Abstract
Purpose
To describe the frequency, type, and perceived effectiveness of physical therapy (PT) interventions for children with Friedreich Ataxia (FA); identify barriers to therapy; and solicit advice from parents.
Method
Parents of 30 children with FA participated in semi-structured interviews. Qualitative and quantitative methods were used to analyze the data.
Results
Sixty-seven percent of children received direct PT. Stretching and strengthening were used most frequently and their perceived usefulness increased as the children aged. Seventy-three percent received home exercise programs; 9% implemented these consistently. External barriers included a lack of expert providers and limited reimbursement. Internal barriers included limited time and energy, lack of awareness of services, and children’s preferences not to be treated differently. Parents advised therapists to become experts, advocates, and use approaches based on family and child preferences.
Conclusions
Outcomes provide a starting point for developing further research, education, and effective interventions for children with FA.
Keywords: child, disabled child/psychology, exercise therapy, family health, Friedreich ataxia, parents, patient(family) preference, physical therapy, professional-family relations
INTRODUCTION
Friedreich Ataxia (FA), an autosomal recessive disease although rare is the most prevalent of the inherited ataxias.1 FA is caused by a defect in a gene located on chromosome 9, which results in altered function of the protein frataxin and a toxic buildup of iron within mitochondria in several tissues. This buildup of toxic byproducts leads to oxidative stress, progressive cellular damage, and impairments especially in the nervous, cardiac, endocrine and musculoskeletal systems. The diagnosis is confirmed through genetic testing when there is a family history or clinical signs consistent with the disease manifestations.2,3,4
The cardinal features of FA include progressive gait and limb ataxia.5 Other essential clinical criteria for diagnosis are: age of onset before 25 years, absent knee and ankle deep tendon reflexes, and the presence of pyramidal signs.6 Symptoms typically emerge between the ages of 5 and 15 years7 with a mean onset of 10.72 (±7.4) years.8 Death occurs at a mean age of 37.5 years9 and is usually secondary to cardiomyopathy, pneumonia or aspiration.10 Recent insights into the pathogenesis of FA, however, give rise to new hope for effective drug interventions2,3 underscoring the need for early recognition. Given the disease hallmarks of gait and limb ataxia, children with no family history of FA, may be referred to physical therapy for evaluation and treatment prior to genetic testing.11 This further reinforces the need for PTs (PTs) to recognize, examine, and intervene with impairments associated with the disease in a timely manner.11
Support for the benefits of physical exercise for patient populations with other degenerative diseases that include ataxia is available in the research literature.12,13 It is reasonable to assume the health and function of individuals with FA would also be maintained or improved by regular participation in an adapted exercise program.11 Yet, at present limited evidence is available to guide specific physical therapy interventions to address impairments or functional concerns with patients with FA.11,14 Evidence exists supporting a role for PTs in helping patients with FA improve their overall aerobic fitness;15 in maintaining proper biomechanical alignment to optimize their function;16 and in obtaining appropriate adaptive mobility equipment to minimize falls as their impairments progress.17,18
Given limited evidence describing appropriate physical therapy interventions for children and families with FA as well as a lack of insight into the family’s and patient’s perceptions further description may provide valuable insight into future research questions and the development of appropriate family and patient-centered plans of care. The purposes of this study were to: describe the frequency, type, and perceived effectiveness of physical therapy interventions received by children with FA; identify potential barriers to therapy; and solicit advice or feedback from parents on factors and activities PTs should consider when treating children with FA.
METHODS
Participants
Forty-five families of children diagnosed with genetically confirmed FA, enrolled in a Phase 2 clinical trial to establish the efficacy of idebenone for patients with FA were asked to volunteer to participate in an expanded history and interview via telephone. Recruitment occurred during a routine follow-up visit to the National Institutes of Health. Informed consent included consent to participate in a recorded telephone interview at a later date.
Children in the phase 2 clinical trial met the following inclusion criteria: genetically confirmed FA; evidence of neurological impairment; body weight between 30 and 80 kg; chronological age between 9 and 17 years; and demonstrated ability to walk 25 feet with or without an assistive device. Children were excluded if they had been exposed to idebenone, coenzyme Q10, or other dietary supplements for a period of at least 1 month before enrollment. Children were enrolled in the phase 2 study following informed consent by their parent or guardian and participant assent. IRB approved this study as an expanded history.
Design
This is a descriptive study using a mixed qualitative and quantitative design. A semi-structured interview protocol was developed that included open and closed ended questions around a guiding framework to facilitate data collection. The interview protocol was reviewed by an NIH panel of experts familiar with research methods as well as with FA. Questions were designed to gather information about the medical history; the frequency, type, and perceived effectiveness of interventions provided; potential barriers to therapy; and advice for new therapists treating children with FA (see Appendix, Supplemental Digital Content 1, at http://links.lww.com/PPT/A35). To facilitate parental recall of details of therapeutic interventions that may have occurred quite some time ago, the time intervals used in the guiding framework were partitioned by years associated with typical progression in school (e.g., preschool, middle school, high school).
Data collection and analyses
Following the written informed consent, 1 of the investigators scheduled a telephone appointment to speak with a parent of each child. At the beginning of the telephone conversation, the purpose of the study was reiterated, and informed consent and permission to record the conversation were reconfirmed. The researcher asked questions following the interview protocol and all responses were recorded. Researchers spoke only to the parent; however, parents of older children frequently consulted their children in responding to the questions posed. All interviews were transcribed and de-identified to preserve the confidentiality of the participants.
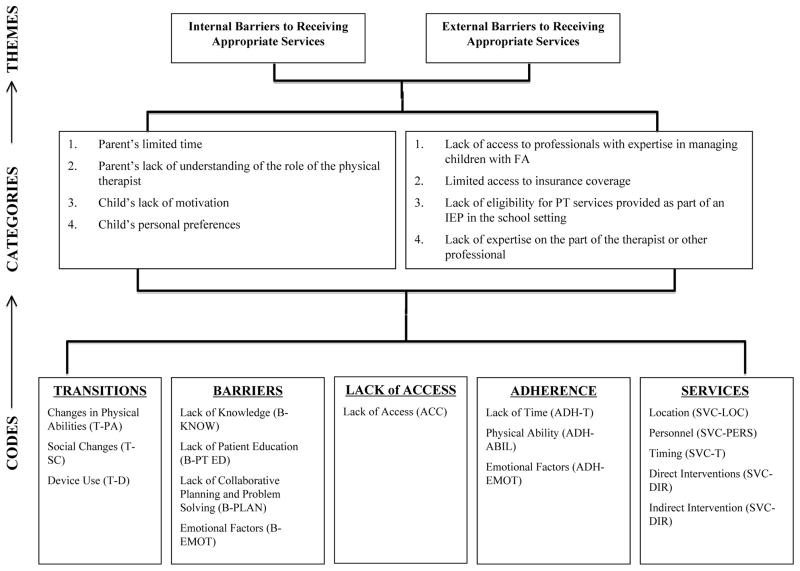
Responses to closed-ended questions were summarized using descriptive statistics. Responses to open-ended questions were analyzed using qualitative methods. One investigator used inductive analysis to search responses for clusters and patterns of meaning.19 From the clusters, codes were defined and a coding schema was developed. Two investigators independently applied the coding schema to a portion of the data. More than 1 code was applied to each response when warranted. Independent analyses were compared and the coding schema was refined further through consensus. The 2 investigators applied the coding schema to another portion of the data and inter-rater reliability of the coding schema was assessed using a kappa statistic. This process continued until an acceptable level of reliability was achieved and 1 investigator finished the analysis, continually seeking emergent and disconfirming data.19 Analysis of the open codes, subsequently led to the development of categories and themes.19 The third investigator was used as a peer reviewer to ensure accurate interpretation of the comments. Figure 1 provides examples of the process used to identify categories and themes.
FIGURE 1.
Example of Codes Leading to Themes
The following major steps were taken to maximize credibility and trustworthiness of the outcomes of this study: 1) multiple researchers were used to independently analyze the raw data; 2) inter-rater reliability measures (kappa statistic) were used to ensure reliability of the coding schema; 3) a third researcher was used as a peer reviewer to confirm the accuracy of the results obtained; 4) a search for negative cases and disconfirming information was ongoing; and 5) low inference data (i.e., verbatim quotes) were obtained and reported to support the themes that emerged.
RESULTS
Description of Participants
The 30 children whose parents agreed to participate in the interview included: 18 males and 12 females, ranging in age from 9 to 17 years, with a mean age of 13.8 years. Seven children were in elementary school; 9 in middle school or junior high, and 14 in high school at the time the interviews were conducted. All the children were Caucasian which is reflective of the predominant ethnicity of those diagnosed with FA.20 The mean age at which signs and symptoms of FA were first noted in this group was 7.1 years, with a range of 1 to 13 years. Genetically confirmed FA, however, occurred at a mean age of 9.6 years, and the gap between the onset of reported signs and symptoms and diagnosis of FA ranged from 1 year to 10 years with 63% of the children diagnosed more than 2 years following onset of signs and symptoms. Early diagnosis was frequently associated with genetic testing following the diagnosis of an older sibling. The children demonstrated a range of system involvement typical of a diagnosis of FA. Sixty-four percent of the children in this sample population were diagnosed with hypertrophic cardiomyopathy, which was determined to be mild by the child’s physician in 31.6% of these cases. None of the children were diagnosed with diabetes mellitus, another comorbidity frequently associated with FA.21 Within this study 18 children (60%) exhibited pes cavus, and 1 child (3%) demonstrated pes planus. Twenty six children (86.7%) had scoliosis; 9 were considered “mild”; 7 “severe”; and 10 were not specified in regards to severity.
Frequency, Type, and Perceived Effectiveness of Physical Therapy Interventions Received
The most frequent direct interventions received were muscle strengthening and stretching followed by balance training. Most parents were not able to specifically recall treatment frequencies or durations, even when the child was currently receiving therapy in the schools. For those who did recall, frequency appeared to range from a monthly consult (in the school or in a specialty clinic) to twice weekly sessions in the school. The parents of 5 children reported their child received episodic outpatient therapy in a nearby center or clinic.
Parent’s perceptions of the usefulness of the strengthening and stretching activities were only slightly better than neutral during the elementary years. However, the perceived usefulness increased as the child became older and likely experienced contractures associated with increasing spasticity and immobility. There were isolated instances, in which a parent enthusiastically endorsed the effectiveness of stretching. For example, 1 parent noted progression of the postural deformities the child was experiencing was halted coincident with receiving physical therapy services. As a group, parents perceived balance training as minimally helpful and it was no longer used as an intervention when the child entered high school as children in this age range primarily used wheelchairs for mobility in the community and school The most frequently identified mobility training was with a walker to assist with transfers and to maneuver shorter distances within the context of the classroom or home; however, reportedly many of the children resisted the use of a walker because they associated it as a device “for old people”. Table 1 summarizes the interventions and perceived usefulness of the interventions received by the children as reported by their parents.
TABLE 1.
Average Perceived Usefulness of Interventions Received
| Intervention | AGE RANGE (years) | |||
|---|---|---|---|---|
|
| ||||
| 0–4 | 5–11 | 12–14 | 15–20 | |
| Mobility training | * | 3.5 (n=6) | 3.0 (n=7) | 3.0 (n=2) |
| Balance training | * | 3.2 (n=12) | 3.3 (n=9) | * |
| Functional training | * | N/A (n=1) | 4.0 (n=2) | * |
| Muscle stretching/strengthening | 4.0 (n=1) | 3.5 (n=14) | 3.9 (n=16) | 4.2 (n=5) |
| Therapy to recover from injury/surgery | * | 4.0 (n=2) | * | 4.0 (n=2) |
| Other therapy (e.g., aquatic therapy, hippotherapy) | * | 5.0 (n=6) | 4.4 (n=6) | 5.0 (n=2) |
0=strongly disagree; not helpful to 5=strongly agree; very helpful scale
n = the number of participants receiving the specified intervention at the time of interview or recalled receiving the intervention in the specified age range.
No responses in this category.
The open ended comments were analyzed using qualitative methods. Substantial inter-rater agreement (Kappa = .69) of the coding schema was established.22 Parents noted a desire for more therapies for their children but described barriers to obtaining appropriate services that were both internal and external to the family unit. They described the home exercise program, in particular, as being both challenging and burdensome. Finally, they offered advice to PTs working with children with FA.
Internal Barriers to Receiving Appropriate Services
Barriers internal to the family unit emerged from both the parents and the children. Parents identified their own limited time and lack of understanding of the role of the PT as barriers. They also identified a lack of motivation and personal preferences on the part of the children as potentially interfering with acquiring appropriate services. The following are examples of direct quotes from the parents:
We really did not pursue because we didn’t know what therapy could do for her. We probably should of though after her surgery.
We have to travel 45 miles each way to bring her to school and then I have to go to work yet… I wish she could do it in her day instead of something else.
I try to stretch her most days and bike most days for muscle building but she doesn’t want to do it.
We did not ever pursue things too much at school but that was because my children wanted it that way.
We’ve got a few things at school to try to make it easier, but she is one of those kids who doesn’t want any special treatment.
External Barriers to Receiving Appropriate Services
External barriers to obtaining appropriate therapies included a lack of access to professionals with expertise in managing children with FA; limited access to insurance coverage; and lack of eligibility for physical therapy services provided as part of an individualized education plan in the school setting. Finally, the parents’ lack of understanding of the role of the therapist coupled with a lack of expertise on the part of the therapist or other professionals at times led to conflicts. The following are exemplary quotes from the parents:
She got therapy before her diagnosis but they didn’t know what they were treating her for so they didn’t know really what to do…just that she had balance that was off. When they told us she had FA, the PT did not know what FA was.
[PT] is also trying to help me with the PE department because they tend to have her do the stopwatch or do work instead of giving her adaptive PE…which is really frustrating because she needs physical education, too.
The insurance would give you 8 weeks or something. That was always frustrating as they did not have an allowance for a chronic degenerative disease that wasn’t going to get better… to have some kind of ongoing service…does help.
During that time they had her in the IEP program, but couldn’t keep her there because her grades were too high. Once she got out of the IEP program the PT stopped.
[The school told] me that until his grades start falling it’s not an academic issue. They won’t give him any services.
So the [therapist] wanted to give him a wheelchair but I [thought] he has got to keep mobile as long as we can. She and I had different philosophies.
Home Exercise Program: A Challenge and a Burden
Twenty-two (73%) of the children received a home exercise program (HEP) as a component of the intervention or sometimes the main mode of intervention. Parents reported the HEP consisted primarily of muscle stretching. However, follow-through and adherence were both challenging and burdensome. While barriers to adherence were generally internal to the family unit, given the prevalence of comments related specifically to the HEP it is being reported as a separate theme. Only 2 (9%) of the parents of children receiving a HEP reported consistent implementation, 9 (41%) reported occasional implementation, and 11 (50%) indicated they and their children do not perform the HEP. While well intentioned, parents reported they often did not have time, they forgot, or the child was simply too tired at the end of a long day to participate. The children also frequently resisted their HEP, which at times led to arguments and increased parent-child stressors. The following are exemplary quotes from the parents:
He should do [exercises] at home but we keep forgetting. [We were] too busy…tend[ed] to forget.
To say that she does [her HEP] consistently would be lying…There were periods where we as parents were bad because of our lifestyles… it’s already tiring for her. She’s had a long day and she tires easy.
You know you got to do it but… she’ll do the exercise for other people but she won’t do it for me. Just working with the parent is not helping.
For a while I would take them [both children with FA] to the local swimming pool and I would ask them to stretch their heels on the pool step and we would argue about it.
Advice for Therapists
Parents had a broad range of advice to offer therapists in working with children and families with FA. The major themes that emerged include: become the expert; be an educator, an advocate and a resource; encourage activity; know your patient and be realistic; encourage socialization and outside activities; and use effective interventions. Table 2 provides quotes illustrating each of these themes.
TABLE 2.
Advice for Physical Therapists Working with Families with Children Diagnosed with FA
| Theme | Sample Quotes |
|---|---|
| Become the Expert | “I felt like I was the expert. No one knows as much. It felt good to go to someone who could tell me.” “It is very encouraging to have someone give us advice about things. It feels good to go to someone who can tell me things as opposed to the other way around. We really feel like we are on our own… Otherwise, you don’t know who to trust.” |
| Be an Educator, an Advocate, and a Resource | “They should be able to instruct for more things at home so that we know what to do with him when he can’t go anymore. Pick things that are easy to do that I can do with him or things he normally would like to do.” “Start it earlier; don’t wait… I would say the earlier the better. Waiting is doing the child a disservice. You can’t get rid of it but you can keep them healthier longer.” “Network and support groups are helpful. Therapists should try and know about these… to be outside the box because you can’t guarantee the therapist will be there all the time.” |
| Encourage activity | “[Emphasize] walking with a walker, those kinds of things. Because last summer we went to ___ to visit my family and there he was sitting most of the day. He was not walking at all. That was a setback for him.” “Encourage people to use the function they have because the more you do it… the people with FA… it’s true that you use it or lose it. Encourage them to stay healthy and active.” “If you can keep the kid active and involved. I have two other kids who are really pistols. They drive him more than anyone else. One thing we learned is when he works out all the time, his coordination improved. He has more control basically. Don’t give up, they can get better.” |
| Know your patient and be realistic | “Don’t push too hard. You need to keep a better eye on how she is doing, on how it affects them. Don’t just take the child’s word for it. Watch for signs that she is too tired… Don’t push them past the point of being too tired.” “Short things that they can finish and feel good about. Something they can accomplish.” “My experience has been that PTs tend to work from a standpoint of, here’s where you are, here’s how we can improve. I think it [should be] here’s where we are, here’s where we want to stay. Well she may be doing fine right now, but I want to make sure she stays fine.” “[The PT should] spend some time with them before starting to work with them in a non-rehab setting just doing what the kid wanted to do and watch them. When they are under the microscope they will try harder to be what they think you want them to be. When they are just being themselves you will see what type of gait they have and other things.” |
| Encourage socialization and outside activities | “We also do horseback riding… That helps to keep the legs from scissoring. They are not scissoring yet, I’m just hoping to avoid it.” “She also quite likes yoga. She needs to go with other children her age to make it fun.” |
| Use Effective Interventions | “Hydrotherapy is excellent, too. There’s no laws of balance; they’re not going to fall. They have freedom in the water that they don’t have on land. And it’s important for them to have that sensation… Even once a week was better than nothing.” “It’s rather the strengthening and stretching, to keep the muscles conditioned as you can… The weight training is really good. That’s something she can do, like try to do 5 reps or 10… things that challenge her are interesting to her, instead of just sitting there and being stretched. She has a little more involvement in it.” “And I think the strength and the toning, I think we try to stress with him that he needs to stay strong and not let his muscles deteriorate because he’s going to need them. We believe with all of our hearts that the answer to this is coming. We try to stress to him that he needs to be ready for that day. And so we think that stretching, toning, and even maybe a little bit of weight training is very beneficial.” |
DISCUSSION
Frequency, Type, and Perceived Effectiveness of Physical Therapy Interventions Received
The therapeutic activities performed with the children whether directly or via a HEP emphasized muscle stretching and to a lesser extent muscle strengthening. This is consistent with recommended components of a general plan for children with FA14 or other degenerative diseases of childhood.23 Stretching activities in all likelihood assisted in maintaining biomechanical alignment of the children’s feet and trunk; this outcome facilitates maintenance of function in children with FA.16 Given the progressive range of motion impairments associated with disease progression, the increased parental perception of the usefulness of stretching as an intervention is also understandable. Balance training was generally not perceived as effective by parents and comments suggested parents felt the progressive ataxia typical of FA was not amenable to balance training. Only 3 children received functional mobility training, and no children were participating in aerobic activities. Both interventions are supported by the literature as potentially effective in maintaining independence and quality of life16,17 and therapists should consider including functional mobility and aerobic training in HEPs and direct intervention programs when working with children and families with FA.
In responding to open-ended questions, the most frequent type of intervention parents recommended was aquatic therapy. Parents indicated water provided children with the ability to exercise freely without the fear of losing their balance or falling. Additionally, parents stressed the importance of encouraging children with FA to stay active and involved in activities they enjoyed. Although, parents were generally not able to recall specific treatment frequencies, most felt their children should be participating in more therapeutic activities to maintain functional independence for as long as possible.
Potential Barriers
Home Exercise Program
Although the majority of the parents reported their children were supposed to be performing a HEP, most identified a number of internal barriers preventing consistent follow-through on the recommended exercises. The reasons given for non-adherence varied from time constraints to fatigue and resistance on the part of the child. This finding is consistent with previous research reporting low HEP adherence among caregivers of children with disabilities and that 50% of parents likely do not adhere with prescribed therapeutic regimes.24
A predominant factor cited for failure to adhere is caregiver stress secondary to the burden of increased care, financial strains, and parental grief reactions to the child’s condition and well-being.24–27 Caring for a child with a progressively disabling neurodegenerative disease and a poor prognosis likely exacerbates all of those factors. Parents caring for a child with progressive disability report higher physical and emotional stress than parents of children with non-progressive disabilities27. In addition, stress may be compounded secondary to parental insecurity in dealing with a rare disease such as FA.27
Given these reported stressors, it is important for therapists working with families with children with FA to be cognizant of strategies to minimize burden and optimize adherence. In other pediatric patient population groups reported in the literature, families were more likely to comply with home exercise programs if they perceived the activities as minimally demanding and if the activities and location of the HEP were sufficiently varied to provide interest.28 Explicit instructions and continued encouragement and support to the family and child may also increase HEP adherence.29 Emphasizing self-motivation and accompanying the prescribed activities with visual and audio instructions may assist with the level of cooperation of adolescent children and potentially decrease conflict similar to that reported by the study participants.30
Perceived Barriers to Obtaining Appropriate Services
The external barriers to obtaining appropriate interventions reported most frequently by parents in this study were related to the expertise of the professionals involved and access to quality physical therapy care. FA is a relatively rare disease and is likely not covered in depth in an entry-level PT program nor is there much written in the literature describing effective physical therapy interventions. It is not surprising that families in this study were frustrated by lack of expertise of therapists and its effect on appropriate care for their child. In a study31 describing perceived barriers to obtaining therapy services for children with the more common diagnosis of cerebral palsy, however, parents also described therapists’ knowledge gap as an impediment to appropriate services.
To implement an effective plan of care and make appropriate referrals, therapists have an obligation to recognize atypical patterns of impairments, use appropriate search strategies of the literature to identify possible interventions, and make referrals or seek assistance when they do not feel qualified to address the child’s needs. If parents could be reassured that the professionals working with their children are proactively seeking information and involved in learning about the appropriate care of their children, satisfaction with care management may improve.32–34 Parents also noted frustration with the lack of expertise of school personnel. Literature supports the sentiment raised by parents in this study regarding frustration surrounding lack of understanding of the condition, inadequate professional training, and inability of school personnel to recognize the child’s needs.35 When implementing care within a school system perceived barriers can be lessened, if the therapist assumes the role of expert and educates others regarding the disease process and potential needs.
Additionally, to minimize conflict and optimize care a family centered approach, which includes families in setting goals and selecting interventions is advocated.35 Families of children with FA often have extensive experience with the healthcare community that may affect their expectations. Expectations of healthcare accumulate from one visit to the next.36 Therefore, expectations of services and goals for the child need to be discussed with all parents to form an appropriate plan of care. Family involvement would likely avoid some of the frustration parents described when they perceived the therapist’s goals as either too ambitious or too unrealistic.
Qualifying for Services and Reimbursement
Children with a degenerative disease or chronic condition often experience difficulty in qualifying for physical therapy.37 An analysis of 1994–1995 Health Interview Survey Disability Follow-back data38 indicated that most children with a disability (75%) receive therapies in the school setting. To qualify for these services, however, the child must qualify for special education services (IDEA) and related service such as physical therapy may be provided for educational purposes. Many children with FA do not require special education services. Yet private health plans in general provide very limited coverage for ongoing care associated with a chronic condition.39 Health plans limit coverage of services for people with progressive disorders deeming services provided to maintain function as not medically necessary.31,37 Most parents in this study were frustrated by the lack of financial access to therapy as evidenced most by those families with children with FA in high school who were no longer eligible to receive any type of service. This finding is consistent with the Leiter’s38 description of services to children with disability decreasing as the child moves from elementary and middle school to high school. Given the challenges these families face in obtaining services for their children, it is imperative for therapists working within the school system to not only educate school personnel, but also become knowledgeable in federal, state and local regulations guiding the provision of rehabilitative services to be able to advocate most effectively for their patients.40,41
Advice to therapists
In providing advice for new therapists, parents suggested ways to overcome some of the barriers they experienced while better integrating the needs and challenges of the families and children into the development of the plan of care. Parents encouraged therapists to know their patients and families, encourage activity, and be realistic. Parents urged therapists to find a balance between challenging the child to maintain or gain function versus recognizing the limitations imposed by fatigue and the need to perhaps focus on maintenance versus improvement. Parents also urged therapists to recognize the challenges the family faces in adhering to demanding, routine, and tedious HEPs. This advice is consistent with the demand for pediatric therapists to deliver services that are embedded into routines and contexts that are meaningful and have value to the child and family.42 Embedding and integrating exercises into the social context of the child and family may enhance adherence and participation. Parents in this study urged therapists to consider activities such as swimming lessons, aquatic therapy, horseback riding and other social activities the child might enjoy with peers and with family. Collaborating with school personnel may optimize the child’s ability to participate with peers in all school-related activities including physical education.
Parents also encouraged therapists to be experts, educators, advocates and resources. They emphasized the need for therapists to become more expert and to advocate for earlier and ongoing therapy for children with FA. Currently many children with FA are referred to physical therapy without a definitive diagnosis.11 As we participate in direct access to a greater extent, more children and families will access physical therapy directly and therefore rely on therapists to implement an effective plan of care and make appropriate referrals. These roles and functions are consistent with Vision 2020 and the core values of the profession. Therapists are encouraged to: assume responsibility for learning; advocate for the health and wellness needs of society including access to physical therapy services; and promote social policies that affect the function and needs of patients.26,43
Limitations
The descriptions and perceptions of the parents in this study regarding physical therapy services for their children with FA are subject to recall bias given the retrospective nature of the data collection. The threat to validity and reliability secondary to a recall bias can be reduced by a well-structured questionnaire.44 The structured questionnaire used to gather information in this study was reviewed by a team of experts and constructed around age periods likely to facilitate recall. Recall was also enhanced by the parents occasionally consulting with their children to confirm or amplify a description. Nevertheless, it is likely all the descriptions provided by the parents related to their child’s therapy were incomplete and represented only part of the total picture of the services provided. Qualitative methods, although not generalizable, are most valuable in providing insights not otherwise available using quantitative methods alone. Numerous strategies were used to optimize the trustworthiness and credibility of these results, however further research is needed in order to generalize these insights to the population of all children diagnosed with FA.
Future Research
Research into effective pharmacological interventions for persons with FA has increased dramatically with the contemporary understanding of the pathogenesis of the disease process.45 Investigating the effect of rehabilitation measures in isolation or in conjunction with pharmacological interventions is critically necessary to improve the outcomes and quality of life in children and families with FA. Parental input provides an entry-point to identifying strategies to overcome barriers to obtaining services, adherence to prescribed activities, as well as effective plans of care that may enhance parent and child satisfaction. Examining the long term social and physical outcomes of children with FA may have policy implications related to defining educational needs and eligibility for reimbursement given the degenerative nature of this disease.
CONCLUSIONS
The information provided by the families in this study can serve as a foundation for understanding parents’ perceptions of the effectiveness of services currently provided to children and families with FA. The findings may enable therapists to develop more effective plans of care that take into consideration the context within which the child and family exist. Additionally, therapists should more frequently integrate therapeutic activities supported by the literature such as aerobic exercise and functional training. Therapists should employ strategies to improve adherence to HEPs such as embedding programs in the social contexts of the child and family. Parents provided advice for therapists new to FA that may help them frame their approach to effective care. Finally, parents articulated barriers they experienced to accessing quality care for their children. Therapists need to embrace their role as expert, educator and advocate in order to assist children and their families overcome these barriers. Prospective studies on the effectiveness of physical therapy interventions and strategies to optimize adherence are needed to add to the limited evidence base for effective care for children with FA.
Supplementary Material
Footnotes
Conflict of Interest statement: The authors declare no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.pedpt.com).
At the time this article was written, Sylvia Morgan was a student at The George Washington University, Doctor of Physical Therapy Program, Washington, DC.
References
- 1.Cossee M, Schmitt M, Campuzano V, et al. Evolution of the Friedreich’s ataxia trinucleotide repeat expansion: founder effect and premutations. Proceedings Of The National Academy Of Sciences Of The United States Of America. 1997;94(14):7452–7457. doi: 10.1073/pnas.94.14.7452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campuzano V, Montermini L, Koenig M, et al. Frataxin is reduced in Friedreich ataxia patients and is associated with mitochondrial membranes. Hum Mol Genet. 1997;6(11):1771–1780. doi: 10.1093/hmg/6.11.1771. [DOI] [PubMed] [Google Scholar]
- 3.Campuzano V, Montermini L, Pandolfo M, et al. Friedreich’s ataxia: Autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science (Washington D C) 1996;271(5254):1423–1427. doi: 10.1126/science.271.5254.1423. [DOI] [PubMed] [Google Scholar]
- 4.Beal MF. Energetics in the pathogenesis of neurodegenerative diseases. Trends Neurosci. 2000;23:298–304. doi: 10.1016/s0166-2236(00)01584-8. [DOI] [PubMed] [Google Scholar]
- 5.Harding A, Zilkha K. ‘Pseudo-dominant’ inheritance in Friedreich’s ataxia. J MedGenet. 1981 Aug;18(4):285–287. doi: 10.1136/jmg.18.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wood N. Diagnosing Friedreich’s ataxia. Arch Dis Child. 1998 Mar;78(3):204–207. doi: 10.1136/adc.78.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harding A. Friedreich’s ataxia: a clinical and genetic study of 90 families with an analysis of early diagnostic criteria and intrafamilial clustering of clinical features. Brain. 1981 Sep;104(3):589–620. doi: 10.1093/brain/104.3.589. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan J. Friedreich’s ataxia is a mitochondrial disorder. Proc Natl Acad Sci U S A. 1999 Sep 28;96(20):10948–10949. doi: 10.1073/pnas.96.20.10948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delatycki M, Williamson R, Forrest S. Friedreich ataxia: an overview. J Med Genet. 2000;37(1):1–8. doi: 10.1136/jmg.37.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shapiro F, Specht L. The diagnosis and orthopaedic treatment of childhood spinal muscular atrophy, peripheral neuropathy, Friedreich ataxia, and arthrogryposis. J Bone Joint Surg. 1993;75:1699–1714. doi: 10.2106/00004623-199311000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Maring J, Croarkin E. Presentation and progression of friedreich ataxia and implications for physical therapy examination. Phys Ther. 2007;87(12):1687–1696. doi: 10.2522/ptj.20060232. [DOI] [PubMed] [Google Scholar]
- 12.Mostert S, Kesselring J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult Scler. 2002;8:16–168. doi: 10.1191/1352458502ms779oa. [DOI] [PubMed] [Google Scholar]
- 13.Surakka J, Romberg A, Mäentaka K, et al. Effects of aerobic and strength exercise on motor fatigue in men and women with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2004 Oct;18(7):737–746. doi: 10.1191/0269215504cr780oa. [DOI] [PubMed] [Google Scholar]
- 14.Blattner K. Friedreich’s ataxia: A suggested physical therapy regimen. Clin Manage. 1988;8(4):14–15. 30. [Google Scholar]
- 15.Fillyaw M, Ades P. Endurance exercise training in Friedreich ataxia. Arch Phys Med Rehab. 1989 Oct;70(10):786–788. [PubMed] [Google Scholar]
- 16.Delatycki M, Holian A, Churchyard A, et al. Surgery for equinovarus deformity in Friedreich’s ataxia improves mobility and independence. Clin OrthopRelat R. 2005;430:138–141. doi: 10.1097/01.blo.0000150339.74041.0e. [serial online] Available from: CINAHL Plus with Full Text, Ipswich, MA. [DOI] [PubMed] [Google Scholar]
- 17.Harris-Love M, Siegel K, Paul S, Benson K. Rehabilitation management of Friedreich ataxia: Lower extremity force-control variability and gait performance. Neurorehab Neural Re. 2004;18:117–124. doi: 10.1177/0888439004267241. [DOI] [PubMed] [Google Scholar]
- 18.Bateni H, Heung E, Zettel J, et al. Can use of walkers or canes impede lateral compensatory stepping movements? Gait Posture. 2004;20:74–83. doi: 10.1016/S0966-6362(03)00098-5. [DOI] [PubMed] [Google Scholar]
- 19.Strauss A, Corbin J. Basics of Qualitative Research. Thousand Oaks, CA: Sage Publications, Inc; 1998. [Google Scholar]
- 20.Pandolfo M. Friedreich ataxia. Arch Neurol-Chicago. 2008 Oct;65(10):1296–1303. doi: 10.1001/archneur.65.10.1296. [DOI] [PubMed] [Google Scholar]
- 21.Watkins P, Thomas P. Diabetes mellitus and the nervous system. J Neurol Neurosur Ps. 1998 Nov;65(5):620. doi: 10.1136/jnnp.65.5.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Portney L, Watkins M, editors. Foundations of Clinical Research: Application to Practice. Upper Saddle River, NJ: Prentice Hall; 2009. [Google Scholar]
- 23.Ciafaloni E, Moxely RT. Treatment options for Duchenne muscular dystrophy. Curr Treat Option N. 2008 Mar;10(2):86–93. doi: 10.1007/s11940-008-0010-4. [DOI] [PubMed] [Google Scholar]
- 24.Rone-Adams S, Stern D, Walker V. Stress and compliance with a home exercise program among caregivers of children with disabilities. Pediatr Phys Ther. 2004 Sep;16(3):140–148. doi: 10.1097/01.PEP.0000136006.13449.DC. [DOI] [PubMed] [Google Scholar]
- 25.McCubbin M. Family stress and family strengths: a comparison of single- and two-parent families with handicapped children. Res Nurs Health. 1989 Apr;12(2):101–110. doi: 10.1002/nur.4770120207. [DOI] [PubMed] [Google Scholar]
- 26.Miller A, Condin C, McKellin W, Shaw N, Klassen A, Sheps S. Continuity of care for children with complex chronic health conditions: parents’ perspectives. BMC Health Serv Res. 2009 Dec 21;9:242. doi: 10.1186/1472-6963-9-242. Available from: MEDLINE with Full Text, Ipswich, MA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dellve L, Samuelsson L, Tallborn A, Fasth A, Hallberg L. Stress and well-being among parents of children with rare diseases: a prospective intervention study. J Adv Nurs. 2006 Feb 15;53(4):392–402. doi: 10.1111/j.1365-2648.2006.03736.x. Available from: CINAHL Plus with Full Text, Ipswich, MA. [DOI] [PubMed] [Google Scholar]
- 28.Takken T, van der Torre P, van der Net J, et al. Development, feasibility and efficacy of a community-based exercise training program in pediatric cancer survivors. Psycho-Oncol. 2009 Apr;18(4):440–448. doi: 10.1002/pon.1484. [DOI] [PubMed] [Google Scholar]
- 29.Prasad S, Cerny F. Factors that influence adherence to exercise and their effectiveness: Application to cystic fibrosis. Pediatr Pulm. 2002 Jul;34(1):66. doi: 10.1002/ppul.10126. [DOI] [PubMed] [Google Scholar]
- 30.Marrero DG, Fremion AS, Golden MP. Improving compliance with exercise in adolescents with insulin-dependent diabetes mellitus: results of a self-motivated home exercise program. Pediatrics. 1988;81(4):519–525. [PubMed] [Google Scholar]
- 31.Cada EA, O’Shea RK. Identifying barriers to occupational and physical therapy services for children with cerebral palsy. J Pediatr Rehabil Med. 2008;1:127–134. [PubMed] [Google Scholar]
- 32.Miller A, Condin C, McKellin W, Shaw N, Klassen A, Sheps S. Continuity of care for children with complex chronic health conditions: parents’ perspectives. BMC Health Serv Res. 2009 Dec 21;9:242. doi: 10.1186/1472-6963-9-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wood D, McCaskill Q, Livingood W, et al. A multi-method assessment of satisfaction with services in the medical home by parents of children and youth with special health care needs (CYSHCN) Matern Child Healt J. 2009;13(1):5–17. doi: 10.1007/s10995-008-0321-9. [DOI] [PubMed] [Google Scholar]
- 34.Garwick A, Patterson J, Bennett CF, Blum RW. Parents’ perceptions of helpful versus unhelpful types of support in managing the care of pre-adolescents with chronic conditions. Arch Pediat Adol Med. 1998;152:665–671. doi: 10.1001/archpedi.152.7.665. [DOI] [PubMed] [Google Scholar]
- 35.Blue-Banning M, Summers JA, Frankland HC, Nelson LL, Beegle G. Dimensions of family and professional partnerships: constructive guidelines for collaboration. Except Children. 2004;70:167–184. [Google Scholar]
- 36.Sobo E, Seid M, Gelhard L. Parent-Identified Barriers to Pediatric Health Care: A Process-Oriented Model. Health Serv Res. 2006 Feb;41(1):148–172. doi: 10.1111/j.1475-6773.2005.00455.x. Available from: Academic Search Complete, Ipswich, MA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scheer J, Kroll T, Neri M, Beatty P. Access barriers for persons with disabilities: the consumer’s perspective. J Disabil Policy Stud. 2003 Feb;13(4):221–230. [Google Scholar]
- 38.Leiter V. The Division of Labor Among Systems of Therapeutic Care for Children with Disabilities. J Disabil Policy Stud. 2005 Winter;16(3):147–155. Available from: Academic Search Complete, Ipswich, MA. [Google Scholar]
- 39.Anderson G, Knickman J. Hanging the chronic care system to meet people’s needs. Health Affair. 2001;20:146–160. doi: 10.1377/hlthaff.20.6.146. [DOI] [PubMed] [Google Scholar]
- 40.Effgen S, Chiarello L, Milbourne S. Updated competencies for PTs working in schools. Pediatr Phys Ther. 2007 Dec;19(4):266–274. doi: 10.1097/PEP.0b013e318158ce90. [DOI] [PubMed] [Google Scholar]
- 41.Rapport M. Legal Guidelines for the Delivery of Special Health Care Services in Schools. Except Children. 1996 May 1;62(6):537–49. Available from: ERIC, Ipswich, MA. [Google Scholar]
- 42.Pretti-Frontczak K, Barr D, Macy M, Carter A. Research and Resources Related to Activity-Based Intervention, Embedded Learning Opportunities, and Routines-Based Instruction: An Annotated Bibliography. Top Early Child Spec. 2003;23(1):29. [Google Scholar]
- 43. [Accessed on Novemeber 11, 2011];Professionalism In Physical Therapy: Core Values. Avaiable at: http://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/BOD/Judicial/ProfessionalisminPT.pdf.
- 44.Hassan E. Recall Bias can be a Threat to Retrospective and Prospective Research Designs. Int J of epidemiol. 2006 Sep 11;3(2):4. [Google Scholar]
- 45.Delatycki MB, Ioannou PA, Churchyard AJ. Friedreich ataxia: from genes to therapies? Med J Australia. 2005;182:439–439. doi: 10.5694/j.1326-5377.2005.tb06779.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.