Abstract
Context
No consensus exists for adjusting inhaled corticosteroid therapy in patients with asthma. Approaches include adjustment at outpatient visits guided by physician assessment of asthma control (symptoms, rescue therapy, pulmonary function), based on exhaled nitric oxide, or on a day-to-day basis guided by symptoms.
Objective
To determine if adjustment of inhaled corticosteroid therapy based on exhaled nitric oxide or day-to-day symptoms is superior to guideline-informed, physician assessment–based adjustment in preventing treatment failure in adults with mild to moderate asthma.
Design, Setting, and Participants
A randomized, parallel, 3-group, placebo-controlled, multiply-blinded trial of 342 adults with mild to moderate asthma controlled by low-dose inhaled corticosteroid therapy (n=114 assigned to physician assessment–based adjustment [101 completed], n=115 to biomarker-based [exhaled nitric oxide] adjustment [92 completed], and n=113 to symptom-based adjustment [97 completed]), the Best Adjustment Strategy for Asthma in the Long Term (BASALT) trial was conducted by the Asthma Clinical Research Network at 10 academic medical centers in the United States for 9 months between June 2007 and July 2010.
Interventions
For physician assessment–based adjustment and biomarker-based (exhaled nitric oxide) adjustment, the dose of inhaled corticosteroids was adjusted every 6 weeks; for symptom-based adjustment, inhaled corticosteroids were taken with each albuterol rescue use.
Main Outcome Measure
The primary outcome was time to treatment failure.
Results
There were no significant differences in time to treatment failure. The 9-month Kaplan-Meier failure rates were 22% (97.5% CI, 14%-33%; 24 events) for physician assessment–based adjustment, 20% (97.5% CI, 13%-30%; 21 events) for biomarker-based adjustment, and 15% (97.5% CI, 9%-25%; 16 events) for symptom-based adjustment. The hazard ratio for physician assessment–based adjustment vs biomarker-based adjustment was 1.2 (97.5% CI, 0.6-2.3). The hazard ratio for physician assessment–based adjustment vs symptom-based adjustment was 1.6 (97.5% CI, 0.8-3.3).
Conclusion
Among adults with mild to moderate persistent asthma controlled with low-dose inhaled corticosteroid therapy, the use of either biomarker-based or symptom-based adjustment of inhaled corticosteroids was not superior to physician assessment–based adjustment of inhaled corticosteroids in time to treatment failure.
Trial Registration
clinicaltrials.gov Identifier: NCT00495157
Asthma is managed by consensus guidelines.1,2 Disease activity varies daily, seasonally, and episodically, presumably related to airway inflammation.3 Accordingly, asthma management requires periodic dose adjustments of controller medications, particularly inhaled corticosteroids. Adjustments have been based on (1) physician assessment of symptoms, activity limitation, rescue albuterol use, lung function, and exacerbations at usual office or clinic visits,1 (2) a biomarker of disease activity (eg, exhaled nitric oxide, sputum eosinophils, methacholine responsiveness),4-10 or (3) the occurrence of symptoms on a day-to-day basis.11-13
We hypothesized that adjustment of inhaled corticosteroids based on symptoms or exhaled nitric oxide would be superior to adjustment based on physician assessment. Our purpose was to ascertain whether symptom-based adjustment (SBA) of inhaled corticosteroids might be a simple and effective strategy for managing asthma therapy in a population of patients with asthma commonly seen in primary care settings, and to ascertain if biomarker-based adjustment (BBA) was superior to physician assessment–based adjustment (PABA).
METHODS
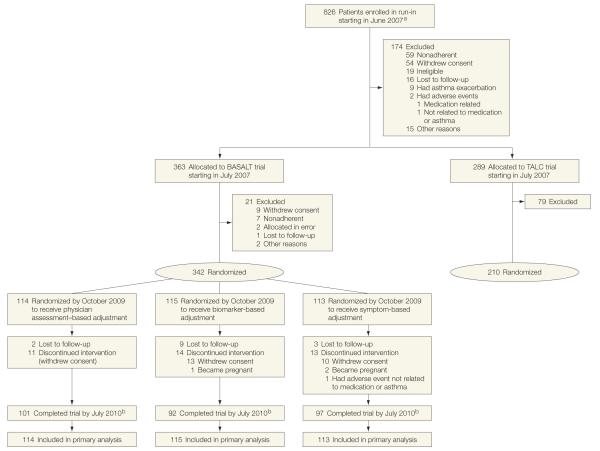
The Best Adjustment Strategy for Asthma in the Long Term (BASALT) randomized trial included 342 participants with mild to moderate persistent asthma; these individuals were recruited cooperatively with a concurrent Asthma Clinical Research Network (ACRN) trial14 (Figure 1). The ACRN data and safety monitoring board and clinical center institutional review boards approved the protocol and consent form; all participants signed a written consent form. Race was self-reported as white, black, or other, and ethnicity as Latino or non-Latino, and recorded to assess representativeness in accordance with National Heart, Lung, and Blood Institute guidelines. All participants had a physician diagnosis of asthma, and either reversible airflow limitation (≥12% improvement in forced expiratory volume in the first second of expiration [FEV1] after 360 μg of albuterol), or airway hyperresponsiveness (provocative concentration of methacholine [<8 mg/mL] causing a 20% drop in FEV1).
Figure 1.
Participant Allocation in BASALT and TALC Trials
Patients were allocated to the Best Adjustment Strategy for Asthma in the Long Term (BASALT) trial based on achievement of forced expiratory volume in the first second of expiration of greater than 70% during the run-in period and concomitant control of symptoms (score of 0 or 1 on each of 3 questions on the Asthma Evaluation Questionnaire; eSupplement at http://www.jama.com). Patients whose lung function was less than 70% of predicted or had quantitatively greater symptom burden were allocated to the Tiotropium Bromide as an Alternative to Increased Inhaled Glucocorticoid in Patients Inadequately Controlled on a Lower Dose of Inhaled Corticosteroid (TALC) trial, which was a concurrently recruited Asthma Clinical Research Network trial.14
aDetails for those screened but ineligible were not collected.
bDropouts were included as censored observations.
We evaluated these approaches to dose adjustment of inhaled corticosteroids in a 3-group trial during 9 months in adults with mild to moderate asthma that was well controlled with low-dose inhaled corticosteroids. The dose of inhaled corticosteroids was adjusted by (1) a strategy based on National Heart, Lung, and Blood Institute guidelines (PABA group), (2) measurement of exhaled nitric oxide (BBA group), or (3) occurrence of symptoms prompting rescue use of albuterol (SBA group). In the first 2 strategy groups, dose adjustments of inhaled corticosteroids were made at the time of clinic visits (every 6 weeks); in the third group, dose adjustment of inhaled corticosteroids was performed by matching inhaled steroid use on a puff-per-puff basis with as-needed albuterol use.
We selected these strategy groups because (1) PABA therapy represents standard care in the United States, (2) BBA in adults using exhaled nitric oxide may achieve good asthma control with reduced total use of inhaled corticosteroids,5 and (3) SBA produces outcomes equivalent to daily controller therapy in patients with mild asthma.11,12 We sought to determine if SBA would be successful in patients with more severe asthma than in our previous study of patients with mild persistent asthma.11
Patients were treated with 2 puffs twice daily of beclomethasone HFA (40 μg/puff) during the run-in period, and if their asthma was acceptably controlled (a score of 0 or 1 on each of 3 questions on the Asthma Evaluation Questionnaire [eSupplement at http://www.jama.com] and predicted bronchodilator FEV1 >70%), they were enrolled in the BASALT trial. This approach yielded a population of participants with well or partially controlled asthma, but excluded those with poorly controlled asthma. During the prerandomization period, patients were given 3 inhalers coded as A, B, and C. Inhaler A contained beclomethasone HFA (40 μg/puff) and inhalers B and C contained placebo. An albuterol inhaler was provided for use as needed for asthma symptoms. Participants were instructed to use 2 puffs twice daily from inhalers A and B, and to use 2 puffs from inhaler C each time they used 2 puffs of albuterol for symptom relief. All metered dose inhalers were equipped with a Doser device (Meditrack Products) to measure adherence during the trial. Patients who demonstrated at least 75% adherence were randomized to 1 of 3 adjustment strategies: PABA, BBA, or SBA.
Beclomethasone HFA was provided at a dosage of 2 puffs twice daily (40 μg/puff) before randomization, corresponding to level 3 treatment. Hence, inhaled corticosteroid therapy could be intensified or deintensified during the trial. Following randomization, beclomethasone HFA was contained only in inhaler A for PABA participants, only in inhaler B for BBA participants, and only in inhaler C for SBA participants. Thereafter, inhaler A was adjusted by an investigator according to guidelines closely resembling the National Heart, Lung, and Blood Institute National Asthma Expert Panel,1 and inhaler B was adjusted according to exhaled nitric oxide measurements. Participants were instructed to use inhaler C only at the time of albuterol use. Subsequent visits occurred 2, 4, 6, 12, 18, 24, 30, and 36 weeks after randomization, at which times outcomes were measured (the BASALT Protocol appears at http://www.acrn.org/BASALT.html).
Our primary outcome was time to first treatment failure, a clinically important worsening of asthma (BOX).11 Hospitalizations, urgent care visits, and other adverse events were recorded at the time of scheduled clinic visits. Spirometry, albuterol reversibility, methacholine responsiveness, sputum eosinophils, daytime and nighttime symptom and rescue β-agonist diaries, Asthma Control Questionnaire, Asthma Symptom Utility Index, and Asthma Quality-of-Life Questionnaire were measured as in previous ACRN trials11 as secondary outcomes. We analyzed the frequency of exacerbations (treatment failures requiring systemic corticosteroids, an unscheduled physician contact for asthma, or severe symptoms linked to lung function decline11), and quantified use of inhaled corticosteroids. The BASALT protocol at http://www.acrn.org/BASALT.html details the frequency and timing of each outcome measure.
Box. Treatment Failure Criteria.
Asthma exacerbation
unscheduled medical contact for increased asthma symptoms that results in use of oral corticosteroids, increased inhaled corticosteroids, or additional medications for asthma.
At-home measurements
any of the following 3 criteria, when not associated with the increased asthma symptoms, satisfies treatment failure criteria:
Prebronchodilator am peak expiratory flow (PEF) of less than 65% of baseline on 2 consecutive mornings, scheduled measurements.
Postbronchodilator PEF of less than 80% of baseline despite 60 minutes of rescue β-agonist treatment. Postbronchodilator PEF may be taken at any time of day.
An increase in albuterol use of more than 8 puffs per 24 hours over baseline use for a period of 48 hours, or more than 16 puffs per 24 hours for more than 48 hours.
In-clinic measurements
Prebronchodilator forced expiratory volume in the first second of expiration (FEV1) values on 2 consecutive sets of spirometric determinations measured 24 to 72 hours apart that are less than 80% of the baseline prebronchodilator value (baseline value for adherence period: FEV1 value at visit 3; baseline for randomization period: FEV1 value at visit 4). All participants found to have an FEV1 of less than 80% of baseline at any center visit but who are not considered to meet treatment failure or exacerbation criteria must be seen again within 72 hours to have FEV1 measured.
Physician judgment for patient safety.
Patient dissatisfaction with asthma control achieved by study regimen.
Requirement for open-label inhaled corticosteroids or another (nonsystemic corticosteroid) new asthma medication (eg, montelukast) without the addition of systemic corticosteroids.
The BASALT trial was a parallel, 3-group trial with 2 primary comparisons: PABA vs SBA and PABA vs BBA. Based on proposed enrollment, we had 87% power to detect a 60% reduction in treatment failure rate (30% vs 12%), as previously observed,5 for an overall α level of .05 (.025 for each primary comparison), and a postrandomization dropout rate of 15%. The comparison between SBA and BBA was exploratory.
To evaluate time to first treatment failure, Kaplan-Meier survival plots and logrank tests were generated. A Cox proportional hazards regression model compared time to first treatment failure with adjustment for covariates of center and baseline FEV1. To accommodate multiple treatment failures, a repeated-measures proportional hazards regression model was fit to time to treatment failure, with adjustment for center and baseline FEV1. Methods for secondary analyses are described in the BASALT protocol.
All analyses followed intention-to-treat principles and incorporated all available data. The statistical models and analyses for the primary and secondary outcomes assumed missing data were missing at random. Because 2 primary comparisons were of interest, PABA vs BBA and PABA vs SBA, comparisons were evaluated for statistical significance at the .025 level, as was the secondary comparison of BBA vs SBA, for both primary and secondary outcomes. Statistical tests were 2-sided and all statistical analyses were performed using SAS version 9.3 (SAS Institute Inc).
RESULTS
Randomization allocated 114 to PABA, 115 to BBA, and 113 to SBA, with no important differences among the groups at baseline. Participant characteristics were consistent with mild to moderate persistent asthma: mean FEV1 was 86% predicted, provocative concentration of methacholine (<3 mg/mL) causing a 20% drop in FEV1, and mean Asthma Control Questionnaire score was 0.75 (Table 1). Details regarding dosing adjustment of inhaled corticosteroids appear in Table 2. The dropout rate during the trial did not differ significantly among groups (20% for BBA vs 11% for PABA vs 14% for SBA). Median adherence in all groups exceeded 95%.
Table 1.
Demographics of Participants
| No. (%) by Adjustment Strategy | ||||
|---|---|---|---|---|
|
|
P Value | |||
| Male sex | 42 (36.8) | 33 (28.7) | 30 (26.5) | .21a |
|
| ||||
| Race/ethnicity | ||||
|
| ||||
| American Indian/Alaska Native | 0 | 0 | 1 (0.9) |
|
|
| ||||
| Asian/Pacific Islander | 1 (0.9) | 2 (1.7) | 10 (8.8) | |
|
| ||||
| Black | 24 (21.1) | 28 (24.3) | 17 (15.0) | |
|
| ||||
| White | 76 (66.7) | 71 (61.7) | 69 (61.1) | |
|
| ||||
| Hispanic | 11 (9.6) | 13 (11.3) | 14 (12.4) | |
|
| ||||
| Otherb | 2 (1.8) | 1 (0.9) | 2 (1.8) | |
|
| ||||
| Skin test atopic statusc | 97 (85.1) | 99 (86.1) | 93 (82.3) | .70a |
|
| ||||
| Mean (SD) | ||||
| Age at visit 1, y | 34.2 (11.9) | 34.8 (11.3) | 36.0 (12.2) | .52d |
|
| ||||
| Duration of asthma (since first diagnosed), y | 20.4 (10.4) | 18.8 (10.3) | 21.3 (12.1) | .21d |
|
| ||||
| Height at visit 1, cm | 168.7 (8.8) | 168.4 (9.1) | 168.1 (9.1) | .89d |
|
| ||||
| Weight at visit 1, kg | 80.2 (22.8) | 82.7 (22.7) | 77.1 (20.4) | .17d |
|
| ||||
| Body mass index at visit 1e | 28.2 (7.9) | 29.0 (7.3) | 27.1 (6.2) | .14d |
|
| ||||
| Prebronchodilator FEV1 At visit 4, L |
3.03 (0.72) | 2.94 (0.74) | 2.90 (0.69) | .34d |
|
| ||||
| % Predicted at visit 4 | 87.7 (12.1) | 86.3 (10.4) | 85.6 (11.0) | .37d |
|
| ||||
| FEV1 at visit 3 Albuterol (4 puffs) reversal, % |
9.6 (6.5) | 9.6 (5.5) | 9.2 (5.8) | .81d |
|
| ||||
| Postalbuterol (4 puffs), L | 3.32 (0.75) | 3.21 (0.81) | 3.16 (0.71) | .31d |
|
| ||||
| am Peak flow 2-week average prior to visit 4, L/min | 460.1 (111.3) | (n = 114) 442.8 (117.5) |
436.9 (104.5) | .26d |
|
| ||||
| pm Peak flow 2-week average prior to visit 4, L/min | 466.5 (112.7) | (n = 114) 445.3 (118.2) |
441.3 (104.0) | .19d |
|
| ||||
| ACQ average score at visit 4f | 0.72 (0.50) | 0.79 (0.54) | 0.73 (0.49) | .57d |
|
| ||||
| AQLQ average score at visit 3g | (n = 112) 6.27 (0.76) |
6.16 (0.77) | 6.25 (0.72) | .48d |
|
| ||||
| ASUI average score at visit 4h | 0.90 (0.10) | 0.88 (0.12) | 0.90 (0.10) | .39d |
|
| ||||
| Exhaled nitric oxide at visit 4, ppbi | (n = 108) 21.38 (0.62) |
(n = 114) 18.88 (0.66) |
(n = 110) 20.78 (0.54) |
.28j |
|
| ||||
| Imputed PC20 at visit 4, mg/mLi | (n = 99) 3.50 (1.43) |
(n = 100) 2.37 (1.54) |
(n = 98) 2.64 (1.27) |
.14j |
|
| ||||
| IgE at visit 2, IU/mLi | (n = 107) 130.0 (1.5) |
(n = 105) 118.9 (1.4) |
(n = 101) 133.8 (1.4) |
.83i |
|
| ||||
| Median (IQR) | ||||
| Two-week average prior to visit 4 Daily symptomsk |
0.05 (0-0.14) | (n = 114) 0.06 (0.01-0.21) |
0.05 (0-0.20) | .26l |
|
| ||||
| Albuterol rescue use (puffs) | 0.04 (0-0.29) | (n = 114) 0.07 (0-0.43) |
(n = 112) 0 (0-0.31) |
.42l |
|
| ||||
| Exhaled breath condensate pH at visit 4 | 8.52 (8.25-8.64) | (n = 110) 8.48 (8.29-8.60) |
(n = 107) 8.47 (8.21-8.61) |
.83l |
|
| ||||
| Sputum eosinophils at visit 3 | (n = 79) 0.40 (0-1.20) |
(n = 67) 0.20 (0-0.80) |
(n = 76) 0.40 (0-1.40) |
.09l |
|
| ||||
| Blood eosinophils at visit 2, /mm3 | (n = 111) 132.0 (100.0-222.0) |
(n = 108) 178.5 (100.0-300.0) |
(n = 108) 169.0 (100.0-224.0) |
.17l |
Abbreviations: ACQ, Asthma Control Questionnaire; AQLQ, Asthma Quality-of-Life Questionnaire; ASUI, Asthma Symptom Utility Index; FEV1, forced expiratory volume in the first second of expiration; IgE, immunoglobulin E; MID, minimal clinically important difference; PC20, provocative concentration of methacholine (<8 mg/mL) causing a 20% drop in FEV1.
Calculated using the Chisq test for differences in proportions among the 3 treatment groups.
The National Institutes of Health did not require additional specification of other so this information was not collected.
At least 1 positive skin test, using the prick-puncture method, and a panel of common aeroallergens.
Calculated using the analysis of variance F test for differences among the 3 treatment groups.
Calculated as weight in kilograms divided by height in meters squared.
A higher score indicates worse asthma control (score range: 0-6; MID: 0.5).15
A higher score indicates a better quality of life (score range: 1-7; MID: 0.5).16
A higher score indicates better asthma control (score range: 0-1; MID: unknown, but a difference of 0.3 is suggested to distinguish between mild to moderate and moderate to severe asthma).
Geometric mean coefficient of variation reported.
Calculated using the analysis of variance F test for differences among the 3 treatment groups on a log scale.
A higher score indicates a greater severity of symptoms (score range: 0-3).
Calculated using the Kruskal-Wallis test for differences among the 3 treatment groups.
Table 2.
Inhaled Steroid Dosing Adjustment
| Control Status | Inhaler Dose Change | |
|---|---|---|
| Physician assessment-based adjustment (inhaler A)a FEV1 ≥85% at baseline Plus symptoms in past 2 wk ≤2 d/wk (all AEQ scores of 0) |
Well controlled | Down 1 level |
| Plus symptoms no worse than mild (AEQ scores of 0 or 1 on each question) | Controlled | Maintain current level |
| FEV1 <85% at baseline, moderate symptoms (any AEQ score of 2 or 3), or meets criteria for treatment failure |
Undercontrolled | Up 1 level |
| Biomarker-based adjustment (inhaler B) Fraction of exhaled nitric oxide, ppb <22 |
Well controlled | Down 1 level |
| 22-35 | Controlled | Maintain current level |
| >35 | Undercontrolled | Up 1 level |
| Inhaled corticosteroids dose levelb | Dose, μg/d | Frequency |
| 1 | None | |
| 2 | 80 (2 puffs) | Once daily (am) |
| 3 | 160 (2 puffs) | Twice daily |
| 4 | 320 (4 puffs) | Twice daily |
| 5 | 640 (8; 4 puffs at double strength) | Twice daily |
Abbreviations: AEQ, Asthma Evaluation Questionnaire; FEV1, forced expiratory volume in the first second of expiration.
Physician was defined as the principal investigator or his/her physician designee, who used a clinical assessment tool similar to the US National Heart, Lung, and Blood Institute guidelines.
All participants began the trial at level 3, from which therapy could be intensified or deintensified. The dose level was the prescribed therapy intensity.
Time to treatment failure, our primary outcome, did not differ significantly among the 3 treatment strategies. The 9-month Kaplan-Meier failure rates were 22% (97.5% CI, 14% to 33%; 24 events) for PABA, 20% (97.5% CI, 13% to 30%; 21 events) for BBA, and 15% (97.5% CI, 9% to 25%; 16 events) for SBA. The hazard ratio (HR) for PABA vs BBA was 1.2 (97.5% CI, 0.6 to 2.3; log-rank P=.68); PABA vs SBA, 1.6 (97.5% CI, 0.8 to 3.3; P=.18); and BBA vs SBA, 1.4 (97.5% CI, 0.6 to 2.9; P = .35) (Figure 2). The 9-month Kaplan-Meier treatment failure rates resulted in average differences of 2 (range: −10 to 14) percentage points for PABA vs BBA and 7 (range: −5 to 19) percentage points for PABA vs SBA (ie, more events for PABA).
Figure 2.
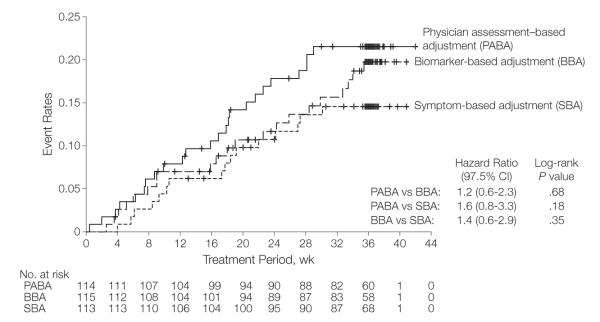
Time to First Treatment Failure
No significant differences among the 3 treatment groups were seen. A confirmatory truncated analysis was performed with truncation at day 258 (week 37), beyond which less than 10% of the study population was still in follow-up. These results confirm the primary analysis with a pairwise P value for PABA vs BBA of .64; PABA vs SBA, P=.15; and BBA vs SBA, P=.33. The hazard ratios and 97.5% confidence intervals were identical to 1 decimal place. Short vertical bars on the curves indicate censored data.
Treatment failure rates were not different among groups when multiple episodes of treatment failure were included (0.43 [97.5% CI, 0.23-0.64] events/person-year for PABA vs 0.27 [97.5% CI, 0.14-0.39] events/person-year for BBA and 0.25 [97.5% CI, 0.10-0.39] events/person-year for SBA; P=.21). The HR for PABA vs BBA was 1.5 (97.5% CI, 0.8-2.9); PABA vs SBA, 1.7 (97.5% CI, 0.9-3.3); and BBA vs SBA, 1.2 (97.5% CI, 0.6-2.3).
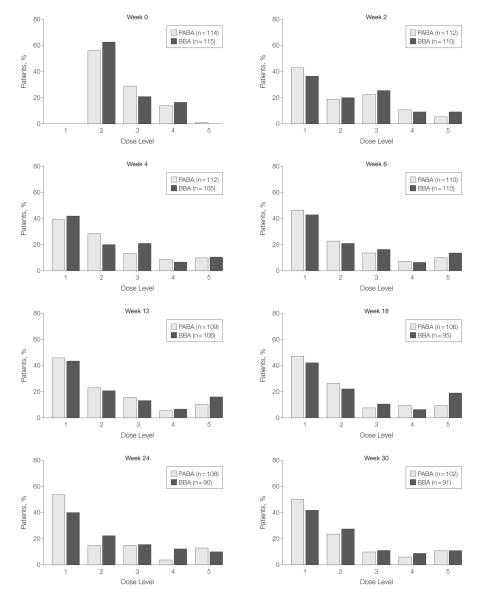
Mean monthly beclomethasone use was higher in both the PABA (1610 μg) and BBA (1617 μg) groups than in the SBA group (832 μg; P=.01 for both comparisons). The frequency distribution of prescribed inhaled corticosteroid doses did not differ between the PABA and BBA groups (P = .99; Figure 3). During the study, participants tended to require less inhaled corticosteroids, with approximately 40% of the participants exhibiting acceptable asthma control while taking no beclomethasone during 1 or more visits. The secondary outcomes appear in eTable 1 at http://www.jama.com.
Figure 3.
Dose Level Distribution of Prescribed Inhaled Corticosteroids
No significant differences in dose distribution were observed between the biomarker-based adjustment (BBA) and the physician assessment–based adjustment (PABA) strategies. Because there was no regularly scheduled dose in the symptom-based adjustment group, equivalent dose distributions cannot be reliably calculated for participants randomized to this group. The corresponding dose and frequency for the dose levels appear in Table 2.
Few days were lost from school or work in our trial (0.25 [97.5% CI, 0.03-0.47] days/person-year for PABA, 0.46 [97.5% CI, 0.08-0.84] days/person-year for BBA, and 0.11 [97.5% CI, 0-0.23] days/person-year for SBA). However, the odds ratio (OR) of missing days was greater for BBA vs either PABA (OR, 2.0 [97.5% CI, 1.1-3.8]; P=.01) or SBA (OR, 4.3 [97.5% CI, 1.9-9.6]; P<.001).
Asthma exacerbation (including multiple episodes) rates did not differ among the treatment groups (0.23 [97.5% CI, 0.10-0.37] events/person-year for PABA vs 0.21 [97.5% CI, 0.10-0.32] events/person-year for BBA and 0.12 [97.5% CI, 0.03-0.21] events/person-year for SBA) (PABA vs BBA, P=.89; PABA vs SBA, P=.11; and BBA vs SBA, P=.13). The HR was 1.1 (97.5% CI, 0.4-2.8) for PABA vs BBA; 2.0 (97.5% CI, 0.8-5.4) for PABA vs SBA; and 1.9 (97.5% CI, 0.7-4.9) for BBA vs SBA.
The mean proportion of treatment failures that progressed to exacerbations did not differ significantly among treatment groups (PABA: 0.58 [SD, 0.46]; BBA: 0.79 [SD, 0.41]; and SBA: 0.48 [SD, 0.47]; P=.13). The comparison between PABA and BBA yielded a pairwise P value of .08; PABA vs SBA, P=.65; and BBA vs SBA, P=.05.
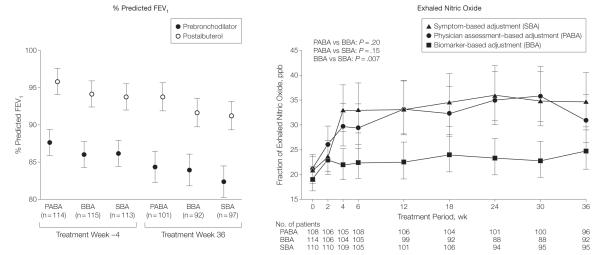
Measures of lung function and asthma symptoms were not significantly different among the groups (Figure 4, eTable 1). Airway responsiveness worsened in the PABA group compared with the BBA group (P<.006; eTable 1), but did not differ when the SBA group was compared with the other 2 groups.
Figure 4.
Mixed-Model Treatment Means of Pulmonary Function and Exhaled Nitric Oxide
The data markers indicate geometric means and the error bars indicate 97.5% confidence intervals. FEV1 indicates forced expiratory volume in the first second of expiration. No significant differences in prebronchodilator FEV1, postbronchodilator FEV1, or albuterol-induced reversibility were observed. The BBA group had very little change in exhaled nitric oxide over the course of the trial because dosing of inhaled corticosteroids was adjusted to control exhaled nitric oxide. The SBA group showed a small and statistically significant increase in exhaled nitric oxide over the course of the trial vs the BBA group (P=.007). Level of exhaled nitric oxide in the SBA group did not differ significantly from the PABA group (P=.15).
Exhaled nitric oxide and sputum eosinophils were not different in the 3 treatment groups at baseline. The increase in exhaled nitric oxide was significantly greater in the SBA group than in the BBA group (P=.007), but did not differ between the BBA and PABA groups or between the SBA and PABA groups (Figure 4). Serious adverse events were uncommon (eTable 2).
Predictors of time to treatment failure were race (P=.001) and albuterol reversibility (P=.004). Hispanic (OR, 3.6; 95% CI, 1.8-7.0) and black (OR, 2.1; 95% CI, 1.2-4.0) participants had significantly greater risk for first treatment failure than did non-Hispanic white participants (P<.02 for both comparisons). A multivariable model confirmed these same predictors for multiple treatment failures. Notably, baseline FEV1, peak flow, symptoms, exhaled nitric oxide, and sputum eosinophils did not predict treatment failure.
There was a significant association of race and efficacy with the SBA and PABA groups (eFigure). Among Hispanic participants, treatment failure was better prevented in the PABA group than in the SBA group, which contrasted with non-Hispanic whites. The HR for treatment failure with PABA vs SBA among non-Hispanic whites was 4.50 (95% CI, 1.42-14.30) and among Hispanics it was 0.30 (95% CI, 0.04-1.80) (comparing HRs yielded P=.01).
We observed an interaction of season with treatment failure in the PABA participants, in whom treatment failure increased 4-fold during autumn, significantly more than in the BBA and SBA groups (P=.02; Figure 5).
Figure 5.
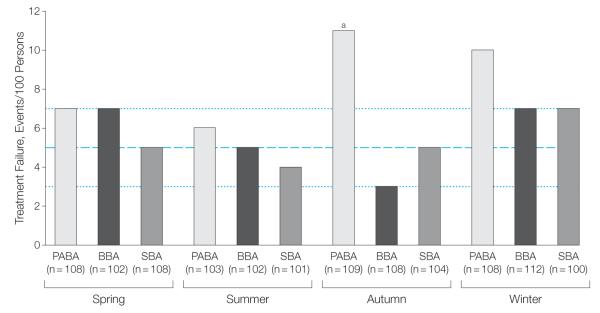
Treatment Failure by Season
Spring included March, April, and May; summer, June, July, and August; autumn: September, October, and November; and winter: December, January, and February. The dotted lines indicate the lower and upper number of all treatment failure events in all groups across the 4 seasons (range, 3-7); the dashed line indicates the middle value of 5 treatment failure events (actual mean of the 10 within-range observations: 5.6). The physician assessment–based adjustment (PABA) group showed a significantly higher number of treatment failure events during autumn vs either the symptom-based adjustment (SBA) group or the biomarker-based adjustment (BBA) group.
aP=.02 for PABA vs BBA and SBA in autumn). We infer from these data that the expected number of treatment failure events for all 3 treatment modalities is typically 5 per 100 persons or about 5%, doubling to 10% to 11% in the autumn and winter within the PABA group.
COMMENT
The principal finding of this blinded, randomized controlled trial was that the rate of episodes of clinical worsening of asthma (ie, treatment failure) associated with instructing participants to take 2 puffs of low-dose beclomethasone every time they took 2 puffs of albuterol for relief of symptoms (SBA group) was not lower than the rate associated with adjusting the dose of inhaled corticosteroids based on physician assessment of symptoms, rescue use of albuterol, and pulmonary function at 6 week intervals (PABA group). Similarly, adjustment of the dose of inhaled corticosteroids based on measurement of exhaled nitric oxide at 6-week intervals (BBA group) was not associated with lower rates of treatment failure compared with PABA. Among the 18 secondary or exploratory outcomes, the outcomes of missed days from school or work and cumulative doses of inhaled corticosteroids were significantly lower in the SBA group compared with the PABA group.
Controller adjustment strategies differ in the features of asthma assessed and in the temporal coupling between changes in these features and adjustments in dose of inhaled corticosteroids. PABA management is a de facto standard of care. The weaknesses are its complexity and its loose temporal relationship between variations in asthma control and adjustment in dose of inhaled corticosteroids. The same is true of adjustments based on sputum eosinophils,7,8 exhaled nitric oxide, or methacholine responsiveness,9 which have had limited penetration into practice. Of available biomarkers, exhaled nitric oxide is the easiest to implement, but adjustment based on exhaled nitric oxide was no more effective than the other strategies.
Symptom-based adjustment strategies are appealing because they are simple to use and empower patients. Whether these features might improve adherence to therapy was not testable in this closely monitored trial. Requiring all participants to use 2 inhalers (A and B) twice daily and a third (inhaler C) with symptoms could easily have masked a benefit in quality of life from the smaller burden of care with the SBA approach.
Other studies have shown symptomdriven treatment with inhaled corticosteroids performing as well as daily treatments. In the Improving Asthma Control Trial (IMPACT),11 participants with mild persistent asthma received daily inhaled corticosteroids, zafirlukast, or placebo, plus 10 days of high-dose inhaled corticosteroids triggered by a symptom-based action plan. Asthma outcomes, including treatment failure, did not differ by treatment. BASALT participants had significantly more severe asthma than IMPACT participants.11 Despite treatment with daily beclomethasone during the BASALT run-in period (contrasted with only as-needed albuterol in IMPACT), mean values for FEV1 (2.96 L [86%]) and AM peak expiratory flow (447 L/m) were significantly lower at randomization in BASALT (vs IMPACT: 3.19 L [89%] for FEV1 and am peak expiratory flow of 465 L/m) (BASALT vs IMPACT: P=.049 for am peak expiratory flow; P<.001 for FEV1).
The Beclomethasone plus Salbutamol Treatment (BEST)12 study showed that as-needed combination therapy with beclomethasone and albuterol was superior to as-needed albuterol alone, and comparable with twice daily beclomethasone plus as-needed albuterol. BEST resembles BASALT in showing that as-needed combination therapy reduces cumulative dose of inhaled corticosteroids. In BEST participants whose asthma was comparable with BASALT, the dose of beclomethasone used was 250 μg/puff, which is 6 times the dose used in BASALT.
O’Byrne et al13 showed that combination formoterol and budesonide for both maintenance and relief of symptoms resulted in better asthma control than scheduled treatment alone. The participants had more severe asthma, and received daily maintenance treatment with inhaled corticosteroids. For US practitioners, it should be noted that use of a single combination inhaler for both maintenance and rescue treatment does not align with current US Food and Drug Administration policy. The innovation of BASALT is to couple the use of reliever and controller treatments that are approved by the Food and Drug Administration for their respective indications in a symptomdriven adjustment strategy.
We observed a slight increase in exhaled nitric oxide in the SBA group (14 ppb vs 5 ppb in BBA; 10 ppb in PABA), which is not surprising because the dose of inhaled corticosteroids in the BBA group was adjusted by fraction of exhaled nitric oxide. Similar small elevations in exhaled nitric oxide have been observed in patients with asthma considered too mild to warrant daily controllers17 and in patients whose asthma is in clinical remission.18
Symptom-based adjustment of inhaled corticosteroids in patients with mild to moderate asthma accomplishes temporal personalization of controller therapy and provides several advantages. Insofar as asthma triggers intensify airway inflammation (eg, allergens, viruses), the prompt increase in anti-inflammatory medication could offset the inflammogenic stimulus. Our observation that PABA participants had significantly more exacerbations during autumn, a period of increased viral infections and allergen exposure, while SBA participants did not, is consistent with this concept. That early intervention may prevent worsening of asthma to exacerbation is suggested by the finding that quadrupling the dose of inhaled corticosteroids at the onset of symptoms reduced the risk of requiring oral corticosteroids.19
Our findings provide reassurance that SBA of inhaled corticosteroids dose may be appropriate in most patients with mild to moderate asthma. Patients with asthma who poorly perceive their symptoms might be expected to have less favorable outcomes with SBA, but we could not directly assess this possibility. Moreover, patients who are poorly adherent to prescribed therapy would be expected to mimic our group of SBA participants, using their therapy only when symptoms dictate. There may be ethnic differences in the associations of adjustment strategies with study outcomes because the small number of Hispanic participants in our study did not have as robust a response to SBA relative to PABA (eFigure). This finding seems unlikely to have been a function of differential access to care or medication, but could reflect linguistic, sociocultural,20,21 or ethnic-specific environmental or pharmacogenetic differences that affect responses to triggers.22,23
Several limitations of our study are worth noting. Our sample size was too small to determine the associations of ethnicity and race with responsiveness to adjustment strategy for most outcomes. It is possible that some nonsignificant outcome differences could achieve significance with a larger sample size. However, the point estimates on most of these outcomes favored SBA over BBA or PABA, so the likelihood of us having missed an important detrimental association is small. Furthermore, findings in well-controlled clinical trials may not translate directly to clinical practice.
Power calculations were performed based on the assumption of a certain treatment failure rate in our population of interest, and a percentage reduction that we deemed as clinically meaningful (60% treatment failure reduction from 30% in the PABA group to 12% in the BBA or SBA groups). These estimates were based on published literature. If we had observed this size of reduction but without statistical significance, our study would have been underpowered. However, we observed reductions in treatment failure rates of 9% (22% for PABA vs 20% for BBA) and 32% (22% for PABA vs 15% for SBA), indicating that the treatment approaches were more similar in preventing treatment failure than anticipated. A very large study might be needed to demonstrate statistical significance for a difference in treatment failure rates of questionable clinical importance.
In summary, among adult participants with mild to moderate persistent asthma, neither the SBA nor the BBA strategy for inhaled corticosteroid therapy was superior to the standard PABA strategy for the outcome of treatment failure.
Supplementary Material
Acknowledgments
Funding/Support: This study was conducted with the support of the Institute for Translational Sciences at the University of Texas Medical Branch, supported in part by a Clinical and Translational Science Award UL1TR000071 from the National Center for Advancing Translational Sciences, National Institutes of Health. The study was also supported by the following National Institutes of Health grants U10 HL074225, U10 HL074227, U10 HL074231, U10 HL074204, U10 HL074212, U10 HL074073, U10 HL074206, U10 HL074208, and U10 HL074218 that were awarded by the National Heart, Lung, and Blood Institute. Teva Pharmaceuticals provided the study drug and matching placebo.
Author Contributions: Dr Calhoun had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs Calhoun and Ameredes contributed equally to the work.
Study concept and design: Calhoun, Ameredes, King, Icitovic, Castro, Cherniak, Chinchilli, Craig, Denlinger, DiMango, Fahy, Grant, Israel, Jarjour, Kazani, Kraft, Kunselman, Lazarus, Lemanske, Martin, Meyers, Peters, Ramsdell, Sorkness, Sutherland, Szefler, Wasserman, Walter, Wechsler, Boushey.
Acquisition of data: Calhoun, Ameredes, Castro, Chinchilli, Denlinger, DiMango, Fahy, Israel, Kazani, Kunselman, Lazarus, Lemanske, Lugogo, Martin, Moore, Pascual, Peters, Ramsdell, Sorkness, Sutherland, Wasserman, Walter, Wechsler, Boushey.
Analysis and interpretation of data: Calhoun, Ameredes, King, Icitovic, Castro, Chinchilli, Denlinger, DiMango, Engle, Fahy, Israel, Kraft, Lazarus, Lemanske, Martin, Meyers, Peters, Ramsdell, Szefler, Wasserman, Wechsler, Boushey.
Drafting of the manuscript: Calhoun, Ameredes, King, Chinchilli, DiMango, Engle, Israel, Lemanske, Martin, Peters, Wasserman, Wechsler, Boushey.
Critical revision of the manuscript for important intellectual content: Calhoun, Ameredes, King, Icitovic, Castro, Cherniak, Craig, Denlinger, DiMango, Fahy, Grant, Israel, Jarjour, Kazani, Kraft, Lazarus, Lemanske, Lugogo, Martin, Meyers, Moore, Pascual, Peters, Ramsdell, Sorkness, Sutherland, Szefler, Wasserman, Walter, Wechsler, Boushey.
Statistical analysis: King, Icitovic, Chinchilli, Engle, Kunselman, Lazarus, Meyers.
Obtained funding: Calhoun, Ameredes, Castro, Chinchilli, Fahy, Israel, Kraft, Lemanske, Martin, Peters, Sutherland, Wasserman, Boushey.
Administrative, technical, or material support: Calhoun, Ameredes, Castro, Cherniak, Chinchilli, Craig, DiMango, Fahy, Grant, Israel, Jarjour, Kazani, Kunselman, Moore, Peters, Ramsdell, Sorkness, Sutherland, Wasserman, Walter, Wechsler, Boushey.
Study supervision: Calhoun, Castro, Chinchilli, Denlinger, DiMango, Israel, Lazarus, Lemanske, Peters, Martin, Moore, Pascual, Ramsdell, Szefler, Wasserman, Walter, Wechsler, Boushey.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Drs Calhoun, Ameredes, and Kazani reported receiving funding from the National Heart, Lung, and Blood Institute (NHLBI) for this study and reimbursement for study travel. Dr King reported receiving funding from the NHLBI for this study and having an NHLBI grant pending. Ms Icitovic and Drs Lazarus and Walter reported receiving funding from the NHLBI for this study. Dr Bleecker reported receiving funding from the NHLBI for this study, study-related travel, review activities, and writing or reviewing this manuscript; consultancies with Aerovance, AstraZeneca, Boehringer, Centocor, GlaxoSmithKline, Genentech, Merck, Novartis, Pfizer, and Roche; lecture fees from Merck; and performing clinical trials at Wake Forest University supported by Boehringer, Centocor, GlaxoSmithKline, MedImmune, Genetech, Aerovance, Ception, AstraZeneca, Novartis, Amgen, Pfizer, Forest, and sanofi-aventis. Dr Castro reported receiving funding from the NHLBI for this study and study-related travel; consultancies with Schering, AsthmaTx, Genentech, IPS, Pulmogen, and sanofi-aventis; grants pending from American Lung Association, AsthmaTx, Amgen, Ception, enentech, MedImmune, Merck, Novartis, GlaxoSmithKline, and sanofi-aventis; lecture fees from Boehringer, Pfizer, Merck, GlaxoSmithKline, Genentech, AsthmaTx; and royalties from Elsevier. Dr Chinchilli reported receiving funding from the NHLBI for this study; and consultancies with GlaxoSmithKline, Merck, AstraZeneca, and Novartis. Dr Craig reported consultancies with CSL Behring, Dyax, Viropharma, and Shire; providing expert testimony in a legal case; grants pending from Viropharma, CSL Behring, Shire, Dyax, Pharming, Forest, Genentech, Biota, GlaxoSmithKline, and Grifols; lecture fees from Viropharma, CSL Behring, Dyax, Merck, Novartis, Genentech, and Teva Pharmaceuticals; and educational development funding from Vietnam Education Foundation. Dr Denlinger reported receiving funding from the NHLBI for this study; funding from the American Thoracic Society; consultancy for Merck; having a grant pending with the National Institutes of Health (NIH); and holding a patent through the Wisconsin Alumni Research Foundation. Ms Engle reported receiving funding from NHLBI for this study; and having a grant pending from the NIH. Dr Fahy reported receiving funding from the NHLBI for this study and study travel; board membership for Cytokinetics; consultancies with Amira, Oxagen, Gilead, GlaxoSmithKline, Amgen, Portola, Five Prime Therapeutics, and Merck; having grants pending with Genentech, Boehringer, Aerovance; and receiving travel support from GlaxoSmithKline, Merck, Amira, and Amgen. Dr Grant reported receiving funding from the NHLBI for this study; serving on the US Food and Drug Administration’s (FDA’s) Allergenic Extracts Advisory Committee; having grants pending with Baxter, Dyax, and Pharming; lecture fees from Shire; payment for manuscript preparation from Lev Pharma; and travel expenses from American Academy of Allergy, Asthma and Immunology (AAAAI), Shire, and the FDA’s Allergenic Extracts Advisory Committee. Dr Israel reported consultancies with Abbott, Amgen, Astellas, Cowen, GlaxoSmithKline, Icagen, Infinity, AstraZeneca, Merck, newMentor, NKT, Novartis, Ono, PDL, Pumatrix, Regeneron, Schering, Sepracor, Teva Pharmaceuticals, and Agenzia; expert testimony for 6 law firms; having grants pending with Aerovance, Amgen, Biota, Genetech, Icagen, Johnson & Johnson, MedImmune, Novartis; speaking fees from Merck and Genentech; and royalties from UpToDate. Dr Jarjour reported receiving funding from the NHLBI for this study; consultancies with AsthmaTx and Genentech; and having grants pending with Merck, GlaxoSmithKline, and Genentech. Dr Kraft reported receiving funding from the NHLBI for this study; grant support from Merck, GE Healthcare, AsthmaTx, Novartis, N30, Genentech, and GlaxoSmithKline; board membership for the American Thoracic Society; royalties from Elsevier; and payment for continuing medical education activities. Ms Kunselman reported receiving funding from NHLBI for this study; having a pending NIH grant; and stock in Merck. Dr Lemanske reported receiving funding from the NHLBI for this study, study travel, data review, manuscript review, and writing assistance; consultancies with Merck, Sepracor, SA Boney, GlaxoSmithKline, AIR, Genentech, Double Helix; having grants pending from the NHLBI and Pharmaxis; speaking fees from the Michigan Public Health Institute, Allegheny General Hospital, American Academy of Pediatrics (AAP), West Allegheny Health System, AAP California chapter, Colorado Allergy Society, Pennsylvania Allergy and Asthma Society, Harvard Pilgrim Health, California Society of Allergy, New York City Allergy Society, World Allergy Organization, and American College of Chest Physicians; a pending patent; and royalties from Elsevier and UpToDate. Dr Lugogo reported receiving funding from the NHLBI for this study and reimbursement for study travel; and having a pending grant from the NIH. Dr Martin reported consultancies with Teva Pharmaceuticals, Merck, AstraZeneca, and Genentech/Novartis; having grants pending with AsthmaNet, Genentech, and MedImmune; lecture fees from Teva Pharmaceuticals, Merck, and Genentech/Novartis; royalties from UpToDate; and payment for educational presentations from Teva Pharmaceuticals and Genentech. Dr Moore reported receiving funding from the NHLBI for this study and study travel; and grants from Aerovance, Amgen, AstraZeneca, Boehringer, Centacor, Ception, Forest, Genentech, GlaxoSmithKline, MedImmune, Novartis, Pfizer, and sanofi-aventis. Dr Pascual reported receiving funding from the NHLBI for this study; consultancies with United Therapeutics and Gilead; and having grants pending from United Therapeutics and Actelion. Dr Peters reported receiving funding from the NHLBI for this study, study travel, data review, manuscript review; consultancies with Aerocrine, AstraZeneca, Airsonnet, Delmedica, GlaxoSmithKline, Merck, and Teva Pharmaceuticals; and lecture fees from Integrity and Merck. Dr Ramsdell reported receiving funding from NHLBI for this study; and receiving a grant from Boehringer. Dr Sutherland reported receiving funding from the NHLBI for this study and study travel; consultancies with Forest, GlaxoSmithKline, Merck, Novartis, Day, and Genentech; having grants pending from Boehringer, Novartis, and the NIH; and fees for educational presentations from Genentech. Dr Szefler reported receiving funding from the NHLBI for this study, study travel, review, and writing; consultancies with Merck, Genentech, Schering, Boehringer, Novartis, and GlaxoSmithKline; having grants pending from GlaxoSmithKline, Ross, and Abbott; lecture fees from Merck; and fees for manuscript preparation from Genentech. Dr Wasserman reported receiving funding from the NHLBI for this study and study travel; employment by the AAAAI; and expert testimony for various law firms. Dr Wechsler reported consultancies with and lecture fees from GlaxoSmithKline, Novartis, Cephalon, Sepracor, Schering, NKT, AsthmaTx, Genzyme, MapPharma, Merck, Genentech, and Boehringer. Dr Boushey reported receiving funding from the NHLBI for this study; consultancies with Merck, GlaxoSmithKline, Genentech, Kalblos, Pharmaxis, Johnson & Johnson; having pending grants from GlaxoSmithKline, Genentech, and the Allergy, Asthma, and Immunology Foundation of Northern California; lecture fees from Breath California; and royalties from McGraw-Hill. Drs Cherniack, DiMango, Meyers, and Sorkness reported no conflicts.
Role of the Sponsor: The National Heart, Lung, and Blood Institute had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Data and Safety Monitoring Board: Andrea J. Apter, MD, MSc, Serpil Erzurum, MD, Barbara Layman, Yancy Phillips, MD, MACP, Bruce M. Psaty, MD, PhD, and James Sheller, MD.
Data Coordinating Center: Kelly Bixler, Lauren Leshak, Jennifer Lucier, Aimee Merchlinski, Melanie Payton, and Ronald Zimmerman.
Site Coordinators and Study Managers: Galveston, Texas: Lisa Sweeney, RN, CTC, Debra Altemus, RN, and Alyson Clayborn, BS. Boston, Massachusetts: Muhammad Zahid, MD, MPH, Kathy Zheng, MPH, and Suzanne Vogt, MS. Denver, Colorado: Jennifer Brandorff, Mary Gill, Juno Pak, and Allen Stevens. Durham, North Carolina: Denise Beaver and Rhonda Webb. Madison, Wisconsin: Ann Sexton, Tiffany Wirth, and Barb Miller. New York, New York: Erin Simpson and Surinder Narula. San Diego, California: Melissa Thrasher, Katie Kinninger, and Paul Ferguson. San Francisco, California: Peggy Cadbury, RN, Jane Liu, MS, and Jean Schenkkan. St Louis, Missouri: Pamela Kemp, RMA, Tina Weber, RN, and Vanessa Curtis, RRT. Winston-Salem, North Carolina: Cheryl Wilmoth and Bob Hmieleski.
Additional Contributions: We gratefully acknowledge the diligent and responsible oversight of the data and safety monitoring board during the design, execution, and analysis of this trial; these individuals were provided a small honorarium by the National Heart, Lung, and Blood Institute for their work. Aaron Deykin, MD, provided helpful advice on experimental design and outcome measures during the design of the trial, but was not compensated for his work. We thank the individuals who worked at the data coordinating center for their careful trial oversight and stewardship of the research data; these persons were compensated as employees of their respective institutions. The Asthma Clinical Research Network Steering Committee expresses its profound thanks to the coordinators and study managers at each site, whose diligence, meticulous effort, and unwavering commitment made the conduct of this study possible; they were compensated for their work as employees of their respective institutions.
Footnotes
Online-Only Material: eSupplement, 2 eTables, the eFigure, and the Author Video Interview are available at http://www.jama.com.
REFERENCES
- 1.National Asthma Education and Prevention Program Expert Panel . Report 3: Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute; Rockville, MD: 2007. NIH Publication 08-4051. [Google Scholar]
- 2.Global Initiative for Asthma [Accessibility verified August 7, 2012];Global strategy for asthma management and prevention. http://www.ginasthma.org/guidelines-gina-report-global-strategy-for-asthma-management.html.
- 3.Sutherland ER. Nocturnal asthma. J Allergy Clin Immunol. 2005;116(6):1179–1186. doi: 10.1016/j.jaci.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 4.Szefler SJ, Mitchell H, Sorkness CA, et al. Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults. Lancet. 2008;372(9643):1065–1072. doi: 10.1016/S0140-6736(08)61448-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith AD, Cowan JO, Brassett KP, et al. Use of exhaled nitric oxide measurements to guide treatment in chronic asthma. N Engl J Med. 2005;352(21):2163–2173. doi: 10.1056/NEJMoa043596. [DOI] [PubMed] [Google Scholar]
- 6.Brightling CE, Green RH, Pavord ID. Biomarkers predicting response to corticosteroid therapy in asthma. Treat Respir Med. 2005;4(5):309–316. doi: 10.2165/00151829-200504050-00002. [DOI] [PubMed] [Google Scholar]
- 7.Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts. Lancet. 2002;360(9347):1715–1721. doi: 10.1016/S0140-6736(02)11679-5. [DOI] [PubMed] [Google Scholar]
- 8.Deykin A, Lazarus SC, Fahy JV, et al. Sputum eosinophil counts predict asthma control after discontinuation of inhaled corticosteroids. J Allergy Clin Immunol. 2005;115(4):720–727. doi: 10.1016/j.jaci.2004.12.1129. [DOI] [PubMed] [Google Scholar]
- 9.Sont JK, Willems LN, Bel EH, et al. Clinical control and histopathologic outcome of asthma when using airway hyperresponsiveness as an additional guide to long-term treatment. Am J Respir Crit Care Med. 1999;159(4 pt 1):1043–1051. doi: 10.1164/ajrccm.159.4.9806052. [DOI] [PubMed] [Google Scholar]
- 10.Leuppi JD, Tandjung R, Anderson SD, et al. Prediction of treatment-response to inhaled corticosteroids by mannitol-challenge test in COPD. Pulm Pharmacol Ther. 2005;18(2):83–88. doi: 10.1016/j.pupt.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Boushey HA, Sorkness CA, King TS, et al. Daily versus as-needed corticosteroids for mild persistent asthma. N Engl J Med. 2005;352(15):1519–1528. doi: 10.1056/NEJMoa042552. [DOI] [PubMed] [Google Scholar]
- 12.Papi A, Canonica GW, Maestrelli P, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. N Engl J Med. 2007;356(20):2040–2052. doi: 10.1056/NEJMoa063861. [DOI] [PubMed] [Google Scholar]
- 13.O’Byrne PM, Bisgaard H, Godard PP, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med. 2005;171(2):129–136. doi: 10.1164/rccm.200407-884OC. [DOI] [PubMed] [Google Scholar]
- 14.Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med. 2010;363(18):1715–1726. doi: 10.1056/NEJMoa1008770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juniper EF, Svensson K, Mörk A-C, Ståhl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med. 2005;99(5):553–558. doi: 10.1016/j.rmed.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Juniper EF, Guyatt GH, Ferrie PJ, Griffith LE. Measuring quality of life in asthma. Am Rev Respir Dis. 1993;147(4):832–838. doi: 10.1164/ajrccm/147.4.832. [DOI] [PubMed] [Google Scholar]
- 17.Childhood Asthma Management Program Research Group Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med. 2000;343(15):1054–1063. doi: 10.1056/NEJM200010123431501. [DOI] [PubMed] [Google Scholar]
- 18.van Den Toorn LM, Prins JB, Overbeek SE, et al. Adolescents in clinical remission of atopic asthma have elevated exhaled nitric oxide levels and bronchial hyperresponsiveness. Am J Respir Crit Care Med. 2000;162(3 pt 1):953–957. doi: 10.1164/ajrccm.162.3.9909033. [DOI] [PubMed] [Google Scholar]
- 19.Oborne J, Mortimer K, Hubbard RB, et al. Quadrupling the dose of inhaled corticosteroid to prevent asthma exacerbations. Am J Respir Crit Care Med. 2009;180(7):598–602. doi: 10.1164/rccm.200904-0616OC. [DOI] [PubMed] [Google Scholar]
- 20.Hardie GE, Janson S, Gold WM, et al. Ethnic differences. Chest. 2000;117(4):935–943. doi: 10.1378/chest.117.4.935. [DOI] [PubMed] [Google Scholar]
- 21.Fritz GK, McQuaid EL, Kopel SJ, et al. Ethnic differences in perception of lung function. Am J Respir Crit Care Med. 2010;182(1):12–18. doi: 10.1164/rccm.200906-0836OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burchard EG, Avila PC, Nazario S, et al. Lower bronchodilator responsiveness in Puerto Rican than in Mexican subjects with asthma. Am J Respir Crit Care Med. 2004;169(3):386–392. doi: 10.1164/rccm.200309-1293OC. [DOI] [PubMed] [Google Scholar]
- 23.Choudhry S, Ung N, Avila PC, et al. Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med. 2005;171(6):563–570. doi: 10.1164/rccm.200409-1286OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.