Abstract
The purpose of this study was to determine the association between anthropometric measures of obesity and all-cause mortality in white and African American men and women. The sample included 14,343 adults 18 to 89 years of age. Height, weight, and waist and hip circumferences were measured, and the BMI (kg/m2), body adiposity index (BAI = ([hip circumference in centimeters]/[height in meters])1.5–18), waist-to-height ratio (WHtR) and waist-to-hip ratio (WHR) were computed. Vital status of the participants was determined from linkage with the National Death Index through 2009. Cox regression was used to assess the association between anthropometry and all1cause mortality, adjusting for age, sex, year of baseline examination, study code, smoking status, alcohol consumption and physical activity. Hazard ratios (HR) are expressed per standard deviation of each variable. A total of 438 deaths occurred during 120,637 person-years of follow-up. All anthropometric markers demonstrated significant associations with all-cause mortality in white subjects. In multivariable-adjusted models, BMI (HR 1.34; 95% CI: 1.19 - 1.50), waist circumference (1.41; 1.25 - 1.60), BAI (1.34; 1.17 - 1.53), WHtR (1.46; 1.28 - 1.65) and WHR (1.40; 1.23 - 1.61) all demonstrated significant relationships with mortality in white participants, but not in African Americans. In categorical analyses, there was a significant association between BMI status and mortality in whites but not African Americans. However, the risk associated with elevated waist circumference was almost identical in whites (1.49; 1.15 – 1.94) and African Americans (1.60; 1.06 – 2.40). In summary, this study has demonstrated race differences in the association between anthropometry and all-cause mortality.
INTRODUCTION
African American men and women can expect to live 5 and 3.5 fewer years than white men and women, respectively, under current mortality patterns (1). African Americans have a higher prevalence of obesity (2) and obesity-related co-morbidities such as type 2 diabetes (3); however, it is not clear how much of the racial gap in life expectancy can be explained by differentials in obesity risk and prevalence. The strength of the relationship between BMI and mortality in African Americans is unclear, as some studies have reported a significant association in men (4-7) or women (6, 8), and others have reported an absent or reduced association in either men (9-11) or women (4, 7, 9-13).
In addition to BMI, waist circumference is another common measure of obesity, as it is highly correlated with total body fat and moderately correlated with visceral adipose tissue (14, 15). Several studies have indicated a significant relationship between waist circumference and mortality in U.S. cohorts (8, 10, 11, 16-20); however, the evidence for a potential differential association among white and African Americans is not consistent (5, 10-12, 17). Racial differences in the risk of mortality related to other indices of adiposity and fat distribution such as waist-to-hip circumference ratio (WHR) and waist-to-height ratio (WHtR) have apparently been investigated in only one previous study to our knowledge (10), and the mortality risk associated with the Body Adiposity Index (BAI)(21) has not yet been studied.
The present study was designed to determine the association of several common anthropometric measures of obesity with all-cause mortality rates in a biracial sample of men and women.
SUBJECTS AND METHODS
Sample
The Pennington Center Longitudinal Study (PCLS) is an on-going investigation of the effects of obesity and lifestyle factors on the development of chronic diseases and premature mortality. The sample is composed of volunteers who have participated in a variety of clinical studies, including diet interventions, weight loss, and other metabolic/physiologic studies conducted at the Pennington Biomedical Research Center (PBRC) in Baton Rouge, Louisiana between 1994 and 2009. All data for this analysis were obtained from baseline screening exams prior to enrolment in a specific study. The current analysis included 14,343 participants (5,506 white women, 3,524 African American women, 4,076 white men and 1,237 African American men) 18 to 89 years of age from 243 different studies. Race was self-identified by the participant. Each participant provided their written informed consent and all PCLS procedures were approved by the PBRC Institutional Review Board.
Baseline Examination
Height and weight were measured using a wall-mounted stadiometer and a digital scale, respectively, after the volunteer removed outer clothing, heavy pocket items and shoes. Waist circumference was measured at the midpoint between the inferior border of the ribcage and the superior aspect of the iliac crest using an inelastic measuring tape. Hip circumference was measured at the level of the greater trochanters using an inelastic measuring tape. The BMI was calculated as weight in kg / height in m2, and the BAI was calculated as ([hip circumference in centimeters]/[height in meters])1.5 – 18, and the WHtR and WHR were computed from their component variables. The sample was categorized into underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5 - 24.9 kg/m2), overweight (BMI 25 –29.9 kg/m2, obese class I (BMI 30 – 34.9 kg/m2) and obese class II (BMI ≥ 35 kg/m2) categories as well as low and high waist circumference (> 88 cm in women and > 102 cm in men)(22).
Covariates
Information on several covariates was collected at baseline for inclusion in the statistical models. Participant age was computed from birth and observation dates, year of examination was included as a covariate to account for potential temporal trends in baseline measurements, and a unique study code identifier was included to account for potential differences in participant characteristics across studies. Smoking status, alcohol consumption, and engagement in leisure-time physical activity were self-reported during the baseline data collection.
Ascertainment of Mortality Status
The vital status of all participants and causes of death were determined by linkage to the National Death Index (23). The primary endpoint for this analysis was death from all causes. All deaths occurring between six months after the baseline assessment and December 31, 2009 were included in the analysis. The average length of follow-up was 8.4 y (SD 4.3 y; maximum 16.0 y).
Statistical Analysis
Cox proportional hazards regression was used to assess the association between the anthropometric measures and all-cause mortality rates, adjusting for a variety of covariates as described below. We present the results of four models: Model - includes all participants, adjusted for age, sex and exam year; Model 2 includes all participants, adjusted for age, sex, year of baseline examination, study code, smoking status (never, former, current, unknown), alcohol consumption (no, yes, unknown) and leisure-time physical activity (<4 h/wk, ≥ 4 h/wk, unknown); Model 3 is limited to participants without a history of stroke, heart disease or cancer at baseline, adjusted for age and sex; and Model 4 is also limited to participants without a history of stroke, heart disease or cancer at baseline, and includes the same covariates as Model 2. Analyses were performed on the combined sample of white and African American participants (with race as a covariate), and then stratified by race. Hazard ratios (HR) are expressed per standard deviation of each independent variable. Hazard ratios were also calculated across BMI (normal weight, overweight, obese class I, obese class II) and waist circumference (low, high) categories. Underweight participants were excluded from this categorical analysis given the small sample size (n = 92) and the small number of deaths (n = 2) in this group.
The full sample size (n = 14,343) was available for analyses of BMI; however, the analytic sample size for other variables varied due to missing data. Further, the full sample size was reduced from 14,343 to 13,930 for models 3 and 4, which were limited to participants who were free of stroke, heart disease and cancer at baseline. The proportional hazards assumption of the Cox regression models were assessed by a statistical test of proportionality with time-dependent variables. These tests revealed no violation of the proportional hazards assumption.
Results
The mean age of the sample at baseline was 41.5 (SD 14.5) years. Age was significantly greater in decedents compared to survivors, and all adiposity indicators were significantly higher at baseline in decedents compared to survivors in the total sample, and in white adults (Table 1). Only waist circumference and WHR were significantly higher in African American decedents compared to survivors. Pearson correlations among the adiposity variables are presented in Table 2. In both white and African Americans, all variables are moderately to highly correlated with each other; however, the correlations between WHR and the other variables are somewhat lower.
Table 1.
Baseline characteristics of participants in the Pennington Center Longitudinal Study by mortality status at follow-up.
| Total Sample |
White American |
African American |
||||
|---|---|---|---|---|---|---|
| Survivors | Decedents | Survivors | Decedents | Survivors | Decedents | |
| N | 13905 | 438 | 9285 | 297 | 4620 | 141 |
| % Female | 63.4 | 47.7 | 57.9 | 44.8 | 74.6 | 53.9 |
| Age (y) | 41.1 (14.3) | 54.9 (14.8)* | 41.8 (15.0) | 56.4 (15.5)* | 39.8 (12.8) | 51.8 (12.4)* |
| Age Group (%) | ||||||
| 18-29 y | 26.9 | 6.9 | 27.5 | 8.4 | 25.6 | 3.6 |
| 30-49 y | 42.7 | 26.3 | 38.5 | 19.9 | 51.1 | 39.7 |
| 50-69 y | 28.6 | 50.0 | 31.6 | 51.2 | 22.5 | 47.5 |
| 70-89 y | 1.9 | 16.9 | 2.4 | 20.5 | 0.9 | 9.2 |
| BMI (kg/m2) | 30.5 (7.2) | 32.3 (8.0)* | 29.8 (7.0) | 32.6 (8.4)* | 32.0 (7.5) | 31.7 (7.1) |
| BMI Category (%) | ||||||
| Underweight | 0.7 | 0.5 | 0.7 | 0.7 | 0.6 | 0 |
| Normal Weight | 22.7 | 13.7 | 26.0 | 13.8 | 16.3 | 13.5 |
| Overweight | 28.9 | 27.2 | 30.3 | 25.6 | 26.2 | 30.5 |
| Obese Class I | 24.0 | 29.7 | 22.6 | 29.0 | 26.9 | 31.2 |
| Obese Class II | 23.7 | 29.0 | 20.5 | 31.0 | 30.1 | 24.8 |
| BAI (%) | 31.3 (7.6) | 32.5 (8.7)* | 30.5 (7.4) | 33.0 (8.9)* | 32.9 (7.8) | 31.4 (8.1) |
| Waist Circumference (cm) | 93.2 (16.9) | 102.6 (18.8)* | 92.6 (17.1) | 103.9 (20.0)* | 94.3 (16.4) | 100.0 (15.7)* |
| Waist Circumference Category (%) | ||||||
| Low | 53.8 | 35.8 | 57.3 | 35.6 | 46.7 | 36.3 |
| High | 46.2 | 64.2 | 35.6 | 64.4 | 53.2 | 63.7 |
| WHtR (cm/cm) | 0.55 (0.10) | 0.60 (0.11)* | 0.55 (0.10) | 0.61 (0.12)* | 0.56 (0.10) | 0.59 (0.10) |
| WHR (cm/cm) | 0.85 (0.10) | 0.92 (0.11)* | 0.86 (0.10) | 0.93 (0.12)* | 0.85 (0.11) | 0.91 (0.09)* |
| Smoking Status (%) | ||||||
| Never | 66.8 | 44.5 | 64.2 | 42.1 | 72.2 | 49.7 |
| Former | 17.1 | 29.5 | 19.4 | 33.3 | 12.5 | 21.3 |
| Current | 7.6 | 13.7 | 7.3 | 11.5 | 8.3 | 18.4 |
| Unknown | 8.5 | 12.3 | 9.2 | 13.1 | 7.1 | 10.6 |
BMI: body mass index; BAI: body adiposity index; WHtR: waist circumference to height ratio; WHR: waist to hip circumference ratio.
p<0.05 between decedents and survivors. Results for continuous variables are presented as mean (SD). High waist circumference defined as >88 cm in women and >102 cm in men. Underweight, normal weight, overweight and obese class I and obese class II defined as BMI <18.5 kg/m2, 18.5 - 24.9 kg/m2, 25 - 29.9 kg/m2, 30 - 34.9 kg/m2 and > 35 kg/m2, respectively.
Table 2.
Correlations among adiposity variables at baseline among participants in the Pennington Center Longitudinal Study.
| BMI | Waist Circumference |
BAI | WHtR | WHR | |
|---|---|---|---|---|---|
| BMI | 0.86 | 0.79 | 0.91 | 0.41 | |
| Waist Circumference | 0.86 | 0.52 | 0.95 | 0.75 | |
| BAI | 0.83 | 0.60 | 0.71 | −0.05 | |
| WHtR | 0.92 | 0.95 | 0.76 | 0.65 | |
| WHR | 0.27 | 0.55 | −0.10 | 0.48 |
Correlations above the diagonal are among whites, and correlations below the diagonal are among African Americans.
BMI: body mass index; BAI: body adiposity index; WHtR: waist circumference to height ratio; WHR: waist to hip circumference ratio.
All correlations are significant at p<0.05.
A total of 438 deaths (131 due to cardiovascular disease, 141 due to cancer, 166 other) occurred over 120,637 person-years of follow-up. The causes of death were similar in white (27.3% due to cardiovascular disease, 34.0% due to cancer, 38.7% other) and African Americans (35.5% due to cardiovascular disease, 28.4% due to cancer, 36.2% other). Each anthropometric index showed a significant association with all-cause mortality rates in the combined sample of white and African Americans; however, there were significant interactions between race and the anthropometric variable in every case except for waist circumference (p = 0.19). After stratification by race, the relationships were universally significant in whites but not in African Americans, with the exception of waist circumference in Model 3 (Table 3).
Table 3.
Hazard ratios (95% confidence intervals) for all-cause mortality associated with anthropometric measurements and indices in white and African American participants in the Pennington Center Longitudinal Study.
| BMI | Waist Circumference | BAI | WHtR | WHR | |
|---|---|---|---|---|---|
| White Americans | |||||
| N | 9582 | 7745 | 6847 | 7745 | 6844 |
| Person-years | 82,875 | 73,756 | 70,359 | 73,756 | 70,337 |
| Deaths | 297 | 264 | 260 | 264 | 259 |
| Model 1 | 1.36 (1.22 - 1.52) | 1.44 (1.27 - 1.63) | 1.36 (1.19 - 1.55) | 1.48 (1.31 - 1.67) | 1.43 (1.26 - 1.64) |
| Model 2 | 1.34 (1.19 - 1.50) | 1.41 (1.25 - 1.60) | 1.34 (1.17 - 1.53) | 1.46 (1.28 - 1.65) | 1.40 (1.23 - 1.61) |
| Model 3 | 1.31 (1.16 - 1.47) | 1.40 (1.24 - 1.59) | 1.34 (1.17 - 1.54) | 1.46 (1.29 - 1.66) | 1.44 (1.25 - 1.64) |
| Model 4 | 1.30 (1.15 - 1.47) | 1.38 (1.21 - 1.58) | 1.33 (1.15 - 1.52) | 1.44 (1.27 - 1.64) | 1.41 (1.23 - 1.62) |
| African Americans | |||||
| N | 4761 | 3861 | 3256 | 3861 | 3256 |
| Person-years | 37,762 | 33,565 | 31,486 | 33,565 | 31,486 |
| Deaths | 141 | 124 | 119 | 124 | 119 |
| Model 1 | 1.01 (0.84 - 1.22) | 1.19 (0.98 - 1.45) | 0.93 (0.74 - 1.16) | 1.13 (0.93 - 1.38) | 1.07 (0.99 - 1.15) |
| Model 2 | 1.01 (0.83 - 1.22) | 1.18 (0.97 - 1.45) | 0.93 (0.74 - 1.16) | 1.12 (0.92 - 1.37) | 1.06 (0.98 - 1.16) |
| Model 3 | 1.03 (0.85 - 1.26) | 1.23 (1.01 - 1.50) | 0.96 (0.76 - 1.22) | 1.16 (0.95 - 1.42) | 1.06 (0.98 - 1.15) |
| Model 4 | 1.03 (0.85 - 1.26) | 1.23 (1.00 - 1.51) | 0.97 (0.77 - 1.23) | 1.16 (0.94 - 1.43) | 1.06 (0.98 - 1.16) |
Model 1: total sample, including age, sex, and exam year as covariates.
Model 2: total sample, including age, sex, exam year, study code, smoking, alcohol consumption and exercise as covariates.
Model 3: participants without heart disease, stroke or cancer at baseline; including age, sex, and exam year as covariates.
Model 4: participants without heart disease, stroke or cancer at baseline; including age, sex, exam year, study code, smoking, alcohol consumption and exercise as covariates.
BMI: body mass index; BAI: body adiposity index; WHtR: waist circumference to height ratio; WHR: waist to hip circumference ratio. Hazard ratios are expressed per standard deviation of each independent variable.
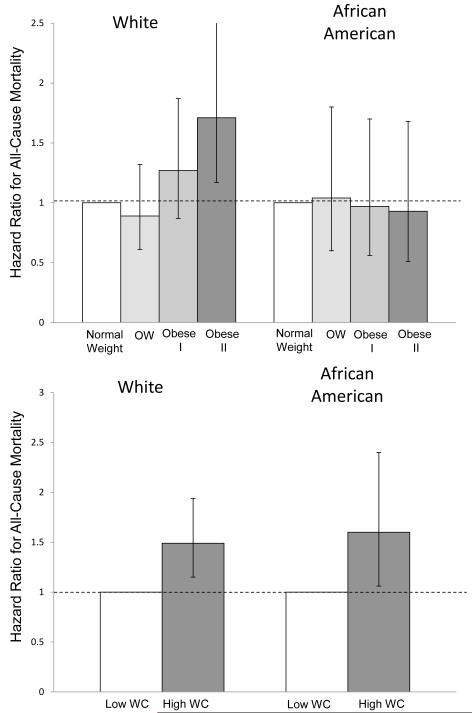
Figure 1 presents hazard ratios across normal weight, overweight and obese I and Obese II categories as well as high and low waist circumference. Among whites, the HRs for mortality were 0.89 [95% CI: 0.61 – 1.32], 1.27 [0.87 – 1.87] and 1.71 [1.17 – 2.51] for overweight, obese class I and obese class II, respectively, compared to normal weight (p for trend <0.0001). Among African Americans, the HRs for mortality were 1.04 [0.60 – 1.80], 0.97 [0.56 – 1.70] and 0.93 [0.51 - 1.68] for overweight, obese class I and obese class II, respectively, compared to normal weight (p for trend = 0.70). The elevated relative risk of mortality associated with waist circumference was almost identical in whites (1.49; 1.15 – 1.94) and African Americans (1.60; 1.06 – 2.40).
Figure 1.
Hazard ratios for all-cause mortality in A) normal weight, overweight, obese class I and obese class II, and B) low and high waist circumference (WC) groups in the Pennington Center Longitudinal Study. Error bars represent 95% confidence intervals. High waist circumference defined as > 88 cm in women and > 102 cm in men. Both models included age, sex, exam year, study code, smoking, alcohol intake and physical activity as covariates.
Discussion
The results of this study indicate that common anthropometric indicators of obesity are more strongly related to all-cause mortality in white Americans than in African Americans. The strength of the associations across the different anthropometric variables in white adults was similar, and the addition of covariates to the models did not markedly attenuate the hazard ratios. Obese white adults had a significantly higher risk of mortality compared to normal weight, but the risk of mortality across BMI-defined categories was not significant in African Americans. African Americans with an elevated waist circumference had a higher risk of mortality compared to those with a low waist circumference.
Several cohort studies have reported significant associations between BMI and mortality among white adults (7, 9, 24). For example, Berrington de Gonzalez and showed a J-shaped relationship between BMI and all-cause mortality, with risks increasing with higher BMI beyond the normal weight range, especially among nonsmokers without a history of disease (24). The results of the present study indicate that the association between BMI and mortality is essentially non-existent in the African American sample, a finding which has been reported in previous studies. For example, follow-up of over a million participants in the Cancer Prevention Study II revealed no increase in mortality associated with BMI in African American women, and a somewhat lower (and non-significant) association with excess weight in African American men, compared with white men (9). Further, there was no association between BMI and mortality in African American men and women In the National Health and Nutrition Examination Survey III Mortality Follow-up Study (10). Recent data from the REGARDS study demonstrated a U-shaped association between BMI and mortality in White participants, but no increased risk of mortality associated with BMI in African American participants (11).
Several additional studies have reported weak or non-existent relationships between BMI and mortality in African Americans. Data for African Americans from Kaiser Permanente revealed a J-shaped relationship between BMI and mortality in men but essentially a flat relationship in women (4). Stevens and colleagues reported that BMI was related to all-cause mortality in African American men and white men, but not in white men or African American women from the Charleston Heart Study (5, 12). Recent data from the Black Women’s Health Study demonstrated a significant, curvilinear relationship between BMI and mortality in African American women (8); however, an earlier study had shown that the association was modified by education: there was a significant association in women with at least a high school education, but not in women without a high school education (13). Taken together, the results of the current study and those of previous studies suggest that the relationship between BMI and mortality is not very robust in African Americans. Further studies are needed using large representative population samples, which are able to explore confounding and effect modification across a wide range of covariates which may help explain the lack of association between BMI and mortality in African Americans.
Waist circumference, WHR, and WHtR were all significantly related to all-cause mortality in a 16-year follow-up of women in the Nurses’ Health Study (18). Similarly, waist circumference and WHR were both positively associated with mortality in the Health Professionals Follow-up Study (19). Waist circumference was also significantly related to all-cause mortality in men and women from the Cancer Prevention Study II Nutrition Cohort (16). Data from the Iowa Women’s Health Study also showed positive associations between waist circumference and all-cause mortality (20). Further, waist circumference demonstrated a significant, linear association with all-cause mortality in the Black Women’s Health Study, but race differences could not be explored since the sample was 100% African American (8). Although none of these studies examined racial differences, the evidence suggests that waist circumference is generally related to mortality among US adults.
Analyses of data from the Charleston Heart Study demonstrated that waist circumference (age-adjusted) was related to all-cause mortality in white women, but not in white men or African Americans (5, 12). Waist circumference was related to all-cause mortality in white but not African Americans in the NIH-AARP study (17). The multivariable-adjusted hazard ratios for all-cause mortality for high versus low waist circumference (88 cm for women, 102 cm in men) were 1.18 (1.15 - 1.22) and 1.20 (1.14 - 1.26) in white men and women, and 1.10 (0.88 – 1.38) and 1.07 (0.83 – 1.38) in African American men and women, respectively (17). In a 12-year follow-up of participants in NHANES III, waist circumference was not related to mortality in white or African Americans, but there was a significant dose-response relationship between WHR and all-cause mortality in white and African American women (but not in men) (10). Results from the REGARDS study demonstrated a significant association between waist circumference and mortality in whites and in African American women (although not as strong), but not in African American men (11). Although there was no linear association between waist circumference or its indices in African Americans in the present study, the magnitude of the association between waist circumference category and mortality was essentially the same as that found in white adults (Figure 1).
The BAI has recently been proposed as an alternative to BMI as an index of obesity (21). The results of this study indicate that BAI has a similar relationship with mortality as BMI and other anthropometric indices (Table 3). This is not surprising, given that BAI and BMI have similar associations with body fat and CVD risk factors (14, 25).
It is unclear what the mechanisms are that could explain the race differences in the relative risks of mortality reported in this study. Despite the lack of association between most anthropometric markers and mortality among African Americans, the absolute death rates (adjusted for age, sex and exam year) were markedly higher in African Americans (54.0/10,000 person years) compared to whites (35.8/10,000 person-years). Visceral adipose tissue has been identified as a potentially dangerous fat depot (26, 27). Previous work in this cohort has demonstrated that VAT is significantly higher in whites than in African Americans, even after controlling for total adiposity (28). This represents a paradox that is difficult to explain. It has also been shown that for a given level of WC or BMI, white men and women have higher levels of VAT than African American men and women; however, these race differences increase at higher levels of waist circumference and BMI (29). To date, the degree to which race differences in social and behavioral characteristics can explain the observed differences in obesity-related mortality risk is not well understood. More research is necessary to clarify the underlying mechanisms behind the observed absolute and relative race differences in mortality risk at different levels of obesity.
The strengths and limitations of this study warrant discussion. Marked strengths of this study include the direct assessment of anthropometric measurements using a standard clinical protocol, and the linkage to the National Death Index for the ascertainment of vital status. Although cause of death was known, the sample sizes were not sufficient to allow for cause-specific analyses. Further, the sample size was not sufficient to allow for sex-specific or age-specific analyses within the two racial groups. Major causes of death change with age, and it is likely that the effects of obesity on mortality vary across different age groups. Although we adjusted for known confounding variables in the association with mortality such as age, sex, smoking, alcohol consumption and physical activity, we cannot rule out the possibility that confounding factors that were not measured at baseline may have introduced bias into the results. Although we did not stratify by smoking status in the main analysis, in a sensitivity analysis that excluded current smokers, the results and significance levels did not change appreciably. The sample included white and African men and women who were volunteers for research studies, and therefore may not be representative of the general population.
In conclusion, this study has demonstrated race differences in the association between common anthropometric markers of obesity and all-cause mortality. The associations were more significant in white adults than in African American adults.
Acknowledgements
The Pennington Center Longitudinal Study is registered at ClinicalTrials.gov (Identifier NCT00959270). This research was supported by the Pennington Biomedical Research Center. PK is supported, in part, by the Louisiana Public Facilities Authority Endowed Chair in Nutrition and SH is funded, in part, by the George A. Bray, Jr. Chair in Nutrition. CB is funded, in part, by the John W. Barton, Sr. Endowed Chair in Genetics and Nutrition. This work was also partially supported by an NORC Center grant #2P30-DK072476-06 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by NIDDK. Special thanks to Connie Murla and Aimee Stewart for data management, as well as the many clinical scientists and staff of the Pennington Biomedical Research Center who have contributed data to the development of the Pennington Center Longitudinal Study.
References
- 1.Murphy SL, Xu J, Kochanek KD. National Vital Statistics Reports. 4. Vol. 60. National Center for Health Statistics; Hyattsville, MD: 2012. Deaths: preliminary data for 2010; pp. 1–68. [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Cowie CC, Rust KF, Byrd1Holt DD, Gregg EW, Ford ES, Geiss LS, Bainbridge KE, Fradkin JE. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care. 2010;33(3):562–8. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wienpahl J, Ragland DR, Sidney S. Body mass index and 15-year mortality in a cohort of black men and women. J Clin Epidemiol. 1990;43:949–60. doi: 10.1016/0895-4356(90)90078-4. [DOI] [PubMed] [Google Scholar]
- 5.Stevens J, Keil JE, Rust PF, Verdugo RR, Davis CE, Tyroler HA, Gazes PC. Body mass index and body girths as predictors of mortality in black and white men. Am J Epidemiol. 1992;135(10):1137–46. doi: 10.1093/oxfordjournals.aje.a116214. [DOI] [PubMed] [Google Scholar]
- 6.Durazo1Arvizu R, Cooper RS, Luke A, Prewitt TE, Liao Y, McGee DL. Relative weight and mortality in U.S. blacks and whites: findings from representative national population samples. Ann Epidemiol. 1997;7(6):383–95. doi: 10.1016/s1047-2797(97)00044-6. [DOI] [PubMed] [Google Scholar]
- 7.Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbeck A, Leitzmann MF. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–78. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 8.Boggs DA, Rosenberg L, Cozier YC, Wise LA, Coogan PF, Ruiz-Narvaez EA, Palmer JR. General and abdominal obesity and risk of death among black women. The New England journal of medicine. 2011;365(10):901–8. doi: 10.1056/NEJMoa1104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 10.Reis JP, Araneta MR, Wingard DL, Macera CA, Lindsay SP, Marshall SJ. Overall obesity and abdominal adiposity as predictors of mortality in U.S. white and black adults. Ann Epidemiol. 2009;19(2):134–42. doi: 10.1016/j.annepidem.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 11.Lakoski SG, Le AH, Muntner P, Judd SE, Safford MM, Levine DA, Howard G, Cushman M. Adiposity, inflammation, and risk for death in black and white men and women in the United States: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. The Journal of clinical endocrinology and metabolism. 2011;96(6):1805–14. doi: 10.1210/jc.2010-3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens J, Keil JE, Rust PF, Tyroler HA, Davis CE, Gazes PC. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med. 1992;152(6):1257–62. [PubMed] [Google Scholar]
- 13.Stevens J, Plankey MW, Williamson DF, Thun MJ, Rust PF, Palesch Y, O’Neil PM. The body mass index-mortality relationship in white and African American women. Obes Res. 1998;6(4):268–77. doi: 10.1002/j.1550-8528.1998.tb00349.x. [DOI] [PubMed] [Google Scholar]
- 14.Barreira TV, Staiano AE, Harrington DM, Heymsfield SB, Smith SR, Bouchard C, Katzmarzyk PT. Anthropometric correlates of total body fat, abdominal adiposity, and cardiovascular disease risk factors in a biracial sample of men and women. Mayo Clin Proc. 2012;87(5):452–60. doi: 10.1016/j.mayocp.2011.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouchard C. BMI, fat mass, abdominal adiposity and visceral fat: where is the ‘beef’? Int J Obes Relat Metab Disord. 2007;31:1552–3. doi: 10.1038/sj.ijo.0803653. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs EJ, Newton CC, Wang Y, Patel AV, McCullough ML, Campbell PT, Thun MJ, Gapstur SM. Waist circumference and all-cause mortality in a large US cohort. Archives of internal medicine. 2010;170(15):1293–301. doi: 10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- 17.Koster A, Leitzmann MF, Schatzkin A, Mouw T, Adams KF, van Eijk JT, Hollenbeck AR, Harris TB. Waist circumference and mortality. American journal of epidemiology. 2008;167(12):1465–75. doi: 10.1093/aje/kwn079. [DOI] [PubMed] [Google Scholar]
- 18.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117(13):1658–67. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 19.Baik I, Ascherio A, Rimm EB, Giovannucci E, Spiegelman D, Stampfer MJ, Willett WC. Adiposity and mortality in men. Am J Epidemiol. 2000;152(3):264–71. doi: 10.1093/aje/152.3.264. [DOI] [PubMed] [Google Scholar]
- 20.Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong C-P, Sellers TA, Lazovich D, Prineas RJ. Associations of general and abdominal obesity with multiple health outcomes in older women: The Iowa Womenȉs Health Study. Arch Intern Med. 2000;160:2117–28. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 21.Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, Xiang AH, Watanabe RM. A better index of body adiposity. Obesity. 2011;19:1083–9. doi: 10.1038/oby.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NIH . The Practical Guide to the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. US NIH; Bethesda, MD: 2000. [Google Scholar]
- 23.MacMahon B. The National Death Index. Am J Public Health. 1983;73:1247–8. doi: 10.2105/ajph.73.11.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, Moore SC, Tobias GS, Anton-Culver H, Freeman LB, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–9. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barreira TV, Harrington DM, Staiano AE, Heymsfield SB, Katzmarzyk PT. Body adiposity index, body mass index, and body fat in white and black adults. JAMA. 2011;306(8):828–30. doi: 10.1001/jama.2011.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, Lopez-Jimenez F, Rao G, St-Onge MP, Towfighi A, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019. doi: 10.1161/CIR.0b013e318233bc6a. [DOI] [PubMed] [Google Scholar]
- 27.Despres JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodes-Cabau J, Bertrand OF, Poirier P. Abdominal obesity and the metabolic syndrome: Contribution to global and cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 28.Katzmarzyk PT, Bray GA, Greenway FL, Johnson WD, Newton RL, Jr., Ravussin E, Ryan DH, Smith SR, Bouchard C. Racial differences in abdominal depot-specific adiposity in white and African American adults. Am J Clin Nutr. 2010;91:71–5. doi: 10.3945/ajcn.2009.28136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, Ravussin E, Ryan DH, Smith SR, Katzmarzyk PT. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: Sex and race differences. Obesity. 2011;19:402–8. doi: 10.1038/oby.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]