Abstract
Background Integration of HIV treatment with other primary care services has been argued to potentially improve effectiveness, efficiency and equity. However, outside the field of reproductive health, there is limited empirical evidence regarding the scope or depth of integrated HIV programmes or their relative benefits. Moreover, the body of work describing operational models of integrated service-delivery in context remains thin. Between 2008 and 2011, the Lusaka District Health Management Team piloted and scaled-up a model of integrated HIV and general outpatient department (OPD) services in 12 primary health care clinics. This paper examines the effect of the integrated model on the organization of clinic services, and explores service providers’ perceptions of the integrated model.
Methods We used a mixed methods approach incorporating facility surveys and key informant interviews with clinic managers and district officials. On-site facility surveys were carried out in 12 integrated facilities to collect data on the scope of integrated services, and 15 semi-structured interviews were carried out with 12 clinic managers and three district officials to explore strengths and weaknesses of the model. Quantitative and qualitative data were triangulated to inform overall analysis.
Findings Implementation of the integrated model substantially changed the organization of service delivery across a range of clinic systems. Organizational and managerial advantages were identified, including more efficient use of staff time and clinic space, improved teamwork and accountability, and more equitable delivery of care to HIV and non-HIV patients. However, integration did not solve ongoing human resource shortages or inadequate infrastructure, which limited the efficacy of the model and were perceived to undermine service delivery.
Conclusion While resource and allocative efficiencies are associated with this model of integration, a more important finding was the model’s demonstrated potential for strengthening organizational culture and staff relationships, in turn facilitating more collaborative and motivated service delivery in chronically under-resourced primary healthcare clinics.
Keywords: HIV and AIDS, integration, primary health care, service-delivery
KEY MESSAGES.
Integration of HIV treatment with other primary care services has been argued to have the potential to improve effectiveness, efficiency and equitability of health systems, but limited empirical evidence exists regarding the scope or depth of integrated programmes or their relative benefits.
A model of integrated HIV and primary outpatient services scaled-up to 12 Zambian primary health care clinics reportedly achieved efficiencies in allocation of human and material resources and improved equitability of service-delivery to HIV and non-HIV patients.
A key benefit of integration at the service delivery level was the model’s capacity to strengthen organizational culture and staff relationships, in turn facilitating more collaborative and motivated service delivery in facilities experiencing chronic under-resourcing.
However, integration did not solve overarching deficiencies in human resources and infrastructure, demonstrating a key limitation of a ‘ground-level’ only approach to integration.
Background
Since the early 2000s, extraordinary amounts of donor funding have been poured into HIV and AIDS in resource-poor settings, aimed primarily at mitigating the disease’s current and future public health and socio-economic costs. More recently, the unprecedented scale and speed of this investment and the concomitant agendas of those providing the funds and implementing the programmes, have generated debate concerning the relative benefits of disease-specific programmes vs broader health systems strengthening (HSS) (El-Sadr and Abrams 2007; Cohn et al. 2011). Central to the debate has been the tension between calls for national health systems to form the basis for all health-related interventions (WHO 2008) and the reality that in many developing countries with the worst HIV epidemics, those same health systems are weak and/or overburdened and so poorly placed to address the most urgent health-related challenges.
A key theme within the disease-specific programmes and HSS debate has been that of integration (Frenk 2009). Integration has been defined variously, but most recently as ‘a spectrum of organizational arrangements relating to the funding, administration, organization, service-delivery and clinical scenarios designed to create connectivity, alignment and collaboration’ (Coker et al. 2010, citing Kodner and Spreeuwenberg 2002). Importantly as Coker and colleagues note, integration is not a binary state, but can occur on a spectrum ranging from minimal, through to partial and ultimately complete integration (Coker et al. 2010). Proponents of integration for HIV programming have argued that it has the potential to improve the effectiveness, cost and utility efficiency and equity of both HIV and non-HIV care (Atun et al. 2010a, 2010b).
Considerable recent commentary has been generated on the topic of integration of HIV programmes, underpinned in part by concern over the recent slow-down in HIV donor funding and a concurrent need to sustain and strengthen in-country capacity to deliver already scaled-up HIV treatment programmes (UNAIDS 2008; Levine and Oomman 2009). In the literature to date, however, the overwhelming focus has been on integration of macro-level systems such as national health financing, national human resourcing and health information systems. With some notable exceptions (Price et al. 2009) and most concentrated on reproductive health (Lush et al. 1999; Mayhew et al. 2000; Smith et al. 2004; Rutenberg and Baek 2005; Mukherjee and Eustache 2007; Vivio et al. 2010) and tuberculosis (Harris et al. 2008; Terris-Prestholt et al. 2008), existing literature has paid far less attention to integration as it relates to service delivery at the primary level. This is surprising in view of growing recognition of the need for robust performance and seamless interrelation between all health system elements as a basis for further progress towards the Millennium Development Goals (MDGs).
For a majority of the world’s population, primary care facilities constitute the only, and therefore the most important, point of access to health care services. In addition, current HIV donor funding mechanisms still disburse considerable sums through non-government organizations (NGOs) and district health offices that oversee or offer support at this level. Understanding the scope and characteristics of different models of integrated service delivery, and their potential strengths and weaknesses within the primary care context thus makes sense from both a public health and a strategic perspective. Although recent research conducted in South East Asia and southern Africa has started to address this question by plotting the scope of integration of HIV administrative and clinical services (Coker et al. 2010; Conseil et al. 2010; Topp et al. 2010), appropriately contextualized empirical evidence describing the features and relative benefits of functional models remains thin (Shigayeva et al. 2010). This is particularly the case for the acutely resource-constrained countries of sub-Saharan Africa where the HIV is most prevalent.
Setting
Zambia has the sixth largest generalized epidemic of HIV in the world with a prevalence of 14.3% amongst adults aged 15–49 years (Central Statistical Office and Ministry of Health 2009). In 2003, the national government of the Republic of Zambia (GRZ) launched a policy promising free and universal access to antiretroviral therapy (ART). By 2010, with support from the United States President’s Emergency Fund for AIDS Relief (PEPFAR) and the Global Fund for AIDS, Tuberculosis and Malaria (GFATM), Zambia had one of the world’s largest HIV treatment programmes, with approximately 350 000 HIV-infected individuals enrolled in treatment. This service was delivered through a network of decentralized HIV-specific clinics co-located in over 150 public primary health care clinics.
Between 2008 and 2009 the Lusaka District Health Management Team, with support from the Centre for Infectious Disease Research in Zambia (CIDRZ), piloted a model that integrated the delivery of HIV and outpatient department (OPD) services in two urban primary health care clinics (Topp et al. 2010). Zambian primary health care clinics generally consist of an OPD, Maternal and Child Health Department, HIV Care and Treatment Department and Tuberculosis Treatment facility. Larger sites may also house a laboratory, tuberculosis diagnostic centre, in-patient department and labour ward. Each department forms part of a single primary health care clinic, resourced (in the first instance) through government funding mechanisms. However, the generally hierarchical nature of clinic operations and the presence of multiple disease- or department-specific donor programmes with particular areas of interest mean that departments often work relatively independently of each other. Patients may be ‘referred’ between departments but in many cases, no formal system links treatment records in different locations. Tracking referrals even within the clinic is thus extremely difficult as responsibility for screening and follow-up may lie in multiple domains with little coherence.
The integrated model was premised on three major modifications to the service delivery arrangement: (1) amalgamation of physical space and patient flow for HIV and OPD services; (2) standardization of HIV and non-HIV medical records and screening forms; and (3) introduction of routine provider-initiated testing and counselling (PITC) for those without a recent record of HIV status. A feasibility study conducted during the pilot demonstrated the model had good working potential, without adversely affecting outpatient or HIV client attendance, showing improved rates of clinic-based HIV counselling and testing, improved measurement and documentation of vital signs for regular outpatient attendees, and a reduction in the perception of stigma associated with seeking HIV care and treatment (Topp et al. 2010; Topp et al. 2011). Between July 2009 and July 2011 the model was scaled up to a further 12 primary care clinics spread across three Zambian provinces. This study had two objectives. First, to document the extent of integration of clinic operations in 12 facilities following implementation of the integrated model; and second, to identify health care providers’ perceptions of the integrated model by comparison to non-integrated services.
Methods
We used a mixed methods approach (Creswell and Piano Clark 2007) incorporating facility surveys, observations and key informant interviews with clinic managers and district officials.
Data on the scope and extent of integration were collated from facility surveys and observational visits carried out by the first author at each facility between June and September 2011, and coupled with primary activity reports documenting the process and scope of integration over the life-course of the integration programme. The survey was carried out in collaboration with clinic managers, and documented whether defined areas of service delivery (for example duty rosters, data management, laboratory services) were fully, partially or not integrated.
Data were entered into an analytical framework adapted from Conseil and colleagues (Conseil et al. 2010) for application to the Zambian health service delivery setting. In the adapted framework, the extent and nature of integration of HIV services in Zambia were investigated through three major service delivery functions, namely: clinic stewardship and governance, clinical services, and clinic-based monitoring and evaluation. Falling underneath these three service delivery functions, we identified 17 indicators of integrated service delivery. For each of the indicators, an ordinal scoring system was used to characterize the degree of integration, ranging from 1 to 3, where 1 = no or very limited integration, 2 = partial integration, and 3 = complete or almost complete integration. The values were not designed to imply benefit gained from integration. As noted elsewhere (Coker et al. 2010) ordinal values enable comparison across multiple entities, while acknowledging the potential for differences across variables including location, catchment population, staffing levels, quality of infrastructure and so forth. Since the tool is based on a health systems framework, it allows for a standardized approach to explore how systems components perform contextually and practically (Atun et al. 2010a). Data were collated, and then independently triangulated by the first and second authors to generate separate assessments for the scope of integration in each clinic. These lists were subsequently jointly reviewed to reach agreement. For clinic six, no pre-implementation data were available, since HIV services were established as an integrated service.
Qualitative data on the relative benefits and challenges of the integrated model were subsequently collected during 15 semi-structured interviews carried out by the first and second authors with each of the 12 clinic managers and 3 District Medical Officers between August and September 2011. Interviews were recorded, transcribed and coded inductively. Transcripts of interviews were reviewed by the first and second authors to generate six major themes providing a lens through which to examine the benefits and problems arising from integrated service delivery. These results were triangulated with observational and survey data, as well as the first and second authors’ own experiences from over 3 years of the programme. Initial interpretations were reflected back to key informants for further input prior to final write-up. The protocol was approved by the institutional review boards of the University of Zambia, Protocol # 003-02-08 (Lusaka, Zambia) and the University of Alabama at Birmingham, Protocol # X080403013 (Birmingham, Alabama, USA) and received clearance from the Zambian Ministry of Health. Written informed consent was sought and received from all interview subjects. Personal and organizational views of informants were not attributed to specific individuals or clinics in order to preserve anonymity.
Findings
For the purposes of this discussion patients enrolled in HIV care and treatment and staff providing HIV care and treatment are referred to as ‘ART patients’ and ‘ART staff’, and patients accessing routine outpatient care or staff providing such care are referred to as ‘OPD patients’ and ‘OPD staff’. The process of implementation of the integrated service delivery model has been previously described (Topp et al. 2010). Of the 12 integrated clinics reviewed, the majority (8) were urban, 2 were peri-urban and 2 were rural facilities. Service characteristics of the clinics varied and are listed in Table 1.
Table 1.
Characteristics of 12 integrated primary health care facilities
| Profile | Month of integration | Catchment population (2010) | 24-hour clinic | Onsite laboratory | ∼ daily outpatient department attendance | HIV clients enrolled (as at Jan 2011) | |
|---|---|---|---|---|---|---|---|
| Clinic 1 | Urban | July 2008 | 31 872 | Yes | No | 80 | 3187 |
| Clinic 2 | Urban | Nov. 2008 | 52 549 | No | No | 100 | 3721 |
| Clinic 3 | P-Urban | Feb. 2009 | 18 050 | No | No | 45 | 1503 |
| Clinic 4 | Urban | April 2009 | 70 219 | No | Yes | 120 | 6513 |
| Clinic 5 | Urban | Oct. 2009 | 47 904 | No | No | 95 | 3109 |
| Clinic 6 | P-Urban | Dec. 2009 | 4772 | No | No | 30 | 2700 |
| Clinic 7 | Urban | Feb. 2010 | 24 822 | No | No | 45 | 856 |
| Clinic 8 | Urban | April 2010 | 74 116 | Yes | Yes | 180 | 12 099 |
| Clinic 9 | Urban | June 2010 | 28 979 | No | No | 60 | 4185 |
| Clinic 10 | Rural | July 2010 | 15 139 | Yes | Yes | 35 | 4018 |
| Clinic 11 | Urban | April 2011 | 275 000 | Yes | Yes | 100 | 4077 |
| Clinic 12 | Rural | May 2011 | 34 612 | No | No | 30 | 2099 |
Scope and extent of integration
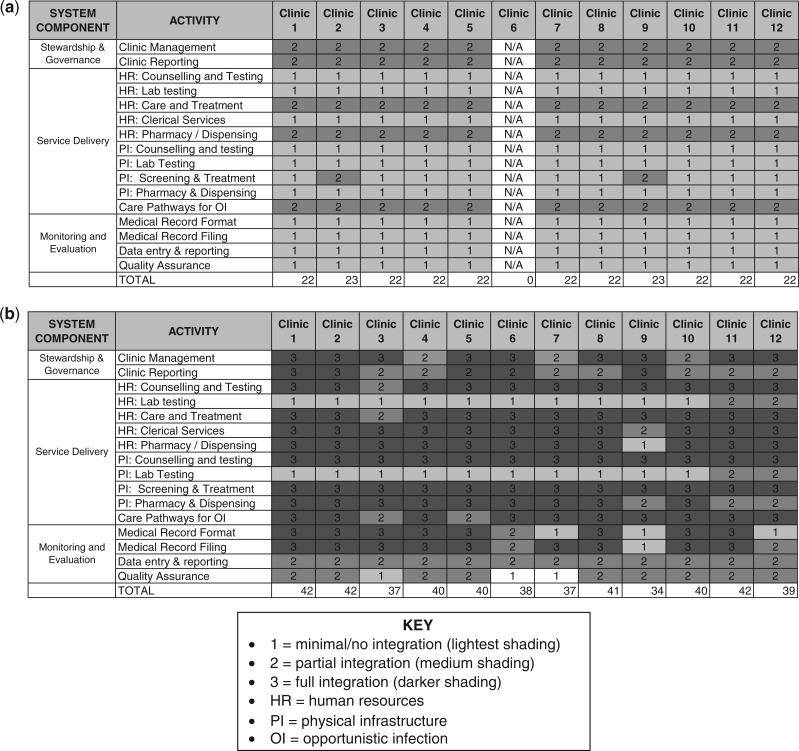
The extent of integrated clinic services resulting from integration are recorded in two figures and listed in Table 2. Figure 1a records the extent of integration across 17 indicators, prior to implementation. Figure 1b, records the extent of integration across the same indicators 6–24 months post-implementation.
Table 2.
Areas of change in integrated clinics
| Area of change | Pre integration | Post integration |
|---|---|---|
| Human resources | Health care workers on separate ART and OPD staff rosters | Single duty-roster for all health care workers in OPD/ART |
| Care pathway | Separate care pathway for ART and OPD patients | Single, harmonized care pathway for all patients |
| Triage / vitals | Only provided to ART patients | Provided to all patients irrespective of HIV-status |
| Medical records | OPD and ART have different patient IDs, patient cards and medical files | Medical files harmonized and patients issued single ID number |
| Medical forms | Pro-forma medical forms for ART patients only | Pro-forma medical forms introduced for OPD clients |
| HIV counselling & testing (C&T) | Voluntary C&T provided in stand-alone room | Routine, in-house C&T for all patients without HIV test result |
| Infrastructure | OPD and ART operations in physically separate locations | OPD and ART housed in same location and serve all patients |
| HIV education | Only provided to ART patients | Provided to all patients irrespective of HIV status |
| Management | Separate OPD and ART Nurse Managers | Joint OPD/ART manager appointed with deputy |
Notes: ART = antiretroviral therapy; OPD = outpatient department.
Figure 1.
Primary health care clinics (a) scope of integration prior to implementation (b) scope of integration 6–24 months post implementation
Implementation of the integrated model had a substantial impact on the organization of clinic-based human resources and infrastructure utilization in the primary health care clinics. Prior to integration, human resources for counselling and testing and clerical services constituted completely separate cadres. Human resources for screening, phlebotomy, pharmacy and dispensing in ART and OPD were the same staff, but these staff worked different times, in different settings, with different resources according to whether they were rostered for an ART or OPD shift. By contrast, after integration, all human resource functions were fully integrated. A single cadre of health care workers worked from a single duty-roster, to provide care jointly to both HIV and OPD clients based on a harmonized patient flow. Table 3 provides an illustrative break-down of staff available in stand-alone vs integrated OPD and ART departments, in a typical mid-sized urban clinic.
Table 3.
Example of daily (per-shift) human resource allocation in a mid-sized urban clinic
| Department | Nurses | CO | MO | Pharmacy dispenser | Lay counsellors | Registry staff |
|---|---|---|---|---|---|---|
| Vertical OPD | 3 | 1 | 0 | 1 | 3 | 3 |
| Vertical ART | 2 | 1 | 0 | 0 | 0 | 0 |
| Integrated | 5 | 2 | 0 | 1 | 3 | 3 |
Notes: CO = clinical officer; MO = medical officer; ART = antiretroviral therapy; OPD = outpatient department.
Prior to integration, the infrastructure allocated for counselling and testing, laboratory testing, care and treatment, pharmacy stores and dispensing were discrete. Following integration, we found that services in almost all clinics had been rearranged such that ART and OPD duty stations were housed in the same rooms, and accessed by all clients irrespective of sero-status. In three cases, pharmacy stores were not fully integrated due to inappropriate (non-air conditioned) or insufficient space. In addition laboratory testing remained separate in all clinics in one district, since tests for ART clients are conducted off-site at a central laboratory. Despite this, collection and labelling of test samples was integrated in all 12 sites as part of integrated phlebotomy services.
A key shift in clinic operations resulting from integration was the harmonization of patient identification numbers, medical records and medical record filing. In eight clinics we found this system in place such that clients presented a patient card to a single registry room, where uniform ART and OPD files were stored according to a single patient identification (ID) system. In four clinics, this system was not in operation upon the site visit—two clinics having never received that element of the intervention due to insufficient storage space, and two clinics having independently reverted to the non-integrated patient ID and filing system.
At all 12 sites surveyed, clinic managers had transitioned from separate ART and OPD duty-rosters, to a single duty-roster covering integrated service-delivery. Additionally, at all 12 clinics, the appointment of a single outpatient manager (or ‘in-charge’) and a deputy manager was part of the implementation package. However, at three clinics we found that managerial duties had been devolved to separate nurse managers for ART and OPD. These duties primarily included collation of month-end reports, responsibility for quality assurance and mentorship.
An integrated patient flow (or care pathway) was a central feature of the integrated service-delivery model. The integrated care pathways introduced during implementation involved routine collection of vital signs (weight, temperature and blood pressure) for all outpatients at a single registration desk, and a first-come, first-served system (excepting medical emergencies) to triage patients to appropriate care. In all 12 primary health care clinics we found that routine collection of vital signs had been adopted. This contrasted with the pre-integration services where only ART clients received this service. Operation of a single triage desk and integrated clinician screening was present in 10 clinics. However, in two clinics (Clinic 3 and 5) we found that the system of integrated patient flow had reverted to a separate ART and OPD triage desk, and separate ART and OPD screening rooms, more closely resembling the pre-integration system.
Perceptions and experiences of integration
Semi-structured interviews with 12 clinic managers and three District Medical Officers explored service providers’ perceptions of integration and revealed a number of commonalities. Table 4 summarizes these findings across six major clinic functions. Below we discuss five recurring themes that arose with respect to the benefits and negative aspects of integration: equity and service provision, knowledge, teamwork, space and infrastructure, and human resources.
Table 4.
Strengths and weaknesses of the integrated model
| Identified strengths | Identified weaknesses | |
|---|---|---|
| Human resourcing |
|
|
| Infrastructure |
|
|
| Management |
|
|
| Patient care |
|
|
| Filing/data management |
|
|
| General resourcing |
|
|
Notes: ART = antiretroviral therapy; OPD = outpatient department; PITC = provider initiated counselling and testing.
Issues of equity and service provision
All key informants commented that integration resulted in a more equitable distribution of resources (human and material) with positive run-on effects for a number of clinic functions. These included fairer distribution of duties amongst staff; a reduction in tension between staff in different departments; improved quality of care for OPD patients through the establishment of additional services; fewer overall drug and equipment stock-outs; reduced stigma associated with accessing HIV testing, care and treatment; and more efficient patient flow.
“Patients benefit as there is always someone to see them unlike in the past, when there were cases where you find there is no nurse in OPD, or no nurse in ART because there is only one nurse available in the clinic.” [Clinic Manager #2, Urban]
“Clients are happy as the white house [ART Department] issue is no longer there and stigma has been reduced due to a single system of patient flow.” [Clinic Manager #4, Rural]
A second important theme arising with respect to integrated service provision was the potential for systems of HIV care to be adapted to strengthen chronic disease care for non-HIV outpatient services. As several managers noted:
“Vital signs are done for all patients and it helps identify conditions such as high blood pressure which used to be missed in the past…” [Clinic Manager #5, Urban]
“PITC has helped diagnosis of HIV and … the OPD form acts as a guide to the [clinicians].” [Clinic Manager #6, Rural]
“It would be good if peer educators giving HIV talks could be trained to give talks on disease such as diabetes too … there is a need.” [Clinic Manager #1, Urban]
Issues of knowledge and capacity building
The role of integration in promoting opportunities for both health care providers and patients to share or gain new knowledge was an important benefit identified by key informants. Examples of this included registry clerks and peer educators receiving training in ART filing and medical record keeping; OPD staff receiving formal ART training and/or mentorship and support from staff already trained in ART; provision of HIV health education talks to all patients, not just those enrolled in ART; and patients’ repeated exposure to information and education through one-on-one PITC sessions.
“The knowledge acquired on handling patients through integration systems training…has made work easier as every staff is able to handle any patient.” [Clinic Manager #1, Urban]
“Health education which is given by peers and benefits all patients as they sit in one area and PITC is offered every time to patients who do not know their status so they come to understand.” [Clinic Manager #8, Urban]
Issues of teamwork and clinic systems
A third theme related to integration raised by interviewees was the establishment of stronger clinic systems. Almost all respondents noted that the integrated system contributed to improved staff morale and teamwork through shared responsibility and mutual understanding of the clinic functions. Management of staff including developing duty rosters and duty allocation, maintaining accountability and generating monthly reports were also noted to be easier under the integrated system.
“[Integration] has helped change staff attitude towards OPD care, because the system in ART for patient care is strong and well established and in place.” [District Official, Lusaka]
“Work culture is much improved because of shared responsibility…staff are easier to manage because they are working together…” [Clinic Manager #4, Urban]
Harmonization of systems including the reorganization of patient flow to reduce duty-station duplication and unification of patient identification numbers and medical records were also distinguished by informants as beneficial features of integration.
“Harmonized number and medical records improves on record keeping and for patients it reduces stigma.” [Clinic Manager #11, Urban]
“The [integrated system] makes tracing files easy as clerks are looking in one place; systems of filing are good as anyone can easily retrieve files.” [Clinic Manager #1, Urban]
Systematized patient care, such as routine collection and recording of patient vital signs, routine offers of HIV testing and use of a standardized clinical form for OPD patients were identified as long-term advantages of the integrated model.
“… now all patients have an opportunity to have vital signs checked and receive health education.” [Clinic Manager #3, Peri-Urban]
“the OPD form acts as a guide to the clinician on what to check for in the patient and there is no freelance screening as there used to be…” [Clinic Manager #7, Urban]
“PITC is being done for all patients who do not know status; this helps clinicians make the right diagnosis and helps with proper patient management.” [Clinic Manager #2, Urban]
Issues of human resources
The need for improved levels of human resources was identified by informants as being a barrier to and challenge of integration. For example, clinic managers noted that although integrated duty rosters made allocation of limited staff members easier, it did not solve the problem of too few health care professionals to begin with. In several more recently integrated facilities, informants noted that insufficient staff members had received formal ART training, making duty allocation difficult and affecting staff morale, since some members were not confident to handle HIV-enrolled clients.
“New staff have not been ART trained and [are] not able to function in an integrated model well; few nurses to cover the duty stations has led to multi-tasking and this causes long waiting times when one staff is covering more than two areas.” [Clinic Manager #3, Peri-Urban]
In addition, several interviewees observed that incoming staff (both clinical and clerical) who had not received the initial training in integrated systems were often ill-equipped to adapt to the integrated service model.
“New clerks coming to the site who did not attend the systems training find it difficult to adapt…staff integration systems training should be done periodically to help new staff.” [Clinic Manager #1, Urban]
Issues of space
Inadequate and/or inappropriate infrastructure was almost universally noted to be a barrier to effective integration of services and in some cases an infection control hazard. Several respondents stated that while reorganization of clinic space had freed up some rooms by reducing duty-station duplication (e.g. a single pharmacy dispensary vs separate ART and OPD dispensaries), it did not ultimately address overall space deficiency. The problem of inadequate space was identified by several clinics as particularly acute with respect to waiting areas, where immune-compromised HIV patients and potentially infectious OPD patients were seated in close proximity with insufficient ventilation.
“Infection control in the corridors is not good; when there is no-one to control the flow of patients and people are crowding together inside…particularly in the rainy season.” [Clinic Manager #5, Urban]
“… despite coming together, space is still not adequate.” [Clinic Manager #10, Rural]
In addition, infrastructure was noted to be a problem because of the increased space required to house now-combined ART and OPD medical files. More than half of respondents noted that without additional space, or transition to an electronic medical record system for OPD, this model of record keeping would be difficult to sustain.
“Registry space quickly runs out due to the increased number of [folder-style] files being opened.” [Clinic Manager #2, Urban]
“Although a bigger space was put in for filing, this was proven to quickly fill up…” [Clinic Manager #5, Urban]
Discussion
Integration of HIV care and treatment is increasingly being championed as a way to achieve the tripartite aims of improved clinical care, better public health and health system outcomes and more cost-efficient programming. Evidence demonstrating just how realistic these claims are, however, remains weak. This study provides evidence of both the scope of integration achieved across various service delivery components by this intervention and of the relative benefits of integration from the perspective of health care providers themselves.
Our results demonstrate that in 12 Zambian facilities, integrating HIV and primary OPD services resulted in a number of organizational and managerial efficiencies. Simplified and harmonized clinic-level systems demonstrated in the facility survey were perceived by health care providers to improve standards of OPD care through routine measurement and recording of vitals, routine opt-out testing for HIV and greater flexibility to use available drug stocks for all patients.
Standardized service delivery through stronger patient care systems has implications for other areas of primary care, most notably chronic non-communicable diseases (NCDs). Our results demonstrate the potential for adapting and integrating the chronic care features of HIV services to other areas of primary health care through relatively simple standardization measures. Although still largely untapped, our findings suggest there is also potential to leverage the expectation that standard clinical investigations should be done and patient records accurately kept for HIV patients, to strengthen these same areas of service-delivery for NCD care at the facility level (El-Sadr et al. 2011; Rabkin and El-Sadr 2011). However, the potential for leveraging HIV systems to broader chronic care ends was not a specific focus of this study and more rigorous application of the principle, and operations research to evaluate it, are urgently needed.
All the clinics involved in this intervention provided prevention of mother-to-child transmission (PMTCT) administered (as throughout Zambia) during antenatal visits in the Maternal and Child Health (MCH) Department by trained nurse-midwives. PMTCT records are located in MCH and thus remain separate from ART records. By and large, the integration of ART and OPD described here was not able to address the separation of PMTCT and ART services, or substantively reduce the burden of record keeping. However, the intervention did encourage efficiencies with respect to duplication of patient IDs and continuum of care, as OPD/ART registry clerks in the integrated clinics were trained to identify and use the PMTCT-issued patient IDs when establishing an OPD/ART medical record for HIV-positive mothers. Anecdotally, this intervention reduced the number of ID numbers issued to a single patient and made it possible to track patient records across different departments. Nonetheless, investigator experience suggests that many HIV-positive women lose their PMTCT numbers accidentally, or in some cases on purpose, preferring to ‘silo’ their identity in different parts of the clinic. This fear is due to stigma associated with health care workers who know their status.
Directly observed therapy short-course (DOTS) for tuberculosis (TB) was provided in all the clinics in this intervention. TB is a notifiable disease, identified and reported primarily through OPD. As such, the integration of OPD and ART had little effect on the work-load related to routine monitoring and record keeping. Nonetheless, several efficiencies with respect to the TB/HIV care pathway were noted. First, the introduction of provider-initiated HIV testing (PITC) prior to clinical screening of patients resulted in more TB patients knowing their HIV status at the time of TB diagnosis. This resulted in patients receiving intensive counselling regarding TB/HIV co-infection and subsequently being expedited for enrolment in ART. Similarly, from a human resources perspective, routine provision of PITC to all patients reduced the burden on chronically understaffed TB departments (typically one nurse supported by 1–3 lay staff) to identify co-infected clients through testing and counselling.
In several instances we found integrated clinics had reverted to separate OPD and ART operations over time. Review of programmatic reports and investigator experience suggests that this occurred for different reasons in different clinics. For example, in some clinics departmental managers sought to maintain influence over ‘their domain’ and shunned an integrated approach where they perceived it to involve more work or to affect ‘their area’ of work. A second reason identified was related to inadequate infrastructure, which forced managers to make decisions about patient care pathways in particular, based on infection control risk. A third reason for reversion to separate operations was related to staff turnover. New or incoming staff who had not received the Integrated Systems Training tended to carry out their duties as if operating in still-separate departments. Contrary to the implementers’ expectations, existing staff often failed to orient new staff in integrated operations. Over time, therefore, and with continuous staff turnover, some clinics (especially more remote sites receiving less project follow-up) reverted to better-known practices of separated OPD and ART. These experiences align with the well-documented slow-pace of institutional change generally, and highlight the importance of understanding individual and institutional agendas before and while attempting such reform.
Recent commentaries have tended to emphasize the potential for integrated services to create organizational and material efficiencies (Deo et al. 2012). Both the facility survey and interview findings from this study demonstrate that integration did facilitate efficiencies, albeit to varying extents across clinics. However, an equally if not more important finding was the potential for service integration to strengthen organizational culture and staff relationships, in turn facilitating more collaborative and motivated service delivery. Explicit examples included the way in which unified duty rosters and staff responsibilities had shifted work culture away from an ‘us and them’ approach and facilitated team work and capacity building between more senior and junior staff. Several managers also noted that following integration they felt empowered to make further adjustments and modifications to clinic operations, as they became accustomed to a more fluid way of thinking about space, systems and staffing. This outcome is less widely recognized in the context of the integration debate and remains difficult to measure or quantify (Mathieu et al. 2006). Nonetheless, strengthened work culture and improved staff relations represent a potentially critical feature of this and similar integrated service models in poorly resourced primary health care clinics in sub-Saharan Africa where the constant pressure to multi-task can result in extremely low morale (Mushi et al. 2011). In such a context, facility-level leadership and adaptation and intra-clinic communication form an important platform for both basic and improved service-delivery outputs (Leykum et al. 2010; Kiwanuka et al. 2011; Scott et al. 2011).
Despite the reported benefits of this intervention, a recurring theme arising from this research was that integration at the level of primary care services alone cannot act as a panacea for weak health systems. Health systems at all levels, including at point-of-care, are complex and context-specific, and functional clinic systems require both ‘hardware’—such as human resources, infrastructure and medical supplies—and ‘software’—such as clinic systems, managerial style and team-work (Ssengooba et al. 2007). In this study, meso- and macro-level problems related to insufficient human resources, inappropriate or poorly maintained infrastructure and weak health financing were identified as factors that limited or even nullified the benefits of service integration (Lehmann et al. 2009; Atun et al. 2010b). As one clinic manager noted, despite reallocation of rooms enabling more efficient use of space, the new model of service delivery was unable to overcome a basic lack of space. This resulted in some rooms being used concurrently for different duty-stations, affecting both the quality and efficiency of services. Conversely, a different manager whose facility had previously benefited from donor-funded infrastructure upgrades noted that the reorganization of duty stations resulting from integration ‘reduced duplication’, ‘freed-up space’ and enabled space to be ‘used evenly’, producing overall positive outcomes. This finding serves to re-emphasize the fact that contextual variability (in this case, facility-level infrastructure) plays an important mediating role in progress towards more broad-reaching programmatic health system and public health goals (Atun et al. 2010a).
Conclusions
The purpose of this study was not to quantify the impact of integration on the quality of medical care, although this may constitute a valid research question in its own right. Rather, by adopting a mixed methods approach and triangulating data from various sources, we sought to provide a more complete picture of the possibilities and challenges inherent to integrated service delivery in this setting, which would not have been possible using a single method (Creswell et al. 2003). The study was observational (enumerating the changes in service organization resulting from integration), as well as exploratory, capturing health care providers’ experiences of that change. By highlighting the context-specific nature of both advantages and disadvantages related to the implementation of this model in Zambia, this work may provide a basis for analytic generalizations; that is, general conclusions derived from specific experiences that provide insights useful for testing in other settings (Gilson et al. 2011).
Our results suggest that while implementation of this model of integrated service delivery may result in more efficient allocation of human and clinical resources, the impact on measurable service-delivery outputs remains heavily influenced by other meso- and macro-level determinants. A more consistently identified benefit of integration from the providers’ perspective was the model’s capacity to strengthen organizational culture and staff relationships, in turn facilitating more collaborative and motivated service delivery. Consideration of these potential benefits, as well as careful assessment of the inherent challenges posed by ongoing human resource shortages and inadequate infrastructure in this setting, should form part the planning process for similar initiatives seeking to integrate HIV care and treatment into primary care service-delivery.
Acknowledgements
The authors acknowledge the staff and patients of the integrated primary health centres, particularly those staff members who consented to be interviewed, and officials from Lusaka District Health Team for their support and encouragement.
Funding
The integration programmes described in this manuscript and elsewhere were supported by a multi-country grant to the Elizabeth Glaser Pediatric AIDS Foundation from the US Centers for Disease Control and Prevention (U62/CCU12354); www.pedaids.org/www.cdc.gov. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
None declared.
References
- Atun R, de Jongh T, Secci F, Ohiri K, Adeyi O. Integration of targeted health interventions into health systems: a conceptual framework for analysis. Health Policy and Planning. 2010a;25:104–11. doi: 10.1093/heapol/czp055. [DOI] [PubMed] [Google Scholar]
- Atun R, de Jongh T, Secci F, Ohiri K, Adeyi O. A systematic review of the evidence on integration of targeted health interventions into health systems. Health Policy and Planning. 2010b;25:1–14. doi: 10.1093/heapol/czp053. [DOI] [PubMed] [Google Scholar]
- Central Statistical Office and Ministry of Health. Zambia Demographic and Health Survey 2007. Lusaka, Zambia: Central Statistical Office; 2009. [Google Scholar]
- Cohn J, Russell A, Baker B, et al. Using global health initiatives to strengthen health systems: a civil society perspective. Global Public Health. 2011;6:687–702. doi: 10.1080/17441692.2010.521165. [DOI] [PubMed] [Google Scholar]
- Coker R, Balen J, Mounier-Jack S, et al. A conceptual and analytical approach to comparative analysis of country case studies: HIV and TB control programmes and health systems integration. Health Policy and Planning. 2010;25(Suppl. 1):i21–31. doi: 10.1093/heapol/czq054. [DOI] [PubMed] [Google Scholar]
- Conseil A, Mounier-Jack S, Coker R. Integration of health systems and priority health interventions: a case study of the integration of HIV and TB control programmes into the general health system in Vietnam. Health Policy and Planning. 2010;25(Suppl. 1):i32–6. doi: 10.1093/heapol/czq055. [DOI] [PubMed] [Google Scholar]
- Creswell JW, Piano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications; 2007. [Google Scholar]
- Creswell JW, Plano Clark VJ, Hanson WE. A Handbook of Mixed Methods in Social and Behavioural Research. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Deo S, Topp SM, Garcia A, Soldner M, Yagci Sokat K, et al. Modeling the Impact of Integrating HIV and Outpatient Health Services on Patient Waiting Times in an Urban Health Clinic in Zambia. PLoS ONE. 2012;7:e35479. doi: 10.1371/journal.pone.0035479. doi:10.1371/journal.pone.0035479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sadr W, Abrams E. Scale-up of HIV care and treatment: can it transform healthcare services in resource-limited settings? AIDS. 2007;21:S65–S70. doi: 10.1097/01.aids.0000298105.79484.62. [DOI] [PubMed] [Google Scholar]
- El-Sadr WM, Rabkin M, Atun R, De Cock KM. Bridging the divide. Journal of Acquired Immune Deficiency Syndromes. 2011;57(Suppl. 2):S59–60. doi: 10.1097/QAI.0b013e31821dba91. [DOI] [PubMed] [Google Scholar]
- Frenk J. Reinventing primary health care: the need for systems integration. The Lancet. 2009;374:170–3. doi: 10.1016/S0140-6736(09)60693-0. [DOI] [PubMed] [Google Scholar]
- Gilson L, Hanson K, Sheikh K, et al. Building the field of health policy and systems research: social science matters. PLoS Medicine. 2011;8:e1001079. doi: 10.1371/journal.pmed.1001079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JB, Hatwiinda SM, Randels KM, et al. Early lessons from the integration of tuberculosis and HIV services in primary care centers in Lusaka, Zambia. International Journal of Tuberculosis and Lung Disease. 2008;12:773–9. [PubMed] [Google Scholar]
- Kiwanuka SN, Rutebemberwa E, Nalwadda C, et al. Interventions to manage dual practice among health workers. Cochrane Database of Systematic Reviews. 2011;7:CD008405. doi: 10.1002/14651858.CD008405.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodner DL, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications–a discussion paper. International Journal of Integrated Care. 2002;2:e12. doi: 10.5334/ijic.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann U, Van Damme W, Barten F, Sanders D. Task shifting: the answer to the human resources crisis in Africa? Human Resources for Health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine R, Oomman N. Global HIV/AIDS funding and health systems: searching for the win-win. Journal of Acquired Immune Deficiency Syndromes. 2009;52:S3–S5. doi: 10.1097/QAI.0b013e3181bbc807. [DOI] [PubMed] [Google Scholar]
- Leykum LK, Parchman M, Pugh J, et al. The importance of organizational characteristics for improving outcomes in patients with chronic disease: a systematic review of congestive heart failure. Implementation Science. 2010;5:66. doi: 10.1186/1748-5908-5-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lush L, Cleland J, Walt G, Mayhew S. Integrating reproductive health: myth and ideology. Bulletin of the World Health Organization. 1999;77:771–7. [PMC free article] [PubMed] [Google Scholar]
- Mathieu JE, Gilson LL, Ruddy TM. Empowerment and team effectiveness: an empirical test of an integrated model. Journal of Applied Psychology. 2006;91:97–108. doi: 10.1037/0021-9010.91.1.97. [DOI] [PubMed] [Google Scholar]
- Mayhew SH, Lush L, Cleland J, Walt G. Implementing the integration of component services for reproductive health. Studies in Family Planning. 2000;31:151–62. doi: 10.1111/j.1728-4465.2000.00151.x. [DOI] [PubMed] [Google Scholar]
- Mukherjee J, Eustache F. Community health workers as a cornerstone for integrating HIV and primary healthcare. AIDS Care. 2007;19(Suppl. 1):S73–S82. doi: 10.1080/09540120601114485. [DOI] [PubMed] [Google Scholar]
- Mushi HP, Mullei K, Macha J, et al. The challenges of achieving high training coverage for IMCI: case studies from Kenya and Tanzania. Health Policy and Planning. 2011;25:395–404. doi: 10.1093/heapol/czq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolic IA, Stanciole AE, Zaydman M. Chronic Emergency: Why NCDs Matter. Washington, DC: The World Bank; 2011. [Google Scholar]
- Price JE, Leslie JA, Welsh M, Binagwaho A. Integrating HIV clinical services into primary health care in Rwanda: a measure of quantitative effects. AIDS Care. 2009;21:608–14. doi: 10.1080/09540120802310957. [DOI] [PubMed] [Google Scholar]
- Rabkin M, El-Sadr WM. Why reinvent the wheel? Leveraging the lessons of HIV scale-up to confront non-communicable diseases. Global Public Health. 2011;6:247–56. doi: 10.1080/17441692.2011.552068. [DOI] [PubMed] [Google Scholar]
- Rutenberg N, Baek C. Field experiences integrating family planning into programs to prevent mother-to-child transmission of HIV. Studies in Family Planning. 2005;36:235–45. doi: 10.1111/j.1728-4465.2005.00064.x. [DOI] [PubMed] [Google Scholar]
- Scott V, Mathews V, Gilson L. Constraints to implementing an equity-promoting staff allocation policy: understanding mid-level managers’ and nurses’ perspectives affecting implementation in South Africa. Health Policy and Planning. 2011;27:138–46. doi: 10.1093/heapol/czr020. [DOI] [PubMed] [Google Scholar]
- Shigayeva A, Atun R, McKee M, Coker R. Health systems, communicable diseases and integration. Health Policy and Planning. 2010;25(Suppl. 1):i4–20. doi: 10.1093/heapol/czq060. [DOI] [PubMed] [Google Scholar]
- Smith E, Murray SF, Yousafzai AK, Kasonka L. Barriers to accessing safe motherhood and reproductive health services: the situation of women with disabilities in Lusaka, Zambia. Disabil Rehabil. 2004;26:121–7. doi: 10.1080/09638280310001629651. [DOI] [PubMed] [Google Scholar]
- Ssengooba F, Rahman SA, Hongoro C, et al. Health sector reforms and human resources for health in Uganda and Bangladesh: mechanisms of effect. Human Resources for Health. 2007;5:3. doi: 10.1186/1478-4491-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terris-Prestholt F, Kumaranayake L, Ginwalla R, et al. Integrating tuberculosis and HIV services for people living with HIV: costs of the Zambian ProTEST Initiative. Cost Effectiveness and Resource Allocation. 2008;6:2. doi: 10.1186/1478-7547-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp SM, Chipukuma JM, Chiko MM, et al. Opt-out provider-initiated HIV testing and counselling in primary care outpatient clinics in Zambia. Bulletin of the World Health Organization. 2011;89:328–35A. doi: 10.2471/BLT.10.084442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp SM, Chipukuma JM, Giganti M, et al. Strengthening health systems at facility-level: feasibility of integrating antiretroviral therapy into primary health care services in Lusaka, Zambia. PLoS One. 2010;5:e11522. doi: 10.1371/journal.pone.0011522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Resources and funding for AIDS. 2008. Online at: http://www.unaids.org/en/PolicyAndPractice/ResourcesAndFunding/default.asp, accessed 6 October 2011.
- Vivio D, Fullerton JT, Forman R, et al. Integration of the practice of active management of the third stage of labor within training and service implementation programming in Zambia. Journal of Midwifery and Women’s Health. 2010;55:447–54. doi: 10.1016/j.jmwh.2010.02.015. [DOI] [PubMed] [Google Scholar]
- WHO. (2008). Towards Universal Access: Scaling up the Prioirty HIV/AIDS Interventison in the Health Sector. Progress Report. Online at: http://www.who.int/entity/hiv/pub/towards_universal_access_report_2008.pdf. Geneva, accessed 26 June 2012.
- WHO. Noncommunicable Diseases: Country Profiles 2011. Geneva: World Health Organization; 2011. [Google Scholar]