Abstract
Background
There is currently no reliable treatment for phantom limb pain (PLP). Chronic PLP and associated cortical abnormalities may be maintained from abnormal peripheral input, raising the possibility that a continuous peripheral nerve block (CPNB) of extended duration may permanently reorganize cortical pain mapping, thus providing lasting relief.
Methods
Three men with below-the-knee (2) or -elbow (1) amputations and intractable PLP received femoral/sciatic or infraclavicular perineural catheter(s), respectively. Subjects were randomized in a double-masked fashion to receive perineural ropivacaine (0.5%) or normal saline for over 6 days as outpatients using portable electronic infusion. Four months later, subjects returned for repeated perineural catheter insertion (“crossover”), and received an ambulatory infusion with the alternate solution. Subjects were followed for up to one year.
Results
By chance, all 3 subjects received saline during their initial infusion and reported little change in their PLP. One subject did not receive crossover treatment; but, the remaining 2 subjects reported complete resolution of their PLP during and immediately following treatment with ropivacaine. One subject experienced no PLP recurrence through the 52-week follow-up period; and, the other reported mild PLP occurring once each week of just a small fraction of his original pain (pre-treatment: continuous PLP rated 10/10; post-treatment: no PLP at baseline with average of 1 PLP episode each week rated 2/10) for 12 weeks (lost to follow-up thereafter).
Conclusions
A prolonged ambulatory CPNB may be a reliable treatment for intractable PLP. The results of this pilot study suggest that a large, randomized clinical trial is warranted.
Introduction
Over 200,000 traumatic and surgical amputations occur annually within the United States alone;1 and, over 1.6-million Americans are currently living with an amputated limb.2 The incidence of phantom limb pain (PLP) ranges from 50–95%3–5 and is usually described as “shooting, stabbing, boring, squeezing, throbbing, and burning.”3,6 The economic toll for chronic nonmalignant pain is measured in the billions of dollars annually.1 There is currently no reliable treatment for PLP.7 While more than 43 methods for treating PLP have been described,8,9 prolonged relief is experienced by fewer than 10% of treated patients (as well as 6% of untreated patients).10 Evidence of the intractable nature of phantom pain may be found in a survey of more than 10,000 amputees who, remarkably, reported only a 1% success rate from available treatment options.11 There are few data from randomized trials to guide treatment, leading the authors of a major review to conclude that there remains a substantial “gap between research and practice in the area of phantom limb pain”.7
Current evidence suggests that when a nerve is severed—as occurs during limb amputation—the barrage of nociceptive input triggers a complex interaction between the peripheral and central nervous systems. Both systems are dynamic, and injury to peripheral nerves provokes changes in the spinal cord, dorsal root ganglia, thalamus, and cerebral cortex which are referred to as “neuronal plasticity”.12,13 Reorganization at the level of the spinal cord may result in “sensitization” in which responses to peripheral stimulation results in an exaggerated response, leading to residual limb allodynia and hyperalgesia.14 Additionally, the somatosensory cortex, which “maps” somato-sensory inputs from the body—each location represented in a specific area of the cortex (i.e., homunculus), undergoes plastic changes of this map following deafferentation.15 For example, the cortical zone representing the fingers may be invaded by adjacent areas following a hand amputation and consequent deafferentation.16
Imaging techniques such as functional magnetic resonance imaging have documented a correlation between PLP and cortical reorganization—with the most intense phantom pain provoking the greatest cortical changes.15 Extraordinarily, when neural input from an amputated limb was blocked with a peripheral nerve block in six patients, three had immediate, complete resolution of their phantom pain; and, within minutes, the cortical abnormalities were corrected for these three individuals.17 Unfortunately, when the single-injection nerve block resolved after a few hours, the phantom pain returned. But, this intriguing result demonstrates that the abnormal mapping—and PLP—that occur with amputation are not necessarily fixed and may be dependent on signaling from the peripheral nervous system. Notably, studies of chronic low back pain demonstrate that cortical thickness and cognitive abilities increased simultaneously 6 months after pain treatment.18 These results demonstrate that chronic-pain-induced functional and structural brain abnormalities are not only reversible, but that treating chronic pain can restore normal brain function.18 In other words, chronic PLP and cortical abnormalities may be maintained from abnormal peripheral input, suggesting that a dense, continuous peripheral nerve block (CPNB) of extended duration—lasting days rather than hours—may permanently reorganize cortical pain mapping, thus providing lasting relief from phantom pain. We therefore designed and executed this randomized, double-masked, placebo-controlled, crossover pilot study to systematically investigate this possible intervention.
Materials and Methods
Enrollment
The local Institutional Review Board (University of California San Diego, San Diego, CA) approved all study procedures, and all subjects provided written, informed consent. The trial was prospectively registered at clinicaltrials.gov (NCT00667264). Subjects offered enrollment included adults (18 years or older) with an existing upper or lower limb amputation (including at least one metacarpal or metatarsal bone, respectively) and existing phantom limb and/or residual limb pain described as at least a 2 on a Numeric Rating Scale of pain (NRS) during the previous week, and occurring on a weekly basis over at least the previous month. Additional inclusion criteria comprised subjects’ desiring an ambulatory perineural infusion for over 6 days; willingness to avoid additional “new” analgesic interventions from 4 weeks prior to at least 4 weeks following catheter placement, and preferably to 6 months following catheter placement; and the availability of a “caretaker” who would transport the subject home following the procedure and remain with the subject for at least the first night of infusion. Exclusion criteria included any known hepatic or renal insufficiency; allergy to the study medications; pregnancy; incarceration; and, possessing a contraindication to perineural catheter placement and/or perineural local anesthetic infusion. Only subjects whose entire residual limb (“stump”) could be anesthetized with the CPNB(s) were included in this pilot study. Subjects’ analgesic regimen remained static from 4 weeks prior to at least 4 weeks (preferably 6 months) following catheter placement.
Catheter insertion
Subjects with below-the-knee or -elbow amputations received ultrasound-guided femoral/popliteal-sciatic or infraclavicular perineural catheter(s), respectively (FlexTip Plus, Teleflex Medical, Reading, PA), as previously described.19–21
Upper extremity amputation
Subjects were positioned in the supine position. With a low-frequency curvilinear array ultrasound transducer in a sterile sleeve, the brachial plexus and axillary artery were identified in a transverse cross-sectional (short axis) view. Once the optimal image of the brachial plexus cords was obtained, a local anesthetic skin wheal was raised cephalad to the ultrasound transducer. A 17 gauge, Tuohy-tip needle (FlexTip, Arrow International, Reading, Pennsylvania) was inserted through the skin wheal in-plane beneath the ultrasound transducer and directed caudad until the needle tip was between the axillary artery and the posterior brachial plexus cord. Normal saline (5 mL) was injected via the needle to open the perineural space to allow subsequent insertion of a flexible 19 gauge perineural catheter 5 cm beyond the needle tip. The needle was removed over the catheter, the catheter tunneled subcutaneously, and the catheter affixed using liquid adhesive, occlusive dressings, and an anchoring device.
Lower extremity amputation
Subjects received two perineural catheters: a femoral and a popliteal-sciatic. The popliteal-sciatic catheter was inserted first with the subject in the prone position, followed by the femoral catheter with the subject in the supine position. With a high-frequency linear array ultrasound transducer in a sterile sleeve, the target nerves were identified in a transverse cross-sectional (short axis) view: the sciatic nerve within the proximal popliteal fossa cephalad to the sciatic bifurcation, and the femoral nerve at the inguinal crease. For each insertion, a local anesthetic skin wheal was raised lateral to the transducer, and a 17 gauge, Tuohy-tip needle (FlexTip, Arrow International, Reading, Pennsylvania) was inserted through the skin wheal in-plane beneath the ultrasound transducer and directed medially until the needle tip was posterior to each target nerve. For each insertion, normal saline (5 mL) was injected via the needle to open the perineural space allowing subsequent insertion of a flexible 19 gauge perineural catheter 5 cm beyond the needle tip. The needle was removed over the catheter, and the catheter affixed as described previously for the infraclavicular catheter above.
Mepivacaine (1.5%, 20 mL) with epinephrine (2.5 μg/mL) was injected via each catheter.
Intervention
Treatment allocation occurred following perineural catheter insertion, with subjects randomized to receive over 6 days of perineural infusion with either ropivacaine (0.4%) or normal saline (placebo). The Investigational Drug Service created computer-generated randomization lists, and prepared all study solutions/pumps to allow investigator/subject masking of treatment group assignments. Perineural infusions were provided on an outpatient basis using portable, programmable, electronic infusion pumps (ambIT PCA, Summit Medical, Salt Lake City, Utah).22 Subjects received a total of 1,100 mL of study fluid from either one (upper extremity) or two (lower extremity) pump(s) and external reservoir combinations. The continuous basal infusion rate was determined by catheter location: femoral 2 mL/h; popliteal-sciatic 5 mL/h; and infraclavicular 7 mL/h. No patient-controlled bolus doses were provided. Subjects or their caretakers removed their perineural catheters one week following insertion. Twelve to 16 weeks following the initial catheter placement, subjects had the option of undergoing this same protocol, only with the alternative (“crossover”) treatment (ropivacaine 0.4% or normal saline).
Outcome measurements
We selected outcome measures that have established reliability and validity, with minimal inter-rater discordance, and are recommended for chronic pain clinical trials by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) consensus statement.23 Data collection occurred in person immediately prior to catheter insertions (both initial and crossover), and subsequently by telephone on Days 3, 8, and 28, as well as at Weeks 12 and 52. The Brief Pain Inventory was used at each of these time points, with responses specified for PLP in the previous 24 hours. In addition, subjects were asked the number of times that they experienced PLP and to rate the worst and average PLP on the NRS, all within the previous week.24 Phantom pain was defined with each questionnaire application as “painful sensations referred to the lost body part.”25,26 Residual limb pain, defined as painful sensations existing within the remaining limb, was excluded. The Patient Global Impression of Change scale is a measure allowing patient evaluation of integrated treatment effects compared with their baseline on a 7-point ordinal scale.23 This measure was applied at each of the post-catheter insertion time points.
Results
Three men with below-the-knee (n=2) or -elbow (n=1) amputations and intractable PLP of at least 12 months duration received ultrasound-guided femoral/sciatic or infraclavicular perineural catheter(s), respectively (Table 1). By chance, all 3 subjects received saline during their initial infusion and reported little change in their PLP (Figure 1). One subject with a below-the-knee amputation returned to active duty overseas prior to receiving his second (crossover) infusion with active drug. However, the remaining 2 subjects reported complete resolution of their PLP during and immediately following treatment with ropivacaine. One subject experienced no PLP recurrence through the 52-week follow-up period; and the other reported mild PLP occurring once each week of just a small fraction of his original pain (pre-treatment: continuous PLP rated 10 on the NRS; post-treatment: no PLP at baseline with average of 1 PLP episode each week rated at 2 on the NRS) for 12 weeks (lost to follow-up at 52 weeks). The Brief Pain Inventory questionnaires and Patient Global Impression of Change ratings reflected these improvements (Table 2).
Table 1.
Subject characteristics
| Subject Number: | 1 | 2 | 3 |
|---|---|---|---|
| Age (yr) | 25 | 27 | 47 |
| Height (cm) | 183 | 188 | 180 |
| Weight (kg) | 114 | 80 | 114 |
| Body mass index (kg/m2) | 34 | 23 | 35 |
| Amputation (below-the-) | Knee | Elbow | Knee |
| Amputation side (right vs. left) | Right | Right | Right |
| Amputation etiology | Traumatic | Surgical | Surgical |
| Years since original amputation (yr) | 2 | 1 | 1 |
| Duration of PLP (yr) | 2 | 1 | 1 |
| Surgical revisions (#) | 1 | 15 | 3 |
| Average incidence of phantom pain/day (#) | Continuous | 7 | 5 |
| Worst PLP in week before intervention (NRS) | 10 | 6 | 7 |
| Average PLP in week before intervention (NRS) | 10 | 5 | 5 |
| PLP immediately prior to intervention (NRS) | 8 | 3 | 2 |
| PLP 15 after mepivacaine bolus (NRS) * | 0 | 0 | 0 |
Initial single-injection mepivacaine 1.5% peripheral nerve block
PLP: Phantom limb pain
NRS: Numeric Rating Scale of pain (0–10; 10 equivalent to the worst imaginable pain)
Figure 1.
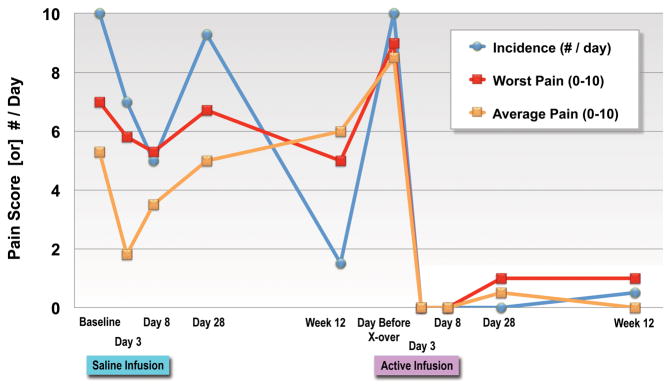
Effects of ambulatory perineural normal saline (placebo) and ropivacaine (“active”) infusions on phantom limb pain severity and incidence (within the previous week, or since the previous time point, whichever was less). Pain severity indicated using a Numeric Rating Scale of 0–10, with 0 equivalent to no pain and 10 equivalent to the worst imaginable pain. Data are expressed as means. “X-over”: crossover treatment with ropivacaine.
Table 2.
Brief Pain Inventory and Patient Global Impression of Change scale (mean values)
| Time Point Following: | Initial Catheter Insertion (Placebo Infusion) | Crossover Catheter Insertion * (Ropivacaine Infusion) | Initial | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time Point (Days): | 0 | 3 | 8 | 28 | 0 | 3 | 8 | 28 | |||
| Time Point (Weeks): | 12 | 12 | 52 | ||||||||
| N = | 3 | 3 | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 1 |
| PLP in previous 24 hours: | |||||||||||
| Least (NRS) | 1 | 3 | 2 | 3 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| Average (NRS) | 5 | 2 | 4 | 5 | 3 | 6 | 0 | 0 | 1 | 0 | 0 |
| Worst (NRS) | 7 | 4 | 5 | 7 | 5 | 9 | 0 | 0 | 1 | 1 | 0 |
| PLP at present time (NRS) | 4 | 2 | 3 | 6 | 3 | 5 | 0 | 0 | 0 | 0 | 0 |
| Relief provided by treatment in the last 24 hours (%/10) | 0 | 0 | 0 | 0 | 10 | 10 | 10 | 5 | 10 | ||
| Pain interferes with (0–10): § | |||||||||||
| General activity | 6 | 3 | 1 | 5 | 3 | 7 | 0 | 0 | 0 | 0 | 0 |
| Mood | 8 | 2 | 2 | 5 | 3 | 6 | 0 | 0 | 0 | 0 | 0 |
| Walking ability | 2 | 3 | 1 | 5 | 3 | 6 | 0 | 0 | 0 | 0 | 0 |
| Normal work | 3 | 4 | 3 | 5 | 3 | 7 | 0 | 0 | 0 | 0 | 0 |
| Relationships | 1 | 2 | 0 | 3 | 1 | 5 | 0 | 0 | 0 | 0 | 0 |
| Sleep | 6 | 4 | 2 | 8 | 5 | 7 | 0 | 0 | 0 | 0 | 0 |
| Enjoyment of life | 5 | 4 | 4 | 8 | 5 | 9 | 0 | 0 | 0 | 0 | 0 |
| Patient Global Impression of Change scale (1–7) Φ | 4 | 4 | 4 | 4 | 7 | 7 | 7 | 7 | 7 | ||
Optional second—or “crossover”—catheter insertion occurred between 12–16 weeks following the initial catheter insertion
PLP: Phantom limb pain
NRS: Numeric Rating Scale of pain (0–10; 10 equivalent to the worst imaginable pain)
0 equivalent to no interference; 10 equivalent to the maximum interference imaginable
1 equivalent to “very much worse”; 4 equivalent to “no change”; and 7 equivalent to “very much improved”
There were no catheter dislocations, protocol deviations, or adverse events.
Discussion
This randomized, double-masked, placebo-controlled, crossover pilot study suggests that a prolonged ambulatory CPNB may be a reliable treatment for intractable PLP. These results may have major clinical implications given the 1.6-million people currently living with an amputated limb in the United States alone;2 high prevalence of PLP following amputation (25–98%, depending on the study);6,10,27 decrease in quality-of-life associated with PLP; and the dearth of reliable treatments for this ailment.7,10,11 However, a large, randomized, controlled clinical trial is required to investigate treating intractable PLP with CPNB in order to draw definitive conclusions.
Published literature
Two case reports describe a total of three patients with PLP immediately following surgical amputation who were treated with multiple-day hospital-based CPNB. These patients experienced complete resolution of their PLP upon initiation of the CPNB, and no return of the phantom pain during the 7–12 month follow-up period.28 In an uncontrolled series of 19 patients also with PLP treated with hospital-based CPNB in the immediate post-amputation period, pain intensity decreased by approximately 50% at 1 and 6 months.29 However, to our knowledge, the present study is the first to systematically investigate CPNB as a possible intervention. Reports to date include CPNB exclusively in the immediate post-amputation period, as opposed to applying CPNB in patients with temporally-remote amputations who already suffer from intractable PLP.
Ambulatory CPNB
There is limited evidence that for surgical amputations, a preemptive local anesthetic infusion via an epidural catheter may decrease the incidence of subsequent PLP.30,31 However, treating chronic, intractable PLP with an epidural is problematic since an epidural infusion may not be provided for upper extremity amputation; and, even when used for lower extremity amputation, the infusion affects both limbs. Bilateral epidural effects require a low dose of local anesthetic to allow sensation in and ambulation using the uninjured limb; the consequence is inadequate analgesic effects in the amputated limb. Furthermore, epidural infusion often causes urinary retention and sympathectomy-induced postural hypotension;32 epidural analgesia thus usually requires hospitalization for close monitoring and possible intervention. The high cost of hospitalization for epidural infusion is a strong deterrent for both research and practical application.
In contrast, CPNB affects only the target peripheral nerves, may be provided for both upper and lower extremity trauma, has no undesirable side effects (although complications may occur, including local anesthetic toxicity, nerve injury, and infection), and may be provided on an ambulatory basis using small, portable pump(s) to infuse the local anesthetic.22 No healthcare facility admission is required for perineural local anesthetic infusion, enabling individuals to remain in the comfort of their own homes without the expense of a prolonged hospitalization. Recent technological advances in electronic, programmable infusion pumps permit extraordinarily precise flow rates with an infusion duration of over a week in a very small, light, portable pump.33 While ambulatory CPNB is no longer an “experimental” technique,34 to date it has been used nearly exclusively to treat acute pain immediately following surgery rather than chronic pain states.22
Relevance
Given chronic pain’s enormous costs to individuals and society as a whole—and the intractable nature of PLP—it is imperative that a reliable, effective treatment be developed. Moreover, the optimal current treatment for phantom pain—systemic opioids—is associated with significant risks such as respiratory depression, cognitive impairment,35 and addiction, especially in populations with co-existing psychopathology (e.g., combat stress, depression).36 In addition, alternative treatments/adjuvants such as gabapentinoids and tricyclic antidepressants also have significant drawbacks, such as impairing the ability to work and function. In contrast, CPNB has no addiction potential, produces no side effects, and does not influence cognitive functioning.
In conclusion, a prolonged ambulatory CPNB may be a reliable treatment for intractable PLP. The results of this pilot study suggest that a large, randomized clinical trial is warranted. Such a multicenter study has been funded by the United States Department of Defense through a 4-year Congressionally Directed Medical Research Program grant; will begin enrollment in 2013; and has an anticipated completion date of 2016.
Acknowledgments
Financial Support: Funding for this project provided by the National Institutes of Health grant GM077026 (P.I.: Dr. Ilfeld) from the National Institute of General Medical Sciences (Bethesda, Maryland); the Clinical and Translational Research Institute, University of California, San Diego (San Diego, California), with funding provided by the National Institutes of Health National Center for Research Resources grant UL1RR031980; the University of California Academic Senate (P.I.: Dr. Ilfeld; San Diego, California); the Department of Anesthesiology, University of California San Diego (San Diego, California); and Summit Medical (Salt Lake City, Utah) provided both an unrestricted research grant and the infusion pumps used in this investigation. This company had no input into any aspect of study conceptualization, design, and implementation; data collection, analysis and interpretation; or manuscript preparation. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the funding entities.
Footnotes
Conflict of Interest: None.
Prior Presentation: Presented, in part, as a scientific abstract at the annual meeting of the American Society of Anesthesiologists in Washington D.C. (United States), October 13-17, 2012.
References
- 1.Bloomquist T. Amputation and phantom limb pain: a pain-prevention model. AANA J. 2001;69:211–7. [PubMed] [Google Scholar]
- 2.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422–9. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Nikolajsen L, Jensen TS. Phantom limb pain. Br J Anaesth. 2001;87:107–16. doi: 10.1093/bja/87.1.107. [DOI] [PubMed] [Google Scholar]
- 4.Hazelgrove JF, Rogers PD. Phantom limb pain--a complication of lower extremity wound management. Int J Low Extrem Wounds. 2002;1:112–24. doi: 10.1177/1534734602001002006. [DOI] [PubMed] [Google Scholar]
- 5.Nikolajsen L, Ilkjaer S, Kroner K, Christensen JH, Jensen TS. The influence of preamputation pain on postamputation stump and phantom pain. Pain. 1997;72:393–405. doi: 10.1016/s0304-3959(97)00061-4. [DOI] [PubMed] [Google Scholar]
- 6.Sherman RA, Sherman CJ. Prevalence and characteristics of chronic phantom limb pain among American veterans. Results of a trial survey. Am J Phys Med. 1983;62:227–38. [PubMed] [Google Scholar]
- 7.Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84–92. doi: 10.1097/00002508-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Sherman RA, Sherman CJ, Gall NG. A survey of current phantom limb pain treatment in the United States. Pain. 1980;8:85–99. doi: 10.1016/0304-3959(80)90092-5. [DOI] [PubMed] [Google Scholar]
- 9.Sherman RA. Published treatments of phantom limb pain. Am J Phys Med. 1980;59:232–44. [PubMed] [Google Scholar]
- 10.Sherman RA, Sherman CJ, Parker L. Chronic phantom and stump pain among American veterans: results of a survey. Pain. 1984;18:83–95. doi: 10.1016/0304-3959(84)90128-3. [DOI] [PubMed] [Google Scholar]
- 11.Sherman RA. Phantom limb pain. Mechanism-based management. Clin Podiatr Med Surg. 1994;11:85–106. [PubMed] [Google Scholar]
- 12.Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959–64. doi: 10.1016/S0140-6736(99)01307-0. [DOI] [PubMed] [Google Scholar]
- 13.Flor H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002;1:182–9. doi: 10.1016/s1474-4422(02)00074-1. [DOI] [PubMed] [Google Scholar]
- 14.Nikolajsen L, Ilkjaer S, Jensen TS. Relationship between mechanical sensitivity and postamputation pain: a prospective study. Eur J Pain. 2000;4:327–34. doi: 10.1053/eujp.2000.0194. [DOI] [PubMed] [Google Scholar]
- 15.Flor H, Elbert T, Knecht S, Wienbruch C, Pantev C, Birbaumer N, Larbig W, Taub E. Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature. 1995;375:482–4. doi: 10.1038/375482a0. [DOI] [PubMed] [Google Scholar]
- 16.Merzenich MM, Nelson RJ, Stryker MP, Cynader MS, Schoppmann A, Zook JM. Somatosensory cortical map changes following digit amputation in adult monkeys. J Comp Neurol. 1984;224:591–605. doi: 10.1002/cne.902240408. [DOI] [PubMed] [Google Scholar]
- 17.Birbaumer N, Lutzenberger W, Montoya P, Larbig W, Unertl K, Topfner S, Grodd W, Taub E, Flor H. Effects of regional anesthesia on phantom limb pain are mirrored in changes in cortical reorganization. J Neurosci. 1997;17:5503–8. doi: 10.1523/JNEUROSCI.17-14-05503.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seminowicz DA, Wideman TH, Naso L, Hatami-Khoroushahi Z, Fallatah S, Ware MA, Jarzem P, Bushnell MC, Shir Y, Ouellet JA, Stone LS. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. The J Neurosci. 2011;31:7540–50. doi: 10.1523/JNEUROSCI.5280-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mariano ER, Loland VJ, Sandhu NS, Bellars RH, Bishop ML, Afra R, Ball ST, Meyer RS, Maldonado RC, Ilfeld BM. Ultrasound guidance versus electrical stimulation for femoral perineural catheter insertion. J Ultrasound Med. 2009;28:1453–60. doi: 10.7863/jum.2009.28.11.1453. [DOI] [PubMed] [Google Scholar]
- 20.Mariano ER, Cheng GS, Choy LP, Loland VJ, Bellars RH, Sandhu NS, Bishop ML, Lee DK, Maldonado RC, Ilfeld BM. Electrical stimulation versus ultrasound guidance for popliteal-sciatic perineural catheter insertion: a randomized controlled trial. Reg Anesth Pain Med. 2009;34:480–85. doi: 10.1097/AAP.0b013e3181ada57a. [DOI] [PubMed] [Google Scholar]
- 21.Mariano ER, Loland VJ, Bellars RH, Sandhu NS, Bishop ML, Abrams RA, Meunier MJ, Maldonado RC, Ferguson EJ, Ilfeld BM. Ultrasound guidance versus electrical stimulation for infraclavicular brachial plexus perineural catheter insertion. J Ultrasound Med. 2009;28:1211–8. doi: 10.7863/jum.2009.28.9.1211. [DOI] [PubMed] [Google Scholar]
- 22.Ilfeld BM, Enneking FK. Continuous peripheral nerve blocks at home: A review. Anesth Analg. 2005;100:1822–33. doi: 10.1213/01.ANE.0000151719.26785.86. [DOI] [PubMed] [Google Scholar]
- 23.Dworkin RH, Turk DC, Peirce-Sandner S, Baron R, Bellamy N, Burke LB, Chappell A, Chartier K, Cleeland CS, Costello A, Cowan P, Dimitrova R, Ellenberg S, Farrar JT, French JA, Gilron I, Hertz S, Jadad AR, Jay GW, Kalliomaki J, Katz NP, Kerns RD, Manning DC, McDermott MP, McGrath PJ, Narayana A, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Reeve BB, Rhodes T, Sampaio C, Simpson DM, Stauffer JW, Stucki G, Tobias J, White RE, Witter J. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain. 2010;149:177–93. doi: 10.1016/j.pain.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 24.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–38. [PubMed] [Google Scholar]
- 25.Manchikanti L, Singh V. Managing phantom pain. Pain Physician. 2004;7:365–75. [PubMed] [Google Scholar]
- 26.Ehde DM, Czerniecki JM, Smith DG, Campbell KM, Edwards WT, Jensen MP, Robinson LR. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Archives of physical medicine and rehabilitation. 2000;81:1039–44. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- 27.Smith DG, Ehde DM, Legro MW, Reiber GE, del Aguila M, Boone DA. Phantom limb, residual limb, and back pain after lower extremity amputations. Clinical orthopaedics and related research. 1999:29–38. doi: 10.1097/00003086-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Lierz P, Schroegendorfer K, Choi S, Felleiter P, Kress HG. Continuous blockade of both brachial plexus with ropivacaine in phantom pain: a case report. Pain. 1998;78:135–7. doi: 10.1016/S0304-3959(98)00128-6. [DOI] [PubMed] [Google Scholar]
- 29.Schley M, Topfner S, Wiech K, Schaller HE, Konrad CJ, Schmelz M, Birbaumer N. Continuous brachial plexus blockade in combination with the NMDA receptor antagonist memantine prevents phantom pain in acute traumatic upper limb amputees. Eur J Pain. 2007;11:299–308. doi: 10.1016/j.ejpain.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 30.Rathmell JP, Kehlet H. Do we have the tools to prevent phantom limb pain? Anesthesiology. 2011;114:1021–4. doi: 10.1097/ALN.0b013e31820fc80d. [DOI] [PubMed] [Google Scholar]
- 31.Karanikolas M, Aretha D, Tsolakis I, Monantera G, Kiekkas P, Papadoulas S, Swarm RA, Filos KS. Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: a prospective, randomized, clinical trial. Anesthesiology. 2011;114:1144–54. doi: 10.1097/ALN.0b013e31820fc7d2. [DOI] [PubMed] [Google Scholar]
- 32.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88–92. doi: 10.1097/00000539-199807000-00019. [DOI] [PubMed] [Google Scholar]
- 33.Ilfeld BM, Morey TE, Enneking FK. New portable infusion pumps: Real advantages or just more of the same in a different package? Reg Anesth Pain Med. 2004;29:371–6. doi: 10.1016/j.rapm.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113:904–25. doi: 10.1213/ANE.0b013e3182285e01. [DOI] [PubMed] [Google Scholar]
- 35.Kendall SE, Sjogren P, Pimenta CA, Hojsted J, Kurita GP. The cognitive effects of opioids in chronic non-cancer pain. Pain. 2010;150:225–30. doi: 10.1016/j.pain.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 36.Solanki DR, Koyyalagunta D, Shah RV, Silverman SM, Manchikanti L. Monitoring opioid adherence in chronic pain patients: assessment of risk of substance misuse. Pain Physician. 2011;14:E119–31. [PubMed] [Google Scholar]


