Abstract
Proper availability of drug on to corneal surface is a challenging task. However, due to ocular physiological barriers, conventional eye drops display poor ocular bioavailability of drugs (< 1%). To improve precorneal residence time and ocular penetration, earlier our group developed and evaluated in situ gel and nanoparticles for ocular delivery. In interest to evaluate the combined effect of in situ gel and nanoparticles on ocular retention, we combined them. We are the first to term this combination as “nanoparticle laden in situ gel”, that is, poly lactic co glycolic acid nanoparticle incorporated in chitosan in situ gel for sparfloxacin ophthalmic delivery. The formulation was tested for various physicochemical properties. It showed gelation pH near pH 7.2. The observation of acquired gamma camera images showed good retention over the entire precorneal area for sparfloxacin nanoparticle laden in situ gel (SNG) as compared to marketed formulation. SNG formulation cleared at a very slow rate and remained at corneal surface for longer duration as no radioactivity was observed in systemic circulation. The developed formulation was found to be better in combination and can go up to the clinical evaluation and application.
KEY WORDS: Gamma scintigraphy, in situ gel, nanoparticle, nanoparticle laden in situ gel, ocular, PLGA, sparfloxacin
Hyperacute bacterial conjunctivitis is a severe, sight threatening ocular infection that warrants immediate ophthalmic work-up and management. Bacterial conjunctivitis requires treatment with antibiotics for 5-7 days that may result in poor patient compliance with conventional dosage forms due to greater frequency of drug administration, that is, 2-3 drops every 2-3 h.[1] This is because in ocular delivery, the physiological constraints imposed by the protective mechanisms of the eye lead to low absorption of drugs, resulting in short duration of the therapeutic effect. When a drug solution is dropped into the eye, the effective tear drainage and blinking action of the eye result in a 10-fold reduction in the drug concentration within 4-20 min.[1] The availability of medicament at corneal surface would be significantly improved if the precorneal residence time of drugs could be increased. Several new preparations such as inserts,[2] collagen shields,[3] and colloidal systems, such as liposomes,[4,5] nanoparticles,[6,7] and nanocapsules[8,9] have been developed for ophthalmic use, not only to prolong the ocular contact time of the vehicle but also to slow down drug elimination.[10] The use of nanotechnology-based drug delivery systems like microemulsions, nanosuspensions, nanoparticles, solid lipid nanoparticles, niosomes, dendrimers, and liposomes has led to the solution of various solubility-related problems of poorly soluble drugs, like dexamethasone, budesonide, ganciclovir, and so on.[11] However, these novel preparations have some disadvantages, such as poor compliance. Out of these novel formulations; in situ gel and nanoparticles have been established as the promising one. In our previous work, we found that these formulations have their own disadvantages. For example, in situ gel remains for 12-15 h,[12] whereas poly lactic co glycolic acid (PLGA) nanoparticles are nonmucoadhesive, so are drained out of eyes quickly.[13] In our present work, we try to combine both these formulation strategies as a nanoparticles suspended in liquid dosage form suitable to be administered by instillation into the eye which, upon exposure to physiological conditions, changes to the gel phase, thus increasing the precorneal residence time of the nanoparticles and enhancing ocular bioavailability. Our group has coined the term “nanoparticle laden in situ gel” for this formulation.[14]
In our study, we used third generation flouroquinolone sparfloxacin for formulation evaluation. Hence, in the present work we develop and evaluate new system, that is, sparfloxacin PLGA nanoparticle laden in situ gel for ophthalmic delivery to improve precorneal residence time and thus ocular bioavailability.
Materials and Methods
Materials
Sparfloxacin was received as kind gift from Micro Labs Ltd. (Chandigarh, India); PLGA (50:50), intravenous = 0.2 dL/g, was obtained from Purac Biomaterial, Singapore), polyvinyl alcohol (PVA, MW 95,000) was obtained from Sigma-Aldrich Chemie GmbH (Steinheim, Germany). Chitosan (practical grade, 75%-85% deacetylated, and molecular weight 150 kDa) was obtained as kind gift from M/s India Sea Foods, India. All other chemicals were of analytical grade.
Preparation of nanoparticle laden in situ gel
Nanoparticles were prepared as per our previous published work.[13] Briefly, nanoprecipitation technique was applied to prepare sparfloxacin nanoparticles. Drug and polymer in ratio of 1:10 (keeping drug 10 mg and PLGA 100 mg) were dissolved in acetone (5 mL) at room temperature. The resulted solution was slowly dropped with speed manually (approx. 0.5 mL/min) into water (20 mL) containing PVA (1.5% w/v) with continuous magnetic stirring at 1800 rpm. Acetone and some water were evaporated, and the final volume of the aqueous suspension was collected. The nanosuspension was then centrifuged at 18,000 rpm, 20°C for 1 h (Remi, India). Nanoparticles were collected and washed (3 times) with distilled water using previously described centrifugation approach and then lyophilized by means of Christ Alpha 1-4 lyophilizator (Christ, Germany) using 1% w/v mannitol as lyoprotectant. Whereas, in situ gel base is prepared by dissolving 0.5% w/v chitosan in 1% v/v acetic acid, pH adjusted to 5.5-6.0 with buffer saline.[12]
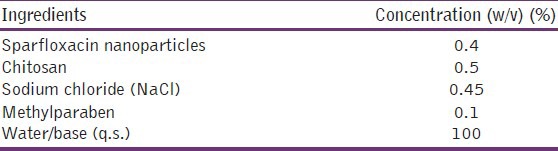
Weighed quantity of drug-loaded freeze-dried nanoparticles (equivalent to the prescribed dose of sparfloxacin 0.3% w/v) were taken and dispersed in the respective 1 ml of placebo in situ gel base (0.5%w/v chitosan solution) to form nanoparticle laden in situ gel. Freeze-dried nanoparticles were weighed accurately on the basis of its drug loading and release pattern [Table 1].[13]
Table 1.
Final composition of sparfloxacin nanoparticles laden in situ gel
Physicochemical characterization
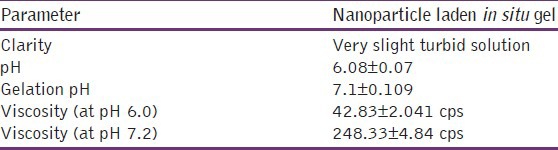
Physicochemical characterization of the developed nanoparticles laden in situ gel were carried out and compiled in Table 2.
Table 2.
Physicochemical characterization of nanoparticles laden in situ gel
Clarity
The clarity of the formulations after and before gelling was determined by visual examination of the formulations under light alternatively against white and black backgrounds.
Gelation pH
Gelation pH is the pH at which the solution form of the formulation was changed to gel. Formulation was taken in a beaker and 1M NaOH was added dropwise with continuous stirring. pH was checked using pH meter. The pH at which sudden change in viscosity was observed and noted is recorded as gelation pH.
Viscosity
Viscosity of formulations were determined by using Brookfield's viscometer (model DV II, spindle no. 02, at 20 rpm), on formulation pH (6.0) and gelation pH near 7.0.
In vivo ocular retention study-Gamma scintigraphy
Gamma scintigraphy is used to assess in vivo precorneal drainage of the developed formulation. Male New Zealand albino rabbits of either sex weighing 1.8-2.5 kg and free of any signs of ocular inflammation or gross abnormality were used in the study. Animals were procured from the animal house of Institute of Nuclear Medicine and Allied Sciences Delhi, India and all study protocols were approved by local institutional animal ethics committee. Sparfloxacin was radiolabeled with Tc-99m by direct labeling method using stannous chloride as reducing agent as per previous reported method.[13] Gamma camera (Millenium VG, USA), autotuned to detect the 140 KeV radiation of Tc99m was used for scintigraphy study. Rabbits were anesthetized using ketamine HCl injection given intramuscularly in a dose of 15 mg/kg body weight. The rabbits were positioned 5 cm in front of the probe and 50 μL of the radiolabeled formulation was instilled onto the left corneal surface of the rabbits. Recording was started 5 s after instillation and continued for 30 min using 128 × 128 pixel matrix. Individual 60 frames (60 × 30 s) were captured by dynamic imaging process. Region of interest was selected on one frame of the image and time-activity curve was plotted to calculate the rate of drainage from eye. A single whole body static image was also taken after 6 h of instillation of drug/formulation. Each formulation was tested on three rabbits.
Results and Discussion
In situ gel and nanoparticles have their own merits and demerits. In situ gel stays only for 12 h, whereas PLGA and conjunctiva is anionic in nature and hence PLGA nanoparticles are not able to be retained for the longer time. To increase the duration, we entrapped PLGA nanoparticles in cationic chitosan in situ gel system. Chitosan is a cationic polymer and hence will make link with both PLGA nanoparticles and conjunctiva and thus increases retention. As chitosan act both as pH sensitive and permeation enhancer, the viscosity of the chitosan increases when it reaches to eye pH at 7.4. This combination will allow nanoparticles to stay for longer duration and provide optimum drug release. To achieve most out of these two delivery systems, we have combined both the system to develop “nanoparticles laden in situ gel.” The nanoparticle size was near 180 nm in concordant with our previously reported results.[13] The quantity of nanoparticles was calculated on the basis of drug loading and release, we have taken 40 mg of SN to prepare 1 ml of respective nanoparticles laden in situ gel (SNG). Final composition of SNG is given in Table 1. The developed nanoparticles laden in situ gels were then evaluated for various physicochemical characteristics as given in Table 2. The preparation is well-dispersed with slight turbidity. After mixing, no difference is found in gelation pH and viscosity of the formulation.
Gamma scintigraphy
Pharmacoscintigraphy is a tool to analyze the retention time of the formulation in cul-de-sac. For gamma scintigraphic studies, sparfloxacin was labeled with radionuclide Tc-99m using stannous chloride as reducing agent. Tc-99m was chosen for the purpose because of its moderate half life (6 h). Further it emits gamma rays, which have relatively low energy as compared to α and β rays, so leads to no serious health hazards to the workers. Sparfloxacin was instantaneously labelled with Tc-99m. Labelling efficiency was checked by instant thin layer chromatography (ITLC) using 100% acetone as mobile phase. The Rf value of free Tc is ~0.9, so it reaches to the top of the ITLC strip while the complexed Tc (drug-Tc complex) cannot travel much due to difference in molecular weight and is retained at the base of ITLC strip. Thus, from the difference in the top and bottom counts, labelling efficiency was calculated. After prelabeling efficiency studies which include labelling parameters like stannous chloride concentration and pH were optimized and a 50 μg stannous chloride concentration at pH 7.0 was found to give the maximum labelling efficiency (95.2%). In these conditions, minimum colloids (1%) were produced. The observation of the acquired gamma camera images showed a good spreading over the entire precorneal area for developed ocular formulations of sparfloxacin [in situ gel (SG), nanosuspension (SN), nanoparticle laden in situ gel (SNG)], immediately after administration as compared to marketed formulation. Marketed formulation cleared very rapidly from the corneal region and reached in to systemic circulation via nasolacrimal drainage system as significant activity was recorded in kidney and bladder after 6 h of ocular administration [Figure 1a], whereas formulations SG, SN, and SNG were retained for longer duration at corneal surface. No significant radioactivity was observed in kidney and bladder after 6 h of administration of these formulations [Figure 1b-d]. To differentiate between these formulations, the curves of the % radioactivity remained on the corneal surface as a function of time (30 min dynamic imaging) was also plotted [Figure 2]. The retention on cornea follows the following sequence:
Figure 1.
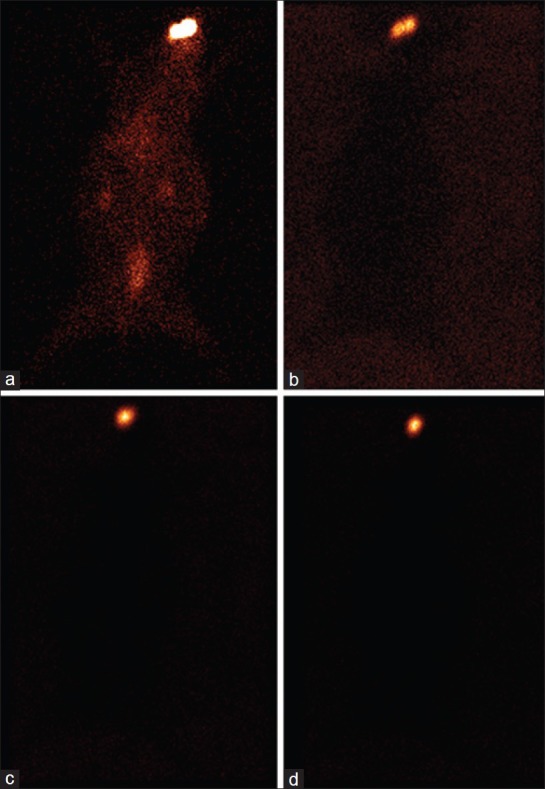
Static images of rabbit after 6 h of administering sparfloxacin formulations (a) marketed, (b) in situ gel, (c) nanosuspension, and (d) nanoparticles laden in situ gel
Figure 2.
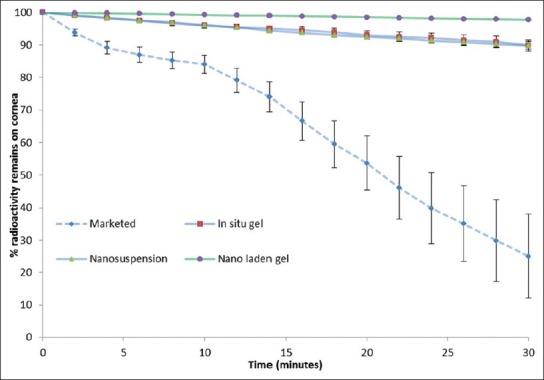
Gamma scintigraphy dynamic study
Marketed formulation < nanosuspension < in situ gel < nanoparticle laden in situ gel
It shows that the nanoparticles laden in situ gel retained for the longer duration in the eye giving extended release than nanosuspension and in situ gel alone, whereas the marketed formulation drained out of the eye with in 30 min. Due to mucoadhesive property of chitosan, in situ gel-based formulation cleared at slowest rate as compare to nanosuspension and retained at corneal surface for longest time duration. Further, the viscosity of chitosan is raised due to change in physiological conditions of pH (>7) and ionic concentration of the formulation upon instillation in to eye as a result of buffering action of the tear fluid. Chitosan also acts as penetration enhancer that increases the transport of drug across cornea.
Conclusion
Our previous study shows that the PLGA nanoparticles, due to smaller size, are able to provide prolong retention on the eye than the marketed formulation. PLGA is an anionic polymer and hence it is nonmucoadhesive in nature. To enhance the efficacy of the nanoparticulate formulation, we incorporate them in cationic chitosan in situ gel to make nanoparticle laden in situ gel, which helps in retention of nanoparticles on the eye. A good spreading and retention of formulation was observed in gamma scintigraphy studies as compared to marketed formulation. In time activity curve, there is a minimal falls in counts/s of formulation as compared to rapid fall of marketed formulation further shows that the nanoparticles laden in situ gel stay for longer time on the eye.
Acknowledgment
Authors are thankful to Council of Scientific and Industrial Research (CSIR), New Delhi to provide Senior Research Fellowship to Himanshu Gupta for conducting this work.
Footnotes
Source of Support: Dr. Himanshu Gupta was recipient of Senior Research Fellowship of Council of Scientific and Industrial Research (Government of India), New Delhi, India
Conflict of Interest: None declared.
References
- 1.Maurice DM. Kinetics of topical applied drugs. In: Saettone MS, Bucci P, Speiser P, editors. Ophthalmic drug delivery: Biopharmaceutical, technological and clinical aspects. Vol. 11. Padova: Liviana Press; 1987. pp. 19–26. [Google Scholar]
- 2.Ding S. Recent developments in ophthalmic drug delivery. Pharm Sci Technolo Today. 1998;1:328–35. [Google Scholar]
- 3.Hill JM, O’Callaghan RJ, Hobden JA, Kaufman E. Corneal collagen shields for ocular drug delivery. In: Mitra AK, editor. Ophthalmic drug delivery systems. New York: Marcel Dekker; 1993. pp. 261–75. [Google Scholar]
- 4.Pleyer U, Lutz S, Jusko W, Nguyen K, Narawane M, Rückert D, et al. Ocular absorption of topically applied FK506 from liposomal and oil formulations in rabbit eye. Invest Ophthalmol Vis Sci. 1993;34:2737–42. [PubMed] [Google Scholar]
- 5.Bochot A, Fattal E, Grossiord JL, Puisieux F, Couvereur P. Characterization of a new ocular delivery system based on a dispersion of liposomes in a thermosensitive gel. Int J Pharm. 1998;162:119–27. [Google Scholar]
- 6.de Campos AM, Diebold Y, Carvaiho EL, Sanchez A, Alonso MJ. Chitosan nanoparticles as new ocular drug delivery system: In vitro stability, in vivo fate, and cellular toxicity. Pharm Res. 2004;21:803–10. doi: 10.1023/b:pham.0000026432.75781.cb. [DOI] [PubMed] [Google Scholar]
- 7.Losa C, Calvo P, Castro E, Vila-Jato JL, Alonso MJ. Improvement of ocular penetration of amikacin sulphate by association to poly (butylcyanoacrylate) nanoparticles. J Pharm Pharmacol. 1991;43:548–52. doi: 10.1111/j.2042-7158.1991.tb03534.x. [DOI] [PubMed] [Google Scholar]
- 8.Losa C, Marchal-Heussler L, Orallo F, Vila-Jato JL, Alonso MJ. Design of new formulations for topical ocular administration: Polymeric nanocapsules containing metipranolol. Pharm Res. 1993;10:80–7. doi: 10.1023/a:1018977130559. [DOI] [PubMed] [Google Scholar]
- 9.De Campos AM, Sánchez A, Gref R, Calvo P, Alonso MJ. The effect of PEG versus a chitosan coating on the interaction of drug colloidal carriers with the ocular mucosa. Eur J Pharm Sci. 2003;20:73–81. doi: 10.1016/s0928-0987(03)00178-7. [DOI] [PubMed] [Google Scholar]
- 10.Bourlais CL, Acar L, Zia H, Sado PA, Needham T, Leverge R. Ophthalmic drug delivery systems: Recent advances. Prog Retin Eye Res. 1998;17:33–58. doi: 10.1016/s1350-9462(97)00002-5. [DOI] [PubMed] [Google Scholar]
- 11.Kayser O, Lemke A, Hernández-Trejo N. The impact of nanobiotechnology on the development of new drug delivery systems. Curr Pharm Biotechnol. 2005;6:3–5. doi: 10.2174/1389201053167158. [DOI] [PubMed] [Google Scholar]
- 12.Gupta H, Aqil M, Khar RK, Ali A, Bhatnagar A, Mittal G, et al. Development and characterization of Tc-99m timolol maleate for evaluating efficacy of in situ ocular drug delivery system. AAPS Pharm Sci Tech. 2009;10:540–6. doi: 10.1208/s12249-009-9238-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta H, Aqil M, Khar RK, Ali A, Mittal G, Bhatnagar A. Sparfloxacin loaded PLGA nanoparticles for sustained ocular drug delivery. Nanomedicine. 2010;6:324–33. doi: 10.1016/j.nano.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Gupta H, Aqil M, Khar RK, Ali A, Bhatnagar A, Mittal G. 37th annual meeting and exposition of the control release society. Portland, Oregon, USA: 2010. Jul 10-14, [Last accessed on 2013 Mar 10]. Levofloxacin nanoparticle laden in situ gel for control ocular drug delivery. Abstract 362 Available from: http://www.gbv.de/dms/tib-ub-hannover/66235561x.pdf . [Google Scholar]


