Abstract
Purpose
To compare 2 strategies, Stage Matched Nursing and Community Intervention (SMN+CI) and Community Intervention (CI) alone in changing cardiovascular risk factors in up to 3 behavioral areas: diet, physical activity, and/or smoking among rural women.
Methods
A 14-month, multisite randomized controlled trial of 117 rural women was conducted. Transtheoretical model was used in identification of stage of change and development of the SMN+CI nursing interventions. A Social-ecological model was used to address issues of rurality in the development of interventions.
Findings
The SMN+CI group was superior on 4 outcomes. There were significant increases in 2 measures of dietary intake; improvement in dietary stage of change for fruits and vegetables; and reduced diastolic blood pressure (DBP) in the SMN+CI group. After log transformation DBP significance was lost. The CI group had a significant reduction in change in total cholesterol; however, significance was lost after control for the initiation of lipid lowering medications. There was a significant reduction in Framingham risk scores pre- to post-intervention, regardless of group.
Conclusions
There continues to be a need to improve cardiovascular risk factors in rural women. There should be an exploration of whether intensified dose and fidelity of the intervention strategies of diet and physical activity are effective in improving anthropometric and laboratory values. Further investigation is warranted into factors influencing the pre- to post-reduction in Framingham risk scores.
Keywords: cardiovascular disease, nursing, rural women, Social-ecological model, Transtheoretical model
Cardiovascular disease (CVD) is the number 1 cause of death in the world. Over one-third of Untied States (US) women aged 20 and older had some form of CVD in 20081;of these, 47.3% were black and 33.8% white. Prevalence rates of CVD specific for rural dwellers are outdated and difficult to extrapolate from national data.2 Rural Healthy People 2010 indicated rural populations have higher CVD morbidity, particularly in the South and Appalachian portions of the US.3 Although some note a higher prevalence of CVD risk factors in rural populations,4 very few studies have specifically identified the cardiovascular risk burden for rural US populations and these are usually small, descriptive, regional studies.5–8 One study conducted in New Mexico found that “rural patients, regardless of ethnicity received significantly fewer targeted CVD treatments and were less likely to reach blood pressure goals compared with urban patients.9(p420)
Most agree there are limitations in access to health care, particularly specialty care, in rural areas. Cardiology services are often regionalized and may be less accessible to rural populations, who must deal with distance and transportation issues. One study found echocardiogram utilization among rural veterans was limited by distance.10 Another study found that transfer of Acute Myocardial Infarction (MI) patients from rural to more tertiary care facilities reduced inhospital mortality; however, women were transferred less frequently,11 possibly indicating another gap in cardiovascular care for rural women.
Smoking, hypertension, hyperlipidemia and diabetes are known major risk factors associated with increased lifetime risk for CVD and decreased median survival rates.1 Elevated levels of C-reactive protein (CRP) may increase the risk of CVD in women.12 Other recognized modifiable risk factors for CVD include physical inactivity, obesity, and abdominal adiposity.13 Although rural often evokes visions of outdoor work with a physically fit population, this is not always the case. As rural America has become less agriculturally based and more mechanized, rural women have fewer opportunities for physical activity, which in turn increases their cardiovascular risk. Although current literature does not answer the question of whether US rural women have a higher CVD burden than their urban counterparts, it is clear that CVD, as the number 1 killer of women,1 is negatively affecting the health of all women including those living in rural areas, and thus intervention is warranted.
Modifying diet, physical activity and smoking can reduce CVD risks and improve morbidity and mortality rates.14 Even modest behavioral changes have benefits, especially if sustained. However, making and sustaining lifestyle modifications is not easily accomplished. A major gap in the literature exists regarding study interventions lasting more than 6 months. Moreover, results are mixed on whether to approach lifestyle modification from sequential or combined interventions.14
The purpose of this study was to compare 2 strategies, Stage Matched Nursing and Community Intervention (SMN+CI), and Community Intervention (CI) alone, in reducing cardiovascular risk factors and improving risk markers among rural women. This study sought to reduce modifiable cardiovascular risk factors in up to 3 behavioral areas: diet, physical activity, and/or smoking.
Theoretical underpinnings for this study included the Transtheoretical model (TM)15 as well as a social-ecological model to account for both environmental and personal systems in health-related behavior and status.16 Transtheoretical model included assessment of stage of change (SOC) at 5 levels (eg, pre-contemplation, contemplation, preparation, action and maintenance).15 The Moos model16 was chosen to help address environmental system limitations (eg, few sidewalks or safe places to exercise in rural communities) and the fact that many rural women drive long distances to work, thus limiting time for physical activity.
Specific aims included determining whether rural women, ages 35 to 65 in the group that received SMN+CI, would have greater changes than those in the CI group on: 1) dietary intake, physical activity, and/or smoking; 2) forward movement through the SOC for behavioral action relative to dietary intake of fruits and vegetables, fats, fiber; intention for weight loss, and physical activity; and 3) improvement on selected modifiable cardiovascular risks as measured on the Framingham Coronary Disease Risk Prediction tool (Framingham), serum levels for CRP, lipids, and cotinine for those reporting smoking within the last 2 years, and anthropometric outcomes including blood pressure (BP), body mass index (BMI), and waist circumference.
METHODS
Design
Promoting Heart Health (PHH) was a randomized controlled trial (RCT). Human subject committee approval was obtained for this study from 2 universities.
Sample
Two hundred and seventy-four (274) rural women were evaluated for eligibility to participate. Barriers to recruitment and participation included 10% of those evaluated with higher than expected CVD burden, including diagnosis of diabetes, Framingham scores of > 20 points, or positive history of a cardiovascular event. Additional recruitment barriers specific to enrolling rural samples (and which have been previously described17) included costs, transportation, and the need for multiple recruitment events over a wide geographic area.
Women enrolled in this study had a Framingham score of ≤ 20 points and were between 35 and 65 years of age, with no history of coronary heart disease (CHD) or diabetes. Subjects who reported medications such as lipid lowering drugs or antihypertensives were included if they had been taking those medications for at least 1 year.
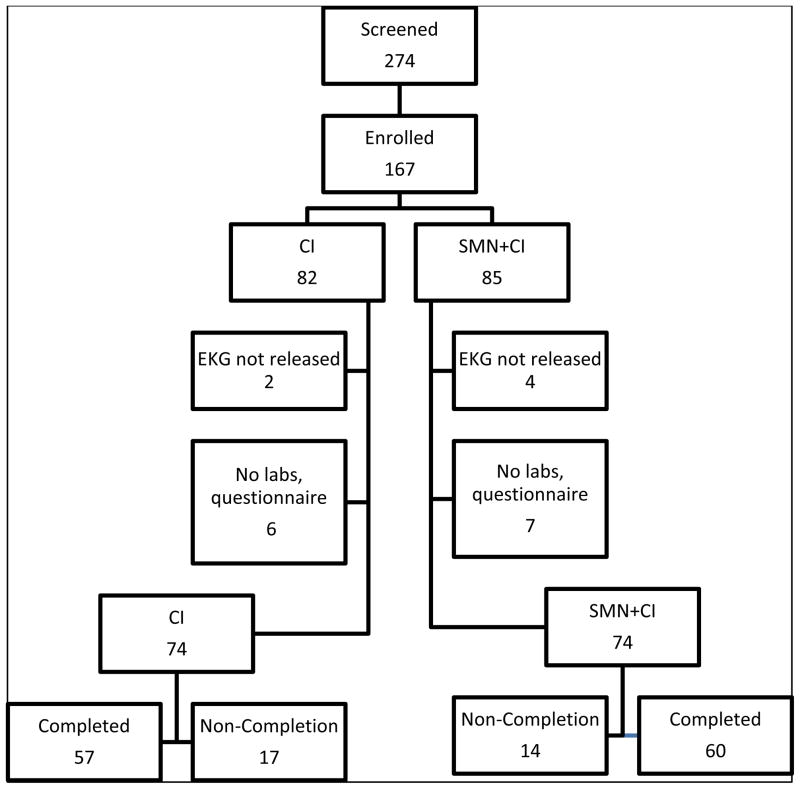
Many rural areas are ethnically homogeneous; for this reason, 2 counties were chosen for recruitment of subjects. Rural county 1 was located in upstate New York (NY) and was predominately Caucasian (98%). Rural county 2 was located in Virginia (VA) with a 12% African American population. Both counties had a rural urban continuum code (RUCC) of 6 on a scale of 1–9.18 The VA site enabled the inclusion of African American women in an attempt to reduce the bias of underrepresentation of this ethnic background in rural CVD research. A power analysis was calculated with α = .05 and ES = .50, resulting in a sample size of 64 per group or N = 128.19 A convenience sample (N = 167) was randomly assigned to SMN+CI or CI groups. Of these, 19 were either medically withdrawn after evaluation of screening electrocardiogram (ECG) or did not complete the first questionnaire. This left 74 women in each of group (N = 148).17 Figure 1 shows the flow of participants through the study. A total of 117 women completed the study physiologic measures, with 110 of these completing the questionnaires. Table 1 shows the demographics for women completing the study and includes columns for the total sample as well as by group. There were no statistically significant differences for any demographic variable between the SMN+CI and CI groups at study entry. The only variance by state was on the self-report of ethnicity with no African American women enrolled from NY.
Figure 1.
Flow of Participants Through Study
Table 1.
Demographics Total Sample and By Group
| Total N (N = 117) | SMN + CI (n = 60) | CI (n = 57) | |
|---|---|---|---|
| Age in years M(SD) | 51 (7.59) | 52 (7.25) | 50 (7.88) |
| Ethnicity N (%) | |||
| Caucasian | 102 (87.2%) | 51 (43.6%) | 51 (43.6%) |
| African American | 10 (8.5%) | 4 (3.4%) | 6 (5.1%) |
| Hispanic | 3 (2.6%) | 3(2.6%) | 0 (0%) |
| Do Not Wish to Answer | 2 (1.7%) | 2 (1.7%) | 0 (0%) |
| Education N (%) | |||
| High School, GED or Less | 30 (25.6%) | 12 (10.3%) | 18 (15.4%) |
| 2-Year College or Less | 48 (41%) | 29 (24.8%) | 19 (16.2%) |
| 4-Year College or Post Graduate | 39 (33.3%) | 19 (16.2%) | 20 (17.1%) |
Procedure
The Community Intervention (CI) consisted of an invitation, extended to all participants, to attend a community-visioning meeting; 1 meeting was held at each site. Meeting participants discussed ways to increase awareness of both female CVD and the local community resources available to women to improve their heart health. A directed round robin exercise elicited and prioritized ideas for new community-based interventions. The NY subjects requested a web-based listing of countywide accessible physical activity sites. The list of sites and photos was posted on the county health department webpage. The VA subjects chose to use an annual health fair organized and held at a primarily African American church as a means to improve heart health in that region. A community organization in each county was given $2,000 to implement each respective idea.
In addition to assessment of SOC for all subjects, TM was used to develop interventions for the SMN+CI group, across multiple behaviors. Interventions were team developed, designed according to the 10 processes of change,15 and approved by a TM consultant (personal communication Sue Rossi, University of Rhode Island). Interventions were also designed to take into consideration the rural living environment using the Moos social-ecological perspective.16 This model helped in designing interventions that accounted for differences in physical environment; for example including ideas for winter outdoor activities in upstate NY and planning physical activity in early morning or later evening in the heat of VA summers. Positive rural environmental factors built into interventions included identifying advantages of space and the cultural aspect of growing vegetables and fruits as well as using seasonal, locally grown foods in a heart healthy diet. Nurses providing the interventions received training on the staged matched interventions in a 2-day workshop.
Each enrolled subject received a pedometer and a monthly diary. The diary included sections for daily recordings of numbers of: 1) servings of various types of food, 2) pedometer steps, and 3) cigarettes smoked. All subjects were paid $5 for each returned diary whether or not completed. Diary and pedometer use were voluntary and are not reported here.
In addition to the community interventions, subjects in the SMN+CI group were also visited 4 times by 1 of 12 Registered Nurses (RNs), using a book of possible interventions for up to 3 areas: diet, physical activity, and/or smoking. Subject and RN negotiated time and place of visit as well as which area(s) to address for each visit.
MEASURES
A booklet containing previously tested instruments measuring dietary intake, 20 physical activity21 and smoking behaviors,22 as well as demographic and SOC measures,22 was given to each participant at the beginning and end of the study. Preintervention anthropometric measures were obtained the day of enrollment and fasting laboratory serums were drawn the following morning. Data reported here include answers to the questionnaires and physiologic measures collected at the time of enrollment and again 14 months later. Post physiologic measures were usually gathered at the same site where subjects had enrolled such as church or workplace. If a subject had scheduling conflicts with the planned final data collection, physiologic measures were obtained by an RN in the home.
Dietary Intake
The National Institute of Health fruit and vegetable food frequency questionnaire (NIH F&V) included 3 subscales: 1) fruit intake by meal, 2) vegetable intake by meal, and 3) total fruit and vegetable daily intake.20 This instrument measures frequency of intake as well as portion size. Validity for this tool was noted as significantly better than previous tools at measuring fruit and vegetable intake, particularly for women.20 Cronbach’s alpha based on standardized items was calculated as .64 for vegetable, .74 for fruit and .82 for fruit and vegetable intake by meal in this study. The NIH Fat and Fiber screener (NIH F&F) provided an estimate of daily percent of energy from fat.23 The Department of Agriculture recommends between 25% and 35% of daily caloric intake be derived from fats.24 The 10 items regarding high fat intake had a Cronbach alpha = .69.
Physical Activity
The Yale Physical Assessment Scale (YPAS) was used to measure Total Time Summary Index (TTSI), Energy Expenditure Summary Index (EESI), and Activity Dimension Summary Index (ADSI) scores.21 Time spent in work, yard work, caretaking, exercise, and recreational activities was calculated to provide a TTSI reported as hours per week. The EESI provided an estimation of energy use, reported as kilocalories (Kcal) per week. The ADSI included the 5 dimensions of vigorous and leisurely walking, moving about, standing, and sitting. The YPAS was designed to capture the lower ranges of physical activity seen in older adults by including activities they might participate in such as light housekeeping and gardening.21 Early work on the YPAS used a 2-week test—data were retested to establish reliability, with correlation coefficients ranging from .42 to .65.21 Significant correlations have been reported between the YPAS and the Stanford 7-day physical activity recall (PAR), establishing YPAS validity.25 The areas of lighter activity measured within the ADSI subscale, such as sitting, standing and moving did not correlate as well as walking and vigorous activity or the total summary of the ADSI with the PAR measure.25 Although initially used with adults 60 and older, the instrument has been used with a variety of groups including postpartum women.26 The YPAS was chosen for this study since little was known about the physical activity levels of this population. The instrument included activities thought to be pertinent to rural women such as gardening and the fact that it had been previously used in a sample that included African American women.25 The average energy expenditure for subjects in this study, at 6,445 Kcal/week, compares well to those in the original work where female subjects expended an average of 6,935 Kcal/week.21
Smoking
Smoking habits were measured with the University of Rhode Island (URI) Model Stage of Change instrument.22 Serum cotinine samples were only drawn for women who reported having smoked in the past 2 years upon entry to the study. Cotinine costs were prohibitive for measurement of all subjects.
Stages of Change (SOC)
Transtheoretical model instruments were used to measure SOC in the areas of diet, physical activity, and smoking.22 Instruments included SOC for dietary intake of fruits and vegetables, fat, fiber, physical activity, smoking, and weight loss intentions. Stage of change was calculated from self-reports about current behavior, whether the individual was considering changing her behavior, and the timeframe in which she expected to make that change.
Framingham Coronary Heart Disease Risk Score (Framingham)
Risk assessment for CHD was derived using the Framingham prediction score sheet for women.27 The Framingham calculates risk of CHD within a 10-year period for those without known heart disease, but it does not predict other CVD risks. The algorithm included age grouped in increments of 5 years, total cholesterol, high-density lipid (HDL), BP, and status as a diabetic and smoker.27 The Framingham risk score sheet for women was found to be valid and reliable in the original work on development of the simple algorithm approach to measuring CHD risk for women.27
Physiologic Measures
Physiologic measurements included systolic and diastolic BP, height, weight, BMI, waist measurements, total cholesterol, LDL, HDL, triglycerides, CRP, and serum cotinine, as indicated above. Blood pressure was measured using the Joint National Commission on Hypertension (JNC VII) criteria28 with 3 measurements, averaging the last 2. Laboratory samples were processed on site or at the closest collaborating hospital lab. Samples were transported to 1 site for analysis using laboratory protocol.
Pre and post Framingham and anthropometric measures for the 117 people completing the study are shown in Table 2. There were no statistically significant differences between the 2 groups (SMN+CI vs CI) before interventions for any of the variables measured.
Table 2.
Pre and Post Intervention Measures by Group and Total Sample
| Preintervention Postintervention |
SMN + CI | CI | N = 117 |
|---|---|---|---|
| SBP | 123 mmhg | 122 mmhg | 122.5 mmhg |
| 120 mmhg | 120 mmhg | 120 mmhg | |
| DBP | 80 mmhg | 78 mmhg | 79 mmhg |
| 76 mmhg | 77 mmhg | 76.5 mmhg | |
| BMI | 31 K/m2 | 30 K/m2 | 30.5 K/m2 |
| 30 K/m2 | 30 K/m2 | 30 K/m2 | |
| Waist | 38 inches | 37 inches | 37.5 inches |
| 38 inches | 36 inches | 37 inches | |
| Framingham | 7 points | 6 points | 6.5 points |
| 4.85 points | 4 points | 4.43 points | |
| Total Cholesterol | 212 mgDL | 212 mgDL | 212 mgDL |
| 212 mgDL | 201 mgDL | 206.5 mgDL | |
| LDL | 145 mgDL | 135 mgDL | 140 mgDL |
| 139 mgDL | 123 mgDL | 131 mgDL | |
| HDL | 56 mgDL | 55 mgDL | 55.5 mgDL |
| 56 mgDL | 55 mgDL | 55.5 mgDL | |
| TG | 131 mgDL | 112 mgDL | 121.5 mgDL |
| 125 mgDL | 116 mgDL | 120.5 mgDL | |
| CRP | 4 mgL | 4 mgL | 4 mgL |
| 3 mgL | 4 mgL | 3.5 mgL | |
| Cotininea | 189 ngML | 188 ngML | 188.5 ngML |
| 158 ngML | 209 ngML | 183.5 ngML |
Systolic blood pressure (SBP), diastolic blood pressure (DBP), body mass index (BMI), total cholesterol (TC), low density lipid (LDL), high density lipid (HDL), triglycerides (TG), and c-reactive protein (CRP).
Cotinine levels available on 15 subjects pre and postintervention.
RESULTS
Alpha was preset at .05. Data analysis included N =117 for physiologic measures. Sample size for analyses of self-report instruments was 110. The physical activity instrument (YPAS) responses of “no answer” or “do not know” were coded as missing data. The number of subjects for computations on the YPAS subscales ranged from 98 to 110.
At the end of the study the SMN+CI group had higher fruit intake by meal (P = .005) and showed greater pre-post change in total fruit and vegetable intake (P = .03). Although the SMN+CI group also ate more vegetables by the end of the study, the difference between the 2 groups was not significant (see Table 3).
Table 3.
Independent t-test and Confidence Intervals on Fruit and Vegetable and Fat Screeners
| SMN+CI(58); CI (52) | Mean (SD) | t | 95%CI | |
|---|---|---|---|---|
| Fruit by meal | SMN + CI | 1.62 (1.26) | 2.89* | (0.189, 1.01) |
| CI | 1.02 (.91) | |||
| Vegetables by Meal | SMN + CI | 2.48 (1.73) | 1.09 | (−2.81, .965) |
| CI | 2.14 (1.54) | |||
| All Fruit & Vegtables | SMN + CI | 5.36 (3.18) | 1.71 | (1.01, .592) |
| CI | 4.62 (3.02) | |||
| Total Fruit & Vegetable | SMN + CI | 1.26 (3.08) | 2.16* | (.085, 1.99) |
| Pre-Post Difference | CI | .22 (1.86) | ||
| % of Energy from Fat | SMN + CI | 30.42 (4.08) | −1.72 | (−3.40, 0.24) |
| CI | 32.00 (5.50) | |||
| % Energy | SMN + CI | −2.52 (4.78) | −.810 | (−2.82, 1.19) |
| Pre-Post Difference in | CI | −1.7 (5.82) |
Statistically significant difference = *. Pre-post difference calculated by subtracting preintervention from postintervention values.
There were no statistically or clinically significant differences in percent of energy from fat by group. A reduction of more than 4% of energy from fat is considered clinically significant.24 The mean reduction for the CI group was 1.7% and it was 2.5% for the SMN+CI group. Both groups had an acceptable mean intake of percentage of energy from fat.
The only physical activity subscale to show a significant correlation with self-reported regular physical activity was the ADSI (r =.55, P = .00). There were no significant differences between groups for either physical activity postintervention or in the change scores calculated by subtracting post from preintervention values and conducting an independent t-test on the change.
Stage of Change was collapsed into 2 groups: 1) preparation or lower and 2) action or higher for analysis since some cells had too few subjects using all 5 SOC. In calculating the proportion of women making changes in SOC, a best-case scenario was used. This scenario occurred with 1 of 2 conditions: 1) when a woman moved from preparation or below to action or higher; or 2) if in action or higher preintervention, stayed in that stage or moved from action to maintenance postintervention. Table 4 shows the number and percentage of those making the best-case scenario change by group for SOC variables. The best-case scenario for dietary fruit and vegetable intake was the only significant SOC measure between groups (χ2 (1)= 6.35, P = .012).
Table 4.
Best-Case Scenario Changes in Stage of Change by Group for Diet: Fruit & Vegetables, Fat, and Fiber; Physical Activity; and Weight Loss Intention
| SOC Measure | Group | Pre (n = 117) (% total) Action or Higher | Post (n = 110) (% total) Action or Higher | Best Scenario (% Group) |
|---|---|---|---|---|
| Diet: Fruit & Vegetable | SMN + CI | 8 (6.8%) | 28 (25.5%) | 28 (68.3%) |
| CI | 12 (10.3%) | 13 (11.8%) | 13 (31.7%) | |
| Diet: Fat | SMN + CI | 23 (19.7%) | 41 (37.3%) | 37 (53.6%) |
| CI | 29 (24.8%) | 35 (31.8%) | 32 (46.4%) | |
| Diet: Fiber | SMN + CI | 31 (26.5%) | 47 (42.7%) | 42 (53.8%) |
| CI | 33 (28.2%) | 40 (36.4%) | 36 (46.2%) | |
| Physical Activity | SMN + CI | 33 21.2%) | 32 (29.1%) | 30 (52.6%) |
| CI | 35 (22.4%) | 31 (28.2%) | 27 (47.4%) | |
| Weight Loss | SMN + CI | 60 (38.5%) | 52 (47.3%) | 23 (56.1%) |
| CI | 57 (36.5%) | 41 (37.3%) | 18 (43.9%) |
Stage of Change (SOC), Stage Matched Nursing and Community Intervention (SMN+CI), Community Intervention (CI). (N = 110)
Framingham scores ranged from −2 to 13 points, M = 4.50, SD = 3.56. There was no significant difference on Framingham by group after the intervention (t (115) = 1.07, P = .28), yet, Framingham scores decreased significantly for the entire sample (t (116) = 6.01, P = .000), despite the fact that 18 (15%) subjects had moved into an older age category adding points to the Framingham calculations.
Anthropometric measures, by group, for both pre and postintervention on the 117 subjects completing the study can be seen in Figure 1. The only statistically significant difference by group in BP was in the pre-post diastolic change. The SMN+CI group had a larger change in DBP (− 4 mmHg) compared to a decrease of − .4 for the CI group. Although the difference in change was statistically significant, a reduction of 4 mmHg would be considered a small and clinically non-significant change in diastolic BP28; this difference disappeared with log transformation of BP data. The mean BP for all participants was 120/77 mmHg postintervention.
Over half (59, 53%) of the subjects lost weight over the 14-month intervention; of those 31 (53%) were in the SMN+CI group. Although the range for weight loss in the SMN+CI group was from 0.5 to 45.5 pounds, the median weight change for this group was only − 0.5 pounds. Zero (0) was the median weight loss for the CI group. Mean BMI was reduced by 1 point over the 14 months for the SMN+CI and unchanged for the CI group. The CI group had a slightly lower waist measurement postintervention. No differences in measures of weight, BMI, or waist circumference were statistically significant.
Lipid levels for the 117 women showed acceptable mean HDL pre and postintervention. Both groups showed a trend level reduction in total cholesterol (P = .09) and LDL (P =.06). Pre-post changes in total cholesterol were calculated. SMN+CI had a mean reduction of .05 mg/dl compared to 11 mg/dl for the CI group (t= 2.36, df = 115, P = .02). This difference turned out to be pharmacologically determined. In the CI group, 7 women compared to 1 woman in SMN+CI reported beginning a lipid lowering drug during the study. After controlling for those on lipid lowering medications, the statistically significant difference in pre to post cholesterol levels by group disappeared.
DISCUSSION
Adding targeted nursing interventions to community interventions significantly improved outcomes for 3 dietary measures: 1) intake of fruit by meal, 2) change in total fruit and vegetable intake (see Table 4), as well as 3) SOC for readiness to intake 5 or more servings of fruits and vegetables. SMN+CI subjects also showed a statistically significant but clinically small decrease in diastolic BP, which disappeared after log transformation. Although both groups reduced total cholesterol, initial analysis indicated a significant pre to post reduction for those in the CI group. Further analysis indicated that 7 women in this group had added a lipid lowering agent after entering the study. After correction for those on lipid lowering medications during the study, there was no longer a significant difference for the CI group. The SMN+CI group had a slight reduction in cholesterol despite only 1 additional subject reporting the initiation of lipid lowering drugs after the beginning of the study.
Lipid lowering medications have been shown to be effective in reducing cholesterol yet these medications are not suitable for everyone and are not without risks. A relationship between statins, a type of lipid lowering medication, and the development of diabetes was suggested from a meta-analysis in 201029 and most recently this link has been reported among post-menopausal women in the Women’s Health Initiative.30 Thus, nursing interventions that trend toward lowering cholesterol through behavior modification should receive consideration. The National Heart Blood and Lung Institute recommends a trial of 3 months on behavioral modification prior to trying lipid lowering medications for women with Framingham risk scores of < 20 as was true of women in this study.31
Both interventions significantly reduced the Framingham risk scores for study participants. There were also trends for increased physical activity in both groups. From these trends it would appear that more study is warranted on the effect of raising individual and community awareness of risks to women’s heart health.
Designing interventions for up to 3 behavioral areas at once was undertaken to help build synergy in addressing heart health holistically. One criticism of research using the Transtheoretical model is that if someone enters a study for a particular behavior they are most likely already willing to work on that behavior, and would thus be beyond precontemplation. The study design allowed us to enroll subjects who were ready to work on 1 behavior and begin additional interventions in areas where women were not yet contemplating change at the time of study enrollment.
Comparison of results to other literature specific to cardiovascular risk factors and rural women is difficult due to differences in age ranges across studies.7,8,32–34 One age-comparable study was found that was successful in reducing BMI and waist circumference using a 12-week classroom intervention that included actual physical activity sessions.32 There were differences between the 2 studies on physiologic variables preintervention (eg, current study participants had an average beginning BMI of 30.5 K/m2 and waist circumference of 37.5 in. compared to 32.75 K/m2 and waist of 40.2 in. in the study of rural overweight and obese midlife women).32 What is unknown is whether the changes seen using the classroom format would have held for a longer timeframe, such as in the PHH study.
Two comparisons can be made between this study and a descriptive report where 87% of the sample consisted of rural women.34 First, initially the women in this sample were more likely to be obese (44.4% vs 38.1%).34 However, by the end of our study only 38.5% of subjects regardless of intervention were obese, which compared favorable to the Pullen et al report.34 Secondly, the SMN+CI group had a higher percentage of subjects in the action and maintenance SOC for dietary fruit and vegetable intake compared to the Pullen study.34 A cluster randomized study lasting 6 months had similar outcomes to this PHH study; however, the sample differed as they used men and women living in 20 housing projects.35 These researchers were also able to increase fruit and vegetable dietary intake in the group receiving individual counseling.35 It is difficult to find studies with interventions in multiple behaviors conducted in a sample of rural women.
Limitations
Consistent with another intervention study,36 the calculated attrition over this 14-month study was 21% based on the completion of 117 subjects. The duration of this study does correct previously recognized design flaws of inadequate time to measure long-term behavioral changes using the Transtheoretical model. Five percent (5%) of those completing the study were African American. The most often cited reason for withdrawal, regardless of race, was “too busy.” High attrition rates in long-term studies are not unexpected. Another limitation is that no true control group, without intervention, was used in this design.
Although all instrumentation was valid and reliable, there is no evidence these tools were previously used in a rural-specific population. The food frequency questionnaire was developed and tested with national samples, which should include representation of rural subjects.20
Glucose and Hemoglobin A1C levels were not drawn since diabetics were excluded from this sample. Inclusion of these measures would strengthen future work, particularly in light of the recent identification of ideal cardiovascular health defined by inclusion of 7 health components, including fasting glucose.37,38
The power calculated for fruit and vegetable intake for this study was .76 given a medium effect size and alpha of .05. Specific variable effect size was unknown prior to this study and thus estimated at .50. Some measures required larger sample sizes to achieve adequate power, (eg, waist measurement by group resulted in d = .34, a small effect size requiring 139 subjects per group in order to project a power of .80).19 Replication of this study with a larger sample size would correct for possible Type II errors on physiologic outcomes.
Multiple RNs provided interventions based on protocols. This approach mirrors the reality of nursing practice. It is possible that some of the lack of significant findings are the result of a Type II error and can be attributed to the lack of fidelity among interventionists.
Intervention programs in rural communities may be affected by informal communication of subjects across intervention groups, thus reducing the impact between groups.39 Familiarity among subjects in rural areas makes designs that feature randomization and adherence to differing protocols between experiential and control groups difficult. Nurses in this study reported anecdotes of those in the SMN+CI group saying they were going to call a friend, who was not assigned a nurse, to let them know about information they were receiving from their nurse. The sharing of information between members of the 2 differing interventions is very likely, given the size of the rural communities and the close-knit nature of the people who live there. Other researchers have speculated cross-contamination of intervention may have adversely affected the ability to clearly show differences between treatment and control outcomes in rural RCT studies.39 While this sharing could be considered an advantage in a community-based intervention, it is a deterrent in a RCT. Crossover effects in rural studies do mirror the reality of practice and research in rural communities.
Implications
The change on Framingham scores from pre to postintervention suggests that both interventions led to reduction in risk for CHD. All women received a cardiovascular screening and were told of their Framingham score, which estimates risk of a CHD event in the next 10 years compared to women in the same age group. They also had a copy of all their screening measurements including weight, waist circumference, BMI, BP, total cholesterol, LDL, and HDL prior to entering the study. Knowing their “numbers” may have been enough information for some women to work on risk reduction whether they worked with the RN in the SMN+CI group or were involved only with the CI. Further work needs to be completed on the premise of whether knowing lab values for cardiac risk markers will motivate women to action. Additional analysis of what factors were present for women who did reduce CVD risks, regardless of group, is warranted.
A design that focuses on intervention fidelity, a larger sample size, and ways of preventing contamination across interventions in small rural areas is needed as a next step. Further work needs to be done among rural women on the most effective means of reducing CVD risks, including anthropometric measures. The nurse intervention was successful in improving subjects’ consumption of fruits and vegetables. Unfortunately, these changes did not translate into a statistical reduction in anthropometric or laboratory values for the SMN+CI group. However, a reduction in the Framingham scores, regardless of group, by an average of 2 points across a study period of 14 months may have clinical as well as statistical significance.
Behavioral changes are needed to reduce modifiable risk of CVD in most populations. Although many are aware of heart healthy behaviors, these lifestyle changes remain either elusive or short-lived for too many people. Rural women and particularly African American rural women are often underrepresented in CVD research, yet their risks are of concern. Clearly more work needs to be done to reduce CVD risks to promote heart health among rural women.
Acknowledgments
This study was funded by the National Institutes of Health, National Institute of Nursing Research, and National Heart Blood and Lung Institute Academic Research Enhancement Award (AREA) 1R15NR009218-01A. The authors would thank the rural women who participated in this study. In addition we would like to acknowledge the assistance of community liaisons Phyllis Highland, MA, Unionville, VA; Mary Hamil Parker, PhD, Alexandria, VA; Vera Buel, BS, Delaware County Public Health Nursing Service; & Dottie Kruppo, Delaware Valley Hospital, Walton, NY. We would like to acknowledge the following RNs for their interventions and assistance in data collection: Mary X. Britten, EdD;1 Maureen Daws, PhDC;1 Alison Dura, MS;1 Theresa N. Grabo, PhD (retired);1 Yvonne Johnston, MPH;1 Irma H. Mahone, PhD;3 Donna Morgan, PhD;1 Mary Ann Nemcek PhD (retired);1 Judy Quaranta, MS;1 Elizabeth Reese, MS (retired);1 Fran Srnka-Debnar, MS;1 and former DSON graduate students Mary Ann Barron, MS, and Elizabeth Austin, PhD. We would like to acknowledge the contribution to the following people for their input into the original concept and design of this study: Geri Britton, PhD;1 Theresa N. Grabo, PhD (retired);1 Gale Spencer, PhD;1 and Elizabeth Merwin, PhD.3 A special acknowledgement goes to the over 50 undergraduate nursing students from the Decker School of Nursing, who assisted with the screenings and data collection in this R15 study. We would like to acknowledge Sedar Atav, PhD;1 and Stephen Samuels, PhD (retired);1 for their assistance with statistical analysis. In addition, we would like to thank Malgosia Krasuska, PhD;1 Lindsay Lake Morgan, PhD (retired);1 Mary Ann Swain, PhD;1 and Steve Wiitala, PhD, for their assistance in manuscript preparation.
Footnotes
The authors have no conflict of interest to report.
References
- 1.Rodger VL, Go AS, Lloyd-Jones DM, et al. Heart Disease and Stroke statistics-2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fahs PS, Kalman M. Matters of the heart: cardiovascular disease and rural nursing. Annu Rev Nurs Res. 2008;26:41–84. [PubMed] [Google Scholar]
- 3.Gamm L, Van Nostrand JF Texas A&M University System. Rural healthy people 2010: a companion document to Healthy people 2010. College Station, TX: Texas A&M University System Health Science Center School of Rural Public Health Southwest Rural Health Research Center; 2003. Southwest Rural Health Research Center, United States. Office of Rural Health Policy. [Google Scholar]
- 4.Swanoski MT, Lutfiyya MN, Amaro ML, Akers MF, Huot KL. Knowledge of Heart Attack and Stroke symptomology: a cross-sectional comparison of rural and non-rural US adults. BMC Public Health. 2012 Apr 10;12(1):283. doi: 10.1186/1471-2458-12-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graves BA. Focused community-based research for eliminating CVD risk disparities in a rural underserved population. Online Journal of Rural Nursing and Health Care. 2012;12(1):67–77. [Google Scholar]
- 6.Harris DE, Hamel L, Aboueissa AM, Johnson D. A cardiovascular disease risk factor screening program designed to reach rural residents of Maine, USA. Rural Remote Health. 2011;11(3):1–15. [PubMed] [Google Scholar]
- 7.Roddy SJ, Walker SN, Larsen J, Lindsey A, Shurmur S, Yates B. CVD risk factors in rural women. Nurse Pract. 2007 Jun;32(6):53–55. doi: 10.1097/01.NPR.0000275357.87192.9e. [DOI] [PubMed] [Google Scholar]
- 8.Hamner J, Wilder B. Knowledge and risk of cardiovascular disease in rural Alabama women. J Am Acad Nurse Pract. 2008 Jun;20(6):333–338. doi: 10.1111/j.1745-7599.2008.00326.x. [DOI] [PubMed] [Google Scholar]
- 9.Colleran KM, Richards A, Shafer K. Disparities in cardiovascular disease risk and treatment: demographic comparison. J Investig Med. 2007 Dec;55(8):415–422. doi: 10.2310/6650.2007.00028. [DOI] [PubMed] [Google Scholar]
- 10.Okrah K, Vaughan-Sarrazin M, Kaboli P, Cram P. Echocardiogram utilization among rural and urban veterans. J Rural Health. 2012;28(2):211–220. doi: 10.1111/j.1748-0361.2011.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muus KJ, Knudson AD, Klug MG, Wynne J. In-hospital mortality among rural Medicare patients with acute Myocardial Infarction: the influence of demographics, transfer, and health factors. J Rural Health. 2011;27(4):394–400. doi: 10.1111/j.1748-0361.2010.00351.x. [DOI] [PubMed] [Google Scholar]
- 12.Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007 Feb 14;297(6):611–619. doi: 10.1001/jama.297.6.611. [DOI] [PubMed] [Google Scholar]
- 13.Villablanca AC, Beckett LA, Li Y, et al. Outcomes of comprehensive heart care programs in high-risk women [corrected] [published erratum appears in J WOMENS HEALTH (15409996) 2010 Sep;19(9):1763] Journal of Women’s Health (15409996) 2010;19(7):1313–1325. doi: 10.1089/jwh.2009.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(4):406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 16.Moos RH. Social-ecological perspectives on health. In: Stone GC, Cohen F, Adler NE, editors. Health Psychology - A Handbook. San Francisco: Jossey-Bass; 1979. pp. 523–547. [Google Scholar]
- 17.Pribulick M, Williams IC, Fahs PS. Strategies to reduce barriers in study recruitment and participation among rural women. Online Journal of Rural Nursing and Health Care. 2010;10(1):22–33. [PMC free article] [PubMed] [Google Scholar]
- 18.Rural Assistance Center. [Accessed January 18, 2010];What is rural? Available at: http://ww.raconline.org.
- 19.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: L. Erlbaum Associates; 1988. [Google Scholar]
- 20.Thompson FE, Kipnis V, Subar AF, et al. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am J Clin Nutr. 2000 Jun 1;71(6):1503–1510. doi: 10.1093/ajcn/71.6.1503. [DOI] [PubMed] [Google Scholar]
- 21.Dipietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Med Sci Sports Exerc. 1993 May;25(5):628–642. [PubMed] [Google Scholar]
- 22.University of Rhode Island. [Accessed 2005];Cancer pervention research center measures. [Web page] Available at: http://www.uri.edu/research/cprc/measures.html.
- 23.Thompson FE, Midthune D, Subar AF, Kahle LL, Schatzkin A, Kipnis V. Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage energy from fat and fibre. Public Health Nutrition. 2004;7(08):1097–1106. doi: 10.1079/PHN2004642. [DOI] [PubMed] [Google Scholar]
- 24.Dietary Guidelines Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2005. United States Health and Human Services United States Department of Agriculture; 2005. [Google Scholar]
- 25.Young DR, Jee SH, Appel LJ. A comparison of the Yale Physical Activity Survey with other physical activity measures. Med Sci Sports Exerc. 2001 Jun;33(6):955–961. doi: 10.1097/00005768-200106000-00015. [DOI] [PubMed] [Google Scholar]
- 26.O’Toole ML, Sawicki MA, Artal R. Structured diet and physical activity prevent postpartum weight retention. J Womens Health (Larchmt) 2003 Dec;12(10):991–998. doi: 10.1089/154099903322643910. [DOI] [PubMed] [Google Scholar]
- 27.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998 May 12;97(18):1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 28.Lenfant C, Chobanian AV, Jones DW, Roccella EJ. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003 Jun;41(6):1178–1179. doi: 10.1161/01.HYP.0000075790.33892.AE. [DOI] [PubMed] [Google Scholar]
- 29.Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. The Lancet. 2010;375(9716):735–742. doi: 10.1016/S0140-6736(09)61965-6. [DOI] [PubMed] [Google Scholar]
- 30.Culver AL, Ockene IS, Balasubramanian R, et al. Statin use and risk of Diabetes Mellitus in postmenopausal women in the Women’s Health Initiative. Arch Intern Med. 2012;172(2):144–152. doi: 10.1001/archinternmed.2011.625. [DOI] [PubMed] [Google Scholar]
- 31.National Heart Lung and Blood Institute, National Institutes of Health. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel III) manuscript version. [Accessed January 06, 2006];Internet Resource; Computer File Date of Entry: 20011107. Available at: http://purl.access.gpo.gov/GPO/LPS15712.
- 32.Folta SC, Lichtenstein AH, Seguin RA, Goldberg JP, Kuder JF, Nelson ME. The Strong Women-Healthy Hearts program: reducing cardiovascular disease risk factors in rural sedentary, overweight, and obese midlife and older women. Am J Public Health. 2009 Jul;99(7):1271–1277. doi: 10.2105/AJPH.2008.145581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perry CK, Rosenfeld AG, Bennett JA, Potempa K. Heart-to-Heart: promoting walking in rural women through motivational interviewing and group support. J Cardiovasc Nurs. 2007 Jul-Aug;22(4):304–312. doi: 10.1097/01.JCN.0000278953.67630.e3. [DOI] [PubMed] [Google Scholar]
- 34.Pullen C, Noble Walker S. Midlife and older rural women’s adherence to U.S. Dietary Guidelines across stages of change in healthy eating. Public Health Nurs. 2002 May-Jun;19(3):170–178. doi: 10.1046/j.0737-1209.2002.19304.x. [DOI] [PubMed] [Google Scholar]
- 35.Ahluwalia JS, Nollen N, Kaur H, James AS, Mayo MS, Resnicow K. Pathway to health: cluster-randomized trial to increase fruit and vegetable consumption among smokers in public housing. Health Psychol. 2007 Mar;26(2):214–221. doi: 10.1037/0278-6133.26.2.214. [DOI] [PubMed] [Google Scholar]
- 36.Riebe D, Blissmer B, Greene G, et al. Long-term maintenance of exercise and healthy eating behaviors in overweight adults. Preventive medicine. 2005;40(6):769–778. doi: 10.1016/j.ypmed.2004.09.023. [DOI] [PubMed] [Google Scholar]
- 37.Shay CM, Ning H, Allen NB, et al. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012 Jan 3;125(1):45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women-2011 update: a guideline from the American Heart Association. Circulation. 2011 Mar 22;123(11):1243–1262. doi: 10.1161/CIR.0b013e31820faaf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bullock L, Everett KD, Mullen PD, Geden E, Longo DR, Madsen R. Baby BEEP: A randomized controlled trial of nurses’ individualized social support for poor rural pregnant smokers. Matern Child Health J. 2009 May;13(3):395–406. doi: 10.1007/s10995-008-0363-z. [DOI] [PubMed] [Google Scholar]