Abstract
Objective:
Parental obesity has been identified as a predominant risk factor for childhood overweight and obesity. We investigated the relationship between parent and child obesity in South Korea, particularly linked with varying family structures.
Subjects and methods:
Data for households with children aged 2–18 years were taken from the pooled data of the Korea National Health and Nutrition Examination Survey (KNHANES) 2007–2010 conducted by the Korea Centers for Disease Control and Prevention (KCDC). The sample consisted of 17 453 individuals (7879 children and 9574 adults) from 5048 households with children for this study. Children's overweight and obesity prevalence was compared using both International Obesity Taskforce (IOTF) and KCDC cutoff points according to parental weight status and household structure. Logistic regression analysis was used.
Results:
Significantly greater odds of overweight and obesity existed among children living with both parents (odds ratio (OR)=3.5, 95% confidence interval (CI): 2.71, 4.65) or one parent (mother: OR=1.6, 95% CI: 1.22, 2.12; father: OR=1.7, 95% CI: 1.37, 1.99). The adjusted ORs for overweight and obesity among children living with overweight mother only or overweight grandparent only were approximately double that of children living with normal-weight mother (OR=2.2, 95% CI: 1.22–3.82) or normal-weight grandparent (OR=2.1, 95% CI: 1.06–4.05).
Conclusion:
Children living with overweight parent(s) or grandparent(s) were positively correlated with the risk for childhood overweight and obesity. Socioeconomic status did not affect the observed relationships in this population, whereas the role of genetic, dietary and activity patterns requires further exploration.
Keywords: children, obesity, overweight, parent, grandparent, family structure
Introduction
In recent decades, the prevalence of childhood overweight and obesity has increased worldwide, with a higher rate of increase projected for South Korea than other high-income countries.1, 2 Over the last 8 years, the prevalence of obesity among South Korean children and adolescents has increased significantly, going from 5.8% in 1997 to 9.7% in 2005 (from 6.1% in 1997 to 11.3% in 2005 for boys and from 5.5% in 1997 to 8.0% in 2005 for girls).3 An extensive literature in other countries has documented the high correlation between child and parental obesity.4, 5, 6
Children are vulnerable to the social and environmental pressures that raise the risk of obesity.7 Clearly, parents affect dietary and activity patterns, particularly among preschoolers and young children, which, ultimately, can impact child weight status.8, 9, 10 While many studies have examined the relationship between parent and child obesity, especially in Europe and the United States, minimal research has examined this in the context of varying household structures, for example, living with both parents vs living in a single parent household.11, 12, 13, 14, 15, 16 Limited research in small samples has explored selected family structure–child obesity relationships in Korea.17, 18, 19
This is the first nationally representative study of this relationship in South Korea.20, 21 We explore the relationship between households headed by both parents, single parents (mother and father) and grandparents, and child overweight and obese status.
Subjects and methods
Study population
We used combined data from the Korea National Health and Nutrition Examination Survey (KNHANES) 2007–2010 conducted by Korea Centers for Disease Control and Prevention (KCDC).22, 23, 24, 25 KNHANES is a cross-sectional and nationally representative survey of non-institutionalized civilians aged 1 year and older in South Korea using a multistage, stratified area probability sampling design for households in different geographic areas and type of residence (apartment vs non-apartment dwelling). Weights indicating the probability of being sampled were assigned to each respondent, enabling the results to represent the entire South Korean population.
The KNHANES consists of four survey components: health interview survey, health behavior survey, health examination survey and nutrition survey. We selected families with children aged 2–18 years who had complete health examination data, representing about 40% of the total sample. The final sample size was 17 453 individuals (7879 children and 9574 adults) from 5048 households with children. KNHANES was approved by the KCDC Institutional Review Board.
Outcome measures
During the Health Examination Survey, height was measured with a SECA 225 (Vogel & Halke, Hamburg, Germany) and body weight was measured on a leveled scale (GL-6000-20, CAS Korea, Seoul, Korea). For each subject, body mass index (BMI) was calculated as weight in kilograms divided by the square of the height in meters.
Definition of obesity in children and adults
Obesity in children was defined according to the BMI cutoff points for age and gender. We determined childhood obesity in terms of BMI26, 27, 28 cutoff points for overweight and obesity defined by the International Obesity Taskforce (IOTF)29, 30 and KCDC.3, 31 The IOTF developed age- and sex-specific definitions of overweight and obesity based on BMI percentile curves that pass through the adult BMI cutoff points of 25 kg m−2 (overweight) and 30 kg m−2 (obesity). We applied these same cutoff points to our data. The KCDC criteria also used age- and sex-specific BMI values and classified children as normal weight (<85th percentile), at risk of overweight (85th to <95th percentile) or obesity (⩾95th percentile) according to the Korean growth charts.32 We classified parents' and other adults' weight status using the World Health Organization (WHO) recommended definition of adult obesity:33 normal weight (BMI <25 kg m−2), overweight (BMI 25–<30 kg m−2) or obesity (BMI ⩾30 kg m−2).
Sociodemographic variables
Parental status was based on the adults with whom each child lived. It was possible to measure both parents: mother, father and grandparent caretakers. Unfortunately, too few households contained both grandparents and one or both adult parents, so we could not unravel multigenerational household structure from caretaker status. Data were unavailable to separate biological from adopted parentage. Sociodemographic variables of interest included were age (2–6, 7–12 and 13–18 years), sex, region (large city, small city and rural), income level (⩾250% minimum cost of living, 120–250% minimum cost of living and <120% minimum cost of living), education of the adult in a household with children (⩾high school diploma vs <high school diploma), education of each parent measured and used (⩾high school diploma in both parents vs <high school diploma in both parents) and household structure (child living with: both parents, mother only, father only and grandparent(s) only).
Statistical analysis
All statistical analyses were conducted using SAS (release 9.2, 2009; SAS Institute Inc., Cary, NC, USA). Chi-square tests were used to examine the prevalence of childhood overweight and obesity according to their parents' and grandparents' weight status among households with children with P<0.05 set for statistical significance. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using multivariable logistic regression models of child overweight and obesity status on adult overweight and obesity status according to household structure. Models were controlled for possible confounding factors including: age groupings, gender, region, income category and education of adult in a household with children.
Results
The demographic and socioeconomic characteristics of the KNHANES population are shown in Table 1. The majority (89.5%) of children lived with both parents, whereas a much smaller proportion was living with a single parent (6.7% living with mothers, 1.4% living with fathers) or grandparents (2.4%). Approximately 70% of adults were educated higher than high school diploma, 46% of the sample population resided in a large city and 41% had income >250% of the poverty threshold.
Table 1. Demographic characteristics of the sample population in KNHANESa, 2007–2010.
| Demographic group | Total |
|---|---|
| Sample size (n) | |
| Number of individuals | 17 453 |
| Children | 7879 |
| Adults | 9574 |
| Number of households with children | 5048 |
| Percent of households with children (%) | 39.8 |
| Mean size of household with children | 3.3 |
| Child gender (%) | |
| Male | 53.0 |
| Age groups of households with children (%) | |
| 2–6 years | 8.9 |
| 7–12 years | 14.3 |
| 13–18 years | 15.5 |
| 19–39 years | 29.6 |
| 40–59 years | 27.1 |
| ⩾60 years | 4.5 |
| Income as percentage of poverty guideline of households with childrenb (%) | |
| Low (<120%) | 17.6 |
| Middle (120–250%) | 41.1 |
| High (⩾250%) | 41.3 |
| Adults (⩾19 years) education of households with children (%) | |
| <High school diploma | 17.2 |
| ⩾High school diploma | 82.8 |
| Region of hosueholds with childrenc (%) | |
| Large city | 44.5 |
| Small city | 40.3 |
| Rural | 15.2 |
| Distribution of households with children (%) | |
| Living with both parents | 89.5 |
| Living with mothers only | 6.7 |
| Living with fathers only | 1.4 |
| Living with grandparents only | 2.4 |
Abbreviations: MCL, minimum cost of living; KNHANES, Korea National Health and Nutrition Examination Survey.
Weighted to be nationally representative.
Calculated values are based on MCL of each year. A family is considered poor if its income falls below the MCL measured by the government as poverty.
Large city: cities with a population size greater than a million; small city: cities with a population size of 50 000 to a million; rural: villages and towns with a population size lesser than 50 000.
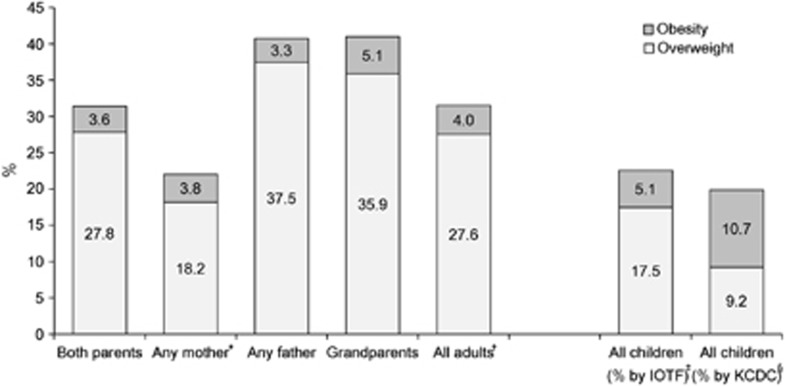
The prevalence of overweight and obesity among all adults in households with children was 27.6% and 4.0%, respectively (Figure 1). These rates differed by gender: nearly twice as many fathers compared with mothers were overweight (37.5% vs 18.2%, respectively). In general, at younger ages, men had higher prevalence rates compared with women.
Figure 1.
The prevalence of overweight and obesity among all age groups in households with children, KNHANES, 2007–2010. *Refers to the percent of (any) mothers/fathers that are overweight or obesity, regardless of household structure. †WHO cutoff points were used to define overweight and obesity in adults (aged ⩾19 years). ‡International Obesity Taskforce (IOTF) cutoff points were used to define overweight and obesity in all children (aged 2–18 years). §Korean cutoff points for children by the Korea Centers for Disease Control and Prevention (KCDC) were used to define overweight and obesity in all children (aged 2–18 years).
Using IOTF cutoff points, three times as many children were classified as overweight compared with obese, at 17.5% and 5.1%, respectively. Using KCDC cutoff points, however, the prevalence of overweight (9.2%) is nearly equal to that of obesity (10.7%). Using KCDC cutoff points, twice as many children in South Korea are considered obese (Figure 1).
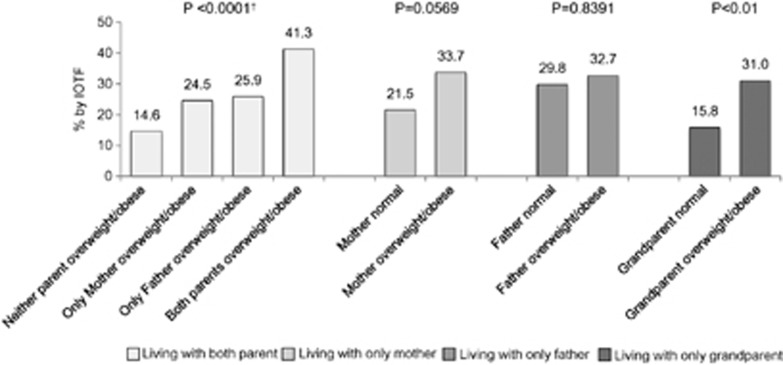
The combined prevalence of child overweight and obesity (using IOTF cutoff points: BMI ⩾25 kg m−2; hereafter overweight and obesity) according to adult weight status by household structure is shown in Figure 2 (results ignoring household structure can be found in Supplementary Information 1). Among children living with parents, 41.3% of children with overweight/obese parents were also overweight/obese, compared with 14.6% of children with normal-weight parents (P<0.001). The prevalence of overweight and obesity among children living with parents when only one parent was overweight/obese was slightly lower than that when both parents were overweight/obese (24.5% among only mother was overweight/obese and 25.9% among only father was overweight/obese; Figure 2). Overweight and obesity prevalence among children living with grandparents only was almost twice as high if the grandparents were also overweight/obese compared with normal weight (31.0 vs 15.8%, respectively; P<0.01). There were no significant differences in the prevalence of child overweight and obesity based on parental overweight and obesity among those living with their mother only (P=0.0569) or father only (P=0.8391). Similar patterns are observed using KCDC cutoff points (Supplementary Information 2–3).
Figure 2.
The prevalence of overweight and obesity* in children according to their parents' weight status in households with children using International Obesity Taskforce (IOTF) cutoff points, KNHANES 2007–2010. *BMI ⩾25 kg m−2 is defined as overweight or obesity. †χ2 tests were used to compare the prevalence of child overweight and obesity according to parents' and grandparents' weight status.
Table 2 shows the adjusted ORs of children's overweight and obesity according to adult weight status (overweight and obese; BMI ⩾25 kg m−2, yes/no) and household structure using IOTF-defined cutoff points. For children living with both parents, the odds were significantly greater for children's overweight and obesity if both parents were overweight/obese (OR=3.5, 95% CI: 2.71–4.65) compared with that when either parent was overweight and obese (mother only (OR=1.6, 95% CI: 1.22, 2.12), father only (OR=1.7, 95% CI: 1.37, 1.99)) (Table 2).
Table 2. Adjusted odds ratiosa, for child overweight and obesityb and obesity by adult weight status and household structure in households with children using IOTF cutoff points, KNHANES, 2007–2010.
| Effect |
By IOTF |
||||
|---|---|---|---|---|---|
|
Overweight and
obesity |
Obesity |
||||
| Adjusted odds ratio | 95% CI | Adjusted odds ratio | 95% CI | ||
| Household structure | Adult weight status | ||||
| Living with both parents | Neither parent overweight and obese | Reference | Reference | ||
| Only mother overweight and obese | 1.6c | 1.22–2.12 | 1.8 | 1.12–2.84 | |
| Only father overweight and obese | 1.7 | 1.37–1.99 | 1.7 | 1.17–2.48 | |
| Both parents overweight and obese | 3.5 | 2.71–4.65 | 5.0 | 3.29–7.54 | |
| Living with only mother | Mother normal weight | Reference | Reference | ||
| Mother overweight and obese | 2.2 | 1.22–3.82 | 3.7 | 1.37–10.21 | |
| Living with only father | Father normal weight | Reference | Reference | ||
| Father overweight and obese | 2.2 | 0.73–6.45 | 3.5 | 0.63–19.57 | |
| Living with only grandparent | Grandparent normal weight | Reference | Reference | ||
| Grandparent overweight and obese | 2.1 | 1.06–4.05 | 1.2 | 0.40–3.42 | |
| Sociodemographic factors | |||||
| Sex | Female | Reference | Reference | ||
| Male | 1.8 | 1.52–2.09 | 2.1 | 1.54–2.97 | |
| Age (years) | 2–6 | Reference | Reference | ||
| 7–12 | 2.3 | 1.87–2.80 | 1.6 | 1.11–2.20 | |
| 13–18 | 1.4 | 1.10–1.72 | 0.7 | 0.46–0.99 | |
| Incomed | High (⩾250%) | Reference | Reference | ||
| Middle (120–250%) | 1.0 | 0.80–1.16 | 0.9 | 0.70–1.27 | |
| Low (<120%) | 1.2 | 0.90–1.54 | 1.4 | 0.93–2.13 | |
| Regione | Rural | Reference | Reference | ||
| Small city | 1.0 | 0.80–1.30 | 0.8 | 0.58–1.16 | |
| Large city | 1.2 | 0.98–1.59 | 0.8 | 0.52–1.12 | |
| Education | <High school diploma | Reference | Reference | ||
| ⩾High school diploma | 1.0 | 0.66–1.42 | 1.5 | 0.84–2.56 | |
| Household size | 1.0 | 0.95–1.12 | 1.0 | 0.85–1.17 | |
Abbreviations: CI, confidence interval; IOTF, International Obesity Taskforce; MCL, minimum cost of living; KNHANES, Korea National Health and Nutrition Examination Survey. Adjusted for child's gender, age, region of residence (large city, small city, rural), highest education of adult in household (⩾12 years vs <12 years) and household income (⩾250% minimum cost of living, 120–250% minimum cost of living, <120% minimum cost of living).
Defined as overweight or obesity, BMI ⩾25 kg m−2 using IOTF cutoff points.
Values in bold indicate statistical significance, P<0.05, based on the 95% CI.
Calculated values based on MCL of each year. A family is considered poor if its income falls below MCL determined by government as poverty guideline.
Large city: cities with population size bigger than a million; small city: cities with population size 50 000 to a million; rural: villages and towns with population size smaller than 50 000.
Among children living with their mother only or grandparents only, the odds of overweight and obesity were significantly greater if the adult in the household was also overweight/obese compared with those children living with normal-weight adult (mother only (OR=2.2, 95% CI: 1.22, 3.82), grandparents only (OR=2.1, 95% CI: 1.06, 4.05)). The highest adjusted OR estimated for obesity was observed among children living with both parents when both parents were overweight/obese (OR=5.0, 95% CI: 3.29, 7.54; see Table 2).
The adjusted odds for child overweight and obesity were significantly higher for males (OR=1.8, 95% CI: 1.52–2.09) compared with females and among 7- to 12-year olds (OR=2.3, 95% CI: 1.87–2.80) and 13- to 18-year olds (OR=1.4, 95% CI: 1.10–1.72) compared with 2- to 6-year olds (Table 2). Similar patterns are observed when overweight and obesity are defined using KCDC cutoff points (Supplementary Information 4).
Discussion
Parental obesity has been identified as a predominant risk factor for childhood overweight and obesity,34, 35 with the heritability of BMI estimated at about 40%.36 Although parental BMI is a readily available marker for the susceptibility to obesity in children,37 the role of household structure according to adult weight status has not previously been examined to the best of our knowledge. In this study, we found that the prevalence of overweight or obesity among children is greater when at least one adult living in the household is also overweight or obesity. Specifically, children living with both parents have significantly increased odds of overweight and obesity if one or both parents are overweight/obese. Living with an overweight/obese mother only or grandparent only was also associated with significantly greater odds of overweight and obesity in children. Results for father were suggestive of a similar relationship if the father was obese, but the sample size was too limited to show a significant relationship.
Numerous studies34, 38, 39, 40, 41, 42 have reported that maternal obesity is a strong independent predictor of childhood obesity. Among Brazilian children, odds of overweight was 1.4 (95% CI: 1.04–1.93) times higher according to maternal overweight (BMI⩾25 kg m−2),42 with similar results observed among elementary school girls in Canada.39 Finally, the ORs of overweight and obesity among preschool children in Japan were significantly positively associated with maternal (OR=2.61, 95% CI: 1.40, 4.85) and parental (both parents) overweight and obesity (OR=2.67, 95% CI: 1.20, 5.92).13 Parents' obesity was associated with overweight of girls aged 2–6 years (OR=2.73, 95% CI: 1.22, 3.40) in a sample of 750 from Seoul, Korea.20 Parents' obesity was positively associated with risk of obesity in children aged 6–19 years (OR=2.81, 95% CI: 1.4–5.64) in a sample of 163 from Asan City, Korea.43 Our results focused on a nationally representative sample of children aged 2–18 years and found an OR of 3.5 that the child would be overweight when both parents were overweight/obese and lower ORs of 1.6 and 1.7 when mother and father were overweight/obese, respectively.
Whitaker et al.34 reported that the ORs for obesity in childhood and young adulthood associated with having one obese parent ranged from 2.2 (95% CI: 1.1, 4.3) at 15–17 years of age to 3.2 (95% CI: 1.8, 5.7) at 1–2 years of age. In this result, the adjusted odds for children being overweight among 7–12 years (OR=2.3, 95% CI: 1.87, 2.80) and 13–18 years (OR=1.4, 95% CI: 1.10, 1.72) were compared with those among 2- to 6-year-old children. There is a higher relationship between parent and children weight status among younger children.18
However, the environmental factors contributing to the expression of obesity among these at-risk children remain unclear.42, 44 Epstein et al. among others reported that parental education and household income are independently associated with overweight and obesity.42 But in our study, we did not find any socioeconomic status measures linked with overweight and obesity.
This study has several limitations. We did not have measures of biological vs adopted parentage. Our sample size for father-headed households was limited. In addition, it is possible that both parental education and income do not affect child obesity because of the relationship between socioeconomic status and parental obesity status. Unfortunately, we feel that we do not have the longitudinal data to unravel this relationship and do not address this potentially important topic.
Childhood obesity is a growing public health issue.43 Although this study adds to our current understanding of the role of the family environment, and household structure in particular, regarding the risk of overweight and obesity among children, more studies are needed to further explore the role of household structure in the context of parental influences.
Results from our study employing a nationally representative sample population suggest that intervention and prevention efforts targeted at families with overweight adults (parents or grandparents), especially where both parents are overweight or in households with overweight single mother, would be effective in obesity prevention programs among children.
Acknowledgments
Funding for this research was provided by the Korea Health Industry Development Institute. We thank Frances Dancy for her helpful administrative assistance; Donna R Miles, PhD, for programming and technical support; and Tom Swasey, for graphic support.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on the Nutrition & Diabetes website (http://www.nature.com/nutd).
Supplementary Material
References
- Popkin BM. The World Is Fat — The Fads, Trends, Policies, and Products That Are Fattening the Human Race. Avery-Penguin Group: New York City, NY, USA; 2008. [Google Scholar]
- WHO Diet, Nutrition and the Prevention of Chronic Disease — Chapter2003
- Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008;51:950–955. [Google Scholar]
- Lake JK, Power C, Cole TJ. Child to adult body mass index in the 1958 British birth cohort: associations with parental obesity. Arch Dis Child. 1997;77:376–380. doi: 10.1136/adc.77.5.376. [DOI] [PubMed] [Google Scholar]
- Food and Nutrition Board . Preventing Childhood Obesity: Health in the Balance. National Academy Press: Washington, DC, USA; 2004. [Google Scholar]
- Committee on Obesity Prevention Policies for Young Children Birch LL, Burns A.(eds)Early Childhood Obesity Prevention Policies Institute of Medicine, National Academy Press: Washington, DC, USA; 2011 [Google Scholar]
- Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ. Obesity prevention: the case for action. Int J Obes Relat Metab Disord. 2002;26:425–436. doi: 10.1038/sj.ijo.0801938. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Harvard University Press; 1979. [Google Scholar]
- Gibson LYBS, Davis EA, Blair E, Jacoby P, Zubrick SR. The role of family and maternal factors in childhood obesity. Med J Australia. 2007;186:591–595. doi: 10.5694/j.1326-5377.2007.tb01061.x. [DOI] [PubMed] [Google Scholar]
- Chen AY, Escarce JJ. Family structure and childhood obesity, Early Childhood Longitudinal Study — Kindergarten Cohort. Prev Chronic Dis. 2010;7:A50. [PMC free article] [PubMed] [Google Scholar]
- Crossman A, Sullivan DA, Benin M. The family environment and American adolescents' risk of obesity as young adults. Soc Sci Med. 2006;63:2255–2267. doi: 10.1016/j.socscimed.2006.05.027. [DOI] [PubMed] [Google Scholar]
- Byrne LK, Cook KE, Skouteris H, Do M. Parental status and childhood obesity in Australia. Pediatr Obes. 2011;6:415–418. doi: 10.3109/17477166.2011.598938. [DOI] [PubMed] [Google Scholar]
- Watanabe E, Lee JS, Kawakubo K. Associations of maternal employment and three-generation families with pre-school children's overweight and obesity in Japan. Int J Obes. 2011;35:945–952. doi: 10.1038/ijo.2011.82. [DOI] [PubMed] [Google Scholar]
- Schmeer KK. Family structure and obesity in early childhood. Soc Sci Res. 2012;41:820–832. doi: 10.1016/j.ssresearch.2012.01.007. [DOI] [PubMed] [Google Scholar]
- McConley RL, Mrug S, Gilliland MJ, Lowry R, Elliott MN, Schuster MA, et al. Mediators of maternal depression and family structure on child BMI: parenting quality and risk factors for child overweight. Obesity. 2011;19:345–352. doi: 10.1038/oby.2010.177. [DOI] [PubMed] [Google Scholar]
- Moens E, Braet C, Bosmans G, Rosseel Y. Unfavourable family characteristics and their associations with childhood obesity: a cross-sectional study. Eur Eating Disord Rev. 2009;17:315–323. doi: 10.1002/erv.940. [DOI] [PubMed] [Google Scholar]
- Kim MK. Overweight among preschool children in Seoul: prevalence and associated factors. Korean J Comm Nutr. 2001;6:121. [Google Scholar]
- Eun-Kyung Kim JP, Ryu So-Yeon, Myeng-Gun Kang. The relationship between parents obesity and childhood obesity cognition and weight-related behaviors. J Korean Soc Matern Child Health. 2006;10:159–168. [Google Scholar]
- Yoo EG, Park SS, Oh SW, Nam GB, Park MJ. Strong parent-offspring association of metabolic syndrome in Korean families. Diabetes Care. 2012;35:293–295. doi: 10.2337/dc11-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Welfare Health Statistics: The Fourth Korea National Health and Nutrition Examination Survey (2007) (in Korean). The Korean Centers for Disease Control and Prevention2008
- Ministry of Health and Welfare Health Statistics: The Fourth Korea National Health and Nutrition Examination Survey (2008) (in Korean). The Korean Centers for Disease Control and Prevention2009
- Ministry of Health and Welfare Health Statistics: The Fourth Korea National Health and Nutrition Examination Survey (2010) (in Korean). The Korean Centers for Disease Control and Prevention2011
- Dinsdale H, Ridler C, Ells LJ.A simple guide to classifying body mass index in children 2011. National Obesity Observatory: Oxford.
- Bellizzi MC, Dietz WH. Workshop on childhood obesity: summary of the discussion. Am J Clin Nutr. 1999;70:173S–175S. doi: 10.1093/ajcn/70.1.173s. [DOI] [PubMed] [Google Scholar]
- Reilly JJ, Dorosty AR, Emmett PM. Avon Longitudinal Study of Pregnancy and Childhood Study Team. Identification of the obese child: adequacy of the body mass index for clinical practice and epidemiology. Int J Obes Relat Metab Disord. 2000;24:1623–1627. doi: 10.1038/sj.ijo.0801436. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Bellizz MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Br Med J. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- Khang YH, Park MJ. Trends in obesity among Korean children using four different criteria. Pediatr Obes. 2011;6:206–214. doi: 10.3109/17477166.2010.490270. [DOI] [PubMed] [Google Scholar]
- Moon JS, Lee SY, Nam CM, Choi J-M, Choe B-K, Seo J-W, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook (in Korean) Korean J Pediatr. 2008;51:1–25. [Google Scholar]
- WHO BMI classification: WHO2012. Available from http://apps.who.int/bmi/index.jsp?introPage=intro_3.html .
- Moll PP, Burns TL, Lauer RM. The genetic and environmental sources of body mass index variability: the Muscatine Ponderosity Family Study. Am J Hum Genet. 1991;49:1243–1255. [PMC free article] [PubMed] [Google Scholar]
- Garn SM, Sullivan TV, Hawthorne VM. Fatness and obesity of the parents of obese individuals. Am J Clin Nutr. 1989;50:1308–1313. doi: 10.1093/ajcn/50.6.1308. [DOI] [PubMed] [Google Scholar]
- Bouchard C, Pérusse L, Rice T, Rao DC. The Genetics of Human Obesity. Marcel Dekker Inc.: New York City, NY, USA; 1998. [Google Scholar]
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. New Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- Heude B, Kettaneh A, Rakotovao R, Bresson JL, Borys JM, Ducimetière P, et al. Anthropometric relationships between parents and children throughout childhood: the Fleurbaix-Laventie Ville Santé Study. Int J Obes. 2005;29:1222–1229. doi: 10.1038/sj.ijo.0802920. [DOI] [PubMed] [Google Scholar]
- O'Loughlin J, Paradis G, Renaud L, Meshefedjian G, Gray-Donald K. Prevalence and correlates of overweight among elementary schoolchildren in multiethnic, low income, inner-city neighbourhoods in Montreal, Canada. Ann Epidemiol. 1998;8:422–432. doi: 10.1016/s1047-2797(98)00009-x. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103:e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- Cutting TM, Fisher JO, Grimm-Thomas K, Birch LL. Like mother, like daughter: familial patterns of overweight are mediated by mothers' dietary disinhibition. Am J Clin Nutr. 1999;69:608–613. doi: 10.1093/ajcn/69.4.608. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- Ramos de Marins VM, Almeida RM, Pereira RA, de Azevedo Barros MB. The relationship between parental nutritional status and overweight children/adolescents in Rio de Janeiro, Brazil. Annu Rev Public Health. 2004;118:43–49. doi: 10.1016/S0033-3506(03)00145-8. [DOI] [PubMed] [Google Scholar]
- Lee S, Kim C, Kim HJ, HS P. Interactive effects of main genotype, caloric intakes, and smoking status on risk of obesity. Asia Pac J Clin Nutr. 2011;20:563–671. [PubMed] [Google Scholar]
- Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. J Am Med Assoc. 1990;264:2519–2623. [PubMed] [Google Scholar]
- Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. New Engl J Med. 1993;329:1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- Kleiser C, Schaffrath Rosario A, Mensink G, Prinz-Langenohl R, Kurth B. Potential determinants of obesity among children and adolescents in Germany: results from the cross-sectional KiGGS Study. BMC Public Health. 2009;9:46. doi: 10.1186/1471-2458-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.