Abstract
Purpose of the Study: While theories of job turnover generally assume a strong correlation between job satisfaction, intention, and retention, such models may be limited in explaining turnover of low-wage health care workers. Low-wage workers likely have a lower ability to act on their employment intentions or plans due to a lack of resources that serve to cushion higher wage workers. In this study, we examine the relationship between job satisfaction, intention, and retention of nursing assistants in nursing homes and the role that “contingency factors” play in employment intentions and retention. We conceptualize “contingency factors” as resource-related constraints (e.g., being a single mother) that likely influence employment trajectories of individuals but can be independent of job satisfaction or intent. Design and Methods: We use survey data from 315 nursing assistants in 18 nursing homes in a U.S. southern state to model employment intentions and retention. Results: We find that job satisfaction and other perceived job characteristics (e.g., workload and perceived quality of care) are significant predictors of an individual’s intent to stay in their job, the occupation of nursing assistant, and the field of long-term care. However, we find that job satisfaction and employment intentions are not significant predictors of retention. Instead, “contingency factors” such as being a primary breadwinner and individual characteristics (e.g., tenure and past health care experience) appear to be stronger factors in the retention of nursing assistants. Implications: Our findings have implications for understanding turnover among low-wage health care workers and the use of proxies such as employment intentions in measuring turnover.
Key Words: Caregiving—formal, Workforce issues, Long-term care
As demonstrated by many scholars of the low-wage workforce, any account of the employment decisions and pathways of low-wage workers must explore the constraints and “push” factors that shape their employment trajectories; see reviews by Newman and Massengill (2006) and O’Connor (2000). Childcare, transportation, or inflexible hours may all interfere with a worker’s ability to stay in their job, even if they enjoy their work and intend to stay with their employer. However, these insights about the causes of turnover among low-wage workers have rarely been incorporated into quantitative studies of retention of health care workers. Most studies have focused heavily on job satisfaction, job quality, and employment intentions as predictors of retention. A recent exception (Mittal, Rosen, & Leana, 2009) is a qualitative study that explored the personal and financial constraints faced by low-wage workers in maintaining employment. Further, studies of the job experiences of health care workers based on one-time surveys have been constrained to use intent to stay as a proxy for retention (Bishop, Weinberg, Leutz, Dossa, & Pfefferle, 2008; Brannon, Barry, Kemper, Schreiner, & Vasey, 2007; Decker, Harris-Kojetin, & Bercovitz, 2009), but given the effects of other personal and resource-related circumstances on turnover, using these measures as proxies for retention may not be appropriate for low-wage populations.
We examine employment expectations (i.e., intent to stay in one’s current position, occupation, or field) and retention of nursing assistants in nursing homes, an overwhelmingly female workforce with wages that generally fall only a few dollars above the minimum wage. With increased concerns about the availability and stability of the health care workforce, there has been substantial growth in research on job satisfaction and turnover intent among nursing assistants (Appelbaum, Berg, Frost, & Preuss, 2003; Banaszak-Holl & Hines, 1996; Bishop et al., 2008; Bishop, Squillace, Meagher, Anderson, & Wiener, 2009; Brannon, Zinn, Mor, & Davis, 2002; Decker et al., 2009; Squillace et al., 2009). However, only a few studies have examined actual retention of these workers and the relationship between job satisfaction, intent to stay, and retention (Castle, Engberg, Anderson, & Men, 2007; Rosen, Stiehl, Mittal, & Leana, 2011).
While job satisfaction and employment intentions are factors in nursing assistant turnover, we expect that the relationship between job satisfaction, intent to stay, and retention is weaker for nursing assistants compared with workers with higher socio-economic status. The impact of a lack of resources on employment may be independent of an individual’s level of job satisfaction, as well as an individual’s intent to stay because individuals often cannot predict when financial, personal, or family constraints will surface. In this study, we refer to these constraints as “contingency factors,” a term that we have borrowed from sociologist Howard Becker. In an essay on organizational commitment, Becker (1960) notes that a person’s present employment activity may be constrained by situational or contextual factors such as cultural expectations (e.g., switching jobs too often may be questioned) or impersonal bureaucratic arrangements (e.g., one cannot leave a job without losing money in a pension fund). We expand Becker’s term, which he primarily applied in his study of middle-class professional men, by extending the concept to include resource-related constraints (as opposed to Becker’s focus on cultural expectations and bureaucratic arrangements) faced by health care workers in a low-wage, feminized occupation.
“Contingency factors” include both financial and personal circumstances, reflecting the vulnerability of low-waged workers to personal and family issues for which they have no cushion of wealth, insurance or safety net protection. We ask, are job satisfaction and employment intentions reliable predictors of retention for low-wage health care workers, or is turnover better explained by financial and personal constraints experienced by these workers? We explore the role that “contingency factors” play in the employment decisions of nursing assistants compared with their overall job satisfaction and employment intentions.
Nursing Assistant Demographics
Nursing assistants comprise a particularly vulnerable segment of the population. Wages for nursing assistants are very low, and benefits are usually minimal (Smith & Baughman, 2007; Temple, Dobbs, & Andel, 2010). Like many other low-wage jobs in the secondary labor market, there are few opportunities for advancement (Baughman & Smith, 2011; Hunter, 2000; Kalleberg, 2011) and minimal rewards for tenure or work experience (Squillace et al., 2009). Nursing assistants are overwhelmingly women, and racial and ethnic minorities are over-represented (Glenn, 1992; Squillace et al., 2009). Twenty-eight percent of nursing assistants working in nursing homes are single mothers compared with 14% of all female workers (Smith & Baughman, 2007). Single mothers and primary breadwinners in low-wage jobs face tremendous challenges in supporting their families and significant constraints in their employment choices (Budig & England, 2001; Edin & Kefalas, 2005).
As “bad jobs,” nursing assistant jobs are not generally supportive of single mothers (Kalleberg, 2009). Nursing assistants often have to work irregular hours, late-night shifts, and weekends, and many nursing assistant jobs do not offer sick days or paid leave. Shift times are extremely rigid, and workers can be fired for clocking-in even a few minutes late (Diamond, 1995; Lopez, 2006). Many nursing assistants are also current or former recipients of public assistance, and previous research has also shown that welfare recipients face many employment challenges, including meeting financial obligations in a low-wage job, finding and paying for childcare, and transportation problems (Edin & Lein, 1997; Holzer, Stoll, & Wissoker, 2004).
Understanding Nursing Assistant Turnover
Job satisfaction and intent to stay among nursing assistants have been studied extensively, especially in long-term care settings (Bishop et al., 2009; Brannon et al., 2007; Ejaz, Noelker, Menne, & Bagaka’s, 2008). While many studies have linked job satisfaction and overall job quality with employment intentions and job commitment (Bishop et al., 2008; Decker et al., 2009), very few studies have explored actual retention of frontline workers at the individual level, and these studies of nursing assistant turnover have found somewhat conflicting results. For example, Castle and colleagues (2007) found that job satisfaction and one measure of intent to leave (out of three) were significant predictors of turnover, but a recent study by Rosen and colleagues (2011) found that job satisfaction was not a predictor of turnover, while turnover intentions were a significant predictor of turnover. Further, neither of these studies include many resource-related characteristics of nursing assistants such as single motherhood or receiving public assistance that may serve as proxies for a constellation of contributing factors to actual retention in multivariate models of turnover. Past studies of nursing assistant turnover have focused heavily on an individual’s satisfaction or dissatisfaction with their current job and their intentions for remaining in their position (Castle et al., 2007; Kiyak, Namazi, & Kahana, 1997; Rosen et al., 2011).
However, models that focus on the cognitive processes of job satisfaction and intent to stay or leave may neglect to take into account unforeseen circumstances that are unrelated to the job experience or employment intentions (Griffeth, Hom, & Gaertner, 2000; Lee, Gerhart, Weller, & Trevor, 2008; Steel, 2002). Turnover scholars Lee and colleagues (2008) propose alternative pathways leading to turnover which incorporate “shocks,” such as an unanticipated job offer or family-related reasons for quitting, where job satisfaction plays a smaller role in predicting turnover. They found that unanticipated job offers and family-related reasons for quitting accounted for nearly half of the turnover in their sample, suggesting that “shocks” may be more the rule than the exception. Low-wage workers such as nursing assistants are particularly vulnerable to employment “shocks” for many of the reasons discussed previously, such as difficulty in finding and paying for childcare or transportation problems. For example, a recent study conducted by Rosen and colleagues (2011) found that a change in family situation was an important reason for 30%–40% of workers who switched jobs or left the occupation of nursing assistant.
Summary and Conceptual Model
To summarize, we have two primary aims in this study. First, we examine the relationship between job satisfaction, intent to stay, and retention among a population of low-wage health care workers. We expect that the relationship between these three outcomes will be weaker in our study population than has been found in studies of the general workforce, such as those reviewed previously. Second, we anticipate that other personal and job circumstances may play an important role in employment decisions and action, and these “contingency factors” may have a direct effect on retention and turnover that is independent of job satisfaction or intent to stay. We argue that nursing assistants have less discretion to act on their preferences or intentions because of their limited financial, personal, and job-related resources. Without resources (e.g., health insurance, money to fix the family car, and money or family to provide sick child care), a large range of “shocks” that do not generally cause turnover could trigger a turnover event for low-wage workers. A conceptual model of the proposed relationships between “contingency factors,” job satisfaction, employment intentions, and retention is shown in Figure 1.
Figure 1.
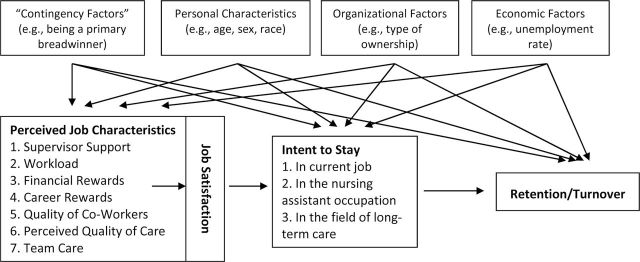
A conceptual model of determinants of nursing assistant retention/turnover.
Methods
Data
This study utilizes data collected from surveys completed by key informants (supervisors or administrators) and nursing assistants at 18 nursing facilities in a southern U.S. state in 2004 and 2005. Key informants were asked to complete an organizational management survey, and the response rate was 100% (n = 18). The mean response rate for nursing assistants was 95% (n = 449). The number of respondents at each of the 18 facilities included in this study ranges from 10 to 48 nursing assistants. Participating organizations for this study were recruited from a waiting list for a workforce intervention for nursing assistants; individual respondents were recruited from all three shifts in a day-long facility-based data collection effort. However, all of the variables being examined in this study, except for retention, were collected before the implementation of the intervention. Paper surveys were administered to respondents at their worksites.
The analytic sample for this study is of 315 respondents, indicating that 30% of the observations have missing data for at least one of the variables of interest. The respondents in the analytic sample are older and have worked in their current positions longer than the dropped sample, are more likely to report higher quality of care by coworkers, and are less likely to be a primary breadwinner, but they do not differ significantly on any of the dependent variables (as determined by logit models). Table 1 contains summary statistics for the analytic sample.
Table 1.
Survey Items and Sample Statistics
| Variable | Description | Mean (SD) or percent | Range |
|---|---|---|---|
| Outcome variables | |||
| Intent: current job | I intend to remain in my current position for the near future (4-point scale, where strongly agree = 4) | 2.84 (.93) | 1-4 |
| Intent: nursing assistant | Three years from now, I would still like to be working as a nursing assistant (4-point scale, where strongly agree = 4) | 2.59 (1.1) | 1-4 |
| Intent: stay in field | Do you think you will be working in the field of LTC 3 years from now? (1 = yes) | 0.61 (.49) | 0-1 |
| Retention | Still employed at facility 1 year later (1 = yes) | 0.86 (.33) | 0-1 |
| Job satisfaction and perceived job characteristics (sample items only) | |||
| Job satisfaction (four items; alpha = 0.79) | On a scale of 1-10, with 1 being very dissatisfied and 10 being very satisfied, how satisfied are you with your current car- egiving position? | 7.19 (1.77) | 1-10 |
| My job measures up to the sort of job I wanted when I took it (Strongly Disagree, Disagree, Agree, and Strongly Agree) | |||
| Supervisor support (eight items; alpha = 0.91) | My supervisor treats me as an equal member of the health care team | 1.35 (.56) | 0-2 |
| My supervisor listens carefully to my observations and opinions | |||
| Workload (three items; alpha = 0.76) | I am physically exhausted at the end of a shift | 2.74 (.59) | 1-4 |
| I am asked to do more work than I can handle | |||
| Financial rewards (three items; alpha = 0.74) | The pay is good | 2.43 (.87) | 1-4 |
| The job security is good | |||
| Career rewards (three items; alpha = 0.78) | The chances for promotion are good | 2.22 (.84) | 1-4 |
| Promotions are handled fairly | |||
| Quality of coworkers (nine items; alpha = 0.80) | Sometimes our nursing assistants take out their bad days on the patients | 2.70 (.50) | 1-4 |
| Some nursing assistants act hostile toward patients | |||
| Perceived quality of care (16 items; alpha = 0.90) | I try to keep the patients' routines in place when caring for them | 3.45 (.36) | 1-4 |
| I treat patients like I would like to be treated | |||
| Team care (four items; alpha = 0.75) | Patients' rooms are kept clean here | 2.84 (.56) | 1-4 |
| All nursing personnel here take responsibility for answering call lights | |||
| Contingencies | |||
| Breadwinner | Indicates whether or not the respondent considers their wages to be the primary source of income for their family (yes = 1) | 60% | 0-1 |
| Single mother | Indicates if the respondent cares for children under 18 who live in the home and is not married (yes = 1) | 31% | 0-1 |
| Public assistance | Indicates whether or not the nursing assistant has received financial assistance from any public source within the last 3 years (yes = 1) | 30% | 0-1 |
| Health insurance | Indicates if the respondent has health insurance from any source (yes = 1) | 78% | 0-1 |
| Individual characteristics | |||
| Age | Age of survey respondent. Logged age is used in all models. | 37.7 (12.9) | 17-72 |
| Female | Indicates whether individual is 0) male or 1) female. | 95% | 0-1 |
| Black | Indicates if respondent is 0) white or 1) black | 50% | 0-1 |
| Other minority | Indicates if respondent is 0) white or 1) other minority | 6% | 0-1 |
| High school degree or less | Recipient of 0) more than 12 years of education, or 1) a high school degree or less | 83% | 0-1 |
| Tenure | The number of years and months that the nursing assistant has been employed at the facility | 4.1 (5.0) | 0.08-32.2 |
| Past job in health care | Indicates if the respondent has held a job in health care prior to her or her current position (yes = 1) | 65% | 0-1 |
| Organizational characteristics | |||
| For-profit | Indicates whether the facility is 0) nonprofit or public or 1) for-profit | 81% | 0-1 |
| Number of beds | Number of licensed beds in facility | 115 (37.4) | 47-180 |
| Economic characteristics | |||
| Unemployment rate | Unemployment rate in the Workforce Development Region | 6.2 (1.1) | 4.6-7.5 |
| Comparable income | The median income of nonactive aides minus the median income of active aides in the Workforce Development Region | $1,541 (1,123) | -778 to 4626 |
N = 315.
Measurement
Dependent Variables.—The dependent variables in this study are intent to stay and retention. Three survey items are used to measure intent to stay and include whether the individual intends to stay (a) in their current position, (b) the occupation of nursing assistant, and (c) the field of long-term care. See Table 1 for a summary of all dependent and independent variables. Table 2 contains the correlation statistics for all dependent and independent variables.
Table 2.
Correlation Table of Dependent and Independent Variables
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | (15) | (16) | (17) | (18) | (19) | (20) | (21) | (22) | (23) | (24) | (25) | (26) | (27) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Retention | 1 | ||||||||||||||||||||||||||
| (2) Intent/job | -0.01 | 1 | |||||||||||||||||||||||||
| (3) Intent/ occupation | 0.02 | 0.42 | 1 | ||||||||||||||||||||||||
| (4) Intent/LTC | -0.17 | 0.38 | 0.38 | 1 | |||||||||||||||||||||||
| (5) Job satisfaction | -0.04 | 0.48 | 0.31 | 0.41 | 1 | ||||||||||||||||||||||
| (6) Supervisor | -0.01 | 0.08 | 0.08 | 0.20 | 0.44 | 1 | |||||||||||||||||||||
| (7) Workload | -0.03 | -0.17 | -0.14 | -0.20 | -0.53 | -0.40 | 1 | ||||||||||||||||||||
| (8) Financial rewards | 0.00 | 0.28 | 0.21 | 0.21 | 0.58 | 0.47 | -0.43 | 1 | |||||||||||||||||||
| (9) Career rewards | -0.03 | 0.22 | 0.15 | 0.23 | 0.53 | 0.52 | -0.44 | 0.60 | 1 | ||||||||||||||||||
| (10) Coworkers | -0.08 | -0.03 | -0.04 | -0.13 | -0.24 | -0.31 | 0.37 | -0.25 | -0.32 | 1 | |||||||||||||||||
| (11) Interpersonal care | -0.06 | 0.14 | 0.16 | 0.10 | 0.31 | 0.22 | -0.08 | 0.15 | 0.19 | -0.10 | 1 | ||||||||||||||||
| (12) Team care | -0.05 | 0.12 | 0.21 | 0.09 | 0.41 | 0.46 | -0.33 | 0.41 | 0.45 | -0.40 | 0.36 | 1 | |||||||||||||||
| (13) Breadwinner | -0.08 | 0.13 | 0.17 | 0.12 | 0.03 | -0.02 | 0.01 | -0.02 | -0.09 | 0.01 | 0.05 | 0.11 | 1 | ||||||||||||||
| (14) Single mom | 0.02 | -0.09 | -0.06 | -0.04 | -0.11 | -0.06 | -0.01 | -0.05 | -0.07 | 0.02 | 0.05 | -0.01 | 0.33 | 1 | |||||||||||||
| (15) Public assistance | -0.05 | 0.01 | -0.03 | 0.04 | -0.05 | 0.04 | -0.03 | -0.02 | -0.01 | 0.02 | 0.02 | -0.07 | 0.18 | 0.47 | 1 | ||||||||||||
| (16) Health insurance | 0.23 | -0.02 | 0.09 | 0.01 | 0.00 | 0.08 | 0.01 | 0.01 | 0.00 | 0.07 | 0.01 | -0.05 | -0.08 | -0.15 | -0.19 | 1 | |||||||||||
| (17) Age (logged) | 0.09 | 0.28 | 0.37 | 0.24 | 0.08 | 0.04 | 0.03 | 0.01 | -0.08 | -0.06 | 0.02 | 0.01 | 0.18 | -0.23 | -0.26 | 0.18 | 1 | ||||||||||
| (18) Female | 0.08 | 0.01 | 0.09 | 0.00 | -0.09 | -0.10 | -0.03 | -0.01 | -0.09 | -0.04 | 0.09 | -0.08 | 0.03 | 0.02 | 0.08 | 0.03 | 0.06 | 1 | |||||||||
| (19) Black | 0.04 | -0.08 | 0.00 | -0.07 | -0.11 | -0.18 | 0.02 | -0.25 | -0.12 | -0.09 | -0.03 | -0.07 | 0.14 | 0.16 | 0.07 | -0.02 | 0.10 | 0.05 | 1 | ||||||||
| (20) Other race | 0.06 | -0.06 | 0.00 | 0.02 | 0.02 | 0.00 | 0.05 | -0.03 | -0.07 | -0.01 | 0.01 | 0.05 | -0.01 | -0.11 | -0.08 | 0.07 | 0.01 | -0.07 | -0.26 | 1 | |||||||
| (21) = High school degree | 0.00 | -0.03 | 0.13 | 0.01 | 0.05 | -0.04 | 0.01 | -0.05 | -0.03 | -0.05 | 0.08 | 0.03 | -0.04 | -0.04 | -0.06 | 0.04 | 0.04 | 0.14 | 0.07 | 0.05 | 1 | ||||||
| (22) Tenure | 0.24 | 0.17 | 0.22 | 0.07 | -0.03 | 0.00 | 0.05 | -0.03 | -0.08 | 0.01 | 0.03 | -0.10 | 0.08 | -0.15 | -0.15 | 0.27 | 0.45 | 0.04 | 0.12 | 0.04 | 0.05 | 1 | |||||
| (23) Past health care | -0.13 | -0.07 | -0.01 | 0.03 | -0.14 | -0.22 | 0.11 | -0.17 | -0.17 | 0.05 | -0.02 | -0.15 | 0.11 | 0.06 | 0.08 | -0.08 | 0.08 | -0.01 | 0.18 | -0.10 | -0.04 | -0.09 | 1 | ||||
| (24) For-profit | -0.05 | -0.11 | -0.06 | 0.04 | -0.02 | -0.13 | -0.03 | -0.09 | -0.02 | 0.00 | -0.03 | -0.06 | -0.02 | -0.04 | 0.00 | -0.07 | -0.04 | 0.01 | 0.23 | -0.05 | 0.12 | 0.01 | 0.14 | 1 | |||
| (25) Size/100 | 0.09 | -0.15 | -0.07 | -0.04 | -0.17 | 0.04 | 0.21 | -0.12 | -0.02 | -0.02 | -0.04 | -0.06 | 0.12 | 0.08 | 0.11 | 0.08 | -0.06 | -0.09 | 0.11 | 0.05 | 0.02 | 0.00 | 0.12 | -0.11 | 1 | ||
| (26) Unemployment rate | 0.06 | -0.07 | -0.03 | -0.05 | -0.10 | -0.14 | 0.14 | -0.03 | -0.18 | 0.15 | -0.12 | -0.18 | 0.04 | 0.13 | 0.09 | 0.07 | -0.06 | 0.03 | -0.07 | 0.13 | 0.08 | 0.05 | 0.02 | 0.05 | 0.10 | 1 | |
| (27) Comparable income | 0.07 | -0.03 | -0.03 | -0.02 | -0.05 | 0.02 | 0.06 | -0.07 | -0.08 | -0.05 | 0.04 | 0.02 | 0.06 | -0.01 | -0.02 | 0.11 | 0.01 | -0.07 | 0.00 | 0.16 | 0.03 | -0.02 | 0.17 | -0.43 | 0.48 | 0.10 | 1 |
Retention indicates whether or not the individual remained in her position approximately 12 months after the survey was administered (yes = 1). Most of the literature on turnover and retention has focused on voluntary turnover. Unfortunately, we are not able to distinguish between voluntary and involuntary turnover because of limitations of the data; however, we also argue that the distinction between voluntary and involuntary turnover is less important when studying the antecedents of termination among low-wage workers. As we have argued previously, low-wage workers face many employment constraints that may contribute to an individual either quitting their job voluntarily or being let go involuntarily (e.g., having a lapse in childcare could lead a person to quit their job or be fired for absenteeism). Previous research has shown that there are strong similarities in the antecedents of quits and dismissals, suggesting that common processes relating to individual circumstances and job design influence both types of job termination (Batt & Colvin, 2011).
Independent Variables.—A job satisfaction scale reflects how content an individual is with his or her job. Four survey items were included in a scale of overall job satisfaction, which has an alpha of .79. (See Table 1 for a sample of specific survey items included in the scale.) In addition, we examine a number of perceived job characteristics, including scales of supervisory support, workload, financial rewards, and career rewards. We also include three scaled measures of perceived quality of care, including the quality of coworkers, the degree of perceived quality of care provided for residents, and the degree to which all staff members work together to provide quality care (referred to as team care). Table 1 includes a sample of survey items included in perceived job characteristic scales as well as alpha statistics. These survey measures were previously validated and are described in detail elsewhere (Morgan, 2005; Morgan & Konrad, 2008).
Also of interest are variables that we have labeled as “contingency factors,” or personal circumstances that may influence retention. These include as follows: being a primary breadwinner, being a single mother, receiving public assistance, and having health insurance. Being a primary breadwinner indicates that the respondent considers herself to be the primary wage earner for her family. Being a single mother indicates that the respondent is not married and cares for children under age 18 in their home. Public assistance indicates that the respondent has received public assistance from any public source (e.g., welfare payments, food stamps) in the last 3 years. The measure of whether the individual has health insurance indicates whether they have health insurance from any source, not just from their employer. We include a general measure of health insurance (rather than whether the individual has employer-based insurance) because we think that not having insurance from any source—an employer, a spouse, or through Medicaid—might put a worker at risk for leaving his or her job.
Control variables included in the model are personal, organizational, and economic factors that have been linked to job satisfaction, intent to stay, and retention. Personal characteristics include age (logged), sex, race/ethnicity, having a high school degree or less (compared with some college), job tenure, and whether the individual has worked in health care in the past. Organizational characteristics include type of ownership and the number of beds (divided by 10) in the facility. Finally, economic characteristics include the regional unemployment rate and comparable income (divided by 1,000), defined as the regional average annual income for nursing assistants no longer working in the field of long-term care minus the annual income for nursing assistants still working in the field of long-term care. This variable is a proxy for the degree of inequality in income between those who stay in the field and those who leave the field (Dill, Morgan, & Konrad, 2010). Organizational characteristics and economic indicators have been shown to be important predictors of turnover in studies of organization-level turnover (Banaszak-Holl & Hines, 1996; Castle & Engberg, 2006; Stearns & D’Arcy, 2008).
Analyses
Two types of models were used in this study. Logistic regression models were used to analyze retention and intent to stay in the field of long-term care, which are binary variables. Ordered logit models were used to analyze the intent to stay in one’s job and intent to stay in the occupation of nursing assistant variables; Brant tests confirmed that the ordered logit models meet the proportional odds assumption. Specification tests confirmed that multicollinearity was not a concern for any of the models; variance inflation factor (VIF) scores were below 2 for all models. All analyses were conducted using Stata 11 software.
Models with intent to stay as the independent variable are in Tables 3 and 4. Table 3 includes job satisfaction as an independent variable, whereas Table 4 includes perceived job characteristics (financial and career rewards, workload, supervisor support, and measures of quality of care) as independent variables, rather than a global measure of job satisfaction. Full models with retention as the dependent variable are in Table 5. We include job satisfaction and perceived job characteristics in separate models to see the individual effects of job characteristics apart from overall job satisfaction.
Table 3.
Determinants of Intent to Stay With Job Satisfaction as Independent Variable
| Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|
| I intend to remain in my current position for the near future | Three years from now, I would still like to be working as a nursing assistant | Do you think you will be working in the field of LTC 3 years from now? | |||||
| Coefficient | (SE) | Coefficient | (SE) | Coefficient | (SE) | ||
| Job satisfaction | 0.65*** | (0.08) | 0.39*** | (0.09) | 0.57*** | (0.09) | |
| Contingency factors | |||||||
| Breadwinner | 0.27 | (0.24) | 0.65* | (0.29) | 0.47 | (0.30) | |
| Single mother | -0.32 | (0.25) | -0.26 | (0.48) | 0.05 | (0.32) | |
| Public assistance | 0.61* | (0.27) | 0.41 | (0.42) | 0.63* | (0.32) | |
| Health insurance | -0.20 | (0.27) | 0.39 | (0.31) | -0.17 | (0.32) | |
| Constant | -11.12*** | (1.73) | |||||
| Cut 1 | 5.66*** | (1.52) | 9.19*** | (1.74) | |||
| Cut 2 | 7.17*** | (1.52) | 10.46*** | (1.82) | |||
| Cut 3 | 9.81*** | (1.65) | 12.09*** | (1.86) | |||
| Pseudo R2 | 0.17 | 0.12 | 0.2 | ||||
Notes: N = 315 nursing assistants in 18 nursing home. Additional control variables are not shown in Tables 3 and 4; full tables available upon request. Models 1 and 2 are ordered logit models; Model 3 is a logit model. Specification tests confirmed that ordered logit model tests meet the proportional odds assumption. Because this study utilizes data from individuals nested within organizations, Huber White Sandwich Estimators were used in all models to correct for clustering of the error terms (Wooldridge, 2002).
*p =.05. **p = .01. ***p = .001.
Table 4.
Determinants of Intent to Stay With Job Quality Characteristics as Independent Variables
| Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|
| I intend to remain in my current position for the near future | Three years from now, I would still like to be working as a nursing assistant | Do you think you will be working in the field of LTC 3 years from now? | |||||
| Coefficient | (SE) | Coefficient | (SE) | Coefficient | (SE) | ||
| Supervisor support | -0.70** | (0.27) | -0.65** | (0.24) | 0.12 | (0.34) | |
| Workload | -0.37 | (0.20) | -0.41* | (0.20) | -0.40 | (0.30) | |
| Financial rewards | 0.46* | (0.23) | 0.39* | (0.18) | 0.24 | (0.26) | |
| Career rewards | 0.58* | (0.25) | 0.30 | (0.17) | 0.48* | (0.23) | |
| Quality of coworkers | 0.19 | (0.35) | 0.64** | (0.2) | -0.15 | (0.3) | |
| Perceived quality of care | 1.03* | (0.43) | 0.48 | (0.45) | 0.50 | (0.42) | |
| Team care | -0.41 | (0.33) | 0.56 | (0.35) | -0.52 | (0.37) | |
| Contingency factors | |||||||
| Breadwinner | 0.46* | (0.21) | 0.57* | (0.29) | 0.73** | (0.28) | |
| Single mother | -0.56 | (0.31) | -0.35 | (0.44) | -0.20 | (0.38) | |
| Public assistance | 0.75** | (0.27) | 0.54 | (0.4) | 0.58 | (0.38) | |
| Health insurance | -0.19 | (0.20) | 0.34 | (0.28) | -0.28 | (0.24) | |
| Constant | -7.62*** | (2.3) | |||||
| Cut 1 | 4.93 | (2.97) | 12.18*** | (2.05) | |||
| Cut 2 | 6.28* | (3.00) | 13.44*** | (2.12) | |||
| Cut 3 | 8.73** | (3.10) | 15.08*** | (2.15) | |||
| Pseudo R2 | 0.12 | 0.13 | 0.15 | ||||
Notes: N = 315 nursing assistants in 18 nursing home. Additional control variables are not shown in Tables 3 and 4; full tables available upon request. Models 1 and 2 are ordered logit models; Model 3 is a logit model. Specification tests confirmed that ordered logit model tests meet the proportional odds assumption. Because this study utilizes data from individuals nested within organizations, Huber White Sandwich Estimators were used in all models to correct for clustering of the error terms (Wooldridge, 2002).
*p =. 05. **p = .01. ***p = .001.
Table 5.
Determinants of Nursing Assistant Retention
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | (SE) | Coefficient | (SE) | Coefficient | (SE) | Coefficient | (SE) | Coefficient | (SE) | |
| Job satisfaction | -0.02 | (0.08) | -0.01 | (0.10) | ||||||
| Intent to stay in job | -0.18 | (0.58) | -0.17 | (0.65) | -0.12 | (0.68) | ||||
| Perceived job characteristics | ||||||||||
| Supervisor support | -0.34 | (0.52) | -0.50 | (0.48) | ||||||
| Workload | -0.24 | (0.53) | -0.34 | (0.50) | ||||||
| Financial rewards | -0.11 | (0.27) | -0.06 | (0.26) | ||||||
| Career rewards | -0.04 | (0.35) | -0.09 | (0.39) | ||||||
| Quality of coworkers | -0.72 | (0.56) | -0.63 | (0.56) | ||||||
| Perceived quality of care | -0.82 | (0.50) | -0.76 | (0.52) | ||||||
| Team care | 0.31 | (0.47) | 0.41 | (0.49) | ||||||
| Contingency factors | ||||||||||
| Breadwinner | -0.94* | (0.41) | -0.94* | (0.42) | -0.94* | (0.42) | -0.74 | (0.38) | -0.92* | (0.37) |
| Single mother | 0.86 | (0.64) | 0.91 | (0.64) | 0.91 | (0.64) | 0.80 | (0.64) | 0.93 | (0.69) |
| Public assistance | -0.31 | (0.61) | -0.32 | (0.63) | -0.32 | (0.63) | -0.21 | (0.58) | -0.35 | (0.66) |
| Health insurance | 0.63 | (0.39) | 0.64 | (0.38) | 0.64 | (0.39) | 0.85* | (0.35) | 0.77* | (0.37) |
| Personal characteristics | ||||||||||
| Age (logged) | 0.17 | (0.67) | 0.2 | (0.70) | 0.2 | (0.70) | -0.03 | (0.59) | 0.09 | (0.62) |
| Female | 1.19 | (0.87) | 1.16 | (0.89) | 1.16 | (0.89) | 1.37 | (0.90) | 1.28 | (0.98) |
| Black | 0.21 | (0.33) | 0.17 | (0.32) | 0.17 | (0.32) | -0.03 | (0.33) | -0.02 | (0.31) |
| Other minority | 1.01 | (1.01) | 0.96 | (1.13) | 0.96 | (1.12) | 0.76 | (0.91) | 0.35 | (0.96) |
| High school degree or less | -0.73 | (0.52) | -0.7 | (0.50) | -0.70 | (0.52) | -0.77 | (0.46) | -0.77 | (0.49) |
| Tenure in job | 0.44* | (0.18) | 0.44* | (0.18) | 0.44* | (0.18) | 0.47* | (0.17) | 0.47* | (0.18) |
| Past health experi-ence | -0.88* | (0.41) | -0.85* | (0.41) | -0.86* | (0.40) | -0.86* | (0.36) | -0.86* | (0.35) |
| Organizational characteristics | ||||||||||
| For-profit | 0.3 | (0.39) | 0.25 | (0.40) | 0.25 | (0.39) | 0.18 | (0.44) | 0.31 | (0.47) |
| Size/10 | 0.1 | (0.06) | 0.09 | (0.07) | 0.09 | (0.07) | 0.10 | (0.06) | 0.11 | (0.08) |
| Economic indicators | ||||||||||
| Unemployment rate | 0.03 | (0.16) | 0.04 | (0.17) | 0.04 | (0.16) | 0.10 | (0.14) | 0.06 | (0.14) |
| Comparable in-come/1000 | 0.18 | (0.23) | 0.19 | (0.24) | 0.19 | (0.24) | 0.19 | (0.21) | 0.21 | (0.24) |
| Constant | -1.31 | (2.59) | -1.36 | (2.53) | -1.30 | (2.55) | 3.94 | (2.82) | 3.58 | (3.13) |
| Pseudo R2 | 0.24 | 0.24 | 0.24 | 0.26 | 0.27 | |||||
Notes: N = 315 nursing assistants in 18 nursing home. The measure of "intent" in model is: "I intend to remain in my current position for the near future." The "intent" variable is dichotomous (0 = disagree or strongly disagree; 1 = agree or strongly agree). We ran additional models of retention with other measures of "intent" included as independent variables, and the findings were similar. Additional models of retention available upon request. Because this study utilizes data from individuals nested within organizations, Huber White Sandwich Estimators were used in all models to correct for clustering of the error terms (Wooldridge, 2002). Finally, we used the Sobel-Goodman mediation test with bootstrapped standard errors to test whether intent to stay mediated the relationship between key independent variables and retention (Ender, 2008). We did not find that intent to stay was a significant mediator between any of the independent variables shown in Tables 3 and 4 and retention.
*p = .05. **p =. 01. ***p = .001.
Results
Intent to Stay
In this section, we outline findings for an individual’s intent to stay in their current job, in the occupation of nursing assistant, and in the field of long-term care. We will then turn from intentions to actual retention behavior in the section that will follow.
Intent to Stay in Current Job.—We found that primary breadwinners and those who were recipients of public assistance (within the last 3 years) were more likely to say that they intended to stay with their current employer in the near future (Tables 3 and 4, Model 1). Job satisfaction is a positive predictor of intent to stay in one’s job, as are many job characteristics. Nursing assistants who report greater financial and career rewards are more likely to intend to stay, as are those who those who report higher quality of care provided at their facility (labeled perceived quality of care). Surprisingly, nursing assistants who report a higher degree of supervisor support are actually less likely to intend to stay in their job (Tables 3 and 4, Model 1). Finally, although it is not shown in Tables 3 and 4, nursing assistants working in larger facilities are more likely to say that they do not intend to stay in their current job.
Intent to Stay in the Occupation.—Similar to our model of intent to stay on the job, primary breadwinners were more likely to say that they intended to stay in the occupation of nursing assistant. Those who reported higher job satisfaction, greater financial rewards, and better relationships with coworkers were also more likely to report that they intended to stay in the occupation, whereas those who reported higher supervisor support were less likely (Tables 3 and 4, Model 2).
Intent to Stay in the Field.—Primary breadwinners and workers who received public assistance (within the last 3 years) were both more likely to say that they intend to be working in the field of long-term care in 3 years. Job satisfaction and career rewards were positive predictors of intent to stay in the field (Tables 3 and 4, Model 3).
Retention
Turning to actual behavior, we find that neither job satisfaction nor any perceived job characteristics, such as workload and measures of quality of care, were significant predictors of actual retention. Further, the correlation between intent to stay and retention in our sample is −.01 (Table 2), and in our multivariate models intent to stay in their current position was not a significant predictor of actual retention (Table 5). Primary breadwinners are less likely to remain in their jobs, even though they were more likely to say that they intended to stay in their job and the field of long-term care, while those with health insurance were more likely to stay in their jobs. Those who have been employed by a facility longer are more likely to remain in their jobs, but those who have worked in health care in the past are less likely to remain in their positions. Organization characteristics and economic factors were not significant predictors of retention. We are able to predict about 25% of the variance in retention (Table 5).
Discussion
Our findings suggest that individual ratings of intentions regarding their current jobs and their actual behavior were not closely related. The correlations between job satisfaction, intent to stay in one’s current position and retention are low and nonsignificant (r = −.04 and r = −0.01, respectively), and neither job satisfaction nor intent to stay were significant predictors in multivariate models of retention. Furthermore, no perceived job characteristics, including supervisory support, career and financial rewards, or different dimensions of quality of care were significant predictors of retention, a finding that is consistent with Rosen and colleague’s (2011) study of nursing assistant turnover. Instead, “contingency factors” and personal characteristics appear to drive retention. This supports our hypothesis that low-wage health care employees have “contingency factors” in their lives that constrain their employment intentions and trigger behavior independently of job satisfaction or expectations of their career pathway.
For example, one of the personal contingencies that we examined in this study was whether an individual was a primary breadwinner. When looking at job satisfaction and intent to stay, primary breadwinners report that they are more satisfied with their jobs than nonbreadwinners and are more likely to say that they intend to stay in their current jobs in the near future. However, primary breadwinners are actually less likely to still be in their jobs after the survey was administered. Similarly, individuals who were receiving public assistance were more likely to say that they intended to remain in their current position in the near future than those not receiving public assistance (within the last 3 years), but they were not significantly more likely to still be employed 1 year later. Why do we find opposite results? It is likely, for example, that individuals receiving public assistance are more systematically vulnerable to resource-related “shocks.” Inconsistent child care, personal or family injury or health issues, transportation problems, and related economic pressures are likely to put these workers in positions where they are “forced” to leave their jobs. Primary breadwinners, on the other hand, are likely trying to find a way to make more money to support themselves and their families, which may mean taking another job that offers marginally higher wages despite their satisfaction with their current caregiving job. Our findings suggest that while primary breadwinners and recipients of public assistance intended to stay in their jobs, they are constrained in their ability to act on their expressed intentions. In contrast, we found that having health insurance was significantly related to retention, but was not significantly related to turnover intentions, a finding that is consistent with the findings of Rosen and colleagues (2011).
We found that individuals who had previously worked in health care before taking their current job were less likely to remain in their job 1 year later. This finding seems to reflect the high degree of mobility of nursing assistants within the field of long-term care (Baughman & Smith, 2011). While many nursing assistants report that nursing assistant work is meaningful and satisfying to them, they are more committed to the occupation and field of long-term care than to their current employers (Diamond, 1992). Therefore, nursing assistants may leave their employer if another nursing facility offers slightly higher wages, sign-on bonuses or some type of health insurance benefits. Alternatively, as discussed previously, nursing assistants may drop out of the labor market temporarily due to “contingency factors” and, when they re-enter the workforce, they take a job with a different employer in the field of long-term care.
Finally, we had one finding that was unexpected; we found that supervisor support was negatively related to intent to stay both in one’s current job and in the occupation of nursing assistant. We suspect that supervisor support might be negatively related to employment intentions because a supportive supervisor likely encourages employees to pursue a better job or higher education. On the other hand, workers who are struggling with the job may get more attention and support from vigilant supervisors. However, these possible interpretations are highly speculative and further research is warranted.
Limitations and Future Research
An important limitation of this study is that we do not know individual’s reasons for leaving their positions. We include proxies for resource-related circumstances that lead to job termination, such as being a single mother or not having health insurance, but we cannot specify the specific mechanisms that led to employee turnover or retention. Further, we cannot distinguish between voluntary and involuntary turnover (although we have suggested that whether an individual was fired or quit voluntarily is not a very meaningful distinction for this group of workers). However, future research could expand our understanding of low-wage worker employment outcomes by directly measuring reasons for employee turnover. Finally, the high level of missing data may be limiting the variability in our independent variables and contributing to the low levels of explained variance in many of our models.
Future research could expand on our study in a number of ways. First, the nursing assistants surveyed for this study were working in organizations that were on a waiting list for a workforce development program, indicating that these employers were more likely to be interested in employee development than a “typical” nursing home. Our model should be tested among a larger and more representative sample of nursing assistants and other low-wage health care workers to see if there is consistency among similar populations. Second, our data were collected before the current economic recession, and studies have shown that turnover among nurse aides has dropped substantially since 2008 (Konrad, Morgan, & Rice, 2010). Data collected more recently would allow researchers to explore predictors of retention in changing economic circumstances.
Conclusion and Implications
Our findings have implications for both practice and research. First, our study suggests that we cannot expect to reduce nursing assistant turnover through the improvement of job satisfaction alone. In an excellent discussion of culture change initiatives in nursing homes, Bishop and colleagues (2008) note that many forms of culture change in nursing homes that aim to improve nursing assistant job satisfaction are similar to high-performance work practices (also called lean management or strategic human resources [HR] management). Workers are given expanded and enhanced job descriptions that give them greater autonomy in their job tasks and greater participation in decisions about patient care (Lopez, 2006). However, most culture change initiatives lack a key component of high-performance work practices—namely, HR practices aimed to attract and develop qualified workers, including good pay, benefits, and advancement opportunities (Bishop et al., 2008).
Given this, an implication of our findings is that organizations likely need to address these key extrinsic job factors in order to affect turnover for low-wage workers such as nursing assistants. Implementing some high-performance work practices without attending to compensation, benefits or career promotion opportunities will likely have an impact on job satisfaction and intent to stay but not necessarily retention. As noted by Bishop and colleagues (2008), nursing homes face severe resource constraints due to low government-regulated rates of reimbursement and a limited private-pay population, making it difficult for nursing homes to make improvements in the wages and benefits of these workers. However, we should acknowledge the limitations of job redesign of nursing assistant positions in nursing homes in reducing turnover without the accompaniment of extrinsic HR incentives (Méhaut et al., 2010).
Finally, our findings imply that research on nursing assistant turnover should not rely on job satisfaction or turnover intent as a proxy for actual turnover or retention. The relationships between these conditions are highly variable in this population, and our study suggests that nursing assistant turnover is driven in large part by factors not related to either the job experience or employment intention.
Funding
This project was originally funded by Robert Wood Johnson Foundation and Atlantic Philanthropies as part of the Better Jobs Better Care initiative. Dr. Dill’s efforts were supported by funding from the Agency for Healthcare Research and Quality (T32HS00032-23) and the National Institute on Aging (T32AG000272-06A2).
Acknowledgments
We are grateful to the editor and reviewers of The Gerontologist for their thoughtful and detailed comments and suggestions.
References
- Appelbaum E., Berg P., Frost A., Preuss G. (2003). The effects of work re-structuring on low wage, low skill workers in US hospitals. In Appelbaum E., Bernhardt A. D., Murnane R. (Eds.), Low-wage America: How employers are reshaping opportunity in the workplace (pp. 33–76). New York: Russell Sage Foundation; [Google Scholar]
- Banaszak-Holl J., Hines M. A. (1996). Factors associated with nursing home staff turnover. The Gerontologist. 36, 512–517 [DOI] [PubMed] [Google Scholar]
- Baughman R. A., Smith K. E. (2011). Labor mobility of the direct care workforce: Implications for the provision of Long-Term care. Health Economics. Advance online publication. doi: 10.1002/hec.1798. [DOI] [PubMed] [Google Scholar]
- Batt R., Colvin A. J. S. (2011). An employment systems approach to turnover: Human resources practices, quits, dismissals. The Academy of Management Journal. 54, 695–717 [Google Scholar]
- Becker H. S. (1960). Notes on the concept of commitment. American Journal of Sociology. 66, 32–40 [Google Scholar]
- Bishop C. E., Squillace M. R., Meagher J., Anderson W. L., Wiener J. M. (2009). Nursing home work practices and nursing assistants’ job satisfaction. The Gerontologist. 49, 611–622 [DOI] [PubMed] [Google Scholar]
- Bishop C. E., Weinberg D. B., Leutz W., Dossa A., Pfefferle S. G. (2008). Nursing assistants’ job commitment: Effect of nursing home organizational factors and impact on resident well-being. The Gerontologist. 48(suppl 1)36–45 [DOI] [PubMed] [Google Scholar]
- Brannon D., Barry T., Kemper P., Schreiner A., Vasey J. (2007). Job perceptions and intent to leave among direct care workers: Evidence from the better jobs better care demonstrations. The Gerontologist. 47, 820–829 [DOI] [PubMed] [Google Scholar]
- Brannon D., Zinn J. S., Mor V., Davis J. (2002). An exploration of job, organizational, and environmental factors associated with high and low nursing assistant turnover. The Gerontologist. 42, 159–168 [DOI] [PubMed] [Google Scholar]
- Budig M. J., England P. (2001). The wage penalty for motherhood. American Sociological Review. 66, 204–225 [Google Scholar]
- Castle N. G., Engberg J. (2006). Organizational characteristics associated with staff turnover in nursing homes. The Gerontologist. 46, 62–73 [DOI] [PubMed] [Google Scholar]
- Castle N. G., Engberg J., Anderson R., Men A. (2007). Job satisfaction of nurse aides in nursing homes: Intent to leave and turnover. The Gerontologist. 47, 193–204 [DOI] [PubMed] [Google Scholar]
- Decker F. H., Harris-Kojetin L. D., Bercovitz A. (2009). Intrinsic job satisfaction, overall satisfaction, and intention to leave the job among nursing assistants in nursing homes. The Gerontologist. 49, 596–610 [DOI] [PubMed] [Google Scholar]
- Diamond T. (1995). Making gray gold: Narratives of nursing home care. Chicago: University of Chicago Press; [Google Scholar]
- Dill J. S., Morgan J. C., Konrad T. R. (2010). Strengthening the long-term care workforce. Journal of Applied Gerontology. 29, 196–214 [Google Scholar]
- Edin K., Kefalas M. (2005). Promises I can keep: Why poor women put motherhood before marriage. Berkeley: University of California Press; [Google Scholar]
- Edin K., Lein L. (1997). Making ends meet: How single mothers survive welfare and low-wage work. New York: Russell Sage Foundation Publications; [Google Scholar]
- Ejaz F. K., Noelker L. S., Menne H. L., Bagaka’s J. G. (2008). The impact of stress and support on direct care workers’ job satisfaction. The Gerontologist. 48(suppl 1)60–70 [DOI] [PubMed] [Google Scholar]
- Ender P. (2008). Program to compute Sobel-Goodman mediation tests. Los Angeles, CA: UCLA Academic Technology Services (Statistical Consulting Group)Retrieved from http://www.ats.ucla.edu/stat/stata/faq/sgmediation.htm [Google Scholar]
- Glenn E. N. (1992). From servitude to service work: Historical continuities in the racial division of paid reproductive labor. Signs. 18, 1–43 [Google Scholar]
- Griffeth R. W., Hom P. W., Gaertner S. (2000). A meta-analysis of antecedents and correlates of employee turnover: Update, moderator tests, and research implications for the next millennium. Journal of Management. 26, 463–488 [Google Scholar]
- Holzer H. J., Stoll M. A., Wissoker D. (2004). Job performance and retention among welfare recipients. The Social Service Review. 78, 343–369 [Google Scholar]
- Hunter L. W. (2000). What determines job quality in nursing homes?. Industrial and Labor Relations Review. 53, 463–481 [Google Scholar]
- Kalleberg A. (2011). Good jobs, bad jobs: The rise of polarized and precarious employment systems in the United States, 1970s-2000s. New York: Russell Sage Foundation, American Sociological Association Rose Series in Sociology; [Google Scholar]
- Kalleberg A. L. (2009). Precarious work, insecure workers: Employment relations in transition. American Sociological Review. 74, 1–22 [Google Scholar]
- Kiyak H. A., Namazi K. H., Kahana E. F. (1997). Job commitment and turnover among women working in facilities serving older persons. Research on Aging. 19, 223–246 [Google Scholar]
- Konrad T. R., Morgan J. C., Rice A. (2010). Descriptive results from the state turnover survey conducted for the office of long-term care of the NC department of health and human services, 2009. Chapel Hill, NC: UNC Institute on Aging; [Google Scholar]
- Lee T. H., Gerhart B., Weller I., Trevor C. O. (2008). Understanding voluntary turnover: Path-specific job satisfaction effects and the importance of unsolicited job offers. The Academy of Management Journal. 51, 651–671 [Google Scholar]
- Lopez S. H. (2006). Culture change management in long-term care: A shop-floor view. Politics & Society. 34, 55 [Google Scholar]
- Méhaut P., Berg P., Grimshaw D., Jaehrling K., Van Der Meer M., Eskildsen J. (2010). Cleaning and nursing in hospitals: Institutional variety and the reshaping of low-wage jobs. In Gautie J., Schmitt J. (Eds.), Low-wage work in the wealthy world (pp. 319–366). New York: Russell Sage Foundation; [Google Scholar]
- Mittal V., Rosen J., Leana C. (2009). A dual-driver model of retention and turnover in the direct care workforce. The Gerontologist. 49, 623–634 [DOI] [PubMed] [Google Scholar]
- Morgan J. C. (2005). Just a job? A mixed method analysis of the work situation of direct care workers in long-term care settings. Dissertation Abstracts International. 66, 09A [Google Scholar]
- Morgan J. C., Konrad T. R. (2008). A mixed-method evaluation of a workforce development intervention for nursing assistants in nursing homes: The case of WIN A STEP UP. The Gerontologist. 48, 71–79 [DOI] [PubMed] [Google Scholar]
- Newman K. S., Massengill R. P. (2006). The texture of hardship: Qualitative sociology of poverty, 1995–2005. Annual Review of Sociology. 32, 423–446 [Google Scholar]
- O’Connor A. (2000). Poverty research and policy for the post-welfare era. Annual Review of Sociology. 26, 547–562 [Google Scholar]
- Rosen J., Stiehl E. M., Mittal V., Leana C. R. (2011). Stayers, leavers, and switchers among certified nursing assistants in nursing homes: A longitudinal investigation of turnover intent, staff retention, and turnover. The Gerontologist. Advance online publication. 10.1093/geront/gnr025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K., Baughman R. (2007). Caring for America’s aging population: A profile of the direct-care workforce. Monthly Labor Review. 130, 20–26 [Google Scholar]
- Squillace M. R., Remsburg R. E., Harris-Kojetin L. D., Bercovitz A., Rosenoff E., Han B. (2009). The national nursing assistant survey: Improving the evidence base for policy initiatives to strengthen the certified nursing assistant workforce. The Gerontologist. 49, 185–197 [DOI] [PubMed] [Google Scholar]
- Stearns S. C., D’Arcy L. P. (2008). Staying the course: Facility and profession retention among nursing assistants in nursing homes. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 63, S113–S121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel R. P. (2002). Turnover theory at the empirical interface: Problems of fit and function. Academy of Management Review. 27(3)346–360 [Google Scholar]
- Temple A., Dobbs D., Andel R. (2010). The association between organizational characteristics and benefits offered to nursing assistants: Results from the national nursing home survey. Health Care Management Review. 35, 324–332 [DOI] [PubMed] [Google Scholar]
- Wooldridge J. M. (2002). Econometric analysis of cross section and panel data. Cambridge, MA: MIT Press; [Google Scholar]


