Abstract
Many multi-level, contextually-relevant, evidenced-based health promotion programs are not disseminated widely. The purpose of this study is to describe the adaptation of a published effective tobacco use cessation intervention, which was implemented and evaluated in a broader population of unionized workers partnering with a Health and Welfare Fund health benefits carrier. Working with HWF administration, 68 tobacco users enrolled. Implementation and effectiveness outcomes indicated most participants (69%) completed all counseling calls and at 16-weeks follow-up, 30.9% reported not using tobacco. The intervention had relatively high levels of implementation, effectiveness, and acceptability but low reach, highlighting issues arising during dissemination.
Keywords: Dissemination, Implementation, Unionized Workers, Tobacco Use Cessation
Traditionally, there has been an expectation that developing and testing interventions with study designs that maximize internal validity (e.g., randomized controlled trials) will over time be naturally transferred to the intended audience.1 However, many effective evidenced-based behavioral programs for cancer prevention and control, among other chronic diseases, are not disseminated on a wide scale. A key issue is to better understand the process of transferring research studies to new settings and populations. Indeed, there are currently urgent ‘calls for action’ for research aimed at addressing this research to practice gap, namely by providing practical research findings that are contextually relevant in particular settings and populations.2,3
While definitions of what constitutes dissemination research vary, Bowen and colleagues propose the following one: “Understanding the movement of evidence-based public health and clinical innovations into practice settings”.2(pp 474) This definition can be applied to research that seeks to use “strategies to introduce or change evidence-based health interventions within specific settings.”2(pp 480) One can further conceptualize models of dissemination by referring to the impetus behind the translation effort, for example those that draw primarily from needs of practice settings (i.e., community-centered model) or from researchers with important study findings (i.e., research to practice model).4 Behavioral change is not the primary outcome under examination; rather, from a dissemination perspective, it is equally important to consider outcomes including the consistency and feasibility of the intervention in the new specified setting. It is important to note that practical or behavioral trials are better suited to obtaining this contextually-relevant information, as opposed to a complete reliance on study designs focused on establishing efficacy and maximizing internal validity, such as randomized controlled trials.1
Rabin and colleagues conducted a systematic review of dissemination research of modifiable risk behaviors (i.e., physical activity, sun protection, diet, and smoking) for cancer prevention.5 Their review yielded 25 separate studies published from 2006 to 2008. Among their key findings, the authors reported that most studies were conducted in school settings and among children, highlighting the lack of dissemination research in other settings and populations, including those intending to reach worksites. Health promotion in worksites is effective for modifying behavioral risk factors particularly when it spans physical and social environments, has leadership support, provides meaningful tailored feedback, links health education with occupational safety, and extends coverage to employees’ families.6 Worksites provide an ideal setting to use effective multi-level, contextually-relevant health promotion for modifiable risk behaviors that can target a large proportion of adults. In order to establish a broad dissemination of effective worksite health promotion, particularly among small-to-medium sized businesses, intervention planners need to collaborate with an overarching entity that can facilitate access and delivery to the workers themselves.
The overall purpose of this study is to describe the adaptation, implementation, and evaluation of Gear Up for Health-Health and Welfare Fund (HWF). A HWF is a non-profit health care fund that administrates health care benefits for participating unionized workers and their dependents. Gear Up for Health-HWF was developed to be delivered to a broad population of unionized workers and was adapted from an evidence-based tobacco use cessation intervention originally developed for motor freight workers [called Gear Up for Health].7 Collectively, the Gear Up for Health studies were a union-management collaboration: originally implemented in worksite settings, and then disseminated through an overarching HWF.
The aims of this paper are to: 1) describe the process of adapting the original Gear Up for Health program to create Gear Up for Health-HWF and 2) examine outcomes of the dissemination process (i.e., reach, implementation, effectiveness and acceptability). These findings are discussed in relationship to the original Gear Up for Health and used to highlight the lessons we learned through the dissemination process that can be applied to future studies.
Methods
Description and Findings from the Original Gear Up for Health
Briefly, the original Gear Up for Health was a telephone-delivered health promotion program focused on tobacco use cessation and weight management among motor freight workers, comprised of truck drivers and/or dock workers from 8 terminal sites in the eastern United States.7 Workers were invited to participate in the intervention composed of 5 telephone counseling calls using principles of motivational interviewing, a tailored feedback report, and targeted written materials. Out of 542 workers who completed the baseline survey, 227 agreed to participate and completed at least 1 telephone counseling call; non-participants included all other respondents to the baseline survey (e.g., those who received no intervention; those who provided a mailing address only and thus received written materials but no counseling calls). Guided by the Social Contextual Model,8 this program utilized qualitative formative research to identify elements of the workers’ social context, for example, supervisory support, and then incorporate these factors into the design of the calls and written materials. Workers self-reported tobacco use on surveys at baseline and 10 months later, a timeline which was comprised of a 4 month intervention plus a 6 month post-intervention period. Participants were more likely to have reported quitting tobacco compared to non-participants: 23.8% vs. 9.1% (site adjusted OR=3.13, 95% CI: 1.22–7.98%, p=0.02).7 There were no significant effects on weight management.7
Development and Description of Gear Up for Health-HWF
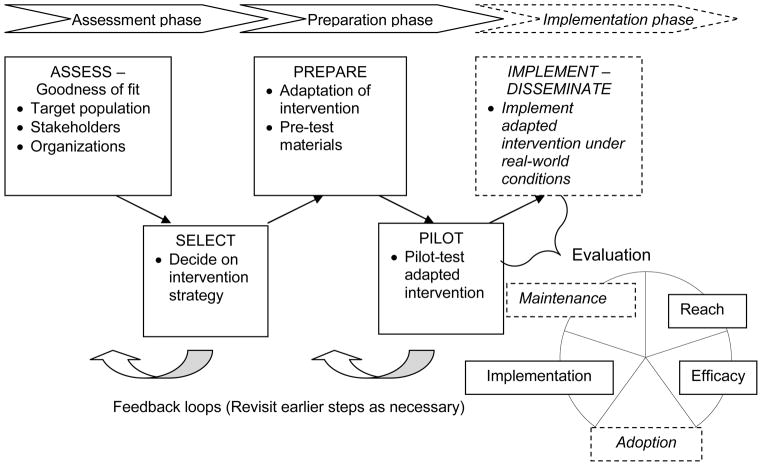
The original Gear up for Health program was offered to Teamsters members in close collaboration with both union and management. When that study was completed, we began to discuss ways in which to disseminate this formerly worksite-based approach more broadly. The development of Gear Up for Health-HWF was guided by our conceptual model, presented in Figure 1, which outlines the steps needed in intervention adaptation and dissemination.9 Together with the evaluation approach described by Glasgow and colleagues, RE-AIM,10 our conceptual model provides the basis for collecting contextually-relevant information regarding the fit of the intervention within a particular organization (e.g., reach, implementation, acceptability) and effectiveness (e.g., tobacco use cessation).
Figure 1.
Conceptual Model
Note: While this conceptual model presents an overall view of the entire dissemination process, Gear Up for Health-HWF focused on the Assessment and Preparation phases. Dashed lines indicate that we did not focus on a particular phase or evaluation piece in Gear Up for Health-HWF.
Through discussions with our partners in the Safety and Health Department of the International Brotherhood of Teamsters, we learned that dissemination of programs like this for their members would most likely be provided through union-affiliated health and welfare funds. Our partners identified and assisted us with building a collaboration with a large New England HWF, which has contracts with 10 local Teamsters chapters providing health care coverage to members and their families. We worked closely with the HWF to determine best strategies for promoting this program among their membership, based on approaches they had used in the past. As part of the ‘Assessment Phase’ of adapting this intervention for dissemination through the HWF, we systematically reviewed the literature on dissemination and other similar tested interventions, and identified the essential elements (i.e., core components) of the program, and those that might be potentially modifiable.9,11 Table 1 shows selected examples of core and modifiable elements and the associated design element in Gear Up for Health-HWF. Since we did not find significant differences for weight in the original Gear Up for Health,7 we decided to remove weight management as a main targeted behavioral outcome.
Table 1.
Selected core and adaptable elements of the original Gear Up for Health program
| Core elements: | Associated element(s): |
|---|---|
| Intervention materials should be responsive to the work environment | Examples include: materials presented tips related to getting enough sleep during shift work; pictures/graphics of trucks and manufacturing |
| Provision of out-bound coaching calls using motivational interviewing (MI): calls to be participant driven | Health educators followed a print MI guide driven by participant needs, barriers, and goals; # of calls reduced from 5 to 4 to encourage completion |
| Provision of tailored feedback: core variables are participants’ name, level of behavior, and current motivation | All core tailoring variables included in feedback report; also included name and photo of counselor; report shortened to 4 pages to encourage reading |
| Provision of NRT | Provided Nicoderm© patch |
| Clear definitions about rights to data access, confidentiality measures, and program sponsorship | Confidentiality of data was presented on survey and during calls; program sponsorship by the CDC displayed on materials |
| Modifiable elements: Material delivery channel: channels such as Internet, print, or others can be considered based on reach and access needs |
Decision was made to keep print format because the HWF didn’t recommend an online program and didn’t know computer usage among members |
| Material sequencing: materials can be delivered all at once or periodically | For ease of delivery for a HWF in the future, all printed materials were delivered in one binder |
As displayed in the conceptual model, intervention activities were coordinated through the HWF in the ‘Preparation Phase’. Through in-person and phone meetings, the research team presented our original and adapted Gear Up for Health materials and recruitment ideas to the HWF administrators for their review and feedback. Based on their experience with contacting their membership, to recruit participants, we posted a message on their website newsletter, mailed colored postcards with our logo, and attended several union meetings to promote the program and provided an information sheet to hand out at meetings that we did not attend. Data Collection. Over approximately 9 months, individuals contacted the study team, were assessed for eligibility (self-reported tobacco use in past 7 days and a HWF covered member), completed a baseline survey either online or over the phone in which a research staff member read the online survey to them, and were enrolled in the Gear Up for Health-HWF program. Respondents were asked to indicate their age; their highest level of education completed; having Hispanic ethnicity and choosing all that apply from race categories; and their current money situation. We also assessed number of quit attempts (“How many serious quit attempts lasting at least 1 day have you made in the last 10 months?”); confidence to quit12 (“How confident are you that you can quit using all forms of tobacco?”) and readiness to quit12 (“Are you seriously thinking about quitting using all tobacco products in the next 6 months?” and “Are you seriously thinking about quitting all tobacco products in the next month?”). Responses to these questions formed three categories: preparation (thinking about quitting within the next 30 days), contemplation (thinking about quitting within the next 6 months), and pre-contemplation (no indication of intent within the next 30 days or 6 months). We assessed 7 groups of common union-based job categories; mean number of hours worked per week over past 4 weeks; their usual work schedule13; and sleep adequacy14 (“How often during the past 4 weeks did you get enough sleep and feel rested upon waking up?”).
Six months after their final counseling call, participants were contacted by mailed letter and a follow up telephone call 1 week later to remind them to complete the survey on-line. If the survey was not completed, then participants were encouraged to complete the survey over the phone during the reminder phone call. Health educators used a computer-based system to track their call schedules, number of call attempts, and call outcomes (e.g., participant not home, etc.)
Intervention Description. Participants were mailed a binder that included a personalized introductory letter, a 4-page tailored feedback report, and 16 targeted tip sheets; and up to 4 coaching calls using motivational interviewing from 1 of 2 health educators were made. The tip sheets were subdivided into 4 topic areas: (1) Quitting tobacco (e.g., local resources); (2) Your workplace (e.g., sleep and shift work); (3) Family and friends (e.g., social support); and (4) Managing your weight (e.g., physical activity). The counseling calls included an introduction; information about confidentiality; learning about the participant’s life and perceived health; assessing current tobacco use and past quit attempts; gathering participant’s self-rated pros, cons, importance, confidence, and readiness to change; discussing NRT and other quitting techniques and plans; and setting goals. The intervention was conducted over 16 weeks.
Analysis Plan. Descriptive statistics of baseline and follow-up survey and process tracking system variables included frequencies and proportions of categorical measures and means and standard deviations of continuous measures. We used the Chi-square test of homogeneity to assess if completion of the final survey and quit status was associated with participant characteristics and if acceptability measures were associated with quit status. We followed an intent-to-treat approach in calculating the quit rate, whereby participants who did not complete the final survey were assumed to be non-quitters.
Results
Reach, Participant Characteristics, and Implementation of Gear Up for Health-HWF
Of the approximately 7,000 unionized workers and dependents covered by the HWF, 68 (1%) individuals contacted us with an interest in participating. All 68 individuals completed the baseline survey, were eligible, and enrolled in the program; 5 subsequently dropped out citing not wanting the counseling (n=3), not providing contact information (n=1), and illness (n=1). The majority completed the baseline survey online (69%). The most frequently cited recruitment method was receiving a mailed study postcard (68%), followed by the newsletter (28%). Most individuals were HWF members (n=52); 15 were spouses of members and 1 was a dependent of a member. Participant characteristics are presented in Table 2. Among these 68 participants, 49 (72%) completed the final survey. The majority completed the final survey online (78%). Comparing those who completed the baseline survey only vs. both the baseline and follow-up survey, there were no statistically significant differences according to gender, age, education level, or baseline level of self-efficacy to quit tobacco. However, those in preparation stage of change at baseline more often completed surveys at both time points compared to those in precontemplation or contemplation (77% vs. 28%, p=0.01).
Table 2.
Participant characteristics, n=68a
| Socio-demographic measures | n (%) |
|---|---|
| Mean age (SD) | 48.4 (9.7) |
| Gender, male | 42 (63) |
| Education, High school or below | 38 (56) |
| Some college/2yr degree | 30 (44) |
| Race, Non-Hispanic white | 65 (96) |
| Money situation, Comfortable, some extras/Enough, no extras | 37 (54) |
| Have to cut back/cannot make ends meet | 31 (46) |
|
| |
| Tobacco measures | |
| Mean quit attempt in past 10 months (SD) | 2.4 (1.6) |
| Confidence to quit, 1: not at all – 5: somewhat confident | 23 (34) |
| 6–10: very confident | 45 (66) |
| Readiness to quit, Pre-contemplation/Contemplation | 7 (10) |
| Preparation | 61 (90) |
|
| |
| Organizational factors | |
| Job category, Skill or craft/Machine operator | 25 (37) |
| Manual labor | 21 (31) |
| Scientific technical/Service work/Clerical/Professional | 21 (31) |
| Mean hours worked per week (SD) | 39.2 (14.4) |
| Work schedule, Day | 44 (66) |
| Afternoon, night, split, irregular, rotating | 23 (34) |
| Adequate sleep, Never, rarely, sometimes | 46 (68) |
| Often, very often | 22 (32) |
Numbers may not add up due to missing data; %s may not sum to 100 due to rounding
All participants received the materials binder; 58 (85%) received NRT; and 47 (69%) completed all 4 coaching calls, 16 (24%) completed 1–3 calls, and 5 (7%) completed no calls.
Effectiveness of Gear Up for Health-HWF
Among respondents to the final survey (n=49), 21 self-reported not using tobacco in the past 7 days. Assuming that non-respondents continued to use tobacco, our results indicate a 7-day quit rate of 30.9% (95% CI: 19.6–42.1%). Among those who reported quitting (n=21), using a scale of 1 (not at all confident) to 10 (very confident), 48% (n=10) rated their confidence to remain quit between 6–9 and 52% (n=11) gave a rating of 10. Among those who did not quit (n=28), using the same scale, 25% (n=7) rated their confidence to quit between 1–5 and 71% (n=20) gave a rating of 6–10 (one participant did not answer). Also among those who did not quit (n=28), 78% (n=22) were in preparation to quit and 18% (n=5) were in precontemplation or contemplation (one participant did not answer). Of the socio-demographic measures in Table 2, only age differed statistically significantly between those who quit and those who did not; such that quitters were older compared to non-quitters (54.6 vs. 45.5 years, p<0.001). Of the organizational factors, job category differed significantly between those who quit and those who did not (skill/craft/machine operators: 36% quit; manual laborers: 10% quit; all other job types: 43% quit; p=0.04). Number of hours worked per week also differed significantly, such that quitters worked more hours compared to non-quitters (45.8 vs. 36.3 hours/week, p=0.02).
Perceived acceptability of Gear Up for Health-HWF is presented in Table 3. Of the factors listed in Table 3, only the perceived number of phone calls from the health counselor was significantly different between quitters and non-quitters, such that more quitters found the number of calls to be ‘just right’ compared to non-quitters (86% vs. 48%, p<0.01).
Table 3.
Acceptability of Gear Up for Health-HWF, overall and according to quit status, n=49a
| Acceptability variables | n (%) | Quit | Did not quit | Original Gear Up for Health |
|---|---|---|---|---|
|
| ||||
| Read the written intervention materials | ||||
| Most or all | 38 (83) | 17 (85) | 21 (81) | 78% |
| A little or some | 8 (17) | 3 (15) | 5 (19) | 22% |
|
| ||||
| Helpfulness of materials to set goals or to quit | ||||
| Very | 22 (47) | 9 (45) | 13 (48) | 44% |
| Not at all/neither/somewhat | 25 (53) | 11 (55) | 14 (52) | 56% |
|
| ||||
| Helpfulness of calls from health counselor | ||||
| Very | 28 (58) | 13 (62) | 15 (56) | 62% |
| Not at all/neither/somewhat | 20 (42) | 8 (38) | 12 (44) | 38% |
|
| ||||
| Number of phone calls | ||||
| Just right | 31 (65) | 18 (86) | 13 (48) | 81% |
| Not enough | 13 (27) | 3 (14) | 14 (52)b, c | 19% c |
| Too many | 4 (8) | |||
Numbers may not add up due to missing data; %s may not sum to 100 due to rounding
Association is statistically significant (p<0.01)
‘not enough’ is combined with ‘too many’ calls
Discussion
Based on a series of adaptations to an evidenced-based health program, Gear Up for Health-HWF is a tobacco use cessation program administered to unionized primarily blue-collar workers through a partnership with a Health and Welfare Fund health benefits carrier. The reported tobacco use quit rate was 30.9% (95% CI: 19.6–42.1%). Among those who did not quit, self-efficacy to quit in the future was high and the majority of participants were in preparation stage of change. As postulated in the Transtheoretical Model, high self-efficacy, increasing pros and decreasing cons of change, and progression (often non-linear) through the stages of change, and specific activities or processes of change is associated with quitting in the future.15
Compared to the original Gear Up for Health, our findings indicate that Gear Up for Health-HWF had similar and relatively high levels of implementation, effectiveness, and acceptability (see Table 3, column 5). For example, in Gear Up for Health-HWF vs. the original Gear Up for Health, the percent of participants who completed most of the counseling calls was 69% vs. 63%16. In addition, the 7-day quit rate (23.8%) from the original Gear Up for Health is within the 95% confidence interval of Gear Up for Health-HWF.7
One issue in dissemination research is the lack of good data on the target population. Although we attained a low level of reach (68 out of approximately 7,000 members, including smokers and nonsmokers, or 1%), it is in line with other studies that used mailed flyers to recruit employees into a behavioral trial.17 Because the HWF did not maintain records on tobacco use among members, we were precluded from implementing targeted recruitment efforts which would have maximized our monetary resources for recruitment. It also precluded us from calculating a more precise estimate of reach since our denominator included both eligible and non-eligible individuals. By calculating the unweighted mean of current smoking prevalence from the 2010 Behavioral Risk Factor Surveillance Survey18 for the five New England states in which members reside covered by the HWF (mean=16.1%), we can estimate that approximately 1,127 (7000 × 0.161) HWF individuals were current smokers. Thus, a more precise estimate (6%) of reach may be considered. This revised reach percentage (6%) is the goal set forth by the North American Quitline Consortium to reduce tobacco-related disease morbidity and mortality.19 Even with these relatively low levels of reach, dissemination of a tobacco intervention among blue-collar workers (who have higher risks of joint exposure to occupational hazards and tobacco use compared to other workers20) may still be worthwhile given appropriate monetary resources and support from the worksite dissemination partner.
A second issue is to determine which aspects of the intervention can be changed and still maintain their effectiveness. Examination of core and modifiable intervention elements suggested that we could reduce the number of counseling calls from 5 to 4, which may have resulted in a lower percentage of participants in the Gear Up for Health-HWF study who found the number of calls to be “just right” compared to the original Gear Up for Health. In addition, perceiving the number of calls to be just right was related to quitting in Gear Up for Health-HWF. As noted by Bowen and colleagues, one aspect of dissemination research that has received little attention is examining whether flexibility in intervention delivery (e.g., the number of counseling calls) should be built into intervention design for different settings.2 It could be that the more diverse worker categories targeted in Gear Up for Health-HWF (compared to the original Gear Up for Health which targeted mobile workers only) may have resulted in a greater need for flexible intervention content delivery. Our finding that quitting tobacco use differed among job categories also points to the need to examine flexible intervention content delivery further.
A third issue is the degree to which the ‘pull’ from the HWF vs. the ‘push’ from the disseminator has an impact on intervention effectiveness.2 While we collaborated with the Teamsters Union and a HWF, we approached the HWF with our research ideas and the study was primarily delivered by our research staff (i.e., we designed and delivered the written materials; our health educators conducted the counseling calls). As opposed to arising solely from the needs of the Health and Welfare Fund itself, our dissemination perspective was primarily a research-to-practice model, as discussed by Wandersman and colleagues.4 In fact, within the HWF, a previous experience with a health management company wishing to deliver a tobacco control intervention to their members had very low enrollment and left a poor impression of working with outside health promotion entities. Further examination of intervention factors (e.g., continuous vs. one-time programs) that would increase the degree of ‘pull’ from the organization are important areas for future research.
Limitations
Although there are notable strengths to this study including the inclusion of multiple measures of contextually relevant information (e.g., reach, implementation), use of evidenced-based behavioral change techniques (e.g., motivational interviewing based coaching, tailored materials), there are also weaknesses. Tobacco use cessation was self-reported and biochemical verification was not obtained. Biochemical verification of quitting may reduce trust among participants in workplace settings in which testing for other drugs can already be common.7 While biochemical verification provides added precision, its value may be off-set in studies in which data collection occurs primarily through telephone and Internet channels,21 as is the case in our study of participants spread over multiple worksites in different states. Our sample size is also small, which limits the generalizability of our data. We also did not include a control group, which limits our ability to isolate the specific effects of our program. However, we believe our research design is in line with current calls for designs beyond the traditional randomized trial3 and contributes to the understanding of low-cost, feasible recruitment and evaluation methods. We also provide only short-term follow-up of a one-time tobacco use cessation program, thus our results can not directly speak to long-term implications for tobacco control.
Conclusion
Adapted from an evidenced-based worksite program, Gear Up for Health-HWF was a tobacco use cessation program resulting from a union-management collaboration and disseminated to workers and their dependents through an overarching HWF. Given the caveats of self-reported tobacco use and a small sample size with no control group, we found relatively high levels of implementation, effectiveness, and acceptability which were similar to the results obtained from the original Gear Up for Health. Even though a low level of reach was obtained, implementing a telephone counseling program with tailored/targeted materials may still have value to a HWF wishing to deliver a tobacco use cessation program to their members, particularly if the costs are distributed over many members and the program is in line with their organizational mission. Future work in this area should examine moderators (e.g., organizational readiness) of adoption of health programs in HWFs and other organizations that could serve the large adult working population in general, and the higher-risk blue-collar population, in particular.
Acknowledgments
Source of Funding: This work was conducted with the support of a grant from the Centers for Disease Control and Prevention (grant number 5 R01 DP001171 to G.S.) and grants from the National Institutes of Health (grant numbers 2 K05 CA108663 and 5 R25 CA057711 to G.S.).
Footnotes
This work would not have been possible without the contributions of the members and leaders of the International Brotherhood of Teamsters and the selected Health and Welfare Fund.
Conflicts of Interest
The authors do not declare any conflicts of interest.
Contributor Information
Lisa Quintiliani, Email: lmquinti@bu.edu, Department of Medicine, Boston University, Boston MA.
Anne Stoddard, Email: astoddard@neriscience.com, Center Statistical Analysis & Research, New England Research Institutes, Watertown MA.
Ruth Lederman, Email: ruth_lederman@dfci.harvard.edu, Center for Community-based Research, Dana-Farber Cancer Institute, Boston MA.
Elizabeth Harden, Email: Elizabeth_harden@dfci.harvard.edu, Center for Community-based Research, Dana-Farber Cancer Institute, Boston MA.
Lorraine Wallace, Email: Lorraine_wallace@dfci.harvard.edu, Center for Community-based Research, Dana-Farber Cancer Institute, Boston MA.
Glorian Sorensen, Email: glorian_sorensen@dfci.harvard.edu, Center for Community-based Research, Dana-Farber Cancer Institute, Boston MA; Professor Department of Health and Social Behavior, Harvard School of Public Health, Harvard University, Boston MA.
References
- 1.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 2.Bowen DJ, Sorensen G, Weiner BJ, et al. Dissemination research in cancer control: where are we and where should we go? Cancer Causes Control. 2009;20(4):473–485. doi: 10.1007/s10552-009-9308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler R, Glasgow RE. A proposal to speed translation of healthcare research into practice: dramatic change is needed. Am J Prev Med. 2011;40(6):637–644. doi: 10.1016/j.amepre.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 4.Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3–4):171–181. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 5.Rabin BA, Glasgow RE, Kerner JF, Klump MP, Brownson RC. Dissemination and implementation research on community-based cancer prevention: a systematic review. Am J Prev Med. 2010;38(4):443–456. doi: 10.1016/j.amepre.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 6.Sparling PB. Worksite health promotion: principles, resources, and challenges. Prev Chronic Dis. 2010;7(1):A25. [PMC free article] [PubMed] [Google Scholar]
- 7.Sorensen G, Stoddard A, Quintiliani L, et al. Tobacco use cessation and weight management among motor freight workers: results of the gear up for health study. Cancer Causes Control. 2010;21(12):2113–2122. doi: 10.1007/s10552-010-9630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: a social-contextual model for reducing tobacco use among blue-collar workers. Am J Pub Health. 2004;94(2):230. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McKleroy VS, Galbraith JS, Cummings B, et al. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18(4 Suppl A):59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- 10.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am J Pub Health. 1999;89(9):1322. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boyle L, Homer M. Using What Works: Adapting Evidence-Based Programs to Fit Your Needs. National Cancer Institute; No date. [Google Scholar]
- 12.Prochaska J, DiClemente C. Self-Change Processes, Self-Efficacy and Decisional Balance across Five Stages of Smoking Cessation. New York, NY: Alan R. Liss, Inc; 1983. [PubMed] [Google Scholar]
- 13.National Institute for Occupational Safety and Health. Quality of worklife questionnaire. 2002 Available at: http://www.cdc.gov/niosh/topics/stress/pdfs/QWLsurvey.pdf.
- 14.Hays R, Stewart A. Sleep Measures. In: Stewart AL, Wares JE, editors. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992. pp. 235–259. [Google Scholar]
- 15.Prochaska J, Redding C, Evers K. Health Behavior and Health Education: Theory, Research, and Practice. 4. San Francisco, CA: Jossey; 2008. The Transtheoretical Model and Stages of Change; pp. 97–121. [Google Scholar]
- 16.Quintiliani L, Yang M, Sorensen G. A process evaluation of tobacco-related outcomes from a telephone and print-delivered intervention for motor freight workers. Addict Behav. 2010;35(11):1036–1039. doi: 10.1016/j.addbeh.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Kiernan M, Phillips K, Fair JM, King AC. Using direct mail to recruit Hispanic adults into a dietary intervention: An experimental study. Ann Behav Med. 2000;22(1):89–93. doi: 10.1007/BF02895172. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control. Behavioral Risk Factor Surveillance System. 2010 Available at: www.cdc.gov/brfss.
- 19.Bronar C, Saul J. Increasing reach of tobacco cessation quitlines: A review of the literature and promising practices. North American Quitline Consortium; Phoenix, AZ: 2009. [Google Scholar]
- 20.Sorensen G, Stoddard A, Hammond SK, et al. Double jeopardy: Workplace hazards and behavioral risks for craftspersons and laborers. Am J Health Promot. 1996;10(5):355–363. doi: 10.4278/0890-1171-10.5.355. [DOI] [PubMed] [Google Scholar]
- 21.Benowitz NL, Jacob P, Ahijevych K, et al. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4(2):149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]