Abstract
Background:
Studying drug use pattern among medical practitioners is of vital importance in the present scenario where irrational drug use and development of drug resistance is becoming rampant.
Objective:
To assess, the pattern of prescribing practices among the general practitioners in a defined rural and urban area of Tamil Nadu.
Materials and Methods:
A community based descriptive study was conducted to collect 600 prescriptions from the catchment areas of rural and urban health training centers of a medical college using prescribing indicators as per the WHO “How to investigate drug use in health facilities” tool.
Results:
This prescription study revealed that multivitamins (19.5%), antibiotics (19.3%), drugs for gastro-intestinal tract (GIT) (18%), analgesic non-steroidal anti-inflammatory drugs/ (NSAID's) (15.1%), and antihistaminic (12.5%) were prescribed frequently. Among the antibiotics, amoxicillin (49.2%) was the most commonly prescribed followed by gentamicin (31.7%). Percentage of prescriptions with an antibiotic was 55% and nearly 62% of the practitioners prescribed drugs by their generic names. As a practice of poly-pharmacy, it was observed that the average number of drugs prescribed in urban and rural area was nearly 5 and 4, respectively. Nearly 80% of the urban and rural practitioners were prescribing at least one injection. Study of the quality of prescriptions revealed that there was poor legibility, high usage of abbreviations, inadequate details of the drugs, and absence of signature by practitioners in the prescriptions.
Conclusion:
This study clearly highlights the practice of poly-pharmacy, low usage of generic drugs, injudicious usage of antibiotics and injections and low usage of drugs prescribed from essential drugs list.
KEY WORDS: Drug prescriptions, essential drugs, general practitioners, inappropriate prescribing, primary care physicians
Introduction
An efficient health-care delivery system is a pre-requisite to achieve better health for all in the 21st century. Appropriate treatment of commonly occurring diseases and injuries and provision of essential drugs are the two vital components of primary health-care concept as per the Alma-Ata declaration of 1978.[1] Essential drugs are those drugs that satisfy the health-care needs of the majority of the population; they should therefore, be available at all times in adequate amounts and in appropriate dosage forms, at a price the community can afford.[2] These drugs are critically required for the management of 90% of commonly occurring medical conditions specific to the area and must meet high standards of quality, safety, and efficacy at a low-cost. It is found that there are more than 60,000 drug formulations available in the Indian drug market.[3] However, 90% of the commonly prevalent diseases can be treated with about 10% of drugs available in the market. There are medical, economic, social, and administrative advantages in popularizing the concept of essential drugs.[4]
Rational use of drugs means reasonable or sensible use of drugs and is defined as appropriate use of drugs, when it is really needed, in appropriate strength, dosage, and duration, which will have a beneficial effect on the individual.[5] Requirements for rational use of drugs will be fulfilled, if the process of prescribing is appropriately, followed. This includes six steps which are, defining the patients problems (diagnosis), defining effective and safe treatment (drugs and non-drug options), selecting appropriate drugs, dosage, and duration, writing a good prescription, giving patients adequate information, and planning to evaluate treatment responses.[6]
Bad prescribing practices leads to ineffective and unsafe treatment, exacerbation or prolongation of illness, distress, and harm to the patient at a higher cost. World-wide more than 50% of all medicines are prescribed, dispensed, or sold inappropriately, while 50% of patients fail to take them correctly. It was seen that the following were the common types of irrational medicine usage such as poly-pharmacy, inappropriate use of antimicrobials, inadequate dosage, over use of injections, failure to prescribe in accordance with clinical guidelines, and self-medications.[5] Irrational medicine use may result in serious morbidity and mortality as well as additional economic burden and leads to reduction in the quality of drug therapy, wastage of resources, increased treatment cost, increased risk for adverse drug reactions, and emergence of drug resistance.[7]
Two of the most commonly seen irrational use of medicines is excessive use of antibiotics and injections. The development of resistant microbes will remain as a problem whenever antimicrobials are used. The misuse and overuse of antimicrobials have exacerbated the problem by adding selection pressures that favor resistance.[8] Antimicrobial resistance is not only a problem for the individual patient, it also reduces the effectiveness of established treatment and poses a major threat to public health by increasing the complexity and cost of treatment and reducing the probability of a successful outcome.[9] Regarding the over use of injections, it is estimated that up to 90% of injections are unnecessary, because alternative, safer routes of administration are available. Excessive use of injections, particularly prevalent in low-income countries, is a widespread hazard to health in countries where injection safety cannot be guaranteed.[10]
Studying drug use pattern among general practitioners (GPs) is of vital importance in the present scenario where irrational drug use and development of drug resistance is becoming rampant. Hence, it has been decided to conduct a study about the prescribing practices among the GPs in a selected urban and rural area of South India using WHO standardized tool.
Materials and Methods
This community based descriptive study was conducted in a randomly selected urban and rural area of Tamil Nadu. The study area consists of urban population of 15,922 distributed in three administrative wards and a rural population of 11,506 distributed in nine villages. A stratified random sampling method was used in the study. Ethical approval was obtained from the Institutional Ethical Committee before starting the study. It was decided to study 300 prescriptions from urban and 300 from rural area. Data were collected by house hold survey using the basic parameters stipulated in the WHO “How to investigate drug use in health facilities” tool.[11] The investigators enquired about the history of visiting a health facility in the catchment area by any member of the family in the past 6 months irrespective of the type of facility (government or private). The available prescription at that time of visit was studied and relevant data was collected using the standardized WHO data collection forms designed for “How to investigate drug use in health facilities.” The study team compiled information on five prescribing indicators and appropriate descriptive tables were generated to demonstrate the findings.
Results
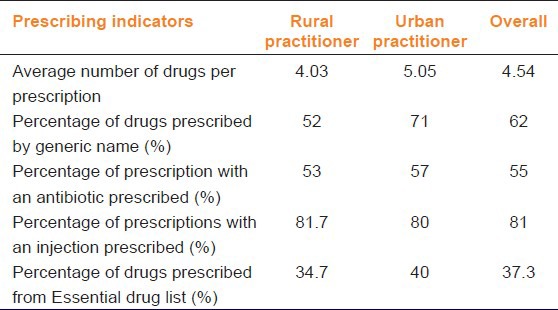
Following observations were made from the study about the drug use patterns based on the prescribing indicators. The act of poly-pharmacy, i.e., prescribing more than or equal to three drugs per prescription was found among urban and rural area GPs. In an average, the number of drugs prescribed by urban and rural area GPs was nearly 5 and 4, respectively. Nearly 71% of urban GPs were prescribing the drugs by generic name, but only 52% of the rural GPs did that. Nearly 80% of the urban and rural GPs were prescribing at least one injection and overall nearly 50% of them were prescribing at least one antibiotic per prescription [Table 1]. It is also observed that 34.7% of rural and 40% of the urban GPs prescribed drugs from the essential drug list, knowingly, or unknowingly.
Table 1.
Distribution of the core drug use indicators based on the prescribing practices
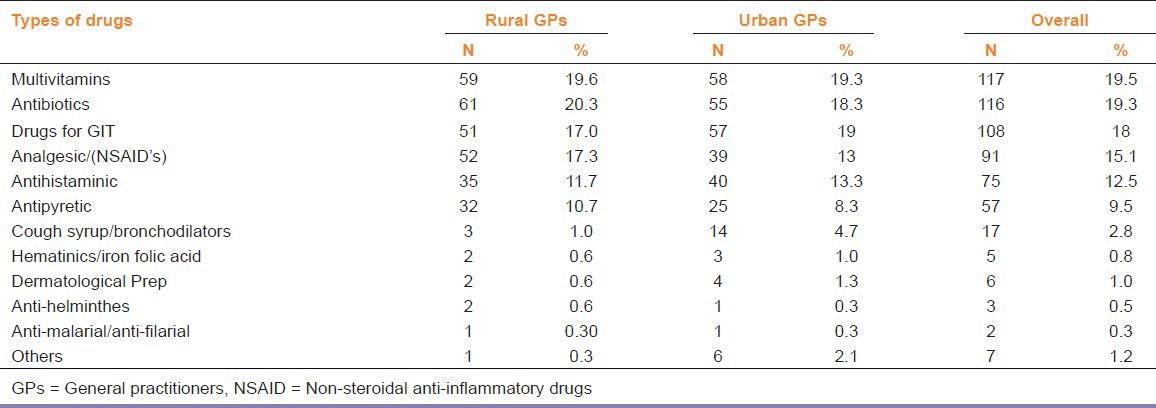
Out of the 600 prescriptions, it was observed that multivitamins were the most commonly prescribed drug followed by antibiotics, drugs used for gastro-intestinal tract diseases, analgesics, antihistamines, and antipyretics [Table 2]. The cough syrup, hematinics, dermatological, anti-helminthic, and anti-malarial drugs were the least prescribed in both the areas during the study period.
Table 2.
Distribution of commonly prescribed drugs by the practitioners
Among the antibiotics prescribed [Table 3], capsule amoxicillin (49.2%) and injection gentamicin (31.7%) were the most commonly prescribed in both urban and rural areas and co-trimoxazole was the least prescribed antibiotic (11.5%). Prescribing injections was a common practice in both areas. It was observed that gentamicin (31.7%), which is an antibiotic and diclofenac sodium (32.5%), which is an analgesic were the most commonly prescribed injections by the GPs [Table 3]. Injection vitamin B12 and paracetamol were also frequently prescribed while ranitidine and chlorpheniramine maleate were the least prescribed injections.
Table 3.
Distribution of commonly prescribed antibiotics and injections by the practitioners
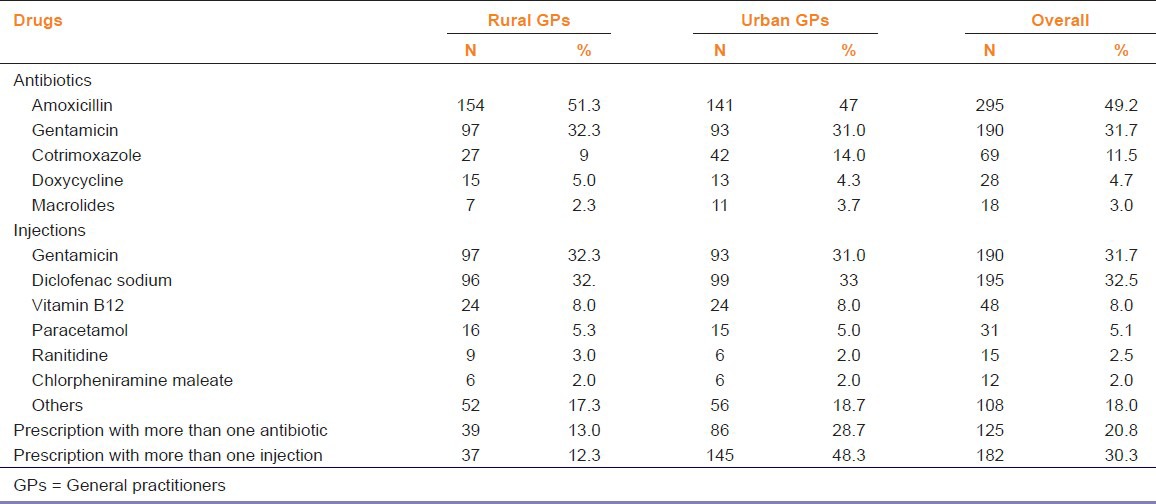
The habit of prescribing more than one antibiotic was seen more among urban GPs (28.7%) when compared to rural GPs (13%). It was also observed that nearly 48.3% of the urban GPs and 12.3% of the rural GPs were prescribing more than one injection per patient [Table 3].
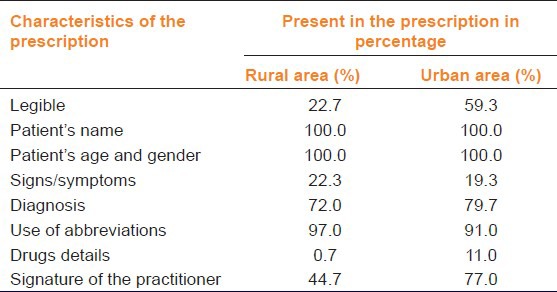
The quality of prescriptions was assessed on the basis of certain characteristics and its outcome was assessed [Table 4]. It was observed that all the GPs entered details of the patient such as name, age, and sex in all prescriptions. Urban GPs (59.3%) wrote more legible prescriptions when compared to the rural GPs (22.7%). Only 72% of the urban and 79.7% of rural GPs wrote the diagnosis in their prescription. Abbreviations were more often used by both urban and rural GPs but the practice was found to be more among rural GPs. Nearly half of the rural GPs and 3/4th of the urban GPs have signed their prescriptions. Details regarding the drug strength and dosage schedule were present only in 0.7% of the rural and 11% of the urban GPs prescriptions.
Table 4.
Characteristics of the prescriptions by rural and urban practitioners
Discussion
Many studies were carried out on the drug use practices in developed and developing countries, using the WHO and International Network for the Rational Use of Drugs (INRUD) standard set of drug indicators to measure the drug use practices at the country level as well as at various regional and individual facilities. These drug use indicators were tested in developing countries by Hogerzeil et al.[12] under action program on essential drugs, WHO and the recommended methods for data collection were presented to improve drug use and prescribing behavior. The main objective of the present study was to find out the current drug use practices in terms of what was prescribed, to the patient during each visit to a health facility among the urban and rural GPs.
On observation about the type of drugs prescribed, it was seen that multivitamins and antibiotics were prescribed most frequently by the GPs. Multivitamins were found in nearly 20% of the prescriptions and this practice of prescribing multivitamins may be done for the placebo effect on the illnesses. A prescription survey from Goa revealed that vitamins and tonics, for which there are few specific medical indications, were used in almost half of all prescriptions.[13] The prescription of tonics and vitamins increased from 20% to 52% with the number of drugs per prescription and contributed to poly-pharmacy and increased cost.[14] Nutritional experts have long been able to prove that most individuals on a balanced diet have no need for vitamin supplements. Much of the additional vitamins supplemented are simply excreted through the kidneys, which is an unnecessary load to it.
Prescriptions with more antibiotics show that there may be an injudicious use of antibiotics for common illnesses in the study area. Antibiotics were prescribed in about 55% of the prescription and among which, amoxicillin was the most commonly prescribed antibiotic followed by gentamicin and this practice was found more among urban GPs. This finding is similar to the studies conducted by Moghadamnia et al.[15] and Hasan[16] where penicillin group of drugs (mostly amoxicillin) were the most commonly prescribed antibiotics followed by sulfonamides. Moghadamnia et al.[15] and Bhartiy et al.[7] mentioned that the most commonly prescribed drugs were antibiotics and NSAIDs. A study carried out in primary and secondary health-care facilities of public/government and private settings at four sites in India revealed that the overall antimicrobial prescription rate was 69.4% and wide variation was observed. Physicians practicing in rural and public/government settings prescribed antimicrobials more frequently than those in urban and private settings. Two-third of all antimicrobials prescribed were penicillin and co-trimoxazole, and more than 40% of prescriptions from private sector were quinolones and cephalosporins.[17] Another study conducted in a small Indian hospital, showed that more than 80% of all admitted patients received antimicrobial drugs such as penicillin, gentamicin, co-trimoxazole, ciprofloxacin, and metronidazole, and all antimicrobial drugs were given empirically with no confirmation of the infective agent.[18]
The injudicious usage of antibiotics may lead to severe antimicrobial resistance, which has been highlighted by World Health Day 2011 theme “Antimicrobial resistance: No action today no cure tomorrow”.[19] There are definite policies/guidelines for appropriate use of antimicrobials at national level in specific national health programs being run in the country, for example, Revised National Tuberculosis Control Programme (RNTCP), National AIDS control programme, etc. For other diseases of public health importance such as enteric fever, diarrheal disease, and respiratory infections the individual hospitals are following their own antimicrobial policies and hospital infection control guidelines. To monitor antimicrobial resistance it is necessary to have regulations for use and misuse of antibiotics in the country, creation of national surveillance system for antibiotic resistance, mechanism of monitoring prescription audits, regulatory provision for monitoring use of antibiotics in human, veterinary and industrial sectors, and identification of specific intervention measures for rational use of antibiotics.[20]
Prescription of more injections has been reported from various studies in developing and developed countries. This study recorded that 81% of the prescriptions were found to be with an injection. Inappropriate drug use studies in Tanzania showed that over 70% of patients attending out-patient clinics at private dispensaries received at least one injection per consultation, a value higher than WHO recommended target of 10%. In a Chinese study, the proportion of prescriptions with an injection was 22.63%,[21] and about 18% of prescriptions were having injections in the study conducted in Lao PDR, Japan.[22]
In a study in Maharashtra, about 25% of the prescriptions contained at least one injection.[23] Injections were given in 77.7% of the studied illness cases in the health facilities in six divisions of Bangladesh.[24] Prescribing more injections per prescription are of concern, considering the likelihood of adverse effects of possible use of unsafe syringes to transmit HIV, hepatitis B and C, and added economic impact on the patient and the health-care system.[25] Furthermore, this generates more biomedical waste in that area.
Based on the WHO prescribing indicators, It was seen that the average number of drugs per prescription was 4.5 (4.03 in the rural area and 5.05 in the urban area). Prescriptions containing five and above drugs were seem to be nearly half of the prescriptions, which shows that there is a practice of poly-pharmacy among the GPs in the study area, which is found to be similar with many studies conducted in and around India with the similar settings.[15,26,27] Nearly one-third of the GPs never prescribed drugs with their generic name ,which may be due to lack of awareness and absence of proper regulatory mechanism over them in prescribing drugs. This finding is found to be similar with the studies conducted by Bhartiy et al.[7] as well as other studies conducted in Manipal,[28] Uzbekistan,[10] and Jordan.[29]
The study of the quality of the prescriptions revealed that there is poor legibility of the prescription, high usage of abbreviations, inadequate details of the illness and the drugs prescribed without mentioning the strength and frequency of administration and without the signature of the doctor in it. This shows that there is a lacuna in the quality of prescriptions given and also shows the lack of enforcement by professional bodies over the GPs on good prescribing practices. Sufficient evidence is now available to persuade policy-makers and health professionals that it is vital to enforce rational drug use among the GPs. If such effective strategies are followed, the quality of health-care can be improved and drug expenditures can be reduced.[30]
Thus, the practice of poly-pharmacy, low usage of generic drugs, injudicious usage of antibiotics, and injections in the prescriptions were prevalent in the study area. The study outcome reflects the practice of irrational prescribing among the GPs in both urban and rural area. Though, short-term outcome of such irrational prescriptions is overlooked, the long-term effect can lead to serious public health problems like antimicrobial drug resistance. The study of the quality of the prescription revealed unsatisfactory results. The GPs are legally bound to give a proper legible prescription, which is intended to serve as a guide for the dispensers and patients for effective use of medicines.
As this being a descriptive study, identification of the factors related to the prescription was not carried out by the investigators. Perhaps studying the prescriptions along with the knowledge and attitude of the medical practitioners might be more ideal in getting the information regarding the rational prescribing practices in this kind of setting. Though the data included both the prescriptions of acute and chronic illnesses, distribution of them in the usage of drugs was not clearly identified by the investigators. With the above limitations, prevalence of irrational prescription of drugs was well identified and the pattern of drug use.
Conclusions
As this study focuses on the prescribing practice among the practitioners and their pattern of drug use, certain areas were identified where intervention can be made to improve their practice. As medical professionals are the group of focus here, where the factors related to them influence a large in better clinical decision making. One of it is evidence based rational prescription of drugs. Since, the practice is largely influenced by knowledge and attitude, importance of it has to be emphasized at the earliest. Undergraduate medical education should focus more on good prescribing practices and rational use of drugs, which will have long-term beneficial effects. Involvement of professional associations to encourage their members in helping to make evidence based rational prescription of drugs may improve the attitude of using those in their practice. Legislation of policies on rational prescribing practice by the government and institutions may help the medical practitioners to improve their motivation which influence to bring the attitude to the practice of it. Thus, we conclude revision of clinical policy is a need of the hour to bring the change at all possible levels for long-term and better clinical outcome in the medical practice.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Declaration of Alma-Ata International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978. [Last cited 2011 Aug 26]. Available from: http://www.who.int/hpr/NPH/docs/declaration_almaata.pdf .
- 2.WHO Expert Committee. The use of essential drugs. World Health Organ Tech Rep Ser. 2000;895:1–61. [PubMed] [Google Scholar]
- 3.Gosh AK, De A, Bala NN. Current problems and future aspects of pharmacovigilance in India. Int J Pharm Biol Sci. 2011;2:15–28. [Google Scholar]
- 4.Levy LM. Advantages and disadvantages of an essential drugs programme. Cent Afr J Med. 1996;42:218–9. [PubMed] [Google Scholar]
- 5.Geneva: World Health Organization; 2002. [Last cited 2011 Jun 17]. Promoting rational use of medicines: Core components (WHO policy perspectives on medicines) Available from: http://www.apps.who.int/medicinedocs/pdf/h3011e/h3011e.pdf . [Google Scholar]
- 6.De Vries TP, Henning RH, Hogerzeil HV, Fresle DA. WHO/DAP/94.11. Geneva: World Health Organization; 1994. [Last cited 2011 June 17]. Treating your patients. Guide to Good Prescribing: A Practical Manual; pp. 33–66. Available from: http://www.archives.who.int/prduc2004/rducd/INRUD_2000_CDROM/Manuals/Guide%20to%20Good%20Prescribing.doc . [Google Scholar]
- 7.Bhartiy SS, Shinde M, Nandeshwar S, Tiwari SC. Pattern of prescribing practices in the Madhya Pradesh, India. Kathmandu Univ Med J (KUMJ) 2008;6:55–9. [PubMed] [Google Scholar]
- 8.Sivagnanam G, Thirumalaikolundusubramanian P, Mohanasundaram J, Raaj AA, Namasivayam K, Rajaram S. A survey on current attitude of practicing physicians upon usage of antimicrobial agents in southern part of India. Med Gen Med. 2004;6:1. [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. WHO/EDM/PAR/2004.5. Geneva: World Health Organization; 2004. [Last cited 2012 Apr 24]. Rational use of medicines. The World Medicines Situation (2004) pp. 75–91. Available from: http://www.apps.who.int/medicinedocs/pdf/s6160e/s6160e.pdf . [Google Scholar]
- 10.Pavin M, Nurgozhin T, Hafner G, Yusufy F, Laing R. Prescribing practices of rural primary health care physicians in Uzbekistan. Trop Med Int Health. 2003;8:182–90. doi: 10.1046/j.1365-3156.2003.00992.x. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organiztion. How to investigate drug use in health facilities: Selected drug use indicators. WHO/DAPI 93. 1. 1993a. [Last cited 17 Jun 2011]. Available from: http://www.apps.who.int/medicinedocs/pdf/s2289e/s2289e.pdf .
- 12.Hogerzeil HV, Bimo, Ross-Degnan D, Laing RO, Ofori-Adjei D, Santoso B, et al. Field tests for rational drug use in twelve developing countries. Lancet. 1993;342:1408–10. doi: 10.1016/0140-6736(93)92760-q. [DOI] [PubMed] [Google Scholar]
- 13.Patel V, Vaidya R, Naik D, Borker P. Irrational drug use in India: A prescription survey from Goa. J Postgrad Med. 2005;51:9–12. [PubMed] [Google Scholar]
- 14.Mhetre NA, Bodhankar SL, Pandit VA, Zambare GN. Study of pattern of drug usage in an urban area. Indian J Pharmacol. 2003;35:316–7. [Google Scholar]
- 15.Moghadamnia AA, Mirbolooki MR, Aghili MB. General practitioner prescribing patterns in Babol city, Islamic Republic of Iran. East Mediterr Health J. 2002;8:550–5. [PubMed] [Google Scholar]
- 16.Hasan MY, Das M, Mourad F. Drug utilization and antibiotic use in the primary health care centres in Sharjah. East Mediterr Health J. 1997;3:444–51. [Google Scholar]
- 17.KI S, Chandy SJ, Jeyaseelan L, Kumar R, Suresh S. Antimicrobial prescription patterns for common acute infections in some rural & urban health facilities of India. Indian J Med Res. 2008;128:165–71. [PubMed] [Google Scholar]
- 18.Blomberg M, Jensen MB, Henry A, Singh ST, Banipal RP, da Cunha-Bang C, et al. Antimicrobial drug use in a small Indian community hospital. Trop Doct. 2010;40:194–8. doi: 10.1258/td.2010.090157. [DOI] [PubMed] [Google Scholar]
- 19.Leung E, Weil DE, Raviglione M, Nakatani H World Health Organization World Health Day Antimicrobial Resistance Technical Working Group. The WHO policy package to combat antimicrobial resistance. Bull World Health Organ. 2011;89:390–2. doi: 10.2471/BLT.11.088435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ministry of Health & Family Welfare. National Policy for Containment of Antimicrobial Resistance - India, 2011. [updated 2011]. Available from: http://www.nicd.nic.in/ncdc_new/ab_policy.pdf .
- 21.Jun Z, Linyun L, Che Z, Yuanrong Y, Fengxi G, Heng Z. Analysis of outpatient prescription indicators and trends in Chinese Jingzhou Area between September 1 and 10, 2006-2009. Afr J Pharm Pharmacol. 2011;5:270–5. [Google Scholar]
- 22.Keohavong B, Syhakhang L, Sengaloundeth S, Nishimura A, Ito K. Rational use of drugs: Prescribing and dispensing practices at public health facilities in Lao PDR. Pharmacoepidemiol Drug Saf. 2006;15:344–7. doi: 10.1002/pds.1169. [DOI] [PubMed] [Google Scholar]
- 23.Potharaju HR, Kabra SG. Prescription audit of outpatient attendees of secondary level government hospitals in Maharashtra. Indian J Pharmacol. 2011;43:150–6. doi: 10.4103/0253-7613.77350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chowdhury AK, Roy T, Faroque AB, Bachar SC, Asaduzzaman M, Nasrin N, et al. A comprehensive situation assessment of injection practices in primary health care hospitals in Bangladesh. BMC Public Health. 2011;11:779. doi: 10.1186/1471-2458-11-779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maselle AY, Mashalla YJ, Kayombo EJ, Mwaiselage JD, Mwamba NE, Kaniki I. Reducing therapeutic injection overuse through patients-prescribers Interaction Group Discussions in Kinondoni District, Dar es Salaam, Tanzania. Tanzan J Health Res. 2011;13:87–92. doi: 10.4314/thrb.v13i1.63093. [DOI] [PubMed] [Google Scholar]
- 26.Saurabh MK, Yadav AK, Gupta P, Singhai A, Saurabh A. Comparative study of prescribing behaviors of government doctors of teaching hospital and private practitioners in Jhalawar City (Rajasthan) J Pharm Sci Res. 2010;2:208–15. [Google Scholar]
- 27.Rahman Z, Nazneen R, Begum M. Evaluation of prescribing pattern of the private practitioners by the undergraduate medical students. Bangladesh J Pharmacol. 2009;4:73–5. [Google Scholar]
- 28.Pati RR. Prescribing pattern among medical interns at the rural health centres of a Medical College, Manipal, Karnataka. Indian J Community Med. 2004;29:128–9. [Google Scholar]
- 29.Otoom S, Batieha A, Hadidi H, Hasan M, Al-Saudi K. Evaluation of drug use in Jordan using WHO patient care and health facility indicators. East Mediterr Health J. 2002;8:544–9. [PubMed] [Google Scholar]
- 30.Laing R, Hogerzeil H, Ross-Degnan D. Ten recommendations to improve use of medicines in developing countries. Health Policy Plan. 2001;16:13–20. doi: 10.1093/heapol/16.1.13. [DOI] [PubMed] [Google Scholar]


