Abstract
Background:
The purpose of this study was to describe the first attempts and performance of health system in Iran in training specialist nurses in the field of diabetes- related care and education.
Materials and Methods:
This was a qualitative content analysis. Three diabetes management planners in the Ministry of Health and Medical Education, three provincial executive authorities of diabetes in the health system and ten nurses who worked as diabetes nurse educators (DNEs) participated in this study. Data obtained through semi-structured face-to-face interviews, a focus group, existing documents, field notes, and multiple observations. Data analysis was guided by the conventional approach of qualitative content analysis.
Findings:
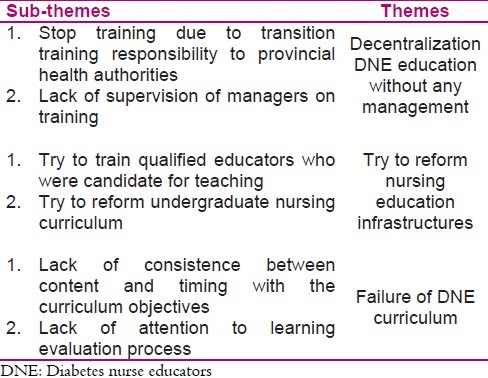
Three major themes and six sub-themes were emerged through data analysis. Main themes were: (a) decentralization diabetes nurse educator training without any management (stop education due to transition training responsibility to provincial health authorities and lack of supervision of managers on training); (b) try to reform nursing education infrastructures (try to train qualified educators who were candidate for teaching to DNEs, try to reform undergraduate nursing curriculum); (c) failure of DNE curriculum (lack of consistency between content and timing with the curriculum objectives and lack of attention to learn evaluation process).
Conclusions:
The findings of this study reflected the failure and multiple challenges in educating nurses working in diabetes units. Despite the fact that important roles were defined for nurses in the action plan for preventing and controlling diabetes, any specific action was not done in preparing nurses for these roles.
Keywords: Diabetes, Iran, nursing education, qualitative research
INTRODUCTION
Diabetes is one of the most prevalent chronic diseases and major health challenges in the 21st century[1] leading to much morbidity and mortality in communities especially in developing countries and a major part of medical expenses is allocated to its care.[2,3] The World Health Organization (WHO) estimates that more than 180 million people worldwide have diabetes.[4] WHO also predicted that the number of people with diabetes will rise to more than 360 million people worldwide by 2030.[5] This increasing number will be from 51 to 72 million (+42%), and from 84 to 228 million (+170%) for developed countries and developing countries, respectively.[6]
While the prevalence of diabetes in 2001 in the population over 20 years were estimated equal to 4.67% (i.e. 1.6 million people) in Iran, but given the increase in elderly population in the one hand and increasing incidence of obesity on the other hand, a 198 percent increase in the incidence of diabetes is expected by 2050.[7] Diabetes for several reasons (including the nature of chronic illness, serious complications, affecting people in working age and reducing their productivity, disability and high rate mortality) is one of the costly diseases to both patients and health care systems all over the world.[3,8,9] The major effect of the disease is on adults of working age, especially in developing countries.[3] Burden of diabetes especially including its complications was reported to be about 306440 years in 2001 in Iran that much of it (154863 years) were related to lost years due to premature disease-related death.[10] The direct and indirect economic burden of diabetes in Iran was reported about 9472.6 million US dollars in 1999.[7]
Accordingly, diabetes mellitus has become one of the principle chronic illnesses requiring careful and ongoing attention. Healthcare providers repeatedly attempt to assist clients with the management of their treatment plan.[11] In fact, one of the most important parts of health care system is the health care workforce who is instrumental in stimulating, implementing, and maintaining change to improve care for chronic conditions.[12,13] However, proper management of diabetes will be possible only if it is based on the set of elements, including a team approach[14–17] because caring for chronic disease requires multiple types of expertise.[17]
In doing so, since 2004, Iran’s health system policy-makers formally placed diabetes in a team approach in Iran health priorities aiming at reducing the incidence of diabetes, better control and reducing incidence and severity of diabetes complications. In national guideline for diabetes prevention and control, four levels of care were defined. Nurse was introduced in the third and fourth levels of the protocol as one of the main anchors.[18] In addition, various administrative and educational roles were defined for them in the third and fourth levels of this protocol.[19] Since health care providers including nurses require appropriate knowledge about diabetes to provide quality services for people with diabetes or high-risk clients[11] national guidelines on diabetes prevention and control planed a formal educational program to train nurses as diabetes nurse educators (DNEs). To the best of our knowledge, no quantitative or qualitative study has been conducted on the process of nurses’ education in this program. Thus, present study asked how the status of educational process was for nurses who worked in diabetes units. Study findings will be effective in recognizing present challenges in DNE training process and improving quality of its related planning.
MATERIALS AND METHODS
The purpose of this study conducted in 2010 was to describe health system’s policies and programs for preparing qualified nurses who play role as DNEs in specialized diabetes units. Since it was possible through answering questions on what, how and why about health system performance, a qualitative approach was conducted and data analysis was done by qualitative content analysis. Qualitative content analysis is a research method that is used in analysis and subjective interpretation of the content of text data[20] through the systematic classification process of coding and identifying themes or patterns.[21,22] Conventional qualitative content analysis is one of three approaches to qualitative content analysis, which is generally used with a study design aimed to describe a phenomenon. This method result in coding categories derived directly and inductively from the raw data.[20,21]
In the present study, given that the only source for data coding and categorization was raw data based on inductive approach, conventional content analysis was selected to describe the studied phenomena. Samples for qualitative data analysis are usually purposeful texts, which can cover required information for answering research questions.[23] The textual data can encompass verbal, print, or electronic data, which obtained through narrative answers, open response questions, interviews, focus groups, observations, or print media (including articles, books or manuscripts).[20] In this study, the textual data from semi-structured individual interviews with key informants, a focus group attended by DNEs, field notes and multiple observations, documents and books (including book of diabetes prevention and control program[19] and memos) were used for qualitative data analysis.
Three diabetes management planners in the Ministry of Health and Medical Education, 3 executive authorities of diabetes, and 10 diabetes-nurses of diabetes units participated in this study. Diabetes management planners, executive authorities of diabetes, and DNE had 15-8 years, 10 months to 4 years, and four months to five years experiences in diabetes management, respectively. Six nurses participated in a focus group, and in other cases, individual semi-structured interviews with participants were conducted.
The present study was conducted in the Department of Fight Against Diseases in Ministry of Health and Medical Education, and Department of Health and some diabetes centers in Isfahan. First, researcher presented the official reference in which the purpose of the study was determined. She introduced herself to participants, took participants’ permission for recording interview, and determined the location and time of interview. Interviews last between 15–40 minutes (the average time was 25 minutes), and focus group last 45 minutes. Focus groups were conducted in three parts (including introducing the group, conducting the group and closing the group).
All individual interviews and focus groups were recorded on the MP4 recording device and then were listen repeatedly, and typed in Microsoft Word Office 2007 software. Material in the book “National Program on Diabetes Prevention and Control” was another source of data collection.
Furthermore, first author attended in the study field repeatedly as a complete observer and sometime as participant-observer, so researcher’s observations formed another part of the data analysis.
After repeated listening, reading and immersing in all collected data, a general picture of them was obtained. Obtained data were read and verbatim meaning unit of them were extracted. For this, at first, exact words of text that expressed key ideas or concepts were highlighted. Then researchers’ notes (i.e. their ideas, thoughts and primary analysis) were added to the text. At this point, meaning units that represent the similar concepts were coded. Then various codes were categorized based on their relationships. Ten significant clusters were provided by these categories. Finally, six sub-themes were organized in three themes.
Multiple strategies (triangulation of data sources and data collection methods, continuous observations) were used to promote trustworthiness. Furthermore, coding process repeatedly revised after coding all data to ensure consistency of coding. In addition, fellow authors read texts and themes and matched it with the text in every stage. This process known as peer debriefing helped to increase acceptance.
The research proposal was approved by the research committee at the Nursing Department of Tarbiat Modares University in Tehran, Iran. Prior to obtaining the respondents written informed consent, all participants were informed of the purpose and design of the study both verbally and in writing. They were informed that at any point during the interview they could quit. In addition, they were reassured that their responses would be kept confidential and their identities would not be revealed in research report.
FINDINGS
Three major themes and six sub-themes were emerged through data analysis (Table 1), which are discussed respectively.
Table 1.
Summary of Study findings
Decentralization DNE education without any management:
Data obtained from multiple sources indicated that formal planned training for nurses was limited to first-year of starting Diabetes Prevention and Control National Project. Training nurses for role playing as DNE was concentrated at first, so candidate nurses all over the country took part in it. One of the diabetes management planners and policy makers expressed:
“We hold four training course for nurses and trained them as DNE.”
Although formal discussions and informal conversations and interviews suggests that none of the trained nurses are working in diabetes centers currently, however in the short interval after starting of national program on diabetes prevention and control, training responsibility has been transited to provincial health authorities. One diabetes management policymaker stated that:
“We started to educate and train various groups including physicians, nurses, nutritionists, which they were trained in several workshops in Tehran and some provinces. Then it was delegated to each province.”
This delegation leads to working as DNE without passing educational course. This means that following that transition no formal training course has been held for nurses who worked as DNE.
Nevertheless, there was no educational program with a clear content and formal training, which was supposed to be held by a team of healthcare officials, specialist physicians, experts in combating with non-communicable diseases, trained doctors, nurses and nutritionists.
Educating Nurses who supposed to take an important role as DNE is either ignored or in some cases limited to a few days education (usually 2–3 days by sending nurses to an Endocrinology and Metabolism Research Center). In these circumstances, the nurse who did not receive any theoretical training and only observed nurses’ practices in Endocrinology and Metabolism Research Center was considered as a trained nurse. The lack of formal training led to employ nurses as DNEs who had lack of a specialized knowledge in the field of diabetes and its care and especially the scientific and practical patient education skills. Therefore, nurses accepted a role without preparation and previous experience.
One of the chief executives of diabetes management in the province said:
“Now, if a nurse comes without passing diabetes courses, we send him/her to a diabetes center to spend several daysthere and be familiar with special responsibilities of diabetes nurse. However, currently there is no structured education.”
Several field observations suggested that nurses working in the diabetes units of province cities (which are the majority of nurses) even did not receive such mentioned training. Therefore, without exception all nurses participating in the study were working as DNE with no training courses.
One of the nurses participating in the focus group said:
“When I started to work as diabetes nurse, they told me these are diabetes-related forms in this folder, and these are patient education pamphlets…you should educate them based on these papers and pass theses pamphlet to them. Oh, even they did not tell me how I should fill these forms…they did not teach me anything.”
Another nurse in the focus group also said:
“I remember nobody noticed me, I had not passed any courses, they choose me for this work (diabetes nurse) with obligation. It was not my interest.”
Another one believed that not only she but also none of the nurses who worked in diabetes units had not passed special courses.
“I never took part in any special courses for this purpose, none of nurses did it.”
Numerous field observations also indicated that none of the nurses in diabetes units took part in the training courses. Nurses were trying to obtain diabetes care-related information through their personal study, using experiences and knowledge of coworkers and physicians in diabetes unit in which they worked. It means they applied experiences of nurses who did not pass special course themselves. One of the nurses said:
“A nurse who worked here before me … held for me three sessions. She told me do not worry, do not be sad… you will be familiar with patients gradually over time.”
She has received three educational sessions from a nurse who worked herself without passing an education course related to diabetes care. However, not all nurses had chance to enjoy coworkers’ experiences and information. One nurses said:
“Similar to others, previous nurse who was head nurse and also was an uneducated diabetes nurse did not give me any special information.”
Another resource for diabetes nurses to obtain information was physician in diabetes unit in which they worked. One nurse said:
“I myself learned some things from our physician.”
Using colleagues’ experiences at least reduced the novice nurses’ anxiety and increased their practical knowledge but considering that, there was no supervision and evaluation of experienced nurse’s knowledge in the diabetes center. Unavoidably, it was possible to transfer invalid and incorrect information to each other. Inasmuch as nurses’ average score in a pre-test were confirmed that nurses could not compensate their knowledge deficit by self-study and their colleagues’ experiences.
The data indicated that a specific supervising and guiding tool for managing DNE education was not considered in macro- and micro-level planning. It means that scientific-strategic manuals and guidelines of National Project on Diabetes Prevention and Control lack any instructions for monitoring the process of staff training including nurses. One of the executive officials said:
“Individual specific evaluation has not designed until now…There is only one thing…if it is done…that we do, we get their function three to six months intervals. It is based on file numbers that they have. Whole unit will be assessed based on their reported statistical data (not one by one employee).”
Lack of program monitoring caused that planners in ministries and the chief executives of the provinces did not have the correct information about training or retraining of nurses. One of the executive stated:
“For example, I went to visit. A nurse sat there… I told her when you took part in retraining program. She answered I came here three years ago from the hospital but they did not hold any educational course for me until now.”
Moreover, one of the nurses in the focus group pointed to the lack of official attention to the educational performance of nurses. He stated:
“I told all the authorities that you just want us a statistics sheet…I think system expected them just this…”
Statements of a policy maker in diabetes management in macro level indicated that despite delegation of health care providers’ education to provinces, there is no actual education especially for nurses. He said:
“They need to constantly learn, to know new diabetes information… Nevertheless, it is done rarely.”
Trying to reform nursing education infrastructures
Analyses of manuscripts represented the concerns of policymakers of diabetes management at macro-level about preparing/providing experts for training DNE. One of the planners said:
“At that time we searched but we did not have diabetes educator in Iran (he means by that time about one decade ago, when diabetes was placed in priorities of health system). We held several workshops for nurses. With holding them at first we found that it is difficult to find someone who comes for teaching nurses, i.e. we did not have any one for this purpose… This simply means we did not have suitable and qualified educators in Iran. They were not very much to find some at every university.”
Two strategies have been adopted in facing this challenge. To address the problem (lack of educators) temporarily, WHO-approved diabetes educators were invited. One participant said:
“We searched and found out that there are few top and well-known educators in the world, and WHO recommend them and International Diabetes Associations also offer them. So we invited them.”
Planners decided to train diabetes educators within the country to provide educator in long term. One participant said:
“We decided to make an educational core group, develop a program for training educators. Then we delegated this responsibility to this core group. They were responsible to go to other places and educate nurses. Anyway, finally in this project we were unsuccessful again although nursing office in Ministry was our coworker in this matter…”
In the other word, planners failed to provide and educate educators of DNE. Lack of experiences in diabetes management and undergraduate nursing curriculum defect were mentioned as an explanation for failure in preparing educators. One participant told us:
“Firstly, we did not have any experience in diabetes. Nurses who were here and have been training had not information in this matter too. Even their professors at university limited their education to textbook. They gave no enough information in this matter to them. I mean students just relied on the notes told in class.”
Undergraduate nursing curriculum failure to prepare students to provide care to patients with chronic diseases such as diabetes has been considered as a serious challenge for planners. One participant said:
“Training our doctors, nurses, and nutrition experts in our universities is not in such level to compensate the country health needs.”
The planners and executive officials of diabetes management believed graduate nurses do not have knowledge and skills to provide services to people with diabetes. One participant said:
“None of our nurses has worked with patients with diabetes in a special and expert manner. They had not a lot of information in this matter. Their most information is about treatment (i.e. how to manage hospitalized patient). They did not receive education in their curriculum.”
Knowledge deficit was not only planers’ concern, but also nurses believed that they do not have correct and adequate knowledge to care for diabetes without specialized courses. A nurse stated:
“Many of these nurses do not have correct and accurate information or if any have, it is incomplete. However, there is not valid information.”
Proposal to reform medical science education curriculum, including nursing, was one of the planners’ measures at the macro level. One participant said:
“We negotiated with the Vice-Chancellery for Education in the Ministry of Health and Medical Education that you should change educational curriculum at least for nurses, nutritionists, and general practitioners. You need to update it in order to prepare students to provide good health services.”
Examining undergraduate nursing curriculum in Iran, which is a centralized program, indicated that twelve hours of all nursing educational period was dedicated to nursing care for endocrine disorders, and just two hours was dedicated to cover diabetes care. During four years academic education, students only spend a six-day period in the real field to earn practical skills in the care of patients with endocrine disorders including diabetes.
Failure of DNE curriculum
Diabetes educator is one of the roles considered for nurses in the diabetes prevention and control. In addition, the book of Diabetes Prevention and Control Program listed some other roles and duties for the nurses in diabetes centers and units that most notably one is management of diabetes unit. With regard to nurse’s educational role, planners believed provided education for nurses was enough to prepare them as diabetes educator. One participant said:
“In fact, we educated nurses as diabetes educators.”
Time intended for education of nurses working in diabetes units as DNE was just two to three days, based on book of Diabetes Prevention and Control Program.[19] Course content included nurse’s role and its importance in the program, the importance of diabetes and its acute and chronic complications, self-monitoring, introducing glucometers, the role of nutrition and exercise in disease control, administration and maintenance of insulin, blood pressure measurements, and providing educational programs for patients and their families.[19] Planners prepared educational content for nurses in a book. One participant said:
“We wrote a book for nurses about caring for diabetes. We invited a group of expert nurses of nursing office who wrote this. We held a workshop. Nurses took part and discussed with each other. These resulted in this book.”
This book was published and distributed in healthcare systems across the country in 2004. Only four of nineteen nurses working in diabetes units knew about availability of such a book, and used it as an educational source for patient education. On the other hand, planners believed that this published source do not meet nurses’ needs for patient education. One of the planners in this regard referred to plans for providing a suitable source and guideline for nurses and said:
“Nurses’ problem should be solved … we must gather all materials and examine them. We must review it and provide a complete and comprehensive text. It must be very complete so when a nurse decides to educate patient, she/he be able to refer to this and find all required material word by word.”
In current DNE curriculum, there is not any content in relation to patient education principles, teaching methods, evaluation methods for patient education. In addition, it does not have definition for time criterion and evaluation method(s) for learning assessment of nurses who took part in educational program. At the same time, it is a considerable point that during the six years of holing national diabetes prevention and control programs, nurses’ knowledge and skills was not assessed. One of the chief executives expressed:
“Well, we did not evaluate it and also no national evaluation mechanism is defined for it.”
Another person in charge stated that:
“We did not deal with evaluation issue. However, evaluation is the first and last letter of all health care issues.”
Data from interviews and several field observations also suggested that scientific competences of nurses working in the diabetes units have not been assessed so far, and they have not received any feedback. One of the nurses stated:
“They do not value the nurses who try to do best and knowledgeable, so it does not encourage others. I think in health system when you want to update your information or you want to work in an educational manner, sometimes manager or health system treats you in such way that you get depressed or frustrated.”
DISCUSSION
Nurses are the backbone of health systems around the world and play a key role in delivering health services.[24] Moreover, the role of nurses in the prevention and management of chronic diseases including diabetes has priorities and importance. Numerous studies (including systematic reviews and clinical trials) confirmed the effective nurse role in patients and family education and consultation and guiding patient towards diabetes self- management.[25,26,7] Therefore, nowadays pressing requirement to increase investment in education for professionals including nurses is felt all over the world and several measures to evaluate and improve nurses’ professional competences especially in the diabetes prevention and management have been assumed.[8,27,28] For example, in Japan at least 1000 hours of experience in diabetes education and passing the relevant tests is necessary for taking Diabetes Educator Certification of the Japanese Certification Board, since 2001. Now, Japanese nurses compose about 5,753 people of 12000 diabetes educators.[29]
Findings of current study showed that nurses were employed in diabetes centers without assessing their diabetes-related knowledge, or necessity of experience in diabetes education, or even without taking any educational course.
Given that diabetes management is centralized in Iran, it seems that inadequate supervision of the planners in the Ministry of Health on provincial health system performance is the most important factor for entering untrained nurses in the field of diabetes management. WHO believes one of the most effective available tools to improving health workers’ competences is supervision.[30] It is necessary to consider that in health system’s organizational chart in the Iran, the single formally defined place to recruit nurses is hospitals. Therefore, diabetes management planners are facing serious challenges for recruiting nurses for diabetes centers and units, which are outpatient centers. However, lacks of supervision caused nurses do not receive education not only at beginning the work but also during their work in diabetes centers, while lifelong learning should be included in the workplace as an inseparable part of staffs’ activities.[30] Siminerio et al.[17] in a cross- sectional study on US nurses’ perception of their role in diabetes care concluded that nurses need education in the field of diabetes in spite of receiving primary education, and patient education and counseling experience. Interestingly, they showed that the specialist nurses felt more need for continuing education than general nurses did. Researches also showed that the higher the educational level of nurses, the more are patient safety and quality care.[31] Nurses in training were in a situation that planners knew about inadequacy of undergraduate nursing curriculum in preparing nurses for education and caring of patients with chronic diseases, and knowledge deficit of nurses who are candidate for diabetes centers.
The insufficiency of undergraduate nursing curricula in preparing nurses to deal with challenges related to chronic diseases is not unique to Iran. WHO also believes the world is rapidly faced with health problems caused by chronic diseases but training, education and skills of health personnel are inadequate to meet today’s requirements for managing patients with chronic diseases.[12] It means that health professionals’ curriculum content do not meet the current needs of the community health systems (i.e. clinical education is not able to respond to changes in the demographic characteristics of patients and thus changes in the needs and expectations of health systems, including required skills and new technology and the quality of care).[32] For any changes, it is necessary to face challenges arising from that change. Nevertheless, we must seriously consider planners’ statements that are indicating they still could not compensate lack of trainers and adequate training programs for diabetes nurse or DNE in spite of a decade of planning for the education of DNE, and its consequence (i.e. employing untrained nurses in the diabetes units). Lee et al. described how they could prepare nurse educators for changing education methods and learning online education within less than a year with a need-based plan (which was reviewed by experts).[33] Neither the time allocated to training nor educational content of DNE curriculum covers nurses’ learning need for playing mentioned roles for them. For example, it does not pay attention to one of the most important nurses’ need i.e. patient education principals. While patient education-related issues is one of the major parts of content in diabetes educator educational courses.
Therefore, the findings reflected the failure and serious and multiple challenges in educating nurses working in diabetes units. Despite this fact that important roles including educator and manager have been defined for nurses in the action plan for preventing and controlling diabetes, any specific action was not done in preparing nurses for these roles. On the other hand, there is no appropriate supervision for nurse’s performance while nurses’ competence has a key role for patient education and guiding them toward self-management. Therefore, it seems that it is necessary to revise management of diabetes nurse education, re-plan education based on update standards, and adjust educational programs based on actual potentials of educational system. Finally, the most important measure is to form actually a system for monitoring, supervising, and evaluating the process of diabetes nurse education.
ACKNOWLEDGMENT
We wish to acknowledge all the participants who contributed in any way for completion of this study. Faculty of Medical Sciences of Tarbiat Modares University, Tehran, Iran, financially supported this study.
Footnotes
Research Article of Tarbiat Modares University, Tehran, Iran
Source of Support: Tarbiat Modares University, Tehran, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Hussain A, Claussen B, Ramachandran A, Williams R. Prevention of type 2 diabetes: a review. Diabetes Res Clin Pract. 2007;76(3):317–26. doi: 10.1016/j.diabres.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Esteghamati A, Khalilzadeh O, Anvari M, Meysamie A, Abbasi M, Forouzanfar M, et al. The economic costs of diabetes: a population-based study in Tehran, Iran. Diabetologia. 2009;52(8):1520–7. doi: 10.1007/s00125-009-1398-4. [DOI] [PubMed] [Google Scholar]
- 3.Khuwaja AK, Khowaja LA, Cosgrove P. The economic costs of diabetes in developing countries: some concerns and recommendations. Diabetologia. 2010;53(3):389–90. doi: 10.1007/s00125-009-1581-7. [DOI] [PubMed] [Google Scholar]
- 4.Kirigia JM, Sambo HB, Sambo LG, Barry SP. Economic burden of diabetes mellitus in the WHO African region. BMC Int Health Hum Rights. 2009;9:6. doi: 10.1186/1472-698X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang JS, Lin SY, Sheu WH, Lee IT, Tseng LN, Song YM. Effects of patient volume on quality of outpatient diabetes care. Diabetes Res Clin Pract. 2009;84(3):e27–e29. doi: 10.1016/j.diabres.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Chuang LM, Tsai ST, Huang BY, Tai TY. The status of diabetes control in Asia-a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabet Med. 2002;19(12):978–85. doi: 10.1046/j.1464-5491.2002.00833.x. [DOI] [PubMed] [Google Scholar]
- 7.Peimani M, Tabatabaei-Malazy O, Pajouhi M. Nurses’ Role in Diabetes Care; A review. Iranian Journal of Diabetes and Lipid Disorders. 2010;9(4):1–9. [In Persian] [Google Scholar]
- 8.Amoah AG, Owusu SK, Acheampong JW, Agyenim-Boateng K, Asare HR, Owusu AA, et al. A national diabetes care and education programme: the Ghana model. Diabetes Res Clin Pract. 2000;49(2–3):149–57. doi: 10.1016/s0168-8227(00)00140-6. [DOI] [PubMed] [Google Scholar]
- 9.Khowaja LA, Khuwaja AK, Cosgrove P. Cost of diabetes care in out-patient clinics of Karachi, Pakistan. BMC Health Serv Res. 2007;7(1):189. doi: 10.1186/1472-6963-7-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abolhasani F, Tehrani MR, Larijani B. Burden of diabetes and its complications in Iran in year 2000. Iranian Journal of Diabetes and Lipid Disorders. 2005;5(1):35–48. [In Persian] [Google Scholar]
- 11.Valdez GM, Dadich KA, Boswell C, Cannon S, Irons BK, Vickers P, et al. Planning and implementing an interdisciplinary diabetes workshop for healthcare professionals. J Contin Educ Nurs. 2007;38(5):232–7. doi: 10.3928/00220124-20070901-02. [DOI] [PubMed] [Google Scholar]
- 12.Pruitt S, Canny J, Epping-Jordan J. Preparing A Health Care Workforce For The 21st Century: The Challenge Of Chronic Conditions. Geneva: World Health Organization; 2005. [Google Scholar]
- 13.Pruitt SD, Epping-Jordan JE. Preparing the 21st century global healthcare workforce. BMJ. 2005;330(7492):637–9. doi: 10.1136/bmj.330.7492.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q. 2003;7(1):73–82. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- 15.Peytremann-Bridevaux I, Staeger P, Bridevaux PO, Ghali WA, Burnand B. Effectiveness of chronic obstructive pulmonary disease-management programs: systematic review and meta-analysis. Am J Med. 2008;121(5):433–43. doi: 10.1016/j.amjmed.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Lemmens KM, Nieboer AP, Huijsman R. A systematic review of integrated use of disease-management interventions in asthma and COPD. Respir Med. 2009;103(5):670–91. doi: 10.1016/j.rmed.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Siminerio LM, Funnell MM, Peyrot M, Rubin RR. US nurses’ perceptions of their role in diabetes care: results of the cross-national Diabetes Attitudes Wishes and Needs (DAWN) study. Diabetes Educ. 2007;33(1):152–62. doi: 10.1177/0145721706298194. [DOI] [PubMed] [Google Scholar]
- 18.Azizi F, Gouya MM, Vazirian P, Dolatshahi P, Habibian S. The diabetes prevention and control programme of the Islamic Republic of Iran. East Mediterr Health J. 2003;9(5–6):1114–21. [PubMed] [Google Scholar]
- 19.Delavari A, Mahdavi Hazave A, Norouzi Nejad A, Yarahmadi SH. National Plan of prevention and control of diabetes. Tehran: Seda Publication; 2004. [In Persian] [Google Scholar]
- 20.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 21.Wildemuth BM. Applications of Social Research Methods to Questions in Information and Library Science. Colorado: Libraries Unlimited; 2009. [Google Scholar]
- 22.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(3):105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Scaling up nursing and midwifery capacity to contribute to the millennium development goals 2008-2009. Proceedings of the 1st Meeting of Focal Points on the Implementation of the Global Programme; 2009 Mar 23-24; Geneva, Switzerland. 2009. [Google Scholar]
- 25.Gabbay RA, Lendel I, Saleem TM, Shaeffer G, Adelman AM, Mauger DT, et al. Nurse case management improves blood pressure, emotional distress and diabetes complication screening. Diabetes Res Clin Pract. 2006;71(1):28–35. doi: 10.1016/j.diabres.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, et al. The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med. 2002;22(4 Suppl):15–38. doi: 10.1016/s0749-3797(02)00423-3. [DOI] [PubMed] [Google Scholar]
- 27.Thomson GA, Medagama A, Dissanayake A, Lenora D, Kumarihamy W, Weremczuk D, et al. Pandemic diabetes: can developed-world health professionals do more to support care in developing countries? European Diabetes Nursing. 2008;5(1):23–7. [Google Scholar]
- 28.Celeste-Harris S, Maryniuk M. Educating Medical Office Staff: Enhancing Diabetes Care in Primary Care Offices. Diabetes Spectrum. 2006;19(3):84–9. [Google Scholar]
- 29.Kawaguchi T. Certified diabetes expert nurse and nurse educators in Japan. Diabetes Res Clin Pract. 2007;77(Suppl 1):S205–S207. doi: 10.1016/j.diabres.2007.01.058. [DOI] [PubMed] [Google Scholar]
- 30.Chen L, Evans D, Evans T. The world health report 2006: working together for health. Geneva: World Health Organization; 2006. [Google Scholar]
- 31.Department of Human Resources for Health. Global Standards for the Initial Education of Professional Nurses and Midwives. Geneva: World Health Organization; 2009. [Google Scholar]
- 32.Greiner AC, Knebel E. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies press; 2003. [PubMed] [Google Scholar]
- 33.Lee D, Paulus TM, Loboda I, Phipps G, Wyatt T, Myers C, et al. Instructional design portfolio: A faculty development program for nurse educators learning to teach online. Tech Trends. 2010;54(6):20–8. [Google Scholar]


