Introduction
Hemophagocytic syndrome (HPS) is a rare, fatal disorder, presenting with fever, pancytopenia, liver dysfunctions, hepatosplenomegaly, hypertriglyceridemia, and hyperferritinemia [1]. HPS may be primary related to genetic mutations or secondary to various infections, malignancies and rheumatic conditions [2]. These antigenic stimuli cause uncontrolled immune reaction with a cytokine storm and activated macrophages that can be fatal. Anecdotal reports of pregnancy-induced HPS are available [3, 4]. We report a case of pregnancy induced HPS which was almost fatal for the mother but she recovered after spontaneous abortion.
Case Report
We hospitalized a 23-year-old pregnant woman (primigravida) at 10th week of gestation with complaints of intermittent fever for 2 weeks. Fever was of moderate grade. It was associated with night sweats, body aches, fatigability, and jaundice. Physical examination revealed that she was febrile. The pulse was 80/min regular and blood pressure was 110/60 mm Hg. She was pale. There were no skin rashes, joint pains, or lymphadenopathy. Liver and spleen were enlarged and palpable, and tender.
Hemogram showed hemoglobin 6.3 gm/dl, total leukocyte count 1880/mm3 and platelets 18,000/mm3. Renal functions were normal. Liver biochemistry showed hyperbilirubinemia (total 3.5 mg/dl and direct fraction of 2.2 mg/dl) and raised serum ALP (1254 U/l). Other liver enzymes were normal. Serum LDH raised (4550 U/l) markedly. Blood and urine cultures, peripheral smear for malarial parasites and sputum AFB were not contributory. Chest skiagram was normal. Serology for hepatitis viruses (B and C), HIV, EBV, malaria, brucella and kala azar was negative. Real-time quantitative polymerase chain reaction for EBV DNA was also negative. CECT chest and abdomen showed enlargement of both liver and spleen. Serum ferritin was >2,200 ng/ml. Serum triglyceride was 588 mg/dl. Antinuclear antibody (immuno-floresence) titer was absent.
We did liver biopsy. It showed a single non-caseating granuloma (Fig. 1) that was negative for acid-fast bacilli. Bone marrow examination revealed evidence of haemophagocytosis with multiple deficiency anemias (Fig. 2). Fever, pancytopenia, hepatosplenomegaly, hyperferritinemia, hypertriglyceridemia and hemophagocytosis in bone marrow present in this patient, suggested the diagnosis of hemophagocytic syndrome.
Fig. 1.
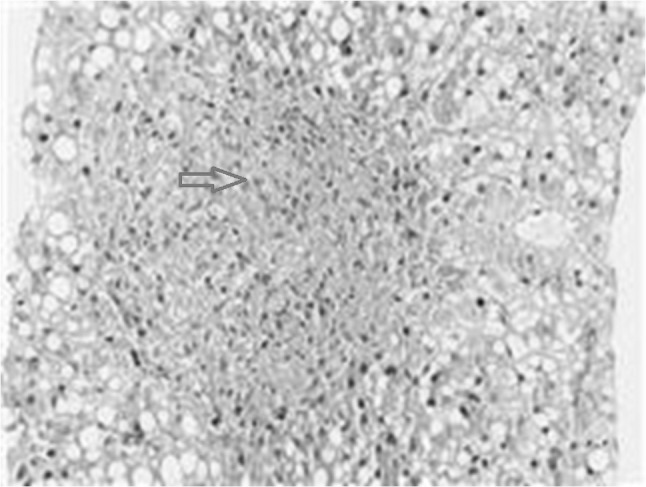
Histopathology of liver biopsy showed a solitary non-caseating granuloma (open arrow)
Fig. 2.
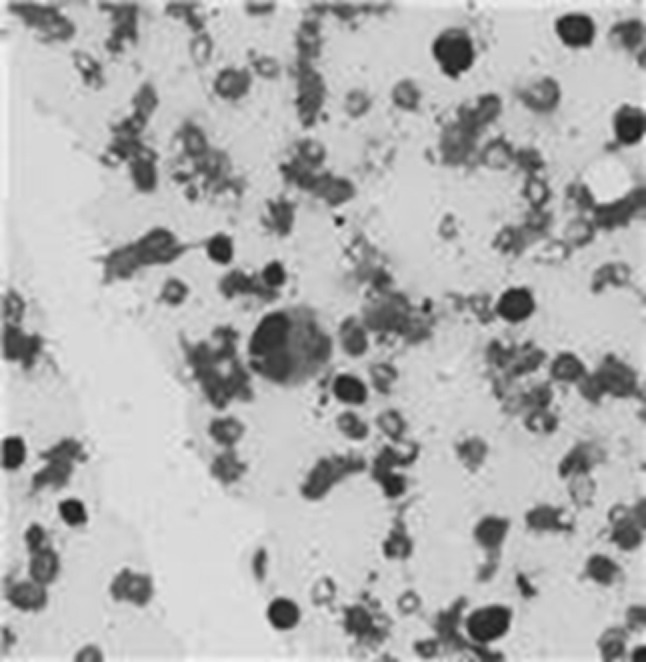
Histopathology of bone marrow aspiration showing haemophagocytosis
She had prednisolone (1 mg/kg) for 3 days. However her general condition deteriorated. She had vaginal bleeding, and aborted spontaneously. Obstetrician evacuated retained products of conception. Patient started improving the next day. Fever decreased in intensity and subsided in 2–3 days. Hepatomegaly and splenomegaly regressed within a week. Her deranged blood chemistry reversed to normal after 2 weeks. Once she started improving, we stopped the steroids. For last 6 months, there is no recurrence and she is asymptomatic.
Discussion
Hemophagocytic lymphohistiocytosis (HLH) is a rare but potentially fatal disease of normal but overactive histiocytes and lymphocytes that commonly appears in infancy, although any age group may be affected. Fever, hepatosplenomegaly, pancytopenia, lymphadenopathy, and skin rashes often comprise the initial presentation [1]. There is accumulation of activated non-malignant macrophages in reticuloendothelial system that undergoes uncontrolled phagocytosis of normal hematopoietic cells. Clinical severity ranges from complete recovery to rapid deterioration and death. HPS may be primary, as observed in familial HPS, X-linked lymphoproliferative syndrome and Chediak-Higashi syndrome or it may be secondary to malignancies (particularly lymphoma), infections (mainly EBV), autoimmune diseases or drugs [2]. Few reports of pregnancy induced HPS are available in the retrieved literature [3, 4].
We report a case of HPS in pregnant woman. Since she had fever, pancytopenia, hepatosplenomegaly, hyperferritinemia, hypertriglyceridemia and hemophagocytosis in bone marrow, the diagnosis of hemophagocytic syndrome was considered [1].
Subsequent to spontaneous abortion, she showed dramatic recovery. This suggested that her disease was related to her pregnancy. Steroids given to her were unrelated to the improvement of disease. Subsequently her disease did not recur. Investigations and clinical profile (no recurrence) ruled out possibility of malignancy, chronic infection like tuberculosis and autoimmune disease.
The pathophysiology of pregnancy induced HPS is not clear. Placenta and fetus have different genetic makeup from the mother and in theory they are at risk of attack from her immune system. In fact, they may be an unusually successful allograft. The placenta functions as an immunological barrier between the mother and the fetus, creating an immunologically privileged site. It uses several mechanisms like Neurokinin B secretion, trophoblast cells lacking typical HLA class I isotypes with syncytium formation, and blocking all maternal antibodies (except IgG) [5]. Still, the placental barrier is not the sole means to evade the immune system, as foreign fetal cells also persist in the maternal circulation on the other side of the placental barrier [6].
Many cases of spontaneous abortion may be present in the same way as maternal transplant rejection. Earlier few authors have hypothesized the feto-maternal trafficking [4]. The evidence came from preeclampsia [7]. Preeclampsia is a form of maternal immune rejection of the genetically foreign fetus due to unsuccessful maternal T-lymphocyte recognition of fetomaternal human lymphocyte antigens. Immature placenta releases trophoblast debris, including syncytiotrophoblast components, soluble RNA, and DNA of fetal origin and even cytotrophoblast cells, into the maternal circulation. This feto-maternal trafficking induces a profound systemic inflammatory response leading to a cytokine storm, mimicking pregnancy-induced HPS [8].
Non-caseating hepatic granuloma in our patient was probably a component of uncontrolled immune system activation. Infections (tuberculosis, brucellosis, and fungus), malignancy (lymphomas), autoimmune diseases (sarcoidosis), and drugs may cause granulumatous hepatitis [9]. Absence of skin rashes and lympadenopathy were not present in the present patient. Therefore their presence is not essential to make the diagnosis of hemophagocytic syndrome.
Thus, the defect in the functioning of placenta as an immunological barrier and feto-maternal trafficking led to an uncontrolled immune reaction to cause HPS in the mother that terminated with spontaneous abortion in our patient. As the termination of the foreign antigen (feto-placental unit) did occur, the immune reaction subsided with complete recovery of disease.
To conclude, the differential diagnosis of pregnant women with fever and pancytopenia should include HPS. Termination of pregnancy might be a distinct therapeutic option. Absence of skin rashes and lympadenopathy is not essential to make the diagnosis of HPS.
References
- 1.Henter JI, Elinder G, Ost A. Diagnostic guidelines for hemophagocytic lymphohistiocytosis. The FHL Study Group of the Histiocyte Society. Semin Oncol. 1991;18:29–33. [PubMed] [Google Scholar]
- 2.Takahashi N, Chubachi A, Kume M, et al. A clinical analysis of 52 adult patients with hemophagocytic syndrome: the prognostic significance of the underlying diseases. Int J Hematol. 2001;74:209–13. [DOI] [PubMed]
- 3.Chmait RH, Meimin DL, Koo CH, et al. Hemophagocytic syndrome in pregnancy. Obstet Gynecol. 2000;95:1022–4. [DOI] [PubMed]
- 4.Teng CL, Hwang GY, Lee BJ, Wang RC, Chou MM. Pregnancy-induced hemophagocytic lymphohistiocytosis combined with autoimmune hemolytic anemia. J Chin Med Assoc. 2009;72:157–159. doi: 10.1016/S1726-4901(09)70043-7. [DOI] [PubMed] [Google Scholar]
- 5.Lowry P. Placenta ‘fools body’s defences’—devising a mechanism by which you could make cells invisible to the immune system could lead to cures for a number of diseases and conditions (University of Reading). BBC NEWS 10 November 2007. Available from URL: www.bbc.co.uk/2/hi/health/7081298.stm. Retrieved on 14.04.2011.
- 6.Williams Z, Zepf D, Longtine J, et al. Foreign fetal cells persist in the maternal circulation. Fertil Steril. 2008;91:2593–2595. doi: 10.1016/j.fertnstert.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Moffett-King A. Natural killer cells and pregnancy. Nat Rev Immunol. 2002;2:656–663. doi: 10.1038/nri886. [DOI] [PubMed] [Google Scholar]
- 8.Redman CW, Sargent IL. Pre-eclampsia, the placenta, and the maternal systemic inflammatory response: a review. Placenta. 2003;24:S21–S27. doi: 10.1053/plac.2002.0930. [DOI] [PubMed] [Google Scholar]
- 9.Behnava B. Diagnostic challenge: hepatic granulomas associated with FUO. Hepatitis Monthly. 2005;5:153–154. [Google Scholar]


