Abstract
Background:
Mood stabilizers are drugs used to steady/balance the mood, and are also used to manage symptoms of aggression and impulsivity. There is disparity in prescription pattern across the globe.
Aim:
The aim of this study was to observe prescription pattern of mood stabilizers for the treatment of bipolar disorder with or without psychotic symptoms.
Materials and Methods:
A sample of 100 adult patients was selected to participate in the study. First 5 patients of bipolar disorder with or without psychotic symptoms from twenty out-patient departments of various consultant psychiatrists of Department of Psychiatry (C.S.M. Medical University, Lucknow) were included in the sample. A written informed consent was obtained and survey method was adopted to conduct the study.
Results and Conclusion:
Lithium was found to be the most frequently prescribed mood stabilizer, sodium valproate ranked second while carbamazepine was least frequently prescribed.
Keywords: Bipolar disorder, mood stabilizers, prescription pattern
INTRODUCTION
Mood stabilizers, as the name suggests, are drugs that are primarily used to steady/balance the mood. These are primarily used in the treatment of bipolar disorder both for acute management as well as for prophylaxis. However, it must be borne in mind that most mood stabilizers, with the exception of lamotrigine and lithium, are primarily anti-manic agents as their efficiency in depressive phase of illness remains questionable. However, for want of a better word and continuing with the common parlance, the authors have continued with the present nomenclature.
Besides bipolar illness and associated “spectrum” conditions, mood stabilizers are also used to manage symptoms of aggression and impulsivity in attention deficit-hyperactivity disorder (ADHD), conduct disorders, and also in borderline personality disorders. There is disparity in prescription pattern from consultant to consultant and from country to country. This study was hence carried out to assess the prescription pattern of mood stabilizers in the department of psychiatry, C.S.M. Medical University (formerly King George's Medical University Lucknow), Lucknow, Uttar Pradesh, which, being a tertiary care centre, gets patients from all walks of life, right from referrals from other centers to new cases entering into mental healthcare for the first time.
MATERIALS AND METHODS
Study design and population
Following a standardized protocol, 100 patients attending adult psychiatry out-patient department (OPD) for the treatment of bipolar disorder were included in the study. Selected patients fulfilled the diagnostic criterion for bipolar disorder with or without psychotic symptoms of the International Classification of Disease, 10th revision (ICD-10).[1] The first 5 patients who were diagnosed as suffering from bipolar disorder with or without psychotic symptoms and attending psychiatric OPD for follow-up were included in the study from 20 consecutive OPDs of various consultant psychiatrists. A written informed consent in the local language (Hindi) was obtained from the patient. Survey method was adopted to conduct the study. Data regarding factors like age, sex, mood stabilizers, and other psychotropic drugs prescribed, and combination of psychotropic medications prescribed were collected. Medications other than psycho-tropics were not recorded.
RESULTS
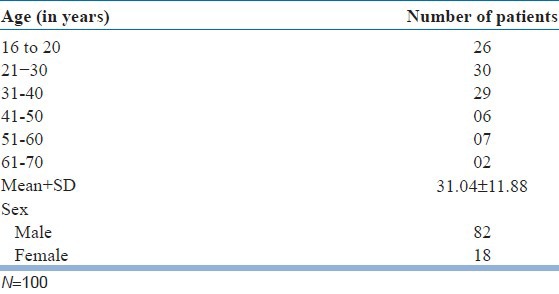
A total of 100 patients were surveyed, of which, 26 patients were of age < 20 years, 30 patients of 21-30 years, 29 patients of 31-40 years, 6 patients of 41-50 years, 7 patients of 51-60 years, and 2 patients were of 61-70 years. Out of 100 patients, 82 were male and 18 were female, with a mean age of 31.45 years [Table 1].
Table 1.
Distribution of age and sex
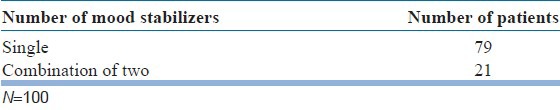
It was observed that 79 patients were prescribed a single mood stabilizer and 21 were prescribed a combination of two mood stabilizers [Table 2].
Table 2.
Number of mood stabilizers prescribed
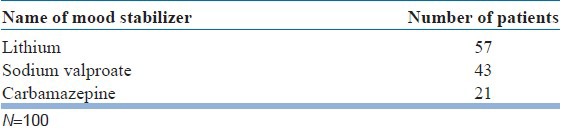
Lithium turned out to be the most frequently prescribed mood stabilizer, and sodium valproate ranked second in the hierarchy of prescriptions. Carbamazepine was the least frequently prescribed mood stabilizer [Table 3].
Table 3.
Frequency of prescribed mood stabilizers in descending order
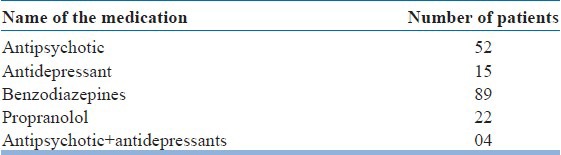
Results showed that 52 patients were prescribed anti-psychotics, 15 patients were prescribed anti-depressants, 89 patients were prescribed benzodiazepines, 22 patients were prescribed propranolol, and 4 patients were prescribed a combination of antipsychotic with antidepressants [Table 4].
Table 4.
Other medications prescribed with mood stabilizers
It is evident from Table 5 that the highest number of patients received a combination of mood stabilizers with antipsychotic and benzodiazepines. Second highest group of patients was prescribed a combination of mood stabilizers and benzodiazepines.
Table 5.
Combination of antidepressants with other psychotropic drugs
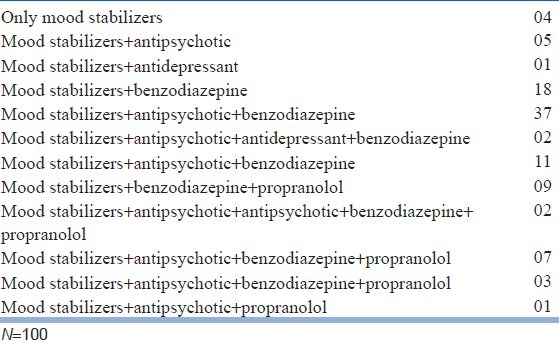
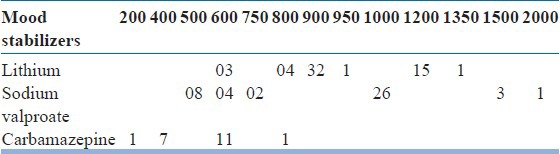
Table 6 shows that lithium was prescribed to most patients in the dose of 900 mg/day. Sodium valproate was most commonly prescribed in dose regimen of 1000 mg/day (26 patients). Among the patients who were prescribed carbamazepine, most received it in dose of 600 mg/day (11 patients).
Table 6.
Number of patients with different dose (in mg/day) of mood stabilizers
DISCUSSION
Male patients far outnumbered females in the present study. This trend highlights the demography of the patient population coming in our OPD. Male members have a higher help seeking behavior as mostly they are economically productive and, at times, the sole bread winners of the family. Although many of the psychiatric conditions have equal incidence in both the genders and some are even more so in females, the patients attending OPDs in most psychiatric centers as well as the indoor patients in psychiatric ward belonged to male gender. This highlights the gender bias prevalent in India and is seen in other South Asian countries as well.
More than half of the sample size comprised of patients between the age group of 21-40 years, highlighting the fact that bipolar disorder tends to effect economically productive sections of our society. Hence, this study emphasizes the need for evolving a better regimen to treat bipolar disorder and greater efforts to ensure regular, long-term compliance on medications.
Majority of patients were prescribed a single mood stabilizer. Most guidelines profess a single mood stabilizer while initiating treatment and using it to maximum possible dose before switching or augmenting it with another agent. Also, since adding another mood stabilizer adds to the cost of the total treatment and most patients coming to our OPD belonged to lower economic strata, this factor too was taken into consideration.
It was observed that 21% of the patients were prescribed a combination of two mood stabilizers. This study hence highlights that polypharmacy is being practiced in treatment of bipolar disorder. Evidence-based polypharmacy and justifying the prescription is the need of the hour and, at times, medications more than one will be required for the management of symptoms and to ensure compliance. Also, this being a tertiary care centre, the patients coming in the OPDs may have been treated outside with other mood stabilizers/antipsychotic and yet not shown improvement. There are also subgroups of patients who may have relapsed despite adequate dosage of a mood stabilizer.
More than half of the patients received lithium. According to a review of the literature by Mark Bauer MD of Brown University, lithium is the only true mood stabilizer, with published studies proving its efficacy in all phases of bipolar treatment, including acute (initial phase) mania and mania prevention, and acute depression and depression prevention. This ability to be all things at once holds out the promise of a simplified one-drug treatment for those fortunate enough to respond.
On the flip side, as an augmenter, the drug can boost the performance of another drug. These days, due to lack of drug companies promoting the drug and the extra care that the doctors must be observed in prescribing it, other medications have become more popular (Pilcher, 2003),[2] although it remains a first choice option on all treatment guidelines. Sodium valproate ranked second in the hierarchy of prescriptions. Carbamazepine was the least frequently prescribed mood stabilizer.
It was also noted that lamotrigene was not prescribed frequently. This could be due to multiple reasons like slow increments in dosage required to reach effective dose, which would warrant frequent OPD visits (our centre receives patients from far flung areas and frequent visits means spending more on travel). Another reason could be fear of adverse drug reactions like drug rash and Steven Johnson Syndrome (more commonly associated with lamotrigene).
It would be interesting to know treatment patterns followed in other institutes of repute and compare them with our findings. Many patients of bipolar disorder first attend OPD during manic phase of illness since it's more disruptive (to attendants and others in general), whereas depressive symptoms are likely to be at times missed by attendants. Hence, the mood stabilizer that is started during that time is likely to be continued in subsequent visits.
Newer mood stabilizers like oxcarbazepine have not been represented in this study. A probable reason for this is the fact that current data still points out to a similar efficacy between carbamazepine and oxcarbazepine with the latter having better side effect profile (Mosolov et al., 2009).[3] In price sensitive patients where these drugs have to be continued for a long time, preference hence has to be given to high efficacy and lower priced drugs.
It was observed that 52 patients were co-prescribed anti-psychotics with mood stabilizers, 15 were co-prescribed antidepressants, 89 received benzodiazepines, 22 were prescribed propranolol with mood stabilizer, and 4 were given a combination of antipsychotic with antidepressants.
It was found that the highest number of patients received a combination of mood stabilizers with an antipsychotic and benzodiazepines, which highlights the need for initial symptomatic management and also highlights the complaints with which the patients present to the OPD, namely aggression (antipsychotics), disturbed sleep (benzodiazepines), and co-morbid anxiety (benzodiazepines).
This study shows that lithium was prescribed to most patients in the dose of 900 mg/day. It has been the authors’ clinical experience that a significant number of patients attending OPD in the department achieve therapeutic levels at the aforementioned dose. It is not possible to comment about long-term use of lithium in this study because observations are based on one time look at the prescription pattern, and this is one of the lacuna for such type of work.
Sodium valproate was prescribed in dose regimen of 1000 mg/day to 26 patients. Among the patients who were prescribed, carbamazepine was received the most in a dose of 600 mg/day. Although recommended doses of carbamazepine are higher, the use of this dose more commonly could be due to the fact that higher doses are associated with greater side effects.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.International Statistical Classification of Diseases and Related Health Problems. 10th Review. Geneva: World Health Organization; 1992. World Health Organization. [Google Scholar]
- 2.Pilcher HR. Drug research: The ups and downs of lithium. Nature. 2003;425:118–20. doi: 10.1038/425118a. [DOI] [PubMed] [Google Scholar]
- 3.Mosolov SN, Kostiukova EG, Ladyzhenskiĭ MIa. Comparative efficacy and tolerability of carbamazepine and oxcarbazepine during long therapy of patients with bipolar and schizoaffective disorders. Zh Nevrol Psikhiatr Im S S Korsakova. 2009;109:36–41. [PubMed] [Google Scholar]


