Abstract
Purpose
A growing body of work examines the association between neighborhood environment and intimate partner violence (IPV). As in the larger literature examining the influence of place context on health, rural settings are understudied and urban and rural residential environments are rarely compared. In addition, despite increased attention to the linkages between neighborhood environment and IPV, few studies have examined the influence of neighborhood context on intimate partner femicide (IPF). In this paper, we examine the role for neighborhood-level factors in differentiating urban and rural IPFs in Wisconsin, USA.
Methods
We use a combination of Wisconsin Violent Death Reporting System (WVDRS) data and Wisconsin Coalition Against Domestic Violence (WCADV) reports from 2004–2008, in concert with neighborhood-level information from the US Census Bureau and US Department of Agriculture, to compare urban and rural IPFs.
Findings
Rates of IPF vary based on degree of rurality, and bivariate analyses show differences between urban and rural victims in race/ethnicity, marital status, country of birth, and neighborhood characteristics. After controlling for individual characteristics, the nature of the residential neighborhood environment significantly differentiates urban and rural IPFs.
Conclusions
Our findings suggest a different role for neighborhood context in affecting intimate violence risk in rural settings, and that different measures may be needed to capture the qualities of rural environments that affect intimate violence risk. Our findings reinforce the argument that multilevel strategies are required to understand and reduce the burden of intimate violence, and that interventions may need to be crafted for specific geographical contexts.
Keywords: rural, epidemiology, geography, social determinants of health, intimate partner violence
Intimate partner violence (IPV) against women is a significant global public health problem,1–4 affecting women across the lifespan and increasing risk for a number of adverse health outcomes, including chronic pain,5 depression,6 and adverse birth outcomes.7 IPV has been defined as “threatened, attempted or completed physical or sexual violence, as well as the infliction of emotional abuse in the context of physical or sexual violence, and includes violence by a spouse, ex-spouse, current or former boyfriend or girlfriend, dating partner, or date.”8 Risk factors for IPV include younger age,9 shorter relationship duration,10 marital status as unmarried or cohabiting,10, 11 alcohol use,12 and lower socioeconomic status.10 Violence rates vary among racial and ethnic groups,11,13 and by geography.14–16 In North America, where this study is based, the mean lifetime prevalence of domestic violence (DV) against women is estimated at 33% physical, 18% sexual and 30% emotional violence.16
An extreme form of IPV is intimate partner femicide (IPF)—the murder of a woman by her intimate partner. In the US, an estimated 30%–50% of murdered women are killed by a current or former intimate partner.17,18 Risk factors for IPF include race, socioeconomic status, and foreign country of birth,19,20 and IPF is often preceded by a history of IPV.19 Risk factors for IPF include abuser unemployment, abuser access to a firearm, having lived with the abuser, having a child by a previous partner in the home with the abuser, previous threats by the abuser, and the combination of the abuser's controlling behavior and the woman's leaving or attempting to leave the relationship.19
Most IPV research has focused on individual risk factors. Recently, more attention has been paid to geographical setting. In 1995, O'Campo et al found a significant neighborhood effect for neighborhood unemployment and per capita income on risk of violence during pregnancy for women in an urban area, while controlling for individual-level variables.9 Miles-Doan followed with 2 spatial analyses of police records in Duval County, Florida (including Jacksonville), finding associations between neighborhood deprivation and IPV rates.21,22 Other researchers have continued this line of inquiry, expanding the range of variables considered, exploring additional study areas, deepening the complexity of analysis, and expanding the range of study findings, although studies have focused on urban populations and nationally representative survey samples.10,12,17,23,24
Most studies have drawn primarily from social disorganization theory to frame research questions. This theory describes how socioeconomic disadvantage and residential instability disrupt social bonds and limit collective ability to maintain social control, increasing the likelihood of deviant behaviors such as violence.25–27 Results of studying the relationship between neighborhood disadvantage and individual risk of IPV have been mixed. Several researchers report significant associations,9,17,28 others report non-significant effects,12 and still others report differential effects based on race/ethnicity,13 or confounding effects between race and neighborhood-level disadvantage.10,17 Residential stability, traditionally hypothesized to have a stabilizing effect in neighborhoods that could reduce violent crime rates, has been found instead to be associated with increased IPV risk,12,28 or to have no association,23 leading researchers to question the meaning of residential instability in an age when it may be associated with higher levels of education and mobility. Some have suggested that residential stability could actually prolong and deepen one's experience of disadvantage.12
Recent work explores the relationship between neighborhood conditions and IPV in non-Western and developing country settings, with more focus on social norms and values. Two studies analyzed the Indian National Family Health Survey, finding a significant effect for a state-level measure of gender equality29 and a gradient effect related to community-level literacy rates.29 A third study found significant effects for community wife beating norms and community violence.30 One study found an association between measures of violence in a woman's immediate geographic environment and risk of individual sexual and physical victimization in Colombia.31 Another found that sociocultural context affects the influence of community characteristics on risk, finding significant associations between women's lack of autonomy and risk of violence only in the less culturally conservative of 2 study regions.32 One study also examined the relationship among neighborhood and state-level socioeconomic status with attitudes toward IPV against women in several African countries.33
Despite the growing body of work examining geographical setting and IPV, rural settings are understudied. Madkour et al noted that the question of “how concentrated disadvantage is related to intimate partner homicide in nonurban counties has not yet been explored.”34 There is reason to believe that characteristics of the residential environment are linked to IPV in rural settings, and that the nature of urban and rural geographical settings may affect risk in different ways. The literature reveals a number of place-related contextual factors that have been linked to a woman's IPV risk, or ability to leave an abusive situation, in rural settings.
Factors identified to be important in rural areas include: geographic isolation (eg, distance from neighbors, police, medical facilities), cultural factors (eg, patriarchal values, religious values emphasizing the marital bond), lack of anonymity/privacy/confidentiality (eg, police, doctors, judges have personal relationships with victim or perpetrator, locations of shelters and safe houses are common knowledge), social isolation (eg, few friends and acquaintances, especially outside of the immediate community), resource/service access (eg, low population density is associated with low resource density), legal system constraints (eg, lack of legal aid, limited enforcement of restraining orders), economic dependence (eg, farm women's income is tied to their place of residence), and firearms (eg, more available or accepted, or subject to fewer controls).15,35–44
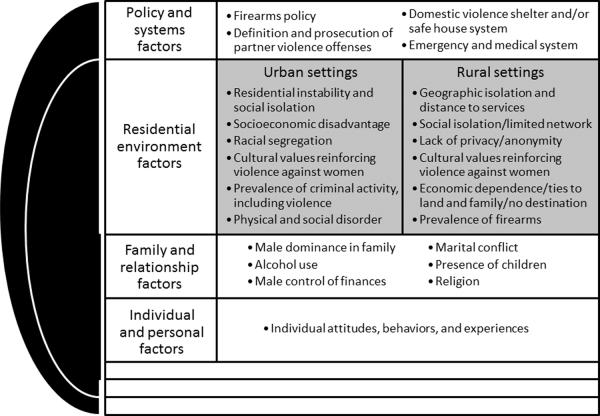
Many have hypothesized that IPV differs in urban and rural settings, but few have documented the differences empirically. We seek to understand how IPF victims and circumstances surrounding their deaths differ in urban versus rural settings, with a specific interest in the residential environmental characteristics experienced by IPF victims. Our work is guided by the conceptual model shown in Figure 1, and it is informed by the social-ecological model of disease proposed by Heise2 relating both social and geographical characteristics to violence against women. Our model specifies possible differences in residential environmental factors that may be associated with IPV in urban versus rural areas. In this paper, we (1) describe characteristics of IPFs in Wisconsin using a unique combination of 2 datasets to avoid misclassification bias, and (2) determine whether and how levels of neighborhood disadvantage and instability—constructs often studied when relating neighborhood setting to IPV—differ among urban and rural intimate partner femicides.
Figure 1.
Conceptual Model Relating Individual, Social and Ecological Factors to Intimate Partner Violence in Urban and Rural Areas
METHODS
Data Sources
We analyzed data from the Wisconsin Violent Death Reporting System (WVDRS) for 2004–2008. WVDRS is part of the National Violent Death Reporting System (NVDRS), which is a population-based active surveillance system that links multiple data sources to provide a census of violent deaths that occur within the borders of participating US states.45 No sampling is employed; all violent deaths are included. Violent deaths are defined, based on the World Health Organization's definition, as deaths resulting from “the intentional use of physical force or power against oneself, another person, or against a group or community.”45 An abstractor at the Wisconsin Department of Health Services generates WVDRS records based on the “manner of death” listed on Wisconsin death certificates.
WVDRS has 2 key limitations. First, IPFs are difficult to identify. Although WVDRS contains codes indicating whether or not a death was “IPV” or “jealousy” related, it does not specify whether the perpetrator was the woman's intimate partner. Other data sources, including the Supplemental Homicide Reports (SHR), have also been subject to misclassification bias on this subject.18 Secondly, WVDRS records reflect knowledge of the violent death fairly soon after it has occurred and are based on official records, and thus do not include extensive information on the perpetrator or circumstances of the deaths. To accurately identify IPFs within WVDRS and to gain a more complete picture of the circumstances, we consulted an additional data source.
The Wisconsin Coalition Against Domestic Violence (WCADV) publishes an annual report on domestic violence homicides, drawing from publicly available information, such as news reports and court records, to provide details of each homicide, with the goal “to construct as accurate a description as possible of key events and circumstances related to each homicide.”46 Reports contain narratives for each death. We used these reports, in addition to files maintained by WCADV for each woman, to validate each death as an IPF and document other circumstances of the homicide not contained in WVDRS, including the woman's relationship with the perpetrator and prior IPV history.
We began with a dataset including all homicides of females age 16 or older within Wisconsin from 2004–2008 (n=216). We then compared WVDRS records with WCADV reports and files and determined 87 deaths to be intimate partner femicides. Because we are interested in the role that neighborhood plays in differentiating urban and rural IPFs, we limited our dataset only to Wisconsin residents for whom the geographic location of the residence could be determined. Our final dataset included 84 IPFs. Additionally, we analyzed US Census 2000 data by census tract to examine urban-rural differences in population demographics to provide a comparison point for our findings.
Urban Versus Rural Designation
Neighborhood was defined as the US Census Tract. We geocoded residential addresses for all femicide victims and linked these point locations to the tract within which they fell. An initial automated run geocoded most of the records; a small number were matched manually, addressing spelling errors, and examining possible alternative city or postal (ZIP) code assignments. In matching records, uncertainty in precise location was considered acceptable if it did not change the neighborhood to which the record would be assigned. We were able to assign all 84 IPFs to neighborhoods.
Census Tract Rural-Urban Commuting Area (RUCA) codes were used to determine victim residence in a rural versus urban area.47,48 RUCA codes use “the standard Bureau of Census Urbanized Area and Urban Cluster definitions in combination with work commuting information to characterize all of the nation's Census tracts regarding their rural and urban status and relationships.”47 Due to the limited sample size, we define “urban” as the “metro” category (n=60, RUCA codes 1–3) and “rural” as the combination of the “micro,” “small town” and “rural” designations (n=24, RUCA codes 4–10). Figure 2 includes 2 maps of our study area with RUCA categories and our definitions of urban and rural areas represented.
Figure 2.
Rural-Urban Commuting Areas in Wisconsin by US Census Tract, 2000
Measures
At the victim level, we explored the victim's age, race/ethnicity (White, Black, other), marital status (never married, married, divorced/widowed), education level (less than high school, high school degree, some college or higher), country of birth (USA or foreign born), and whether she was known to be pregnant at the time of or within a year prior to death.
At the level of the perpetrator and relationship, we examined perpetrator age, relationship (husband, boyfriend, ex-husband/boyfriend), condition of relationship (intact or in some stage of dissolution), the presence of young children in the household or family, and indications of an IPV history, such as restraining orders or reports of the woman leaving the relationship due to violence. If no mention was made of trouble in the relationship, it was considered to be “intact.” In categorizing relationship with the perpetrator, a fiancé was categorized as a boyfriend and a longtime partner was categorized as a husband.
Homicide characteristics studied include weapon type causing the fatal injury (firearm, sharp/knife, other), number of penetrating wounds (wounds made by a gun or knife), victim alcohol use prior to the homicide, whether the homicide occurred in the home, and the status of perpetrator after homicide (alive, committed suicide, other; eg, contemplated or attempted suicide or died from a non-suicide event).
At the neighborhood level, we explored 2 measures—an index of concentrated disadvantage, and a measure of residential instability. We developed a Concentrated Disadvantage Index, as employed previously.12 Following previous researchers,12 and to focus on constructs embedded within Social Disorganization Theory, we determined that our Index would include the following variables from the 2000 US Census: proportion of the population on public assistance, proportion below the poverty line, proportion single-parent households, and proportion unemployed. We then used a Principal Components Analysis to identify variable loadings within the first component; these loadings were used as weights, multiplied by the z-score of each census tract's variable value, to form our Index. We also measured residential instability as the proportion of individuals living in a different house than they had 5 years before, based on US Census 2000 estimates.
Statistical Analysis
We undertook descriptive analyses of all IPFs (n=84). We calculated rates of IPF by degree of rurality and then compared the characteristics of urban and rural IPF victims and circumstances surrounding the deaths using Fisher's exact test, given our small sample size. We also made a direct comparison of marital status and relationship with the perpetrator to determine whether the 2 variables measured the same intimate partner relationship. Because clear differences emerged (see Table 1), we fit 2 sets of models based on each of these 2 constructs. Multivariable logistic regression analyses were performed to determine whether neighborhood-level characteristics were associated with rural residence, controlling for individual-level characteristics. We considered age, race, marital status, relationship with perpetrator, and level of education at the individual level, and concentrated disadvantage and residential Instability at the neighborhood level. We first constructed an individual-level model, and then we proceeded to consider neighborhood context. Collinearity between disadvantage and instability revealed a correlation of r =.49. Separate analyses of neighborhood disadvantage and instability showed similar effect directions and sizes as models considering them simultaneously. Tertiles for concentrated disadvantage and residential instability were defined separately for rural and urban women. The Hosmer-Lemeshow goodness of fit test49 indicated a satisfactory model fit. A statistical significance (alpha) level of .05 was specified. STATA/IC 11 (STATCorp, College Station, Texas) was used to perform all statistical analyses and a combination of Esri ArcMap 10 (Esri, Redlands, California) and Google Maps™ (Google Inc., Mountain View, California) mapping service were used for geocoding and neighborhood assignment. This analysis underwent human subjects review.
Table 1.
Comparison of Marital Status and Relationship to Perpetrator Among Intimate Partner Femicides in Wisconsin, 2004–2008
| Relationship to Perpetrator (n, row %, column %) | |||
|---|---|---|---|
| Marital Status | Boyfriend | Husband | Former husband or boyfriend |
| Never married | 19 (70.37%, 65.52%) | 1 (3.70%, 3.57%) | 7 (25.93%, 25.93%) |
| Married | 2 (5.26%, 6.90%) | 24 (63.16%, 85.71%) | 12 (31.58%, 44.44%) |
| Divorced/widowed | 8 (42.11%, 27.59%) | 3 (15.79%, 10.71%) | 8 (42.11%, 29.63%) |
US Census Data Analysis
To compare our findings to general patterns of demographic differences among Wisconsin's urban and rural areas, we conducted an analysis of US Census data by census tract. We calculated odds ratios to illustrate the relationships between demographics of interest and rurality, using the same RUCA definitions employed in our analysis of WVDRS data to define urban and rural areas. Odds ratios relating age groups included women ages 16 and older, while analyses of race, marital status, educational attainment, disadvantage, and instability included women ages 18 and older, due to the data categories available from the US Census Bureau. To examine disadvantage and instability, tertiles were defined for all census tracts combined, whereas tertiles for these variables as entered into our models were defined for urban and rural women separately.
RESULTS
Descriptive and Bivariate Analyses
Table 2 shows rates of IPF by degree of rurality. The highest rate was observed in the small town category, followed by the metropolitan, rural, and micropolitan categories. Table 3 shows characteristics of the IPF deaths and Table 4 shows results of bivariate analyses comparing urban and rural deaths. The median age of victims was 37, with a wide range from age 16 to 75. Similarly, the median age of perpetrators was 40, with a range from 18–79. Age was not significantly different between urban and rural women.
Table 2.
Intimate Partner Femicide Rates by Degree of Rurality in Wisconsin, 2004–2008
| RUCA category | IPFs | Woman-years | rates per 1 million woman-years |
|---|---|---|---|
| RUCA “metro” | 60 | 7,295,495 | 8.22 |
| RUCA “micro” | 6 | 1,190,310 | 5.04 |
| RUCA “smalltown” | 10 | 1,019,385 | 9.81 |
| RUCA “rural” | 8 | 1,124,790 | 7.11 |
| RUCA micro-smalltown-rural combined | 24 | 3,334,485 | 7.20 |
| Total | 84 | 10,629,980 | 7.90 |
rates are calculated using Census 2000 estimates for women ages 16 or older by US Census Tract. Shaded rows indicate categories used in our comparison of urban and rural IPFs.
Table 3.
Characteristics of IPF Deaths in Wisconsin, USA, 2004–2008 (n=84)
| Victim Characteristics | N (%) or median [range] |
|---|---|
|
| |
| Age (WVDRS,WCADV) | 37 [16,75] |
|
| |
| Race (WVDRS) | |
| White | 49 (58.33) |
| Black | 16 (19.05) |
| Hispanic | 6 (7.14) |
| Asian | 6 (7.14) |
| Other or Unspecified | 7 (8.33) |
|
| |
| Marital status (WVDRS) | |
| Never married | 27 (32.14) |
| Married | 38 (45.24) |
| Divorced | 15 (17.86) |
| Widowed | 4 (4.76) |
|
| |
| Level of education (WVDRS) | |
| 8th grade | 5 (5.95) |
| Some high school | 10 (11.90) |
| High school degree (or GED) | 34 (40.48) |
| Some college | 7 (8.33) |
| Associate's degree | 12 (14.29) |
| Bachelor's degree | 13 (15.48) |
| Master's degree | 2 (2.38) |
| Unknown | 1(1.19) |
|
| |
| Country of birth (WVDRS) | |
| USA | 73 (86.90) |
| Foreign | 7 (8.33) |
| Unknown | 4 (4.76) |
|
| |
| Pregnant within year of death (WVDRS) | |
| No | 61 (72.62) |
| Yes | 5 (5.95) |
| Within last year | 2 (2.38) |
| Unknown | 16 (19.05) |
| Perpetrator and Relationship Characteristics | N (%) or median [range] |
|---|---|
|
| |
| Perpetrator age (WCADV) | 40 [18,79] |
|
| |
| Perpetrator relationship | |
| Husband | 26 (30.95) |
| Estranged husband | 11 (13.10) |
| Ex-husband | 5 (5.95) |
| Boyfriend | 28 (33.33) |
| Estranged boyfriend | 1 (1.19) |
| Ex-boyfriend | 10 (11.90) |
| Fiancé | 1 (1.19) |
| Longtime partner | 2 (2.38) |
|
| |
| Relationship condition | |
| Intact | 35 (41.67) |
| Unstable | 9 (10.71) |
| Ending | 21 (25.00) |
| Recently finished | 4 (4.76) |
| Finished | 15 (17.86) |
|
| |
| Couple with young children (ages 0–18) | |
| Yes | 42 (50.00) |
| No | 15 (17.86) |
| Unknown | 27 (32.14) |
|
| |
| History of IPV | |
| Yes | 38 (45.24) |
| Possible | 7 (8.33) |
| Unknown | 39 (46.43) |
| Homicide Characteristics | N (%) or median [range] |
|---|---|
|
| |
| Weapon type causing fatal injury (WVDRS) | |
| Beating (personal-fists, feet) | 2 (2.38) |
| Beating (blunt object) | 8(9.52) |
| Burn | 2 (2.38) |
| Suffocation/strangulation | 7 (8.33) |
| Sharp object | 21 (25.00) |
| Firearm | 36 (42.86) |
| Poison | 3 (3.57) |
| Unknown | 5 (5.95) |
|
| |
| Number of penetrating wounds (WVDRS) | |
| No wounds | 23 (27.38) |
| One wound | 15 (17.86) |
| Multiple wounds | 28 (33.33) |
| Unknown | 18 (21.43) |
|
| |
| Suspected alcohol use by victim (WVDRS) | |
| No | 52 (61.90) |
| Yes | 17 (20.24) |
| Unknown | 15 (17.86) |
|
| |
| Homicide took place in the home (WVDRS) | |
| No | 19 (22.62) |
| Yes | 63 (75.00) |
| Unknown | 2 (2.38) |
|
| |
| Perpetrator status after homicide (WCADV) | |
| Alive | 49 (58.33) |
| Alive, but contemplated suicide | 1 (1.19) |
| Alive, but attempted suicide | 3 (3.57) |
| Alive, but attempted suicide by cop | 1 (1.19) |
| Committed suicide | 27 (32.14) |
| Deceased (legal or family intervention) | 3 (3.57) |
| Geographical Characteristics | N (%) or median [range] |
|---|---|
|
| |
| Concentrated Disadvantage Index (urban) | −0.64 [−1.66, 9.75) |
| Concentrated Disadvantage Index (rural) | −0.52 [−1.45, 7.71] |
|
| |
| Residential Instability (urban) | 0.44 [0.22, 0.96] |
| Residential Instability (rural) | 0.37 [0.24, 0.75] |
Table 4.
Characteristics of Urban Versus Rural Intimate Partner Femicides
| Geographical location | ||||
|---|---|---|---|---|
|
| ||||
| Victim Characteristics | Urban (n=60, 71%) (n, %) | Rural (n=24, 29%) (n, %) | Unadjusted Odds Ratio (95% CI) | P value |
|
| ||||
| Victim's Age (WVDRS, WCADV) | .306 | |||
| 16–24 | 13 (21.67) | 5 (20.83) | Referent | |
| 25–34 | 15 (26.67) | 4 (16.67) | 0.65 (0.11, 3.77) | |
| 35–44 | 15 (25.00) | 11 (45.83) | 1.91 (0.45, 8.83) | |
| 45+ | 16 (26.67) | 4 (16.67) | 0.65 (0.11, 3.77) | |
|
| ||||
| Victim's Race (WVDRS) | .003a | |||
| White | 29 (48.33) | 20 (83.33) | Referent | |
| Black | 16 (26.67) | 0 (0.00) | 0.00 (0.00,0.37) | .001a |
| Other | 15 (25.00) | 4 (16.67) | 0.39 (0.08, 1.48) | .163 |
|
| ||||
| Victim's Marital status (WVDRS) | .050a | |||
| Never married | 23 (38.33) | 4 (16.67) | Referent | |
| Married | 22 (36.67) | 16 (66.67) | 4.18 (1.09 19.49) | .028a |
| Divorced/Widowed | 15 (25.00) | 4 (16.67) | 1.53 (0.24, 9.54) | .700 |
|
| ||||
| Victim's Level of education (WVDRS) | .304 | |||
| Less than HS degree | 13 (22.03) | 2 (8.33) | Referent | |
| HS degree | 22 (37.29) | 12 (50.00) | 0.28 (0.03, 1.63) | |
| Some college or higher | 24 (40.68) | 10 (41.67) | 2.71 (0.46, 28.58) | |
|
| ||||
| Victim's Country of birth (WVDRS) | .029a | |||
| USA | 49 (81.67) | 24 (100.00) | Referent | |
| Foreign or unknown | 11 (18.33) | 0 (0.00) | 0 (0.00, 0.74) | .029a |
|
| ||||
| Pregnant within year of death (WVDRS) | .099 | |||
| No or Unknown | 57 (95.00) | 20 (83.33) | Referent | |
| Yes | 3 (5.00) | 4 (16.67) | 3.8 (0.58, 27.71) | |
| Perpetrator and Relationship Characteristics | Urban (n=60, 71%) (n, %) | Rural (n=24, 29%) (n, %) | Unadjusted Odds Ratio (95% CI) | P value |
|---|---|---|---|---|
|
| ||||
| Perpetrator age (WCADV) | .985 | |||
| 16–24 | 8 (13.33) | 4 (16.67) | Referent | |
| 25–34 | 12 (20.00) | 4 (16.67) | 0.67 (0.09, 4.81) | |
| 35–44 | 22 (36.67) | 9 (37.50) | 0.82 (0.16, 4.70) | |
| 45+ | 18 (30.00) | 7 (29.17) | 0.78 (0.14, 4.73) | |
|
| ||||
| Perpetrator relationship to victim (WCADV) | .055 | |||
| Boyfriend | 25 (41.67) | 4 (16.67) | Referent | |
| Husband | 16 (26.67) | 12 (50.00) | 4.69 (1.13, 22.88) | |
| Ex- or estranged | 19 (31.67) | 8 (33.33) | 2.63 (0.59, 13.55) | |
| husband or boyfriend | ||||
|
| ||||
| Relationship condition (WCADV) | 1.000 | |||
| Intact | 25 (41.67) | 10 (41.67) | Referent | |
| In trouble | 35 (58.33) | 14 (58.33) | 1.00 (0.34, 2.89) | |
|
| ||||
| Couple with young children ages 0–18 (WCADV) | .767 | |||
| Yes | 29 (48.33) | 13 (54.17) | Referent | |
| No | 12 (20.00) | 3 (12.50) | 0.56 (0.09, 2.61) | |
| Unknown | 19 (31.67) | 8 (33.33) | 0.94 (0.28, 3.02) | |
|
| ||||
| History of IPV (WCADV) | .378 | |||
| Unknown | 25 (41.67) | 14 (58.33) | Referent | |
| Possible | 5 (8.33) | 2 (8.33) | 1.40 (0.19, 16.41) | |
| Yes | 30 (50.00) | 8 (33.33) | 0.48 (0.15, 1.47) | |
| Homicide Characteristics | Urban (n=60, 71%) (n, %) | Rural (n=24, 29%) (n, %) | Unadjusted Odds Ratio (95% CI) | P value |
|---|---|---|---|---|
|
| ||||
| Weapon (WCADV) | .240 | |||
| Shot | 24 (40.00) | 13 (54.17) | Referent | |
| Stabbed | 21 (35.00) | 4 (16.67) | 0.35 (0.07, 1.40) | |
| Other | 15 (25.00) | 7 (29.17) | 0.86 (0.23, 3.00) | |
|
| ||||
| Weapon type causing fatal injury (WVDRS) | .560 | |||
| Firearm | 24 (40.00) | 12 (50.00) | Referent | |
| Sharp | 17 (28.33) | 4 (16.67) | 0.47 (0.10, 1.94) | |
| Other | 19 (31.67) | 8 (33.33) | 0.84 (0.25, 2.80) | |
|
| ||||
| Number of penetrating wounds (WVDRS) | .583 | |||
| No wounds | 16 (26.67) | 7 (29.17) | Referent | |
| One wound | 11 (18.33) | 4 (16.67) | 0.83 (0.14, 4.31) | |
| Multiple wounds | 18 (30.00) | 10 (41.67) | 1.27 (0.34, 4.93) | |
| Unknown | 15 (25.00) | 3 (12.50) | 0.46 (0.07, 2.53) | |
|
| ||||
| Suspected alcohol use by victim (WVDRS) | .695 | |||
| No | 37 (61.67) | 15 (62.50) | Referent | |
| Yes | 11 (18.33) | 6 (25.00) | 1.35 (0.34, 4.87) | |
| Unknown | 12 (20.00) | 3 (12.50) | 0.62 (0.10, 2.78) | |
|
| ||||
| Homicide took place in the home (WVDRS) | .780 | |||
| No | 14 (23.73) | 5 (21.74) | Referent | |
| Yes | 45 (76.27) | 18 (78.26) | 1.12 (0.32, 4.56) | |
| *2 missing values | ||||
|
| ||||
| Perpetrator status after homicide (WCADV) | .935 | |||
| Alive | 34 (56.67) | 15 (62.50) | Referent | |
| Committed suicide | 20 (33.33) | 7 (29.17) | 0.79 (0.23, 2.52) | |
| Other | 6 (10.00) | 2 (8.33) | 0.76 (0.07, 4.92) | |
| Geographical Characteristics | Urban (n=60, 71%) (n, %) | Rural (n=24, 29%) (n, %) | Unadjusted Odds Ratio (95% Cl) | P value |
|---|---|---|---|---|
|
| ||||
| Concentrated Disadvantage Index (Census 2000) | 11 (18.33) | 6 (25.00) | Referent | .804 |
| Lowest tertile | 15 (25.00) | 5 (20.83) | 0.61 (0.12, 3.16) | .720 |
| Middle tertile | 34 (56.67) | 13 (54.17) | 0.70 (0.19, 2.82) | .552 |
| Highest tertile | ||||
|
| ||||
| Instability (Census 2000) | .032a | |||
| Lowest tertile | 7 (11.67) | 7 (29.17) | Referent | |
| Middle tertile | 24 (40.00) | 12 (50.00) | 0.50 (0.11,2.13) | .339 |
| Highest tertile | 29 (48.33) | 5 (20.83) | 0.17 (0.03, 0.88) | .024a |
Significant at alpha = .05
Race differed significantly between urban and rural women (P = .003), with no Black women murdered in rural areas, and a lower proportion of women of “other” races or ethnicities murdered in rural areas than urban ones. Fully 83% of rural women murdered were white. In addition, all women murdered in rural areas were born in the United States, as opposed to 82% in urban areas (P = .029).
Nearly half of all victims were married and marital status was significantly different between urban and rural areas (P = .050). Compared to their urban counterparts, the odds of women in rural areas being married compared to having never been married were 4 times greater (OR=4.18, 95%CI=[1.09, 19.49]; P = .028).
Slightly over 40% of victims had a high school education. Level of education did not significantly differentiate urban and rural women. Pregnancy at time of death or within a year before death was not significantly different among urban and rural women and represented 6% of all women.
Type of relationship with the perpetrator was marginally significantly different (P value = .055), with a smaller proportion of women in rural areas murdered by a boyfriend, as compared to a husband. This mirrors the findings with regard to marital status, with a higher proportion of rural women married. Perpetrator age, condition of the relationship, presence of young children, and history of IPV were not significantly different between urban and rural deaths. In almost 60% of both urban and rural deaths, there were indications of trouble in the relationship, with 25% of deaths showing an indication that the relationship was moving toward dissolution at the time of death. In almost half of the deaths, the couple was known to have young children.
No homicide characteristics examined (weapon type, number of penetrating wounds, suspected alcohol use, whether homicide took place in the home, whether the perpetrator committed suicide) were significantly different for urban versus rural deaths. Firearms were the most common weapon causing the fatal injury (43%). Seventy-six percent of urban and 78% of rural deaths took place in the home. In 33% of urban and 29% of rural deaths, the perpetrator committed suicide.
Fully 71% of victims lived in urban areas. Residential instability differed among rural and urban women, with women living in neighborhoods with higher instability less likely to be rural than to be urban (high to low instability OR=.17, 95%CI=[0.03, 0.88]). Neighborhood disadvantage did not differ significantly between urban and rural women.
Multivariate Analyses
Results of our multivariate analyses are shown in Table 5. We began with the individual-level predictors age, race, marital status, and level of education. Race was dichotomized to white/other due to small numbers. Both race and marital status were significantly associated with rural setting, with non-white women less likely to be rural (OR=0.15, 95%CI=[0.04, 0.57]), and married women more likely to be rural than never married women (OR=7.04, 95%CI=[1.61, 30.88]). When controlling for neighborhood disadvantage, race and maritalw.
Table 5.
Models Differentiating Urban and Rural Intimate Partner Femicides Using Marital Status (n=84)
| Characteristic | Model 1: Individual-level model using marital status % correctly classified: 78.6% Area Under Curve (AUC): 0.71 OR (95% CI), P value | Model 2: Individual-level model with neighborhood disadvantage % correctly classified: 79.8% Area Under Curve (AUC): 0.80 OR (95% CI), P value | Model 3: Individual-level model with residential instability % correctly classified: 75.0% Area Under Curve (AUC): 0.83 OR (95% CI), P value | Model 4: Individual-level model with neighborhood disadvantage and residential instability % correctly classified: 79.8% Area Under Curve (AUC): 0.84 OR (95% CI), P value | Unadjusted Odds Ratios based on US Census 2000 Proportions of Wisconsin women |
|---|---|---|---|---|---|
|
| |||||
| Victim's Age | |||||
| 16–24 | Referent | Referent | Referent | Referent | Referent |
| 25–34 | 0.67 (0.11, 4.07) | 0.73 (0.11, 4.63) | 0.62 (0.09, 4.20) | 0.83 (0.11, 6.52) | 0.92 (0.91, 0.93) |
| 35–44 | 1.53 (0.30, 7.83) | 1.62 (0.30, 8.59) | 1.31 (0.24, 7.03) | 1.37 (0.23, 7.97) | 1.06 (1.05, 1.07) |
| 45+ | 0.38 (0.06, 2.42) | 0.44 (0.06, 3.13) | 0.26 (0.04, 1.93) | 0.38 (0.05, 3.04) | 1.26 (1.25, 1.27) |
| Overall P value = .332 | Overall P value = .462 | Overall P value = .277 | Overall P value = .552 | (women age 16+) | |
|
| |||||
| Victim's Race | |||||
| White | Referent | Referent | Referent | Referent | Referent |
| Other | 0.15 (0.04, 0.57)a | 0.14 (0.03, 0.55)a | 0.13 (0.03, 0.54)a | 0.08 (0.02, 0.41)a | 0.23 (0.22, 0.24) |
| Overall P value = .006 | Overall P value = .005 | Overall P value = .005 | Overall P value = .002 | (women age 18+) | |
|
| |||||
| Victim's Marital status | |||||
| Never married | Referent | Referent | Referent | Referent | Referent |
| Married | 7.04 (1.61, 30.88)a | 7.19 (1.61, 31.99)a | 7.76 (1.59, 37.91)a | 8.68 (1.63, 46.22)a | 1.64 (1.62,1.65) |
| Divorced/Widowed | 1.84 (0.29, 11.59) | 1.79 (0.28, 11.37) | 1.90 (0.26, 14.09) | 1.74 (0.23, 13.33) | 1.42 (1.41, 1.44) |
| Overall P value = .018 | Overall P value = .018 | Overall P value = .018 | Overall P value = .016 | (women age 18+) | |
|
| |||||
| Victim's Level of education | |||||
| Less than HS degree | Referent | Referent | Referent | Referent | Referent |
| HS degree | 3.14 (0.51, 19.36) | 3.18 (0.51, 19.70) | 2.22 (0.32, 15.46) | 1.97 (0.27, 14.27) | 1.09 (1.08, 1.10) |
| Some college or higher | 1.49 (0.22, 9.97) | 1.61 (0.24, 11.04) | 0.91 (0.12, 7.07) | 0.95 (0.12, 7.76) | 0.73 (0.72, 0.74) |
| Overall P value = .328 | Overall P value = .356 | Overall P value = .373 | Overall P value = .541 | (women age 18+) | |
|
| |||||
| Concentrated Disadvantage Index | c | ||||
| Least disadvantage | b | Referent | b | Referent | Referent |
| Moderate disadvantage | 1.27 (0.24, 6.84) | 1.50 (0.26, 8.56) | 4.12 (4.09, 4.15) | ||
| Most disadvantage | 1.51 (0.33, 6.96) | 4.15 (0.68, 25.51) | 1.75 (1.73, 1.76) | ||
| Overall P value = .870 | Overall P value = .281 | (women age 18+) | |||
|
| |||||
| Residential Instability | c | ||||
| Least instability | Referent | Referent | Referent | ||
| Moderate instability | b | b | 0.58 (0.12, 2.81) | 0.47 (0.09, 2.15) | 0.81 (0.80, 0.82) |
| Most instability | 0.17 (0.03, 0.97)* | 0.08 (0.01, 0.63)* | 0.28 (0.28, 0.28) | ||
| Overall P value = .106 | Overall P value = .043 | (women age 18+) | |||
Significant at alpha = .05
These variables were not examined in this particular model, so there is no data.
A direct comparison between model results and odds ratios derived from US Census data for deprivation and instability may not be appropriate because the tertiles for these measures as included in the models were computed separately for urban and rural IPF victims.
When adding neighborhood instability to our individual-level model, high instability is significantly associated with rurality, with women living in high instability neighborhoods less likely to be rural (high to low instability OR=0.17, 95%CI=[0.03, 0.97]). With neighborhood disadvantage and instability examined simultaneously, the effects for race and instability increase in magnitude, with women living in neighborhoods with more residential instability much less likely to be rural (high to low instability OR=0.08, 95%CI=[0.01, 0.63]). A comparison of our model findings to census-derived odds ratios (Table 5) reveals that the effects we find for race and marital status are stronger than the differences we would expect given the overall patterns of these demographic features in rural and urban Wisconsin environments. In addition, the effect we find for highly unstable residential environments is stronger than what would be expected given our knowledge of patterns of residential instability in Wisconsin.
Substitution of perpetrator relationship for marital status (see Table 6 in supplemental materials) did not substantially change the effects of neighborhood-level factors, nor the effect for race. Perpetrator relationship as husband was marginally significantly associated with rurality, when compared to relationship as boyfriend.
DISCUSSION
Evidence suggests linkages between characteristics of residential environments and IPV. Evidence also suggests that while geographic setting may be associated with partner violence in both urban and rural settings, the nature of the influence may be different. Here, we begin to empirically examine the differences between urban and rural residential environments associated with IPF.
We find that a commonly used measure of disadvantage differs in urban versus rural environments (Table 2). When taking rurality into account in defining disadvantage, we find no difference between urban and rural IPFs in terms of their exposure to disadvantage. This finding raises a number of questions for future research. First, do commonly used measures of concentrated disadvantage reflect the nature of rural poverty? Rural poverty is often linked to different economic factors than urban poverty, with occupational categories such as agriculture taking a more prominent place. Future work should identify measures that most appropriately capture the nature of rural poverty. Furthermore, should neighborhood definitions have similar geographical sizes in rural and urban areas, and does the concept of a “neighborhood” have equal relevance in each setting? A recent systematic review considered different approaches to defining rural environments, including administrative boundaries and distance measures, finding a range of approaches currently in practice.50 Finally, how does one best define rurality itself? Little consensus exists in the literature; the measure used here is imperfect and to some degree dependent on a small sample size. We do not distinguish different degrees (small town, rural, remote) or types (farm, non-farm) of rurality. Future work should examine both spatial and conceptual definitions of rural environments.
Regarding residential instability, we find that higher levels of instability are linked with urbanicity, even after crafting a measure of residential instability that accounts for differences between urban and rural areas. While instability has been used to indicate potential disruption of neighborhood social cohesion and increased violence risk, this may not hold true in rural areas. In rural settings, residential stability could be an indication of entrenched social relationships similar to the notions of lack of privacy and anonymity cited as a problem for rural women experiencing IPV.42 With little change in residence over time and low population density, it is likely that a woman and her abuser are known to many in their neighborhood or region, including police, judicial representatives, health care providers, and shelter or safe house personnel.36 Overall, our findings indicate the possibility of a different role for neighborhood context in affecting intimate violence risk in rural settings, and suggest that different measures may be needed to capture the qualities of rural environments that affect intimate violence risk.
In addition to our findings regarding neighborhood residential environments, there are additional results worth emphasizing. In our study area, as illustrated in our Census-based comparisons, non-white race/ethnicity is a feature of urban populations. In addition, although marital status differs among both our study population and the population of Wisconsin generally—with more rural women than urban women reported as married—the impact of IPF on children is similar and strong (50% of deaths). Perpetrator suicide is a significant factor in intimate partner femicides (32%). Firearms may play a larger role in rural areas (54% rural, 40% urban), although our sample size would not allow for the detection of this difference. Others have suggested that firearms are more prevalent in rural areas and may play a larger role in IPV.37 It is known that alcohol use by the victim is known not to be a factor in 62% of deaths. IPFs predominantly take place in the home (75%) and relationships are often in some stage of dissolution (58%), with a partner leaving the relationship often a catalyzing event. History of IPV is known more often in urban (50%) than rural (33%) deaths, which may be attributable to under-reporting in rural areas; our analysis was unable to determine whether this is due to an actual difference in patterns of violence or because of more effective reporting or documentation in urban areas. Finally, we find that marital status does not measure the same quantity as relationship with the perpetrator. Future work should identify new approaches to capture the nature of intimate relationships and how they relate to IPV and IPF risk.
Our analysis is subject to some important limitations. The small sample size and resulting lack of clustering by neighborhood limited our ability to utilize multilevel modeling or related analysis approaches. The small sample size also affected our ability to detect more subtle differences that may differentiate urban and rural IPFs. In addition, it is well known that the choice of neighborhood definition may affect analysis results;51 given the small sample size and inability to utilize analysis strategies that would allow a more complete consideration of geographical variation, we elected to consider only the census tract. RUCA codes are available for census tract, postal (ZIP) code, and county, and we considered census tract to be the most appropriate of these definitions given its size and relative stability over time.52 Rurality can be defined in numerous ways. Researchers with access to larger databases should consider a more refined definition of urban and rural, for instance including a separate category for suburban deaths or considering variation across the spectrum of rurality. We analyzed victim data from 2004–2008 in concert with Census data from the year 2000; this temporal mismatch could introduce error. Our sample was limited to Wisconsin residents, and it cannot be directly generalized to other populations.
Boyle et al recently argued: “Given that IPV is a product of social context, it is not at all clear that traditional medical approaches such as individual screening and intervention will represent effective or efficient strategies for reducing IPV. An alternative is to focus on the social determinants of IPV with a view to identifying modifiable characteristics for prevention.”53 We agree with this sentiment and with other researchers54 who argue that a future direction for research relating neighborhood residential environments to health should focus on modifiable characteristics of neighborhoods in order to have the most impact on policy, practice, and eventually prevention. With regard to IPV, future work should consider resource access and emergency response, among other factors, and should include a more thorough examination of non-urban settings. Our findings reinforce the argument that multilevel strategies will be required to understand and reduce the burden of intimate violence, and that interventions may need to be crafted for specific geographical contexts.
Supplementary Material
Acknowledgments
Thanks to Amy Schlotthauer and Donna Peterson of the Medical College of Wisconsin Injury Research Center; Becky Turpin of the Wisconsin Department of Health Services; the Wisconsin Coalition Against Domestic Violence and consultant Jane Sadusky; and Medical College of Wisconsin Reference Librarian Rita Sieracki. This work was supported in part by the Clinical & Translational Science Institute of Southeast Wisconsin: NIH UL1RR031973. The Wisconsin Violent Death Reporting System is supported by cooperative agreement #U17/CCU523099 from the US Centers for Disease Control and Prevention (CDC) at the Wisconsin Department of Health Services, Injury and Violence Prevention Program. The views expressed in this report do not necessarily reflect the official policies of the Department of Health Services, nor does mention of trade names, commercial practices, or organizations imply endorsement by the US government or the funding sources named.
REFERENCES
- 1.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. 2006 Oct 7;368(9543):1260–1269. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 2.Heise L, Ellsberg M, Gottmoeller M. A global overview of gender-based violence. International Journal of Gynecology & Obstetrics. 2002 Sep;78(Suppl 1):S5–14. doi: 10.1016/S0020-7292(02)00038-3. [DOI] [PubMed] [Google Scholar]
- 3.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002 Oct 5;360(9339):1083–1088. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 4.Watts C, Zimmerman C. Violence against women: global scope and magnitude. Lancet. 2002 Apr 6;359(9313):1232–1237. doi: 10.1016/S0140-6736(02)08221-1. [DOI] [PubMed] [Google Scholar]
- 5.Wuest J, Merritt-Gray M, Ford-Gilboe M, Lent B, Varcoe C, Campbell JC. Chronic pain in women survivors of intimate partner violence. Journal of Pain. 2008 Nov;9(11):1049–1057. doi: 10.1016/j.jpain.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Bonomi AE, Thompson RS, Anderson M, et al. Intimate partner violence and women's physical, mental, and social functioning. Am J Prev Med. 2006 Jun;30(6):458–466. doi: 10.1016/j.amepre.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Saltzman LE, Johnson CH, Gilbert BC, Goodwin MM. Physical abuse around the time of pregnancy: an examination of prevalence and risk factors in 16 states. Maternal and Child Health Journal. 2003 Mar;7(1):31–43. doi: 10.1023/a:1022589501039. [DOI] [PubMed] [Google Scholar]
- 8.Saltzman LE. Intimate partner violence surveillance: uniform definitions and recommended data elements. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Atlanta, Georgia: 1999. [Google Scholar]
- 9.O'Campo P, Gielen AC, Faden RR, Xue X, Kass N, Wang MC. Violence by male partners against women during the childbearing year: A contextual analysis. Am J Public Health. 1995;85(8):1092–1097. doi: 10.2105/ajph.85.8_pt_1.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Wyk JA, Benson ML, Fox GL, DeMaris A. Detangling Individual-, Partner-, and Community-Level Correlates of Partner Violence. Crime & Delinquency. 2003;49(3):412. [Google Scholar]
- 11.Jones AS, Gielen AC, Campbell JC, et al. Annual and lifetime prevalence of partner abuse in a sample of female HMO enrollees. Women's Health Issues. 1999;9(6):295–305. [Google Scholar]
- 12.Li Q, Kirby RS, Sigler RT, Hwang SS, LaGory ME, Goldenberg RL. A multilevel analysis of individual, household, and neighborhood correlates of intimate partner violence among low-income pregnant women in Jefferson County, Alabama. Am J Public Health. 2010;100(3):531–539. doi: 10.2105/AJPH.2008.151159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cunradi CB, Caetano R, Clark C, Schafer J. Neighborhood poverty as a predictor of intimate partner violence among White, Black, and Hispanic couples in the United States: A multilevel analysis. Ann Epidemiol. 2000;10(5):297–308. doi: 10.1016/s1047-2797(00)00052-1. [DOI] [PubMed] [Google Scholar]
- 14.Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Womens Health Issues. 2004 Jan-Feb;14(1):19–29. doi: 10.1016/j.whi.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Lanier C, Maume MO. Intimate Partner Violence and Social Isolation Across the Rural/Urban Divide. Violence Against Women. 2009;15(11):1311–1330. doi: 10.1177/1077801209346711. [DOI] [PubMed] [Google Scholar]
- 16.Alhabib S, Nur U, Jones R. Domestic violence against women: systematic review of prevalence studies. Journal of Family Violence. 2010;25(4):369–382. [Google Scholar]
- 17.Benson ML, Wooldredge J, Thistlethwaite AB, Fox GL. The Correlation between Race and Domestic Violence is Confounded with Community Context. Soc Probl. 2004;51(3):326–342. [Google Scholar]
- 18.Campbell JC, Glass N, Sharps PW, Laughon K, Bloom T. Intimate partner homicide: review and implications of research and policy. Trauma Violence Abuse. 2007 Jul;8(3):246–269. doi: 10.1177/1524838007303505. [DOI] [PubMed] [Google Scholar]
- 19.Campbell JC, Webster D, Koziol-McLain J, et al. Risk factors for femicide in abusive relationships: results from a multisite case control study. Am J Public Health. 2003 Jul;93(7):1089–1097. doi: 10.2105/ajph.93.7.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frye V, Galea S, Tracy M, Bucciarelli A, Putnam S, Wilt S. The role of neighborhood environment and risk of intimate partner femicide in a large urban area. Am J Public Health. 2008;98(8):1473–1479. doi: 10.2105/AJPH.2007.112813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miles-Doan R. Violence between spouses and intimates: Does neighborhood context matter? Soc Forces. 1998 Dec;77(2):623–645. [Google Scholar]
- 22.Miles-Doan R, Kelly S. Geographic concentration of violence between intimate partners. Public Health Rep. 1997 Mar-Apr;112(2):135–141. [PMC free article] [PubMed] [Google Scholar]
- 23.Browning CR. The Span of Collective Efficacy: Extending Social Disorganization Theory to Partner Violence. Journal of Marriage & Family. 2002;64(4):833–850. [Google Scholar]
- 24.Dekeseredy WS, Schwartz MD, Alvi S, Tomaszewski E. Perceived collective efficacy and women's victimization in public housing. Criminal Justice: International Journal of Policy and Practice. 2003 Feb;3(1):5–27. [Google Scholar]
- 25.Sampson RJ, Groves WB. Community structure and crime: Testing social-disorganization theory. American Journal of Sociology. 1989:774–802. [Google Scholar]
- 26.Shaw CR, McKay HD. Juvenile delinquency and urban areas. University of Chicago Press; Chicago: 1942. [Google Scholar]
- 27.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997 Aug 15;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 28.Benson ML, Fox GL, DeMaris A, van Wyk J. Neighborhood Disadvantage, Individual Economic Distress and Violence Against Women in Intimate Relationships. Journal of Quantitative Criminology. 2003 Sep;19(3):207–235. [Google Scholar]
- 29.Ackerson LK, Kawachi I, Barbeau EM, Subramanian S. Effects of individual and proximate educational context on intimate partner violence: A population-based study of women in India. Am J Public Health. 2008 Mar;98(3):507–514. doi: 10.2105/AJPH.2007.113738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koenig MA, Ahmed S, Stephenson R, Jejeebhoy SJ, Campbell J. Individual and Contextual Determinants of Domestic Violence in North India. Am J Public Health. 2006;96(1):132–138. doi: 10.2105/AJPH.2004.050872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McQuestion MJ. Endogenous social effects on intimate partner violence in Colombia. Soc Sci Res. 2003;32(2):335–345. [Google Scholar]
- 32.Koenig MA, Ahmed S, Hossain MB, Khorshed Alam Mozumder AB. Women's status and domestic violence in rural Bangladesh: individual- and community-level effects. Demography. 2003 May;40(2):269–288. doi: 10.1353/dem.2003.0014. [DOI] [PubMed] [Google Scholar]
- 33.Uthman OA, Moradi T, Lawoko S. The independent contribution of individual-, neighbourhood-, and country-level socioeconomic position on attitudes towards intimate partner violence against women in sub-Saharan Africa: A multilevel model of direct and moderating effects. Soc Sci Med. 2009;68(10):1801–1809. doi: 10.1016/j.socscimed.2009.02.045. [DOI] [PubMed] [Google Scholar]
- 34.Madkour AS, Martin SL, Halpern CT, Schoenbach VJ. Area disadvantage and intimate partner homicide: an ecological analysis of North Carolina counties, 2004–2006. Violence Vict. 2010;25(3):363–377. doi: 10.1891/0886-6708.25.3.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riddell T, Ford-Gilboe M, Leipert B. Strategies Used by Rural Women to Stop, Avoid, or Escape From Intimate Partner Violence. Health Care Women Int. 2009;30(1/2):134–159. doi: 10.1080/07399330802523774. [DOI] [PubMed] [Google Scholar]
- 36.Grama JL. Women Forgotten: Difficulties Faced by Rural Victims of Domestic Violence. American Journal of Family Law. 2000 Fall;14(3):173. 2000. [Google Scholar]
- 37.Adler C. Unheard and unseen rural women and domestic violence. J Nurse Midwifery. 1996;41(6):463–466. doi: 10.1016/s0091-2182(96)00066-3. [DOI] [PubMed] [Google Scholar]
- 38.Goeckermann CR, Hamberger LK, Barber K. Issues of domestic violence unique to rural areas. Wis Med J. 1994 Sep;93(9):473–479. [PubMed] [Google Scholar]
- 39.Pittenger J. Domestic abuse: complicated by rural living. Wis Med J. 1997 Aug;96(8):22–24. [PubMed] [Google Scholar]
- 40.Gallup-Black A. Twenty Years of Rural and Urban Trends in Family and Intimate Partner Homicide: Does Place Matter? Homicide Studies: An Interdisciplinary & International Journal. 2005 May;9(2):149–173. [Google Scholar]
- 41.Murty SA, Peek-Asa C, Zwerling C, Stromquist AM, Burmeister LF, Merchant JA. Physical and Emotional Partner Abuse Reported by Men and Women in a Rural Community. Am J Public Health. 2003;93(7):1073–1075. doi: 10.2105/ajph.93.7.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teaster PB, Roberto KA, Dugar TA. Intimate Partner Violence of Rural Aging Women. Family Relations. 2006;55(5):636–648. [Google Scholar]
- 43.Peek-Asa C, Wallis A, Harland K, Beyer K, Dickey P, Saftlas A. Rural Disparity in Domestic Violence Prevalence and Access to Resources. J Womens Health. 2011 Sep 15; doi: 10.1089/jwh.2011.2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krishnan SP, Hilbert JC, Pase M. An examination of intimate partner violence in rural communities: results from a hospital emergency department study from Southwest United States. Fam Community Health. 2001 Apr;24(1):1–14. doi: 10.1097/00003727-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention . National Violent Death Reporting System Coding Manual Version 3. National Center for Injury Prevention and Control; 2008. [Google Scholar]
- 46.Wisconsin Domestic Violence Homicide Report 2009. Madison, WI: 2010. Wisconsin Coalition Against Domestic Violence. [Google Scholar]
- 47.WWAMI Rural Health Research Center Rural-Urban Commuting Area Codes. Vol 2011 [Google Scholar]
- 48.US Department of Agriculture Economic Research Service Rural-Urban Commuting Area Codes. 2000;Vol 2011 [Google Scholar]
- 49.Hosmer DW, Lemeshow S. Applied logistic regression. John Wiley & Sons; New York: 1989. [Google Scholar]
- 50.De Marco A, De Marco M. Conceptualization and measurement of the neighborhood in rural settings: a systematic review of the literature. J Community Psychol. 2010;38(1):99–114. [Google Scholar]
- 51.Flowerdew R, Manley DJ, Sabel CE. Neighbourhood effects on health: does it matter where you draw the boundaries? Soc Sci Med. 2008 Mar;66(6):1241–1255. doi: 10.1016/j.socscimed.2007.11.042. [DOI] [PubMed] [Google Scholar]
- 52.Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian S, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census-defined geographic areas--the Public Health Disparities Geocoding Project. Am J Public Health. 2002;92(7):1100. doi: 10.2105/ajph.92.7.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boyle MH, Georgiades K, Cullen J, Racine Y. Community influences on intimate partner violence in India: Women's education, attitudes towards mistreatment and standards of living. Soc Sci Med. 2009;69(5):691–697. doi: 10.1016/j.socscimed.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 54.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010 Feb;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.