Abstract
Context:
Literature suggests glottic view is better with straight blades while tracheal intubation is easier with curved blades.
Aims:
To compare glottic view and ease of intubation with Macintosh, Miller, McCoy blades and the Trueview® laryngoscope.
Settings and Design:
This prospective randomised study was undertaken in operation theatres of a 550 bedded tertiary referral cancer centre after approval from the Institutional Review Board.
Methods:
We compared the Macintosh, Miller, McCoy blades and the Trueview® laryngoscope for glottic visualisation and ease of tracheal intubation; in 120 patients undergoing elective cancer surgery; randomly divided into four groups. After induction of anaesthesia laryngoscopy was performed and trachea intubated. We recorded: Visualisation of glottis (Cormack Lehane grade), ease of intubation, number of attempts; need to change the blade and need for external laryngeal manipulation.
Statistical Analysis:
Demographic data, Mallampati classification were compared using the Chi-square test. A P<0.05 was considered significant.
Results:
Grade 1 view was obtained most often (87% patients) with Trueview® laryngoscope. Intubation was easier (Grade 1) with Trueview® and McCoy blades (93% each). Seven patients needed two attempts; one patient in Miller group needed three attempts. No patient in McCoy and Trueview® Groups required external laryngeal manipulation.
Conclusions:
We found that in patients with normal airway glottis was best visualised with Miller blade and Trueview® laryngoscope however, the trachea was more easily intubated with McCoy and Macintosh blades and Trueview® laryngoscope.
Keywords: Cormack lehane grade, external laryngeal manipulation, intubation, laryngoscopy
INTRODUCTION
Airway management is the primary responsibility of the anaesthesiologists: To secure, preserve and protect it during induction, maintenance and recovery from anaesthesia. Failure to manage airway can lead to catastrophic results; death or worse; brain damage. Most anaesthesia mishaps occur at the time of induction of anaesthesia.[1] Orotracheal intubation is the most common method used to secure and maintain airway. A variety of methods are available for intubation: Digital or tactile method, lighted stylet, intubating LMA, fibre optic endoscopic intubation and conventional direct laryngoscopy.
Glottic view during laryngoscopy can be classified using Cormack Lehane grading[2] or percentage of glottic opening (POGO Score).[3] Glottic view can be improved by external manipulation of larynx using either backward-upward-rightward pressure (BURP) or Bimanual Laryngoscopy. The need for external manipulation and the number of attempts are indicators of difficulty encountered during laryngoscopy and intubation.
Literature[4] suggests that glottis is viewed better with the straight blades while tracheal intubation is easier with the curved blades. We therefore, compared the Macintosh, Miller, McCoy blades and the Trueview® laryngoscope (Truphatek International Ltd, Netanya, Israel), which incorporates a prism in a straight blade, for glottic visualisation and ease of tracheal intubation.
METHODS
This prospective randomised study was conducted after obtaining approval from the Institutional Review board. One hundred and twenty adult patients, based on convenience sampling, were included who had given written informed consent. These patients were ASA grade I or II, between 18 years and 70 years of age, were undergoing elective cancer surgery under general anaesthesia requiring endotracheal intubation. Patients were excluded if they refused consent, were pregnant, had potential difficult mask ventilation and/or anticipated difficult intubation or had pathology in neck, upper respiratory tract and upper alimentary tract. A detailed routine pre-anaesthetic check-up was performed in the pre-anaesthesia check-up clinic; where airway was assessed using Mallampati Scale, Inter-incisor gap, jaw slide and normalcy of neck movements; and routine laboratory investigations were obtained. As per random numbers generated by computer the patients were divided in four groups of 30 each: Group 1: Macintosh, Group 2: McCoy, Group 3 Miller and Group 4: Trueview® laryngoscope.
In the operating room, pulse oximeter, electrocardiograph, capnography and automated non-invasive blood pressure were attached for monitoring and intravenous access was secured. Demographic data such as age, sex and weight of the patient was noted. Airway assessment was once again carried out using Samsung and Young's modification[5] of the Mallampati classification. The patient was asked to sit, open the mouth maximally, and protrude the tongue but not phonate. Visibility of the oral and pharyngeal structures was then classified by an observer sitting at the same level as the patient.
Class I: Soft palate, fauces, uvula, pillars visible
Class II: Soft palate, fauces, portion of uvula, visible
Class III: Soft palate, base of uvula visible
Class IV: Only hard palate visible.
A Doughnut-shaped pillow and hard sponge square pillow, was placed under the head of the patient to obtain classical sniffing position. The patient was pre-oxygenated with 100% oxygen for 3 min. Anaesthesia was then induced with 1-3 mg/kg of propofol or thiopentone sodium 5 mg/kg, fentanyl 2 μg/kg. Feasibility of ventilation with a face mask was checked prior to injection of non-depolarising muscle relaxant. After ventilation was confirmed vecuronium was administered and the patient was ventilated with isoflurane 0.5-1% in 50:50 mixture of O2 and N2O for 3 min then ventilated for 1 min with 100% O2. The laryngoscopy and intubation were carried out in classical intubating position by a single anaesthesiologist. This investigator had trained for 2 months with all laryngoscope blades until he had obtained sufficient familiarity. We studied following aspects during tracheal intubation.
Visualisation of laryngeal inlet: This was graded using Cormack Lehane (CL) Grades:
Grade 1: Complete glottis visible
Grade 2: Anterior glottis not seen
Grade 3: Epiglottis seen but not glottis
Grade 4: Epiglottis not seen.
Ease of intubation: This was graded as follows:[4]
Grade 1: Intubation easy
Grade 2: Intubation requiring an increased anterior lifting force and assistance to pull the right corner of the mouth upwards to increase space
Grade 3: Intubation requiring multiple attempts and a curved stylet
Grade 4: Failure to intubate with the assigned laryngoscope.
If the view after laryngoscopy was more than CL Grade 2 external laryngeal manipulation was carried out. The need for external manipulation was classified as Grade 1: No requirement of external laryngeal manipulations and Grade 2: Requirement of external laryngeal manipulation.
Number of attempts was noted. After failure at first attempt stylet was used. Patients were ventilated with 100% oxygen between attempts at laryngoscopy and intubation so that no patient was allowed to desaturate below 95%. After 3 attempts at intubation with assigned blade, patients were intubated using Macintosh blade.
Statistical analysis
Demographic data, Mallampatti Classification and other variables were compared using the Chi-square test using SPSS version 16. A P<0.05 was taken to assume statistical significance.
RESULTS
This study was carried out over a period of 8 months. During the first 2 months, the anaesthesiologist practiced with all laryngoscope blades until he was proficient. The patients included in the study were between 18 years and 70 years of age. The mean age, weight and Mallampati scores were similar in patients undergoing intubation with different laryngoscope blades [Tables 1 and 2]. All patients were easy to ventilate and there were no failed intubations.
Table 1.
Demographics

Table 2.
MPC grading

Grade 1 view was obtained most often (87% patients) using the Trueview® laryngoscope [Table 3]. This was followed by Miller (83%), then McCoy (77%) and then the Macintosh blade (63%). This was not statistically significant and intubation was easier (Grade 1) with Trueview® and McCoy blades (93% each). The ease of intubation was similar with these two blades as with Macintosh blade, i.e., 90% of patients had Grade 1 intubation. With the Miller blade, Grade 1 ease at intubation was seen only in 57% patients [Table 4]. The difference between McCoy, Trueview® and Miller groups was statistically significant (P=0.01). Most patients were intubated at the first attempt with all laryngoscopes [Table 5]. Only seven patients needed 2 attempts, while one patient in Miller group needed 3 attempts. Seven patients in Macintosh group and three patients in Miller group [Table 6] required external laryngeal manipulation. No patient in either McCoy or Trueview® group required external laryngeal manipulation.
Table 3.
Glottic visualization

Table 4.
Ease of intubation
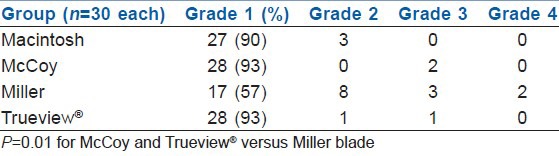
Table 5.
No. of attempts at intubation
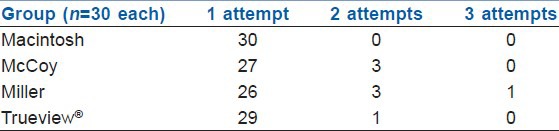
Table 6.
Need for external laryngeal manipulation

DISCUSSION
We undertook this study to confirm the hypothesis that glottic visualization is better with straight blade however; intubation is easier with the curved blades. Patients undergoing head and neck cancer surgery for intraoral pathology were excluded as the presence of disease in oral cavity itself may lead to difficulty in glottic visualisation and intubation and our aim was to compare use of the various laryngoscopes in patients with normal anatomy. Inclusion of these patients may have confounded the results of our study; as it is difficult to match patients with equal “degrees” of difficult intubation.
In two patients in the Miller Group, the glottis was visible (CL Grade 2 view), but the trachea impossible to intubate with that blade in 3 attempts, we had to switch to Macintosh blade to intubate the trachea (CL Grade 3 view, which improved to Grade 2 on BURP). We found that the quality of glottic visualisation was best with True-View laryngoscope and Miller blade. Even with McCoy blade, a Grade I view was obtained in 77% of patients. Macintosh blade performed the worst (63% Grade I view). This difference was not statistically significant, probably reflecting small sample size. These findings are corroborated by our other findings. We found external laryngeal manipulation was more often needed with Macintosh blade (23%) as compared to Miller blade (10%). Benumof and Cooper[6] demonstrated that external laryngeal manipulation improved glottic visualization.
The difference in glottic visualisation can also be explained by the mechanics of laryngoscopy with different types of blades. With the Macintosh blade, the curvature of the blade acts as a visual “hill;” interrupting the line of sight, called the “Crest of the Hill” effect.[7] Whereas with the Miller or any other straight blade, the volume of tissue required to be displaced to obtain the view is lower. While using Macintosh blade to achieve the same glottic view as with a straight blade, the tongue must be displaced more into the submandibular space. With Macintosh blade, the oral axis makes an angle with the laryngeal axis, masking the glottis as it is covered by the epiglottis and this interferes with glottic view. When the McCoy blade is used, the epiglottis is lifted out of the way improving glottic exposure. Thus, the force required is reduced as the tongue only needs to be displaced laterally. The TrueView® laryngoscope incorporates a prism. Due to this prism, an optical view is offered around the corner, without having to align oral, pharyngeal and laryngeal axes.
Cinefluroscopic studies[8,9] suggest that with the Macintosh blade, the hyoid and vallecula are pushed anteriorly and caudally as compared with the Miller blade. This also explains why the movement of cervical vertebrae is less with the Miller blade. Achen et al.[10] compared laryngeal view obtained by using the Miller blade with paraglossal approach, to that with the Macintosh blade. The Miller blade enabled greater than 25% of the vocal cords to be seen in 95% of the cases, whereas with Macintosh blade this was achievable in only 80% cases. Uchida et al.[11] found that when laryngoscopy was performed with neck in neutral position the grade of glottic view improved with use of McCoy blade from Grade 2 to 3 views obtained with Macintosh blade. In a Japanese study[12] the views obtained with McCoy blade were the best (82 Grade I views) then with Miller blade (72 Grade I views) while Grade I view was obtained in least number of patients (47 Grade I views) with the Macintosh blade. Arino et al.[4] found that laryngoscopic views obtained with Belscope (98/100 Grade I views) and Miller (96/100 Grade I views) blades were similar. The levering tip of the McCoy blade laryngoscopes significantly improved the laryngoscopic view (87/100 Grade I views) as compared to that without the use of the levering tip (69/100 Grade I views). The Macintosh blade fared the worst (72/100 grade views).
Cheung et al.[13] found that the glottic view was significantly better with the Flexiblade, a type of levering laryngoscope blade similar to the McCoy, than the Macintosh laryngoscope. Another study[14] compared Trueview® laryngoscope with Macintosh blade. Trueview® laryngoscope produced better glottic view with less maximum force applied during intubation than when using Macintosh blade. Li et al.[15] found better glottic view with Trueview® laryngoscope than Macintosh blade in patients with Cormack-Lehane grade <1. They suggested that Truview can be used in patients with anticipated difficult intubation. In a study in manikins[16] study Truview® laryngoscope provided a better view of glottis.
In our study, intubation was easier with Trueview® and McCoy blades (93% Grade 1 intubation in each group) and almost as easy as with Macintosh blade. With the Miller blade, Grade 1 ease at intubation was achieved in 57% patients. The difference between McCoy (as wells as Trueview®) and Miller was statistically significant (P=0.01). The difference between Macintosh and Miller did not reach statistical significance, it suggested a trend towards easier intubation with Macintosh (P=0.09), probably reflecting small sample size. In a manikin study[16] 20 anaesthetists (12 trainees and eight consultants) compared the Truphatek Truview EVO2 with a conventional Macintosh size 3 blade. Though glottic view was better, Trueview® did not reduce the intubation time or the ease of tracheal tube placement with respect to conventional Macintosh blade.
Most of our patients were intubated at the first attempt. All (30) patients in Macintosh group were intubated at the first attempt, as compared to Miller blade (26 patients). Seven patients needed two attempts; three each in McCoy and Miller groups and one patient in Trueview® group; while one patient in Miller group needed three attempts.
CONCLUSION
In this prospective randomised controlled study in patients with normal airway, we found that glottis visualisation is best achieved with straight blades such as Miller blade and Trueview® laryngoscope. Tracheal intubation however, is easier with McCoy and Macintosh blades and Trueview® laryngoscope.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Cheney FW, Posner KL, Caplan RA. Adverse respiratory events infrequently leading to malpractice suits. A closed claims analysis. Anesthesiology. 1991;75:932–9. doi: 10.1097/00000542-199112000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 3.Levitan RM, Kinkle WC, Levin WJ, Everett WW. Laryngeal view during laryngoscopy: A randomized trial comparing cricoid pressure, backward-upward-rightward pressure, and bimanual laryngoscopy. Ann Emerg Med. 2006;47:548–55. doi: 10.1016/j.annemergmed.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 4.Arino JJ, Velasco JM, Gasco C, Lopez-Timoneda F. Straight blades improve visualization of the larynx while curved blades increase ease of intubation: A comparison of the Macintosh, Miller, McCoy, Belscope and Lee-Fiberview blades. Can J Anaesth. 2003;50:501–6. doi: 10.1007/BF03021064. [DOI] [PubMed] [Google Scholar]
- 5.Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 6.Benumof JL, Cooper SD. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J Clin Anesth. 1996;8:136–40. doi: 10.1016/0952-8180(95)00198-0. [DOI] [PubMed] [Google Scholar]
- 7.Racz GB. Improved vision modification of the Macintosh laryngoscope. Anaesthesia. 1984;39:1249–50. doi: 10.1111/j.1365-2044.1984.tb06446.x. [DOI] [PubMed] [Google Scholar]
- 8.LeGrand SA, Hindman BJ, Dexter F, Weeks JB, Todd MM. Craniocervical motion during direct laryngoscopy and orotracheal intubation with the Macintosh and Miller blades: An in vivo cinefluoroscopic study. Anesthesiology. 2007;107:884–91. doi: 10.1097/01.anes.0000291461.62404.46. [DOI] [PubMed] [Google Scholar]
- 9.Watts AD, Gelb AW, Bach DB, Pelz DM. Comparison of the Bullard and Macintosh laryngoscopes for endotracheal intubation of patients with a potential cervical spine injury. Anesthesiology. 1997;87:1335–42. doi: 10.1097/00000542-199712000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Achen B, Terblanche OC, Finucane BT. View of the larynx obtained using the Miller blade and paraglossal approach, compared to that with the Macintosh blade. Anaesth Intensive Care. 2008;36:717–21. doi: 10.1177/0310057X0803600515. [DOI] [PubMed] [Google Scholar]
- 11.Uchida T, Hikawa Y, Saito Y, Yasuda K. The McCoy levering laryngoscope in patients with limited neck extension. Can J Anaesth. 1997;44:674–6. doi: 10.1007/BF03015455. [DOI] [PubMed] [Google Scholar]
- 12.Bito H, Nishiyama T, Higarhizawa T, Sakai T, Konishi A. Determination of the distance between the upper incisors and the laryngoscope blade during laryngoscopy: Comparisons of the McCoy, the Macintosh, the Miller, and the Belscope blades. Masui. 1998;47:1257–61. [PubMed] [Google Scholar]
- 13.Cheung RW, Irwin MG, Law BC, Chan CK. A clinical comparison of the Flexiblade and Macintosh laryngoscopes for laryngeal exposure in anesthetized adults. Anesth Analg. 2006;102:626–30. doi: 10.1213/01.ane.0000185035.89265.3c. [DOI] [PubMed] [Google Scholar]
- 14.Barak M, Philipchuck P, Abecassis P, Katz Y. A comparison of the Truview blade with the Macintosh blade in adult patients. Anaesthesia. 2007;62:827–31. doi: 10.1111/j.1365-2044.2007.05143.x. [DOI] [PubMed] [Google Scholar]
- 15.Li JB, Xiong YC, Wang XL, Fan XH, Li Y, Xu H, et al. An evaluation of the TruView EVO2 laryngoscope. Anaesthesia. 2007;62:940–3. doi: 10.1111/j.1365-2044.2007.05182.x. [DOI] [PubMed] [Google Scholar]
- 16.Miceli L, Cecconi M, Tripi G, Zauli M, Della Rocca G. Evaluation of new laryngoscope blade for tracheal intubation, Truview EVO2: A manikin study. Eur J Anaesthesiol. 2008;25:446–9. doi: 10.1017/S0265021508003657. [DOI] [PubMed] [Google Scholar]


