Abstract
Inflammation is thought to be involved in the pathophysiology of bipolar disorder (BP) and metabolic syndrome. Prior studies evaluated the association between metabolic profiles and cytokines only during certain mood states instead of their changes during treatment. We enrolled drug-naïve patients with BP-II and investigated the correlation between changes in mood symptoms and metabolic indices with changes in plasma cytokine levels after 12 weeks of pharmacological treatment. Drug-naïve patients (n = 117) diagnosed with BP-II according to DSM-IV criteria were recruited. Metabolic profiles (cholesterol, triglyceride, HbA1C, fasting serum glucose, body mass index (BMI) and plasma cytokines (TNF-α, CRP, IL-6, and TGF-β) were measured at baseline and 2, 8, and 12 weeks post-treatment. To adjust within-subject dependence over repeated assessments, multiple linear regressions with generalized estimating equation methods were used. Seventy-six (65.0%) patients completed the intervention. Changes in plasma CRP were significantly associated with changes in BMI (P = 1.7E-7) and triglyceride (P = 0.005) levels. Changes in plasma TGF-β1 were significantly associated with changes in BMI (P = 8.2E-6), cholesterol (P = 0.004), and triglyceride (P = 0.006) levels. However, changes in plasma TNF-α and IL-6 were not associated with changes in any of the metabolic indices. Changes in Hamilton Depression Rating Scale scores were significantly associated with changes in IL-6 (P = 0.003) levels; changes in Young Mania Rating Scale scores were significantly associated with changes in CRP (P = 0.006) and TNF-α (P = 0.039) levels. Plasma CRP and TGF-β1 levels were positively correlated with several metabolic indices in BP-II after 12 weeks of pharmacological intervention. We also hypothesize that clinical symptoms are correlated with certain cytokines. These new findings might be important evidence that inflammation is the pathophysiology of clinical symptoms and metabolic disturbance in BP-II.
Trial Registration
ClinicalTrials.gov NCT01188148.
Introduction
Bipolar II disorder (BP-II), defined as recurrent episodes of depression and hypomania, is frequently misdiagnosed in clinical settings [1]–[4]. It is believed that BP-II is greatly under diagnosed in clinical practice and lacks in-depth research because BP-II has been regarded as a “milder form of Bipolar I disorder (BP-I)” [5], [6]. However, long-term follow-ups show that patients with BP-II have a more chronic course, more mood episodes, more major and minor depressive episodes, and shorter inter-episodes, all of which last longer than those of patients with BP-I [7]–[9]. In addition, suicidal risk seems to be particularly elevated in BP-II [10]. The high rate of suicide in BP-II may be explained by frequent misdiagnoses of the disorder followed by ineffective treatment [11], [12].
Inflammation appears to be involved in the pathophysiology, phenomenology, and treatment response of BP [13]. Activation of the inflammatory response system and increased activity of the proinflammatory cytokines interleukin-6 (IL-6), C-reactive protein (CRP), and tumor necrosis factor (TNF-α) were found during acute manic and depressive states [14], [15] [16]–[18]. However, whether these phenomena are state-dependent and normalize in remission remains controversial [19], [20]. These discrepancies may be explained by methodological differences such as heterogeneity in sample characteristics, sample size, medication received, and not controlling for known comorbidities [13]. However, an understanding of an association between inflammation and BP might reveal novel pathophysiology and treatment options, and it might even benefit investigating using anti-inflammatory medications to treat BP [21], [22].
Patients with BP have a higher prevalence of metabolic syndrome than do the general population [23]–[25]. Obesity is more prevalent in BP and is associated with a worse prognosis and with suicide attempts [26]. Several possible factors might contribute to the high risk of metabolic disturbance in patients with BP. Treatment with second-generation antipsychotics and mood stabilizers such as valproate has been associated with altered lipid profiles [27]–[30]. In addition, dysfunction of the HPA axis, dysregulation of hormones, and neurotransmitters in BP might also contribute to metabolic disturbance [31]–[34].
It has been hypothesized that the increased risk for obesity in populations with mood disorder is a consequence of shared pathophysiological pathways. Obesity is proposed as a chronic low-grade proinflammatory state [35]; alterations in CRP and proinflammatory cytokines such as TNF-α and IL-6 are commonly reported in obesity [36]–[38]. Increased plasma transforming growth factor (TGF)-β1, an anti-inflammatory cytokine, was correlated with dyslipidemia in an animal model [39]. Taking these findings together, the bidirectional relationship between metabolic abnormality and BP may be a consequence of aberrant inflammatory networks. Clarifying the correlation between inflammatory markers and the metabolic profile in BP is worth further investigation.
Most studies have evaluated only the association between metabolic disturbance and inflammatory markers during certain mood states instead of evaluating their changes over a prolonged course of treatment. In the present study, we enrolled drug-naïve patients with BP-II and measured their plasma cytokine levels and metabolic indices before and after they had undergone a 12-week pharmacological intervention. We investigated the correlation between changes in inflammatory markers and metabolic indices after 12 weeks of treatment. The correlation between changes in these inflammatory markers and in clinical symptoms was also investigated.
Methods
Ethic Statement
The research protocol was approved by the Institutional Review Board for the Protection of Human Subjects at Tri-Service General Hospital and at National Cheng Kung University Hospital. After the study protocol had been completely described to the participants, they all signed written informed consent forms before the trial started and before blood samples were drawn.
Patient selection
This study is a subgroup analysis of a clinical trial (Trial registration: NCT01188148 at https://register.clinicaltrials.gov/). The protocol for this trial and supporting CONSORT checklist are available as supporting information; see Checklist S1 and Protocol S1. The original study was a randomized, double-blind, controlled 12-week trial, aimed to investigate whether treating bipolar II disorder with valproate (VPA) plus add-on memantine is more effective than VPA alone (Lee et al., unpublished). The original study protocol was to examine 4 subgroups: VPA + placebo, VPA + memantine, VPA + placebo + cognitive behavioral group therapy, VPA + memantine + cognitive behavioral group therapy. However, because of staff shortage, we were unable to perform cognitive behavioral group therapy. Therefore, only the two groups undergoing pharmacotherapy were included in for the entire 12-week study period. Because the aim of the current study was to investigate the association between inflammation and metabolic profiles, we used only patients from the placebo group for this subgroup analysis to avoid the influence of add-on memantine, which is not a routinely used medication in the treatment of bipolar II disorder. In this way, the result would be more applicable to daily practice.
The study population was recruited from outpatient and inpatient settings in Tri-Service General Hospital in Taipei and at National Cheng Kung University Hospital in Tainan, Taiwan. The inclusion criteria were: a) Patients with BP-II initially evaluated in an interview by an attending psychiatrist and followed-up with a more detailed interview with a clinical psychologist using the Chinese Version of the Modified Schedule of Affective Disorder and Schizophrenia-Life Time (SADS-L) [40], which has good inter-rater reliability [41], to determine Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnoses; b)Han Chinese; c) between 18 and 65 years old. The exclusion criteria were: 1) a major mental illness, borderline personality disorder, drug dependence, or a cognitive disorder other than BP-II; 2) previous use of any psychotropic agent; 3) taking any anti-inflammatory medication before or during the trial period.
Although DSM-IV-TR [42] criteria require a minimum duration of 4 days of hypomania, current epidemiologic data samples [2], [7], [43]–[46] suggest that a 2-day duration is more prevalent in the community; therefore, we used the 2-day minimum for hypomania when diagnosing BP-II.
Study Design
After they had been enrolled in this study, the patients were given open-label valproic acid (500 mg and 1000 mg daily [50–100 μg/ml in plasma]). Only limited use of benzodiazepines (lorazepam; up to 8-mg/day) or fluoxetine (up to 20 mg/day) was allowed as concomitant medication for insomnia, agitation, or irritability. The doses were adjusted based on each patient's clinical manifestations and tolerance. In case of side-effect intolerance or clinical worsening, the patients were withdrawn earlier. The severity of mood symptoms was assessed using the Young Mania Rating Scale (YMRS) [47] and the Hamilton Depression Rating Scale (HDRS) [48], [49]. Clinical ratings were done by research psychiatrists who were trained and experienced in using the rating scales. Symptom severity was assessed at baseline and at 2, 8, and 12 weeks. After the initiation of pharmacological treatment, BMI, lipid profile (cholesterol, triglyceride, high density lipoprotein (HDL), low density lipoprotein (LDL)), fasting serum glucose level, and glycosylated hemoglobin (HbA1C) were measured at baseline and at each visit when symptom severity was assessed.
Ten milliliters of whole blood was withdrawn from the antecubital vein of each patient. Plasma was isolated from the whole blood after it had been centrifuged at 3000 g for 15 min at 4°C, and then it was immediately stored at −80°C. Cytokine levels were quantified using an antibody pair assay system (Flexia; BioSource Intl., Camarillo, CA). Sample processing and data analysis were done according to the manufacturer's instructions. The immunological parameters–CRP, TNF-α, TGF-β, and IL-6–were measured at baseline and at each visit when symptom severity was assessed.
Statistical Analysis
SPSS 18 for Windows was used for statistical computations. Significance was set at P<0.05. Repeated measurements were used to investigate the association of plasma cytokine levels with the metabolic profile (BMI, lipid profile, fasting serum glucose level, and HbA1C) and symptom severity before and after pharmacological treatment. Because all cytokine levels were distributed erratically and showed a significant level of positive skew (Table 1), arithmetic transformations were used to produce approximately normal distributions for further analysis; log (x+1) was used for cytokine levels. To evaluate the possible correlations of the plasma cytokines with the metabolic profile (BMI, lipid profile, fasting serum glucose level, and HbA1C) and symptom severity, the multiple linear regression model was used. The statistical method, the generalized estimating equation (GEE) [50], was set up for multiple linear regression in repeated-measures studies which can accommodate randomly missing data [51]. In the current study, GEE analysis was used to investigate the correlations of the plasma cytokines (dependent variables) with the metabolic profile and symptom severity (all parameters of which were independent variables); time effects (treatment period from baseline to week 12), gender and age were controlled for. To adjust for multiple comparisons, a Bonferroni correction for multiple comparisons was done.
Table 1. Mean HDRS score, YMRS score, and cytokine and metabolic profiles before and after pharmacological treatment.
| Baseline | After 12 Weeks | |
| Number (n) | 117 | 76 |
| Gender (male/female) (n) | 65/52 | 45/31 |
| Age, mean (SD), (years) | 30.66±11.11 | 30.3±11.1 |
| Age at onset (years) | 17.5±5.4 | |
| Number of episodes | 4.3±2.6 | |
| HDRS1 score, mean (SD) | 19.2±5.4 | 9.4±6.5 |
| YMRS2score, mean (SD) | 9.5±4.6 | 5.8±3.9 |
| BMI, mean (SD), (kg/m2) | 23.4±4.9 | 24.3±4.7 |
| Glucose AC, mean (SD), (mg/dL) | 89.8±17.1 | 86.4±25.2 |
| Triglyceride, mean (SD), (mg/dL) | 92.2±73.3 | 97.4±64.8 |
| Cholesterol (total), mean (SD),(mg/dL) | 179.5±35.1 | 183.5±35.1 |
| HDL-C, mean (SD), (mg/dL) | 58.2±16.0 | 58.4±16.0 |
| LDL-C, mean (SD), (mg/dL) | 109.9±30.4 | 112.5±30.9 |
| HbA1C, mean (SD), (%) | 5.54±0.48 | 5.61±1.32 |
| Depakine level, mean (SD), (mg/L) | 67.5±23.5 | |
| CRP (ng/mL) | 1906.6±1916.8 | 1459.5±1630.5 |
| TGF-β1 (pg/mL) | 30788.9±16364.5 | 27145.3±16269.8 |
| TNF-α(pg/mL) | 1.74±1.70 | 1.63±1.80 |
| IL-6 (pg/mL) | 1.51±1.75 | 1.46±2.01 |
VPA: valproate; HDRS: Hamilton Depression Rating Scale; YMRS: Young Mania Rating Scale; CRP: C-reactive protein; TGF-β1: transforming growth factor β1; TNF-α: tumor necrosis factor α; IL-6: interleukin 6.
The power analysis was done using G-Power 3 software [52], [53], and the effect-size conventions were determined according to Buchner et al. [52].
Results
The trial ran from 1st August, 2008 to 31st July, 2012. The first patient was recruited on 2009/8/25 while the last enrolled patient finished on 2012/5/30. One hundred seventeen patients were recruited. All patients with BP-II were first diagnosed, and that they had no history of taking mood stabilizers or antipsychotics was verified.
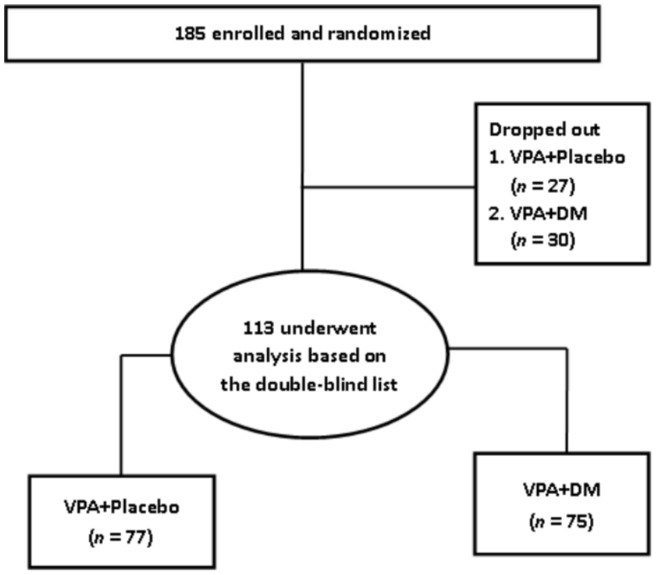
At baseline, 117 patients were assessed. One hundred and three patients were assessed when the trial proceeded to week 2. At week 8, eighty patients were assessed. In the end, seventy-six (65.0%) of the 117 patients completed the 12-week pharmacological treatment and metabolic profile survey (Figure 1) The demographic and clinical characteristics, baseline and endpoint HDRS and YMRS scores, metabolic profiles, and plasma cytokine levels of the patients are shown in Table 1.
Figure 1. Consort flow chart of recruitment.
Correlation analysis was done on all patients in the placebo group. Changes in plasma CRP levels were significantly associated with changes in BMI (P = 1.7E-7) and triglyceride (P = 0.005) levels (Table 2). However, changes in plasma CRP levels were not associated with changes in cholesterol, HDL, LDL, or HbA1C levels. Changes in plasma TGF-β1 levels were significantly associated with changes in BMI (P = 8.2E-6), cholesterol (P = 0.004), and triglyceride (P = 0.006) levels, but not with the changes in HDL, LDL, or HbA1C levels. Changes in plasma TNF-α and IL-6 levels were not associated with any of the changes in metabolic indices after the 12-week treatment (Table 2). Changes in HDRS scores were significantly associated with changes in IL-6 (P = 0.003) levels. In addition, the changes in YMRS scores were significantly associated with changes in CRP (P = 0.006) and TNF-α (P = 0.039) levels (Table 2). However, if we correct for multiple comparisons, only the associations between CRP and TGF-α1 with BMI (both P<0.001) remain significant.
Table 2. Correlation of changes in metabolic profiles and cytokines before and after 12 weeks of pharmacological treatment.
| CRP | TGF-β1 | IL-6 | TNF-α | |||||||||
| B | 95%CI | P | B | 95%CI | P | B | 95%CI | P | B | 95%CI | P | |
| HDRS | 0.624 | −0.28–1.53 | 0.176 | 0.062 | −1.58–1.70 | 0.941 | 2.41 | 0.81–4.0 | 0.003 | 0.027 | −1.31–1.37 | 0.969 |
| YMRS | 0.958 | 0.28–1.64 | 0.006 | −0.47 | −1.62–0.67 | 0.416 | 0.034 | −0.70–0.77 | 0.929 | 0.62 | 0.03–1.21 | 0.039 |
| Triglyceride | 28.03 | 8.6–47.5 | 0.005 | 30.98 | 8.9–53.0 | 0.006 | 14.14 | −2.3–30.6 | 0.092 | −0.066 | −12.6–12.5 | 0.992 |
| Cholesterol | −3.571 | −9.3–2.2 | 0.223 | 13.36 | 4.3–22.5 | 0.004 | −2.21 | −8.0–3.6 | 0.457 | −2.215 | −8.3–3.9 | 0.478 |
| HDL | −4.203 | −8.7–0.3 | 0.067 | 1.07 | −7.5–9.7 | 0.807 | 8.73 | −0.7–18.1 | 0.070 | −0.511 | −3.4–4.4 | 0.799 |
| LDL | −4.682 | −12.1–2.8 | 0.220 | 12.4 | −2.2–27.0 | 0.095 | 0.73 | −8.4–9.8 | 0.876 | −4.366 | −12.8–4.0 | 0.308 |
| BMI | 3.23 | 2.0–4.4 | 1.7E–7** | 5.27 | 3.0–7.6 | 8.2E–6** | −0.067 | −0.3–0.2 | 0.589 | −0.088 | −0.92–0.27 | 0.285 |
| HbA1C | 0.032 | −0.04–0.11 | 0.408 | 0.042 | −0.03–0.12 | 0.283 | 0.034 | −0.02–0.09 | 0.233 | 0.024 | −0.05–0.95 | 0.505 |
CRP: C-reactive protein; TGF-β1: transforming growth factor β1; TNF-α: tumor necrosis factor α; IL-6: interleukin 6.
P<0.001.
The study had a power of approximately 0.33 to detect a small effect, and 0.99 to detect medium and large effects for multiple regression analysis (N = 117). In this power analysis, the effect-size conventions were determined according to Buchner et al. [52] as follows: small effect size = 0.02, medium effect size = 0.15, large effect size = 0.35 for the multiple regression model (alpha = 0.05).
Discussion
We found an association between changes in BMI and CRP, one of the markers of low-grade inflammation. This might mean that elevated levels of CRP are also indicators of a relative increase in BMI. The positive association between CRP and BMI is widely known [54]–[57] in healthy controls and other populations (diabetes, hypertension). A significant association between high CRP and prevalence of metabolic syndrome has been reported [58]. Another study [59] also reported that elevated levels of CRP in adulthood are related to changes in BMI between childhood and adulthood [59]. Our findings about the positive association between the longitudinal changes in BMI and CRP support a positive association of BMI and CRP in drug naïve patients with BP-II. In addition, we also report a possible positive association of change in CRP and triglyceride levels which did not survive the correction of multiple comparisons. Whether this finding supports past studies [60]–[62] that suggest the probable involvement of CRP with metabolic syndrome and obesity still requires further study.
CRP is an acute-phase reactant synthesized in the liver largely in response to proinflammatory cytokines. Adipose tissue can produce proinflammatory cytokines that subsequently increase CRP production [63]. CRP does not cross the blood-brain barrier (BBB) in trace amounts; however, during systemic inflammation and obesity, CRP may increase paracellular permeability of the BBB and impair BBB function [64]. In addition, the level of CRP may indicate the status of inflammation in the brain, which might decrease neurotrophic support and lead to brain dysfunction [65]; such dysfunction is also associated with the pathogenesis of BP. Our findings support the hypothesis that inflammation is the common underlying pathogenesis for the frequently comorbid BP and metabolic disturbances.
The current study also provided initial evidence of a positive correlation between TGF-β1 and and BMI. TGF-β1 induces plasminogen activator inhibitor 1 (PAI-1) synthesis and is associated with BMI in humans [66], [67]. However, our findings of the positive correlation between TGF-β and triglycerides and cholesterol did not survive the correction of a multiple comparison. TGF-β1 is a potent anti-inflammatory cytokine that regulates various physiological processes, including cell proliferation, cell differentiation, extracellular matrix synthesis, and the immune response. It has been implicated in the pathogenesis of autoimmune disease, carcinogenesis, and cardiovascular disease [68]–[70]. Evidence indicates that TGF-β is implicated in significantly higher cardiovascular disease plasma levels of activated TGF-β in patients with coronary heart disease [71]. The correlation between hypercholesterolemia and TGF-β1 has been hypothesized to be caused by activation of the innate immune response, inflammation, and fibrosis [39].Our findings confirmed a positive association between BMI and increased plasma TGF-β1in BP-II. Combining the positive association of plasma CRP and TGF-β1 with BMI and possibly dyslipidemia, we propose that the positive association is a result of activation of the immune response, which warrants study of the mechanisms involved.
However, we found no significant association of the metabolic profile with plasma IL-6 and TNF-α levels, as was previously reported [56], [72]. This inconsistency may be explained by different study designs and the study participants in the current study. We analyzed the association of changes in metabolic profiles and inflammatory factors instead of cross-sectional correlations, as was done in previous studies. In addition, all participants in the current study were drug naïve patients with BP-II undergoing initial short-term pharmacological intervention. The long-term metabolic influences and their association with the inflammatory factors in our patients require additionalfollow-up and investigation.
In treating neuropsychiatric disorders, being able to identify and quantify peripheral biomarkers for diagnosis or monitoring treatment responses still remains a clinical goal. We reported that the decreases in HDRS scores over the study period were associated with decreases in IL-6 levels, and that the decreases in YMRS scores were associated with the decreases in CRP and TNF-α levels. However, these findings did not survive correction for multiple comparisons. Based on our findings, we propose that changes the levels of plasma cytokines may be associated with the severity of mood symptoms in patients with BP-II in a prolonged course of treatment instead of in a cross-sectional study. Other studies [15], [17] have suggested that changes in proinflammatory cytokines may be related to the pathophysiology of BP and to the response to pharmacological treatment. A change in IL-6 levels according to mood state is one of the most consistent findings in BP [15], [16]. Our finding supports a report [73] that IL-6 was positively correlated with HDRS scores. In addition, our data suggest that changes plasma CRP may be associated with the severity of manic symptoms, which agrees with Dickerson et al. [14], who said that mania symptoms but not HDRS scores were associated with the increased production of CRP. The possible association between cytokines and clinical symptoms found in the current study requires additional study to confirm. In addition, whether the combination of these cytokines may be used as biomarkers for the severity of BP-II still requires further investigation using a larger sample size.
Our study has some limitations. First, we measured plasma cytokines in the current study because previous studies suggested that changes in peripheral cytokine expression levels may partially reflect the changes in peripheral levels. However, we were unable to draw a definitive conclusion about this hypothesis [74]. Second, except for the correlation between changes in CRP and TNF-α with changes in BMI, most of our positive findings did not survive correction for multiple testing. Further studies with larger samples are needed to verify our results. To achieve enough power (0.8) for detection of small effect (0.02), we would need a target size around N = 395. Third, it is possible that the medication permitted in the study obscured the mood correlation between cytokines and metabolic indices. Although we tried to limit concomitant treatment medication to only three drugs, our results should still be taken with caution. Fourth, the 2-day duration for hypomania used in the current study is not widely accepted. The positive finding in the current study may not apply to patients with BP-II diagnosed according to the DSM-IV-TR criteria of the 4-day duration for hypomania. Fifth, we did not control for the baseline severity of patients. Unlike past studies that focused on only one pole of the mood spectrum, we assessed both the YMRS and HDRS scores for subsyndromal manic symptoms that were presented in over half of bipolar depressive episodes yet frequently not assessed [75]. By evaluating symptoms on both poles of the mood spectrum, our clinical evaluation is more comprehensive, which may better reflect the association of cytokines and the symptoms of BP. Finally, our study focused only on the metabolic influences after short-term pharmacological intervention. The long-term metabolic influences in our patients require additional follow-up and investigation.
In conclusion, our study provides initial evidence of a positive correlation between plasma CRP and TGF-β1 levels and BMI in drug-naïve patients with BP-II after 12 weeks of pharmacological intervention. The specific roles of cytokines in regulating and maintaining peripheral metabolic health require additional investigation. We also hypothesize that clinical symptoms are correlated with certain cytokines. Whether these cytokines can be used as biomarker of BP-II warrants additional studies. We expect that knowledge of the function of plasma cytokines in metabolic disturbances will benefit the development of novel therapies to modify cytokine levels in order to control both clinical symptoms and metabolic disturbances in BP-II.
Supporting Information
CONSORT Checklist.
(DOC)
Trial Protocol.
(DOC)
Funding Statement
This work was supported in part by grant NSC98-2314-B-006-022-MY3 (to RBL) and NSC98-2314-B-006-022-MY3 (to SYL) from the Taiwan National Science Council, grant DOH 95-TD-M-113-055 (to RBL) from the Taiwan Department of Health, grant NHRI-EX-97-9738NI (to RBL) from the Taiwan National Health Research Institute, and the National Cheng Kung University Project for Promoting Academic Excellence and Developing World Class Research Centers. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Akiskal HS, Pinto O (1999) The evolving bipolar spectrum. Prototypes I, II, III, and IV. Psychiatr Clin North Am 22: 517–534, vii. [DOI] [PubMed]
- 2. Angst J, Gamma A, Sellaro R, Lavori PW, Zhang H (2003) Recurrence of bipolar disorders and major depression. A life-long perspective. Eur Arch Psychiatry Clin Neurosci 253: 236–240. [DOI] [PubMed] [Google Scholar]
- 3. Benazzi F (2001) Bipolar II depression in late life: prevalence and clinical features in 525 depressed outpatients. J Affect Disord 66: 13–18. [DOI] [PubMed] [Google Scholar]
- 4. Benazzi F, Akiskal HS (2003) Refining the evaluation of bipolar II: beyond the strict SCID-CV guidelines for hypomania. J Affect Disord 73: 33–38. [DOI] [PubMed] [Google Scholar]
- 5. Angst J (2007) The bipolar spectrum. Br J Psychiatry 190: 189–191. [DOI] [PubMed] [Google Scholar]
- 6. Vieta E, Suppes T (2008) Bipolar II disorder: arguments for and against a distinct diagnostic entity. Bipolar Disord 10: 163–178. [DOI] [PubMed] [Google Scholar]
- 7. Judd LL, Akiskal HS, Schettler PJ, Coryell W, Maser J, et al. (2003) The comparative clinical phenotype and long term longitudinal episode course of bipolar I and II: a clinical spectrum or distinct disorders? J Affect Disord 73: 19–32. [DOI] [PubMed] [Google Scholar]
- 8. Pallanti S, Quercioli L, Pazzagli A, Rossi A, Dell'Osso L, et al. (1999) Awareness of illness and subjective experience of cognitive complaints in patients with bipolar I and bipolar II disorder. Am J Psychiatry 156: 1094–1096. [DOI] [PubMed] [Google Scholar]
- 9. Vieta E, Gastó C, Otero A, Nieto E, Vallejo J (1997) Differential features between bipolar I and bipolar II disorder. Comprehensive Psychiatry 38: 98–101. [DOI] [PubMed] [Google Scholar]
- 10.Rihmer Z, Pestality P (1999) Bipolar II disorder and suicidal behavior. Psychiatr Clin North Am 22: 667–673, ix–x. [DOI] [PubMed]
- 11. Ghaemi SN, Boiman E, Goodwin FK (2000) Insight and outcome in bipolar, unipolar, and anxiety disorders. Compr Psychiatry 41: 167–171. [DOI] [PubMed] [Google Scholar]
- 12. MacQueen GM, Young LT (2001) Bipolar II disorder: symptoms, course, and response to treatment. Psychiatr Serv 52: 358–361. [DOI] [PubMed] [Google Scholar]
- 13. Goldstein BI, Kemp DE, Soczynska JK, McIntyre RS (2009) Inflammation and the phenomenology, pathophysiology, comorbidity, and treatment of bipolar disorder: a systematic review of the literature. J Clin Psychiatry 70: 1078–1090. [DOI] [PubMed] [Google Scholar]
- 14. Dickerson F, Stallings C, Origoni A, Boronow J, Yolken R (2007) Elevated serum levels of C-reactive protein are associated with mania symptoms in outpatients with bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 31: 952–955. [DOI] [PubMed] [Google Scholar]
- 15. Kim YK, Jung HG, Myint AM, Kim H, Park SH (2007) Imbalance between pro-inflammatory and anti-inflammatory cytokines in bipolar disorder. J Affect Disord 104: 91–95. [DOI] [PubMed] [Google Scholar]
- 16. Knijff EM, Breunis MN, Kupka RW, de Wit HJ, Ruwhof C, et al. (2007) An imbalance in the production of IL-1beta and IL-6 by monocytes of bipolar patients: restoration by lithium treatment. Bipolar Disord 9: 743–753. [DOI] [PubMed] [Google Scholar]
- 17. O'Brien SM, Scully P, Scott LV, Dinan TG (2006) Cytokine profiles in bipolar affective disorder: focus on acutely ill patients. J Affect Disord 90: 263–267. [DOI] [PubMed] [Google Scholar]
- 18. Soderlund J, Olsson SK, Samuelsson M, Walther-Jallow L, Johansson C, et al. (2011) Elevation of cerebrospinal fluid interleukin-1ss in bipolar disorder. J Psychiatry Neurosci 36: 114–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Boufidou F, Nikolaou C, Alevizos B, Liappas IA, Christodoulou GN (2004) Cytokine production in bipolar affective disorder patients under lithium treatment. J Affect Disord 82: 309–313. [DOI] [PubMed] [Google Scholar]
- 20. Knijff EM, Ruwhof C, de Wit HJ, Kupka RW, Vonk R, et al. (2006) Monocyte-derived dendritic cells in bipolar disorder. Biol Psychiatry 59: 317–326. [DOI] [PubMed] [Google Scholar]
- 21. Brietzke E, Kapczinski F (2008) TNF-alpha as a molecular target in bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 32: 1355–1361. [DOI] [PubMed] [Google Scholar]
- 22. Nery FG, Monkul ES, Hatch JP, Fonseca M, Zunta-Soares GB, et al. (2008) Celecoxib as an adjunct in the treatment of depressive or mixed episodes of bipolar disorder: a double-blind, randomized, placebo-controlled study. Hum Psychopharmacol 23: 87–94. [DOI] [PubMed] [Google Scholar]
- 23. Ferguson JM, Shingleton RN (2007) An open-label, flexible-dose study of memantine in major depressive disorder. Clin Neuropharmacol 30: 136–144. [DOI] [PubMed] [Google Scholar]
- 24. Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, et al. (2006) A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 63: 856–864. [DOI] [PubMed] [Google Scholar]
- 25. Zarate CA Jr, Singh JB, Quiroz JA, De Jesus G, Denicoff KK, et al. (2006) A double-blind, placebo-controlled study of memantine in the treatment of major depression. Am J Psychiatry 163: 153–155. [DOI] [PubMed] [Google Scholar]
- 26. Fagiolini A, Frank E, Scott JA, Turkin S, Kupfer DJ (2005) Metabolic syndrome in bipolar disorder: findings from the Bipolar Disorder Center for Pennsylvanians. Bipolar Disord 7: 424–430. [DOI] [PubMed] [Google Scholar]
- 27. Bowden CL, Calabrese JR, McElroy SL, Gyulai L, Wassef A, et al. (2000) A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry 57: 481–489. [DOI] [PubMed] [Google Scholar]
- 28. Reynolds MF, Sisk EC, Rasgon NL (2007) Valproate and neuroendocrine changes in relation to women treated for epilepsy and bipolar disorder: a review. Curr Med Chem 14: 2799–2812. [DOI] [PubMed] [Google Scholar]
- 29. Elmslie JL, Porter RJ, Joyce PR, Hunt PJ, Shand BI, et al. (2009) Comparison of insulin resistance, metabolic syndrome and adiponectin in overweight bipolar patients taking sodium valproate and controls. Aust N Z J Psychiatry 43: 53–60. [DOI] [PubMed] [Google Scholar]
- 30. Chang HH, Yang YK, Gean PW, Huang HC, Chen PS, et al. (2010) The role of valproate in metabolic disturbances in bipolar disorder patients. J Affect Disord 124: 319–323. [DOI] [PubMed] [Google Scholar]
- 31. Kenna HA, Jiang B, Rasgon NL (2009) Reproductive and metabolic abnormalities associated with bipolar disorder and its treatment. Harv Rev Psychiatry 17: 138–146. [DOI] [PubMed] [Google Scholar]
- 32. Steen NE, Methlie P, Lorentzen S, Hope S, Barrett EA, et al. (2011) Increased systemic cortisol metabolism in patients with schizophrenia and bipolar disorder: a mechanism for increased stress vulnerability? J Clin Psychiatry 72: 1515–1521. [DOI] [PubMed] [Google Scholar]
- 33. Taylor V, MacQueen G (2006) Associations between bipolar disorder and metabolic syndrome: A review. J Clin Psychiatry 67: 1034–1041. [DOI] [PubMed] [Google Scholar]
- 34. Vogelzangs N, Penninx BW (2011) [Depressive symptoms, cortisol, visceral fat and metabolic syndrome]. Tijdschr Psychiatr 53: 613–620. [PubMed] [Google Scholar]
- 35. Karalis KP, Giannogonas P, Kodela E, Koutmani Y, Zoumakis M, et al. (2009) Mechanisms of obesity and related pathology: linking immune responses to metabolic stress. FEBS J 276: 5747–5754. [DOI] [PubMed] [Google Scholar]
- 36. Bullo M, Garcia-Lorda P, Megias I, Salas-Salvado J (2003) Systemic inflammation, adipose tissue tumor necrosis factor, and leptin expression. Obes Res 11: 525–531. [DOI] [PubMed] [Google Scholar]
- 37. Das UN (2001) Is obesity an inflammatory condition? Nutrition 17: 953–966. [DOI] [PubMed] [Google Scholar]
- 38. Bornstein SR, Schuppenies A, Wong ML, Licinio J (2006) Approaching the shared biology of obesity and depression: the stress axis as the locus of gene-environment interactions. Mol Psychiatry 11: 892–902. [DOI] [PubMed] [Google Scholar]
- 39. Zhou X, Johnston TP, Johansson D, Parini P, Funa K, et al. (2009) Hypercholesterolemia leads to elevated TGF-beta1 activity and T helper 3-dependent autoimmune responses in atherosclerotic mice. Atherosclerosis 204: 381–387. [DOI] [PubMed] [Google Scholar]
- 40. Endicott J, Spitzer RL (1978) A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry 35: 837–844. [DOI] [PubMed] [Google Scholar]
- 41. Huang SY, Lin WW, Ko HC, Lee JF, Wang TJ, et al. (2004) Possible interaction of alcohol dehydrogenase and aldehyde dehydrogenase genes with the dopamine D2 receptor gene in anxiety-depressive alcohol dependence. Alcohol Clin Exp Res 28: 374–384. [DOI] [PubMed] [Google Scholar]
- 42.American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorder-IV-TR. Washington: American Psychiatric Association.
- 43. Akiskal HS, Djenderedjian AM, Rosenthal RH, Khani MK (1977) Cyclothymic disorder: validating criteria for inclusion in the bipolar affective group. Am J Psychiatry 134: 1227–1233. [DOI] [PubMed] [Google Scholar]
- 44. Akiskal HS, Rosenthal RH, Rosenthal TL, Kashgarian M, Khani MK, et al. (1979) Differentiation of primary affective illness from situational, symptomatic, and secondary depressions. Arch Gen Psychiatry 36: 635–643. [DOI] [PubMed] [Google Scholar]
- 45. Angst J (1998) The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord 50: 143–151. [DOI] [PubMed] [Google Scholar]
- 46. Benazzi F (2001) Is 4 days the minimum duration of hypomania in bipolar II disorder? Eur Arch Psychiatry Clin Neurosci 25: 32–34. [DOI] [PubMed] [Google Scholar]
- 47. Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133: 429–435. [DOI] [PubMed] [Google Scholar]
- 48. Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6: 278–296. [DOI] [PubMed] [Google Scholar]
- 50. Zeger SL, Liang KY, Albert PS (1988) Models for longitudinal data: a generalized estimating equation approach. Biometrics 44: 1049–1060. [PubMed] [Google Scholar]
- 51. Shen CW, Chen YH (2012) Model selection for generalized estimating equations accommodating dropout missingness. Biometrics 68: 1046–1054. [DOI] [PubMed] [Google Scholar]
- 52.Buchner A, Faul F, Erdfelder E (1996) G-power: A Priori, Post Hoc, and Compromise Power Analyses for the Macintosh. Version 2.1.1. ed. Germany.: University of Trier, Trier.
- 53. Faul F, Erdfelder E, Buchner A, Lang A (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41: 1149–1160. [DOI] [PubMed] [Google Scholar]
- 54. Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB (1999) Elevated C-reactive protein levels in overweight and obese adults. JAMA 282: 2131–2135. [DOI] [PubMed] [Google Scholar]
- 55. Bermudez EA, Ridker PM (2002) C-reactive protein, statins, and the primary prevention of atherosclerotic cardiovascular disease. Prev Cardiol 5: 42–46. [DOI] [PubMed] [Google Scholar]
- 56. Marques-Vidal P, Velho S, Waterworth D, Waeber G, von Kanel R, et al. (2012) The association between inflammatory biomarkers and metabolically healthy obesity depends of the definition used. Eur J Clin Nutr 66: 426–435. [DOI] [PubMed] [Google Scholar]
- 57. Zimmet P, Boyko EJ, Collier GR, de Courten M (1999) Etiology of the metabolic syndrome: potential role of insulin resistance, leptin resistance, and other players. Ann N Y Acad Sci 892: 25–44. [DOI] [PubMed] [Google Scholar]
- 58. Vuksan-Cusa B, Sagud M, Jakovljevic M (2010) C-reactive protein and metabolic syndrome in patients with bipolar disorder compared to patients with schizophrenia. Psychiatr Danub 22: 275–277. [PubMed] [Google Scholar]
- 59. Saltevo J, Vanhala M, Kautiainen H, Laakso M (2007) Levels of adiponectin, C-reactive protein and interleukin-1 receptor antagonist are associated with the relative change in body mass index between childhood and adulthood. Diab Vasc Dis Res 4: 328–331. [DOI] [PubMed] [Google Scholar]
- 60. Grundy SM (1999) Hypertriglyceridemia, insulin resistance, and the metabolic syndrome. Am J Cardiol 83: 25F–29F. [DOI] [PubMed] [Google Scholar]
- 61. Laaksonen DE, Niskanen L, Nyyssonen K, Punnonen K, Tuomainen TP, et al. (2004) C-reactive protein and the development of the metabolic syndrome and diabetes in middle-aged men. Diabetologia 47: 1403–1410. [DOI] [PubMed] [Google Scholar]
- 62.Verma S, Yeh ET (2003) C-reactive protein and atherothrombosis–beyond a biomarker: an actual partaker of lesion formation. Am J Physiol Regul Integr Comp Physiol 285: R1253–1256; discussion R1257–1258. [DOI] [PubMed]
- 63. Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, et al. (1997) Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab 82: 4196–4200. [DOI] [PubMed] [Google Scholar]
- 64. Hsuchou H, Kastin AJ, Mishra PK, Pan W (2012) C-Reactive Protein Increases BBB Permeability: Implications for Obesity and Neuroinflammation. Cell Physiol Biochem 30: 1109–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zhu CB, Blakely RD, Hewlett WA (2006) The proinflammatory cytokines interleukin-1beta and tumor necrosis factor-alpha activate serotonin transporters. Neuropsychopharmacology 31: 2121–2131. [DOI] [PubMed] [Google Scholar]
- 66. Alessi MC, Bastelica D, Morange P, Berthet B, Leduc I, et al. (2000) Plasminogen activator inhibitor 1, transforming growth factor-beta1, and BMI are closely associated in human adipose tissue during morbid obesity. Diabetes 49: 1374–1380. [DOI] [PubMed] [Google Scholar]
- 67. Porreca E, Di Febbo C, Vitacolonna E, Baccante G, Di Castelnuovo A, et al. (2002) Transforming growth factor-beta1 levels in hypertensive patients: association with body mass index and leptin. Am J Hypertens 15: 759–765. [DOI] [PubMed] [Google Scholar]
- 68. Grainger DJ, Kemp PR, Metcalfe JC, Liu AC, Lawn RM, et al. (1995) The serum concentration of active transforming growth factor-beta is severely depressed in advanced atherosclerosis. Nat Med 1: 74–79. [DOI] [PubMed] [Google Scholar]
- 69. Majesky MW, Lindner V, Twardzik DR, Schwartz SM, Reidy MA (1991) Production of transforming growth factor beta 1 during repair of arterial injury. J Clin Invest 88: 904–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Massague J (1990) The transforming growth factor-beta family. Annu Rev Cell Biol 6: 597–641. [DOI] [PubMed] [Google Scholar]
- 71. Wang XL, Liu SX, Wilcken DE (1997) Circulating transforming growth factor beta 1 and coronary artery disease. Cardiovasc Res 34: 404–410. [DOI] [PubMed] [Google Scholar]
- 72. Moon YS, Kim DH, Song DK (2004) Serum tumor necrosis factor-alpha levels and components of the metabolic syndrome in obese adolescents. Metabolism 53: 863–867. [DOI] [PubMed] [Google Scholar]
- 73. Brietzke E, Stertz L, Fernandes BS, Kauer-Sant'anna M, Mascarenhas M, et al. (2009) Comparison of cytokine levels in depressed, manic and euthymic patients with bipolar disorder. J Affect Disord 116: 214–217. [DOI] [PubMed] [Google Scholar]
- 74. Pan W, Kastin AJ (1999) Penetration of neurotrophins and cytokines across the blood-brain/blood-spinal cord barrier. Adv Drug Deliv Rev 36: 291–298. [DOI] [PubMed] [Google Scholar]
- 75. Goldberg JF, Perlis RH, Bowden CL, Thase ME, Miklowitz DJ, et al. (2009) Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry 166: 173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT Checklist.
(DOC)
Trial Protocol.
(DOC)