Abstract
AIM:
Study was aimed to assess the accuracy of drug dose and its frequency in patients with renal dysfunction in a tertiary care hospital.
MATERIALS AND METHODS:
This was a retrospective observational study. Patients > 18 years old, with the serum creatinine (SCr) level > 1.4 mg/dl were included. Drugs prescribed to these patients were recorded in case record form. Drugs for which the dose was adjusted according to the clinical response to therapy, not according to SCr level (i.e., angiotensin converting enzyme inhibitors, diuretics, B blockers, anti-diabetics, etc.) were not taken into consideration. Based on the creatinine clearance which was calculated by Cockroft-Gault formula, dose and frequency of prescribed drugs were assessed using “Drug prescribing in renal failure – dosing guidelines for adults, 4th edition” and by another literature. Data was analyzed using Statistical Product and Service Solutions by IBM corporation version 17.0 software.
RESULTS:
Total 278 indoor patients were screened, out of which 205 patients included. Total drugs prescribed to the patients were 1338 with the average of 6.53 drugs per patient. Out of these 180 (13.45%) drugs needed dose adjustment. Among them only 34 (18.89%) drugs were adjusted appropriately, and rest 146 (81.11%) were not adjusted. The most common group of drug that need dose adjustment was anti-microbials (144, 80%) with levofloxacin as individual drug.
CONCLUSION:
This study emphasizes the importance of patients with renal dysfunction and implementing appropriate dose adjustments. This study also suggests intervention such as on-line information to assist dose guidelines and participation of clinical pharmacologist could improve patient outcome.
KEY WORDS: Chronic kidney disease, clearance, creatinine, dose adjustment
The percentage of patients with renal impairment is increasing with the aging of the population. It is estimated that today 10% of the population has some kind of renal impairment.[1,2] Since a significant number of drugs are eliminated through the kidneys, it is often necessary to adjust their dose according to renal function. Even though dosage of some drugs in renal impairment is necessary, numerous studies have shown a large number of inadequate drug doses in patients with renal impairment.[3,4,5,6]
The risks of toxicity of medicines are higher in patients with chronic kidney disease. particularly in elder patients. Furthermore, risk of developing advanced disease and related adverse events caused by age-related in renal function and use of multiple medications to treat co-morbidities made them more vulnerable population.[7] The proper dosing of medications for patients with renal impairment can maximize the therapeutic efficacy, minimize toxicity, and cost.[8,9,10,11]
Dosages of drugs cleared renally are based on renal function calculated as Glomerular Filtration Rate (GFR) or Creatinine Clearance (CrCl). Dosing recommendations for individual drugs can be found in Drug Prescribing in Renal Failure: Dosing Guidelines for Adults[12] and various other literatures. The guidelines are divided into three GFR categories (less than 10 mL/min/1.73 m2, 10 to 50 mL/min/1.73 m2, and more than 50 mL/min/1.73 m2), encompassing an up to 10-fold range in renal function.[7] Examples of drugs requiring dose adjustment in patients with renal impairment mostly include antibiotics, digoxin, H2-receptor antagonists, and ACE-I.[13]
The aim of this study was to assess the appropriateness of the drug dose adjustment in hospitalized patients with kidney dysfunction.
Materials and Methods
Study design
This was a retrospective observational study conducted at Shree Krishna Hospital, which is a 550 bedded multi speciality and tertiary care teaching rural hospital. From July 2009 to November 2009, all hospitalized patients were screened from the System department of our hospital based on the Serum creatinine (SCr) level and age of the patient. Then record files of those screened patients were analyzed from the Medical Record Section of the hospital. Patients having SCr level more than 1.4 mg/dl and age more than 18 years irrespective of gender were included in the study. Only systemic drug therapy was included. Exclusion criteria were patients under hemodialysis or continuous ambulatory peritoneal dialysis (CAPD), patients with dehydration and patients with muscular diseases (muscular dystrophy, polymyositis, rhabdomyolysis). The following parameters were collected for all the patients with renal dysfunction: Age, gender, weight, date of admission and discharge, department, diagnosis, and prescription order and filled up in case record form. Patients’ whose SCr level substantially fluctuating, (increase or decrease of more than 1 mg/dl) could be recorded several times. Prescription orders were recorded 24 h after the laboratory reports were available.
Drugs for which the dose was adjusted according to the clinical response to therapy, not according to SCr level (i.e., ACE-I, diuretics, β blockers, anti-diabetics, etc.) were not taken into consideration.[14]
Ethics
Study protocol was reviewed by Human Research Ethics Committee of the Institute, and permission was taken.
Patients included in the analysis were those who belonged to stages 3, 4, and 5 according to the guidelines of the National Kidney Foundation[7] as patients in stage 1 or 2 usually having adequate kidney function were not included. CrCl was calculated for all the patients and those with CrCl < 60 ml/min were included in the analysis. CrCl was calculated using the Cockroft Gault equation.[15] CrCl 60 ml/min was considered the threshold for renal impairment. Patients included in the analysis belonged to the following stages of renal impairment: Stage 3 (CrCl 30-60 ml/min), stage 4 (CrCl 15-29 ml/min), and stage 5 (CrCl < 15 ml/min).[7] The regimen for any drug was rated “appropriate” when the dose was suitable based on the patient's CrCl. Prescription of any drug was rated “inappropriate” when the dosage prescribed was not in conformity with the adjustment required with regard to the patient's CrCl. The reference used to check for the appropriateness on the dose was “Drug prescribing in renal failure – dosing guidelines for adults, 4th edition”[12] and by another literature. Administered doses of each studied drug were compared with the recommended doses.
Statistical analysis
Data was systematized and analyzed using SPSS version 17.0 software. Parameters of the patients were expressed as frequency and percentage of inadequate and adequate drug dose adjustment. The statistical significance of the differences between groups was compared by Pearson Chi-square test. A P < 0.05 was considered significant.
Results
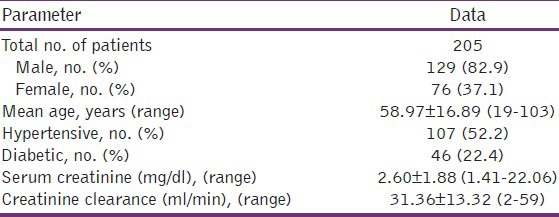
From July 2009 to November 2009, total 278 Indoor patients were screened. And from that 205 patients were included according to inclusion criteria and rest 73 patients were excluded (45 – either on hemodialysis or on CAPD, 28 – dehydration). Study profile is given in Figure 1. Mean age of the study sample was found to be 58.97 years and mean serum CrCl was found to be 2.60. Demographic data of the included patients is shown in Table 1.
Figure 1.
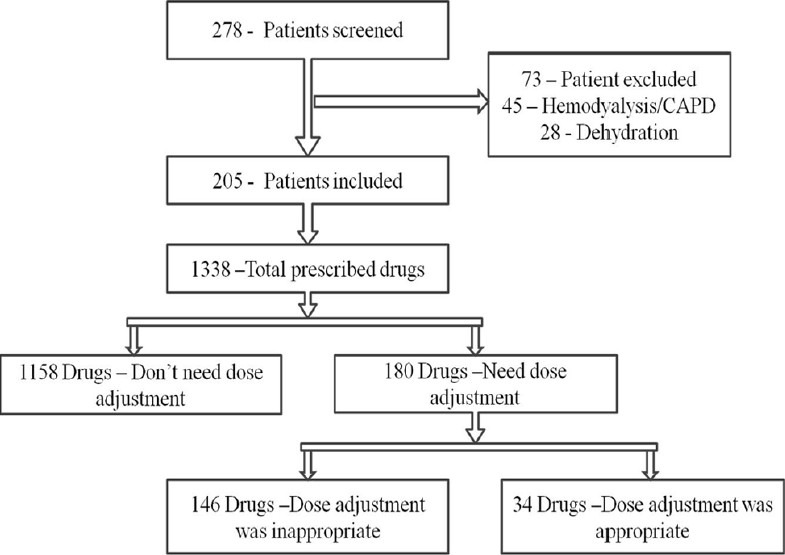
Study profile
Table 1.
Characteristics of included patients
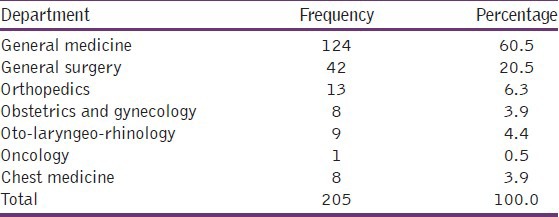
Among the total included patients, maximum patients were from General Medicine Department (60.5%), followed by General Surgery Department (20.5%). Detail is given in Table 2. As per staging of chronic kidney diseases (CKD), 113 (55.1%) of patients were belonged to stage 3, 65 (31.7%) of patients were belonged to stage 4 and 27 (13.2%) to stage 5.
Table 2.
List of patients according to department
Total drugs prescribed to the patients were 1338 with the average of 6.53 drugs per patient. Out of these 180 (13.45%) drugs needed dose adjustment according to respective CrCl. From 180 drugs only 34 (18.89%) drugs were adjusted according to CrCl and rated as “appropriate”, and rest 146 (81.11%) drugs were not adjusted and rated as “inappropriate”.
Appropriateness of the group of drugs and individual drugs are given in Figures 2 and 3. The most common group found to be prescribed inappropriately was anti-microbials, which was 115 times prescribed inappropriately (dose/frequency/both were not adjusted according to CrCl). This was followed by analgesic group of drugs and drugs from the gastro-intestinal group.
Figure 2.
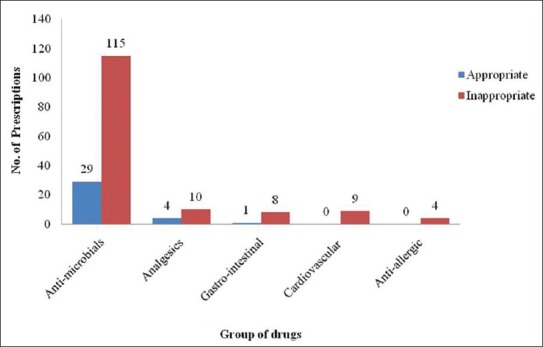
Appropriateness of group of drugs prescribed to study sample
Figure 3.
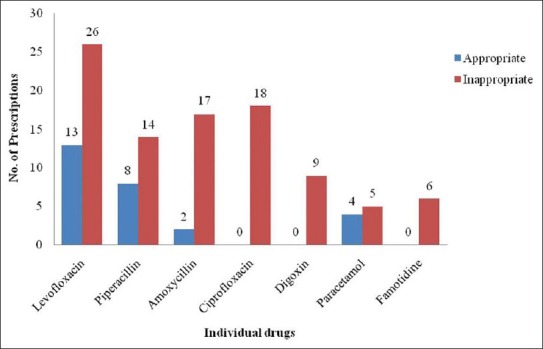
Appropriateness of individual drug prescribed to study sample
In case of individual drugs, levofloxacin was found to be prescribed maximally inappropriately (26 times) followed by ciprofloxacin and amoxycillin. Apart from anti-microbials, dose of digoxin was not adjusted appropriately (9 times) which was followed by famotidine and paracetamol.
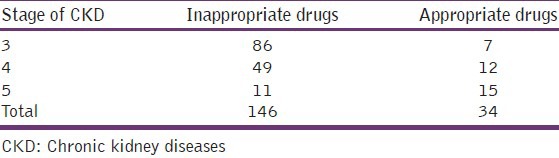
The frequency of appropriate and inappropriate drugs in different stage of the CKD is listed in Table 3. In CKD stage 3, 4, and 5 number of drugs prescribed inappropriately were 86, 49, and 11 respectively, while frequencies of appropriateness were 7, 12, and 15. P value according to Chi-square test is found to be 0.0001, which is significant.
Table 3.
Frequency of appropriate and inappropriate drugs in different stages of CKD
Discussion
The pharmacokinetic parameters such as drug bioavailability, protein binding, biotransformation, volume of distribution, and renal excretion are altered in patients with renal impairment. This is mostly important for drugs for which the fraction excreted unchanged is high. To avoid the risk of drug toxicity among patients with reduced renal function, medication doses should be adjusted based on the estimated CrCl, co-morbid disease, and co-prescribed medications.[16] Several recent studies have indicated that dosing errors and the risk of toxicity are common among patients with renal impairment. In agreement with other studies, our results showed widespread dosing errors among patients with renal impairment.[3,17]
In our study, most common groups of drugs that required dose adjustment is anti-microbials (n = 144, 80%) followed by analgesics (n = 14, 7.78%), cardio-vascular drugs (n = 9, 5%), gastro-intenstinal drugs (n = 9, 5%) and anti-allergic drugs (n = 4, 2.22%). Same result is seen in Soetikno, et al.[18] done in Indonesia and Sweileh, et al.[16] done in Palestine. Authors are not able to found similar study done in India. Same order of inappropriateness is seen among different groups of drugs. Individual drug wise most common drug that required dose adjustment is levofloxacin (n = 39, 21.66%), followed by piperacillin (n = 22, 12.22%), amoxicillin (n = 19, 10.56%), and ciprofloxacin (n = 18, 10%). Soetikno et al.[18] also supports our result.
Several reasons could be cited for this inappropriate dosing. The large number and the continuously increasing list of drugs that required dose adjustment makes it difficult for medical staff to remain updated on dose adjustment issues. Furthermore, it seems that there is an underestimation or lack of knowledge of the importance regarding CrCl in determining the appropriate medication dose. Fluctuating renal function, rapid changing in SCr values might not permit appropriate estimation of renal function. In our study, CrCl and body weight needed to calculate, the CrCl were missing from most of the patients’ medical files. It is important that CrCl be calculated and documented for all patients for dose calculation. Using SCr level as the only indicator of renal function is not accurate. In our study, approximately 10% of the patients with normal or borderline SCr, were having low CrCl suggesting that normal SCr does not exclude renal impairment. A third possible reason is the lack of continuing medical education that focuses on the importance of this issue. Charts for dose adjustments are needed and should be available for the prescriber. Better therapeutic monitoring is needed and could be achieved through clinical pharmacologist's participation. Another professional source for information regarding dose adjustment is the drug information center. SCr level is often inappropriate to assess actual renal function and leads to underestimation of renal impairment, particularly in the elderly. The assessment of CrCl requires a 24 h urine collection which is often difficult to perform, but its estimation with the Cockcroft Gault formula, taking into account patient's weight, age and SCr level, also provides an accurate assessment of renal function.[19]
Possible reasons for the predominance of the anti-microbial are the most frequent and careless use of them, admissions in critical care unit, perioperative use of them in surgical wards. And last reason is we neglect most of the cardio-vascular drugs that require dose adjustment frequently after the anti-microbial group, because, most of the time they are adjusted according to the clinical response. Despite an explicit need for dose titration in patients with renal impairment, adjustment should not be made based on pharmacokinetic considerations only. For example, cardiovascular medications such as ACE-I (e.g., enalapril) or ί-blocking agents (e.g., atenolol), spironolactone diuretic should be prescribed according to clinical end points such as blood pressure or heart rate.
In this study, frequencies in appropriateness of drugs in different stages of CKD were calculated, and it was clearly found that dosing error was gradually decreased as staging of CKD was advancing e.g., with lesser CrCl. This finding suggests that physician become more alert at the time of worsening of the patients and tried to reduce the dose of drugs as per guidelines.
This study showed that dosing errors are common among hospitalized patients with impaired renal function. Most of these dosing errors were made during hospital stay, suggesting that better patient observation and dose calculation is needed. In conclusion, hospitalized patients are at risk for adverse outcomes due to prescribing errors related to inappropriate use of medication dose. This information should be considered in the development of strategies to prevent adverse patient outcomes resulting from such errors.
Strategies to adjust drug dosage in renal dysfunction may help to individualize drug therapy and, thus, contribute to drug safety. Principles to increase the safety of drug prescription in patients with renal dysfunction are to select the appropriate drugs in patients with renal dysfunction, e.g., by taking into consideration the possibility of drug interaction and doses.[20,21] A stepwise approach to assist physicians in prescribing drug therapy for patients with renal dysfunction is initial assessment, which includes a history and physical examination, calculates CrCl, chooses a loading dose and maintenance dose, and monitoring drug level principally drugs with narrow therapeutic margin.[22,23]
There are several limitations of our study like we took only one prescription out of the whole record file to check the drug appropriateness. Analysis in this study was done according to drug classification and not according to the individual patients. Then we have not checked that how much amount of dose is excessively given (quantitative difference).
As dosing guidelines, we used the recommendations from the Drug prescribing in renal failure – dosing guidelines for adults, 4th edition.[12] When the recommendations were not available or clear enough, we used another available literature. We noticed significant differences in recommendations for dosages of the same drugs, which additionally complicates drug dosage in patients with renal impairment. It is clear that there is a need to have universal guidelines for drug dosage in patients with renal impairment.
In conclusion, this study emphasizes the importance of improving the identification of patients with renal dysfunction, estimating their CrCl, and implementing appropriate dose adjustments according to these estimates. This study also suggests other interventions, which could improve patient-specific outcomes such as on-line information to assist dose guidelines, access to individuals trained in pharmacokinetics, implementation of pharmacokinetic dose consultation services in departments of clinical pharmacology, and daily participation of clinical pharmacologist during doctor's ward visits.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.van Dijk EA, Drabbe NR, Kruijtbosch M, De Smet PA. Drug dosage adjustments according to renal function at hospital discharge. Ann Pharmacother. 2006;40:1254–60. doi: 10.1345/aph.1G742. [DOI] [PubMed] [Google Scholar]
- 2.Pillans PI, Landsberg PG, Fleming AM, Fanning M, Sturtevant JM. Evaluation of dosage adjustment in patients with renal impairment. Intern Med J. 2003;33:10–3. doi: 10.1046/j.1445-5994.2003.00330.x. [DOI] [PubMed] [Google Scholar]
- 3.Salomon L, Deray G, Jaudon MC, Chebassier C, Bossi P, Launay-Vacher V, et al. Medication misuse in hospitalized patients with renal impairment. Int J Qual Health Care. 2003;15:331–5. doi: 10.1093/intqhc/mzg046. [DOI] [PubMed] [Google Scholar]
- 4.Salomon L, Levu S, Deray G, Launay-Vacher V, Brücker G, Ravaud P. Assessing residents’ prescribing behavior in renal impairment. Int J Qual Health Care. 2003;15:235–40. doi: 10.1093/intqhc/mzg034. [DOI] [PubMed] [Google Scholar]
- 5.Long CL, Raebel MA, Price DW, Magid DJ. Compliance with dosing guidelines in patients with chronic kidney disease. Ann Pharmacother. 2004;38:853–8. doi: 10.1345/aph.1D399. [DOI] [PubMed] [Google Scholar]
- 6.van Dijk EA, Drabbe NR, Kruijtbosch M, De Smet PA. Dosage adjustments according to renal function at discharge: A comparison of 3 hospitals. Ann Pharmacother. 2006;40:2276–7. doi: 10.1345/aph.1H380. [DOI] [PubMed] [Google Scholar]
- 7.Munar MY, Singh H. Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician. 2007;75:1487–96. [PubMed] [Google Scholar]
- 8.Peterson JP, Colucci VJ, Schiff SE. Using serum creatinine concentrations to screen for inappropriate dosage of renally eliminated drugs. Am J Hosp Pharm. 1991;48:1962–4. [PubMed] [Google Scholar]
- 9.Goldberg DE, Baardsgaard G, Johnson MT, Jolowsky CM, Shepherd M, Peterson CD. Computer-based program for identifying medication orders requiring dosage modification based on renal function. Am J Hosp Pharm. 1991;48:1965–9. [PubMed] [Google Scholar]
- 10.Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA, et al. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. JAMA. 1997;277:307–11. [PubMed] [Google Scholar]
- 11.Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA. 1997;277:301–6. [PubMed] [Google Scholar]
- 12.Aronoff GR, Berns JS, Brier ME, Golper TA, Morrison G, Singer I, et al. 4th ed. Michigan: American College of Physicians; 1999. Drug prescribing in renal failure: Dosing Guidelines for Adults. [DOI] [PubMed] [Google Scholar]
- 13.Taeschner W, Vozeh S. Pharmacokinetic drug data. In: Speight TM, Holford NH, editors. Avery's Drug Treatment. 4th ed. Auckland: Adis International; 1997. pp. 1629–64. [Google Scholar]
- 14.Markota NP, Markota I, Tomic M, Zelenika A. Inappropriate drug dosage adjustments in patients with renal impairment. J Nephrol. 2009;22:497–501. [PubMed] [Google Scholar]
- 15.Matzke GR, Frye RF. Drug therapy individualization for patients with renal insufficiency. In: Dipiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, editors. Pharmacotherapy: A Pathophysiological Approach. 7th ed. New York: McGraw Hill Companies; 2008. pp. 833–44. [Google Scholar]
- 16.Sweileh WM, Janem SA, Sawalha AF, Abu-Taha AS, Zyoud SH, Sabri IA, et al. Medication dosing errors in hospitalized patients with renal impairment: A study in Palestine. Pharmacoepidemiol Drug Saf. 2007;16:908–12. doi: 10.1002/pds.1412. [DOI] [PubMed] [Google Scholar]
- 17.Blix HS, Viktil KK, Moger TA, Reikvam A. Use of renal risk drugs in hospitalized patients with impaired renal function–an underestimated problem? Nephrol Dial Transplant. 2006;21:3164–71. doi: 10.1093/ndt/gfl399. [DOI] [PubMed] [Google Scholar]
- 18.Soetikno V, Effendi I, Nafrialdi, Setiabudy R. A survey on the appropriateness of drug therapy in patients with renal dysfunction at the internal medicine ward FMUI/Dr. Cipto Mangunkusumo Hospital. Med J Indones. 2009;18:108–13. [Google Scholar]
- 19.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 20.Matzke GR, Frye RF. Drug administration in patients with renal insufficiency. Minimising renal and extrarenal toxicity. Drug Saf. 1997;16:205–31. doi: 10.2165/00002018-199716030-00005. [DOI] [PubMed] [Google Scholar]
- 21.Tett SE, Kirkpatrick CM, Gross AS, McLachlan AJ. Principles and clinical application of assessing alterations in renal elimination pathways. Clin Pharmacokinet. 2003;42:1193–211. doi: 10.2165/00003088-200342140-00002. [DOI] [PubMed] [Google Scholar]
- 22.Swan SK, Bennett WM. Drug dosing guidelines in patients with renal failure. West J Med. 1992;156:633–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Kappel J, Calissi P. Nephrology: 3. Safe drug prescribing for patients with renal insufficiency. CMAJ. 2002;166:473–7. [PMC free article] [PubMed] [Google Scholar]


