT step and either the Advantage cDNA PCR kit (Clontech Laboratories) or the Herculase Enhanced Polymerase Blend (Stratagene, La Jolla, Calif.) for the PCR step according to protocols specified by the manufacturers. Sequence analysis was performed as described above. In several instances, recovered viruses did not contain the intended mutations in the L gene, suggesting that the viruses were derived from a cDNA that had recombined with the pTM(L1) support plasmid during the rescue. Therefore, support plasmids containing the appropriate L gene mutations were used for the recovery of mutant recombinants from cDNA. rHPIV1 mutants that were successfully recovered were biologically cloned by two rounds of serial terminal dilutions using LLC-MK2 monolayer cultures in 96-well plates (Costar; Corning Inc., Corning, N.Y.). The presence of the introduced mutation in each biologically cloned rHPIV1 mutant was confirmed by sequence analysis of vRNA using RT-PCR as described above.
Replication of mutant rHPIV1s in LLC-MK2 cells at various temperatures.
The ts phenotype for each of the mutant rHPIV1 viruses was determined by comparing its level of replication to that of rHPIV1 at 32 and 36 through 40°C as described previously (50). Briefly, each virus was serially diluted 10-fold in 96-well LLC-MK2 monolayer cultures in L-15 media (Quality Biologicals or Gibco-Invitrogen, Inc.) containing trypsin and antibiotics. Replicate plates were incubated at the temperatures indicated above for 6 days, and virus-infected cultures were detected by hemadsorption with guinea pig erythrocytes. The virus titer at each temperature was determined in two to six separate experiments and is expressed as the log10 50% tissue culture infectious dose per milliliter (TCID50/ml). The reduction in titer at elevated temperature was compared to the titer at 32°C, and a mean reduction in titer was determined. The shutoff temperature of an rHPIV1 mutant is defined as the lowest temperature at which the reduction in virus titer compared to its titer at 32°C was 100-fold greater than that of wild-type rHPIV1 at the same temperature. A mutant is defined as temperature sensitive if its reduction in replication at 40°C, i.e., the titer at 32°C minus that at 40°C, is 100-fold or greater than that of wild-type rHPIV1. As a reference in some experiments, rHPIV3 wild type (11) and rHPIV3 cp45 (46) were concurrently tested as described above except that trypsin was not added and the final concentration of FBS was 5%.
For rHPIV3 viruses bearing one or two of the HPIV3cp45 mutations imported from the F protein (I420V and A450T), the level of temperature sensitivity was determined by plaque enumeration at the set of temperatures described above. HPIV3 plaques were identified by immunoperoxidase staining with HPIV3 HN protein monoclonal antibodies, as described previously (46).
Replication of rHPIV1 mutant viruses in the respiratory tract of hamsters and challenge with wild-type HPIV1.
Four- to five-week-old Golden Syrian hamsters were inoculated intranasally with 0.1 ml of L-15 medium containing 106.0 TCID50 of a wild-type or mutant HPIV. Lungs and nasal turbinates were harvested on day 4 postinfection, and the titer of virus was determined as previously described (39). The mean log10 TCID50/g was calculated for each group of six hamsters. With some of the viruses, the experiment was performed two or three times to give a total of 12 or 18 hamsters, respectively, in a group. In a separate experiment, groups of 6 or 12 hamsters were infected with 106 TCID50 of wild-type rHPIV1 or one of the mutants, serum samples were collected at 3 to 4 weeks, and the animals were challenged with 106 TCID50 of the biologically derived HPIV1/Wash/64 on either day 35 or 36 postimmunization. Lungs and nasal turbinates were harvested on day 4, and the virus titer was determined as described above.
Determination of serum antibody response in hamsters.
The level of HPIV1 antibodies in serum samples collected as described above was determined by using a neutralization assay. Twofold serial dilutions of hamster serum were combined with an equal volume of virus suspension containing approximately 150 TCID50 of a modified rHPIV1 (rHPIV1-FRSV) that served as a novel indicator virus. This modified rHPIV1 expressed the RSV fusion protein as an additional gene unit inserted upstream of the HPIV1 N gene (data not shown) and was generated in a manner analogous to that previously described for B/HPIV3-FRSV (43). rHPIV1-FRSV expresses the RSV fusion protein at a high level, resulting in rapid syncytium formation, facilitating the detection of infected cultures without hemadsorption or immunostaining, and the sensitivity of this virus to neutralization by HPIV1-specific antibodies is equivalent to that of wild-type HPIV1 (data not shown). The virus and serum mixture was incubated at 37°C for 1 h and transferred to LLC-MK2 monolayers in 96-well plates. After a 1-h adsorption period, the monolayers were washed twice to remove residual serum, and trypsin-containing Opti-MEM I was added. The cultures were incubated at 32°C for 5 days, and infected cultures were identified by the presence of syncytia. The neutralization titer is the dilution of serum at which 50% of the cultures were infected.
RESULTS
Introduction of ts and non-ts attenuating point mutations into rHPIV1.
Wild-type HPIV1/Wash/64 was recently recovered from a full-length antigenomic cDNA (39), making it possible to use reverse genetic methods to develop a live-attenuated HPIV1 vaccine. In order to do so, it would be necessary to identify mutations that could be introduced to yield attenuated HPIV1 derivatives. HPIV3, a member of the same Respirovirus genus, has a promising vaccine candidate, HPIV3cp45, that appears to be satisfactorily attenuated and immunogenic for infants and young children (30). The mutations in the HPIV3cp45 vaccine candidate have been identified and characterized (45, 46). Therefore, we first attempted to generate a live-attenuated recombinant HPIV1 vaccine candidate containing the complete set of ts and non-ts mutations imported from HPIV3cp45. The 15 mutations in HPIV3cp45 are indicated in Fig. 1A by large and small asterisks. Based on nucleotide and protein sequence alignments (Fig. 1B), only 12 of these (Fig. 1A, large asterisks) could be imported into HPIV1. The remaining three HPIV3cp45 mutations (Fig. 1A, small asterisks), which include two noncoding mutations in the 3′ leader at nucleotides 24 and 45 and an S389A coding change in the N protein (Fig. 1 and Table 1, mutation set no. 1), could not be imported into HPIV1 because the homologous positions in HPIV1 already have the same nucleotide or amino acid assignment as that of HPIV3cp45 (Fig. 1B). Thus, of the seven HPIV3cp45 mutations in the 3 leader and N gene (Fig. 1 and Table 1, mutation set no. 1), only four could be imported into HPIV1, and these four were imported as a set.
For the 12 HPIV3cp45 mutations that could be imported into HPIV1, in five cases the wild-type assignment at the sequence position in question was not identical between HPIV1 and HPIV3, despite the overall conservation of each region based on sequence alignment: these five positions include nucleotide 28 in mutation set no. 1 and mutations no. 2, no. 6, no. 7, and no. 11 (Fig. 1 and Table 1). Thus, the exact wild-type assignments of the homologous positions were not necessarily conserved between wild-type HPIV3 and HPIV1. Also, for the mutations involving the N, C, M, F, and HN proteins (Fig. 1 and Table 1, mutations no. 1, no. 2, no. 4, no. 5 and no. 7), the positions that were identified by sequence alignment as being homologous between HPIV3 and HPIV1 involve residues whose positions differ slightly by number in the corresponding amino acid sequences, whereas the noncoding nucleotide changes in the leader (part of mutation set 1) and coding changes in the L protein (mutations no. 9, no. 10, and no. 11) do correspond exactly by sequence position. These differences in wild-type assignment and spacing notwithstanding, the homologous position for each of the 12 imported mutations that was identified in HPIV1 by sequence alignment was modified to have the assignment of rHPIV3cp45.
Several attempts at recovering virus from an HPIV1 cDNA bearing all 12 of the mutations imported from HPIV3cp45 (rHPIV1cp45) or from a recombinant containing all of the HPIV3cp45 mutations except for those in the L protein (rHPIV1 3′-N-C-M-F-HNcp45) did not yield viable virus, which contrasted with our previous experience with HPIV3, in which similar combinations of cp45 mutations were readily recovered to yield viable HPIV3 mutants that replicated efficiently at permissive temperature (46). Thus, it apparently was not possible to isolate a viable rHPIV1 virus with the set of 12 HPIV3cp45 mutations or with the indicated subset of 9 of these mutations.
We therefore sought to generate viruses bearing single or small sets of HPIV3cp45 mutations to determine which individual HPIV3cp45 mutation or set of mutations might specify the attenuation phenotype in an rHPIV1 backbone. The single mutants or sets of mutants that could be successfully imported from HPIV3cp45 into viable rHPIV1 were as follows (Fig. 1B and Table 1): (i) mutation set no. 1, whose transferable mutations include two noncoding leader mutations, a noncoding mutation in the N gene start signal, and the V99A mutation in N; (ii) single mutations no. 2 (C protein, CS102T), no. 4 (M:P195T), no. 5 (F:I423V), no. 6 (F:S453T), no. 7 (HN:R386A), no. 9 (L:Y942H), no. 10 (L:L992F), and no. 11 (L:L1558I); (iii) a combination of the two F mutations (no. 5 plus no. 6); and (iv) three combinations of the L mutations, no. 9 plus no. 10, no. 10 plus no. 11, and no. 9 plus no. 10 plus no. 11. In addition, rHPIV1 viruses bearing the F170S mutation in the C protein from MPIV1 (mutation no. 3 in Fig. 1B) or the F456L mutation in the L protein from RSV (mutation no. 8 in Fig. 1B) were recovered. Each HPIV1 mutant was biologically cloned and grew to a reasonably high titer (≥106.5 TCID50/ml) (Table 2). The presence of the introduced mutations in the recovered viruses was confirmed by sequencing of RT-PCR products generated from vRNA (data not shown). Only one out of four attempts to recover a rHPIV1 virus containing all three HPIV3cp45 mutations in the L gene (mutations no. 9 plus no. 10 plus no. 11) was successful. Furthermore, the single successful recovery yielded a virus that contained two additional, adventitious point mutations within the L gene: an L1759Q and a C1832Y substitution. Since these mutations were not present in the original cDNA clone, it is likely that they developed either during rescue or during subsequent passage in cell culture. Also, a recombinant virus containing both the Y942H (no. 9) and L1558I (no. 11) mutations within the L protein could not be recovered. These results suggest that, whereas the combination of mutations at positions 942 and 1558 were compatible in HPIV3 (45), they were incompatible when imported as a pair into HPIV1. However, these two mutations apparently are compatible in HPIV1 when imported as a triplet in combination with the L992F (no. 10) mutant, perhaps also dependent on the further acquisition of second site mutations such as those identified at positions 1759 and 1832.
TABLE 2.
Replication of recombinant wild-type and mutant rHPIV1s and control HPIV3s at permissive and restrictive temperatures in vitro
| Virus | Mutation no.a | Mean titer at 32°C | Mean log10 reduction in virus titer at the indicated temp (°C)b
|
||||
|---|---|---|---|---|---|---|---|
| 36 | 37 | 38 | 39 | 40 | |||
| rHPIV1 | 7.8 | −0.1 | 0.5 | 0.9 | 1.3 | 2.3 | |
| rHPIV1 C:F170SMPIV1 | 3 | 7.3 | 0.2 | 0.6 | 1.2 | 2.0 | 2.3 |
| rHPIV1 L:F456LRSV | 8 | 7.1 | 0.7 | 2.4 | 4.9 | ≥5.6 | ≥5.9 |
| rHPIV1 3′-N V99Acp45 | 1 | 7.5 | 1.8 | 2.0 | 4.5 | 5.8 | ≥6.3 |
| rHPIV1 C:S102Tcp45 | 2 | 8.0 | ND | ND | ND | 1.5 | 2.8 |
| rHPIV1 M:P195Tcp45 | 4 | 7.5 | ND | ND | ND | 0.3 | 2.0 |
| rHPIV1 F:I423Vcp45 | 5 | 7.2 | ND | ND | ND | 0.7 | 3.5 |
| rHPIV1 F:S453Tcp45 | 6 | 7.2 | 1.7 | 2.0 | 3.7 | 4.0 | ≥6.0 |
| rHPIV1 F:I423V/S453Tcp45 | 5 + 6 | 6.5 | 2.8 | 2.8 | 3.5 | 4.3 | ≥5.5 |
| rHPIV1 HN:R386Acp45 | 7 | 7.0 | 2.0 | 2.7 | 4.2 | ≥5.3 | ≥5.5 |
| rHPIV1 L:Y942Hcp45 | 9 | 8.0 | 1.4 | 3.1 | 5.1 | 5.8 | ≥6.5 |
| rHPIV1 L:L992Fcp45 | 10 | 8.1 | 0.2 | 0.3 | 1.3 | 1.4 | 2.5 |
| rHPIV1 L:L1558Ip45 | 11 | 7.8 | 0.4 | 0.2 | 2.5 | 2.4 | 4.7 |
| rHPIV1 L:Y942H/L992Fcp45 | 9 + 10 | 7.5 | 0.5 | 2.5 | 5.3 | ≥5.7 | ND |
| rHPIV1 L:L992F/L1558Icp45 | 10 + 11 | 7.5 | 0.0 | 0.5 | 2.3 | 4.5 | ND |
| rHPIV1 L:Y942H/L992F/L1558Icp45d | 9 + 10 + 11 | 7.5 | 1.3 | 4.8 | ≥6.3 | ND | ND |
| rHPIV3 wtc | 8.3 | −0.1 | 0.1 | −0.1 | 0.0 | −0.2 | |
| rHPIV3 F:I420V | 5 | 6.7 | ND | ND | ND | 0.0 | 0.8 |
| rHPIV3 F:A450T | 6 | 7.0 | ND | ND | ND | 0.0 | −0.2 |
| rHPIV3 F:I420V/A450T | 5 + 6 | 7.5 | ND | ND | ND | 1.1 | 1.5 |
| rHPIV3 cp45 | 8.1 | 0.9 | 3.4 | 5.6 | ≥6.5 | ≥6.7 | |
Each value is the mean of at least two experiments. Values in bold type indicate temperatures at which the mean log10 reduction versus 32°C was ≥2.0 log10 compared to that of the wild-type rHPIV. The lowest temperature shown in bold is the shutoff temperature. ND, not determined.
wt, wild-type.
Contains two additional, adventitious mutations in the L coding sequence: LI759Q and C1852Y.
In HPIV3cp45, the two amino acid substitution mutations imported as a set in the F protein specify a non-ts attenuation phenotype (46). However, it was not known if one or both amino acid mutations are required for this attenuation phenotype. Therefore, two rHPIV3 mutants were generated, each containing one of the two amino acid substitutions in the F protein (mutations no. 5 and no. 6), and each was viable (Table 2). These mutants provided a direct comparison with the rHPIV1 mutants described above containing either one or both F mutations no. 5 and no. 6 (rHPIV1 F:I423Vcp45, rHPIV1 F:S453Tcp45, and rHPIV1 F:I423V/S453Tcp45). In total, 15 rHPIV1 and 2 rHPIV3 viruses were recovered.
Characterization of the level of replication of the rHPIV1 mutant viruses in LLC-MK2 cells at permissive and restrictive temperatures.
The 15 rHPIV1 viruses bearing one or more of the mutations imported from HPIV3, MPIV1, or RSV were tested for the ability to replicate at permissive temperature (32°C) versus a range of higher temperatures (36 to 40°C) by titration on LLC-MK2 monolayers, which showed that many of the single amino acid substitutions that specified a ts phenotype in the parental heterologous virus from which they were derived also specified a ts phenotype in rHPIV1, including mutations at positions 456 (no. 8), 942 (no. 9), and 1558 (no. 11) of the L protein (Table 2). The rHPIV1s bearing a mutation at amino acid 456 (no. 8) or 942 (no. 9) of the L protein had shutoff temperatures of 38 or 37°C, respectively, while the mutation at amino acid 1558 (no. 11) specified a shutoff temperature of 40°C. Similarly, some of the combinations of mutations imported from HPIV3cp45 specified a ts phenotype in both rHPIV3 (45, 46) and rHPIV1, including recombinants bearing the combination of 3′ leader and N gene mutations (mutation set no. 1, rHPIV1 3′-N V99Acp45 virus), the combination of Y942H and L992F mutations in the L protein (rHPIV1 Y942H/L992Fcp45; no. 9 plus no. 10), the combination of L992F and L1558I L protein mutations (rHPIV1 L: L992F/L1558Icp45; no. 10 plus no. 11), or a combination of all three mutations in L (rHPIV1 L:Y942H/L992F/L1558Icp45; no. 9 plus no. 10 plus no. 11) (Table 2). The L992F (no. 10) mutation in the L protein alone did not confer a ts phenotype in HPIV1, but it did in HPIV3cp45 (45) (Table 2). However, its inclusion augmented the level of temperature sensitivity, i.e., lowered the shutoff temperature, of the L1558I (no. 11) mutation in the virus rHPIV1 L:L992F/L1558Icp45 (Table 2).
The imported F:S453Tcp45 and HN:R386Acp45 mutations were at residues that were not conserved in the homologous positions in HPIV1 and HPIV3 (Fig. 1). Interestingly, although the A450T (no. 6) mutation did not specify the ts phenotype in HPIV3, the corresponding F:S453Tcp45 mutation did so in the rHPIV1 background (Table 2). Likewise, the rHPIV1 HN:R386Acp45 (no. 7) mutation specified the ts phenotype in rHPIV1 (Table 2) but not in rHPIV3 (46).
The recombinant bearing the non-ts attenuating mutation imported from the C protein of MPIV1 (no. 3; rHPIV1 C:F170SMPIV1) was also non-ts in HPIV1 (Table 2). Several of the non-ts mutations imported from HPIV3cp45, including those at position 102 in the C protein (no. 2), position 195 in the M protein (no. 4), or position 423 of the F protein (no. 5), also did not confer a ts phenotype in rHPIV1 (Table 2).
Characterization of the level of replication of mutant rHPIV1s in hamsters.
The ability of the 15 rHPIV1 mutants containing either a single mutation imported from HPIV3cp45, MPIV1, or RSV or a combination of mutations imported from HPIV3cp45 to replicate in the upper and lower respiratory tract of hamsters was examined. The peak level of wild-type HPIV1 replication in the respiratory tract of hamsters occurs on day 4 postinfection. The level of replication of the rHPIV1 mutants in the upper (nasal turbinates) and lower (lungs) respiratory tract of infected hamsters on day 4 was compared to that of wild-type rHPIV1, wild-type rHPIV3, or rHPIV3cp45 control viruses (Table 3). Among the single amino acid mutations, rHPIV1 bearing the L protein Y924H (no. 9) or F456L (no. 8) mutation or the C protein F170S mutation (no. 3) specified a 100-fold or greater reduction in replication in both the upper and lower respiratory tract of hamsters compared to that of the unmodified parent virus. This finding identified three new highly attenuating mutations for HPIV1. Two of these mutations were of the ts variety, namely Y942H (no. 9) and F456L (no. 8) in the L protein, while the third was non-ts, namely F170S (no. 3) in the C protein. A fourth mutation, the L1558I mutation in the L protein (no. 11), resulted in a 100-fold restriction of replication in the lower but not the upper respiratory tract of hamsters and represents an additional attenuating ts mutation.
TABLE 3.
Replication of wild-type and mutant HPIVs and control HPIV3s in the respiratory tract of hamstersa
| Virusb | Mutation no.c | No. of animalsd | Mean virus titer (log10 TCID50/g ± SEe)
|
|
|---|---|---|---|---|
| Nasal turbinate | Lung | |||
| rHPIV1 | 18 | 4.7 ± 0.1 | 5.2 ± 0.2 | |
| rHPIV1 C:F170SMPIV1 | 3 | 12 | 2.5 ± 0.1f | 2.5 ± 0.1f |
| rHPIV1 L:F456LRSV | 8 | 12 | 2.0 ± 0.2f | 1.7 ± 0.1f |
| rHPIV1 L:L992Fcp45 | 10 | 12 | 4.5 ± 0.1 | 3.6 ± 0.2 |
| rHPIV1 M:P195Tcp45 | 4 | 6 | 4.0 ± 0.2 | 4.2 ± 0.2 |
| rHPIV1 C:S102Tcp45 | 2 | 6 | 3.9 ± 0.1 | 4.2 ± 0.1 |
| rHPIV1 F:I423Vcp45 | 5 | 6 | 3.9 ± 0.2 | 4.5 ± 0.3 |
| rHPIV1 HN:R386Acp45 | 7 | 6 | 3.7 ± 0.0 | 4.3 ± 0.2 |
| rHPIV1 3′-N V99Acp45 | 1 | 6 | 3.7 ± 0.1 | 4.0 ± 0.2 |
| rHPIV1 L:L1558Icp45 | 11 | 12 | 3.3 ± 0.2 | 2.9 ± 0.1f |
| rHPIV1 F:S453Tcp45 | 6 | 6 | 3.2 ± 0.1 | 3.7 ± 0.1 |
| rHPIV1 L:Y942Hcp45 | 9 | 12 | 2.4 ± 0.2f | 2.2 ± 0.2f |
| rHPIV1 L:L992F/L1558Icp45 | 10 + 11 | 6 | 2.5 ± 0.0f | 2.0 ± 0.4f |
| rHPIV1 L:Y942H/L992Fcp45 | 9 + 10 | 6 | 2.0 ± 0.3f | 1.6 ± 0.1f |
| rHPIV1 L:Y942H/L992F/L1558Icp45 | 9 + 10 + 11 | 6 | 1.5 ± 0.1f | 1.9 ± 0.2f |
| rHPIV1 F:I423V/S453Tcp45 | 5 + 6 | 6 | ≤1.5 ± 0.0f | ≤1.5 ± 0.0f |
| rHPIV3 | 6 | 6.2 ± 0.2 | 5.7 ± 0.4 | |
| rHPIV3 F:A450T | 6 | 6 | 6.9 ± 0.1 | 5.8 ± 0.3 |
| rHPIV3 F:I420V | 5 | 6 | 5.9 ± 0.1 | 4.9 ± 0.4 |
| rHPIV3 F:I420V/A450T | 5 + 6 | 6 | 4.5 ± 0.1 | 3.3 ± 0.4f |
| rHPIV3 cp45 | 6 | 2.8 ± 0.1f | 1.6 ± 0.1f | |
Hamsters were inoculated intranasally with 106 TCID50 of the indicated virus. Nasal turbinates and lung tissues from each group were harvested on day 4. Virus present in the tissues was quantified by serial dilution on LLC-MK2 monolayer cultures at 32°C.
rHPIV1 mutant viruses are divided into two groups. The single-point mutations imported from MPIV1 and RSV are listed first, and the single or combination mutations from HPIV3cp45 are listed second. Three control viruses, rHPIV3, rHPIV3 F:I420V/A450T, and rHPIV3cp45, and the individual F mutations in rHPIV3 are listed last. Within each group of viruses, mutants are listed from the least to most attenuated in the upper respiratory tract.
Indicates the number of animals used to calculate the titer, representing either one (6), two (12), or three (18) independent experiments, respectively.
SE, standard error.
Values in bold represent a 100-fold or greater reduction in titer compared to the titer of the respective wild-type rHPIV1 or rHPIV3.
Combinations of HPIV3cp45 mutations in the L protein of HPIV1 resulted in an increase in attenuation. The combination of the Y942H and L992F L protein mutations (no. 9 plus no. 10) was somewhat more restrictive for the lower respiratory tract of hamsters than the virus containing the Y942H (no. 9) mutation alone, and the combination of both the L992F and L1558I mutations (no. 10 plus no. 11) was more restrictive for replication in both the upper and lower respiratory tracts than either the L992F (no. 10) or L1558I (no. 11) mutation alone (Table 3), indicating that in addition to contributing to the ts phenotype, the L992F mutation contributed to an attenuation phenotype. The mutant rHPIV1 containing the combination of all three of the L mutations imported from HPIV3cp45 (no. 9 plus no. 10 plus no. 11) was more highly restricted for replication than mutants bearing any two of the L mutations (Table 3); however, it is not known to what extent the other two adventitious mutations in the L protein (L1759Q and C1832Y) that arose during recovery of this virus from cDNA might have contributed to its attenuation phenotype.
In both rHPIV1 and rHPIV3, the combination of the two mutations in F (no. 5 plus no. 6) resulted in a virus that was more attenuated than either single mutant alone and yielded the most attenuated rHPIV1 mutant of the set of 15 tested. In comparison, rHPIV1 bearing the single F protein mutation S453T (no. 6) was restricted only about 30-fold in both the upper and lower respiratory tracts of hamsters, while the other single F protein mutation, I423V (no. 5), conferred less than a 6-fold reduction in replication. Recombinant HPIV3s bearing either of the HPIV3cp45 F protein mutations alone were neither restricted for replication in hamsters (Table 3) nor ts (Table 2). This finding indicates that, for HPIV3, the two cp45 F mutations are required to be present together to confer the non-ts att phenotype. In comparison, rHPIV1 containing both mutations (rHPIV1F:I423V/S450T) possessed both the ts and att phenotypes, and the double-mutant virus was more restricted in vivo than its HPIV3 counterpart. The recombinant viruses in this study were examined for their level of replication on day 4 postinfection. Future studies are planned to further characterize the level of shedding over a 10-day period of rHPIV1 candidate vaccines containing appropriate sets of attenuating mutations in a nonhuman primate animal model such as the African green monkey.
It was of interest to compare the effect of each of the cp45 mutations in the HPIV1 backbone versus that of HPIV3 with respect to the ts and att phenotypes (Table 4). Interestingly, a number of the HPIV3cp45 mutations had a more profound phenotypic effect in the rHPIV1 backbone than in that of HPIV3. For example, three rHPIV1 derivatives were both substantially more ts (>2°C difference) and substantially more att (>10-fold difference) than rHPIV3 derivatives containing the same mutations: these viruses included the F546L mutation in L (no. 8), the Y942H mutation in L (no. 9), and the combination of the I423Y and S453T mutations in F (no. 5 plus no. 6) that was noted above. A fourth rHPIV1, containing the S453T mutation in F (no. 6), can also be included in this group because it was substantially more ts and moderately more att than its HPIV3 counterpart. Two other rHPIV1 derivatives were not significantly more ts than their rHPIV3 counterparts but were substantially more att: namely, viruses bearing F170S in the C protein (no. 3) and the combination of L992F and L1558I in the L protein (no. 10 plus no. 11). Two other rHPIV1 derivatives shown in Table 4 were substantially more ts than their HPIV3 counterparts without a significant difference in att: namely, viruses bearing R386A in HN (no. 7) and the set of leader and N gene mutations (3′-N V99A; mutation set no. 1). Conversely, the effects of several mutations were greater in the HPIV3 backbone than in that of HPIV1. Specifically, in three cases, the att phenotype was greater in HPIV3 than in HPIV1; these include the S102T C mutation (no. 2), the L992F L mutation (no. 10), and the combination of the Y942H and L992F L mutations (no. 9 plus no. 10). In the remaining three mutants, there was either a lack of significant phenotype in either viral backbone or an inconsistent difference between the effect in HPIV3 versus that in HPIV1. There was no apparent pattern indicating whether or not the wild-type amino acid assignments at the importation sites in HPIV1 were conserved between HPIV1 and HPIV3.
TABLE 4.
Comparison of the level of temperature sensitivity in vitro and replication in the respiratory tract of hamsters of homologous mutations in rHPIV1 versus rHPIV3
| Mutant rHPIV1 | Mutation no.a | In vitro ts phenotypeb in:
|
In vivo mean fold-reduction of virus replication in respiratory tract of hamstersb
|
||||
|---|---|---|---|---|---|---|---|
| Nasal turbinate
|
Lung
|
||||||
| rHPIV1 | rHPIV3c | rHPIV1 | rHPIV3 | rHPIV1 | rHPIV3 | ||
| rHPIV1 C:F170SMPIV1 | 3 | non-ts | non-tsd | 158 | 500 | 500 | 16 |
| rHPIV1 L:F456LRSV | 8 | 38 | 40e | 500 | 8 | 3,160 | 4 |
| rHPIV1 C:S102Tcp45 | 2 | non-ts | non-ts | 6 | 100 | 10 | 800 |
| rHPIV1 M:P195Tcp45 | 4 | non-ts | non-ts | 5 | <4 | 10 | <4 |
| rHPIV1 F:I423Vcp45 | 5 | non-ts | non-ts | 6 | <4 | 5 | 6 |
| rHPIV1 F:S453Tcp45 | 6 | 38 | non-ts | 32 | −5 | 32 | 1 |
| rHPIV1 HN:R386Acp45 | 7 | 37 | non-ts | 10 | <4 | 8 | 5 |
| rHPIV1 L:Y942Hcp45 | 9 | 37 | 40 | 200 | 6 | 1,000 | 70 |
| rHPIV1 L:L992Fcp45 | 10 | non-ts | 40 | <4 | 1,000 | 40 | 100 |
| rHPIV1 L:L1558Icp45 | 11 | 40 | 39 | 25 | 4,000 | 200 | 6 |
| rHPIV1 3′-N V99Acp45 | 1 | 38 | 40 | 10 | <4 | 16 | <4 |
| rHPIV1 F:I423V/S453Tcp45 | 5 + 6 | 36 | non-ts | ≥1,585 | 50 | ≥5,010 | 250 |
| rHPIV1 L:Y942H/L992Fcp45 | 9 + 10 | 37 | 38 | 500 | >10,000 | 3,980 | >10,000 |
| rHPIV1 L:L992F/L1558Icp45 | 10 + 11 | 39 | 40 | 158 | 45 | 1,585 | 55 |
| rHPIV1 L:Y942H/L992F/L1558Icp45 | 9 + 10 + 11 | 37 | 39 | ≥1,585 | 398 | 1,995 | 6,300 |
Underlined values indicate at least a 2°C reduction in shutoff temperature or a >10-fold reduction in replication for the indicated virus compared to its heterologous counterpart bearing the same mutation(s).
Data from the present studies and from previous studies (12, 45, 46, 49) of rHPIV1 compared to rHPIV3.
The C protein F170S mutation in MPIV1 resulted in a 105-fold reduction in the 50% lethal dose compared to the wild-type virus in mice and an approximately 1,000-fold reduction in replication in the lungs of infected mice (16).
The L protein F521L mutation in RSVcpts530 resulted in a shutoff temperature of 39°C and a 10-fold reduction of replication in the upper respiratory tract of mice (27).
Immunization of hamsters with rHPIV1 mutants and efficacy against challenge with the biologically derived wild-type HPIV1/Wash/64.
Hamsters were immunized with selected rHPIV1 mutant viruses and, after 35 or 36 days, were challenged with a biologically derived wild-type HPIV1. Attenuated rHPIV1 vaccine candidates bearing the C:F170S (no. 3), L:F456L (no. 8), L:L992F (no. 10), or L:L558I (no. 11) single mutation or the L:L992F/L558I (no. 10 plus no. 11) pair of mutations induced both a neutralizing antibody response in serum and resistance to HPIV1 challenge (Table 5). Three other viruses were overattenuated for hamsters, as indicated by a poor antibody response to infection and a lack of induction of protection against challenge; these include those bearing the L:Y942H (no. 9) single mutation, the F:I423V/S453T (no. 5 plus no. 6) combination, or the L:Y942H/L992F/L1558I (no. 9 plus no. 10 plus no. 11) combination (Table 5). The remaining tested mutant, bearing the combination of Y942H/L992F (no. 9 plus no. 10), induced a low-to-moderate level of HPIV1-specific antibody in serum and protection against challenge.
TABLE 5.
Immunization of hamsters with rHPIV1 mutant viruses and their efficacy against challenge with wild-type HPIV1
| Immunizing virusa | Mutation numberb | No. of animals | Titer of neutralizing antibody in serumc | Mean challenged virus titere (log10 TCID50/g ± SE)
|
|
|---|---|---|---|---|---|
| Nasal turbinate | Lung | ||||
| rHPIV1 | 12 | 6.4 ± 0.1 | 1.5 ± 0.4 | 1.5 ± 0.1 | |
| rHPIV1 C:F170SMPIV1 | 3 | 6 | 6.2 ± 0.4 | 1.9 ± 0.3 | 1.5 ± 0.1 |
| rHPIV1 L:F456LRSV | 8 | 6 | 4.5 ± 0.2 | 3.3 ± 0.7 | 2.8 ± 0.5 |
| rHPIV1 F:I423V/S453Tcp45 | 5 + 6 | 6 | ≤1.0 ± 0.0 | 4.8 ± 0.2 | 3.4 ± 0.5 |
| rHPIV1 L:Y942Hcp45 | 9 | 6 | 1.2 ± 0.2 | 5.1 ± 0.4 | 4.3 ± 0.2 |
| rHPIV1 L:L992Fcp45 | 10 | 6 | 4.5 ± 0.8 | 1.7 ± 0.2 | ≤1.5 ± 0.0 |
| rHPIV1 L:L1558Icp45 | 11 | 6 | 5.1 ± 0.6 | 2.2 ± 0.2 | ≤1.5 ± 0.0 |
| rHPIV1 L:Y942H/L992Fcp45 | 9 + 10 | 6 | 2.4 ± 0.9 | 4.0 ± 0.5 | 2.9 ± 0.6 |
| rHPIV1 L:L992F/L1558Icp45 | 10 + 11 | 6 | 5.0 ± 0.5 | 2.4 ± 0.3 | 2.0 ± 0.3 |
| rHPIV1 L:Y942H/L992F/L1558Icp45 | 9 + 10 + 11 | 6 | ≤1.0 ± 0.0 | 4.6 ± 0.5 | 4.0 ± 0.5 |
| Nonef | 12 | ≤1.0 ± 0.0 | 5.1 ± 0.1 | 4.8 ± 0.3 | |
Hamsters were immunized intranasally with 106 TCID50 of the indicated virus.
The mean titer of neutralizing antibody in serum collected 3 to 4 weeks postimmunization (reciprocal mean log2 ± standard error [SE]). The preimmunization titer on day 0 was ≤1.0.
Hamsters were challenged with 106 TCID50 of biologically derived wild-type HPIV1/Wash/64 virus on day 35 or 36 postinoculation. Lungs and nasal turbinates were harvested on day 4 postchallenge.
Values in bold show a 100-fold or greater reduction in titer compared to the titer of the control group that was not immunized.
The animals were administered the L15 medium that was used as diluent for the virus groups.
DISCUSSION
The ability to introduce predetermined mutations into live recombinant virus via reverse genetics provides tremendous flexibility for developing improved live-attenuated virus vaccines. However, it is necessary to have a specific strategy for developing attenuated derivatives from the wild-type recombinant parent. Wild-type HPIV1 was recently recovered from cDNA (39), but there was a complete lack of any known mutations that attenuate HPIV1. However, other studies with recombinant HPIV3 have shown that attenuating mutations could be developed by importing known attenuating mutations from related heterologous viruses into HPIV3 by using sequence alignments as a guide (12, 49). In the present study, this strategy was used to identify a series of point mutations that confer the att phenotype when imported singly or in combination into HPIV1, which provides a strategy for the expedited development of live-attenuated HPIV1 vaccine candidates.
One of the major sources of the mutations that were evaluated for importation into HPIV1 was the HPIV3cp45 virus, which is an excellent HPIV3 vaccine candidate that exhibits a satisfactory balance between attenuation and immunogenicity and retains the attenuation phenotype after replication in vivo (29, 30). This phenotypic stability is provided by four single attenuating mutations and one pair of attenuating mutations, namely, one non-ts mutation in C, a set of two non-ts mutations in F, and three independent ts mutations in L (45, 46). HPIV3cp45 also contains nine other mutations involving nucleotide substitutions in noncoding regions or amino acid substitutions; none of these was significantly attenuating when introduced previously into wild-type HPIV3 on its own or in several combinations (45, 46), although the possibility exists that these additional mutations contribute to the cp45 phenotype when present with the full complement of mutations. Out of the total of 15 amino acid or nucleotide differences between HPIV3cp45 and its wild-type parent (46, 51), 12 of these, including the 5 single or paired att mutations, could be imported into rHPIV1 to attempt to rapidly produce an HPIV1 vaccine. However, a viable rHPIV1 vaccine bearing all 12 mutations could not be recovered from cDNA. We also found that one set of L protein mutations, namely, Y942H and L1558I (no. 9 plus no. 11), could also not be recovered in infectious virus and that the set of all three cp45 L protein mutations (no. 9 plus no. 10 plus no. 11) could be recovered only at a reduced efficiency and only with the acquisition of adventitious mutations in L. While this finding indicated that incompatibility among L protein mutations might be involved in the inability to recover HPIV1 containing all 12 cp45 mutations, we were also unable to recover rHPIV1 containing a subset of 9 mutations that did not include the 3 in L. Thus, there was also apparently an incompatibility within this subset of nine. Since this strategy of importing the full set of cp45 mutations into rHPIV1 did not yield a vaccine candidate, we next sought to pursue a second strategy previously employed for RSV and HPIV3 vaccine development (4, 8, 10, 36), namely, the identification of individual attenuating mutations that then can be assembled in various combinations of two or more mutations into an rHPIV1 vaccine candidate. The importation of mutations, both singly and in combinations, into rHPIV1 from HPIV3cp45 and also from mutants of MPIV1 and RSV identified a series of mutations in C, F, and L that each imposed a 100-fold or greater reduction in replication of rHPIV1 in the upper or lower respiratory tract of hamsters.
Two attenuating mutations in C, one from HPIV3cp45 and one from MPIV1, were introduced into rHPIV1. The mutation C:S102T from HPIV3cp45 (no. 2) attenuated HPIV3 wild-type virus at least 100-fold in both the lungs and nasal turbinates but attenuated HPIV1 wild-type virus only 10-fold or less (Table 4). The amino acid residue 102 in C is not conserved between HPIV3 and HPIV1, which might explain its lack of attenuation in the rHPIV1 background. In contrast, the F170 residue in C (no. 3) is conserved among MPIV1, HPIV1, and HPIV3, and its importation from MPIV1 into both rHPIV3 (12) and HPIV1 conferred an attenuation phenotype for both the upper and lower respiratory tract of hamsters (Table 4). In MPIV1, the F170S mutation in C also conferred a high level of attenuation of replication in the lower respiratory tract of mice (16). It was previously found that the F170S mutation in the C protein of HPIV3 also specified a high level of attenuation in nonhuman primates (12), indicating that the ability of this mutation to attenuate parainfluenza viruses in vivo operates in three different viral backbones, MPIV1, HPIV1 and HPIV3, and in three different animal species, mice, hamsters, and African green monkeys. Hamsters infected with a recombinant HPIV1 bearing the F170S mutation in C were protected against challenge with wild-type virus. Thus, the F170S mutation has three desirable properties for incorporation into an rHPIV1 vaccine candidate: it imparts a non-ts attenuation phenotype and is immunogenic and protective.
The attenuation conferred by the F170S mutation in C of MPIV1 (no. 3) is most likely based on the ability of the set of four C proteins (C′, C, Y1, and Y2) to modulate the host's immune response by inhibition of interferon (IFN) signaling through the Jak/Stat pathway by targeting Stat 1 for degradation (17-19). The F170S mutation in MPIV1 inhibited the ability of the C protein to bind Stat 1 (17). Also, the F170S mutation is associated with a loss in the ability of MPIV1 to inhibit the induction of IFN-β by infected cells (52). Thus, it is reasonable to hypothesize that the attenuation phenotype of the F170S mutation in HPIV1 similarly reflects the loss of the ability to inhibit both the induction of IFN-α and IFN-β and the establishment of an IFN-mediated antiviral state. It is becoming increasingly clear that attenuation of a variety of respiratory viruses can be achieved by mutation in a protein whose function is to inhibit the host's IFN response (15, 19, 20).
A second non-ts att mutation was previously identified in the F gene of HPIV3cp45, involving a set of two amino acids (I420V and A450T, no. 5 plus no. 6) that were substituted for those in wild-type HPIV3 F. However, the phenotype associated with each mutation individually in HPIV3 had not been investigated previously. In the present study, we found that neither of the individual amino acid substitutions in F of HPIV3 conferred the att phenotype in hamsters, indicating that the two amino acid substitutions act synergistically. In both rHPIV1 and rHPIV3, the conserved I420V mutation (I423V in HPIV1; no. 5) did not specify the ts or att phenotype when present as a single mutation (Table 4). In contrast, in HPIV1, the nonconserved S453T mutation (no. 6) specified both the ts and a partial att (32-fold reduction in replication) phenotype as a single mutation. The double mutant rHPIV1 F:I423V/S453T was highly ts, whereas in the HPIV3 background the homologous mutants were not ts. Thus, the nonconserved substitution at residue 453 in HPIV1 specified an unexpected phenotype in both the single and double mutants. The double rHPIV1 I423V/S453T mutant was also the most attenuated rHPIV1 mutant identified (Table 4), indicating that the two mutations act synergistically in HPIV1, as is the case for HPIV3. This greater level of temperature sensitivity and attenuation of the F gene mutation pair in HPIV1 than in HPIV3 might be a partial explanation for our failure to isolate the rHPIV1cp45 derivatives bearing this pair of F mutations in the context of other HPIV3cp45 mutations, since this virus was the least efficient of all of the mutants for replication in vitro at the permissive temperature of 32°C. Although the double mutant was overattenuated in hamsters, the hamster is not a natural host, and the virus might be less restricted and appropriately attenuated in humans. Thus, the single S453T or the double I423V/S453T mutation might be useful attenuating mutations in an rHPIV1 vaccine.
Four amino acid substitutions were introduced individually or in various combinations into the L polymerase of HPIV1. One, the F456L mutation imported from the L gene of RSV cpts530 (no. 8), specified the ts and att phenotypes when introduced into either HPIV1 or HPIV3 (49) (Table 4). However, in both RSV and HPIV3, this mutation specified only a modest ts attenuation phenotype in the upper respiratory tract of hamsters (27, 49). In contrast, the L protein F456L mutation in rHPIV1 conferred a higher level of temperature sensitivity and was highly attenuating for replication in the respiratory tract of hamsters (Table 4). Although it was highly attenuated for replication, it did provide partial protection against challenge with wild-type HPIV1 in the lower respiratory tract of hamsters.
It has previously been demonstrated that each of the three cp45 mutations in the L protein imparted both the ts phenotype and an att phenotype when placed individually into an rHPIV3 wild-type backbone (45). In HPIV1, the L protein mutations at amino acids 942 (no. 9) and 1558 (no. 11) specified both the ts and att phenotypes, but the mutation at position 992 was not ts and was only weakly attenuating, specifying a 40-fold restriction in replication in the lower respiratory tract alone. rHPIV1 mutants bearing various combinations of the three cp45 mutations were recovered, and the following observations were made. First, it was not possible to isolate an rHPIV1 mutant containing the pair of mutations at 942 and 1558, even though this double mutant was readily recovered and propagated in the HPIV3 background (45). In addition, it was difficult to isolate a mutant containing all three mutations, and the triple mutant that was isolated has adventitious mutations in L that might have been necessary for its rescue. These observations suggest that complex interactions are occurring among the L gene mutations in the rHPIV1 background, as has been previously observed in the HPIV3 background (45). Second, combining the cp45 L mutations in rHPIV1 led to an increase in temperature sensitivity or attenuation. Third, of the three tested combinations of the three cp45 L protein mutations, two (Y942H/L992F, no. 9 plus no. 10; and Y942H/L992F/L1558I, no. 9 plus no. 10 plus no. 11) were overattenuated in the hamster, while the third (L992F/L1558I, no. 10 plus no. 11) induced a neutralizing antibody response and resistance to HPIV1 challenge in hamsters. This finding indicates that such a combination of mutations might be useful in an HPIV1 vaccine.
Thus, 8 of 15 rHPIV1 mutants bearing imported individual or combined mutations from heterologous paramyxoviruses were moderately (40-fold) to highly (100- to 5,000-fold) attenuated for replication in either the lower or upper respiratory tract of hamsters. Both non-ts and ts attenuating mutations were identified. Immunization of hamsters with rHPIV1 mutants bearing one or two such imported mutations induced resistance to challenge with wild-type HPIV1. It should now be possible to begin to produce live-attenuated HPIV1 vaccine candidates containing multiple ts and non-ts mutations that are both genetically stable and immunogenic. Live-attenuated HPIV1 vaccines can also serve as vectors for the glycoproteins of heterologous viruses to protect against the disease caused by HPIV1 and other human pathogens, as has been demonstrated for BPIV3 and HPIV3 (13, 43, 44, 47, 48).
Acknowledgments
We thank Joe Blaney, Sheila Nolan, and Emmalene Bartlett for helpful reviews of the manuscript.
REFERENCES
- 1.Atmar, R. L., E. Guy, K. K. Guntupalli, J. L. Zimmerman, V. D. Bandi, B. D. Baxter, and S. B. Greenberg. 1998. Respiratory tract viral infections in inner-city asthmatic adults. Arch. Intern. Med. 158:2453-2459. [DOI] [PubMed] [Google Scholar]
- 2.Belshe, R. B., and F. K. Hissom. 1982. Cold adaptation of parainfluenza virus type 3: induction of three phenotypic markers. J. Med. Virol. 10:235-242. [DOI] [PubMed] [Google Scholar]
- 3.Chanock, R. M., B. R. Murphy, and P. L. Collins. 2001. Parainfluenza viruses, p. 1341-1379. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 1. Lippincott Williams & Wilkins, Philadelphia, Pa.
- 4.Collins, P. L., and B. R. Murphy. 2002. Respiratory syncytial virus: reverse genetics and vaccine strategies. Virology 296:204-211. [DOI] [PubMed] [Google Scholar]
- 5.Collins, P. L., S. S. Whitehead, A. Bukreyev, R. Fearns, M. N. Teng, K. Juhasz, R. M. Chanock, and B. R. Murphy. 1999. Rational design of live-attenuated recombinant vaccine virus for human respiratory syncytial virus by reverse genetics. Adv. Virus Res. 54:423-451. [DOI] [PubMed] [Google Scholar]
- 6.Cortez, K. J., D. D. Erdman, T. C. Peret, V. J. Gill, R. Childs, A. J. Barrett, and J. E. Bennett. 2001. Outbreak of human parainfluenza virus 3 infections in a hematopoietic stem cell transplant population. J. Infect. Dis. 184:1093-1097. [DOI] [PubMed] [Google Scholar]
- 7.Counihan, M. E., D. K. Shay, R. C. Holman, S. A. Lowther, and L. J. Anderson. 2001. Human parainfluenza virus-associated hospitalizations among children less than five years of age in the United States. Pediatr. Infect. Dis. J. 20:646-653. [DOI] [PubMed] [Google Scholar]
- 8.Crowe, J. E. 2001. Respiratory syncytial virus vaccine development. Vaccine 20(Suppl. 1):S32-S37. [DOI] [PubMed] [Google Scholar]
- 9.Crowe, J. E., Jr., P. T. Bui, G. R. Siber, W. R. Elkins, R. M. Chanock, and B. R. Murphy. 1995. Cold-passaged, temperature-sensitive mutants of human respiratory syncytial virus (RSV) are highly attenuated, immunogenic, and protective in seronegative chimpanzees, even when RSV antibodies are infused shortly before immunization. Vaccine 13:847-855. [DOI] [PubMed] [Google Scholar]
- 10.Crowe, J. E., Jr., P. L. Collins, R. M. Chanock, and B. R. Murphy. 1997. Vaccines against respiratory syncytial virus and parainfluenza virus type 3, p. 711-725. In M. M. Levine, G. C. Woodrow, J. B. Kaper, and G. S. Cobon (ed.), New generation vaccines, 2nd ed. Marcel Dekker, Inc., New York, N.Y.
- 11.Durbin, A. P., S. L. Hall, J. W. Siew, S. S. Whitehead, P. L. Collins, and B. R. Murphy. 1997. Recovery of infectious human parainfluenza virus type 3 from cDNA. Virology 235:323-332. [DOI] [PubMed] [Google Scholar]
- 12.Durbin, A. P., J. M. McAuliffe, P. L. Collins, and B. R. Murphy. 1999. Mutations in the C, D, and V open reading frames of human parainfluenza virus type 3 attenuate replication in rodents and primates. Virology 261:319-330. [DOI] [PubMed] [Google Scholar]
- 13.Durbin, A. P., M. H. Skiadopoulos, J. M. McAuliffe, J. M. Riggs, S. R. Surman, P. L. Collins, and B. R. Murphy. 2000. Human parainfluenza virus type 3 (PIV3) expressing the hemagglutinin protein of measles virus provides a potential method for immunization against measles virus and PIV3 in early infancy. J. Virol. 74:6821-6831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fiore, A. E., C. Iverson, T. Messmer, D. Erdman, S. M. Lett, D. F. Talkington, L. J. Anderson, B. Fields, G. M. Carlone, R. F. Breiman, and M. S. Cetron. 1998. Outbreak of pneumonia in a long-term care facility: antecedent human parainfluenza virus 1 infection may predispose to bacterial pneumonia. J. Am. Geriatr. Soc. 46:1112-1117. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Sastre, A. 2001. Inhibition of interferon-mediated antiviral responses by influenza A viruses and other negative-strand RNA viruses. Virology 279:375-384. [DOI] [PubMed] [Google Scholar]
- 16.Garcin, D., M. Itoh, and D. Kolakofsky. 1997. A point mutation in the Sendai virus accessory C proteins attenuates virulence for mice, but not virus growth in cell culture. Virology 238:424-431. [DOI] [PubMed] [Google Scholar]
- 17.Garcin, D., J. B. Marq, S. Goodbourn, and D. Kolakofsky. 2003. The amino-terminal extensions of the longer Sendai virus C proteins modulate pY701-Stat1 and bulk Stat1 levels independently of interferon signaling. J. Virol. 77:2321-2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcin, D., J. B. Marq, L. Strahle, P. le Mercier, and D. Kolakofsky. 2002. All four Sendai virus C proteins bind Stat1, but only the larger forms also induce its mono-ubiquitination and degradation. Virology 295:256-265. [DOI] [PubMed] [Google Scholar]
- 19.Gotoh, B., T. Komatsu, K. Takeuchi, and J. Yokoo. 2001. Paramyxovirus accessory proteins as interferon antagonists. Microbiol. Immunol. 45:787-800. [DOI] [PubMed] [Google Scholar]
- 20.Gotoh, B., T. Komatsu, K. Takeuchi, and J. Yokoo. 2002. Paramyxovirus strategies for evading the interferon response. Rev. Med. Virol. 12:337-357. [DOI] [PubMed] [Google Scholar]
- 21.Hall, S. L., C. M. Sarris, E. L. Tierney, W. T. London, and B. R. Murphy. 1993. A cold-adapted mutant of parainfluenza virus type 3 is attenuated and protective in chimpanzees. J. Infect. Dis. 167:958-962. [DOI] [PubMed] [Google Scholar]
- 22.Hall, S. L., A. Stokes, E. L. Tierney, W. T. London, R. B. Belshe, F. C. Newman, and B. R. Murphy. 1992. Cold-passaged human parainfluenza type 3 viruses contain ts and non-ts mutations leading to attenuation in rhesus monkeys. Virus Res. 22:173-184. [DOI] [PubMed] [Google Scholar]
- 23.Heikkinen, T., M. Thint, and T. Chonmaitree. 1999. Prevalence of various respiratory viruses in the middle ear during acute otitis media. N. Engl. J. Med. 340:260-264. [DOI] [PubMed] [Google Scholar]
- 24.Henderson, F. W., A. M. Collier, M. A. Sanyal, J. M. Watkins, D. L. Fairclough, W. A. Clyde, Jr., and F. W. Denny. 1982. A longitudinal study of respiratory viruses and bacteria in the etiology of acute otitis media with effusion. N. Engl. J. Med. 306:1377-1383. [DOI] [PubMed] [Google Scholar]
- 25.Itoh, M., Y. Isegawa, H. Hotta, and M. Homma. 1997. Isolation of an avirulent mutant of Sendai virus with two amino acid mutations from a highly virulent field strain through adaptation to LLC-MK2 cells. J. Gen. Virol. 78:3207-3215. [DOI] [PubMed] [Google Scholar]
- 26.Jokinen, C., L. Heiskanen, H. Juvonen, S. Kallinen, M. Kleemola, M. Koskela, M. Leinonen, P. R. Ronnberg, P. Saikku, M. Sten, A. Tarkiainen, H. Tukiainen, K. Pyorala, and P. H. Makela. 2001. Microbial etiology of community-acquired pneumonia in the adult population of 4 municipalities in eastern Finland. Clin. Infect. Dis. 32:1141-1154. [DOI] [PubMed] [Google Scholar]
- 27.Juhasz, K., B. R. Murphy, and P. L. Collins. 1999. The major attenuating mutations of the respiratory syncytial virus vaccine candidate cpts530/1009 specify temperature-sensitive defects in transcription and replication and a non-temperature-sensitive alteration in mRNA termination. J. Virol. 73:5176-5180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Juhasz, K., S. S. Whitehead, P. T. Bui, J. M. Biggs, J. E. Crowe, C. A. Boulanger, P. L. Collins, and B. R. Murphy. 1997. The temperature-sensitive (ts) phenotype of a cold-passaged (cp) live attenuated respiratory syncytial virus vaccine candidate, designated cpts530, results from a single amino acid substitution in the L protein. J. Virol. 71:5814-5819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karron, R. A., R. B. Belshe, P. F. Wright, B. Thumar, B. Burns, F. Newman, J. C. Cannon, J. Thompson, T. Tsai, M. Paschalis, S. L. Wu, Y. Mitcho, J. Hackell, B. R. Murphy, and J. M. Tatem. 2003. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in young infants. Pediatr. Infect. Dis. J. 22:394-405. [DOI] [PubMed] [Google Scholar]
- 30.Karron, R. A., P. F. Wright, F. K. Newman, M. Makhene, J. Thompson, R. Samorodin, M. H. Wilson, E. L. Anderson, M. L. Clements, B. R. Murphy, and R. B. Belshe. 1995. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in healthy infants and children. J. Infect. Dis. 172:1445-1450. [DOI] [PubMed] [Google Scholar]
- 31.Lewis, V. A., R. Champlin, J. Englund, R. Couch, J. M. Goodrich, K. Rolston, D. Przepiorka, N. Q. Mirza, H. M. Yousuf, M. Luna, G. P. Bodey, and E. Whimbey. 1996. Respiratory disease due to parainfluenza virus in adult bone marrow transplant recipients. Clin. Infect. Dis. 23:1033-1037. [DOI] [PubMed] [Google Scholar]
- 32.Marx, A., H. E. Gary, Jr., B. J. Marston, D. D. Erdman, R. F. Breiman, T. J. Torok, J. F. Plouffe, T. M. File, Jr., and L. J. Anderson. 1999. Parainfluenza virus infection among adults hospitalized for lower respiratory tract infection. Clin. Infect. Dis. 29:134-140. [DOI] [PubMed] [Google Scholar]
- 33.Marx, A., T. J. Torok, R. C. Holman, M. J. Clarke, and L. J. Anderson. 1997. Pediatric hospitalizations for croup (laryngotracheobronchitis): biennial increases associated with human parainfluenza virus 1 epidemics. J. Infect. Dis. 176:1423-1427. [DOI] [PubMed] [Google Scholar]
- 34.Matsuoka, Y., J. Curran, T. Pelet, D. Kolakofsky, R. Ray, and R. W. Compans. 1991. The P gene of human parainfluenza virus type 1 encodes P and C proteins but not a cysteine-rich V protein. J. Virol. 65:3406-3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moeller, K., I. Duffy, P. Duprex, B. Rima, R. Beschorner, S. Fauser, R. Meyermann, S. Niewiesk, V. ter Meulen, and J. Schneider-Schaulies. 2001. Recombinant measles viruses expressing altered hemagglutinin (H) genes: functional separation of mutations determining H antibody escape from neurovirulence. J. Virol. 75:7612-7620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy, B. R., and P. L. Collins. 2002. Live-attenuated virus vaccines for respiratory syncytial and parainfluenza viruses: applications of reverse genetics. J. Clin. Investig. 110:21-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murphy, B. R., E. J. Park, P. Gottlieb, and K. Subbarao. 1997. An influenza A live attenuated reassortant virus possessing three temperature-sensitive mutations in the PB2 polymerase gene rapidly loses temperature sensitivity following replication in hamsters. Vaccine 15:1372-1378. [DOI] [PubMed] [Google Scholar]
- 38.Murphy, B. R., D. D. Richman, E. G. Chalhub, C. P. Uhlendorf, S. Baron, and R. M. Chanock. 1975. Failure of attenuated temperature-sensitive influenza A (H3N2) virus to induce heterologous interference in humans to parainfluenza type 1 virus. Infect. Immun. 12:62-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Newman, J. T., S. R. Surman, J. M. Riggs, C. T. Hansen, P. L. Collins, B. R. Murphy, and M. H. Skiadopoulos. 2002. Sequence analysis of the Washington/1964 strain of human parainfluenza virus type 1 (HPIV1) and recovery and characterization of wild-type recombinant HPIV1 produced by reverse genetics. Virus Genes 24:77-92. [DOI] [PubMed] [Google Scholar]
- 40.Power, U. F., K. W. Ryan, and A. Portner. 1992. The P genes of human parainfluenza virus type 1 clinical isolates are polycistronic and microheterogeneous. Virology 189:340-343. [DOI] [PubMed] [Google Scholar]
- 41.Reed, G., P. H. Jewett, J. Thompson, S. Tollefson, and P. F. Wright. 1997. Epidemiology and clinical impact of parainfluenza virus infections in otherwise healthy infants and young children <5 years old. J. Infect. Dis. 175:807-813. [DOI] [PubMed] [Google Scholar]
- 42.Rochat, S., H. Komada, and D. Kolakofsky. 1992. Loss of V protein expression in human parainfluenza virus type 1 is not a recent event. Virus Res. 24:137-144. [DOI] [PubMed] [Google Scholar]
- 43.Schmidt, A. C., J. M. McAuliffe, B. R. Murphy, and P. L. Collins. 2001. Recombinant bovine/human parainfluenza virus type 3 (B/HPIV3) expressing the respiratory syncytial virus (RSV) G and F proteins can be used to achieve simultaneous mucosal immunization against RSV and HPIV3. J. Virol. 75:4594-4603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schmidt, A. C., D. R. Wenzke, J. M. McAuliffe, M. St. Claire, W. R. Elkins, B. R. Murphy, and P. L. Collins. 2002. Mucosal immunization of rhesus monkeys against respiratory syncytial virus subgroups A and B and human parainfluenza virus type 3 by using a live cDNA-derived vaccine based on a host range-attenuated bovine parainfluenza virus type 3 vector backbone. J. Virol. 76:1089-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Skiadopoulos, M. H., A. P. Durbin, J. M. Tatem, S. L. Wu, M. Paschalis, T. Tao, P. L. Collins, and B. R. Murphy. 1998. Three amino acid substitutions in the L protein of the human parainfluenza virus type 3 cp45 live attenuated vaccine candidate contribute to its temperature-sensitive and attenuation phenotypes. J. Virol. 72:1762-1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Skiadopoulos, M. H., S. Surman, J. M. Tatem, M. Paschalis, S. L. Wu, S. A. Udem, A. P. Durbin, P. L. Collins, and B. R. Murphy. 1999. Identification of mutations contributing to the temperature-sensitive, cold-adapted, and attenuation phenotypes of the live-attenuated cold-passage 45 (cp45) human parainfluenza virus 3 candidate vaccine. J. Virol. 73:1374-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skiadopoulos, M. H., S. R. Surman, J. M. Riggs, P. L. Collins, and B. R. Murphy. 2001. A chimeric human-bovine parainfluenza virus type 3 expressing measles virus hemagglutinin is attenuated for replication but is still immunogenic in rhesus monkeys. J. Virol. 75:10498-10504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Skiadopoulos, M. H., S. R. Surman, J. M. Riggs, C. Orvell, P. L. Collins, and B. R. Murphy. 2002. Evaluation of the replication and immunogenicity of recombinant human parainfluenza virus type 3 vectors expressing up to three foreign glycoproteins. Virology 297:136-152. [DOI] [PubMed] [Google Scholar]
- 49.Skiadopoulos, M. H., S. R. Surman, M. St. Claire, W. R. Elkins, P. L. Collins, and B. R. Murphy. 1999. Attenuation of the recombinant human parainfluenza virus type 3 cp45 candidate vaccine virus is augmented by importation of the respiratory syncytial virus cpts530 L polymerase mutation. Virology 260:125-135. [DOI] [PubMed] [Google Scholar]
- 50.Skiadopoulos, M. H., T. Tao, S. R. Surman, P. L. Collins, and B. R. Murphy. 1999. Generation of a parainfluenza virus type 1 vaccine candidate by replacing the HN and F glycoproteins of the live-attenuated PIV3 cp45 vaccine virus with their PIV1 counterparts. Vaccine 18:503-510. [DOI] [PubMed] [Google Scholar]
- 51.Stokes, A., E. L. Tierney, C. M. Sarris, B. R. Murphy, and S. L. Hall. 1993. The complete nucleotide sequence of two cold-adapted, temperature-sensitive attenuated mutant vaccine viruses (cp12 and cp45) derived from the JS strain of human parainfluenza virus type 3 (PIV3). Virus Res. 30:43-52. [DOI] [PubMed] [Google Scholar]
- 52.Strahle, L., D. Garcin, P. Le Mercier, J. F. Schlaak, and D. Kolakofsky. 2003. Sendai virus targets inflammatory responses, as well as the interferon-induced antiviral state, in a multifaceted manner. J. Virol. 77:7903-7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thompson, J. D., D. G. Higgins, and T. J. Gibson. 1994. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 22:4673-4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van den Hoogen, B. G., J. C. de Jong, J. Groen, T. Kuiken, R. de Groot, R. A. Fouchier, and A. D. Osterhaus. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat. Med. 7:719-724. [DOI] [PMC free article] [PubMed] [Google Scholar]