Abstract
Background and Aim:
Results of previous studies have been conflicting on the efficacy of extracorporeal shock wave therapy (ESWT) in the treatment of plantar fasciitis. We evaluated the effects of ESWT on plantar fasciitis in terms of ultrasonographic and subjective evaluations.
Materials and Methods:
In this randomized placebo-controlled trial, patients with plantar fasciitis were assigned to receive ESWT (4000 shock waves/session of 0.2 mJ/mm2) in 3 sessions at weekly intervals) or sham therapy (n = 20 in each group). Outcomes were documented by the ultrasonographic appearance of the aponeurosis and by patients’ pain scores, performed at baseline and 12 weeks after completion of the therapy.
Results:
The two groups were similar in baseline characteristics. Over the study period, plantar fascia thickness significantly reduced in the ESWT group (4.1 ± 1.3 to 3.6 ± 1.2 mm, P < 0.001), but slightly increased in the sham group (4.1 ± 0.8 to 4.5 ± 0.9 mm, P = 0.03). Both groups showed significant pain improvement over the course of the study (P < 0.001), though pain scores were significantly more reduced in the ESWT than the sham group (-4.2 ± 2.9 vs. -2.7 ± 1.8, P = 0.049).
Conclusions:
Extracorporeal shock wave therapy contributes to healing and pain reduction in plantar fasciitis and ultrasound imaging is able to depict the morphologic changes related to plantar fasciitis as a result of this therapy.
Keywords: Extracorporeal shock wave therapy, plantar fasciitis, ultrasound
INTRODUCTION
Plantar fasciitis is one of the most common causes of foot pain in adults, with the peak incidence occurs between ages 40 and 60 years in the general population.[1] In up to a third of the cases it may be bilateral, and heel spurs often coexist, but whether they have a causal role in the etiology of the disease is still unknown.[2,3] The etiology of plantar fasciitis is multifactorial. Suggested risk factors include those conditions that increase the pressure at the plantar surface such as obesity, prolonged standing, flat feet, and reduced ankle dorsiflexion.[4] The high incidence in runners suggests that, at least in this population, plantar fasciitis might be due to an injury by repetitive microtrauma.[5,6]
The diagnosis of plantar fasciitis is clinical and local point tenderness is the hallmark for diagnosis, while laboratory testing is not helpful nor necessary for the diagnosis.[7] However, radiography is required to rule out other disorders, especially calcaneal stress fractures. Ultrasonography of the foot is also useful in diagnosis and treatment follow-ups with indicating plantar fascial thickening, hypoechogenicity at the insertion upon the calcaneus, and features of edema including blurring of the boundary between the fascia and surrounding tissues and decreased echogenicity.[8–10] Diagnostic accuracy of ultrasonography for the diagnosis of plantar fasciitis is acceptable (sensitivity 80% and specificity 88.5%),[11] and Doppler ultrasound can improve the accuracy and provide additional information on local hyperemia as well.[12]
The treatment of plantar fasciitis is primarily conservative, initially with rest and icing to give pain relief. Non-steroidal anti-inflammatory drugs (NSAIDs), local injection of steroids, and electrotherapy and physiotherapy with stretching exercises are also used.[7] In about 10% of the cases who do not respond to such treatments, surgical intervention is suggested.[13]
Extracorporeal shock wave therapy (ESWT) is a noninvasive procedure used in rehabilitation therapy that is recently being applied in the treatment of tendinopathies and also plantar fasciitis.[14–20] In ESWT, shock waves are generated by means of electrohydraulic, piezoelectric, and electromagnetic methods. There are some possible mechanisms mentioned for the efficacy of shock wave therapy. The transmitted waves may have effects on physiology of pain receptor,[21] and also, through microtrauma, they may initiate healing processes by the release of molecular agents and growth factors leading to neovascularization.[22]
Despite increasing use of ESWT in the treatment of plantar fasciitis, few well-controlled trials have been conducted to approve its efficacy with conflicting results.[14,20,23] Therefore, we conducted a randomized, placebo-controlled trial to evaluate the efficacy of ESWT in the management of plantar fasciitis. The outcome was documented by the ultrasonographic appearance of the aponeurosis, as well as by subjective pain scores.
MATERIALS AND METHODS
Patients and settings
This randomized, placebo-controlled trial was conducted from Jun 2010 to Jul 2011 on adult patients with a clinical diagnosis of plantar fasciitis referred to the outpatient clinics of Alzahra University Hospital, Isfahan (IRAN). Patients with plantar heel pain for at least three months and point tenderness at or near the medial calcaneal insertion of the plantar fascia, who had no satisfactory response to common treatments such as NSAIDs and physiotherapy were included. Patients with diabetes, additional foot or ankle pathology (including instability, arthritis, generalized polyarthritis, diffuse heel pad tenderness), local dermatological problems, neurological abnormalities, history of recent trauma or foot surgery, connective tissue or infectious diseases, malignancy, or vasculitis and pregnant patients or those who received anticoagulant therapy in the preceding six months were not included. Considering type I error (alpha) = 0.05 and study power = 80%, with minimum expected difference of 1 score in 11-point scale for pain assessment, the sample size was calculated as at least 20 patients in each group. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences and informed consent was obtained from all patients. Also, the trial was registered in Iranian Registry of Clinical Trials IRCT2012072910439N1.
Intervention
Patients were randomly assigned (by a random table list) to receive ESWT (n = 20) or identical sham therapy as the placebo (n = 20) by weekly interval for three consecutive weeks. We used the site of maximum local tenderness as the target area for shock waves with Duolith SD1 shock wave machine. Patient in the intervention group received 2000 focused shock waves and 2000 radial pulses in three sessions (4000 shock waves/session of 0.2 mJ/mm2) at weekly intervals. ESWT dose and treatment schedule were based on the previous studies.[14,20,23,24,25] For the placebo group sham treatment was done where standard contact of radial and focus probe with the skin was provided. The machine makes a noise with every shock wave delivered and, in order to enhance the sham design, minimal energy pulses (0.04 mJ/mm2) were generated.[23,24]
Assessments
Ultrasonographic evaluation was carried out before and after the therapy. Ultrasound was performed by the same radiologist, using a 10 MHz linear array transducer. Both heels of the participants were scanned in two-dimensional (2D) real-time B mode. We took care to obtain comparable views of the contralateral sides. Sagital imaging of the plantar fascia was performed with the transducer aligned along the longitudinal axis of the aponeurosis. Quantitative evaluation of plantar fasciitis was achieved by measurement of its thickness about 2 cm distal of the medial calcaneal tuberosity. In addition, qualitative assessment including echogenic appearance of plantar fascia and its fibrillary pattern was done. For subjective pain assessment, all subjects completed a numerical rating scale (NRS) for foot pain (from 0 = no pain to 10 = the most severe pain) during the daily activity.
All assessments (pain and ultrasonographic evaluation) were repeated three months after completion of the therapy. Along this time, conservative managements including stretching exercise, using NSAIDs, and heel pad were considered in both groups.
Statistical analysis
Data were analyzed with SPSS software for windows, version 16.0 (SPSS Inc., Chicago IL., USA). A paired samples t-test was used to ascertain significant changes in both plantar fascia thickness and subjective sub-calcaneal pain over the experimental period, and an independent t-test was used for detecting any significant differences in these two parameters between the two groups. The Pearson correlation coefficient was employed to investigate the relationship between continuous variables. A result was considered to be statistically significant if the observed significance level (P value) was <0.05.
RESULTS
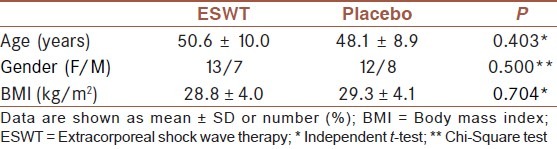
During the study period, 40 patients with plantar fasciitis were enrolled and completed the study [Figure 1]. Demographic characteristics of the patients are outlined in Table 1. There was no significant difference between the two groups in baseline characteristics.
Figure 1.
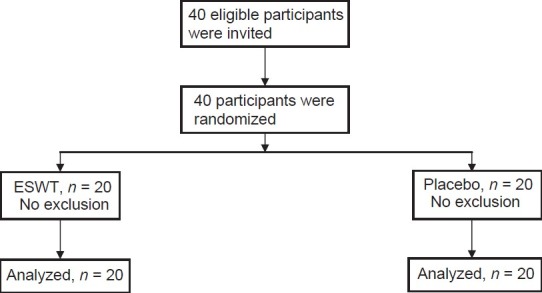
Participants’ flow diagram
Table 1.
Demographic characteristics of the two groups
Data regarding plantar fascia thickness and pain scores are presented in Table 2. In two patients who had severe pain, abnormal fluid collection was seen surrounding the plantar fascia. Initially there were no significant differences between the mean plantar fascia thickness of the two groups (P = 0.95). After treatment, the mean plantar fascia thickness was significantly decreased in the ESWT group (P < 0.001), while it was slightly increased in the placebo group (P = 0.03), Figure 2.
Table 2.
Comparison of pain scores and plantar fascia thickness before and after the study within and between the two groups
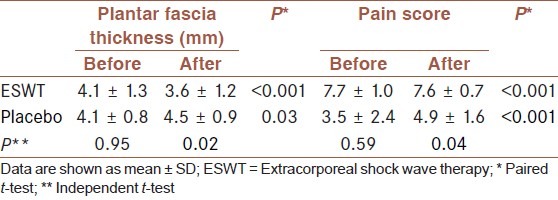
Figure 2.
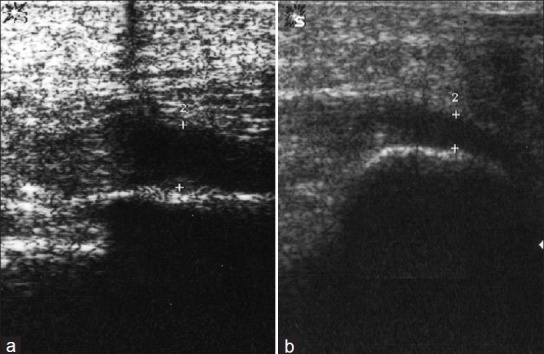
Post-treatment plantar fascia thickness in the placebo (a) and ESWT (b) groups
Regarding the NRS pain scores, no significant difference were observed between the pain scores of the two groups at baseline (P = 0.59), but after three months follow-up, pain scores was significantly lower in the ESWT group than in the placebo group (P = 0.04). Both groups showed significant pain improvement over the course of the study, although reduction of NRS score in the intervention group was significantly greater than in the placebo group (-4.2 ± 2.9 vs. -2.7 ± 1.8, P = 0.049).
To find factors associated with better response to ESWT, we splatted the groups and analyzed data from the ESWT group. Results showed a significant inverse correlation between plantar fascia thickness change and BMI (r = -0.597, P = 0.005). The association between change in pain score and change in plantar fascia thickness was not significant (r = 0.365, P = 0.114).
DISCUSSION
There are various options for the treatment of plantar fasciitis, but a lot of them are not satisfactory effective and some of them are associated with risks.[7] For example, glucocorticoid injections can provide temporary pain relief; however, repeated injections may cause atrophy of the heel pad,[26] and even plantar fascia rupture.[27] Surgical interventions, on the other hand, can alter the biomechanics of the foot[28] and prolonged the healing process.[29] Accordingly, ESWT has been proposed as a therapeutic option for plantar fasciitis, as well as some other musculoskeletal complaints.[18] During the past decade, ESWT has become increasingly used worldwide, and based on some well-controlled trials; recently it was approved by the FDA for treatment of plantar fasciitis in the USA.[30] A placebo-controlled multicentre trial of ESWT by Haake and colleagues in subjects with chronic plantar fasciitis indicated superior improvement in the active treatment than the placebo group.[20] In another randomized trial, Rompe et al., assigned patients to stretching or low energy shock wave therapy and at the 2-month assessment authors found a greater mean change in Foot Function Index cumulative score and a higher patient satisfaction for those who were treated with stretching. These results were stable at the 4-month follow-up, but no difference found between the groups at the 15-month follow-up, though use of NSAIDs was more common among patients treated with shock wave therapy.[31] In another placebo-controlled trial by Speed et al., on adults with plantar fasciitis, no beneficial effects were observed for shock wave therapy (0.12 mJ/mm2) versus the sham placebo over a 6-month period.[23] These results, however, might be due to the moderate dose ESWT effects comparable with placebo effects. The differences between various studies in the efficacy of ESWT in plantar fasciitis may be related to a number of factors including differences in study populations, heterogeneity of treatment parameters such as shock wave intensity, geometry of the shock wave focus, focal energy, different placebos and different machine design. Use of different outcome measures can also prevent direct comparisons between studies.
There is no consensus on the appropriate ESWT dosage and treatment parameters remain empirical. An emphasis is placed upon the use of a feasible regime with minimal side effects. Although the technique is widely reported to be safe, there is a potential for hemorrhage and local soft tissue damage through cavitations.[32] This appears to be more likely with the high doses. For this reason, a moderate radial and focus dose regime using an electromagnetic generator was chosen in our study, which avoided the need for administration of local anesthetic or significant post- treatment rest. Significant adverse effects were not noted in our study, in agreement with the experience of others[33] and the results indicated that moderate dose of ESWT has significant beneficial effects over placebo. Although, pain intensity in the sham group was significantly reduced over the experimental period, ultrasonograghy showed slightly increase in plantar fascia thickness. These results indicate that other factors can lead to false impressions of a placebo effect, such as spontaneous improvement and fluctuation of symptoms.
CONCLUSIONS
In summary, while ultrasound imaging is able to depict the morphologic changes related to plantar fasciitis, ESWT can contribute to healing and pain reduction in plantar fasciitis. Further studies are required to find the mechanisms of action of ESWT in the treatment of plantar fasciitis.
ACKNOWLEDGMENTS
This study was supported by the Isfahan University of Medical Sciences (Research project Number 389450). Authors are thankful to Dr. Ali Gholamrezaei who helped us in data analysis and editing this report.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Tu P, Bytomski JR. Diagnosis of heel pain. Am Fam Physician. 2011;84:909–16. [PubMed] [Google Scholar]
- 2.Labovitz JM, Yu J, Kim C. The role of hamstring tightness in plantar fasciitis. Foot Ankle Spec. 2011;4:141–4. doi: 10.1177/1938640010397341. [DOI] [PubMed] [Google Scholar]
- 3.Levy JC, Mizel MS, Clifford PD, Temple HT. Value of radiographs in the initial evaluation of nontraumatic adult heel pain. Foot Ankle Int. 2006;27:427–30. doi: 10.1177/107110070602700607. [DOI] [PubMed] [Google Scholar]
- 4.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for Plantar fasciitis: A matched case-control study. J Bone Joint Surg Am. 2003;85:872–7. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Knobloch K, Yoon U, Vogt PM. Acute and overuse injuries correlated to hours of training in master running athletes. Foot Ankle Int. 2008;29:671–6. doi: 10.3113/FAI.2008.0671. [DOI] [PubMed] [Google Scholar]
- 6.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd- Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician. 2011;84:676–82. [PubMed] [Google Scholar]
- 8.Mahowald S, Legge BS, Grady JF. The correlation between plantar fascia thickness and symptoms of plantar fasciitis. J Am Podiatr Med Assoc. 2011;101:385–9. doi: 10.7547/1010385. [DOI] [PubMed] [Google Scholar]
- 9.McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: A systematic review and meta-analysis. J Foot Ankle Res. 2009;2:32. doi: 10.1186/1757-1146-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karabay N, Toros T, Hurel C. Ultrasonographic evaluation in plantar fasciitis. J Foot Ankle Surg. 2007;46:442–6. doi: 10.1053/j.jfas.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Sabir N, Demirlenk S, Yagci B, Karabulut N, Cubukcu S. Clinical utility of sonography in diagnosing plantar fasciitis. J Ultrasound Med. 2005;24:1041–8. doi: 10.7863/jum.2005.24.8.1041. [DOI] [PubMed] [Google Scholar]
- 12.Walther M, Radke S, Kirschner S, Ettl V, Gohlke F. Power Doppler findings in plantar fasciitis. Ultrasound Med Biol. 2004;30:435–40. doi: 10.1016/j.ultrasmedbio.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Neufeld SK, Cerrato R. Plantar fasciitis: Evaluation and treatment. J Am Acad Orthop Surg. 2008;16:338–46. doi: 10.5435/00124635-200806000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Roehrig GJ, Baumhauer J, DiGiovanni BF, Flemister AS. The role of extracorporeal shock wave on plantar fasciitis. Foot Ankle Clin. 2005;10:699–712. doi: 10.1016/j.fcl.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Chuckpaiwong B, Berkson EM, Theodore GH. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome predictors. J Foot Ankle Surg. 2009;48:148–55. doi: 10.1053/j.jfas.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Gerdesmeyer L, Frey C, Vester J, Maier M, Weil L, Jr, Weil L, Sr, et al. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: Results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med. 2008;36:2100–9. doi: 10.1177/0363546508324176. [DOI] [PubMed] [Google Scholar]
- 17.Seil R, Wilmes P, Nuhrenborger C. Extracorporeal shock wave therapy for tendinopathies. Expert Rev Med Devices. 2006;3:463–70. doi: 10.1586/17434440.3.4.463. [DOI] [PubMed] [Google Scholar]
- 18.Sems A, Dimeff R, Iannotti JP. Extracorporeal shock wave therapy in the treatment of chronic tendinopathies. J Am Acad Orthop Surg. 2006;14:195–204. doi: 10.5435/00124635-200604000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Ogden JA. Extracorporeal shock wave therapy for plantar fasciitis: Randomised controlled multicentre trial. Br J Sports Med. 2004;38:382. doi: 10.1136/bjsm.2004.011601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haake M, Buch M, Schoellner C, Goebel F, Vogel M, Mueller I, et al. Extracorporeal shock wave therapy for plantar fasciitis: Randomised controlled multicentre trial. BMJ. 2003;327:75–77. doi: 10.1136/bmj.327.7406.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu YH, Lun JJ, Chen WS, Chong FC. The electrophysiological and functional effect of shock wave on peripheral nerves. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:2369–72. doi: 10.1109/IEMBS.2007.4352803. [DOI] [PubMed] [Google Scholar]
- 22.Mariotto S, de Prati AC, Cavalieri E, Amelio E, Marlinghaus E, Suzuki H. Extracorporeal shock wave therapy in inflammatory diseases: Molecular mechanism that triggers anti-inflammatory action. Curr Med Chem. 2009;16:2366–72. doi: 10.2174/092986709788682119. [DOI] [PubMed] [Google Scholar]
- 23.Speed CA, Nichols D, Wies J, et al. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res. 2003;21:937–40. doi: 10.1016/S0736-0266(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 24.Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: A randomized controlled trial. JAMA. 2002;288:1364–72. doi: 10.1001/jama.288.11.1364. [DOI] [PubMed] [Google Scholar]
- 25.Gollwitzer H, Diehl P, von KA, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: A prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg. 2007;46:348–57. doi: 10.1053/j.jfas.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 26.Tatli YZ, Kapasi S. The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies. Curr Rev Musculoskelet Med. 2009;2:3–9. doi: 10.1007/s12178-008-9036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19:91–7. doi: 10.1177/107110079801900207. [DOI] [PubMed] [Google Scholar]
- 28.Tweed JL, Barnes MR, Allen MJ, Campbell JA. Biomechanical consequences of total plantar fasciotomy: A review of the literature. J Am Podiatr Med Assoc. 2009;99:422–30. doi: 10.7547/0990422. [DOI] [PubMed] [Google Scholar]
- 29.Sammarco GJ, Helfrey RB. Surgical treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 1996;17:520–6. doi: 10.1177/107110079601700902. [DOI] [PubMed] [Google Scholar]
- 30.Henney JE. From the food and drug administration: shock wave for heel pain. JAMA. 2000;284:2711. doi: 10.1001/jama.284.21.2711-jfd00010-2-1. [DOI] [PubMed] [Google Scholar]
- 31.Rompe JD, Cacchio A, Weil L, Jr, Furia JP, Haist J, Reiners V, et al. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surg Am. 2010;92:2514–22. doi: 10.2106/JBJS.I.01651. [DOI] [PubMed] [Google Scholar]
- 32.Delius M, Draenert Y, Bosner M. Effect of extracorporeal shock waves on bone: A review of shock wave experiments and the mechanisms of action of shock wave action. In: Siebert W, Buch M, editors. Extracorporeal Shock Waves in Orthopaedics. Berlin: Springer-Verlag; 1997. [Google Scholar]
- 33.Ogden JA, Alvarez RG, Marlow M. Shockwave therapy for chronic proximal plantar fasciitis: A meta-analysis. Foot Ankle Int. 2002;23:301–8. doi: 10.1177/107110070202300402. [DOI] [PubMed] [Google Scholar]


