Abstract
Nonmedical factors and diagnostic certainty contribute to variation in clinical decision making, but the process by which this occurs remains unclear. We examine how physicians’ interpretations of patient sex/gender affect diagnostic certainty and, in turn, decision making for coronary heart disease (CHD). Data are from a factorial experiment of 256 physicians who viewed one of 16 video vignettes with different patient-actors presenting the same CHD symptoms. Physician participants completed a structured interview and provided a narrative about their decision-making processes. Quantitative analysis showed that diagnostic uncertainty reduces the likelihood that physicians will order tests and medications appropriate for an urgent cardiac condition in particular. Qualitative analysis revealed that a subset of physicians applied knowledge that women have “atypical symptoms” as a generalization, which engendered uncertainty for some. Findings are discussed in relation to social-psychological processes that underlie clinical decision making and the social framing of medical knowledge.
Health care disparities result from a complex intersection of individual and systemic factors, one of which is variation in physicians’ decision making (Fincher et al. 2004; McKinlay 1996; Smedley, Stith, and Nelson 2003). Substantial research shows that physicians’ decisions vary by patient and physician characteristics, organizational setting and features of health care systems (Adams et al. 2008; LaVeist et al. 2003; McKinlay et al. 2007; Shackelton et al. 2009; van Ryn and Fu 2003; von dem Knesebeck et al. 2008) as well as level of diagnostic uncertainty (Balsa et al. 2003; Lutfey et al. 2009a). Yet, the processes by which these nonmedical factors intersect with uncertainty and impact physicians’ decisions remain poorly understood. This paper examines how physician interpretation of patient sex/gender—i.e., the “entanglement” (Springer, Mager Stellman, and Jordan-Young 2011) of biological sex with social patterns of gender—influences diagnostic certainty and, in turn, creates variation in treatment decisions for coronary heart disease (CHD).
Disparities in cardiac treatments between men and women have been reduced but not eliminated. Recent research shows that women are less likely than men to receive a range of CHD medications and procedures (Bell and Nappi 2000; Correa-de-Araujo et al. 2006; Galvao et al. 2006; Gold and Krumholz 2006; Shaw et al. 2008). Women fare worse than men on quality indicators for care of cardiovascular disease despite similar insurance coverage (Bird et al. 2007; Chou et al. 2007). Sex/gender disparities are most pronounced for younger women, although slight differences persist for older women as well (Gan et al. 2000; Gold and Krumholz 2006). We focus on clinical decision making as a potential contributor to remaining sex/gender differences in CHD care.
BACKGROUND
Sex/Gender Differences in Social Context
Since the1980s, medical researchers have made a concerted effort to incorporate women’s experiences into the medical knowledge base by examining biological differences (Epstein 2007). The 2001 Institute of Medicine report Exploring the Biological Contributions to Human Health: Does Sex Matter? concludes that sex-based differences in genetics and physiology extend beyond the reproductive system and calls for a systematic study of biological differences (Wizemann and Pardue 2001). Subsequent research has investigated female-specific health patterns, including for cardiovascular disease (Epstein 2007; Mieres et al. 2011; Mosca et al. 2004).
Early medical knowledge of CHD symptomology resulted primarily from studies with men (Springer et al. 2011). As an example of a portrayal of typical symptoms, a current widely-used atlas of cardiology (Runge and Ohman 2004) illustrates the manifestation of angina with a picture of a grey-haired Caucasian man clutching his chest while leaving a restaurant. The effort to incorporate women in the knowledge base yielded the belief that women more often than men have “atypical symptoms” (Charney 2002; Lefler and Bondy 2004; McSweeney, Lefler, and Crowder 2005; O’Keefe-McCarthy 2008; Patel, Rosengren, and Ekman 2004), which contributes to the context in which a physician interprets symptoms and makes clinical decisions.
Medical knowledge about sex/gender differences in CHD and health generally joins a broad array of beliefs, roles, expectations, and norms (i.e., gender) that are “entangled” (Springer et al. 2011) with biological characteristics (i.e., sex). Sex/gender is pervasive in social interactions and provides a significant source of information about what to expect from others. As such, it is not surprising that sex/gender impacts communication between patients and providers (DiMatteo, Murray, and Williams 2009; Mast 2007; Street 2002) and clinical decisions (Di Caccavo and Reid 1998). For example, an experiment that held constant patient communication and symptom presentation showed that physicians’ diagnostic and management decisions for the same CHD symptoms differed by patient sex/gender (Adams et al. 2008; Arber et al. 2006).
Role of diagnostic certainty
Uncertainty is a common feature of clinical decision making (Beresford 1991) and an important factor for understanding disparities that arise from the clinical encounter (Smedley et al. 2003). For the case of CHD, previous research has identified a relationship between patient sex/gender, diagnostic certainty, and treatment decisions. Physicians are less certain about a CHD diagnosis for women patients than for men (Bonte et al. 2008; (Lutfey et al. 2010; Lutfey and McKinlay 2009; Maserejian, Lutfey, and McKinlay 2009b), and this lower certainty is more common for middle-aged than older women patients (Arber et al. 2006; Lutfey et al. 2009a; Maserejian et al. 2009a). Moreover, physicians with lower levels of diagnostic certainty are less likely to prescribe a CHD medication or test (Lutfey et al. 2009a; Lutfey et al. 2009b).
These results suggest a pathway: a physician’s view of patient sex/gender affects diagnostic certainty (Figure 1, boxes A and C), which in turn affects management of CHD (Figure 1, boxes C and D).1 Our first aim is to further specify the way in which certainty affects management of CHD by (i) distinguishing CHD tests and medications appropriate for more and less urgent cardiac situations and (ii) testing whether the effect of certainty differs for men and women patients.
Figure 1.
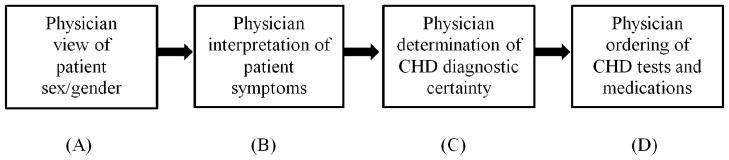
Pathway from a physician’s observation of patient sex/gender to management of coronary heart disease (CHD)
Mechanisms by which sex/gender can impact physicians’ decisions
Our second aim is to identify a mechanism by which physicians’ interpretations of patient sex/gender influences diagnostic certainty for CHD (Figure 1, box B). Research has identified three mechanisms by which a patient characteristic might enter into clinical decision making: statistical discrimination, stereotyping, and prejudice (Burgess et al. 2006; Smedley et al. 2003; van Ryn and Fu 2003).
In a clinical setting, statistical discrimination refers to the application of rules of conditional probability to determine a diagnosis. Under conditions of uncertainty, probabilistic decision making is a rational strategy (Balsa, McGuire, and Meredith 2005; Smedley et al. 2003). The Bayesian model of clinical decision making calls for physicians to determine the probability that a patient has a condition by weighing (i) the probability that a symptom will be observed given that the condition is present, (ii) prior knowledge about the probability of the condition being present in the population, and (iii) the probability that the symptom is observed in an individual patient.
Statistical discrimination can lead to disparities in clinical decision making in two ways (Balsa and McGuire 2001; Balsa et al. 2005; Ketcham et al. 2009; Maserejian et al. 2009b; Smedley et al. 2003). The prevalence hypothesis suggests that, lacking a clear diagnosis with high certainty, a physician may rely more heavily on prior knowledge about the probability of the condition being present in the population or group. This may lead to a poor match between patient needs and care provided due to underweighting patient-specific information, incorrectly recalling population-based prevalence rates, or using inaccurate prevalence rates (Lutfey et al. 2010; McKinlay 1996). The miscommunication hypothesis suggests that a physician may have trouble understanding a patient’s symptoms due to communication barriers and, therefore, rely more heavily on population-based prevalence rates with the same potential of a poor match between needs and treatments.
For CHD, a video vignette experiment has addressed the prevalence and miscommunication hypotheses (Maserejian et al. 2009b). The experimental design held constant patient presentation of symptoms (including verbal and nonverbal signals), thereby controlling for the miscommunication hypothesis; yet, differences in CHD certainty and treatments by patient sex/gender remained. A statistical test showed that respondents were not relying on population-based rates of CHD prevalence among men and women to determine diagnostic certainty, bringing evidence against the prevalence hypothesis.
A second potential mechanism is stereotyping, or the application of generalizations based on group membership. Stereotyping arises from the widespread practice of social categorization (Smedley et al. 2003) and is a “highly adaptive cognitive strategy” (van Ryn and Fu 2003) for quickly making sense of information, particularly when individualized information is lacking or under conditions of fatigue, anxiety, or time constraints (Burgess et al. 2006; Muroff et al. 2007).
The efficiency gained by utilizing group-based generalizations is counterbalanced by the risk of disregarding individualized information. Categorization tends to amplify differences between groups while minimizing within-group differences (Smedley et al. 2003), and people tend to interpret and remember information in ways that are consistent with their beliefs about a group (Smedley et al. 2003). In a clinical setting, the need to make decisions quickly without full information creates a situation in which physicians may apply generalized knowledge about women or men to aid in clinical decisions. To our knowledge, no prior studies have examined whether using group-based generalizations contributes to persistent sex/gender disparities in CHD treatments.
A third potential mechanism is prejudice--or a negative, unfounded bias based on social group membership (Dovidio et al.1996). Although the Institute of Medicine report Unequal Treatment: Confronting Racial and Ethnic Disparities did not find substantial evidence of physicians exhibiting overt prejudice, the authors acknowledge that prejudice can be implicit and subtle (Balsa et al. 2005; Smedley et al. 2003), making it difficult to observe and measure. Although we know of no evidence that prejudice contributes to sex/gender disparities in CHD treatments, it remains a potential mechanism.
Stereotyping and prejudice may occur purposefully or operate in the background of cognitive processing. For CHD, a previous analysis of the dataset we use revealed that physicians consciously consider heart disease for both women and men but are more likely to discount a cardiac diagnosis for women (Lutfey et al. 2010). We extend the effort to understand why physicians are less certain of a CHD diagnosis for women patients by further examining the mechanism by which physicians’ interpretations of patient sex/gender affect diagnostic certainty.
DATA AND METHODS
To address the two aims of the study, we used a mixed method vignette-based experimental design. We conducted statistical analyses to further specify the way that certainty affects management of CHD. Based on these and previously reported statistical results from our dataset, we utilized qualitative methods to investigate in an open-ended manner how physicians incorporate patient sex/gender (whether via prevalence rates, stereotypes, and/or prejudice) into their determination of diagnostic certainty.
Research design and data
Data are from a video vignette factorial experiment that isolated the effects of seven design factors on physician management of CHD: four patient characteristics (age, sex/gender, race, socioeconomic status), two physician attributes (sex/gender, years of clinical experience), and cognitive priming. Due to the balanced experimental design, the effects of the design factors are independent, thereby circumventing the common problem of confounding. The video vignettes hold constant symptom presentation and communication style. Detailed descriptions of the study have been reported previously (Lutfey et al. 2010; Lutfey and McKinlay 2009).
In brief, 16 video vignettes represented all combinations (24) of patient age (55/75), sex/gender, race (black/white), and socioeconomic status (higher/lower). In each vignette, patient-actors presented with the same CHD signs and symptoms: chest pain that worsens with exertion and is relieved with rest, pain between the shoulder blades, elevated blood pressure, and stress. Since patients do not typically present as textbook cases, the vignette included symptoms that could suggest a gastrointestinal diagnosis and mood-related symptoms. The professional actors in each vignette were rehearsed to use the same words and gestures.
Primary care physicians were recruited to evenly fill four cells stratified by sex/gender and more/less clinical experience (≥22 or ≤12 years). We completed 256 interviews (16 vignettes x four physician cells x two priming conditions x two replications) in 2006–07. Two interviewers conducted all interviews in person and were present throughout study activities. Interviewer training included medical vocabulary, pilot interviews, and quality control sessions.
After viewing a vignette, each participant identified diagnoses being considered, assigned a certainty for each diagnosis on a scale of 0–100, and formulated a management plan (including tests and medications). This information was coded and analyzed quantitatively.
Physicians then participated in an open-ended “think aloud” interview during which they were asked to explain how they developed their differential diagnoses and treatment plan as well as how this related to diagnostic certainty. Interviewers did not ask respondents to comment on sex/gender, rendering any sex/gender-related information respondent-initiated. The think-aloud narratives were audio-taped and transcribed verbatim.
The study was approved by New England Research Institutes’ Institutional Review Board, and all participants signed an informed consent form. Each participant received an honorarium ($200).
Analytic strategy
Quantitative analyses utilized the full sample (N=256). We used multivariate logistic modeling to predict the likelihood of physicians’ ordering a CHD test or medication when all design variables were included without physician certainty (Model 1) and then with all design variables plus physician certainty (Model 2). An interaction term for patient sex/gender and CHD certainty was also included initially; because the effect was not significant, the interaction term was not retained in the final model.2 Odds ratios were calculated for a 10-point change in CHD certainty on a scale of 0–100.
The dependent variable, CHD-appropriate tests and medications, was grouped according to whether the tests and medications were appropriate for situations in which a physician had a sense of urgency about a cardiac condition. Based on the input of a clinical consultant, urgent tests included cardiac enzymes, cardiac stress test, echocardiogram, and EKG/ECG; non-urgent tests included cardiac risk profile, fasting lipid profile, and tests coded as “other.” Urgent medications included aspirin or other anti-platelet agent, beta-blocker, and nitrate/vasodilator; non-urgent medications were calcium channel blocker, diuretic, lipid-lowering agent, and medications coded as “other.” A third group, “tests only,” represented decisions to order CHD tests but no medications.
Given the balanced experimental design, the effects of design factors (patient characteristics, physician attributes, and priming status) are orthogonal and independent in models that do not include physician certainty. As expected, no significant differences were observed between unadjusted and adjusted models that did not include physician certainty. In the models that include physician certainty, we fit both the unadjusted and adjusted models, and none of the estimates changed substantially. As a result, we present only the adjusted models for clarity.
We do not present results for design variables other than patient sex/gender because the effects of all design variables are reported elsewhere (Lutfey et al. 2010) and we limit this analysis to explaining how physicians’ interpretations of patient sex/gender influence clinical decision making in relation to diagnostic certainty.
Qualitative analysis of the think-aloud narratives utilized one full replication (N=128) to maintain balance across the seven experimental design factors. Since the qualitative data was in the form of physician narratives, we coded each transcript as a “diagnostic story” using narrative analysis (Kohler Riessman 2008). As such, coding identified the important elements raised in the story, the order the elements were raised, and how story elements impacted reported actions.
Open codes included type of introduction; the order in which possible diagnoses were raised; factors affecting decisions; decision-making processes indicated through the narrative; any influence of available resources on decision making; treatment approach; any sense of urgency, uncertainty, and/or anxiety; social support or spousal influence; mention of disease rates; biological descriptors; and reference to atypical symptom presentations (including descriptions of symptoms being “atypical,” “vague,” or “nonspecific” as respondents often used these terms together). Within each of these categories, detailed codes were developed to reflect differences in the way physicians worked through the diagnosis and decided on treatment.
Respondent descriptions of relying more heavily on population-based prevalence rates of CHD among men and women than on patient-specific information or of using inaccurate prevalence rates would provide evidence for statistical discrimination via the prevalence hypothesis. The use of video vignettes controlled for the miscommunication hypothesis by ensuring that the language and gestures of all patient-actors were the same. Descriptions of applying generalized knowledge of women or men as a group in order to interpret an individual patient’s symptoms would provide evidence for the use of a stereotype, and descriptions of negative, unfounded bias against men or women would indicate prejudice.
Two coders were used to interpret physicians’ references to the origin of mood-related symptoms and the role of the vignette patient’s spouse as respondents often addressed these topics in a less straightforward manner; coding discrepancies were resolved through discussion until consensus was reached. Other coding was completed by a single coder to ensure consistency, and the first two authors met regularly to discuss coding and analysis.
Analysis examined differences in physicians’ narratives for women and men patients and how themes varied according to age within sex/gender groups. Analysis began by noting differences in the frequency of codes between sex/gender groups by age in order to identify categories of interest. Detailed analysis of the quotations within these categories yielded emergent themes across transcripts in each group.
RESULTS
Diagnostic certainty affects physician ordering of “urgent” cardiac treatments
Multivariate logistic modeling to examine the effect of patient sex/gender on physician ordering of CHD medications and tests appropriate for urgent and non-urgent cardiac situations followed two steps (Table 1). Model 1 included patient sex/gender and the other design variables without physician certainty; in this model, physicians appeared to be less likely to order an urgent medication (OR 0.57, p=0.035) or urgent test (OR 0.21, p=0.059) for women patients than men patients. Yet, when certainty was added (Model 2), the odds ratio coefficients for an effect of patient sex/gender on these outcomes moved closer to 1 (i.e., became less important) and were no longer statistically significant.
Table 1.
Adjusted effectsa of patient sex/gender and physician certainty on ordering CHD medications and tests
| Medications | Tests only (no medications) | Testsb Urgent |
||
|---|---|---|---|---|
| Urgent | Not urgent | |||
| Model 1: all design variables without physician certainty | ||||
| Patient sex/gender (woman) | ||||
| Odds ratio | .57 | 2.42 | 1.53 | .21 |
| (CI)c | (.34, .96) | (.71, 8.27) | (.91, 2.58) | (.04, 1.06) |
| P-value | .035 | .16 | .11 | .059 |
| Model 2: all design variables with physician certainty | ||||
| Patient sex/gender (woman) | ||||
| Odds ratio | .73 | 2.39 | 1.26 | .37 |
| (CI) | (.42, 1.28) | (.69, 8.29) | (.73, 2.17) | (.07, 2.08) |
| P-value | .27 | .17 | .41 | .26 |
| Physician certaintyd | ||||
| Odds ratio | 1.41 | .98 | .79 | 1.57 |
| (CI) | (1.23, 1.62) | (.76, 1.26) | (.69, .91) | (1.13, 2.18) |
| P-value | <.001 | .88 | <.001 | .008 |
|
| ||||
| Test for interaction: patient gender x physician certainty | ||||
| P-value | .97 | .63 | .47 | .73 |
Notes:
Results shown are adjusted for all design variables, including patient characteristics (age, race, SES), provider attributes (sex/gender, experience), and priming status.
Results for non-urgent tests are not reported due to small cell size (n=4).
CI = odds ratio confidence interval
Odds ratios and confidence intervals for physician certainty reflect a 10-point increase in certainty on a scale of 0–100. Inverse odds ratios are available upon request.
These results show that the apparent direct effect of patient sex/gender on physician management of CHD disappeared and physician certainty became the driver for predicting the likelihood that physicians would order CHD-appropriate tests and medications. Specifically, a 10-point increase in certainty led to an approximate 41% increase in the likelihood of ordering an urgent medication, a 57% increase in the likelihood of ordering an urgent test, and a 21% decrease in the likelihood of ordering a test without a medication. Inverting the odds ratios, lower physician certainty decreased the likelihood of ordering CHD medications and tests appropriate for a situation perceived as urgent and increased the likelihood of ordering a test without an accompanying medication.
In addition, the lack of a significant interaction between patient sex/gender and physician certainty showed that the effect of an established level of certainty on ordering CHD tests and medications (Figure 1, boxes C and D) did not differ for women and men patients. Taken together with previously published quantitative results from this same dataset showing that a physician’s interpretation of patient sex/gender reduced diagnostic certainty (Lutfey et al. 2010; Lutfey and McKinlay 2009; Maserejian et al. 2009b), the cumulative evidence from our dataset provides empirical grounding for the qualitative analysis to focus on how physicians’ views of sex/gender intersect with diagnostic certainty rather than directly influencing ordering.
Qualitative findings reveal that physicians were concerned about women with cardiac disease, but the belief that women have “atypical symptoms” was a double-edged sword for certainty.
Physicians are as concerned about cardiac disease for women as for men
In their qualitative narratives, physicians spoke of a similar, if not slightly higher, level of concern about CHD for women as for men. This concern was communicated both in the order of possible diagnoses raised and in descriptions of decision-making processes. Physicians raised a cardiac-related condition within the first three possible diagnoses for 95% (61/64) of men patients and 100% of women patients. In addition, about half of respondents described their decision-making process as attempting to “rule out” the most life threatening possibility, and this was most common for middle-aged women patients (60%) and least common for elderly men (47%). Similarly, physicians who spoke of focusing on cardiac disease first because of the high risk of that diagnosis more often were diagnosing women patients than men (55% vs. 38%, respectively), and this view was most common among physicians interpreting symptoms presented by middle-aged women patients (63%).
A physician diagnosing a middle-aged woman provided a typical explanation of the level of concern:
I have to consider coronary artery disease, and of course that’s the most important of all of these diagnoses, so that goes to the top of my list. So, she can die of coronary artery, but these other things, she’s not going to die of probably. So, my first goal is to diagnose or not diagnose coronary artery disease.
-man physician, more experience
Given that physicians voiced this concern slightly more often for women patients than for men, why is it that women were less likely than men to receive CHD treatments appropriate for urgent cardiac situations?
Physicians view male sex/gender as a “risk factor” but at times interpret women’s symptoms as “atypical”
A similar number of respondents diagnosing both men and women included sex and/or gender in their narratives (47% and 53%, respectively); however, the meaning that physicians attached to sex/gender differed for men and women patients. Among men patients, physicians commonly mentioned sex/gender and age as significant CHD risk factors. For example, a physician who viewed the vignette of an elderly man patient said the following factors impacted her certainty level: “Age, sex, …also the fact that he doesn’t call this a pain but a discomfort; however, it’s worrying him” (woman physician, more experience). For middle-aged men, physicians typically took note of age and sex/gender and looked for additional risk factors to strengthen the case for CHD. A physician diagnosing a middle-aged man offered a typical explanation:
The first thing I did was assess his risk factors for cardiac disease when he was describing indigestion… He’s a 55-year-old male which makes him already with one risk factor. When the doctor also mentioned that he was hypertensive, that gave me a second risk factor. When he gave the history that his wife says he hasn’t been taking care of himself and he hasn’t a [regular] doctor, that gave me an unknown lipid status. So, he had multiple cardiac risk factors from the beginning.
-woman physician, less experience
Two ways in which physicians structured their diagnostic stories demonstrated the importance they gave to sex/gender as a risk factor for men patients. First, compared to those diagnosing women patients, respondents diagnosing men patients—especially elderly men--more often began their diagnostic narratives by listing patient characteristics, particularly sex/gender and age. Typical of introductions of this type was: “A 75-year-old male with a new onset of worrisome discomfort in his chest--certainly, risk factors for ischemic disease include his age, male gender, [and] elevated blood pressure” (man physician, less experience).
Second, among the decision-making processes described by physicians, interpreting symptoms in the context of risk factors was used most often for elderly men and least often for middle-aged women (41% vs. 22%, respectively). Typical descriptions of the decision-making process for a man patient were:
I think epidemiology when I think about heart disease. …If you have a 75-year-old male that’s hypertensive and he has anything happening … below his chin, …for him to have a cardiac event in the next ten years is pretty high.
-man physician, more experience
This is a 70-year-old man, so his age is that he’s at cardiac risk factor already. That he’s obese…is another set up for coronary artery disease. Doesn’t seem that he was a man who had a healthy lifestyle. And symptoms are pretty typical--triggered by a large meal and stress.
-woman physician, more experience
For women patients, an elderly age was often raised as a risk factor for CHD, but some physicians’ views of a woman’s sex/gender led to interpreting the symptoms presented as “atypical.” For example, a physician who viewed an elderly woman patient said, “Well, based on her age—that always puts her at higher risk for cardiac disease. And, I know that sometimes women will just have stomach sensations instead of chest pressure” (man physician, less experience). Similarly, another physician said, “Well, her age. A woman at age 70--they could present atypically so the fact that her symptoms aren’t a typical angina, it doesn’t mean it isn’t” (man physician, more experience). Physicians spoke of age as a decision-making factor as often for elderly women as for middle-aged men (56% and 53%, respectively), making sex/gender the factor that introduced a different interpretation of symptoms.
For middle-aged women patients, sex/gender took on even more salience for physicians’ interpretations. Age was viewed inconsistently as physicians associated it both with a higher likelihood of cardiac disease (at times due to menopausal status) and with a lower likelihood. Yet, physicians’ interpretation of symptoms as “atypical,” “nonspecific,” or “vague” was even more common when a woman patient was middle-aged. Of the 30 physicians who described atypical symptoms or presentations, 25 were interpreting the symptoms of women patients, and 17 of those were diagnosing middle-aged women. For example, a woman physician with more experience described the “precipitating factors and the actual global presentation” of a middle-aged woman as “an atypical presentation but consistent with female ischemic coronary disease.” Similarly, another physician said:
Well, she was having, her location of pain was kind of vague between upper abdomen and lower chest, and her symptoms were very vague, so that made me suspicious for heart diseases, especially because she’s a woman and they don’t get always the typical heart symptoms.
- woman physician, less experience
In contrast, among physicians who used the words “typical” or “classic” to describe the patient’s symptoms in relation to cardiac disease, seven of eight were referring to men patients.
In short, physicians interpreted the same symptom presentation differently for men and women patients. As part of the experimental design, both women and men actor-patients followed the same script and were rehearsed to use the same gestures; however, for a subset of physicians, the same words and gestures carried a different meaning when presented by a woman.
This subset of physicians invoked group-based knowledge that women are more likely to have atypical symptoms for cardiac disease and applied that knowledge as a generalization (i.e., as a stereotype). For example, a physician explained her diagnostic process for an elderly woman in this way:
A lot of women are very nonspecific and vague, which is the difference of why you have to pay attention to their details as opposed to men because cardiovascular risk is the biggest cause of death in women and is usually with vague symptoms that they complain about. So, once she stated that it was different from her usual reflux that made me think, “Number one, okay, well what about cardiac?” … With her [pain] going to her back, sometimes women will have pain that goes to their back.
-woman physician, less experience
The physician began with a general statement about women’s presentation of cardiac symptoms and used that as a backdrop for interpreting the specific symptoms of the patient at hand.
Other physicians began with the specific patient’s history, and the general statement about women’s presentation was used to make sense of the patient’s symptoms. As a physician diagnosing a middle-aged woman said:
My main concern with this patient was for coronary artery disease. She did have a history of what appeared to be heartburn, but now it’s having an unusual character. And, based on the fact that she’s been having mood swings, …she’s probably menopausal, this could be a presentation of coronary artery disease which is probably slightly atypical but typical for a postmenopausal or perimenopausal female.
-woman physician, less experience
Similarly, another physician explained: “She’s a black female with not absolutely typical chest pain, but women don’t have typical chest pain” (woman physician, more experience).
As these excerpts illustrate, applying knowledge that women experience atypical symptoms for CHD in a generalized way was used as context for diagnosing a particular patient, especially a middle-aged woman. Even though the experimental design held constant patient presentation, about two of every five physicians viewing women patients (25/64) invoked the notion of atypical symptoms, and this shaped how they interpreted the symptoms presented.
The double-edged sword of “atypical symptoms”
Utilizing knowledge of atypical symptoms as a generalization to aid in diagnosing women patients proved to be a double-edged sword. For some physicians, interpreting women’s symptoms in the context of “atypical symptoms” served as a catalyst to look for cardiac disease. A physician diagnosing a middle-aged woman provided an explanation common for this group:
In a woman, unfortunately, one of the problems you get, too, with women are they are more likely to have somewhat complex or symptom complexes that are not, that can be somewhat tricky. And, I don’t want to miss this. So, that would be crucial that we looked at that in a pretty aggressive fashion.
-man physician, more experience
For others, the generalized belief that women’s CHD symptoms are atypical engendered sufficient uncertainty to justify including other possibilities in their treatment strategies or even moving away from cardiac disease. For example, a physician diagnosing a middle-aged woman said that he “was thinking cardiac initially given her age and that she’s female she could have atypical chest pain” but later broadened his treatment plan. He explained, “Because I think in the vignette she was very vague about some things and she was equivocal on a lot of direct questions, [and] that kind of broadens my net as opposed to narrowing my scope of what I’m looking for” (man physician, less experience).
Similarly, another physician began the diagnostic narrative with CHD being the “highest priority” due to chest pain with apparent shortness of breath and relieved by rest; however, this same physician ended his narrative by saying, “Well, as I was saying, atypical chest pain—that means possibly not cardiac, and so GERD would fall under that” (man physician, less experience). Although symptom presentation was the same across vignettes, physicians decided to attend to cardiac issues as the first or only treatment strategy less often for middle-aged women than other patients (13% vs. 25% for middle-aged men, 31% for elderly men, 32% for elderly women).
Even for elderly women, the diagnostic clarity afforded by an older age did not always overcome the uncertainty that accompanied an interpretation of symptoms as atypical. For example, a physician who viewed an elderly woman explained that the cardiac diagnosis was the most serious but that several other potential diagnoses required attention as well.
So, risk factors for her would be her age, postmenopausal female, high blood pressure … So, I would be going with atypical chest pain wanting to rule out the more serious…diagnosis first—ischemic heart disease—but also ruling out worsening reflux disease, possibility of gallbladder disease, …other electrolyte abnormalities, or even thyroid disease as well as anxiety or depression symptoms, which seem to be concomitant at this time.
-woman physician, less experience
In this way, symptoms that were interpreted as atypical appeared both to put CHD “on the list” and to require that a range of alternate diagnoses be pursued simultaneously.
Interpreting symptoms as atypical also led a subset of physicians away from cardiac treatments. For example, a physician viewing an elderly woman said:
Initially, I was thinking about coronary disease because of the importance of missing that diagnosis, even though the symptoms were a little vague… So, with the referred pain to the back, I felt that was much less important now, that being coronary disease, so then I would pursue the gallbladder disease evaluation from that point but in a fairly urgent manner such as to get confirmatory tests that day or the next day, that being a gallbladder ultrasound.
- man physician, more experience
Interpreting symptoms as vague presented a difficult decision about how to proceed with testing, and the physician’s perceived need to confirm or rule out a GI diagnosis within 24 hours suggested that he remained uncertain about whether to pursue the cardiac or GI diagnosis.
The gap between considering cardiac disease and deciding to pursue other diagnoses appeared to be related to the effect that interpreting symptoms as atypical had on a physician’s level of certainty. Among physicians who addressed how their treatment plans were related to their diagnostic certainty, those diagnosing women more often described their strategy as “exploratory” compared to those viewing men (47% vs. 39%, respectively) and less often spoke of “confirming” a diagnosis for which they were certain (16% vs. 45%, respectively). A physician viewing a middle-aged woman patient illustrated the connection in this way: “I think at this point it’s more exploratory just the fact that, as I said, females tend to have more of an atypical presentation for angina and underlying coronary artery disease” (man physician, less experience).
Another physician diagnosing a middle-aged woman described a “high suspicion” of cardiac disease but also a high level of uncertainty:
Well, number one, I don’t have a final conclusion by any means or stretch [of the] imagination. The beginning of her anamnesis is she indicated…chest symptoms, which were rather nonspecific but very important, and therefore she is a high suspicion of having some cardiac condition. …In this case, we are dealing with a totally incomplete clinical evaluation… without having really any evidence to support anything at all…
-man physician, more experience
For this physician, interpretating symptoms as nonspecific coupled with a lack of test results meant that “all treatment is…of little importance until we reach more secure diagnosis.” Conclusions such as these stood in contrast to the narratives of risk factors leading to cardiac tests and treatments that were typical of physicians viewing men patients. 3
DISCUSSION
This analysis utilized mixed methods to further specify a pathway suggested by prior research: physicians’ views of patient sex/gender shapes their interpretation of symptoms and affects diagnostic certainty, which in turn affects management of CHD. The quantitative results extend knowledge about how certainty affects CHD management by showing that lower diagnostic certainty reduces the likelihood of a physician ordering CHD medications and tests appropriate for urgent situations while increasing the likelihood of ordering a test without an accompanying medication. Physicians were not ignoring the possibility of CHD for women patients; rather, those with lower diagnostic certainty were more conservative in their treatment approach. This opens the possibility for delayed care or poorer outcomes for women who present with the same CHD symptoms as men.
Qualitative analysis revealed that applying knowledge that women have atypical symptoms as a generalization was a mechanism by which a physician’s interpretation of patient sex/gender influences diagnostic certainty. Physicians who invoked knowledge of atypical symptoms did not speak of giving more weight to population-based prevalence rates of CHD among men and women than to patient-specific information or of using inaccurate prevalence rates. This negative finding supported previous quantitative results that statistical discrimination via the prevalence hypothesis was not a mechanism behind the persistent sex/gender disparity in CHD treatments (Maserejian et al. 2009b). Physician narratives also did not provide evidence of prejudice against women patients; in fact, physicians voiced concern about CHD slightly more often for women than for men patients.
Instead, physicians who invoked the notion of atypical symptoms spoke in general terms about “atypical” symptoms being “typical” for women or that women as a group do not always present with typical symptoms. These physicians were using knowledge of atypical symptoms as a goal-modified stereotype (Burgess et al. 2006). That is, physicians consciously applied their knowledge that women have atypical symptoms for CHD with the goal of enhancing comprehension, and this influenced their interpretation of the symptoms.
This finding underscores that symptoms are not static stimuli but rather are actively interpreted by a provider. Given that vignette patient-actors of both sex/gender groups presented symptoms with the same verbal and nonverbal signals, the differential interpretation of symptoms for women and men patients was constructed by the physician in an attempt to make sense of patient-specific information. This result provides an additional case of the active construction of biological differences (Fausto-Sterling 2000).
In the language of symbolic interactionism, the subset of physicians who invoked atypical symptoms were confronted with a stimulus (patient presentation of symptoms) and engaged in a process of actively assigning meaning to the stimulus within a social context, which in turn shaped their behavior (O’Brien 2006). The evidence that social factors contribute to the interpretation of symptoms does not mean that biology and evidence-based medicine are completely constructed. Rather, results from this study indicate that the way in which medical knowledge is applied (regardless of the actual biological basis) can contribute to variation in clinical decisions.
A full review of the literature regarding the biological basis of sex/gender differences in CHD is beyond the scope of this article, but it is relevant that a review of research examining differential symptoms of myocardial infarction by sex/gender revealed inconsistent results (Chen, Woods, and Puntillo 2005). Although studies have documented non-chest pain symptoms more often in women than men, there also is evidence of “more similarities than differences” in CHD symptoms (Milner et al. 1999), no difference in reports of chest pain by men and women (Goldberg et al. 1998), women having a similar or slightly higher prevalence of self-reported angina than men (Hemingway et al. 2008), and chest pain not always being the chief complaint for either women or men (Milner et al. 2004). The lack of a clear consensus may explain why physicians who invoked atypical symptoms did not reference a proportion of women who present with atypical symptoms, as would be expected if statistical discrimination were the mechanism at work.
Instead, the lowered diagnostic certainty among some physicians may reflect an unintended consequence of the label “atypical.” Framing research findings about some women’s experiences in opposition to an established norm (i.e., the “typical” CHD symptoms believed to be more often experienced by men) may inadvertently convey that this category of symptoms is inherently less certain. That some physicians in this sample used “atypical” along with “vague” and “nonspecific” supports this interpretation. Framing symptoms associated with a social group in terms of difference (rather than expanding the normative symptoms to include the full range) may create a “double-edged sword” in practice.
These findings indicate that physicians participate in the common human practice of using generalized knowledge to aid in interpreting information and that the framing of medical knowledge may influence their interpretations in unintended ways. Just as the naming of a diagnosis provides meaning to patients and occurs in a social frame (Jutel 2009), the label attached to group-based differences in symptoms shapes the meaning of those symptoms. Analysis of this dataset showed that differential interpretations of symptoms and the attached diagnostic certainty contributed to variation in clinical decisions, particularly regarding treatment decisions appropriate for an urgent cardiac situation. The finding that only a subset of physicians in the sample applied generalized knowledge about atypical symptoms and that this resulted in lower certainty for a portion of these physicians appears to be in line with the reduced magnitude of the sex/gender disparity in CHD treatments.
Limitations and Future Research
This study’s experimental design brings important advantages but also potential limitations. The strong internal validity of an experimental design is offset by a risk to external validity from using video vignettes rather than observing actual patient-provider encounters. As previously described (Lutfey et al. 2010), considerable effort was made to ensure the clinical authenticity of the video vignette, as evidenced by 89.8% of respondents reporting that the vignette patient was “very typical” or “reasonably typical” of their patients. In addition, respondents viewed the vignette in the context of their practice day and were instructed to respond to the patient’s symptoms as they typically would in their practice.
The experimental design prioritizes the assembly of a purposive sample so that physician characteristics of interest (sex/gender and experience level) are varied systematically. This limited the feasibility of pursuing a larger sample. For examining a disparity that has reduced in magnitude over time, the difference that remains is apparent in only a subset of patient/physician encounters, which further limits the sample size of interest. In addition, due to characteristics of the population of primary care physicians, we were unable to systematically vary respondents by other potentially important factors, e.g., race/ethnicity or practice type.
Future research is needed in several areas. We do not provide a statistical test of the full pathway. Our quantitative results taken together with previously published results from the same dataset demonstrate the full pathway, but future analyses should test the full pathway simultaneously using a structural equation model. Diagnostic certainty as a mediator between physicians’ interpretations of patient sex/gender and CHD management also needs to be tested against other potential mediating factors. In addition, our dataset does not allow for a quantitative test of the use of stereotyping or prejudice, and results from a prior statistical analysis of our data that found evidence against the use of statistical discrimination (Maserejian et al. 2009b) need to be replicated.
The causal direction of the relationship between uncertainty and stereotyping (or other heuristic devices) needs further examination. Previous research suggests that uncertainty opens a space for the utilization of heuristic devices, such as stereotypes (Balsa et al. 2003; Smedley et al. 2003); however, we demonstrate that the use of a goal-modified stereotype can create uncertainty rather than the other way around.
Also unclear from this analysis are why some physicians invoked the knowledge of atypical symptoms as a generalization while others did not and why utilizing this knowledge had a “double edged” effect on treatment decisions. More research is needed to understand what factors (e.g., practice culture) may explain this variation.
In conclusion, physicians utilize multiple, compounding heuristic devices to aid in clinical decision making, and these decision rules can either enhance or detract from optimal diagnostic and treatment decisions (Balsa et al. 2003; Bornstein and Emler 2001; Lutfey and McKinlay 2009). This analysis contributes to efforts to answer a specific question: How can we explain the reduced but persistent sex/gender disparity in CHD treatments? Findings further specify a pathway (diagnostic uncertainty) and identify a mechanism (a goal-modified sex/gender stereotype) that can account for at least part of the remaining disparity. Taken together with previous analyses, the cumulative evidence suggests that invoking the notion that women have “atypical symptoms” lowers diagnostic certainty for some physicians; in turn, lower diagnostic certainty reduces physician ordering of “urgent” CHD medications and tests. These results extend our knowledge about how nonmedical factors can lead to variation in clinical decisions and, ultimately, disparities in healthcare.
Biographies
Lisa Welch is Director of the Center for Qualitative Research at New England Research Institutes. Her current research focuses on health disparities, clinical decision making, and help seeking.
Karen Lutfey is Associate Professor of Health and Behavioral Sciences at University of Colorado Denver. While at New England Research Institutes, she was Co-Principal Investigator for the study on which this article is based. Her research interests include medical decision making, stigma, health disparities, and health policy.
Eric Gerstenberger is a Research Scientist/Biostatistician at New England Research Institutes, where he works on multiple projects, including clinical trials, registries, and clinical decision-making research.
Matthew Grace is a graduate student in the Department of Sociology at Indiana University and was a research assistant at New England Research Institutes during the analysis for this article. His research interests include the patient-provider relationship, social networks, and health disparities.
Footnotes
The authors thank Leigh Simmons for her clinical consultation and John McKinlay and the reviewers for providing insightful comments. This study was supported by the National Heart, Lung, and Blood Institute grant HL079174. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
We focus on patient rather than physician sex/gender because empirical evidence showed no significant difference by physician sex/gender for CHD diagnostic certainty or for ordering tests and medications (Lutfey et al. 2010). Unpublished analysis showed no interaction effect between physician and patient sex/gender for physicians’ CHD certainty or treatment decisions. In our analysis, physician sex/gender had a significant influence on ordering a non-urgent medication or urgent test, but this was not related to diagnostic certainty (the focus of this analysis).
The quantitative analysis used three sets of logistic models for four outcomes: ordering an urgent medication, a non-urgent medication, a test only, or an urgent test. Set 1 included patient sex/gender and the other design variables; Set 2 added diagnostic certainty; Set 3 added the interaction term. Details are available from the corresponding author.
Although respondents applied the generalized belief of “atypical symptoms,” they did not invoke the widely recognized sex/gender stereotype that women’s physical complaints often stem from a psychological cause. Details are available from the corresponding author.
References
- Adams Ann, Buckingham Christopher, Lindenmeyer Antje, McKinlay John, Link Carol, Marceau Lisa, Arber Sara. The Influence of Patient and Doctor Gender on Diagnosing Coronary Heart Disease. Sociology of Health and Illness. 2008;30:1–18. doi: 10.1111/j.1467-9566.2007.01025.x. [DOI] [PubMed] [Google Scholar]
- Arber Sara, McKinlay John, Adams Ann, Marceau Lisa, Link Carol, O’Donnell Amy. Patient Characteristics and Inequalities in Doctors’ Diagnostic and Management Strategies Relating to CHD: A Video-Simulation Experiment. Social Science & Medicine. 2006;62:103–15. doi: 10.1016/j.socscimed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- Balsa Ana, McGuire Thomas. Statistical Discrimination in Health Care. Journal of Health Economics. 2001;20:881–907. doi: 10.1016/s0167-6296(01)00101-1. [DOI] [PubMed] [Google Scholar]
- Balsa Ana, McGuire Thomas, Meredith L. Testing for Statistical Discrimination in Health Care. Health Services Research. 2005;40:227–52. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsa Ana, Seiler Naomi, McGuire Thomas, Gregg Bloche M. Clinical Uncertainty and Healthcare Disparities. American Journal of Law and Medicine. 2003;29:203–19. [PubMed] [Google Scholar]
- Bell Dawn, Nappi Jean. Myocardial Infarction in Women: A Critical Appraisal of Gender Differences in Outcomes. Pharmacotherapy. 2000;20:1034–44. doi: 10.1592/phco.20.13.1034.35034. [DOI] [PubMed] [Google Scholar]
- Beresford E. Uncertainty and the Shaping of Medical Decisions. Hastings Center Report. 1991;21:6–11. [PubMed] [Google Scholar]
- Bird C, Fremont A, Bierman A, Wickstrom S, Shah M, Rector T, Horstman T, Escarce J. Does Quality of Care for Cardiovascular Disease and Diabetes Differ by Gender for Enrollees in Managed Care Plans? Womens Health Issues. 2007;17:131–8. doi: 10.1016/j.whi.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Bonte M, von dem Knesebeck Olaf, Siegrist J, Marceau Lisa, Link Carol, Arber Sara, Adams Ann, McKinlay John. Women and Men with Coronary Heart Disease in Three Countries: Are They Treated Differently? Women’s Health Issues. 2008;18:191–8. doi: 10.1016/j.whi.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein B, Emler A. Rationality in Medical Decision Making: A Review of the Literature on Doctors’ Decision-Making Biases. Journal of Evaluation in Clinical Practice. 2001;7:97–107. doi: 10.1046/j.1365-2753.2001.00284.x. [DOI] [PubMed] [Google Scholar]
- Burgess Diana, van Ryn Michelle, Crowley-Matoka Megan, Malat Jennifer. Understanding the Provider Contribution to Race/Ethnicity Disparities in Pain Treatment: Insights from Dual Process Models of Stereotyping. Pain Medicine. 2006;7:119–34. doi: 10.1111/j.1526-4637.2006.00105.x. [DOI] [PubMed] [Google Scholar]
- Charney P. Presenting Symptoms and Diagnosis of Coronary Heart Disease in Women. Journal of Cardiovascular Risk. 2002;9:303–7. doi: 10.1097/01.hjr.0000044516.34172.df. [DOI] [PubMed] [Google Scholar]
- Chen W, Woods S, Puntillo K. Gender Differences in Symptoms Associated with Acute Myocardial Infarction: A Review of the Research. Heart & Lung. 2005;34:240–7. doi: 10.1016/j.hrtlng.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Chou A, Scholle S, Weisman C, Bierman A, Correa-de-Araujo R, Mosca L. Gender Disparities in the Quality of Cardiovascular Disease Care in Private Managed Care Plans. Women’s Health Issues. 2007;17:120–30. doi: 10.1016/j.whi.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Correa-de-Araujo Rosaly, Stevens Beth, Moy Ernest, Nilasena David, Chesley Francis, McDermott Kelly. Gender Differences across Racial and Ethnic Groups in the Quality of Care for Acute Myocardial Infarction and Heart Failure Associated with Comorbidities. Women’s Health Issues. 2006;16:44–55. doi: 10.1016/j.whi.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Di Caccavo Antonietta, Reid Fraser. The Influence of Attitudes toward Male and Female Patients on Treatment Decisions in General Practice. Sex Roles. 1998;38:613–629. [Google Scholar]
- DiMatteo M, Murray C, Williams S. Gender Disparities in Physician-Patient Communication among African American Patients in Primary Care. Journal of Black Psychology. 2009;35:204–27. [Google Scholar]
- Dovidio J, Brigham J, Johnson B, Gaertner S. Stereotyping, Prejudice, and Discrimination: Another Look. In: Macrae N, Stangor C, Hewstone M, editors. Stereotypes and Stereotyping. New York: Guilford; 1996. pp. 276–319. [Google Scholar]
- Epstein Steven. Inclusion: The Politics of Difference in Medical Research. Chicago, IL: The University of Chicago Press; 2007. [Google Scholar]
- Fausto-Sterling Anne. Sexing the Body. New York: Basic Books; 2000. [Google Scholar]
- Fincher C, Williams J, MacLean V, Allison J, Kiefe C, Canto J. Racial Disparities in Coronary Heart Disease: A Sociological View of the Medical Literature on Physician Bias. Ethnicity & Disease. 2004;14:360–71. [PubMed] [Google Scholar]
- Galvao Marie, Kalman Jill, DeMarco Teresa, Fonarow Gregg, Galvin Catherine, Ghali Jalal, Moskowitz Robert. Gender Differences in In-Hospital Management and Outcomes in Patients with Decompensated Heart Failure: Analysis from the Acute Decompensated Heart Failure National Registry (ADHERE) Journal of Cardiac Failure. 2006;12:100–7. doi: 10.1016/j.cardfail.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Gan Sandra, Beaver Shelli, Houck Peter, MacLehose Richard, Lawson Herschel, Chan Leighton. Treatment of Acute Myocardial Infarction and 30-Day Mortality among Women and Men. New England Journal of Medicine. 2000;343:8–15. doi: 10.1056/NEJM200007063430102. [DOI] [PubMed] [Google Scholar]
- Gold Lauren, Krumholz Harlan. Gender Differences in Treatment of Heart Failure and Acute Myocardial Infarction: A Question of Quality or Epidemiology? Cardiology in Review. 2006;14:180–6. doi: 10.1097/01.crd.0000194093.53005.f0. [DOI] [PubMed] [Google Scholar]
- Goldberg R, O’Donnell C, Yarzebski J, Bigelow C, Savageau J, Gore J. Sex Differences in Symptom Presentation Associated with Acute Myocardial Infarction: A Population-Based Perspective. American Heart Journal. 1998;136:189–95. doi: 10.1053/hj.1998.v136.88874. [DOI] [PubMed] [Google Scholar]
- Hemingway Harry, Langenberg Claudia, Damant Jacqueline, Frost Chris, Pyörälä Kalevi, Barrett-Connor Elizabeth. Prevalence of Angina in Women Versus Men: A Systematic Review and Meta-Analysis of International Variations across 31 Countries. Circulation. 2008;117:1526–36. doi: 10.1161/CIRCULATIONAHA.107.720953. [DOI] [PubMed] [Google Scholar]
- Jutel Annemarie. Sociology of Diagnosis: A Preliminary Review. Sociology of Health & Illness. 2009;31:278–99. doi: 10.1111/j.1467-9566.2008.01152.x. [DOI] [PubMed] [Google Scholar]
- Ketcham Jonathan, Lutfey Karen, Gerstenberger Eric, Link Carol, McKinlay John. Physician Clinical Information Technology and Health Care Disparities. Medical Care Research and Review. 2009;66:658–81. doi: 10.1177/1077558709338485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler Riessman Catherine. Narrative Methods for the Human Sciences. Thousand Oaks, CA: Sage Publications; 2008. [Google Scholar]
- LaVeist T, Arthur M, Morgan A, Plantholt S, Rubinstein M. Explaining Racial Differences in Receipt of Coronary Angiography: The Role of Physician Referral and Physician Specialty. Medical Care Research and Review. 2003;60:453–67. doi: 10.1177/1077558703255685. [DOI] [PubMed] [Google Scholar]
- Lefler L, Bondy K. Women’s Delay in Seeking Treatment with Myocardial Infarction: A Meta-Synthesis. Journal of Cardiovascular Nursing. 2004;19:251–68. doi: 10.1097/00005082-200407000-00005. [DOI] [PubMed] [Google Scholar]
- Lutfey Karen, Eva Kevin, Gerstenberger Eric, Link Carol, McKinlay John. Physician Cognitive Processing as a Source of Diagnostic and Treatment Disparities in Coronary Heart Disease: Results of a Factorial Priming Experiment. Journal of Health and Social Behavior. 2010;51:16–29. doi: 10.1177/0022146509361193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutfey Karen, Link Carol, Grant Richard, Marceau Lisa, McKinlay John. Is Certainty More Important than Diagnosis for Understanding Race and Gender Disparities?: An Experiment Using Coronary Heart Disease and Depression Case Vignettes. Health Policy. 2009a;89:279–87. doi: 10.1016/j.healthpol.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutfey Karen, Link Carol, Marceau Lisa, Grant Richard, Adams Ann, Arber Sara, Siegrist Johannes, Böente Markus, von dem Knesebec Olaf, McKinlay John. Diagnostic Certainty as a Source of Medical Practice Variation in Coronary Heart Disease: Results from a Cross-National Experiment of Clinical Decision Making. Medical Decision Making. 2009b;29:606–18. doi: 10.1177/0272989X09331811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutfey Karen, McKinlay John. What Happens along the Diagnostic Pathway to CHD Treatment? Qualitative Results Concerning Cognitive Processes. Sociology of Health and Illness. 2009;31:1077–92. doi: 10.1111/j.1467-9566.2009.01181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maserejian Nancy, Link Carol, Lutfey Karen, Marceau Lisa, McKinlay John. Disparities in Physicians’ Interpretations of Heart Disease Symptoms by Patient Gender: Results of a Video Vignette Factorial Experiment. Journal of Women’s Health (Larchmt) 2009a;18:1661–7. doi: 10.1089/jwh.2008.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maserejian Nancy, Lutfey Karen, McKinlay John. Do Physicians Attend to Base Rates? Prevalence Data and Statistical Discrimination in the Diagnosis of Coronary Heart Disease. Health Services Research. 2009b;44: 1933–49. doi: 10.1111/j.1475-6773.2009.01022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mast Marianne. On the Importance of Nonverbal Communication in the Physician-Patient Interaction. Patient Education and Counseling. 2007;67:315–8. doi: 10.1016/j.pec.2007.03.005. [DOI] [PubMed] [Google Scholar]
- McKinlay John. Some Contributions from the Social System to Gender Inequalities in Heart Disease. Journal of Health and Social Behavior. 1996;37:1–26. [PubMed] [Google Scholar]
- McKinlay John, Link Carol, Freund Karen, Marceau Lisa, O’Donnell Amy, Lutfey Karen. Sources of Variation in Physician Adherence with Clinical Guidelines: Results from a Factorial Experiment. Journal of General Internal Medicine. 2007;22:289–96. doi: 10.1007/s11606-006-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McSweeney J, Lefler L, Crowder B. What’s Wrong with Me? Women’s Coronary Heart Disease Diagnostic Experiences. Progress in Cardiovascular Nursing. 2005;20:48–57. doi: 10.1111/j.0889-7204.2005.04447.x. [DOI] [PubMed] [Google Scholar]
- Mieres J, Heller G, Hendel R, Gulati M, Boden W, Katten D, Shaw L. Signs and Symptoms of Suspected Myocardial Ischemia in Women: Results from the What is the Optimal Method for Ischemia Evaluation in WomeN? Trial. Journal of Women’s Health (Larchmt) 2011;20:1261–8. doi: 10.1089/jwh.2010.2595. [DOI] [PubMed] [Google Scholar]
- Milner K, Funk M, Richards S, Wilmes R, Vaccarino V, Krumholz H. Gender Differences in Symptom Presentation Associated with Coronary Heart Disease. American Journal of Cardiology. 1999;84:396–9. doi: 10.1016/s0002-9149(99)00322-7. [DOI] [PubMed] [Google Scholar]
- Milner K, Vaccarino V, Arnold A, Funk M, Goldberg R. Gender and Age Differences in Chief Complaints of Acute Myocardial Infarction (Worcester Heart Attack Study) American Journal of Cardiology. 2004;93:606–8. doi: 10.1016/j.amjcard.2003.11.028. [DOI] [PubMed] [Google Scholar]
- Mosca L, Appel L, Benjamin E, Berra K, Chandra-Strobos N, Fabunmi R, Grady D, Haan C, Hayes S, Judelson D, Keenan N, McBride P, Oparil S, Ouyang P, Oz M, Mendelsohn M, Pasternak R, Pinn V, Robertson R, Schenck-Gustafsson K, Sila C, Smith SC, Jr, Sopko G, Taylor A, Walsh B, Wenger NK, Williams C. Evidence-Based Guidelines for Cardiovascular Disease Prevention in Women. Circulation. 2004;109:672–93. doi: 10.1161/01.CIR.0000114834.85476.81. [DOI] [PubMed] [Google Scholar]
- Muroff Jordana, Jackson James, Mowbray Carol, Himle Joseph. The Influence of Gender, Patient Volume and Time on Clinical Diagnostic Decision Making in Psychiatric Emergency Services. General Hospital Psychiatry. 2007;29:481–8. doi: 10.1016/j.genhosppsych.2007.08.008. [DOI] [PubMed] [Google Scholar]
- O’Brien Jodi. Symbolic Interactionism: A Perspective for Understanding Self and Social Interaction. In: O’Brien Jodi., editor. The Production of Reality. Thousand Oaks, CA: Pine Forge Press; 2006. pp. 44–62. [Google Scholar]
- O’Keefe-McCarthy S. Women’s Experiences of Cardiac Pain: A Review of the Literature. Canadian Journal of Cardiovascular Nursing. 2008;18:18–25. [PubMed] [Google Scholar]
- Patel H, Rosengren A, Ekman I. Symptoms in Acute Coronary Syndromes: Does Sex Make a Difference? American Heart Journal. 2004;148:27–33. doi: 10.1016/j.ahj.2004.03.005. [DOI] [PubMed] [Google Scholar]
- Runge Marschall, Ohman Magnus. Netter’s Cardiology. Philadelphia: Saunders; 2004. [Google Scholar]
- Shackelton Rebecca, Link Carol, Marceau Lisa, McKinlay John. Does the Culture of a Medical Practice Affect the Clinical Management of Diabetes by Primary Care Providers? Journal of Health Services Research & Policy. 2009;14:96–103. doi: 10.1258/jhsrp.2009.008124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw Leslee, Shaw Richard, Noel Bairey Merz C, Brindis Ralph, Klein Lloyd, Nallamothu Brahmajee, Douglas Pamela, Krone Ronald, McKay Charles, Block Peter, Hewitt Kathleen, Weintraub William, Peterson Eric. Impact of Ethnicity and Gender Differences on Angiographic Coronary Artery Disease Prevalence and In-Hospital Mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation. 2008;117:1787–801. doi: 10.1161/CIRCULATIONAHA.107.726562. [DOI] [PubMed] [Google Scholar]
- Smedley Brian, Stith Adrienne, Nelson Alan. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washinton, D.C: Institute of Medicine. The National Academies Press; 2003. [PubMed] [Google Scholar]
- Springer K, Mager Stellman J, Jordan-Young R. Beyond a Catalogue of Differences: A Theoretical Frame and Good Practice Guidelines for Researching Sex/Gender in Human Health. Social Science and Medicine. 2011;74:1817–1824. doi: 10.1016/j.socscimed.2011.05.033. [DOI] [PubMed] [Google Scholar]
- Street Richard., Jr Gender Differences in Health Care Provider-Patient Communication: Are They due to Style, Stereotypes, or Accommodation? Patient Education and Counseling. 2002;48:201–6. doi: 10.1016/s0738-3991(02)00171-4. [DOI] [PubMed] [Google Scholar]
- van Ryn Michelle, Fu Steven. Paved with Good Intentions: Do Public Health and Human Service Providers Contribute to Racial/Ethnic Disparities in Health? American Journal of Public Health. 2003;93:248–55. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von dem Knesebeck Olaf, Bonte M, Siegrist J, Marceau Lisa, Link Carol, Arber Sara, Adams Ann, McKinlay John. Country Differences in the Diagnosis and Management of Coronary Heart Disease - A Comparison between the US, the UK and Germany. BMC Health Services Research. 2008;8:198. doi: 10.1186/1472-6963-8-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wizemann Theresa, Pardue Mary-Lou. Exploring the Biological Contributions to Human Health: Does Sex Matter? Washington D.C: National Academy of Sciences; 2001. [PubMed] [Google Scholar]


