Abstract
Background:
Different additives have been used to prolong brachial plexus block. We performed a prospective, randomised, double-blind study to evaluate the effect of dexamethasone added to lidocaine on the onset and duration of supraclavicular brachial plexus block as this is the most common type of brachial block performed in our institute.
Methods:
Sixty American Society of Anaesthesiologist's physical status I and II patients undergoing elective hand, forearm and elbow surgery under brachial plexus block were randomly allocated to receive either 1.5% lidocaine (7 mg/kg) with adrenaline (1:200,000) and 2 ml of normal saline (group C, n=30) or 1.5% lidocaine (7 mg/kg) with adrenaline (1:200,000) and 2 ml of dexamethasone (8 mg) (group D, n=30). The block was performed using a nerve stimulator. Onset and duration of sensory and motor blockade were assessed. The sensory and motor blockade of radial, median, ulnar and musculocutaneous nerves were evaluated and recorded at 5, 10, 20, 120 min, and at every 30 min thereafter.
Results:
Two patients were excluded from the study because of block failure. The onset of sensory and motor blockade (13.4±2.8 vs. 16.0±2.3 min and 16.0±2.7 vs. 18.7±2.8 min, respectively) were significantly more rapid in the dexamethasone group than in the control group (P=0.001). The duration of sensory and motor blockade (326±58.6 vs. 159±20.1 and 290.6±52.7 vs. 135.5±20.3 min, respectively) were significantly longer in the dexamethasone group than in the control group (P=0.001).
Conclusion:
Addition of dexamethasone to 1.5% lidocaine with adrenaline in supraclavicular brachial plexus block speeds the onset and prolongs the duration of sensory and motor blockade.
Keywords: Adrenaline, brachial plexus block, dexamethasone, lidocaine, supraclavicular block
INTRODUCTION
Prolonging the duration of sensory and motor blockade of regional anaesthetic techniques is often desirable. This provides adequate anaesthesia for prolonged surgeries and produces pain relief in the immediate postoperative period. Various adjuncts have been used to prolong brachial block and corticosteroids have been studied recently as adjuncts to local anaesthetics in regional block. Dexamethasone in bupivacaine microspheres has been shown to prolong peripheral nerve block in animals.[1,2,3] Dexamethasone in microspheres also prolongs local analgesia on subcutaneous injection and in intercostal nerve block.[4,5] In addition, dexamethasone has been shown to prolong the duration of axillary brachial block.[6] Since supraclavicular block is the most common type of brachial block performed in our institute, we sought to evaluate the effect of dexamethasone in this block. A previous study evaluated the effect of dexamethasone added to a mixture of lidocaine with adrenaline and bupivacaine in supraclavicular brachial block.[7] Since bupivacaine itself is long acting, doubts existed whether dexamethasone would prolong the actions of shorter-acting local anaesthetics.
The aim of our study was to evaluate the effect of dexamethasone 8 mg added to 7 mg/kg of lidocaine (1.5%) with adrenaline (1:200,000) on the onset time and duration of supraclavicular brachial plexus block in patients undergoing hand, forearm and elbow surgeries.
METHODS
Hospital Ethics Committee approval and written informed consent from patients were obtained. American Society of Anaesthesiologists (ASA) class I and II patients aged 20-70 years undergoing elective surgery of hand, forearm or elbow were included in the study. Patients with uncontrolled diabetes mellitus or hypertension, peripheral neuropathy, hepatic or renal disease, pregnant patients, patients with acid peptic disease and known allergy or hypersensitivity to local anaesthetic drugs were excluded from the study. Patients were fasted for 6 h before the surgery and premedicated with oral diazepam 0.15 mg/kg on the night before and on the morning of surgery.
Randomisation was done by a computer-generated table of random numbers. Patients were randomly allocated to receive either freshly prepared 1.5% lidocaine (7 mg/kg) with adrenaline (1:200,000) and 2 ml of normal saline (group C, n=30) or freshly prepared 1.5% lidocaine (7 mg/kg) with adrenaline (1:200,000) and 8 mg dexamethasone (2 ml) (group D, n=30). An anaesthesiologist not involved in performance of brachial plexus block or collection of data prepared all the local anaesthetic mixtures and adjuvant drugs and labelled them using the computer-generated random number.
In the operation theatre, intravenous (IV) access was secured with 18-G cannula on the contralateral hand and monitors were connected (pulse oximetry, electrocardiography and noninvasive arterial blood pressure monitoring). Oxygen was administered via a Hudson mask at a rate of 5 l/min. Supraclavicular brachial plexus block was performed under aseptic precautions with the patient in supine position without a pillow, and head turned slightly to the opposite side. The arm to be anaesthetised was adducted and the hand extended along the side towards the ipsilateral knee as far as possible. We used a nerve stimulator (Innervator®, Fisher and Paykel Electronics Ltd, Auckland, New Zealand) with a 22-G, 5-cm insulated needle for precise localisation of the brachial plexus. A skin wheal was raised in the interscalene groove 1.5-2 cm posterior to the midpoint of clavicle. The subclavian artery was usually palpable at this site. The nerve stimulator frequency was set at 1 Hz and the intensity of the stimulating current was initially set to deliver 2 mA. The insulated needle was inserted through the skin wheal in a posterior, caudal and medial direction until a distal motor response was elicited. The position of the needle was considered acceptable when an output current ≤0.6 mA still elicited a distal motor response. At this point, the local anaesthetic mixture, 2 ml less than the total volume prepared, was injected in increments after negative aspiration for blood and air. The remaining 2 ml was diluted to 4 ml and used for intercostobrachial nerve block to prevent tourniquet pain.
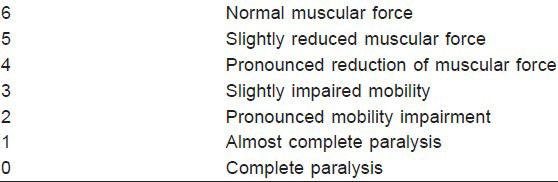
Sensory and motor blockade of radial, median, musculocutaneous and ulnar nerves were recorded at 5, 10, 20 and 120 min, and every 30 min thereafter. Sensory block of each nerve was assessed by pinprick and compared with the same stimulation on the opposite hand. Sensory block of each nerve was rated by the patient on a verbal analogue scale (VAS) from 100 (normal sensation) to 0 (no sensation). Motor block of each nerve was evaluated by thumb abduction (radial nerve), thumb adduction (ulnar nerve), thumb opposition (median nerve), and pronation of forearm and flexion of elbow in supination (musculocutaneous nerve). Motor block of each nerve was quantified using a modification of the Lovett rating scale [Table 1].
Table 1.
Modified Lovett rating scale for quantification of muscle force
The onset time of sensory and motor blockade was defined as the time between the last brachial injection of local anaesthetic to the total abolition of pinprick response and complete paralysis, respectively, in all nerve distributions. The duration of sensory block was defined as the time interval between brachial injection of local anaesthetic and the first postoperative pain. The duration of motor block was defined as the time interval between the local anaesthetic administration and complete recovery of motor function in all nerve distributions. The patients and the anaesthesiologists who performed the block and who collected patient data were blinded as to the mixture used or group allocation.
Heart rate, arterial pressure, respiratory rate and oxygen saturation were recorded just before the block and at regular intervals thereafter. Patients were observed for any side effects and complications. When the patient first complained of pain after operation, intramuscular (IM) injection diclofenac sodium 1.5 mg/kg was given. In addition, patients received injection morphine 2 mg IV boluses every 10 min until verbal analogue pain scores reduced to less than 30.
Sample size calculation was done based on a previous study in which the onset of sensory blockade in control group and study group were 11±4 and 14±5 min, respectively. It was estimated that a minimum of 24 patients in each group would be required to have a 90% power of detecting a 3-min difference in onset time with 95% confidence interval. Statistical analysis was performed with SPSS for Windows (SPSS Inc., Chicago, IL, USA), version 16.0. For analysis of demographic data and comparison of groups, χ2, unpaired Student's t-test and Mann–Whitney U-test were performed. P<0.05 were considered to be significant.
RESULTS
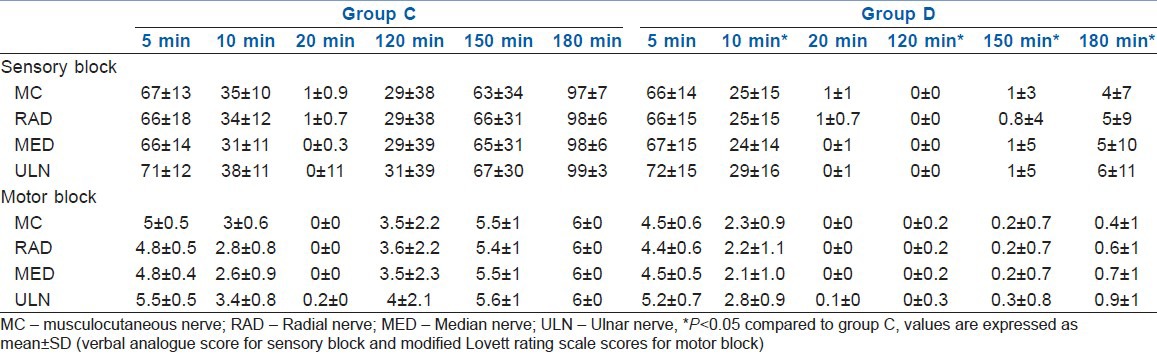
Two patients were excluded from the study because of unsuccessful blockade [Table 2]. The groups of patients were comparable with respect to patient age, weight, gender ratio and duration of surgery. The onset of sensory and motor blockade were significantly more rapid in the dexamethasone group (13.4±2.8 vs. 16±2.3 min and 16.0±2.7 vs. 18.7±2.8 min, respectively) than in the control group (P=0.001). The duration of sensory and motor blockade were also significantly longer in the dexamethasone group (326.0±58.6 vs. 159.0±20.1 min and 290.6±52.7 vs. 135.5±20.3 min, respectively) than in the control group (P=0.001). The VAS scores and motor block scores of all four nerves at 10, 120, 150 and 180 min were significantly lower in the dexamethasone group than in the control group (P<0.05) [Table 3]. In addition, motor block scores of musculocutaneous and radial nerves were significantly lower in the dexamethasone group at 5 min. There were no side effects or complications observed in either group. Intraoperative and postoperative patient vital parameters such as heart rate, blood pressure and oxygen saturation were stable.
Table 2.
Patient characteristics
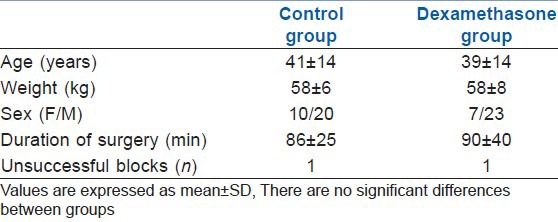
Table 3.
Sensory and motor blockade of supraclavicular brachial plexus block
DISCUSSION
Our study showed that addition of 8 mg of dexamethasone to 1.5% lidocaine with adrenaline 1:200,000 for supraclavicular brachial plexus block results in a significantly shorter onset time and a significantly prolonged duration of sensory and motor blockade. The VAS scores and motor block scores as assessed by Lovett rating scale[8] were not significantly different between groups at 20 min probably because once complete block was established, there was no difference in the intensity of block.
The dose of lidocaine used in our study is the maximum recommended dose of lidocaine in adrenaline containing solutions.[9] The duration of sensory and motor block in the control group (159±20 min and 135±20 min, respectively) was moderately longer compared to previous study that also used 1.5% lidocaine (98±33 min and 130±31 min, respectively)[6] probably because we used lidocaine with adrenaline 1:200,000.
The 3.3% incidence of failure of block in our study is much lower than other reports of failure in supraclavicular block using nerve stimulator.[10,11]
In previous studies, dexamethasone prolonged the duration of sensory and motor blockade of brachial plexus block.[6,12] However, our study showed that dexamethasone also shortens the onset time of sensory and motor block, which is in contrast to the previous studies in which there was no difference in the onset of sensory and motor block among groups.[6] The reason for shortened onset time is obscure. This needs to be re-examined in subsequent studies.
Other studies have demonstrated that addition of dexamethasone to bupivacaine microspheres prolongs the duration of blockade of the peripheral nerves.[1,2,3] Dexamethasone in bupivacaine microspheres also prolonged local analgesia when injected subcutaneously[4] and in intercostal nerve blockade.[5] Dexamethasone has also been found to enhance the analgesia of intravenous regional anaesthesia (IVRA) and reduce postoperative analgesic requirement.[13] Also, addition of other steroids like methylprednisolone to local anaesthetics in axillary block has been shown to significantly prolong the duration of analgesia and motor block.[14]
The mechanism of dexamethasone-induced prolongation of peripheral nerve blockade is not well understood. Dexamethasone alone does not exhibit analgesic effects when incorporated into microspheres.[2] It is commonly attributed to its anti-inflammatory action. This is supported by the finding that the degree of block prolongation had the same rank order as the relative anti-inflammatory potencies of glucocorticoids and is completely reversed by administration of a specific glucocorticoid receptor antagonist.[1,2] These effects are, therefore, mediated via the classic glucocorticoid receptor and are local effects rather than systemic since incorporation of dexamethasone has not been shown to alter kinetics of bupivacaine release from microcapsules.[2] Action on glucocorticoid receptor is proposed to alter the functioning of ion channels or produce local acidosis in nerve cell, thereby reducing the concentration of local anaesthetic required to produce conduction failure or trapping the highly ionised bupivacaine molecule into the neuronal cell.[1,5] Both these events would produce an extended action of local anaesthetics. Dexamethasone has been shown to inhibit nitric oxide synthase,[15] a mediator of local anaesthetic tachyphylaxis.
Although the mechanism of action of glucocorticoids in backache (as epidural steroid injection) and facet syndrome may be inhibition of phospholipase A2, it appears that this may not be the mechanism in peripheral nerve blockade given the rapid onset of action of dexamethasone in such blocks. Corticosteroids reduce conduction in nociceptive C fibres in an animal model.[16] It has been shown that onset of this effect was instantaneous and persisted for the duration of the steroid application.
There is concern that benzyl alcohol in commercial preparations of methylprednisolone could have contributed to the prolongation of axillary brachial plexus block.[4,17] Alcohol is frequently used for neurolytic nerve blocks and is toxic to nerves. In our study, the dexamethasone preparation did not contain benzyl alcohol.
As dexamethasone has been shown to prolong analgesia and motor block in previous studies where adrenaline was not part of the anaesthetic mixture, it appears that block prolongation was indeed due to dexamethasone. We used adrenaline with lidocaine because we targeted surgeries that would take about 90-100 min. With respect to the onset of block, further studies are required to test this without adrenaline in supraclavicular block.
CONCLUSION
In conclusion, addition of dexamethasone (8 mg) to lidocaine 1.5% with adrenaline in supraclavicular brachial plexus block results in a faster onset and prolonged duration of sensory and motor blockade. Further studies are required to elucidate the precise mechanism of action of dexamethasone.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Curley J, Castillo J, Hotz J, Uezono M, Hernandez S, Lim J, et al. Prolonged regional nerve blockade: Injectable biodegradable bupivacaine/polyester microspheres. Anesthesiology. 1996;84:1401–10. doi: 10.1097/00000542-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Castillo J, Curley J, Hotz J, Uezono M, Tigner J, Chasin M, et al. Glucocorticoids prolong rat sciatic nerve blockade in vivo from bupivacaine microspheres. Anesthesiology. 1996;85:1157–66. doi: 10.1097/00000542-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Drager C, Benziger D, Gao F, Berde C. Prolonged intercostal nerve blockade in sheep using controlled-release of bupivacaine and dexamethasone from polymer microspheres. Anesthesiology. 1998;89:969–79. doi: 10.1097/00000542-199810000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Hotte K, Werner MU, Lacouture PG, Kehlet H. Dexamethasone prolongs local analgesia after subcutaneous infiltration of bupivacaine microcapsules in human volunteers. Anesthesiology. 2002;96:1331–5. doi: 10.1097/00000542-200206000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Kopacz DJ, Lacouture PG, Wu D, Nandy P, Swanton R, Landau C. The dose response and effects of dexamethasone on bupivacaine microcapsules for intercostal blockade (T9 to T11) in healthy volunteers. Anesth Analg. 2003;96:576–82. doi: 10.1097/00000539-200302000-00050. [DOI] [PubMed] [Google Scholar]
- 6.Movofegh A, Razazian M, Hajimaohamadi F, Meysamic A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–7. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 7.Golwala MP, Swadia VN, Dhimar AA, Sridhar NV. Pain relief by dexamethasone as an adjunct to local anaesthetics in supraclavicular brachial plexus block. J Anaesthesiol Clin Pharmacol. 2009;25:285–8. [Google Scholar]
- 8.Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78:507–13. doi: 10.1213/00000539-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Strichartz GR, Berde CB. Local anesthetics. In: Miller RD, editor. Miller's anesthesia. 6th ed. Philadelphia: Elsevier Churchill Livingstone; 2005. pp. 573–603. [Google Scholar]
- 10.Williams SR, Chouinard P, Arcand G, Harris P, Ruel M, Boudreault D, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg. 2003;97:1518–23. doi: 10.1213/01.ANE.0000086730.09173.CA. [DOI] [PubMed] [Google Scholar]
- 11.Arcand G, William SR, Chouinard P, Boudreault D, Harris P, Ruel M, et al. Ultrasound-guided infraclavicular versus supraclavicular block. Anesth Analg. 2005;101:886–90. doi: 10.1213/01.ANE.0000159168.69934.CC. [DOI] [PubMed] [Google Scholar]
- 12.Iyer CP, Ross L, Joshi G, Robertson B. Efficacy of ropivacaine with or without dexamethasone for enhancing extremity nerve blocks. Reg Anesth Pain Med. 2005;30:A42. [Google Scholar]
- 13.Bigat Z, Boztug N, Hadimioglu N, Cete N, Coskunfirat N, Ertok E. Does dexamethasone improve the quality of intravenous regional anesthesia and analgesia? A randomized, controlled clinical study. Anesth Analg. 2006;102:605–9. doi: 10.1213/01.ane.0000194944.54073.dd. [DOI] [PubMed] [Google Scholar]
- 14.Stan T, Goodman EJ, Bravo-Fernandez C, Holbrook CR. Adding methylprednisolone to local anesthetic increases duration of axillary block. Reg Anesth Pain Med. 2004;29:380–1. doi: 10.1016/j.rapm.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Salvemini D, Settle SL, Masferrer JL, Seibert K, Currie MG, Needleman P. Regulation of prostaglandin production by nitric oxide: An in vivo analysis. Br J Pharmacol. 1995;114:1171–8. doi: 10.1111/j.1476-5381.1995.tb13330.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johansson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibers. Acta Anaesthesiol Scand. 1990;34:335–8. doi: 10.1111/j.1399-6576.1990.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 17.Lipman ZJ, Isaacson SA. Potentially concerning reason why adding methylprednisolone to local anesthetic may increase the duration of axillary block. Reg Anesth Pain Med. 2005;30:114–5. doi: 10.1016/j.rapm.2004.09.001. [DOI] [PubMed] [Google Scholar]


