Abstract
Purpose: Individuals receiving postacute care in skilled nursing facilities often require complex, skilled care provided by licensed nurses. It is believed that a stable set of nursing personnel is more likely to deliver better care. The purpose of this study was to determine the relationships among licensed nurse retention, turnover, and a 30-day rehospitalization rate in nursing homes (NHs). Design and Methods: We combined two data sources: NH facility-level data (including characteristics of the facility, the market, and residents) and the Florida Nursing Home Staffing Reports (which provide staffing information for each NH) for 681 Florida NHs from 2002 to 2009. Using a two-way fixed effects model, we examined the relationships among licensed nurse turnover rates, retention rates, and 30-day rehospitalization rates. Results: Results indicate that an NH’s licensed nurse retention rate is significantly associated with the 30-day rehospitalization rate (est. = −.02, p = .04) controlling for demographic characteristics of the patient population, residents’ preferences for hospitalization, and the ownership characteristics of the NH. The NHs experiencing a 10% increase in their licensed nurse retention had a 0.2% lower rehospitalization rate, which equates to 2 fewer hospitalizations per NH annually. Licensed nurse turnover is not significantly related to the 30-day rehospitalization rate. Implications: These findings highlight the need for NH administrators and policy makers to focus on licensed nurse retention, and future research should focus on the measures of staff retention for understanding the staffing/quality relationship.
Key Words: Nursing homes, Turnover, Retention, Rehospitalization
After acute hospitalization, many older medically complex patients are often discharged directly from intensive care units to receive postacute care in nursing homes (NHs). This skilled nursing care accounts for more than $20 billion in Medicare costs annually (Centers for Medicare & Medicaid Services, 2010). In order for Medicare beneficiaries to be qualified for skilled nursing facility (SNF) benefits, they should have been hospitalized for at least three days and require daily skilled nursing or rehabilitative services. Therefore, many post acute NH patients need treatments more sensitive to and contingent on the skilled care provided by the professional nurses (registered nurses [RN] and licensed professional nurses).
Recent reports indicate that approximately one fourth of Medicare SNF patients are readmitted to the hospital within 30 days (MedPAC [Medicare Payment Advisory Commission], 2006; Mor, Intrator, Feng, & Grabowski, 2010). Although rehospitalizations are often necessary, previous research has estimated that approximately 28% to 40% of hospital readmissions might be avoided with high-quality SNF care (MedPAC, 2006; Saliba et al., 2000). In order to prevent rehospitalization of these Medicare beneficiaries receiving postacute care in SNFs, appropriate follow-up care is needed, and a higher professional nurse staffing level increases the capacity of NHs to care for these clinically complex residents (Decker, 2006; Kramer & Fish, 2001). Licensed nurses in NHs consist of RNs and licensed practical nurses (LPNs). The RNs primary roles are to assess resident health, develop treatment plans, and supervise LPNs and other direct care staff. LPNs in NHs provide direct patient care that includes taking vital signs and administering medications. Although LPNs scope of practice is more limited than that of RNs, studies have shown that LPNs often provide more hours of nursing care per day than RNs (Harrington et al., 2008).
Licensed nurses in NHs are important in preventing rehospitalizations as, collectively, they conduct resident assessments, monitor changes in status, interact with family members, and contact physicians regarding significant changes (Decker, 2006). Research has indicated that licensed nurses’ clinical care knowledge, care coordination, and professional oversight contribute to better quality of care in NHs (Castle & Anderson, 2011), and higher RN staffing levels as well as the ratio of skilled to unskilled nurses have been linked to fewer postacute rehospitalizations (Decker, 2008; Intrator et al., 2007; Intrator, Zinn, & Mor, 2004).
It is believed that a stable set of nursing personnel is more likely to deliver better care. Furthermore, several literatures have repeatedly shown that high staff turnover rates are associated with poor quality of care (Bostick, Rantz, Flesner, & Riggs, 2006; Castle & Engberg, 2005; Horn et al., 2010; Zimmerman, Gruber-Baldini, Hebel, Sloane, & Magaziner, 2002). High staff turnover, particularly among licensed nurses, may make it difficult to assess residents and implement care plans, may reduce familiarity between staff and residents, making detection of complications and failing health more difficult, and may affect quality through insufficient supervision and training. Higher licensed nurse turnover has been found to be associated with activities of daily living (ADLs) decline (Horn et al., 2010), and the RN turnover has been found to be associated with infections and hospitalization (Zimmerman et al., 2002). However, some have suggested that some turnover is not necessarily detrimental to the organization (Alexander, Bloom, & Nuchols, 1994; Brannon, Zinn, Mor, & Davis, 2002; Halbur & Fears, 1986), and others have found that the relationship between licensed nurse turnover and quality is not linear (Castle, Engberg, & Men, 2007; Weech-Maldonado, Meret-Hanke, Neff, & Mor, 2004).
Although much literature has been devoted to examining nursing staff turnover, often calculated as the number of terminations in 1 year divided by the total number of staff (Donoghue, 2010), less attention has been paid to NH’s proportions of licensed nurses with long periods of continuous service, or its retention of licensed nurse staff. Castle and Engberg (2008) found that RN stability (defined in their study as the percent of RNs with a tenure of 5 or more years at the facility) is associated with decreased physical restraint use, the prevalence of moderate to severe pain, pressure sores, and indwelling catheters. However, the relationship between licensed nurse retention and rehospitalization remains unknown.
Retention, although a conceptually different measure of staff stability from turnover, has the same potential to influence care and reduce spending on hiring and training. The turnover calculation may reflect turnover for the same position and does not capture the number of employees who are experienced in their roles. Because facilities may not only have a high turnover rate but also have a high retention rate, it is important to investigate NHs’ “stayers” as they represent experienced staff who may contribute to better standards of care quality despite high turnover levels. “Stayers” are important to the NH as they hold the institutional memory, receive facility-specific training, retain knowledge and practice strategies, know the long-stay residents, implement facility-specific protocols, and make it possible to efficiently incorporate new staff into the existing culture and practice.
Conceptual Framework for Assessing the Relationships of Licensed Nurse Turnover and Retention and Rehospitalization
Using Grabowski and colleagues’ (2008) NH decision-making model to hospitalize a NH resident, we assume that the NHs’ rehospitalization rate is based on the welfare and preferences of the residents, preferences of the providers, and the financial implications of hospitalization. The welfare of the residents is related to the sociodemographics and health conditions. In addition, a resident’s welfare is affected by the facility care practices and policies regarding staffing levels, composition of staff, facility resources, and resident care practices. The residents’ preferences for hospitalization will be reflected by, for example, the presence of advance directives, particularly “do not hospitalize” orders. The providers’ attitudes regarding hospitalization will be based on a number of factors such as staff workloads, training, and communication with residents and their families. Finally, financial factors relate to the NH payment rates and ownership status. Based on this framework, we hypothesize that staffing characteristics that influence residents’ welfare and providers’ preferences, specifically the NH’s licensed nurse turnover and retention rates, will be related to rehospitalization of NH residents, controlling for demographic characteristics of the patient population, the preferences of the residents for hospitalization, and the financial factors of the NH.
Patients who are discharged from hospital and admitted to an NH may require treatments more sensitive to and dependent on licensed nursing care. Therefore, preventing a rehospitalization requires appropriate follow-up care in an NH (Stone & Hoffman, 2010), and NHs must have a staff of experienced licensed nurses to provide this care. Theory would suggest that a greater nursing staff presence and decreased workload would be related to better resident welfare and more positive attitudes from physicians and, subsequently, decreased rehospitalizations from the NH setting. Therefore, we hypothesize that facilities with higher rates of licensed nurse retention will have lower rates of rehospitalization as there will be a larger proportion of staff who are familiar with residents, thus facilitating early identification of emerging clinical problems. Additionally, staff with longer tenure in a facility will be more familiar with the assessment, documentation and communication processes, and the facility’s policies and procedures. In addition, we hypothesize that facilities with higher rates of licensed nurse turnover will have higher rehospitalization rates as inexperienced staff may not be able to identify and assess changes or care for residents in ways to maintain their health.
Design and Methods
Data
Data come from an internal file of the LTCFocUS.org, a product of the Shaping Long-Term Care in America Project, being conducted at the Brown University Center for Gerontology and Healthcare Research and supported, in part, by the National Institute on Aging. The internal file is not restricted in the way that the publicly available file is (i.e., that cells with <10 observations are not missing). The data include information on the health and functional status of NH residents, characteristics of facilities, state policies relevant to long-term care services and financing, and data characterizing the markets in which facilities exist. This data set combines the Online Survey Certification and Reporting data (administrative data collected by state survey agencies during nursing facility annual certification inspections); the Minimum Data Set (MDS), resident level data related to resident clinical and functional status; the Area Resource File, a national county level health resources database maintained by the Health Resources and Services Administration that contains data about the health professionals and facilities in each county; and the Residential History File, a data resource developed at the Brown University Center for Gerontology and Healthcare Research that is built using the Medicare Enrollment data, Medicare claims data, and MDS data to track individuals as they move through the long-term care system (Intrator, Hiris, Berg, Miller, & Mor, 2011). In addition to the facility and market characteristics, these data measure resident characteristics of individuals who were in the NH on the first Thursday in April of the given year and therefore reflect the prevalence of NH residents with several characteristics.
Turnover, retention, and staffing data come from the Florida Nursing Home Staffing Report. Pursuant to Florida Statutes section 400.141, each facility must report to the Agency for Health Care Administration the average quarterly staff to resident ratios, number of employed staff during that quarter, number of individuals employed by the facility for at least a year during that quarter, and the number of terminated staff, during the quarter, who had been employed by the facility for at least 3 months. Semiannually, the information is self-reported by NHs and subjected to audit. The Florida law stipulates that facilities must maintain a combined (LPN and RN) licensed nurse ratio of 1.0hr per resident day (HPRD), and, therefore, providers submit staffing data for total licensed nurses. The quarterly data are used to calculate the annual turnover rates for licensed nurses, the retention rate for licensed nurses, and the certified nursing assistant (CNA) HPRD and the licensed nurse HPRD in these analyses.
The sample includes a total of 5,153 facility-year observations from 681 free-standing Medicare and Medicaid certified Florida NHs. Hospital-based facilities were excluded from the analyses, because they are very different in terms of resident severity, structure, and care practice. The NH had to be in operation at least one full year for inclusion in the study.
Outcome Variables
The outcome variable of interest is the 30-day rehospitalization rate, which, from the LTCfocUS data, is defined as the proportion of NH residents who were rehospitalized from the NH within 30 days in a calendar year. The Residential History File was used to determine the proportion of facility residents who were rehospitalized within 30 days of a base hospitalization, where a base hospitalization is an acute care hospitalization from the NH. In these calculations, the denominator is the number of hospitalizations from the facility per year and the numerator is the number of rehospitalizations within 30 days of discharge per facility per year.
Independent Variables
Our two independent variables reflecting staffing characteristics that influence the resident welfare and providers’ preferences for hospitalization, annual licensed nurse turnover, and retention rates are calculated from the staffing data reported by quarters. Licensed nurse turnover, a continuous variable, is calculated by dividing the number of terminated (both voluntary and involuntary) licensed nurses who had been employed by the NH at least 90 days by the number of employed licensed nurses (Castle, 2006).
| Turnover = Sum of terminated licensed nurses in the four quarters/Average number of licensed nurses employed during each quarter of the year. |
The licensed nurse retention rate is calculated by dividing the number of licensed nurses who were reported to have been employed for at least 1 year by the number of current licensed nurses at the facility (Donoghue, 2010).
| Retention = Average licensed nurses employed for at least a year in each quarter for the year/Average number of licensed nurses employed during each quarter for year. |
Director of Nursing is not included in the licensed nurse calculations.
Control Variables
In order to control for inherent differences in NHs’ rehospitalization rates, several facility-level annualized time-varying covariates are included that are shown to be associated with the risk of hospitalization from the nursing home (Grabowski, Stewart, Broderick, & Coots, 2008), and variable selection is guided by our conceptual framework.
To control for resident welfare (as approximated by average demographic characteristics, average health characteristics, resident care practices, and facility resources), we included average age, gender (percent female), and race (percent black) as they have been shown to influence hospitalization risk (Castle & Mor, 1996; Gruneir, Miller, Feng, Intrator, & Mor, 2008). The NH residents’ health—such as physical and cognitive disability as well as a number of specific health characteristics—has been found to be generally associated with the risk of hospitalization (Cai, Mukamel, Veazie, Katz, & Temkin-Greener, 2011; Grabowski et al., 2008). Therefore, we included the average ADL score (Hawes et al., 1995), the average RUGS case-mix index (Fries et al., 1994), and the percent of residents who (a) have a high score (5 or 6) on the Cognitive Performance Scale, indicating severe cognitive impairment (Carter & Porell, 2005; Morris et al., 1994), (b) have a urinary tract infection, and (c) are diagnosed with congestive heart failure. To measure resident care practices, we included the percent of residents who were on a ventilator or had an indwelling catheter.
In order to isolate the effect of turnover and retention on rehospitalization, we also controlled for facility resources using a number of organizational characteristics. We controlled for the facility’s CNA and licensed nurse HPRD, and the presence of a physician extender (defined as the presence of either a nurse practitioner or a physician’s assistant) as they have been suggested to be related to hospitalization of NH residents (Carter & Porell, 2003; Intrator, Castle, & Mor, 1999; Intrator et al., 2007; Intrator & Mor, 2004). Intrator and colleagues (1999) proposed that the existence of specialty units indicated greater facility capabilities to avoid hospitalizations. However, Decker (2008) suggested the association between SCUs and hospitalization rates was perhaps because hospitals may be more likely to discharge patients with high acuity to NHs with specialty care units, thereby increasing risk of hospitalization. We included a dummy variable to indicate whether the facility has a specialty care unit.
To account for residents’ preferences for hospitalization, we included the percent of residents who have advance directives: (a) do not resuscitate and (b) do not hospitalize orders.
Finally, we controlled for the effects of financial factors on the decision to hospitalize postacute patients by including time-varying characteristics, such as the facility occupancy rate, as a proxy for financial stability (Weech-Maldonado, Neff, & Mor, 2003) as well as two measures of residents’ payer sources—percent Medicaid and percent Medicare (Cai et al., 2011). Hospital utilization may also be affected by the local health care resources available. Therefore, we controlled for the number of inpatient hospital beds per 1,000 persons aged 65 years and older in the county (Intrator et al., 2007).
Analyses
For these analyses, generalized linear models were used to estimate the relationships among licensed nurse turnover, licensed nurse retention, and rehospitalization using the XTREG procedure in STATA 11.0 (StataCorp, 2009). In addition to the potential time-varying confounders listed earlier, we controlled for time trends using a set of year dummy variables. Huber-White robust variance estimators were applied to adjust for within-facility clustering over time. Sensitivity analyses were conducted by lagging the dependent variable, rehospitalization rate, so that we could test if the retention in year (t) has an effect on the rehospitalization rate (t + 1).
Results
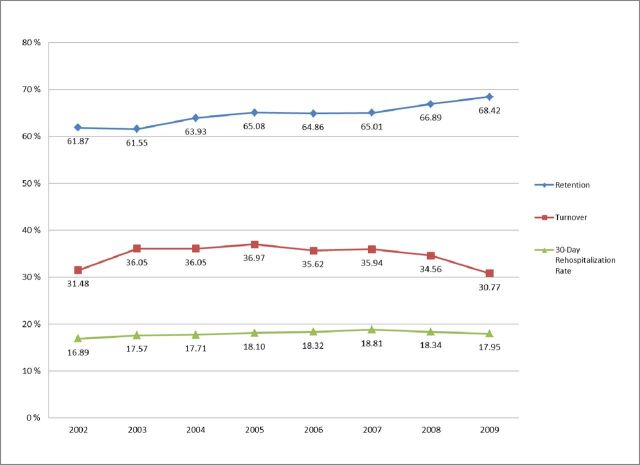
Our final sample consists of 681 NHs over an 8-year period (5,153 facility-year observations). Descriptive analyses indicate that Florida NHs had an average annual licensed nurse retention rate of 64.4% and a turnover rate of 34.7% for the study period (see Figure 1). Annual licensed nurse retention was significantly and negatively correlated with licensed nurse turnover (r = −.41, p < .001; see Table 1). On average, Florida’s NHs had an average staffing ratio of 2.78 CNA HPRD and 1.19 licensed nurse HPRD over the study period (see Table 2). Higher licensed nurse staffing ratios were associated with higher licensed nurse retention rates (r = .02, p = .02) and lower licensed nurse turnover rates (r = −.08, p < .001). The NHs in Florida had on average 122 beds, 58% were owned by a chain, about 74% were for profit, having an average occupancy rate of 88%. In addition, 45% employed a physician extender and about 23% had a specialty care unit. Approximately, 57% of residents were funded primarily by Medicaid and 19% by Medicare.
Figure 1.
Florida nursing homes licensed nurse retention, licensed nurse turnover, and 30-day rehospitalization rate (2002–2009).
Table 1.
Correlation Matrix of Independent and Control Variables
| Licensed nurse retention rate | Licensed nurse turnover rate | Average age | Percent female | Percent black | Average ADL score | Average RUGS score | Percent high CPS | Percent on ventilator | Percent with UTI | Percent with catheter | Percent with CHF | Percent with DNR | Percent with DNH | Occupancy | Percent Medicaid | Percent Medicare | CNA HPRD | Licensed nurse HPRD | Physician extender | Specialty care unit | Hospital beds/ 1,000 65+ | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Licensed nurse retention rate | 1.00 | |||||||||||||||||||||
| Licensed nurse turnover rate | −.41 | 1.00 | ||||||||||||||||||||
| Average age | .09 | −.05 | 1.00 | |||||||||||||||||||
| Percent female | .05 | .00 | .69 | 1.00 | ||||||||||||||||||
| Percent black | −.03 | −.01 | −.60 | −.41 | 1.00 | |||||||||||||||||
| Average ADL Score | .10 | −.02 | .26 | .26 | −.23 | 1.00 | ||||||||||||||||
| Average RUGS score | −.01 | .03 | −.08 | −.04 | −.08 | .63 | 1.00 | |||||||||||||||
| Percent high CPS | .05 | −.05 | .10 | .11 | −.14 | .35 | .10 | 1.00 | ||||||||||||||
| Percent on ventilator | .03 | −.03 | −.23 | −.13 | .07 | .14 | .30 | .11 | 1.00 | |||||||||||||
| Percent with UTI | −.08 | .05 | .11 | .07 | −.19 | .13 | .31 | −.06 | .04 | 1.00 | ||||||||||||
| Percent with catheter | −.06 | .06 | −.17 | −.18 | .01 | .15 | .45 | −.07 | .20 | .31 | 1.00 | |||||||||||
| Percent with CHF | −.03 | .03 | .21 | .21 | −.13 | .12 | .16 | −.02 | −.03 | .12 | .11 | 1.00 | ||||||||||
| Percent with DNR | .03 | .01 | .55 | .38 | −.54 | .14 | −.15 | .11 | −.13 | .10 | −.13 | .11 | 1.00 | |||||||||
| Percent with DNH | .05 | .00 | .18 | .11 | −.17 | .08 | .00 | .05 | −.03 | .04 | −.04 | .10 | .27 | 1.00 | ||||||||
| Occupancy | .10 | .04 | .16 | .17 | −.07 | .08 | −.08 | .03 | −.11 | −.04 | −.08 | .02 | .10 | .06 | 1.00 | |||||||
| Percent Medicaid | −.02 | .03 | −.54 | −.28 | .49 | −.29 | −.26 | −.05 | −.02 | −.22 | −.10 | −.03 | −.31 | −.09 | .05 | 1.00 | ||||||
| Percent Medicare | −.02 | .07 | .34 | .26 | −.31 | .32 | .35 | −.02 | −.02 | .18 | .11 | .11 | .12 | .06 | .12 | −.54 | 1.00 | |||||
| CNA HPRD | .05 | −.06 | −.05 | −.10 | −.01 | .16 | .24 | .05 | .24 | .05 | .06 | .00 | .02 | .02 | −.16 | −.19 | .02 | 1.00 | ||||
| Licensed nurse HPRD | .02 | −.08 | −.10 | −.09 | −.04 | .16 | .32 | .11 | .39 | .08 | .17 | −.01 | −.06 | −.03 | −.23 | −.25 | .10 | .60 | 1.00 | |||
| Physician extender | −.04 | .04 | −.03 | −.01 | −.01 | .00 | .02 | −.02 | −.05 | .05 | −.02 | −.01 | .05 | .08 | .07 | .01 | .02 | −.01 | −.05 | 1.00 | ||
| Specialty Care Unit | .01 | −.04 | .04 | −.01 | −.10 | −.07 | −.12 | .19 | .02 | −.04 | −.12 | −.06 | .11 | .07 | .04 | −.01 | −.04 | −.03 | −.01 | .11 | 1.00 | |
| Hospital beds/ 1,000 65+ | −.02 | −.01 | −.13 | −.03 | .30 | .00 | .01 | −.01 | .02 | −.03 | −.02 | .01 | −.19 | −.06 | .04 | .09 | −.07 | −.03 | −.01 | .02 | −.02 | 1.00 |
Notes: N = 681 nursing homes and 5,153 facility year observations; ADL = activities of daily living; RUGS = Resource Utilization Groups; CPS = Cognitive Performance Scale; UTI = urinary tract infection; CHF = congestive heart failure; DNR = do not resuscitate; DNH = do not hospitalize; SCU = Special Care Unit; FTEs = full-time equivalent; CNA = certified nursing assistant; HPRD = hours per resident day.
Table 2.
Characteristics of Florida Nursing Homes in Sample
| Variable | Definition | Data source | Mean (SD) or % | |
|---|---|---|---|---|
| Main independent variables | ||||
| Licensed nurse retention rate | Licensed nurse yearly retention rate | FNHSR | 64.40 | (16.09) |
| Licensed nurse turnover rate | Licensed nurse yearly turnover rate | FNHSR | 34.73 | (20.63) |
| Resident characteristics | ||||
| Age | Mean age at assessment across residents in facility | MDS | 80.97 | (5.91) |
| Female | Percent of female residents in facility | MDS | 70.43 | (12.02) |
| Black | Percent of non-Hispanic black residents in facility | MDS | 14.47 | (16.57) |
| ADL Score | Mean “Long ADL” score in facility last 7 days | MDS | 16.68 | (2.44) |
| RUGS score | Mean RUGS value across residents in facility | MDS | .81 | (.06) |
| High CPS | Percent of residents with high CPS (5,6) in facility | MDS | 22.00 | (12.22) |
| Percent on ventilator | Percent of residents on a ventilator | MDS | .22 | (1.31) |
| Percent with UTI | Percent of residents with a UTI | MDS | 10.47 | (5.86) |
| Percent with catheter | Percent of residents with a catheter | MDS | 7.43 | (4.86) |
| Percent with CHF | Percent of residents with CHF | MDS | 15.63 | (7.19) |
| DNR | Percent of residents with DNR order in facility | MDS | 47.68 | (20.21) |
| DNH | Percent of residents with DNH order in facility | MDS | 1.57 | (3.90) |
| Facility characteristics | ||||
| Total beds | Total number of licensed beds in facility | OSCAR | 122.41 | (46.63) |
| Chain membership | Facility is part of a chain | OSCAR | 58.05% | |
| For profit ownership | Facility is run for profit | OSCAR | 73.93% | |
| Occupancy | Percent occupied beds | OSCAR | 88.30 | (11.33) |
| Medicaid | Percent Medicaid primary payer | OSCAR | 57.30 | (20.79) |
| Medicare | Percent Medicare primary payer | OSCAR | 18.73 | (11.99) |
| Physician extender | Any physician extender FTEs | OSCAR | 45.34% | |
| SCU | Facility has any SCUs (excluding ventilator) | OSCAR | 23.15% | |
| CNA HPRD | Certified nursing assistant hours per resident day | FNHSR | 2.78 | (.32) |
| Licensed nurse HPRD | Licensed nurse hours per resident day | FNHSR | 1.19 | (.30) |
| Market characteristics | ||||
| Urban | Rural/urbandichotomy | ARF | 91.58% | |
| Hospital beds/1,000 65+ | No. of hospital beds/1,000 population aged 65+ in county | ARF | 20.04 | (12.31) |
Note: N = 681 nursing homes and 5,153 facility year observations; SD = Standard deviation; FNHSR = Florida Nursing Home Staffing Report; MDS = minimum data set; ADL = activities of daily living; RUGS = Resource Utilization Groups; CPS = Cognitive Performance Scale; UTI = urinary tract infection; CHF = congestive heart failure; DNR = do not resuscitate; DNH = do not hospitalize; OSCAR = Online Survey, Certification and Reporting data set; SCU = Special Care Unit; FTEs = full-time equivalent; CNA = certified nursing assistant; HPRD = hours per resident day; ARF = Area Resource File.
Results from the two-way fixed effect models indicate that a facility’s licensed nurse retention rate is significantly associated with the 30-day rehospitalization rate (est. = −.02, p = .04) controlling for resident, facility, and market characteristics (see Table 3). To facilitate interpretation, we also converted the licensed nurse retention rate into quartiles. In the same covariate-adjusted regression model, we found that NHs with licensed nurse retention in the highest quartile had a rehospitalization rate that was about 1 percentage point lower than NHs with a retention rate less than 55%. Licensed nurse turnover is not significantly related to the 30-day rehospitalization rate. Additional results from the model indicate that facilities with a higher percentage of black residents, younger residents, and those with a lower percent of Medicaid residents have a higher 30-day rehospitalization rate.
Table 3.
Two-way Fixed Effects Model Results: Relationships Among Licensed Nurse Retention, Turnover, and 30-Day Rehospitalization Rates (2002–2009)
| Est | Std err | p value | |
|---|---|---|---|
| Main independent variables | |||
| Licensed nurse retention rate | −.02 | .01 | .04 |
| Licensed nurse turnover rate | .00 | .01 | .98 |
| Control variables | |||
| Resident welfare | |||
| Average age | −.14 | .06 | .02 |
| Percent female | −.01 | .02 | .70 |
| Percent black | .07 | .02 | .00 |
| Average ADL Score | .03 | .09 | .78 |
| Average RUGS score | 4.92 | 3.41 | .15 |
| Percent high CPS | −.01 | .01 | .62 |
| Percent on ventilator | −.14 | .11 | .21 |
| Percent with UTI | −.02 | .02 | .39 |
| Resident care practices | |||
| Percent with catheter | −.03 | .03 | .28 |
| Percent with CHF | .05 | .02 | .05 |
| Residents’ preferences | |||
| Percent with DNR | −.02 | .01 | .10 |
| Percent with DNH | .03 | .05 | .47 |
| Financial factors | |||
| Occupancy | −.007 | .01 | .59 |
| Percent Medicaid | −.03 | .01 | .01 |
| Percent Medicare | .01 | .02 | .42 |
| Facility resources | |||
| CNA HPRD | .33 | .61 | .59 |
| Licensed nurse HPRD | .56 | .61 | .36 |
| Physician extender | .06 | .22 | .79 |
| Specialty Care Unit | .12 | .38 | .75 |
| Hospital Beds/1,000 65+ | .02 | .03 | .60 |
Notes: Robust standard errors adjusted for clustering within facility. Year and facility dummy variables not shown. The first year, 2002, was the reference. N = 681 nursing homes and 5,153 facility year observations; Est. = Estimate; Std Err = robust standard error; ADL = activities of daily living; RUGS = Resource Utilization Groups; CPS = Cognitive Performance Scale; UTI = urinary tract infection; CHF = congestive heart failure; DNR = do not resuscitate; DNH = do not hospitalize; OSCAR = Online Survey Certification and Reporting data set; CNA = certified nursing assistant; HPRD = hours per resident day.
Sensitivity analyses were conducted to ensure that the observed relationship between retention and hospitalization rate was causal (higher retention was related to decreased rehospitalizations). Results (not presented) indicate that higher licensed nurse retention the year prior is associated with a decreased rehospitalization rate (est. = −.02, p = .02). In the lagged analyses, licensed nurse turnover was again not significantly associated with the facility’s rehospitalization rate.
Discussion
This study is among the first in examining both the retention and the turnover rate of licensed nurses to determine which one is the most important in reducing rehospitalizations. Results from our study partially confirm our hypotheses that licensed nurse turnover and retention are related to the rehospitalization rate of NHs. Specifically, our results indicate that licensed nurse retention is related to the 30-day rehospitalization rate, although licensed nurse turnover had no effect on rehospitalization. This partially confirms our hypothesis that staffing characteristics influencing residents’ welfare and providers’ preferences for hospitalization, which are approximated by the licensed nurse retention rate, are related to the 30-day rehospitalization rate of NH residents. In concrete terms, the average NH in Florida, over the study period, had approximately 108 residents and 1.24 hospitalizations per person year. With an average rehospitalization rate of 21%, approximately 28 residents were rehospitalized in each NH for each year. Therefore, if a facility increased their retention rate by 10%, they would reduce their rehospitalization rate to approximately 26 residents per year.
Our findings indicate that licensed turnover is not significantly related to rehospitalization but, contrary to our hypothesis, is consistent with another study measuring the relationship of licensed nurse turnover to potentially preventable hospitalizations (Young, Barhydt, Broderick, Colello, & Hannan, 2010). Turnover presumably counts the churning of people in to and out of a small number of positions and does not characterize the stability of staff in a facility. Rather, it can measure the instability of a particular position, which is less likely to affect a large portion of the facility. It is likely that retention is a better measure for licensed nurses as it reflects the organizational experience of nursing staff. Retention of licensed nursing staff fosters organization-specific knowledge and experience, thereby improving quality. Having nursing staff familiar with the organization-specific policies and procedures, the type of postacute care that particular facility provides, the discharge and follow-up process with hospitals, and the signs and symptoms of deteriorating health can decrease the rehospitalization rate (Ouslander et al., 2011). Therefore, our results indicate that NHs need to focus on retaining licensed staff in an effort to reduce the 30-day rehospitalization rate.
The findings from this analysis have implications for NH administrators, owners of NHs and chains, state legislators, policymakers, and industry professionals. Several studies on turnover of NH staff have been stimulated by the negative association that is believed to exist between the turnover and the quality of care (Castle, 2001; Castle & Engberg, 2008; Weech-Maldonado et al., 2004; Zimmerman et al., 2002), as well as the expenses associated with recruiting and training new staff (Mukamel et al., 2009; Seavey, 2004). Many have asserted that reducing turnover is the key to ensuring high quality of care (Staw, 1980). However, our results indicate that it is licensed nurse retention, as opposed to licensed nurse turnover, that is related to the 30-day rehospitalizations. In an industry where turnover is inevitable, it is worthwhile for administrators to focus on strategies to retain their skilled workers in an effort to decrease their rehospitalization rate.
Improving licensed nurse retention would have financial benefit for NH administrators and owners of NHs. By increasing licensed nurse retention, providers could cut down on the economic costs of advertising, recruiting, hiring, and training new staff. While there is no general consensus on the expense of replacing a licensed nurse, it is believed to be close to 25% of the annual compensation or more (O’Malley, 2000). However, Mukamel and colleagues showed that the association between direct care staff turnover and costs is negative (Mukamel et al., 2009), that is, on net, turnover is associated with cost savings. Turnover of direct care staff has persisted for decades and suggests that for the majority of NHs it is part of their cost minimizing strategy. However, the CMS Nursing Home Value-Based Purchasing demonstration (White et al., 2009) provides additional payments to NHs that achieve a higher performance or improvement on select quality measures. Three of these measures include nursing staff turnover, retention, and potentially avoidable hospitalizations. Thereby, with this new financial quality incentive, it may be worthwhile for NHs to explore personnel strategies to increase retention, decrease turnover, and, consequently, reduce the number of rehospitalizations. Furthermore, Medicare reimbursement is a significant portion of NH revenue and preferred to Medicaid reimbursement. It might be a competitive advantage to change facility practice in an effort to reduce rehospitalizations, as long as it is appropriate, because NHs with lower readmissions are also more likely to be attractive to hospitals. Medicare payment bundling is one of a number payment reforms aimed to decrease federal spending on health care (Guterman, Davis, Schoen, & Stremikis, 2009). It would be in the postacute providers’ best interests to take steps in positioning themselves to become the most desirable partner for a hospital if bundled payment becomes a reality.
In addition, Section 3025 of the Patient Protection and Affordable Care Act provides that beginning on October 1, 2012, hospitals that have a high rate of Medicare readmissions will be subjected to Medicare payment reductions. It is estimated that hospitals that report higher-than-expected 30-day readmission rates for patients who had been hospitalized with heart attacks, heart failure, and pneumonia could face Medicare reimbursement reductions anywhere from 1% in the first year to 3% by 2015. Therefore, SNFs that want to form preferred provider relationships should focus on decreasing their hospital readmission rate in order to attract hospitals discharging Medicare patients. This would be reflected through the capability of SNFs to care for patients in their own setting instead of readmitting that patient in hospital likely requiring an experienced, highly qualified nursing staff.
The magnitude of our finding is substantial when we examine the potential savings to the Medicare program. Assuming an average Medicare Diagnosis-Related Group payment per hospitalization of $5,000, findings from our study indicate that if the State of Florida increased their licensed nurse retention rate by 10%, there would be a reduction of 1,352 rehospitalizations and a savings to Medicare of approximately $6,767,000. Medicare payment reforms such as the value-based purchasing and bundled payments for episodes of care may change the current incentives to rehospitalize residents. However, this could result in the quality of care problems if NHs lack resources to provide care for these patients by having inexperienced nurse or shortages of licensed nurse. It is important that experienced licensed nurses are available for surveillance and medication management: two issues important in preventing rehospitalization. Therefore, it is important that support and resources are provided to facilities to retain their licensed nurses in an effort to decrease the rehospitalization rate.
Limitations
It is necessary to note the limitations of our study. Although we understand that the job duties of RNs and LPNs vary, we were limited to examining combined licensed nurse staffing, turnover, and retention because of how the Florida data were collected. Future research would benefit by examining the differences between RN and LPN staffing, turnover, and retention and the relation of each to rehospitalization. In addition, although we use an accepted measure of turnover, our measure is conservative because it only takes into account individuals who were terminated and who had been employed for at least 3 months. Also, we are unable to distinguish between voluntary and involuntary turnover, and this may have different effects on quality. Our measure of retention is only reported by the number of individuals who have been in the facility for at least a year. Therefore, we are unable to track tenure of individuals. Future research should look at tenure and stability of nursing staff and the relationship to rehospitalizations. Furthermore, we are unable to include other staffing factors that may be important in terms of influencing rehospitalization, such as the use of agency staff and the educational background of staff.
Because we examine the facility’s 30-day rehospitalization rate for residents admitted to a hospital from a NH, we are unable to determine if differences exist between those admitted from the community and those long-stay residents who were returning to the NH. Providers may have different incentives to re-hospitalize certain types of residents, and future research should examine the relationships of licensed nurse turnover and retention to the rehospitalization rates of the two separate populations. Furthermore, appropriate versus inappropriate rehospitalization cannot be addressed in the analyses. Therefore, future research should examine the rates of appropriate versus avoidable rehospitalizations and how they relate to licensed nurse turnover. The other major drawback of using the facility-level data from ltcfocus.org is the inability to risk adjust hospitalizations at the person level. Future research would benefit by examining the rates of risk-adjusted rehospitalization rates.
Although Florida is the fourth largest state, a state with the highest proportion of elders, a state with more than 75,000 NH residents (Harrington, Carrillo, & Blank, 2008), and a state with higher staffing than average (Hyer et al., 2011), it is still a single state, and therefore, the results of this study may not be generalizable. It is our hope that despite these limitations, our results will provide grounds for future research and improvement in this area.
Conclusion
Hospital discharges to SNF occur for a large number of Medicare beneficiaries with one fourth of these patients readmitted to the hospital within 30 days. The results from this study indicate that licensed nurse retention is related to the 30-day rehospitalization rates of facilities and highlight the need for NH administrators and policy makers to target improvements in licensed nurse retention. Additionally, we must consider that licensed nurse turnover is not nearly as important to rehospitalization rates as licensed nurse retention, and, therefore, future research should focus on the measures of retention for understanding the staffing/quality relationship.
Funding
This work was supported by the National Institute on Aging (P01AG027296) and the Agency for Healthcare Research and Quality (5T32HS000011).
References
- Alexander J. A., Bloom J. R., Nuchols B. A. (1994). Nursing turnover and hospital efficiency: An organizational level analysis. Industrial Relations. 33, 505–520 [Google Scholar]
- Bostick J. E., Rantz M. J., Flesner M. K., Riggs C. J. (2006). Systematic review of studies of staffing and quality in nursing homes. Journal of the American Medical Directors Association. 7, 366 37610.1016/j.jamda.2006.01.024 [DOI] [PubMed] [Google Scholar]
- Brannon D., Zinn J. S., Mor V., Davis J. (2002). An exploration of job, organizational, and environmental factors associated with high and low nursing assistant turnover. The Gerontologist. 42, 159–16810.1093/geront/42.2.159 [DOI] [PubMed] [Google Scholar]
- Cai S., Mukamel D. B., Veazie P., Katz P., Temkin-Greener H. (2011). Hospitalizations in nursing homes: Does payer source matter? Evidence from New York State. Medical Care Research and Review. 68, 559–57810.1177/1077558711399581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter M. W., Porell F. W. (2003). Variations in hospitalization rates among nursing home residents: The role of facility and market attributes. The Gerontologist. 43, 175–19110.1093/geront/43.2.175 [DOI] [PubMed] [Google Scholar]
- Carter M. W., Porell F. W. (2005). Vulnerable populations at risk of potentially avoidable hospitalizations: The case of nursing home residents with Alzheimer’s disease. American Journal of Alzheimers Disease and Other Dementias. 20, 349–35810.1177/153331750502000605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle N. G. (2001). Administrator turnover and quality of care in nursing homes. The Gerontologist. 41, 757–76710.1093/geront/41.6.757 [DOI] [PubMed] [Google Scholar]
- Castle N. G. (2006). Measuring staff turnover in nursing homes. The Gerontologist. 46, 210–21910.1093/geront/46.2.210 [DOI] [PubMed] [Google Scholar]
- Castle N. G., Anderson R. A. (2011). Caregiver staffing in nursing homes and their influence on quality of care: Using dynamic panel estimation methods. Medical Care. 49, 545–55210.1097/MLR.0b013e31820fbca9 [DOI] [PubMed] [Google Scholar]
- Castle N. G., Engberg J. (2005). Staff turnover and quality of care in nursing homes. Medical Care. 43, 616–626 [DOI] [PubMed] [Google Scholar]
- Castle N. G., Engberg J. (2008). Further examination of the influence of caregiver staffing levels on nursing home quality. The Gerontologist. 48, 464–47610.1093/geront/48.4.464 [DOI] [PubMed] [Google Scholar]
- Castle N. G., Engberg J., Men A. (2007). Nursing home staff turnover: Impact on nursing home compare quality measures. The Gerontologist. 47, 650–66110.1093/geront/47.5.650 [DOI] [PubMed] [Google Scholar]
- Castle N. G., Mor V. (1996). Hospitalization of nursing home residents: A review of the literature, 1980–1995. Medical Care Research and Review. 53, 123–14810.1177/107755879605300201 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services (2010). National health expenditure database Retrieved from http://www.cms.hhs.gov/NationalHealthExpendData/downloads/tables.pdf
- Decker F. H. (2006). Nursing staff and the outcomes of nursing home stays. Medical Care. 44, 812–82110.1097/01.mlr.0000218832.24637.2e [DOI] [PubMed] [Google Scholar]
- Decker F. H. (2008). The relationship of nursing staff to the hospitalization of nursing home residents. Research in Nursing and Health. 31, 238–25110.1002/nur.20249 [DOI] [PubMed] [Google Scholar]
- Donoghue C. (2010). Nursing home staff turnover and retention: An analysis of national level data. Journal of Applied Gerontology. 29, 89–10610.1177/0733464809334899 [Google Scholar]
- Fries B. E., Schneider D. P., Foley W. J., Gavazzi M., Burke R., Cornelius E. (1994). Refining a case-mix measure for nursing homes: Resource utilization groups (RUG-III).. Medical Care. 32, 668–685 [DOI] [PubMed] [Google Scholar]
- Grabowski D. C., Stewart K. A., Broderick S. M., Coots L. A. (2008). Predictors of nursing home hospitalization: A review of the literature. Medical Care Research and Review. 65, 3–3910.1177/1077558707308754 [DOI] [PubMed] [Google Scholar]
- Gruneir A., Miller S. C., Feng Z., Intrator O., Mor V. (2008). Relationship between state Medicaid policies, nursing home racial composition, and the risk of hospitalization for black and white residents. Health Services Research. 43, 869–88110.1111/j.1475-6773.2007.00806.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guterman S., Davis K., Schoen C., Stremikis K. (2009, March). Reforming provider payment: Essential building block for health reform. The Commonwealth Fund [Google Scholar]
- Halbur B. T., Fears N. (1986). Nursing personnel turnover rates turned over: Potential positive effects on resident outcomes in nursing homes. The Gerontologist. 26, 70–7610.1093/geront/26.1.70 [DOI] [PubMed] [Google Scholar]
- Harrington C., Carrillo H., Blank B. W. (2008). Nursing facilities, staffing, residents and facility deficiencies, 2001 through 2007. San Francisco, CA: Department of Social and Behavioral Sciences, University of California; [Google Scholar]
- Hawes C., Morris J. N., Phillips C. D., Mor V., Fries B. E., Nonemaker S. (1995). Reliability estimates for the minimum data set for nursing home resident assessment and care screening (MDS). The Gerontologist. 35, 172–17810.1093/geront/35.2.172 [DOI] [PubMed] [Google Scholar]
- Horn S. D., Sharkey S. S., Hudak S., Smout R. J., Quinn C. C., Yody B., et al. (2010). Beyond CMS quality measure adjustments: Identifying key resident and nursing home facility factors associated with quality measures. Journal of the American Medical Directors Association. 11, 500–50510.1016/j.jamda.2009.10.008 [DOI] [PubMed] [Google Scholar]
- Hyer K., Thomas K. S., Branch L., Harman J., Weech-Maldonado R., Johnson C. E. (2011). The influence of nurse staffing levels on quality of care in nursing homes. The Gerontologist. 51, 610–61610.1093/geront/gnr050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O., Castle N. G., Mor V. (1999). Facility characteristics associated with hospitalization of nursing home residents: Results of a national study. Medical Care. 37, 228–237 [DOI] [PubMed] [Google Scholar]
- Intrator O., Grabowski D. C., Zinn J., Schleinitz M., Zhanlian F., Miller S., et al. (2007). Hospitalization of nursing home residents: The effects of states’ Medicaid payment and bed-hold policies. Health Services Research. 42, 1651–167110.1111/j.1475-6773.2006.00670.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O., Hiris J., Berg K., Miller S. C., Mor V. (2011). The residential history file: Studying nursing home residents’ long-term care histories. Health Services Research. 46, 120–13710.1111/j.1475-6773.2010.01194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O., Mor V. (2004). Effect of state Medicaid reimbursement rates on hospitalizations from nursing homes. Journal of the American Geriatric Society. 52, 393–39810.1111/j.1532-5415.2004.52111.x [DOI] [PubMed] [Google Scholar]
- Intrator O., Zinn J., Mor V. (2004). Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. Journal of the American Geriatrics Society. 52, 1730–173610.1111/j.1532-5415.2004.52469.x [DOI] [PubMed] [Google Scholar]
- Kramer A. M., Fish R. (2001). The relationship between nurse staffing levels and the quality of nursing home care.. Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes: Phase II Final Report.. Cambridge, MA: Abt Associates for the Centers and Medicare and Medicaid Services; [Google Scholar]
- MedPAC (Medicare Payment Advisory Commission) (2006). A data book: Healthcare spending and the Medicare program. Washington, DC: Medicare Payment Advisory Commission; [Google Scholar]
- Mor V., Intrator O., Feng Z., Grabowski D. (2010). The revolving door of rehospitalization from skilled nursing facilities. Health Affairs. 29, 57–6410.1377/hlthaff.2009.0629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J. N., Fries B. E., Mehr D. R., Hawes C., Philips C., Mor V., et al. (1994). MDS cognitive performance scale. Journal of Gerontology, Medical Sciences. 49, M174–M18210.1093/geronj/49.4.M174 [DOI] [PubMed] [Google Scholar]
- Mukamel D. B., Spector W. D., Limcangco R., Wang Y., Feng Z., Mor V. (2009). The costs of turnover in nursing homes. Medical Care. 47, 1039–104510.1097/MLR.0b013e3181a3cc62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley M. N. (2000). Creating commitment: How to attract and retain talented employees by building relationships that last. New York: Wiley; [Google Scholar]
- Ouslander J. G., Lamb G., Tappen R., Herndon L., Diaz S., Roos B. A., et al. (2011). Interventions to reduce hospitalizations from nursing homes: Evaluation of the INTERACT II collaborative quality improvement project. Journal of the American Geriatrics Society. 59, 745–75310.1111/j.1532-5415.2011.03333.x [DOI] [PubMed] [Google Scholar]
- Saliba D., Kington R., Buchanan J., Bell R., Wang M., Lee M., et al. (2000). Appropriateness of the decision to transfer nursing facility residents to the hospital. Journal of the American Geriatric Society. 48, 154–163 [DOI] [PubMed] [Google Scholar]
- Seavey D. (2004, October). The cost of frontline turnover in long-term care. (Practice & Policy Report: 1–3) New York: Better Jobs Better Care; [Google Scholar]
- StataCorp (2009). Stata statistical software: Release 11. College Station, TX: StataCorp LP; [Google Scholar]
- Staw B. M. (1980). The consequences of turnover. Journal of Occupational Behavior. 1, 253–273 [Google Scholar]
- Stone J., Hoffman G. J. (2010). Medicare hospital readmissions: Issues, policy options and PPACA. In Service C. R. (Ed.), CRS report for congress. Washington, DC: Congressional Research Service; [Google Scholar]
- Weech-Maldonado R., Meret-Hanke L., Neff M. C., Mor V. (2004). Nurse staffing patterns and quality of care in nursing homes. Health Care Management Review. 29, 107–116 [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R., Neff G., Mor V. (2003). Does quality of care lead to better financial performance?: The case of the nursing home industry. Health Care Management Review. 28, 201–216 [DOI] [PubMed] [Google Scholar]
- White A., Hurd D., Moore T., Kramer A., Hittle D., Fish R. (2009). Nursing Home Value-Based Purchasing Demonstration Contract # 500-00-0032, T.O. #1 Design Refinements. Cambridge, MA: Abt Associates; [Google Scholar]
- Young Y., Barhydt N. R., Broderick S., Colello A. D., Hannan E. L. (2010). Factors associated with potentially preventable hospitalization in nursing home residents in New York State: A survey of directors of nursing. Journal of the American Geriatrics Society. 58, 901–90710.1111/j.1532-5415.2010.02804.x [DOI] [PubMed] [Google Scholar]
- Zimmerman S., Gruber-Baldini A. L., Hebel J. R., Sloane P. D., Magaziner J. (2002). Nursing home facility risk factors and hospitalization: Importance of registered nurse turnover, administration, and social factors. Journal of the American Geriatrics Society. 50, 1987–199510.1046/j.1532-5415.2002.50610.x [DOI] [PubMed] [Google Scholar]