Abstract
Context
The quality of health care and the financial costs affected by receiving care represent two fundamental dimensions for judging health care performance. No existing conceptual framework appears to have described how quality influences costs.
Methods
We developed the Quality-Cost Framework, drawing from the work of Donabedian, the RAND/UCLA Appropriateness Method, reports by the Institute of Medicine, and other sources.
Findings
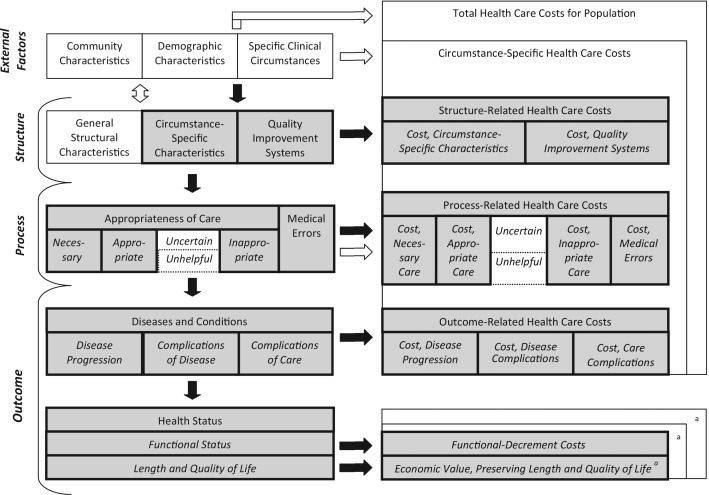
The Quality-Cost Framework describes how health-related quality of care (aspects of quality that influence health status) affects health care and other costs. Structure influences process, which, in turn, affects proximate and ultimate outcomes. Within structure, subdomains include general structural characteristics, circumstance-specific (e.g., disease-specific) structural characteristics, and quality-improvement systems. Process subdomains include appropriateness of care and medical errors. Proximate outcomes consist of disease progression, disease complications, and care complications. Each of the preceding subdomains influences health care costs. For example, quality improvement systems often create costs associated with monitoring and feedback. Providing appropriate care frequently requires additional physician visits and medications. Care complications may result in costly hospitalizations or procedures. Ultimate outcomes include functional status as well as length and quality of life; the economic value of these outcomes can be measured in terms of health utility or health-status-related costs. We illustrate our framework using examples related to glycemic control for type 2 diabetes mellitus or the appropriateness of care for low back pain.
Conclusions
The Quality-Cost Framework describes the mechanisms by which health-related quality of care affects health care and health status–related costs. Additional work will need to validate the framework by applying it to multiple clinical conditions. Applicability could be assessed by using the framework to classify the measures of quality and cost reported in published studies. Usefulness could be demonstrated by employing the framework to identify design flaws in published cost analyses, such as omitting the costs attributable to a relevant subdomain of quality.
Keywords: quality of health care; economics; cost-benefit analysis; models, theoretical; diabetes mellitus, type 2
When assessing a health care system or a facet of care, the fundamental dimensions of performance should include the quality of the care provided and the economic costs related to receiving that care. The U.S. health care system does not function well on either dimension. The most comprehensive study of quality to date found that for adults, care adhered to basic recommendations about what should or should not be done only 55 percent of the time (McGlynn et al. 2003). Although health outcomes in the United States lag far behind those in Canada, Australia, Germany, France, and the United Kingdom, in 2009, per-capita health care expenditures were about twice as high (Commonwealth Fund Commission 2011). Policymakers and observers have recently become hopeful, however, about the possibility of improving quality while simultaneously saving money (IOM 2010a, 2010b, 2010c). Accordingly, numerous studies have examined the costs attributable to poor quality, the relationship between performance on quality measures and health care expenditures, and the costs and health effects associated with improvement programs. Several new policies have been designed to spur improvements in quality and reduce health care costs in the United States, such as establishing accountable care organizations, incentives for adopting health information technology, and penalties for hospital-acquired complications (Berwick 2011; Blumenthal 2011; Kaushal et al. 2006; Milstein 2009).
When policymakers, researchers, and other decision makers work on a policy issue like this one, a shared framework can create a common understanding of the issues and facilitate the design of analyses. We know of no conceptual model or framework, however, that describes how specific dimensions of quality produce variations in health care and other types of costs. Even so, the authors of well-known conceptual models addressing quality have contemplated economic matters. Donabedian excluded costs from his well-known quality-of-care model, choosing to focus on clinical issues rather than value-laden questions of balancing costs against health benefits (Donabedian 1980). Yet during the same time period, he published several articles on health care costs, including one describing a production function for health outcomes at different expenditure levels (Donabedian, Wheeler, and Wyszewianski 1982). In 2001, the Institute of Medicine (IOM) defined six dimensions of quality: effectiveness, safety, efficiency, timeliness, patient-centeredness, and access (IOM 2000, 2010a). Effectiveness and safety relate to increasing the likelihood of favorable health outcomes. Efficiency is an economic construct, which the IOM defines as maximizing performance (i.e., health care outcomes) by producing the best possible outputs from a given set of resources or inputs (IOM 2010a). In the field of health economics, several conceptual frameworks focus on efficiency, but agreement about how to define efficiency and the related concept, value, is limited (AQA 2006; IOM 2009, 2010a; McGlynn 2008; Medicare Payment Advisory Commission 2006; National Quality Forum 2010; Palmer and Torgerson 1999). Yet none of these works describes how quality influences costs or efficiency.
The lack of such a conceptual framework creates a confusing situation in which numerous analyses purport to examine quality and costs but each analysis measures something different from the next. Table 1 illustrates this phenomenon using examples of studies addressing glycemic control for type 2 diabetes mellitus over the long term or the treatment of uncomplicated low back pain. Some studies report structural measures of quality, such as implementing an integrated program that helps primary care physicians manage diabetes, along with the costs of conducting the program. Others describe process measures, such as adhering to guidelines that recommend active modalities for physical therapy for low back pain, and estimate associated health care expenditures. Finally, some authors have estimated changes in health outcomes and outcome-related costs, such as reductions in macrovascular complications with improved glycemic control and the associated health care and disability costs. While there are valid reasons for choosing different measures of quality and costs, a conceptual framework would make it easier to understand the selections made. A framework would also remind researchers of variables that may be conceptually relevant, preventing their inadvertent omission from an analysis.
TABLE 1.
Examples of Studies Addressing the Quality of Glycemic Control among People with Type 2 Diabetes Mellitus or Quality of Care for Low Back Pain and Some Measure of Cost
| Study | Description of Study |
|---|---|
| Studies of Associations between Measures of Quality and Measures of Cost in Patient Populations | |
| Fritz et al. 2008 | Methods: Determined whether or not patients with low back pain had received physical therapy services that adhered to guidelines (involved exercise or therapeutic activities). |
| Key Findings: The 28.0% of patients receiving guideline-adherent care had $202 lower physical therapy charges. During the year following physical therapy care, receiving adherent care was associated with a lower likelihood of receiving prescription medication (46.2% vs. 57.2%), magnetic resonance imaging (8.3% vs. 15.9%), or epidural injections (5.3% vs. 12.1%); charges were not significantly different ($2,049 vs. $3,427) (inflated to 2009 dollars). | |
| Measures of Quality: Modified Oswestry Disability Questionnaire, pain rating scale, duration of physical therapy care, receipt of care during the year after physical therapy care. | |
| Measures of Cost: Number of physical therapy visits, physical therapy charges, charges associated with CPT codes for low back pain and collected for prescription medication, office or emergency room visits, inpatient/surgical services, and diagnostic procedures. | |
| Menzin et al. 2001 | Methods: Assigned adult members of the Fallon Clinic to three groups based on HbA1c: good (<8%), fair (8 to 10%), and poor control (>10%). Compared inpatient admissions for various complications and associated charges across the groups. |
| Key Findings: Over three years, the adjusted rate of inpatient treatment per 100 patients was 13 for good, 16 for fair, and 31 for poor control. Corresponding mean adjusted charges were $1,507, $2,145, and $4,724, respectively. Among the 30% of subjects with long-term diabetic complications, the adjusted admissions per 100 patients (mean charges) were estimated to be 30 ($4,056) for good, 38 ($5,921) for fair, and 74 ($12,930) for poor control, respectively (inflated to 2009 dollars). | |
| Measures of Quality: HbA1c test result category (< 8%, 8 to 10%, >10%). | |
| Measures of Cost: Mean adjusted charges for inpatient care (hospital and skilled nursing facility) over three years. | |
| Studies Estimating the Cost of Existing Quality Problems | |
| Caro, Ward, and O'Brien 2002 | Methods: Used a model based on existing epidemiologic studies to create a simulated cohort of 10,000 patients with diabetes, estimating complication rates for macrovascular disease, nephropathy, retinopathy, neuropathy, and hypoglycemia. Estimated the direct medical costs associated with the complications from all-payer databases, surveys, and literature. |
| Major Findings: The average per-patient medical care costs for diabetes-related complications over thirty years were $68,037, largely due to macrovascular disease (inflated to 2009 dollars). | |
| Measures of Quality: Modeled risk of macrovascular disease, nephropathy, retinopathy, neuropathy, and hypoglycemia over thirty years. | |
| Measures of Cost: Modeled cumulative average cost of diabetes-related complications per patient over thirty years. | |
| Minshall et al. 2005 | Methods: Used the CORE diabetes model to estimate the long-term savings associated with averting the major complications that result from diabetes, modeling attaining HbA1c goals of <7% and <6.5% versus current population values. |
| Key Findings: Reducing the average HbA1c to 7% nationwide would eliminate $39.8 billion (inflated to 2009 dollars) in direct medical expenditures for type 2 diabetes-related complications over ten years, plus an additional $17.2 billion in costs related to disability, lost productivity, and premature mortality. | |
| Measures of Quality: HbA1c test result over ten years, modeled risk of fifteen diabetes-related complications and nonspecific mortality over ten years. | |
| Measures of Cost: Modeled direct medical care expenses over ten years; modeled costs associated with lost productivity, premature mortality, and disability over ten years. | |
| Studies of Efforts to Change Quality That Included Measures of Cost | |
| Kotsos et al. 2009 | Methods: Enrolled patients from a large insurer in a nurse-led disease management program that emphasized self-care for low back pain. Compared outcomes with controls from a period preceding the program. |
| Key Findings: Costs per diseased member per month were lower during the intervention period for imaging, surgery, and medications. | |
| Measures of Quality: Existence of nurse-led self-care disease management program. | |
| Measures of Cost: Program costs per diseased member per month for low-back pain specific services, including physical therapy, imaging, manipulation, steroid injections, surgery, and medications. | |
| Monte et al. 2009 | Methods: Patients were referred to the MedSense program, a pharmacist-led, patient-centered pharmacotherapy management program. For one year from the enrollment date, followed HbA1c and other metabolic parameters as well as medical and prescription-related costs. |
| Key Findings: HbA1c declined by 1.1% at twelve months. Other accompanying metabolic parameters improved by 40% to 64%. By twelve months, mean costs decreased by $222 relative to baseline (inflated to 2009 dollars). | |
| Measures of Quality: Existence of a pharmacist-led, patient-centered pharmacotherapy management program, HbA1c test result, fasting glucose test result, outcomes for diabetes unrelated to glycemic control, use of medication (aspirin, ACE/ARB, statin, insulin), use of nephropathy screening. | |
| Measures of Cost: Direct medical and prescription expenditures from the payer perspective. | |
| Studies Determining the Cost-Effectiveness of Efforts to Change Quality | |
| Kahn et al. 2008 | Methods: Used NHANES data for 1998 to 2004 and the Archimedes model to estimate the cost-effectiveness of the maximum feasible attainment of HEDIS HbA1c goals for diabetes over thirty years. |
| Key Findings: The maximum feasible attainment over thirty years would cost $56,666/quality-adjusted life year (inflated to 2009 dollars). | |
| Measures of Quality: HbA1c test result <7%, fasting plasma glucose test result <110 mg/dl, incidence of hypoglycemic attacks, body mass index <30 kg/m2, control of cardiovascular disease risk factors, quality-adjusted life years. | |
| Measures of Cost: Cost of prevention activities over thirty years, assuming maximum feasible performance (with subcategories for HbA1c, fasting plasma glucose, etc.), total cost of preventive plus other medical care over thirty years, total cost per quality-adjusted life year (did not consider cost of any quality improvement activities). | |
| McRae et al. 2008 | Methods: Assessed the cost effectiveness of an integrated approach to assisting general practitioners (GPs) with diabetes management in Australia using five years of data from the program and the UKPDS Outcomes Model. |
| Key Findings: Most clinical measures improved or were unchanged over five years. The program led to projected improvements in expected life years and Quality Adjusted Life Expectancy (QALE), with incremental cost effectiveness ratios of $A8,106 per life year saved and $A9,730 per year of QALE gained. | |
| Measures of Quality: Existence of integrated approach to assisting general practitioners with diabetes management, HbA1c test result, control of cardiovascular disease risk factors, life years, quality-adjusted life expectancy. | |
| Measures of Cost: Costs of integrated approach program, costs of primary care services arising from adherence to the guidelines and drug costs, hospitalization costs, cost per quality-adjusted life expectancy. | |
| Strong et al. 2006 | Methods: Two randomized controlled trials in a large health maintenance organization enrolled adults who were not being considered for surgery in group educational programs on self-care, one led by laypersons and the other by psychologists. |
| Key Findings: Patients assigned to the lay and psychologist groups had 14.3 and 26.2 additional low-impact back pain days, respectively, compared with usual care. Each additional low-impact back pain day cost $9.70 and $6.13 for the lay-led and psychologist-led interventions, respectively. | |
| Measures of Quality: Roland Disability Score, “low impact days.” | |
| Measures of Cost: Intervention costs (labor, mailing costs), total costs of back pain care in the one-year postrandomization (costs of back pain-related services, excluding inpatient care), net cost per “low impact day.” | |
Note: Costs were inflated to 2009 dollars using the Consumer Price Index (Bureau of Labor Statistics 2012).
Given these considerations, we offer the Quality-Cost Framework. For examples, we used studies of glycemic control for type 2 diabetes and of the treatment of low back pain. We selected these conditions because they are common; their care affects clinical outcomes as well as associated costs; and some quality problems and interventions have been well studied.
Before describing the Quality-Cost Framework, we must define quality of care and costs because the terms’ connotations vary (Donabedian 1980). Our framework emphasizes “health-related quality,” which we define by drawing from Donabedian's 1982 exposition on quality and costs: “The highest quality care is that which yields the greatest expected improvement in health status, health being defined broadly to include physical, physiological, and psychological dimensions” (Donabedian, Wheeler, and Wyszewianski 1982, 976). Our framework distinguishes health-related from non-health-related dimensions of quality (those not expected to affect health) for three reasons: (1) improving health is the fundamental objective of health care; (2) health-related and non-health-related dimensions of quality influence costs differently; and (3) the two types of dimensions can sometimes be negatively associated.
Consider, for example, satisfaction, an important dimension of quality from the patient's perspective (Browne et al. 2010). Satisfaction appears to have both health-related and non-health-related components. Some studies show that higher satisfaction is associated with better health outcomes, yet perhaps surprisingly, other investigations have found the reverse, including one nationwide study that found higher patient satisfaction with outpatient care was associated with increased mortality (Browne et al. 2010; Fenton et al. 2012). On the one hand, patient satisfaction promotes adherence to treatment (Browne et al. 2010), which should improve outcomes. On the other hand, providers sometimes face stark choices between promoting satisfaction and optimizing health. One example is deciding whether to discontinue opioids for patients with chronic, noncancer pain who exhibit vague signs of misuse, which may indicate an increased risk for addiction and overdose. In addition to occasionally conflicting with the goal of improving health, striving to improve satisfaction can also promote discretionary health care expenditures. Amenities such as concierge services, luxury waiting areas, and gourmet hospital meals increase discretionary health care expenditures but produce no health benefits. Both patients and society value—and may be willing to pay for—non-health-related dimensions of quality, including services that improve satisfaction but not physical or psychological health. Yet to facilitate distinctions between higher-value and lower-value health care, a framework examining the effect of quality on costs should distinguish non-health-related from health-related expenditures.
To define costs, the framework focuses on health care and health status–related costs. Health care costs are expenditures for health care and costs to patients and families, such as the value of time spent in care, self-care, and informal caregiving activities; and the expenditures related to these activities, such as for special diets. Health status–related costs are costs related to declines in the ability to function (which we refer to as “functional-decrement costs”), and the economic value associated with losses of quality and quantity of life. We discuss specific categories later.
Conceptual Framework
The objectives of the Quality-Cost Framework are to (1) explain how variations in health-related quality can create variations in health care and other economic costs and (2) facilitate the design and evaluation of empirical studies examining how quality influences costs (see figure 1). The framework builds on the work of Donabedian, RAND researchers, the Institute of Medicine, the standard methods for cost-effectiveness analyses, and the methods used in cost-benefit analyses outside the health care sector.
FIGURE 1.
Quality-cost framework.
Note: aOuter and inner boxes represent total and circumstance-specific functional-decrement costs, respectively.
We intend the framework to apply to a variety of analyses, including cost, cost-effectiveness, and econometric analyses. The quality and cost elements that are relevant to a particular analysis depend on its purpose, perspective, time horizon, patient population, target diseases or conditions, study design, and setting. The framework accommodates various units of analysis, such as the patient, service, episode, and complication.
Donabedian Model
The familiar Donabedian model is made up of structure, process, and outcome. Structure represents the resources used to provide care, like provider specialties, equipment, and institutional protocols. It also includes the formal and informal systems through which health care is financed and delivered, for example, health care policies, insurance markets, provider availability, and types of delivery systems. Process means the components of interactions between patients and providers, such as physical examination maneuvers, tests, and various forms of communication. Outcome is the patient's health status after receiving care as well as the incremental intermediate changes leading up to changes in health status. Structure influences process, and in turn, process influences outcome (Brook, McGlynn, and Cleary 1996; Donabedian 1966, 1980, 1982, 1985).
The Quality-Cost Framework draws on the Donabedian model with three modifications. First, we identified three external factors that influence both quality and cost but are not dimensions of quality: (1) the specific clinical indications or circumstances that set the care process in motion and define the target population, (2) the demographic characteristics of the target population, and (3) the characteristics of the community in which the health care system is functioning. Depending on the scope of the analysis, the specific clinical circumstances can be defined either broadly or narrowly. Broadly defined clinical circumstances would include adults who need primary care services; a narrower example would be diabetics with early nephropathy. In this article, we used glycemic control for type 2 diabetes and care for low back pain as examples of specific clinical circumstances. Demographic characteristics are the target population's age, gender, race, ethnicity, education, cultural values, and the like. By characteristics of the community, we mean determinants of health that reflect the setting beyond the target population characteristics, such as location, weather, employment opportunities, sanitation, transportation, and parks.
The second modification of the Donabedian model was adding subdomains to structure, process, and outcome, which we discuss in detail later. These subdomains might need to be modified or expanded in the future, if, for example, new categories of quality problems were identified as major causes of morbidity and mortality.
The third modification was, of course, extending the causal chain of events to encompass economic costs attributable to health-related quality issues. The subdomains of structure, process, and outcome each generate corresponding categories of economic costs, most of which are attributable to health-related quality issues (shaded in figure 1). Costs are categorized by the quality-of-care issues to which they are most immediately attributable. For example, if the level of quality associated with a subdomain changes, any costs that would be certain to change as a result are considered attributable costs, regardless of whether the costs entail equipment, other types of resources, or health care services. Table 2 provides examples for each external factor and subdomain in the framework.
TABLE 2.
Examples Illustrating Domains in Quality-Cost Framework, Drawing from Publications on Glycemic Control for Type 2 Diabetes Mellitus or Treatment of Low Back Pain
| Quality Element | Examples of External Factors or Quality Elements | Cost Associated with Example | Citations |
|---|---|---|---|
| External Factors | |||
| Community Characteristics | Country | Across four European countries, adherence to four overuse measures for low back pain was similar, but resource utilization and costs varied greatly. | Gandjour, Telzerow, and Lauterbach 2005 |
| Demographic Characteristics | Education Zip code (surrogate for income) Gender |
Education and zip code are associated with process measures of care for diabetes, HbA1c levels, and cost. Gender is associated with cost. | Bachmann et al. 2003; Brandle et al. 2003; Franks and Fiscella 2002 |
| Specific Clinical Circumstances | Time since diagnosis. | Both HbA1c and costs rise over time from diagnosis. | Trogdon and Hylands 2008; United Kingdom Prospective Diabetes Study Group et al. 2000 |
| Structure | Attributable Structure-Related Costs | ||
| General Structural Characteristics | Practice Structure: Large multispecialty group practice versus solo private practice. | Large groups will have greater market power and may be able to negotiate higher fees. | Berenson et al. 2012 |
| Practice Structure: Patient-centered medical home versus traditional practice. | Patients attending patient-centered medical homes were more likely to receive HbA1c tests and less likely to receive imaging tests for back pain, compared with traditional practices. | Devries et al. 2012 | |
| Medications: A tiered pharmacy benefit plan charges patients different amounts for brand and generic medications, but the tiers do not depend on diagnosis or medical necessity. | Tiers may discourage patients from using more costly medications. If those medications are more effective, short-term pharmaceutical costs would decline, but long-term costs of complications could increase. | N/Aa | |
| Circumstance-Specific Characteristics | Provider Services: Care by surgeons versus primary care doctors. | Cost differences would be due to visit utilization rates and cost per visit. Workers’ compensation patients who saw a surgeon first were 78% more likely to receive early magnetic resonance imaging than those who saw a primary care physician. | Graves et al. 2012 |
| Capital Expenditures: Purchasing a digital camera that takes retinal photographs would facilitate detection of diabetic retinopathy. | Costs represent the expenditure associated with purchasing a retinal imaging camera for retinopathy screening. | N/A | |
| Quality Improvement Systems | National Program: HEDIS program. | The costs associated with the HEDIS program include costs to NCQA as well as health plans’ monitoring costs. | N/A |
| Payer- or Provider-Based Program: Disease-management programs and patient-education programs. | Disease management programs cost $38 to $1,500 per person with diabetes annually (inflated to 2009 dollars). | Beaulieu, Cutler, and Ho 2006; Bureau of Labor Statistics 2012; Rothman et al. 2006; Sidorov et al. 2002 | |
| Of studies examining disease management programs, 36% found improvements in processes or outcomes for diabetes, and 16% did for back pain; cost decreased in 14% of studies. | Ofman et al. 2004 | ||
| Payer-Based Program: Pay-for-performance programs. | Some pay-for-performance programs for diabetes pay physicians 1.5% to 7.5% of fees, or an amount per member per month depending on the number of quality metrics attained. | Chen et al. 2010; Rosenthal et al. 2005; Young et al. 2007 | |
| Process | Attributable Process-Related Costs | ||
| Underuse of Necessary Care | Frequency of HbA1c Testing: Among diabetics in a national study, 17% had HbA1c tests every six months; 23% of these had an HbA1c ≥ 8% and, among them, 69% had providers recommend medication changes. Among those who received HbA1c tests less often, 41% had an HbA1c ≥ 8% and, among them, 26% had providers recommend medication changes. | Increasing HbA1c testing and medication adjustments from baseline to 100% of recommended rates would increase health care expenditures by $327 per person with diabetes annually (2009 dollars). | Nuckols et al. 2011 |
| Use of Appropriate Care | HbA1c Treatment Goal: American Diabetes Association encourages an HbA1c goal < 7% for many nonpregnant patients but leaves which patients to the discretion of providers due to the complexities of assessing the risks and benefits. | The additional cost of attaining this optional goal does not appear to have been compared with the cost of attaining the basic goal of < 8%. | American Diabetes Association 2011 |
| Acute Low Back Pain: American College of Physicians/American Pain Society guideline (weakly) recommends considering spinal manipulation when patients do not improve with self-care. | The attributable costs would be related to the utilization of spinal manipulation. | Chou et al. 2007 | |
| Use of Care of Uncertain Appropriateness | Medication for Diabetes: American Diabetes Association guideline discusses but makes no recommendation regarding the use of oral antihyperglycemic agents versus insulin among patients who are hospitalized. | Insulin requires much more frequent assessment of blood glucose and more frequent administration than oral agents do, so nursing costs are likely to be higher. | American Diabetes Association 2011 |
| Care for Low Back Pain: American College of Physicians/American Pain Society guideline notes that data are insufficient to recommend for or against interferential therapy, low-level laser therapy, shortwave diathermy, or ultrasonography; and data are inconsistent on back school. | The attributable costs would be related to the utilization of these services. | Chou et al. 2007 | |
| Use of Unhelpful Care | Primary Prevention of Diabetes: American Diabetes Association guideline recommends against using metformin to prevent diabetes among patients with impaired glucose tolerance and mild obesity because lifestyle changes are more effective. | Metformin is inexpensive. Lifestyle changes may be more effective, but the costs to patients in terms of time involved may be substantial, given the need to exercise regularly and manage a strict diet. | American Diabetes Association 2011 |
| Care for Low Back Pain: American College of Physicians/American Pain Society guideline notes that transcutaneous electrical nerve stimulation and traction have not been shown to be effective for chronic low back pain. | The attributable costs would be related to the utilization of these services. | Chou et al. 2007 | |
| Overuse of Inappropriate Care | American Heart Association guideline recommends against routine radionuclide stress testing for patient over age forty with diabetes without symptoms and with a negative test within two years. Risks include radiation exposure and false positive results, which may lead to cardiac catheterization. | A nuclear stress test costs $549.98. | Hendel et al. 2009; Medicare Physician Fee Schedule Look-Up |
| Imaging for Low Back Pain: American College of Physicians/American Pain Society guideline recommends against imaging for patients with uncomplicated low back pain. Risks include radiation exposure, increased use of surgery, and illness “labeling.” | The attributable costs would be related to the utilization of the imaging services. | Chou et al. 2007 | |
| Interventional Therapies for Low Back Pain: American Pain Society guideline recommends against prolotherapy for patients with nonspecific back pain, and intradiscal steroid injections, on the basis of good evidence showing risks but no net benefits. | The attributable costs would be related to the utilization of these services. | Chou et al. 2009b | |
| Medical Errors | Medication Errors and Diabetes: A “U” for units can be mistaken for a zero. If an order for “1U” of insulin is misread as “10” units and administered to a patient, a glucose infusion may be needed to prevent hypoglycemia. | Costs associated with a glucose infusion include nursing labor, materials for administering intravenous treatments, and dextrose solutions. | Joint Commission 2012 |
| Outcome | |||
| Diseases and Conditions | Attributable Outcome-Related Health Care Costs | ||
| Disease Progression | HbA1c Test Result | Improvements in glycemic control were followed by reductions in primary care visits relative to a control population. | Wagner et al. 2001 |
| Hospitalization and Glycemic Control | Having a HbA1c of 10% or higher was associated with hospitalization costs of $7,727, while those with mean HbA1c of < 7% had costs of $3,192 (inflated to 2009 dollars). | Bureau of Labor Statistics 2012; Menzin et al. 2010 | |
| Progression of Acute to Chronic Low Back Pain: Giving patients an “advice book” lowered the percentage of the population developing persistent pain from 14.1% to 10.5%. | Health care costs attributable to persistent pain would include provider visits, medications, and tests. | Coudeyre et al. 2007 | |
| Complications of Disease | Long-Term Diabetes Complications: Over the long term, complications include retinopathy, neuropathy, nephropathy, and macrovascular disease. | The average per-patient medical care costs for diabetes-related complications over thirty years were $68,037, largely due to macrovascular disease (inflated to 2009 dollars). | Bureau of Labor Statistics 2012; Caro, Ward, and O'Brien 2002 |
| Chronic Low Back Pain | Total annual health care costs for patients with chronic low back pain in the United Kingdom were double those of the matched controls without chronic back pain (£1,074 versus £516). | Hong et al. 2012 | |
| Complications of Care | Complications of Glycemic Control: Hypoglycemia is a predictable consequence of intensifying the treatment of diabetes. | When hypoglycemia requires treatment, it costs $125 to $170 per event, depending on severity and setting (2009 dollars). | Bodmer et al. 2008; Nuckols et al. 2011 |
| Complications of Interventional Procedures for Low Back Pain: Local pain, meningitis, abscess, headache, and paralysis, etc. | Costs associated with treating the complications. | Chou et al. 2009a | |
| Health Status | Attributable Health Status–Related Costs | ||
| Health Status | Kahn et al. estimated that achieving the maximum possible attainment of HbA1c goals would add 38,389 QALYs nationwide. | Not applicable in cost-effectiveness analyses. | Kahn et al. 2008 |
| Loss ofFunction | Diabetes: Reducing the average HbA1c to 7% nationwide would avoid disability, lost productivity, and premature mortality. (Note: overlaps with next category.) | The nationwide savings associated with avoiding this disability, lost productivity, and premature mortality would be $17.2 billion (inflated to 2009 dollars) over ten years. | Bureau of Labor Statistics 2012; Minshall et al. 2005 |
| Low Back Pain: Physical therapy that adheres to guideline recommendations (involves exercise or therapeutic activities) is associated with 17% greater improvement on a disability scale than physical therapy that does not. | Costs associated with disability. | Fritz et al. 2008 | |
| Low Back Pain: 43% of all workers experience back pain, and 42% of these individuals experience exacerbations, which are responsible for substantial absenteeism and presenteeism. | Back pain cost U.S. employers $7.40 billion per year as of 2004, with 85.4% of the costs explained by presenteeism. | Ricci et al. 2006 | |
| Loss of Lengthand Qualityof Life | Diabetic retinopathy leads to blindness, which has a substantial effect on peoples’ abilities to do the things that they enjoy. | People may be willing to pay some sizable amount to reduce the risk of diabetes-related blindness. | N/A |
Note:
N/A = Not applicable.
Structure
Structure is divided into (1) circumstance-specific structural characteristics, (2) quality improvement systems, and (3) general structural characteristics. Besides defining each subdomain, we also discuss how variations in quality influence costs.
Circumstance-specific characteristics represent the types of facilities, equipment, providers, and other structural features that influence care processes and clinical outcomes in the context of specific clinical circumstances. Examples are the resources involved in caring for patients with type 2 diabetes or for patients with low back pain. The costs associated with facilities and equipment include capital expenditures, which provider organizations recoup through clinical revenue when the facilities and equipment are used. For providers, costs depend on the frequency of visits and the reimbursement per visit.
Quality improvement systems are circumstance-specific structural characteristics that are specifically designed to improve quality of care, such as ensuring that patients receive necessary care. Examples are quality improvement systems, interventions designed to improve glycemic control among diabetics, and interventions to reduce inappropriate radiological imaging of patients with uncomplicated back pain. Associated costs are for the labor, facilities, and other resources used in designing, testing, implementing, and maintaining quality improvement systems. These costs are seldom billed directly to health care payers and patients but may be passed on through higher fees.
General structural characteristics may or may not influence care processes in a given clinical circumstance. If they do, the effect is not circumstance specific or intentional. For example, large multispecialty groups and small private practices have different patterns of care; the former are more likely to have developed protocols or to offer group visits. This may result in different processes and outcomes for patients with diabetes or back pain. In addition to influencing care processes directly, general structural characteristics may interact with external factors to affect total health care costs. Because of their greater market power, large multispecialty group practices are often able to charge higher fees than solo practitioners can (Berenson et al. 2012). General structural characteristics can, therefore, influence health care costs through multiple mechanisms.
Process
Process has two subdomains, appropriateness and medical errors, because these problems cause substantial morbidity and mortality (Brennan et al. 1991; IOM 2000, 2001; McGlynn et al. 2003; Thomas et al. 2000). It does not exclude other types of quality problems, like low interrater reliability (e.g., when two providers reach different conclusions on diagnostic tests).
Since 1986, RAND has used the RAND/UCLA Appropriateness Method (RAM) to define four categories of appropriateness of care (Brook et al. 1986; Fitch et al. 2001). This method is a multidisciplinary, two-round, modified-Delphi process that quantitatively synthesizes published literature and the expert judgment of a group regarding clinical appropriateness. It has been used to develop appropriateness criteria for at least sixteen surgical procedures (Lawson et al. 2011), as well as quality measures for the most common causes of morbidity and mortality, among many other conditions (McGlynn et al. 2003). It has good interrater reliability as well as content, construct, and predictive validity. Panel recommendations regarding appropriateness have been consistent with the results of subsequent randomized trials, and patients have had better survival and quality of life when care adheres to measures developed using this method (Higashi et al. 2005; Quintana et al. 2006; Shekelle 2004; Shekelle, Chassin, and Park 1998; Shekelle et al. 1998).
For our framework, we used the original appropriateness categories, subdividing one of them.
Necessary care is care for which the potential benefits to the patient exceed the risks to such a degree that the care must be offered.
Appropriate (but not necessary) care is care for which the benefits exceed the risks but not to the degree that the care is judged necessary.
Care of uncertain appropriateness is care for which the benefits and risks are uncertain.
Unhelpful care is care for which the benefits and risks are known to be equal or mixed (RAND previously combined the preceding two categories).
Inappropriate care means care for which the risks to the patient exceed the potential benefits to such a degree that the care must not be provided. (Fitch et al. 2001)
Underuse represents a failure to offer necessary care (patients can decline care) (Fitch et al. 2001). Underuse generally increases the risk of disease progression and disease complications. McGlynn and colleagues documented instances of underuse among 46 percent of U.S. adults (McGlynn et al. 2003). Underuse lowers process-related health care costs in the short term because the necessary care is not provided. Consequently, eliminating underuse increases short-term costs. The costs related to changes in rates of complications are discussed later.
In contrast, clinical overuse means providing inappropriate care (Fitch et al. 2001), and it increases the risk of complications of care. RAND and the framework define overuse fairly narrowly. While some economists consider overuse to include the frequent utilization of health care services with minimal health benefits (and low risks), our framework instead classifies services with minimal benefits as unhelpful care. Making this distinction is important because inappropriate care can lead to complications that are both harmful and costly. In contrast, unhelpful care is simply an inefficient allocation of health care resources. McGlynn and colleagues found that clinical overuse applied to 11 percent of U.S. adults (McGlynn et al. 2003). Because clinical overuse means that patients receive inappropriate care, it leads to short-term process-related health care costs; therefore, eliminating overuse creates short-term cost offsets. We discuss the longer-term costs attributable to complications later.
Much of the care that patients receive lies between underuse and overuse. Appropriate care improves health to a lesser degree than necessary care does, and it increases short-term process-related health care costs.
Care of uncertain appropriateness and unhelpful care are not measures of health-related quality because by definition, they are not known to affect health outcomes. The framework distinguishes care of uncertain appropriateness from unhelpful care because their cost implications differ. For example, health care payers often cover care of uncertain appropriateness, but some strive to curtail unhelpful care when they can identify it. In fact, care of uncertain appropriateness represents a substantial proportion of health care expenditures because the data on risks and benefits are limited for the majority of widely used tests and treatments (IOM 1985). Appropriateness is also uncertain for experimental therapies, which payers may cover for patients with unusual or severe conditions. Unhelpful care is common, too, such as the services identified by the 2012 Choosing Wisely Campaign (Cassel and Guest 2012).
Differentiating between care of uncertain appropriateness and unhelpful care can be challenging when the data are less than optimal, because appropriateness then lies in the eye of the beholder. Some questions of interest to health care payers are rarely addressed by research, such as the ideal number of doctor visits for patients with a given problem. Moreover, even when multiple studies have addressed a question, rigor may be lacking or results may conflict. Financial incentives may affect how providers and payers interpret imperfect data: payers have an incentive to limit care that is probably unhelpful, while providers paid on a fee-for-service basis have an incentive to offer care that might be helpful, even if the probability of benefit is low. Nevertheless, because neither unhelpful care nor care of uncertain appropriateness represents a subdomain of quality, any costs they produce are circumstance-specific expenditures rather than attributable to health-related quality (in figure 1, represented by unshaded boxes surrounded by dashed lines).
The IOM defines medical errors as the failure to complete a planned action as intended or the use of a wrong plan to achieve an aim (IOM 2000). Conceptually, medical errors and appropriateness overlap because many errors involve underuse (e.g., some “errors of omission”) or overuse (e.g., some “errors of commission”). Other errors involve misuse, that is, doing something in a manner that increases the risk of avoidable harm. Underuse increases the risk of disease progression and disease complications; overuse and misuse increase the risk of complications of care. Medical errors sometimes create process-related costs, such as when corrective actions are needed, creating labor and other types of costs. For example, after a medication administration error, a patient may require an antidote. If an X-ray detects a retained instrument at the end of surgery, removing the object will prolong the operation. The costs associated with the complications of medical errors are usually of greater concern than the costs of errors, however, which brings our discussion to outcomes and their associated costs.
Outcome
Outcome-related domains are (1) diseases and conditions and (2) health status.
Diseases and conditions represent clinical complaints, syndromes, disorders, and diagnoses that are influenced by care. As these develop or worsen, they create new indications for care that lead to outcome-related health care costs. The diseases and conditions domain contains three subdomains: (1) disease progression, (2) complications of the original disease, and (3) complications of care. Disease progression is a worsening of the original disease or condition. It often generates costs by leading to a higher utilization of provider visits, more intensive forms of treatment, and, sometimes, a need for additional diagnostic tests. Complications of the original disease are new diseases or conditions resulting from the original disease or condition. Complications of care are new diseases or conditions that result from care rather than the original disease or condition. Complications can result from overuse or medical errors, or they can occur even if apparently adequate quality care has been provided.
When applying the framework, some disorders could serve as the “specific clinical circumstance” that sets care processes in motion, the “disease or condition” that results from care processes, or both. For example, diabetic nephropathy with proteinuria is often used as an outcome in studies of glycemic control. Alternatively, diabetic nephropathy could be selected as the focus of a quality improvement intervention on the use of ACE inhibitors among people with proteinuria. For patients with multiple comorbidities, the “specific clinical circumstance” could refer to multiple conditions, and many different outcomes would be relevant.
Whether caused by diseases or by care, complications can generate costs by creating a need for new types of tests and treatments. Payers are starting to reimburse certain services differently when they appear to have been for a complication of care. Under Medicare payment policies, hospitals have historically received augmented payments when new complications arose during hospitalization, including many complications resulting from medical errors. But beginning in 2008, Medicare disallowed the augmented payments for a few complications, and other payers are starting to follow suit (Milstein 2009).
Complications and disease progression, in turn, adversely affect health status, reducing the patient's ability to function as well as length and quality of life. The definition of health-related quality that we borrowed from Donabedian describes a broad concept of health status that includes both physical and psychological well-being. The same is true of widely used instruments for measuring changes in health-related quality of life (Cheak-Zamora, Wyrwich, and McBride 2009; Donabedian, Wheeler, and Wyszewianski 1982; Hanmer 2009; Ware, Kosinski, and Keller 1996; Ware and Sherbourne 1992). Thus, the Quality-Cost Framework is compatible with cost-effectiveness analysis, which converts health-related quality of life to a measure of health utility, often reported in quality-adjusted life years (QALYs).
Although cost-effectiveness analysis is widely used in health care, some stakeholders, such as employers, may be interested in understanding the monetary costs associated with decrements in health status, such as the costs associated with declines in the ability to work. This information may be more relevant to their needs and easier to understand than an abstract concept like health utility. For this reason, the Quality-Cost Framework subdivides health status into functional status and length and quality of life. The corresponding categories of costs are functional-decrement costs and the economic value of preserving length and quality of life.
Functional status is the ability to work and perform tasks around the home. Functional-decrement costs are the fiscal consequences of declines in the ability to function, including losses of wages as well as the need to hire others to perform tasks around the home. Loss of wages can result from a complete inability to work, absenteeism (time off work), presenteeism (reduced productivity at work), and fewer career advancement opportunities.
Although length and quality of life can be measured, assessing the economic value associated with changes in these health states can be even more challenging. Willingness-to-pay studies are commonly used in policy decision making outside the health care sector and are sometimes performed to support cost-benefit analyses in health care settings as well. By using carefully designed surveys or by studying purchasing decisions that are affected indirectly, economists attempt to measure people's willingness to pay for things that they cannot actually purchase (Stokey and Zeckhauser 1978), or they may use other methods of valuing length and quality of life (Eggleston et al. 2009; Minshall et al. 2005). Our framework defines the economic value of length and quality of life as the additional amount that people in the target population and specific clinical circumstances are willing to pay in order to receive a level of care that would enhance their length or quality of life, after accounting for all other health care and disability costs.
Discussion
A conceptual framework can serve several practical purposes. A framework can help clarify important concepts and terms, facilitating communication among individuals working in a field. By describing plausible cause-and-effect relationships, a framework can sharpen analytical questions and aid the development of testable hypotheses. Because a conceptual framework delineates the factors influencing those cause-and-effect relationships, it can help investigators identify potential mediating variables, confounding factors, and sources of endogeneity, thereby revealing or improving analytical rigor and completeness. Finally, a framework can help investigators determine whether important questions might have been overlooked by previous researchers and thereby stimulate novel lines of inquiry. These statements are true, of course, only if a conceptual framework has been well formulated. Here we hope that the Quality-Cost Framework, which is built on influential streams of work by Donabedian, RAND researchers, the Institute of Medicine, and others, does not fall short.
The next step in this research is to validate the framework by applying it to collections of articles on the quality of care and costs for a few conditions. To assess the framework's applicability, its subdomains can be used to classify measures of quality and cost in published studies. To examine the framework's usefulness, it could be applied for the purpose of identifying design flaws in cost analyses. One important flaw would be omitting categories of costs that appear relevant on the basis of the clinical circumstances, subdomains of quality affected by the study, and the study's perspective. Applying the framework to the studies in table 1, we found that some contain such flaws. Both Kahn and colleagues and Monte and colleagues omitted the cost of quality improvement interventions that would, or did, drive changes in HbA1c values (Kahn et al. 2008; Monte et al. 2009). In contrast, Strong and colleagues considered costs attributable to two back-pain interventions and downstream effects on health care utilization (structure and process subdomains), but they did have not have the statistical power to include costs related to rare outcomes, such as hospitalization (Strong et al. 2006). The existence of such design flaws in published analyses suggests that our framework may be useful to researchers and analysts as they plan future studies. Ultimately, we plan to conduct a systematic review of studies that examined the net cost or cost-effectiveness of efforts to improve the quality of care for many conditions and then to use the framework as one of several tools for evaluating the quality of those studies. This would enable us to determine, in those studies that meet basic methodological standards, how frequently improving the quality of care is cost-effective or cost saving.
One limitation of our framework is that it does not explain how economic factors influence quality, which is, arguably, as important as how quality affects costs. To thoroughly explore how economic factors influence quality, an entirely different conceptual framework would be needed. However, the quality side of our framework does include some economic factors, because the Donabedian model considers health insurance laws and regulations, health insurance premiums, rates of insurance in the population, fee schedules, and so forth, to be structural dimensions of health-related quality. Also, we have included other patient-level economic factors, such as income, in our demographic characteristics. Since the Quality-Cost Framework focuses on health-related quality, it excludes non-health-related dimensions of quality of interest to consumers; so the relationship between non-health-related dimensions of quality and costs could also be the subject of a different conceptual framework.
Conclusion
The Quality-Cost Framework elucidates the mechanisms by which health-related quality of care affects health care and other types of costs, such as those associated with changes in health status. Additional work will be needed to validate the framework by applying it to collections of published studies for multiple clinical conditions. Assessments should include applicability, meaning the ability to classify measures of quality and cost using the framework, and usefulness, meaning the ability to identify design flaws in published cost analyses using the framework. Over the long term, we hope that the Quality-Cost Framework can facilitate discussions of health care policies, programs, and quality interventions by creating a common understanding of how quality affects costs.
Acknowledgments
Teryl Nuckols was supported by a Mentored Clinical Scientist Career Development Award (K08) from the Agency for Healthcare Research and Quality (grant no. HS17954). There were no other funding sources for this work. Robert H. Brook, ScD, MD and Peter Hussey, PhD, with the RAND Corporation, and Mark Cullen, MD, of Stanford University, provided helpful comments on the work.
References
- American Diabetes Association. Standards of Medical Care in Diabetes—2011. Diabetes Care. 2011;34:S11–61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AQA Performance Measures Workgroup. AQA Principles of “Efficiency” Measures. 2006. Available at http://www.aqaalliance.org/files/PrinciplesofEfficiencyMeasurementApril2006.doc (accessed May 23, 2012)
- Bachmann MO, Eachus J, Hopper CD, Smith G Davey, Propper C, Pearson NJ, Williams S, Tallon D, Frankel S. Socio-economic Inequalities in Diabetes Complications, Control, Attitudes and Health Service Use: A Cross-Sectional Study. Diabetic Medicine. 2003;20:921–29. doi: 10.1046/j.1464-5491.2003.01050.x. [DOI] [PubMed] [Google Scholar]
- Beaulieu N, Cutler D, Ho K. The Business Case for Diabetes Disease Management for Managed Care Organizations. Forum for Health Economics & Policy. 2006;9:1318–34. [Google Scholar]
- Berenson RA, Ginsburg PB, Christianson JB, Yee T. The Growing Power of Some Providers to Win Steep Payment Increases from Insurers Suggests Policy Remedies May Be Needed. Health Affairs (Millwood) 2012;31:973–81. doi: 10.1377/hlthaff.2011.0920. [DOI] [PubMed] [Google Scholar]
- Berwick DM. Making Good on ACOs’ Promise—The Final Rule for the Medicare Shared Savings Program. New England Journal of Medicine. 2011;365:1753–56. doi: 10.1056/NEJMp1111671. [DOI] [PubMed] [Google Scholar]
- Blumenthal D. Wiring the Health System—Origins and Provisions of a New Federal Program. New England Journal of Medicine. 2011;365:2323–29. doi: 10.1056/NEJMsr1110507. [DOI] [PubMed] [Google Scholar]
- Bodmer M, Meier C, Krahenbuhl S, Jick SS, Meier CR. Metformin, Sulfonylureas, or Other Antidiabetes Drugs and the Risk of Lactic Acidosis or Hypoglycemia: A Nested Case-Control Analysis. Diabetes Care. 2008;31:2086–91. doi: 10.2337/dc08-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandle M, Zhou H, Smith BR, Marriott D, Burke R, Tabaei BP, Brown MB, Herman WH. The Direct Medical Cost of Type 2 Diabetes. Diabetes Care. 2003;26:2300–2304. doi: 10.2337/diacare.26.8.2300. [DOI] [PubMed] [Google Scholar]
- Brennan TA, Hebert LE, Laird NM, Lawthers A, Thorpe KE, Leape LL, Localio AR, Lipsitz SR, Newhouse JP, Weiler PC, Hiatt HH. Hospital Characteristics Associated with Adverse Events and Substandard Care. JAMA. 1991;265:3265–69. [PubMed] [Google Scholar]
- Brook RH, Chassin MR, Fink A, Solomon DH, Kosecoff J, Park RE. A Method for the Detailed Assessment of the Appropriateness of Medical Technologies. International Journal of Technology Assessment in Health Care. 1986;2:53–63. doi: 10.1017/s0266462300002774. [DOI] [PubMed] [Google Scholar]
- Brook RH, McGlynn EA, Cleary PD. Quality of Health Care. Part 2: Measuring Quality of Care. New England Journal of Medicine. 1996;335:966–70. doi: 10.1056/NEJM199609263351311. [DOI] [PubMed] [Google Scholar]
- Browne K, Roseman D, Shaller D, Edgman-Levitan S. Analysis & Commentary. Measuring Patient Experience as a Strategy for Improving Primary Care. Health Affairs (Millwood) 2010;29:921–25. doi: 10.1377/hlthaff.2010.0238. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. Medical Component of the Consumer Price Index. 2012. Available at http://www.bls.gov/data/ (accessed June 13, 2012)
- Caro JJ, Ward AJ, O'Brien JA. Lifetime Costs of Complications Resulting from Type 2 Diabetes in the U.S. Diabetes Care. 2002;25:476–81. doi: 10.2337/diacare.25.3.476. [DOI] [PubMed] [Google Scholar]
- Cassel CK, Guest JA. Choosing Wisely: Helping Physicians and Patients Make Smart Decisions about Their Care. JAMA. 2012;307:1801–2. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and Validity of the SF-12v2 in the Medical Expenditure Panel Survey. Quality of Life Research. 2009;18:727–35. doi: 10.1007/s11136-009-9483-1. [DOI] [PubMed] [Google Scholar]
- Chen JY, Tian H, Juarez D Taira, Hodges KA, Jr, Brand JC, Chung RS, Legorreta AP. The Effect of a PPO Pay-for-Performance Program on Patients with Diabetes. American Journal of Managed Care. 2010;16:e11–19. [PubMed] [Google Scholar]
- Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical Interventional Therapies for Low Back Pain: A Review of the Evidence for an American Pain Society Clinical Practice Guideline. Spine. 2009a;34:1078–93. doi: 10.1097/BRS.0b013e3181a103b1. [DOI] [PubMed] [Google Scholar]
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM. Interventional Therapies, Surgery, and Interdisciplinary Rehabilitation for Low Back Pain: An Evidence-Based Clinical Practice Guideline from the American Pain Society. Spine. 2009b;34:1066–77. doi: 10.1097/BRS.0b013e3181a1390d. [DOI] [PubMed] [Google Scholar]
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, Owens DK. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Annals of Internal Medicine. 2007;147:478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- Commonwealth Fund Commission. Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2011. 2011. Available at http://www.commonwealthfund.org/∼/media/Files/Publications/Fund%20Report/2011/Oct/1500_WNTB_Natl_Scorecard_2011_web.pdf (accessed May 23, 2012)
- Coudeyre E, Tubach F, Rannou F, Baron G, Coriat F, Brin S, Revel M, Poiraudeau S. Effect of a Simple Information Booklet on Pain Persistence after an Acute Episode of Low Back Pain: A Non-Randomized Trial in a Primary Care Setting. PLoS One. 2007;2:e706. doi: 10.1371/journal.pone.0000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries A, Li CH, Sridhar G, Hummel JR, Breidbart S, Barron JJ. Impact of Medical Homes on Quality, Healthcare Utilization, and Costs. American Journal of Managed Care. 2012;18:534–44. [PubMed] [Google Scholar]
- Donabedian A. Evaluating the Quality of Medical Care. The Milbank Memorial Fund Quarterly. 1966;44(3):166–206. [PubMed] [Google Scholar]
- Donabedian A. Explorations in Quality Assessment and Monitoring. Vol. 1, The Definition of Quality and Approaches to Its Assessment. Ann Arbor, MI: Health Administration Press; 1980. [Google Scholar]
- Donabedian A. Explorations in Quality Assessment and Monitoring. Vol. 2, The Criteria and Standards of Quality. Ann Arbor, MI: Health Administration Press; 1982. [Google Scholar]
- Donabedian A. Explorations in Quality Assessment and Monitoring. Vol. 3, The Methods and Findings of Quality Assessment and Monitoring: An Illustrated Analysis. Ann Arbor, MI: Health Administration Press; 1985. [Google Scholar]
- Donabedian A, Wheeler JR, Wyszewianski L. Quality, Cost, and Health: An Integrative Model. Medical Care. 1982;20:975–92. doi: 10.1097/00005650-198210000-00001. [DOI] [PubMed] [Google Scholar]
- Eggleston KN, Shah ND, Smith SA, Wagie AE, Williams AR, Grossman JH, Berndt ER, Long KH, Banerjee R, Newhouse JP. The Net Value of Health Care for Patients with Type 2 Diabetes, 1997 to 2005. Annals of Internal Medicine. 2009;151:386–93. doi: 10.7326/0003-4819-151-6-200909150-00003. [DOI] [PubMed] [Google Scholar]
- Fenton JJ, Jerant AF, Bertakis KD, Franks P. The Cost of Satisfaction: A National Study of Patient Satisfaction, Health Care Utilization, Expenditures, and Mortality. Archives of Internal Medicine. 2012;172:405–11. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, McDonnell M, van het Loo J, Vader J, Kahan JP. The RAND/UCLA Appropriateness Method User's Manual. Santa Monica, CA: RAND Corporation; 2001. [Google Scholar]
- Franks P, Fiscella K. Effect of Patient Socioeconomic Status on Physician Profiles for Prevention, Disease Management, and Diagnostic Testing Costs. Medical Care. 2002;40:717–24. doi: 10.1097/00005650-200208000-00011. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Cleland JA, Speckman M, Brennan GP, Hunter SJ. Physical Therapy for Acute Low Back Pain: Associations with Subsequent Healthcare Costs. Spine. 2008;33:1800–1805. doi: 10.1097/BRS.0b013e31817bd853. [DOI] [PubMed] [Google Scholar]
- Gandjour A, Telzerow A, Lauterbach KW. European Comparison of Costs and Quality in the Treatment of Acute Back Pain. Spine. 2005;30:969–75. doi: 10.1097/01.brs.0000158944.54033.60. [DOI] [PubMed] [Google Scholar]
- Graves JM, Fulton-Kehoe D, Martin DP, Jarvik JG, Franklin GM. Factors Associated with Early Magnetic Resonance Imaging Utilization for Acute Occupational Low Back Pain: A Population-Based Study from Washington State Workers’ Compensation. Spine. 2012;37:1708–18. doi: 10.1097/BRS.0b013e31823a03cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanmer J. Predicting an SF-6D Preference-Based Score Using MCS and PCS Scores from the SF-12 or SF-36. Value in Health. 2009;12:958–66. doi: 10.1111/j.1524-4733.2009.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, Pohost GM, Williams KA. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119:e561–87. doi: 10.1161/CIRCULATIONAHA.109.192519. [DOI] [PubMed] [Google Scholar]
- Higashi T, Shekelle PG, Adams JL, Kamberg CJ, Roth CP, Solomon DH, Reuben DB, Chiang L, MacLean CH, Chang JT, Young RT, Saliba DM, Wenger NS. Quality of Care Is Associated with Survival in Vulnerable Older Patients. Annals of Internal Medicine. 2005;143:274–81. doi: 10.7326/0003-4819-143-4-200508160-00008. [DOI] [PubMed] [Google Scholar]
- Hong J, Reed C, Novick D, Happich M. Costs Associated with Treatment of Chronic Low Back Pain: An Analysis of the UK General Practice Research Database. Spine. 2012;38(1):75–82. doi: 10.1097/BRS.0b013e318276450f. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Assessing Medical Technologies. Washington, DC: National Academies Press; 1985. [Google Scholar]
- IOM (Institute of Medicine) To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Value in Health Care: Accounting for Cost, Quality, Safety, Outcomes, and Innovation Workshop Summary. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Future Directions for the National Healthcare Quality and Disparities Reports. Washington, DC: National Academies Press; 2010a. [PubMed] [Google Scholar]
- IOM (Institute of Medicine) The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: National Academies Press; 2010b. [PubMed] [Google Scholar]
- IOM (Institute of Medicine) Value in Health Care: Accounting for Cost, Quality, Safety, Outcomes and Innovation: Workshop Summary. Washington, DC: National Academies Press; 2010c. [PubMed] [Google Scholar]
- Joint Commission. Facts about the Official “Do Not Use” List. 2012. Available at http://www.jointcommission.org/assets/1/18/Do_Not_Use_List.pdf (accessed March 5, 2013)
- Kahn R, Robertson RM, Smith R, Eddy D. The Impact of Prevention on Reducing the Burden of Cardiovascular Disease. Diabetes Care. 2008;31:1686–96. doi: 10.2337/dc08-9022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushal R, Jha AK, Franz C, Glaser J, Shetty KD, Jaggi T, Middleton B, Kuperman GJ, Khorasani R, Tanasijevic M, Bates DW, Brigham and Women's Hospital CPOE Working Group Return on Investment for a Computerized Physician Order Entry System. Journal of the American Medical Informatics Association. 2006;13:261–66. doi: 10.1197/jamia.M1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotsos T, Muldowney K, Chapa G, Martin JE, Linares A. Challenges and Solutions in the Evaluation of a Low Back Pain Disease Management Program. Population Health Management. 2009;12:39–45. doi: 10.1089/pop.2008.0038. [DOI] [PubMed] [Google Scholar]
- Lawson EH, Gibbons MM, Ingraham AM, Shekelle PG, Ko CY. Appropriateness Criteria to Assess Variations in Surgical Procedure Use in the United States. Archives of Surgery. 2011;146:1433–40. doi: 10.1001/archsurg.2011.581. [DOI] [PubMed] [Google Scholar]
- McGlynn EA. Identifying, Categorizing, and Evaluating Health Care Efficiency Measures—Final Report. Rockville, MD: Southern California Evidence-Based Practice Center / RAND Corporation; 2008. [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The Quality of Health Care Delivered to Adults in the United States. New England Journal of Medicine. 2003;348:2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- McRae IS, Butler JR, Sibthorpe BM, Ruscoe W, Snow J, Rubiano D, Gardner KL. A Cost Effectiveness Study of Integrated Care in Health Services Delivery: A Diabetes Program in Australia. BMC Health Services Research. 2008;8:205. doi: 10.1186/1472-6963-8-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Increasing the Value of Medicare. Washington, DC: 2006. [Google Scholar]
- Medicare Physician Fee Schedule Look-Up. Available at http://www.cms.hhs.gov/PFSlookup/ (accessed May 10, 2012)
- Menzin J, Korn JR, Cohen J, Lobo F, Zhang B, Friedman M, Neumann PJ. Relationship between Glycemic Control and Diabetes-Related Hospital Costs in Patients with Type 1 or Type 2 Diabetes Mellitus. Journal of Managed Care Pharmacy. 2010;16:264–75. doi: 10.18553/jmcp.2010.16.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzin J, Langley-Hawthorne C, Friedman M, Boulanger L, Cavanaugh R. Potential Short-Term Economic Benefits of Improved Glycemic Control: A Managed Care Perspective. Diabetes Care. 2001;24:51–55. doi: 10.2337/diacare.24.1.51. [DOI] [PubMed] [Google Scholar]
- Milstein A. Ending Extra Payment for “Never Events”—Stronger Incentives for Patients’ Safety. New England Journal of Medicine. 2009;360:2388–90. doi: 10.1056/NEJMp0809125. [DOI] [PubMed] [Google Scholar]
- Minshall ME, Roze S, Palmer AJ, Valentine WJ, Foos V, Ray J, Graham C. Treating Diabetes to Accepted Standards of Care: A 10-Year Projection of the Estimated Economic and Health Impact in Patients with Type 1 and Type 2 Diabetes Mellitus in the United States. Clinical Therapeutics. 2005;27:940–50. doi: 10.1016/j.clinthera.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Monte SV, Slazak EM, Albanese NP, Adelman M, Rao G, Paladino JA. Clinical and Economic Impact of a Diabetes Clinical Pharmacy Service Program in a University and Primary Care-Based Collaboration Model. Journal of the American Pharmacists Association. 2009;49:200–208. doi: 10.1331/JAPhA.2009.08160. [DOI] [PubMed] [Google Scholar]
- National Quality Forum. Measurement Framework: Evaluating Efficiency across Patient-Focused Episodes of Care. 2010. Available at http://www.qualityforum.org/Publications/2010/01/Measurement_Framework__Evaluating_Efficiency_Across_Patient-Focused_Episodes_of_Care.aspx (accessed March 5, 2013)
- Nuckols TK, McGlynn EA, Adams J, Lai J, Go MH, Keesey J, Aledort JE. Cost Implications to Health Care Payers of Improving Glucose Management among Adults with Type 2 Diabetes. Health Services Research. 2011;46:1158–79. doi: 10.1111/j.1475-6773.2011.01257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ofman JJ, Badamgarav E, Henning JM, Knight K, Gano AD, Jr, Levan RK, Gur-Arie S, Richards MS, Hasselblad V, Weingarten SR. Does Disease Management Improve Clinical and Economic Outcomes in Patients with Chronic Diseases? A Systematic Review. American Journal of Medicine. 2004;117:182–92. doi: 10.1016/j.amjmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- Palmer S, Torgerson DJ. Economic Notes: Definitions of Efficiency. BMJ. 1999;318:1136. doi: 10.1136/bmj.318.7191.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintana JM, Escobar A, Arostegui I, Bilbao A, Azkarate J, Goenaga JI, Arenaza JC. Health-Related Quality of Life and Appropriateness of Knee or Hip Joint Replacement. Archives of Internal Medicine. 2006;166:220–26. doi: 10.1001/archinte.166.2.220. [DOI] [PubMed] [Google Scholar]
- Ricci JA, Stewart WF, Chee E, Leotta C, Foley K, Hochberg MC. Back Pain Exacerbations and Lost Productive Time Costs in United States Workers. Spine. 2006;31:3052–60. doi: 10.1097/01.brs.0000249521.61813.aa. [DOI] [PubMed] [Google Scholar]
- Rosenthal MB, Frank RG, Li Z, Epstein AM. Early Experience with Pay-for-Performance: From Concept to Practice. JAMA. 2005;294:1788–93. doi: 10.1001/jama.294.14.1788. [DOI] [PubMed] [Google Scholar]
- Rothman RL, So SA, Shin J, Malone RM, Bryant B, Dewalt DA, Pignone MP, Dittus RS. Labor Characteristics and Program Costs of a Successful Diabetes Disease Management Program. American Journal of Managed Care. 2006;12:277–83. [PubMed] [Google Scholar]
- Shekelle PG. The Appropriateness Method. Medical Decision Making. 2004;24:228–31. doi: 10.1177/0272989X04264212. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Chassin MR, Park RE. Assessing the Predictive Validity of the RAND/UCLA Appropriateness Method Criteria for Performing Carotid Endarterectomy. International Journal of Technology Assessment in Health Care. 1998;14:707–27. doi: 10.1017/s0266462300012022. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Kahan JP, Bernstein SJ, Leape LL, Kamberg CJ, Park RE. The Reproducibility of a Method to Identify the Overuse and Underuse of Medical Procedures. New England Journal of Medicine. 1998;338:1888–95. doi: 10.1056/NEJM199806253382607. [DOI] [PubMed] [Google Scholar]
- Sidorov J, Shull R, Tomcavage J, Girolami S, Lawton N, Harris R. Does Diabetes Disease Management Save Money and Improve Outcomes? A Report of Simultaneous Short-Term Savings and Quality Improvement Associated with a Health Maintenance Organization-Sponsored Disease Management Program among Patients Fulfilling Health Employer Data and Information Set Criteria. Diabetes Care. 2002;25:684–89. doi: 10.2337/diacare.25.4.684. [DOI] [PubMed] [Google Scholar]
- Stokey E, Zeckhauser R. A Primer for Policy Analysis. New York: Norton; 1978. [Google Scholar]
- Strong LL, Von Korff M, Saunders K, Moore JE. Cost-Effectiveness of Two Self-Care Interventions to Reduce Disability Associated with Back Pain. Spine. 2006;31:1639–45. doi: 10.1097/01.brs.0000224528.75951.03. [DOI] [PubMed] [Google Scholar]
- Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, Howard KM, Weiler PC, Brennan TA. Incidence and Types of Adverse Events and Negligent Care in Utah and Colorado. Medical Care. 2000;38:261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- Trogdon JG, Hylands T. Nationally Representative Medical Costs of Diabetes by Time Since Diagnosis. Diabetes Care. 2008;31:2307–11. doi: 10.2337/dc08-1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Kingdom Prospective Diabetes Study Group. Gray A, Raikou M, McGuire A, Fenn P, Stevens R, Cull C, Stratton I, Adler A, Holman R, Turner R. Cost Effectiveness of an Intensive Blood Glucose Control Policy in Patients with Type 2 Diabetes: Economic Analysis alongside Randomised Controlled Trial (UKPDS 41) BMJ. 2000;320:1373–78. doi: 10.1136/bmj.320.7246.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC. Effect of Improved Glycemic Control on Health Care Costs and Utilization. JAMA. 2001;285:182–89. doi: 10.1001/jama.285.2.182. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Medical Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual Framework and Item Selection. Medical Care. 1992;30:473–83. [PubMed] [Google Scholar]
- Young GJ, Meterko M, Beckman H, Baker E, White B, Sautter KM, Greene R, Curtin K, Bokhour BG, Berlowitz D, Burgess JF., Jr Effects of Paying Physicians Based on Their Relative Performance for Quality. Journal of General Internal Medicine. 2007;22:872–76. doi: 10.1007/s11606-007-0185-5. [DOI] [PMC free article] [PubMed] [Google Scholar]