Abstract
BACKGROUND:
It is increasingly evident that visceral adipose tissue plays a leading role in the pathogenesis of the metabolic syndrome. Unfortunately, accurate quantification of intra-abdominal visceral fat is cumbersome and expensive. Epicardial fat represents the component of visceral fat distributed around the heart, and is readily and non-invasively assessed by echocardiography.
AIMS:
To determine the correlation of epicardial fat with anthropometric parameters in a healthy population of Asian-Indians.
MATERIALS AND METHODS:
A prospective, cross-sectional study was conducted as part of a community outreach program from December to March 2011. Individuals over 18 years of age were included in the study. Anthropometric data was collected for all patients. Epicardial fat was assessed in parasternal long and short axes.
RESULTS:
350 healthy individuals were included in the study. Of them, 66.7% were males. Mean age was 42.7 ± 15.3 years (range 18-84). Mean body-mass index (BMI) and waist circumference were 23.3 ± 4.5 kg/m2 (range 15.2-34.3) and 80.2 ± 13.3 cm (range 43-115) respectively. Mean epicardial fat in both axes was 2.6 ± 1.3 mm (range 0.3-7.0). Epicardial fat measured in both axes correlated well with weight (r = 0.399, P < 0.001), waist circumference (r = 0.522, P < 0.001) and BMI (r = 0.471, P < 0.001). Epicardial fat also correlated with age (r = 0.559, P < 0.001).
CONCLUSIONS:
There is an excellent correlation between epicardial fat measured by echocardiography and anthropometric parameters of metabolic syndrome.
Keywords: Anthropometric measurements, epicardial fat, metabolic syndrome visceral fat
INTRODUCTION
Visceral obesity is recognized as an important risk-factor for the development of most features of metabolic syndrome, such as insulin resistance, diabetes, dyslipidemia, and hypertension,[1,2,3,4,5,6,7] and has been linked with all-cause mortality in elderly population.[7] Detection and quantification of visceral adipose tissue (VAT), the fat deposited around the internal organs, is crucial for identifying visceral obesity, and can be achieved by non-invasive imaging techniques including computed tomography (CT) and the gold standard technique – magnetic resonance imaging (MRI).[8,9,10] Although accurate, these modalities are time-consuming and expensive, and in the case of CT require radiation exposure. Abdominal ultrasonographic techniques have now been developed for calculation of VAT.[11,12,13]
Anthropometric measurements have been extensively evaluated as surrogate markers for VAT. Their major drawback is their relative imprecision.[14,15] Waist circumference is however, widely accepted as a robust predictor of visceral fat,[16] a marker of cardiometabolic risk,[17] and an indicator of risk of development of type 2 diabetes mellitus.[18]
Assessment of intra-thoracic VAT within the pericardial and epicardial fat sub-compartments by MRI and/or CT, has been shown to correlate with intra-abdominal VAT.[19,20] Intra-thoracic VAT has also been positively associated with hypertension,[19] insulin resistance,[19] elevated triglycerides,[19] the metabolic syndrome,[20] and coronary artery disease.[21] In addition to the close relationship between abdominal visceral fat and epicardial fat – a fact partially explained by their common embryological origin,[22] epicardial fat can potentially influence coronary atherogenesis and myocardial function directly.[23]
This study was performed to determine the correlation of echocardiographically determined epicardial fat with commonly utilized anthropometric measurements in a population of healthy Asian-Indian individuals.
MATERIALS AND METHODS
Study settings
The study was conducted as a part of community based project at three different places within a 10 mile radius from Kasturba hospital, Manipal in coastal Karnataka (south India).
It was prospective and cross-sectional in design. 350 consecutive healthy subjects without hypertension, diabetes, dyslipidemia, or any other chronic medical illness were included in the study. Obesity was not used as an exclusion criterion. All participants had a blood pressure below 130/85 mm Hg. Subjects below 18 years of age were excluded from the study. Blood glucose and dyslipidemia were not estimated prior to inclusion in the study. Previous diagnosis with hypertension, diabetes, dyslipidemia or any other chronic medical illness, or past history of receiving any form of therapy for these conditions was an exclusion criterion.
Institutional ethical committee approval was obtained prior to the study. All subjects gave informed consent prior to inclusion in the study.
Anthropometric data were collected in all the subjects including weight, height, and waist circumference. Weight (to the nearest 0.1 kg) and height (to the nearest 0.5 cm) were measured while the subjects were fasting and wearing only their undergarments. Body-mass index (BMI) was calculated by dividing the body weight (in kilograms) by height squared (in meters) and was used to quantify obesity. Waist circumference was measured mid-waist, between the lower rib margin and the iliac crest while the subjects were standing with their heels together, with quiet respiration. A waist circumference greater than 80 cm in women and 90 cm in men was considered indicative of truncal/abdominal obesity.[17]
Each subject underwent transthoracic two-dimensional guided M-mode echocardiography. Echocardiograms were performed with a General Electric Company (GE) Vivid E echo machine by standard techniques with subjects in the left lateral decubitus position. Echocardiograms were recorded on videotape. The echocardiographic study required recording of 10 cycles of two-dimensional parasternal long- and short-axis views and 10 cycles of M-mode with optimal cursor beam orientation in each view.[24,25] Epicardial fat thickness was measured on the free wall of the right ventricle from both parasternal long- and short-axis views. In these views, epicardial adipose tissue was visualized as an echo-free space [Figure 1]. Measurement of epicardial fat on right ventricle was chosen as this point has been shown to have the highest absolute epicardial fat layer thickness.[26] Moreover, parasternal long- and short-axis views allow the most accurate measurement of epicardial adipose tissue on the right ventricle with optimal cursor beam orientation in each view.
Figure 1.
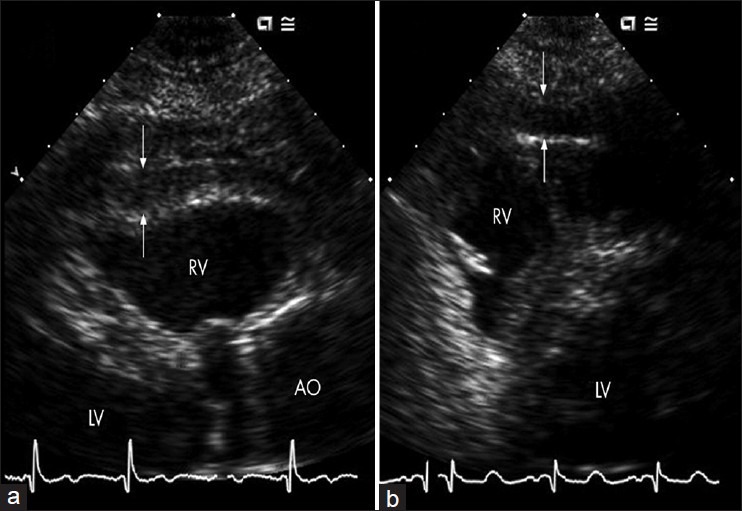
Transthoracic echocardiogram showing a large area of epicardial adipose tissue (white arrows) on free wall of right ventricle (a and b). RV: right ventricle, LV: Left ventricle, Ao: Aorta
Hypertrophy of the right ventricle trabecular and moderator band, even when present, did not confound epicardial adipose tissue calculation.[26]
Statistical analysis
All data was analyzed using SPSS Statistics version 17.0 (Chicago IL, USA). Continuous variables were presented as mean ± SD. Chi-square test was used to determine the association of various anthropometric parameters with epicardial fat thickness. Pearson's correlation was performed on echocardiographic, anthropometric, and clinical variables to identify correlates of epicardial fat. P < 0.05 were considered to indicate statistical significance.
RESULTS
Of the 350 individuals included in the study, 223 (63.7%) were males.
Mean age at the time of participation in the study was 42.79 ± 15.3 years (range 18-84). Mean values of anthropometric parameters were as follows: Height 157.35 ± 11.4 cm, weight 57.66 ± 14 kg, BMI 23.29 ± 4.5 kg/m2 (range 15.2-34.3), waist circumference 80.24 ± 13.4 cm (range 43-115). Mean epicardial fat in both parasternal long axis and short axis was 2.6 ± 1.3 mm (range 0.3-7.0). Anthropometric measurements according to gender are summarized in Table 1.
Table 1.
Body composition and visceral adipose tissue measures in men and women
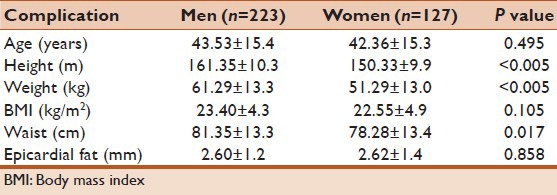
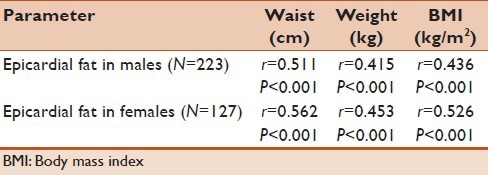
Pearson's correlation showed a strong, positive correlation between epicardial fat thickness obtained from echocardiogram and BMI, which was statistically significant (r = 0.469, P < 0.001). Similar positive correlations were seen for epicardial fat thickness versus waist circumference (r = 0.529, P < 0.001), epicardial thickness versus weight (r = 0.346, P < 0.001) and epicardial fat thickness versus age (r = 0.625, P < 0.001). Scatter plot diagrams were corroboratory [Figures 2 and 3]. There was also a strong correlation between epicardial fat versus age and anthropometric measurements in both males and females as shown in Table 2.
Figure 2.
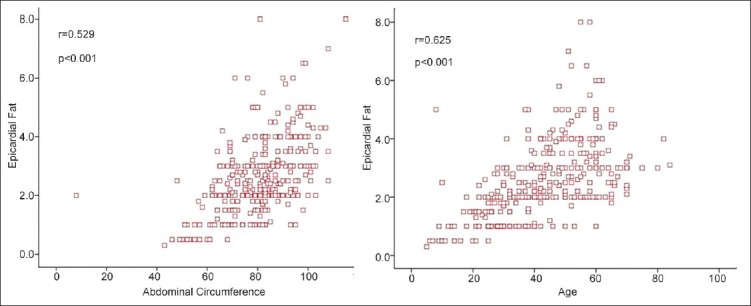
Scatter plot of echocardiographic epicardial fat thickness versus waist circumference (left) and age (right)
Figure 3.
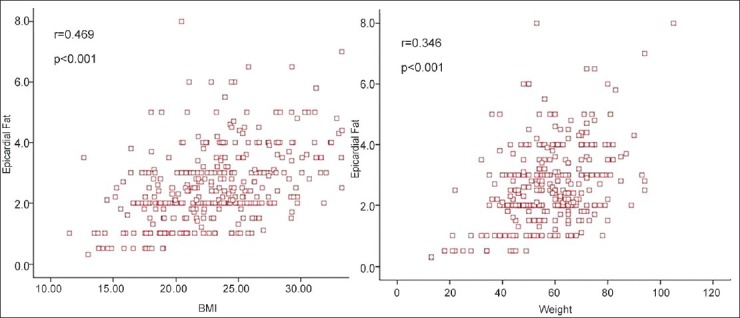
Scatter plot of echocardiographic epicardial fat thickness versus body-mass index (left) and weight (right)
Table 2.
Correlation of epicardial fat with anthropometric parameters in males and females
No significant difference was found in epicardial adipose tissue between men and women.
DISCUSSION
There is a limited data available on the correlation of anthropometric parameters with epicardial fat thickness. A recent study by Kim et al.[27] in obese adolescents in South Korea showed good correlation between these parameters and echocardiographically determined epicardial fat thickness. However, similar data is lacking in the Asian-Indian population where no large studies have been conducted to validate these findings. Moreover, there were several shortcomings in the study by Kim et al., including a relatively small sample size, and inclusion of only obese subjects in the study population. We attempted to further validate these findings by performing a community based study including healthy individuals, in order to determine whether the relationship between anthropometric measurements and epicardial fat thickness was strong regardless of the presence or absence of obesity.
Similar to the findings by Kim et al., our study showed a positive association between epicardial adipose tissue and BMI.
Our data also suggests that body fat distribution, particularly abdominal fat tissue, correlates strongly with epicardial fat. This was evidenced by the robust correlation of epicardial adipose tissue thickness with waist circumference. Waist circumference is widely accepted as an indicator of subjects with adverse metabolic profile and high cardiovascular risk, and has been positively correlated with abdominal fat content.[16] The vigorous association demonstrated in our study between epicardial fat and anthropometric measures of obesity strengthens the position of epicardial fat thickness as an accurate indicator of VAT and by extension, cardiometabolic risk. Moreover, epicardial adipose tissue assessment scores over waist circumference in terms of precision and reproducibility.
Abdominal ultrasonography has also suggested as an inexpensive and safe technique to determine VAT. While some reports have described good correlation between ultrasound measurements and CT images of VAT[13] with waist circumference,[13] other studies have reported poor reproducibility.[28]
In contrast, the thickness of the epicardial adipose tissue sub-compartment can be measured easily and conveniently by transthoracic echocardiography and correlates with MRI-determined epicardial fat and intra-abdominal VAT.[29] Assessment of epicardial adipose tissue by echocardiography can also be conveniently carried out in the course of routine evaluation of morphological and functional cardiac parameters in patients with obesity, diabetes, and hypertension. Precaution should be exercised; however, as epicardial adipose tissue can produce an echo-free space that might be mistaken for pericardial fluid.[30]
A brief comparison with similar studies conducted on other ethnic populations revealed comparable correlation of epicardial fat thickness with various anthropometric parameters. Two Italian studies by Iacobellis[29] and Vicennati[31] for instance, yielded strong correlation between epicardial fat and waist circumference and BMI similar to the study by Kim et al., however, both studies were limited by a small sample size, and the study by Vicennati was also restricted to obese women, limiting application of the results to the general population. In comparison, a recent Chinese study by Lai et al.,[32] was similar to our own study in terms of enrolled individuals – this study also demonstrated significant correlation between epicardial fat and weight, waist circumference and BMI.
Our study adds to this body of evidence, by validating these results in a healthy Asian-Indian population.
Determination of whether a similar association exists in this population between epicardial adipose tissue thickness and biochemical parameters of metabolic syndrome would constitute the next step and requires further investigation.
ACKNOWLEDGMENTS
We sincerely thank the patients and relatives for their co-operation and consent for publication of data in the medical journal.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Albu JB, Kovera AJ, Johnson JA. Fat distribution and health in obesity. Ann N Y Acad Sci. 2000;904:491–501. doi: 10.1111/j.1749-6632.2000.tb06505.x. [DOI] [PubMed] [Google Scholar]
- 2.Doll S, Paccaud F, Bovet P, Burnier M, Wietlisbach V. Body mass index, abdominal adiposity and blood pressure: Consistency of their association across developing and developed countries. Int J Obes Relat Metab Disord. 2002;26:48–57. doi: 10.1038/sj.ijo.0801854. [DOI] [PubMed] [Google Scholar]
- 3.Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, et al. Abdominal adiposity and coronary heart disease in women. JAMA. 1998;280:1843–8. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- 4.Rexrode KM, Buring JE, Manson JE. Abdominal and total adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord. 2001;25:1047–56. doi: 10.1038/sj.ijo.0801615. [DOI] [PubMed] [Google Scholar]
- 5.Peiris AN, Sothmann MS, Hoffmann RG, Hennes MI, Wilson CR, Gustafson AB, et al. Adiposity, fat distribution, and cardiovascular risk. Ann Intern Med. 1989;110:867–72. doi: 10.7326/0003-4819-110-11-867. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura T, Tokunaga K, Shimomura I, Nishida M, Yoshida S, Kotani K, et al. Contribution of visceral fat accumulation to the development of coronary artery disease in non-obese men. Atherosclerosis. 1994;107:239–46. doi: 10.1016/0021-9150(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 7.Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: The Rotterdam study. Int J Obes Relat Metab Disord. 2001;25:1730–5. doi: 10.1038/sj.ijo.0801787. [DOI] [PubMed] [Google Scholar]
- 8.Ross R, Shaw KD, Martel Y, de Guise J, Hudson R, Avruch L. Determination of total and regional adipose tissue distribution by magnetic resonance imaging in android women. Basic Life Sci. 1993;60:177–80. doi: 10.1007/978-1-4899-1268-8_40. [DOI] [PubMed] [Google Scholar]
- 9.Sharma RC, Kramsch DM, Lee PL, Colletti P, Jiao Q. Quantitation and localization of regional body fat distribution – A comparison between magnetic resonance imaging and somatometry. Obes Res. 1996;4:167–78. doi: 10.1002/j.1550-8528.1996.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 10.Ross R, Léger L, Morris D, de Guise J, Guardo R. Quantification of adipose tissue by MRI: Relationship with anthropometric variables. J Appl Physiol. 1992;72:787–95. doi: 10.1152/jappl.1992.72.2.787. [DOI] [PubMed] [Google Scholar]
- 11.Armellini F, Zamboni M, Robbi R, Todesco T, Rigo L, Bergamo-Andreis IA, et al. Total and intra-abdominal fat measurements by ultrasound and computerized tomography. Int J Obes Relat Metab Disord. 1993;17:209–14. [PubMed] [Google Scholar]
- 12.Ribeiro-Filho FF, Faria AN, Kohlmann O, Jr, Ajzen S, Ribeiro AB, Zanella MT, et al. Ultrasonography for the evaluation of visceral fat and cardiovascular risk. Hypertension. 2001;38:713–7. doi: 10.1161/01.hyp.38.3.713. [DOI] [PubMed] [Google Scholar]
- 13.Ferrozzi F, Zuccoli G, Tognini G, Castriota-Scanderbeg A, Bacchini E, Bernasconi S, et al. An assessment of abdominal fatty tissue distribution in obese children. A comparison between echography and computed tomography. Radiol Med. 1999;98:490–4. [PubMed] [Google Scholar]
- 14.Bonora E, Micciolo R, Ghiatas AA, Lancaster JL, Alyassin A, Muggeo M, et al. Is it possible to derive a reliable estimate of human visceral and subcutaneous abdominal adipose tissue from simple anthropometric measurements? Metabolism. 1995;44:1617–25. doi: 10.1016/0026-0495(95)90084-5. [DOI] [PubMed] [Google Scholar]
- 15.van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Visser M. Abdominal diameters as indicators of visceral fat: Comparison between magnetic resonance imaging and anthropometry. Br J Nutr. 1993;70:47–58. doi: 10.1079/bjn19930104. [DOI] [PubMed] [Google Scholar]
- 16.Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75:683–8. doi: 10.1093/ajcn/75.4.683. [DOI] [PubMed] [Google Scholar]
- 17.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome – A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 18.Wei M, Gaskill SP, Haffner SM, Stern MP. Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans – A 7-year prospective study. Obes Res. 1997;5:16–23. doi: 10.1002/j.1550-8528.1997.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 19.Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: The Framingham Heart Study. Circulation. 2008;117:605–13. doi: 10.1161/CIRCULATIONAHA.107.743062. [DOI] [PubMed] [Google Scholar]
- 20.Thanassoulis G, Massaro JM, Hoffmann U, Mahabadi AA, Vasan RS, O’Donnell CJ, et al. Prevalence, distribution, and risk factor correlates of high pericardial and intrathoracic fat depots in the Framingham heart study. Circ Cardiovasc Imaging. 2010;3:559–66. doi: 10.1161/CIRCIMAGING.110.956706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu Y, Cheng X, Hong K, Huang C, Wan L. How to interpret epicardial adipose tissue as a cause of coronary artery disease: A meta-analysis. Coron Artery Dis. 2012;23:227–33. doi: 10.1097/MCA.0b013e328351ab2c. [DOI] [PubMed] [Google Scholar]
- 22.Sacks HS, Fain JN. Human epicardial adipose tissue: A review. Am Heart J. 2007;153:907–17. doi: 10.1016/j.ahj.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 23.Karastergiou K, Evans I, Ogston N, Miheisi N, Nair D, Kaski JC, et al. Epicardial adipokines in obesity and coronary artery disease induce atherogenic changes in monocytes and endothelial cells. Arterioscler Thromb Vasc Biol. 2010;30:1340–6. doi: 10.1161/ATVBAHA.110.204719. [DOI] [PubMed] [Google Scholar]
- 24.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–67. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 25.Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: Results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–83. doi: 10.1161/01.cir.58.6.1072. [DOI] [PubMed] [Google Scholar]
- 26.Schejbal V. [Epicardial fatty tissue of the right ventricle: Morphology, morphometry and functional significance] Pneumologie. 1989;43:490–9. [PubMed] [Google Scholar]
- 27.Kim SJ, Kim HS, Jung JW, Kim NS, Noh CI, Hong YM. Correlation between epicardial fat thickness by echocardiography and other parameters in obese adolescents. Korean Circ J. 2012;42:471–8. doi: 10.4070/kcj.2012.42.7.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bellisari A, Roche AF, Siervogel RM. Reliability of B-mode ultrasonic measurements of subcutaneous adipose tissue and intra-abdominal depth: Comparisons with skinfold thicknesses. Int J Obes Relat Metab Disord. 1993;17:475–80. [PubMed] [Google Scholar]
- 29.Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: A new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003;88:5163–8. doi: 10.1210/jc.2003-030698. [DOI] [PubMed] [Google Scholar]
- 30.Ansari A, Rholl AO. Pseudopericardial effusion: Echocardiographic and computed tomographic correlations. Clin Cardiol. 1986;9:551–5. doi: 10.1002/clc.4960091105. [DOI] [PubMed] [Google Scholar]
- 31.Vicennati V, Cavazza C, Garelli S, Pizzi C, Bugiardini R, Rinaldi E, et al. Anthropometric, hormonal and nutritional correlates of epicardial fat in obese women. Endocrine Abstracts. 2012;29:1233. [Google Scholar]
- 32.Lai YH, Yun CH, Yang FS, Liu CC, Wu YJ, Kuo JY, et al. Epicardial adipose tissue relating to anthropometrics, metabolic derangements and fatty liver disease independently contributes to serum high-sensitivity C-reactive protein beyond body fat composition: A study validated with computed tomography. J Am Soc Echocardiogr. 2012;25:234–41. doi: 10.1016/j.echo.2011.09.018. [DOI] [PubMed] [Google Scholar]


