Abstract
In recent years there has been widespread acceptance that cognitive behavior therapy (CBT) is the treatment of choice for bulimia nervosa. The cognitive behavioral treatment of bulimia nervosa (CBT-BN) was first described in 1981. Over the past decades the theory and treatment have evolved in response to a variety of challenges. The treatment has been adapted to make it suitable for all forms of eating disorder—thereby making it “transdiagnostic” in its scope— and treatment procedures have been refined to improve outcome. The new version of the treatment, termed enhanced CBT (CBT-E) also addresses psychopathological processes “external” to the eating disorder, which, in certain subgroups of patients, interact with the disorder itself. In this paper we discuss how the development of this broader theory and treatment arose from focusing on those patients who did not respond well to earlier versions of the treatment.
In recent years there has been widespread acceptance that cognitive behavior therapy (CBT) is the treatment of choice for bulimia nervosa (National Institute for Health and Clinical Excellence, 2004; Wilson, Grilo, & Vitousek, 2007; Shapiro et al., 2007). The cognitive behavioral treatment of bulimia nervosa (CBT-BN) was first described in 1981 (Fairburn, 1981). Several years later, Fairburn (1985) described further procedural details along with a more complete exposition of the theory upon which the treatment was based (Fairburn, Cooper, & Cooper, 1986). This theory has since been extensively studied and the treatment derived from it, CBT-BN (Fairburn, Marcus, & Wilson, 1993), has been tested in a series of treatment trials (e.g., Agras, Crow, et al., 2000; Agras, Walsh, et al., 2000; Fairburn, Jones, et al., 1993). A detailed treatment manual was published in 1993 (Fairburn, Jones, et al., 1993). In 1997 a supplement to the manual was published (Wilson, Fairburn, & Agras, 1997) and the theory was elaborated in the same year (Fairburn, 1997a).
CBT-BN has evolved over the past decade in response to a variety of challenges: Its procedures have been refined, particularly those addressing patients’ overevaluation of shape and weight, and it has been adapted to make it suitable for all forms of eating disorder, thereby making it “transdiagnostic” in its scope (see Fairburn, 2008; Fairburn, Cooper, & Shafran, 2003). The new version of the treatment, termed enhanced CBT (CBT-E), also addresses psychopathological processes “external” to the eating disorder, which, in certain subgroups of patients, interact with the disorder itself. In this paper we discuss how the development of this broader theory and treatment arose from focusing on those patients who did not respond well to earlier versions of the treatment.
The Cognitive Behavioral Theory of Bulimia Nervosa
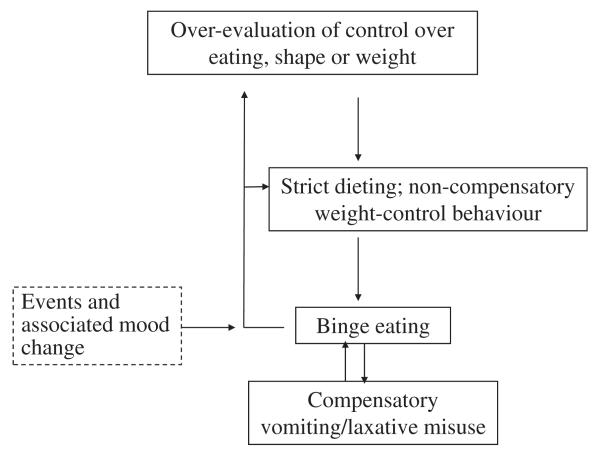
According to the cognitive behavioral theory of bulimia nervosa, central to the maintenance of the disorder is the patient’s overevaluation of shape and weight, the so-called “core psychopathology” (see Fig. 1, which shows in schematic form the core eating disorder maintaining mechanisms). Most other features can be understood as stemming directly from this psychopathology, including the dietary restraint and restriction, the other forms of weight-control behavior, the various forms of body checking and avoidance, and the preoccupation with thoughts about shape, weight, and eating (see Fairburn, 2008).
Figure 1.
A schematic representation of the cognitive behavioral theory of the maintenance of bulimia nervosa (modified from Fairburn, Cooper, & Shafran, 2003).
The only feature of bulimia nervosa that is not obviously a direct expression of the core psychopathology is binge eating. The cognitive behavioral theory proposes that binge eating is largely a product of a form of dietary restraint (attempts to restrict eating), which may or may not be accompanied by dietary restriction (actual undereating). Rather than adopting general guidelines about how they should eat, patients try to adhere to multiple demanding, and highly specific, dietary rules and tend to react in an extreme and negative fashion to the (almost inevitable) breaking of these rules. Even minor dietary slips are viewed as evidence of lack of self-control. Patients respond to such rule-breaking by temporarily abandoning their dietary restraint, thus succumbing to the urge to eat that arises from the restraint (and any accompanying dietary restriction), the result being a short-lived period of uncontrolled eating (i.e., an episode of subjective or objective binge eating). This produces the distinctive pattern of eating that characterizes bulimia nervosa in which attempts to restrict eating are interrupted by repeated episodes of binge eating. The binge eating in turn maintains the core psychopathology by intensifying patients’ concerns about their ability to control their eating, shape, and weight. It also encourages yet greater dietary restraint, thereby increasing the risk of further binge eating. Patients’ dietary slips and binges are particularly prone to occur in response to adverse day-to-day events and negative moods, in part because it is difficult to maintain dietary restraint under such circumstances and in part because binge eating both temporarily ameliorates negative mood states and it distracts patients from thinking about their difficulties.
A further process maintains binge eating among those who practice compensatory purging (i.e., those who induce vomiting or take laxatives in response to specific episodes of binge eating). Patients’ belief that purging will minimize weight gain results in the undermining of a major deterrent to binge eating. They do not realize that vomiting only retrieves part of what has been eaten, and laxatives have little or no effect on energy absorption (see Fairburn, 1995).
This cognitive behavioral theory is supported by a variety of lines of evidence (for details, see Fairburn et al., 2003) and it has clear implications for treatment. It suggests that if treatment is to have a lasting impact on binge eating and purging, the one aspect of the disorder that most patients want to change, it also needs to address extreme dieting, overevaluation of shape and weight, and any tendency for a patient’s eating to change in response to adverse events and negative moods.
CBT of Bulimia Nervosa
CBT for bulimia nervosa is designed to address each of the maintaining processes outlined in the cognitive behavioral theory above. The treatment is outpatient-based and, as evaluated in treatment trials, involves 15 to 20 sessions over approximately 5 months. A range of cognitive behavioral procedures are used with the cornerstone being a specific sequence of cognitive behavioral tasks and “experiments” set within the context of a personalised version of the cognitive behavioral theory of maintenance.
As noted there is a substantial body of evidence supporting CBT-BN, and the findings indicate that CBT-BN is the leading treatment. However, at best, half the patients who start treatment make a full and lasting response. Between 30% and 50% of patients cease binge eating and purging, and a further proportion show some improvement while others drop out of treatment or fail to respond (Wilson & Fairburn, 2007). These findings led us to ask the question, “Why aren’t more people getting better?” (Fairburn et al., 2003).
Why Aren’t More People Getting Better?
We examined various explanations (for a detailed discussion of these see Fairburn et al., 2003) for why there has not been a greater response to CBT-BN and, on the basis of our clinical experience, concluded that the cognitive behavioral theory needed to be extended to embrace four additional maintaining mechanisms that, in certain subgroups of patients, contribute to the maintenance of the eating disorder: clinical perfectionism, mood intolerance, low self-esteem, and interpersonal difficulties. We provide two case illustrations of patients treated using the focused form of the intervention (see Table 1 for an outline of treatment) that highlight how failure to address these additional mechanisms might account for treatment nonresponse. This is followed by a brief description of the revised theory and the evidence that supports it.
Table 1.
The Core Elements of the Focused Form of Enhanced Cognitive Behavioral Treatment
| Stage One |
| The aims are to engage the patient in treatment and change. |
|
| Stage Two |
| This is a transitional stage. |
|
| Stage Three |
| The aim is to address the key mechanisms that are maintaining the patient’s eating disorder. |
|
| Stage Four |
| The aims are to ensure that progress made in treatment is maintained and that the risk of relapse is minimised. |
|
Two Case Illustrations1
Patient A
Patient A was a 27-year-old woman referred by her primary care physician for the treatment of an eating disorder. Initial assessment indicated that she was suffering from an eating disorder that met DSM-IV (American Psychiatric Association, 1994) diagnostic criteria for bulimia nervosa. She had been dissatisfied with her weight since adolescence and began dieting to lose weight during her last 2 years at high school. At this time she weighed 130 lbs (59 kg; BMI=22.5). She had always pushed herself to achieve and had done well academically, but felt under added pressure to perform well in her final school examinations. Adhering to a strict diet helped her to feel more confident and in control and she initially lost 15 lbs (7 kg). The weight loss and consequent change in shape also represented a valued achievement in that she felt that she had finally managed to attain some success in an important area of her life (achieving her desired shape and weight) that had previously eluded her. She continued to restrict her eating while at university and gradually lost more weight, particularly at times when she felt under pressure to perform well. In the year before her initial assessment she started a new demanding job, which she enjoyed. However, she again felt under pressure to do well and lost further weight, reducing her weight to 98 lbs (44.4 kg; BMI=16.9). At this stage she met criteria for a diagnosis of anorexia nervosa. By the time she was seen for assessment she had been experiencing episodes of binge eating for several months and her weight had risen to 103 lbs (46.7 kg; BMI=17.8).
The patient described her daily food intake as consisting of a small bowl of cereal in the morning, a salad for lunch, and a small helping of pasta and vegetables in the evening. On some occasions she would add a yoghurt or apple to her diet. She weighed all her food and her daily eating routine varied little. The patient described a range of rigid dietary rules concerning the type and quantity of food that she would allow herself to eat. Any breaking of these rules would lead to an episode of binge eating during which she would typically eat a large tub of ice cream and 4 to 5 large cookies. These occurred on average twice each week. Eating with others was problematic as it risked her breaking her rules and because she disliked being seen while eating. Hence, she avoided eating out. The patient exercised each day, alternating between running (at least 5 miles) and cycling (at least 15 miles), and felt that she only deserved to eat if she had completed the requisite amount of exercise. She recorded her exercising on a spreadsheet and was always trying to improve on her performance.
The patient was extremely concerned about her weight and shape. She weighed herself daily and she repeatedly checked her shape by scrutinizing parts of her body (to see if she was “failing” and becoming fat) and by comparing her body with that of objectively thin women. Her other prominent concern was the quality of her performance in two areas of life: her work and her close friendships. In both of these areas she had goals that were as exacting as those she pursued with regard to eating and exercise. She was striving to work harder than all her colleagues and to meet certain targets about the exact amount of “quality” time she spent with her various friends.
Initially the treatment of Patient A proceeded well. The therapist was able to engage the patient in the process of treatment and provided education about the psychological, social, and physical effects of maintaining a low weight. The patient showed interest in understanding the eating disorder and what was maintaining it. She responded well to the case formulation, was excellent at self-monitoring in real time, and appeared to understand the benefits of change and weight regain. She had more difficulty reducing the frequency of her weight checking and on relying instead on the weight recorded with the therapist at the beginning of her treatment sessions, but did begin to manage this after several weeks.
Considerable difficulties were encountered in helping the patient to act consistently on her decision not to undereat and thereby allow herself to regain weight. The introduction of regular eating required her to add three snacks to her existing pattern of three meals. She did this, albeit reluctantly, as she was able to incorporate the snacks without breaking her rules regarding the type and quantity of food that she permitted herself. However, she was not consistently able to increase the amount that she ate. When she did manage to increase her food intake, her intense concerns about weight gain, and the loss of control that it represented (to her), resulted in her weighing herself more frequently outside of sessions. She reacted to any perceived increase in weight by thinking that she was becoming “fat” and by reducing her eating. Thus, although there were small increases in her weight (recorded during the weekly in-session weighing), these were counterbalanced by decreases and, over time, her weight remained largely unchanged. She was also resistant to making any changes in her exercise routine.
A review of the patient’s progress revealed that the major obstacle to change was her overevaluation of the importance of controlling her shape, weight, and eating. An attempt to reduce the importance attached to these domains of life was unsuccessful as she was unwilling to do anything that would reduce the time she spent on work, exercise and her close friendships (because she feared that this would risk her performing less well in these areas). Equally, attempts to address the repeated body checking proved unsuccessful. It appeared that the importance (to her self-evaluation) of striving to meet her standards in multiple areas of life was proving an obstacle to change. She accepted this but was nevertheless unable (as she saw it) to “lower her standards” with regard to controlling her shape, weight, and eating, nor was she able to do so in the areas of exercise, work, and friendships. This was due to the influence of what we term “clinical perfectionism.”
Patient B
Patient B was a 23-year-old college student who met DSM-IV diagnostic criteria for bulimia nervosa. She had been dissatisfied with her weight since early adolescence and began dieting to lose weight at age 16. Initially she lost about 14 lbs (6 kg) in weight but then found it progressively more difficult to stick to her diet and began experiencing episodes of binge eating and vomiting. Over the subsequent 6 years her weight fluctuated between 117 lbs (53 kg; BMI=20) and 137 lbs (62 kg; BMI=24). At assessment the patient described her daily food intake as consisting of a very small bowl of cereal for breakfast and a small salad for lunch. She often tried to delay these meals or to skip them altogether. She reported episodes of binge eating on most evenings (a typical binge including a loaf of bread, a large family-size carton of ice cream, and a packet of cookies). During such evenings she would vomit up to five times. The patient described a range of rigid dietary rules about how much she should eat at each meal and she avoided eating foods that she regarded as fattening and likely to trigger binges. At assessment she weighed 143 lbs (65 kg; BMI=25).
Patient B found her body “repulsive” and had avoided weighing herself for the past 6 months. At times she checked her body in the mirror (to see “how fat she was”) and she sometimes measured herself, but at other times she would avoid seeing her body as far as possible. She always avoided wearing tight-fitting clothes.
In addition, to her weight and shape concerns, Patient B reported marked short-lived mood fluctuations characterized by anxiety or anger. In the past she had cut herself to relieve tension and more recently she had used large amounts of alcohol (a bottle or more of wine a night) to “numb” herself. She reported that binge eating also helped her to modulate her mood.
As with Patient A, this patient responded positively to the case formulation as she felt it “explained” her eating disorder. She was only partially successful at real-time self-monitoring as she abandoned recording when experiencing adverse mood states.
After 4 weeks of treatment the patient’s frequency of binge eating had decreased. Problem-solving helped her to address the events and circumstances that triggered binges, and this was successful on some occasions, but the patient continued to binge eat several times a week. A detailed review of the mechanisms responsible for these binges revealed that changes in mood were the usual proximal trigger. Indeed, it was concluded that a major process maintaining the patient’s eating disorder was her inability to tolerate certain emotional states, a phenomenon that we term “mood intolerance.” Instead of dealing appropriately with adverse mood states, she was using binge eating (and on occasions alcohol) to reduce her awareness of these states (and the associated cognitions) and to neutralize it.
The Extended Cognitive Behavioral Theory of the Maintenance of Bulimia Nervosa
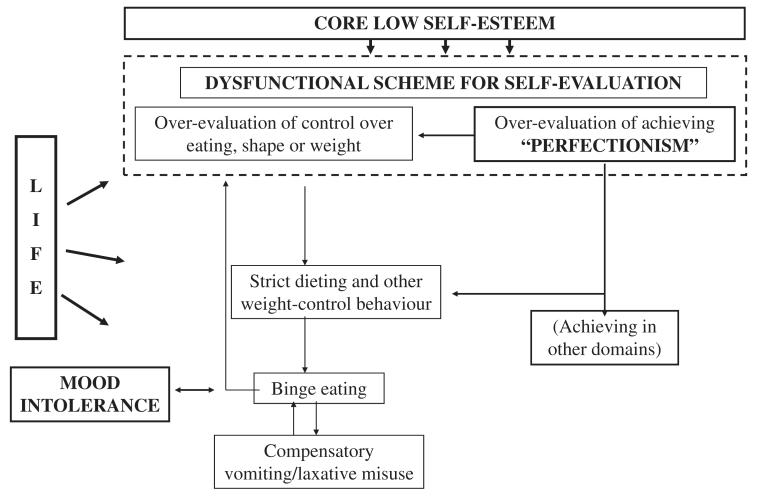
In the light of our experience with patients such as those described, we proposed that in certain patients one or more of four additional maintaining processes interact with the core eating disorder maintaining mechanisms (shown in Fig. 1) and that when this occurs they constitute further obstacles to change. The first of these maintaining mechanisms concerns the influence of extreme perfectionism (“clinical perfectionism”) as shown by Patient A. The second concerns difficulty coping with intense mood states (“mood intolerance”), seen in Patient B. The two other mechanisms concern the impact of unconditional and pervasive low self-esteem (“core low self-esteem”), and marked interpersonal problems (“interpersonal difficulties”). Limitations on space prevent us from providing clinical illustrations of these latter two mechanisms.
This new theory represents an extension of the original theory illustrated in Fig. 1. Fig. 2 shows in schematic form both the core maintaining mechanisms and the four hypothesised additional mechanisms.
Figure 2.
A schematic representation of the extended cognitive behavioral theory of the maintenance of bulimia nervosa. “Life” is shorthand for interpersonal life (from Fairburn, Cooper, & Shafran, 2003).
Clinical Perfectionism
We have defined “clinical perfectionism”—that is, perfectionism of clinical significance (Shafran, Cooper, & Fairburn, in 2002)—as the overevaluation of striving for, and achieving, personally demanding standards, despite adverse consequences. The suggestion is that at the heart of this psychopathology is a system for self-evaluation in which self-worth is judged largely on the basis of striving to achieve demanding goals and success at meeting them. Thus we view clinical perfectionism as an example of a dysfunctional system for self-evaluation much like the “core psychopathology” of eating disorders. We regard it as external to the eating disorder in the sense that it is not an inherent or necessary feature of the disorder. However, when perfectionism is present and personally demanding standards are applied to eating, weight, and shape and their control, they intensify aspects of the eating disorder. Patients may, for example, diet especially intensely and exercise particularly rigorously not only to control their weight and shape but also to achieve success at striving towards and meeting demanding personal goals.
Perfectionism is well-known to co-occur with eating disorders (see Shafran et al., 2002; Wonderlich, 2002). Under these circumstances, our clinical observations indicate that there is often an interaction between the two with the patients’ perfectionist standards being applied to their attempts to control eating, shape, and weight, as well as to other aspects of their life (e.g., their performance at work or sport). As in other expressions of clinical perfectionism (Shafran et al., 2002), there is fear of failure (i.e., with respect to eating disorder psychopathology, these are expressed as fears of overeating, “fatness,” and weight gain); frequent and selective attention to performance (such as frequent shape and weight checking, calorie counting, weighing food, etc.); and self-criticism arising from negatively biased appraisals of performance. The resulting secondary negative self-evaluation in turn encourages even more determined striving to meet valued goals—including, in this case, striving to meet goals in the domain of controlling eating, shape, and weight—thereby serving to maintain the eating disorder. In the case of Patient A, we hypothesized that this interaction was an obstacle to the patient ceasing to undereat and to modifying her weight and shape checking, both of which were contributing to the maintenance of her disorder. We predicted that, for patients such as A, were clinical perfectionism to be moderated, a potent additional network of maintaining mechanisms would be removed, thereby facilitating change. Details of how this might be achieved are provided in the comprehensive treatment guide (Fairburn, 2008).
Mood Intolerance
The original version of the cognitive behavioral theory recognized that adverse mood states can disrupt dietary restraint and constitute a trigger of binge eating (Fairburn et al., 1986). It subsequently became clear that in some patients there is a more complex relationship between emotional states and binge eating (e.g., Meyer, Waller, & Waters, 1998; Polivy & Herman, 1993; Steinberg, Tobin, & Johnson, 1990; Stice, 1994; Waller, 2002).
In our expanded conceptualization we proposed that a subgroup of patients with eating disorders (such as Patient B) have what may be termed “mood intolerance.” Usually this intolerance is of adverse mood states, such as anger, anxiety, or depression, but in some cases there is intolerance of all intense mood states including positive ones (e.g., excitement). Instead of accepting changes in mood and dealing appropriately with them, these patients engage in what may be termed “dysfunctional mood modulatory behavior.” This reduces their awareness of the triggering mood state (and the associated cognitions), and also neutralizes it, but at a personal cost. The dysfunctional mood modulatory behavior may take the form of self-injury (e.g., cutting, punching, or burning themselves), which has the effect of rapidly dissipating the initial mood state, or it may involve taking psychoactive substances (e.g., alcohol, tranquilizers) to directly modify how they feel. Both classes of behavior are not uncommon among patients with eating disorders (e.g., Claes, Vandereycken, & Vertommen, 2001; Holderness, Brooks-Gunn, & Warren, 1994; Paul, Schroeter, Dahme, & Nutzinger, 2002).
It is often not clear whether patients with mood intolerance actually experience unusually intense mood states or whether they are especially sensitive to normal mood states. Often, in our experience, both appear to be the case. Either way, cognitive processes commonly contribute to the phenomenon; for example, such patients typically respond to incipient mood change by thinking that they will not be able to cope with the resulting feelings and thoughts, a reaction that can amplify the triggering mood state.
Among patients with an eating disorder and mood intolerance, binge eating, vomiting, and intense exercising can become habitual means of mood modulation. In the case of Patient B, we hypothesized that both the excessive alcohol intake and the binge eating had become ways of modulating her intense moods. We predicted that were mood intolerance to be addressed in such patients, a powerful additional process maintaining the disorder would be removed. A detailed account of the approach we use to address mood intolerance is provided in the complete treatment guide (Fairburn, 2008).
Core Low Self-esteem
While most patients with bulimia nervosa are self-critical as a result of their failure to achieve their goals, a form of negative self-evaluation that generally reverses with successful treatment, there is a subgroup whose self-evaluation is more pervasively negative. Thus, rather than simply thinking negatively about themselves as a result of their inability to control their eating, shape, and weight, these patients have, in our view, an unconditional negative view of themselves which contributes to their permanent identity. Their negative self-judgments are autonomous and largely independent of performance: In other words, they are neither affected much by events and circumstances nor by changes in the state of the eating disorder.
Such “core low self-esteem” tends to obstruct change in general. This is through two main mechanisms. First, it creates hopelessness about the capacity to change, thereby undermining patients’ compliance with treatment; and second, it results in their pursuing, with particular determination, achievement in valued domains (in this case control over eating, shape, and weight). The state is self-perpetuating since these patients show particularly pronounced negative cognitive processing biases coupled with overgeneralization, with the result that any perceived “failure” is interpreted as confirmation that they are failures as people, thereby reaffirming their overall negative view of themselves.
Given the many barriers to change that arise as a result of core low self-esteem, it is not surprising that clinical experience and some research findings have suggested that such patients respond particularly poorly to treatment (Fairburn, Kirk, O’Connor, Anastasiades, & Cooper, 1987; Fairburn Peveler, Jones, Hope, & Doll, 1993). On the other hand, were their core low self-esteem to be addressed, we predicted that these patients’ outcome would improve as a result.
Interpersonal Difficulties
The original cognitive behavioral account of the maintenance of bulimia nervosa paid little attention to patients’ circumstances—other than acknowledging that the proximal triggers of binge eating were commonly interpersonal in nature. The need to broaden this focus has been made especially clear by the research on interpersonal psychotherapy (IPT). This indicates that an exclusively interpersonal treatment is about as effective as CBT in the longer-term (Agras, Walsh, et al., 2000; Fairburn, Jones, et al., 1993; Fairburn et al., 1995) despite the fact that it does not directly address any of the maintaining mechanisms identified by the cognitive behavioral theory (Fairburn, 1997b).
There can be no doubt that interpersonal processes contribute in a variety of ways to the maintenance of all forms of eating disorder. Four examples may be used to illustrate this point. First, in younger patients, family tensions often intensify resistance to eating. It can be argued that this reflects a short-term intensification of their need for a sense of “control,” a need that is displaced onto dietary self-control (Fairburn, Shafran, & Cooper, 1999). Second, it is obvious that certain interpersonal environments magnify concerns about controlling eating, shape, and weight. These include families in which there are other members with an eating disorder, and occupations in which there is pressure to be slim. Third, as already noted, adverse interpersonal events commonly precipitate episodes of binge eating, and there is evidence that patients with bulimia nervosa may be especially sensitive to social interactions (Steiger, Gauvin, Jabalpurwala, Seguin, & Stotland, 1999). Fourth, long-term interpersonal difficulties undermine self-esteem which, as noted earlier, is prone to result in patients striving even harder to achieve valued goals, such as success at controlling eating, shape, and weight. It is also relevant that there is evidence that disturbed interpersonal functioning predicts a poor response to treatment (Agras, Crow, et al., 2000; Steiger, Leung & Thibaudeau, 1993). In summary, we thought that there were good reasons to propose that interpersonal difficulties could perpetuate eating disorders and that their resolution might facilitate change.
An Evaluation of the New, Enhanced Form of CBT (CBT-E)
On the basis of this “extended” theory of the maintenance of bulimia nervosa, we developed two versions of CBT-E, a “focused” version that exclusively addresses the processes maintaining the eating disorder psychopathology (Fairburn, Cooper, Shafran, Bohn, Hawker, Murphy, et al., 2008) and a “broad” version that also addresses one or more of the four additional hypothesized maintaining processes (Fairburn Cooper, Shafran, Bohn, & Hawker, 2008). Both versions are transdiagnostic in scope. Treatment involves 20 individual treatment sessions over 20 weeks, the first 4 weeks being common to both forms of treatment (Fairburn, Cooper, & Shafran, 2008). We have recently compared these two forms of CBT-E in the context of a two-site randomized controlled trial (Fairburn et al., 2009). The trial was unusual in that focused on the treatment of outpatients with any form of eating disorder provided that their BMI was over 17.5. Therefore, by definition, these patients met DSM-IV diagnostic criteria for bulimia nervosa or eating disorder NOS. As those who are significantly underweight (BMI 17.5 and below) require a longer treatment, they were not included in this study.
One hundred and fifty-four patients were entered into the trial. Treatment was on an individual basis and it followed the CBT-E protocol of 20 treatment sessions over 20 weeks. Treatment was followed by a 60-week closed period of follow-up. After 4 weeks of treatment (the period when the two treatments are the same) the therapists rated the severity of each patient’s clinical perfectionism, mood intolerance, core low self-esteem, and interpersonal difficulties. These ratings were made prior to the therapist learning which treatment the patient was then going on to receive and were used to identify patients with marked additional psychopathology of the type that the broad form of CBT-E is designed to target. The outcome of these patients was compared with that of the remainder in relation to the form of CBT-E that the patient actually received.
At the end of 20 weeks of treatment, over half the randomized patients (52.7% and 53.3% of those with bulimia nervosa and eating disorder NOS respectively) had a level of eating disorder features less than 1 SD above the community mean, and at 60-week follow-up the comparable figures were 61% and 46%. These figures suggest that CBT-E might be more effective than CBT-BN (see for comparison Agras, Walsh, et al., 2000), especially in light of the inclusive nature of the sample, although a direct comparison of CBT-BN and CBT-E would be needed to substantiate this conclusion. In the full sample there was no difference between the two forms of CBT-E and, not surprisingly, the subgroup with marked additional psychopathology (about 40% of the sample) responded less well in general than the remainder. However, within this subgroup, those who received the broad form of CBT-E did better than those who received the focused version, whereas, interestingly, the reverse pattern of findings was present within the remaining patients with the focused version being superior to the broad version.
Clinical and Research Implications
This program of work illustrates the value of focusing attention on those patients who benefit least from treatment. Doing so resulted in the enhanced form of CBT, which appears to be markedly more effective and more useful (in terms of the full range of patients treated) than its forerunner, CBT-BN.
However the finding regarding the relative effects of the two forms of CBT-E must be viewed as tentative. To determine its robustness, further comparisons of the two forms of CBT-E are needed. In the meantime, it is our view that it would seem reasonable to use the present findings to guide clinical practice. Thus the simpler focused form of the treatment should be viewed as the default form of CBT-E as it is easier to learn and implement, with the new, more complex, form being reserved for patients of the type that previously benefited least from treatment.
Acknowledgments
We are grateful to the Wellcome Trust. Without the Trust’s sustained support over the past 25 years this work would not have been possible. CGF is supported by a Principal Research Fellowship (046386) and ZC is supported by a programme grant (046386). The transdiagnostic trial (also funded by the Wellcome Trust) was conducted in collaboration with Professor Robert Palmer of the University of Leicester. Shawnee Basden helped prepare the manuscript.
Footnotes
Details about the cases have been modified to protect the identity of the clients.
References
- Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HC. Outcome predictors for the cognitive behavioral treatment of bulimia nervosa: data from a multisite study. American Journal of Psychiatry. 2000;157:1302–1308. doi: 10.1176/appi.ajp.157.8.1302. [DOI] [PubMed] [Google Scholar]
- Agras WS, Walsh BT, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry. 2000;57:459–466. doi: 10.1001/archpsyc.57.5.459. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed Author; Washington, DC: 1994. [Google Scholar]
- Claes L, Vandereycken W, Vertommen H. Self-injurious behaviors in eating-disordered patients. Eating Behaviors. 2001;2:263–272. doi: 10.1016/s1471-0153(01)00033-2. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. A cognitive behavioral approach to the management of bulimia. Psychological Medicine. 1981;11:707–711. doi: 10.1017/s0033291700041209. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive-behavioral treatment for bulimia. In: Garner DM, Garfinkel PE, editors. Handbook of psychotherapy for anorexia nervosa and bulimia. Guilford Press; New York: 1985. pp. 160–192. [Google Scholar]
- Fairburn CG. Overcoming binge eating. Guilford Press; New York: 1995. [Google Scholar]
- Fairburn CG. Eating disorders. In: Clark DM, Fairburn CG, editors. Science and practice of cognitive behavior therapy. Oxford University Press; Oxford: 1997a. pp. 209–241. [Google Scholar]
- Fairburn CG. Interpersonal psychotherapy for bulimia nervosa. In: Garner DM, Garfinkel PE, editors. Handbook of treatment for eating disorders. Guilford Press; New York: 1997b. pp. 278–294. [Google Scholar]
- Fairburn CG. Eating disorders: the transdiagnostic view and the cognitive behavioral theory. In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. Guilford Press; New York: 2008. pp. 7–22. [Google Scholar]
- Fairburn CG, Cooper Z, Cooper PJ. The clinical features and maintenance of bulimia nervosa. In: Brownell KD, Foreyt JP, editors. Handbook of eating disorders: Physiology, psychology and treatment of obesity, anorexia and bulimia. Basic Books; New York: 1986. pp. 389–404. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, Hawker DM, Wales JA, Palmer RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. American Journal of Psychiatry. 2009;166:311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behavior therapy for eating disorders: A ‘transdiagnostic’ theory and treatment. Behavior Research and Therapy. 2003;41:509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Enhanced cognitive behavior therapy for eating disorders (“CBT-E”): An overview. In: Fairburn CG, editor. Cognitive Behavior Therapy and Eating Disorders. Guilford Press; New York: 2008. pp. 23–34. [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R, Bohn K, Hawker DM. Clinical perfectionism, core low self-esteem and interpersonal problems. In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. Guilford Press; New York: 2008. pp. 197–220. [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R, Bohn K, Hawker DM, Murphy R, Straebler S. Enhanced cognitive behavior therapy for eating disorders: the core protocol. In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. Guilford Press; New York: 2008. pp. 45–193. [Google Scholar]
- Fairburn CG, Jones R, Peveler RC, Hope RA, O’Connor ME. Psychotherapy and bulimia nervosa: The longer-term effects of interpersonal psychotherapy, behavior therapy and cognitive behavior therapy. Archives of General Psychiatry. 1993;50:419–428. doi: 10.1001/archpsyc.1993.01820180009001. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Kirk J, O’Connor ME, Anastasiades P, Cooper PJ. Prognostic factors in bulimia nervosa. British Journal of Clinical Psychology. 1987;26:223–224. doi: 10.1111/j.2044-8260.1987.tb01349.x. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Marcus MD, Wilson GT. Cognitive-behavioral therapy for binge eating and bulimia nervosa: a comprehensive treatment manual. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment and treatment. Guilford Press; New York: 1993. pp. 361–404. [Google Scholar]
- Fairburn CG, Norman PA, Welch SL, O’Connor ME, Doll HA, Peveler RC. A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Archives of General Psychiatry. 1995;52:304–312. doi: 10.1001/archpsyc.1995.03950160054010. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Peveler RC, Jones R, Hope RA, Doll HA. Predictors of twelve-month outcome in bulimia nervosa and the influence of attitudes to shape and weight. Journal of Consulting and Clinical Psychology. 1993;61:696–698. doi: 10.1037//0022-006x.61.4.696. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Shafran R, Cooper Z. A cognitive behavioral theory of anorexia nervosa. Behavior Research and Therapy. 1999;37:1–13. doi: 10.1016/s0005-7967(98)00102-8. [DOI] [PubMed] [Google Scholar]
- Holderness CC, Brooks-Gunn J, Warren MP. Comorbidity of eating disorders and substance abuse: review of the literature. International Journal of Eating Disorders. 1994;16:1–34. doi: 10.1002/1098-108x(199407)16:1<1::aid-eat2260160102>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Meyer C, Waller G, Waters A. Emotional states and bulimic psychopathology. In: Hoek HW, Treasure JL, Katzman MA, editors. Neurobiology in the treatment of eating disorders. Wiley; Chichester: 1998. pp. 271–287. [Google Scholar]
- National Institute for Health and Clinical Excellence Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related disorders. 2004 Retrieved from http://www.nice.org.uk/CG009. [PubMed]
- Paul T, Schroeter K, Dahme B, Nutzinger DO. Self-injurious behavior in women with eating disorders. American Journal of Psychiatry. 2002;159:408–411. doi: 10.1176/appi.ajp.159.3.408. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Etiology of binge eating: psychological mechanisms. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment and treatment. Guilford Press; New York: 1993. pp. 173–205. [Google Scholar]
- Shafran R, Cooper Z, Fairburn CG. Clinical perfectionism: Acognitive-behavioral analysis. Behavior Research and Therapy. 2002;40:773–791. doi: 10.1016/s0005-7967(01)00059-6. [DOI] [PubMed] [Google Scholar]
- Shapiro J, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik CM. Bulimia nervosa treatment: A systematic review of randomised controlled trials. International journal of Eating Disorder. 2007;40:321–336. doi: 10.1002/eat.20372. [DOI] [PubMed] [Google Scholar]
- Steiger H, Leung F, Thibaudeau J. Prognostic value of pretreatment social adaptation in bulimia nervosa. International Journal of Eating Disorders. 1993;14:269–276. doi: 10.1002/1098-108x(199311)14:3<269::aid-eat2260140305>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Steiger H, Gauvin L, Jabalpurwala S, Seguin JR, Stotland S. Hypersensitivity to social interactions in bulimic syndromes: relationship to binge eating. Journal of Consulting and Clinical Psychology. 1999;67:765–775. doi: 10.1037//0022-006x.67.5.765. [DOI] [PubMed] [Google Scholar]
- Steinberg S, Tobin D, Johnson C. The role of bulimic behaviors in affect regulation: Different functions for different subgroups? International Journal of Eating Disorders. 1990;9:51–55. [Google Scholar]
- Stice E. Review of the evidence for a sociocultural model of bulimia nervosa and an exploration of the mechanisms of action. Clinical Psychology Review. 1994;14:633–661. [Google Scholar]
- Waller G. The psychology of binge eating. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity: A comprehensive handbook. 2nd ed Guilford Press; New York: 2002. pp. 98–102. [Google Scholar]
- Wilson GT, Fairburn CG. Eating disorders. In: Nathan PE, Gordon JM, editors. Guide to treatments that work. 3rd ed Oxford University Press; New York: 2007. pp. 559–592. [Google Scholar]
- Wilson GT, Fairburn CG, Agras WS. Cognitive-behavioral therapy for bulimia nervosa. In: Garner DM, Garfinkel P, editors. Handbook of treatment for eating disorders. Guilford Press; New York: 1997. pp. 67–93. [Google Scholar]
- Wilson GT, Grilo CM, Vitousek KM. Psychological treatments of eating disorders. American Psychologist. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA. Personality and eating disorders. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity: a comprehensive handbook. 2nd ed Guilford Press; New York: 2002. pp. 204–209. [Google Scholar]