Abstract
For a total knee replacement (TKR) to function well, the patella must track centrally in the trochlear groove. Lateral retinacular release (LR) is performed as an integral step in TKR to avoid maltracking. Patellar resurfacing and infra patellar fat pad excision are other small surgical procedures performed during TKR that can also easily deprive the patella of its vascularity. A three phase bone scan helps in the assessment of patellar vascularity. Literature review reveals a variable association (10-56%) of LR and patellar hypovascularity in Caucasians.
Objective:
LR release done in TKR is known to compromise patellar viability, while its extent and severity is still debated. Our prospective study was undertaken to evaluate the effects of LR on patella along with other variables like patellar resurfacement, fat pad excision, patelloplasty on knees by 99mTechnetium labeled methylene diphosphonate (99mTc MDP) three phase bone scintigraphy (TBS).
Materials and Methods:
45 TKRs were done between Jan 05 and Jan 06. Of them, 15 patients (21 knees) of primary TKR were considered prospectively. Patients undergoing uni/bilateral TKR due to symptomatic knee osteoarthritis were only selected for this study. Pre- and immediate postoperative TBS was done with modified positioning of knee joints (adducted, externally rotated and flexed to 30°) to visualize patellae away from knee joint, which otherwise gets superimposed on the femoral condyles. A follow-up TBS at 8-10 weeks was done in patients showing immediate post-op patellar hypovascularity.
Results:
12/21 knees (57%) needed LR. Of these 12 knees, 8 (66%) showed hypovascularity; whereas 9 knees with no LR, 1 knee showed hypovascularity. All 9 knees (8 post LR+1 without LR) with hypovascularity underwent TBS again at 8-10 weeks and were found to show improvement in their vascularity status in all cases.
Conclusion:
Our study showed a higher incidence of LR in our population (57%). Association of LR and patellar ischemia was significant, about 16 times the risk. MDP bone scintigraphy is the only objective tool to quantify patellar vascularity. Overall 42.8% knees post-TKR had a transient patellar ischemia, and 38% of them were following LR. All of them recovered at 8-10 weeks postoperatively.
Keywords: Lateral release, patellar ischemia, Tc methylene diphosphonate bone scan, total knee replacement
INTRODUCTION
Complications associated with the patella and patellar component of the prosthesis are important causes of failure in a total knee arthroplasty.[1,2] Potential complications involving the patella include patellar tendon avulsion (often associated with a previous high tibial osteotomy), patellofemoral instability due to inadequate soft-tissue balancing and component failure caused by factors such as a metal-backed component, recurrent instability, loosening or fracture. Apart from all these, hemarthrosis and osteonecrosis of the patella are high on the list[1,2] as patellar vascularity is at stake during a TKR procedure unrelated to the surgeon's expertise.
Lateral retinacular release (LR) is a surgical procedure during TKR, performed to ensure patellar tracking and provide knee stability.[3] Tracking is the term used to describe the movement of the patella in the knee and should ideally be centered anteriorly in the femur at the trochlear groove.[4] There are two ways of correcting this patellar maltracking during TKR, firstly by removal of patellar osteophytes and secondly by LR release that can further prevent patellar subluxation or dislocation.[5] Some patients have a genetic predisposition to retinacular tightness and can have a laterally riding patellae.[6] Trauma to the patella is another important etiology for patellar misalignment which results in inflammation and fibrosis of the retinaculum pulling the patella off the track.
Diagnostic arthroscopy is extremely helpful in defining and quantitating articular damage in TKR patients with associated patellofemoral disease.[7] The initial arthroscopy, preceding LR, should rule out other intraarticular pathologies, quantitate and localize synovitis, correlate patellar tracking with radiographic findings, quantitate and characterize articular lesions and rule out loose bodies elsewhere in the knee.[8]
The standard technique employed during TKR is an arthroscopic medial parapatellar incision along with a median incision in the quadriceps tendon and medial retinaculum that can sever the lateral superior geniculate artery [Figure 1]. Tight ligaments on the lateral side of the patella are cut to allow it to slide towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery.[9]
Figure 1.
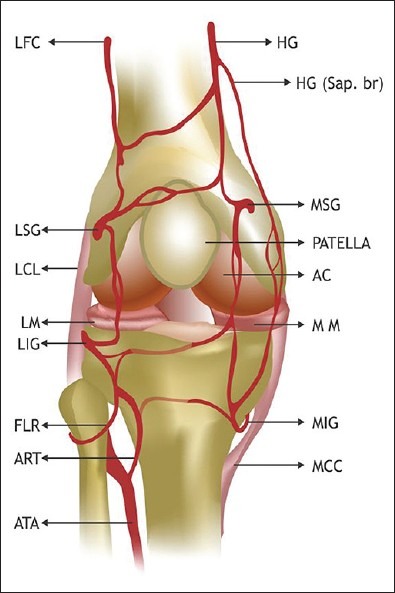
Depicts the arterial supply of the right knee joint.HG: Highest genicular, MSG:Medial superior genicular, AC: Articular cartilage, MM:Medial meniscus, MIG: Medial inferior genicular, MCC:Medial cruciate ligament, LFC:Lateral femoral circumflex (descending branch), LCL:Lateral cruciate ligament, LM:Lateral meniscus, LIG:Lateral inferior genicular, FLR:Fibular branch, ART:Anterior recurrent tibial, ATA:Anteriortibial artery
Busch and DeHaven's[10] review on LR opine that it works well for patients with persistent knee pain associated with tilt and less severe articular degeneration. Similarly Ogilvie-Harris et al. have noted that results are not as good when there is more advanced patellar arthrosis.[11] There are conflicting reports on the association of LR with patellar hypovascularity.
Our objective was to evaluate prospectively the effects of LR on patella vascularity, estimate the risk of patellar ischemia and the influence of other variables like patellar resurfacement, fat pad excision, patelloplasty using 99mTechnetium labeled methylene diphosphonate (99mTc MDP) three phase bone scintigraphy (TBS).
MATERIALS AND METHODS
Selection criteria
Forty-five TKRs performed from Jan 05 to Jan 06 at our institution were analyzed. 15 patients (21 knees) [male:female=5:10, age range 52-86 years (average, 68 years)] were included in this study.Inclusion criteria were: Patients undergoing uni/bilateral total knee replacement due to symptomatic knee osteoarthritis. Patients with (i) trauma leading to TKR, (ii) congenital ligament laxity (iii) associated back or foot/ankle pain which overshadows knee pain, (iv) any overlying skin disorder, (v) revision or unicondylar TKR, (vi) inability to walk unaided for short distances preoperatively, and (vii) previous history of stroke or other neurological conditions were excluded.
Our study group mainly consisted of knees with severe osteoarthritis and rheumatoid arthritis (11:10). Preoperative deformity was valgus in 12, varus in 7, and fixed flexion deformity in 2. Preoperative radiographs included anteroposterior, lateral projections of the knee and skyline views of the patellae with knees in a 60° flexion. Pre- and postoperative TBS of the knees was performed in all patients.
Procedure of TBS
Lower limb positioning was modified for this procedure. Knee joints were adducted, externally rotated and flexed to 30° during TBS imaging to visualise bilateral patellae away from the knee joint. 740 MBq of 99mTc MDP was injected intravenously and TBS was performed using a dual head variable angle gamma camera. Dynamic images were acquired at 2 sec/frame for 60 sec at 140 KeV photo peak with 20% window using high-resolution collimators, on a dual head variable angle ECam and a 128×128 matrix. Soft tissue phase images were acquired after 10 min of injection with a 128×128 matrix for 500K counts. Three hours delayed anterior, posterior images of knees were acquired in 256×256 matrix for 500K counts (skeletal phase). Lateral views of the knees were also acquired for quantification. Patellar MDP uptake quantification was performed preoperatively and also at various stages of postoperative follow-up using a region ratio method (target to non-target ratio, TNT ratio). A fixed region of interest (ROI) was marked on each patella (‘Target’) and replicated on the proximal most femoral shaft (‘Non-Target’) that was visually reported as normal. The MDP uptake in each of these ROI's was noted as radioactive counts and the ratios of the count in the target ROI to non-target ROI were calculated separately in the preoperative and postoperative scans in all three phases of TBS[12,13] Figure 2].
Figure 2.
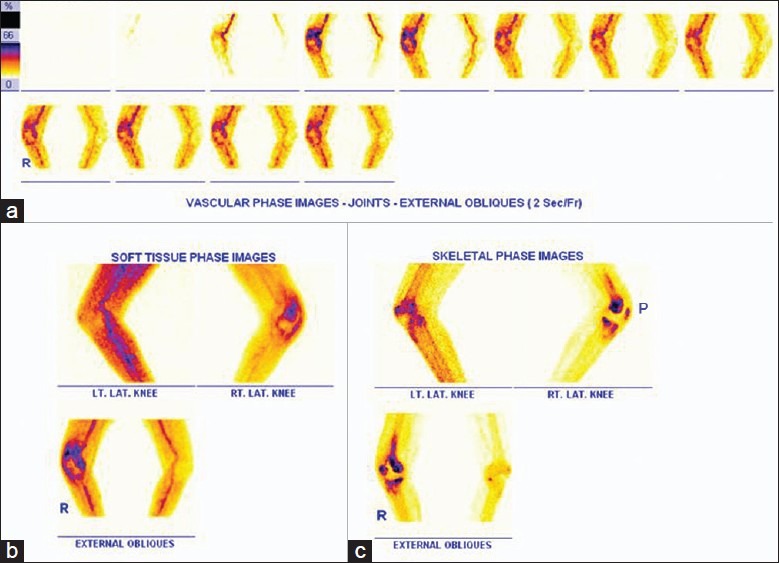
Display of a regional three phase bone scan (TBS) that was performed with 740 MBq of 99mTc MDP given as IV. (a) Immediate dynamic, (b) soft tissue phase and (c) 3 hours later skeletal phase images of both knee joints were acquired using high resolution collimators on a dual head variable angle Gamma camera. Note the technical modification in limb positioning for simultaneous assessment of patellae (Annotation P denotes patella), i.e. limbs are adducted, externally rotated with 30° flexion of the knees to separate the patella from the femoral condyle)
Procedure of TKR
All knees were exposed through a vertical midline skin incision and medial parapatellar retinacular incision, thus sacrificing all the medial patellar blood supply. Before closure, the knee was flexed to test for patellar tracking by the “no thumbs” or “towel clip” tests.[14] If the patella was maltracking, lateral release was done 1 cm lateral to the patella, patellar and quadriceps tendons upto the vastus lateralis superiorly. No attempt was made to preserve the superior lateral geniculate vessels. The knee prostheses used were press fit condylar type, i.e. PFC-PCS in 13 knees, LCS in 2, Inor in 3 and LPS Nexgen in 3.
Other parameters noted for each patient were patellar resurfacement, fat pad excision and patelloplasty. Patellar resurfacement is a surgeon dependent procedure and the decision whether to resurface the patella or not during TKR remains controversial. Traditionally one of the three options is considered: Always resurface, never surface or selectively resurface the patella. Excision of the fat pad is common in TKR to enhance surgical exposure, however, the effect of this on patellar tendon contracture and range of motion has not been clearly established. Patelloplasty is done by incising peripatellar tendinous attachment to a depth of about 1-2 mm in an attempt to do a patellar neurectomy, which could alleviate patellar pain when the patella is not resurfaced. Postoperative radiographs, same as preoperative, were repeated. Pre- and postoperative joint line, patellar height as assessed by radiographs were measured and calculated. TBS was repeated postoperatively on the 7th day in patients who had unilateral, simultaneous or staged TKR and in between the 7th and 21st day in patients undergoing staggered TKRs with the 2nd knee being done 1-2 weeks after the first [Figure 3]. All 9 knees (8 following LR+1 without LR) with hypovascularity underwent TBS again at 8-10 weeks and were found to show improvement in their vascularity status in all cases and may berelated to patellar remodeling effects or other locally inflammatory etiologies [Figure 4].
Figure 3.
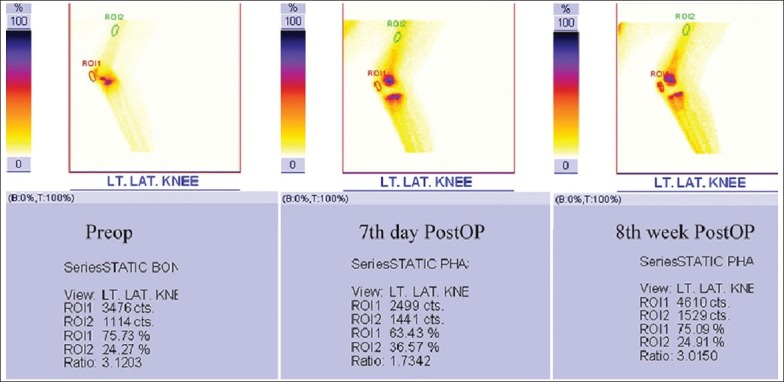
This is a summed image of the left knee joint in pre-op, 7th day and 8th week post-op showing transient patellar ischemia in the immediate post-op phase which improves at the 8th post-op week. Region Ratio was calculated on the lateral knee image as depicted in this image. The region of interest (ROI) was marked on the patella (‘Target’) and proximal most femoral shaft (‘Non-Target’) that was assumed to be normal. The uptake of MDP in each of these ROI's as marked on the images, was noted as radioactive counts and the ratios of the counts in target ROI's to non-target ROI's (target to non-target ratio-TNT ratio) were calculated separately
Figure 4.
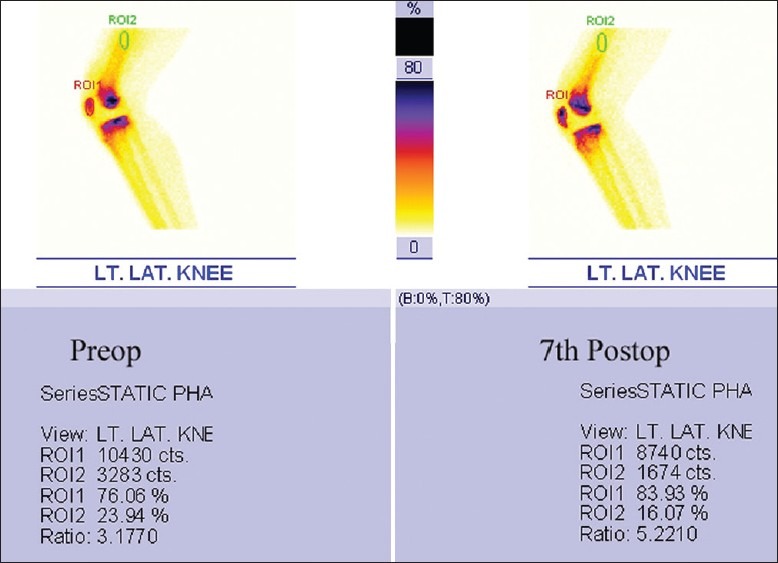
Lateral (summed) images of the left knee joint in pre-op, and 7th post-op day showing no immediate post TKR patellar ischemia, thus there is preserved patellar vascularity, confirmed by quantitation
Two experienced nuclear medicine physicians, unaware of the extent of the surgery, independently interpreted the pre- and postoperative TBS qualitatively and quantitatively. Pre-op bone scans were compared for determining postop patellar hypovascularity. If the postoperative bone scans were suggestive of patellar hypovascularity, the scan was repeated at 8 and 10 weeks postop by which time the patella usually revascularises.
RESULTS
Fifty-seven percent (12/21 knees) of our patients needed LR during TKR. Of 12 lateral releases, 8 (66%)resulted in hypovascularity; whereas of the 9 knees which did not have LR, only one knee showed hypovascularity.The visual interpretation of TBS by the two consultants concurred in all cases. However, in one case, quantification showed the patella to be hypovascular, though the visual assessment was thought to be normal (preserved vascularity).
Statistical analysis
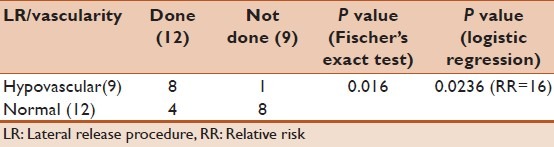
Fisher's exact test (2 tailed) showed that the association of patellar hypovascularity with a lateral release was significant (P value 0.016) [Table 1]. The odds ratio for lateral release versus patellar vascularity was 15.95, which meant that the relative risk for getting a hypovascular patella was approximately 16 times(P value 0.0236).
Table 1.
Association of patellar hypovascularity and lateral release. Number of patients are shown in brackets
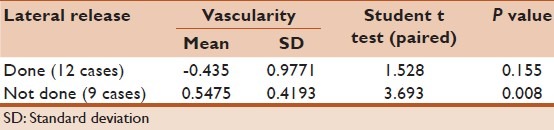
The difference in the target to non-target ratio, between the preoperative and postoperative scans was calculated. The mean and standard deviation of these differences were calculated separately for each of the 2 groups. Student t test (paired) was applied on which the P value (0.155) was found to be insignificant in patients post LR [Table 2] and the degree of hypervascualrity without LR was significant (P value 0.008).
Table 2.
Quantification and statistical analysis of patellar vascularity when lateral release is done/not done
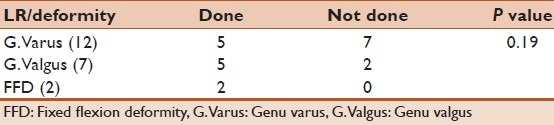
Subtotal fat pad excision meant sparing very little fat pad; whereas partial excision meant excising 50% or less of the fat pad.[15–17] When partial excision of the fat pad was done, the vascularity was not affected, whereas two-thirds of the knees with subtotal excision had compromised vascularity. The statistical association of fat pad excision was significant (P values 0.017) [Table 3]. With the present numbers, there was no relationship of vascularity with patellar resurfacement or patelloplasty. As the association of LR with patellar hypovascularity was found to be statistically significant, we attempted to examine the association of the need for LR with various parameters like preoperative diagnosis (Indication), preoperative knee deformity, alteration in jointline and in patellar height (radiologically). However the results were variable probably due to a small sample size. By applying Fischer's exact/Pearson Chi square tests, the association of the following parameters with L.R) were ascertained. In patients with rheumatoid knees and those with preoperative deformities, P value was not found to be significant for rheumatoid knees (P value 0.056) [Table 4]. Using a 3×2 Fischer exact test analysis for knees with valgus and varus deformities P value was not statistically significant, P value 0.19 [Table 5].
Table 3.
Association of patellar vascularity with fat pad excision FPE (subtotal versus partial fat pad excision). Number of patients denoted in brackets
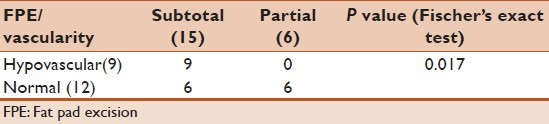
Table 4.
Association of need for lateral release with indication. Number of patients denoted in brackets
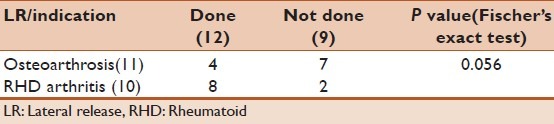
Table 5.
Association of need for lateral release during TKR in patients with preoperative limb deformity using 2 tailed, 3×2 Fischer exact test analysis. Number of patients denoted in brackets
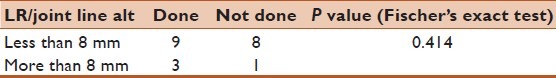
Jointline elevation causes patella infera which increases patellofemoral stress and malalignment.[18] Jointline was found to be elevated by X-ray (> 8 mm) in 4 cases, out of which 3 cases needed LR. Due to a small cohort, however, this association was not found to be statistically significant P value 0.414 [Table 6].
Table 6.
Association of need for lateral release (LR) with knee joint line alteration
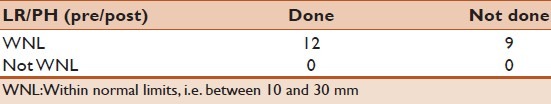
Since there were no cases with patella infera or alta preoperatively and postoperatively, correlating patellar height with need for LR was not possible [Table 7].
Table 7.
Association of need for lateral release (LR) with patellar height (PH) identified by X-ray
All 9 knees (8 following LR+1 without LR) with hypovascularity underwent TBS again at 8-10 weeks and were found to show improvement in their vascularity status in all cases and may be related to patellar remodelling effects or other locally inflammatory etiologies. The difference in the TNT Ratios between the 3rd scan (at 8-10 weeks) and the second scan (immediate postop) was calculated and was found that the mean value was 1.129, SD was 0.7198. On applying a Student's t test (t=3.841), P value was 0.0121; therefore, indicating a statistically significant improvement in vascularity. At 6 and 12 weeks follow-up, 8 knees had symptoms related to the patellofemoral joint in addition to other non-specific symptoms.
DISCUSSION
Various studies in the literature, all on caucasian knees have demonstrated a variable association, ranging between 10% as per Wetzner et al.[15] and 56% as per Scuderi et al.[18] between lateral release and patellar hypovascularity as evaluated by bone scintigraphy. Numerous authors have reported LR as a cause of patellar ischemia.[15,17]
LR should be done when maltracking results in patellofemoral instability producing fatigue, difficulty in standing up from a chair or descending stairs, medial tibial pain and stiffness on flexion leading to secondary arthrofibrosis when femoral component malrotation is the cause.[19,20] Scott et al.[21] in their study reported all three cases of fractured patella in TKR showing osteonecrosis histologically and all of them had LR done. In contrast, Ritter et al.[22,23] in two separate studies reported that osteonecrosis is not related to LR and mention a statistically significant higher incidence of patellar stress fractures when LR is not performed. The latter of these two studies, which include scintigraphic assessment, also matched for age, gender, and indication, by including patients who underwent bilateral TKRs with LR done on one side only.
Gelfer et al.[24] have found that transient patellar ischaemia occurs in 13.5% of individuals even when LR is not done and that it might be related to symptoms of anterior knee pain. But in the present study, association of LR with patellar hypovascularity seems significant. However, a larger number of patients is needed to control for confounding variables and also to determine the association of patellar hypovascularity with fat pad excision, pre-existing deformities and joint line elevation.
We found that overall 9/21 knees, i.e. 42.8% of knees post TKR had a transient ischemia, and 38% (8/21) of them were following LR. All of them recovered at 8 to10 weeks postoperatively. It remains to be seen if the patients with LR or the initial transient ischaemia are more prone for any patellar complications, which has been a contentious issue as per the studies in the Caucasian population. TBS is found to be very useful in quantifying the patellar uptake in all three phases, however proper positioning is essential to separate patella from femoral condylar uptake and could eliminate the errors due to variability in limb position.Our study shows that the objective quantification method of calculating the target to non-target ratio was more accurate other than the qualitative visual interpretation method described earlier.
CONCLUSION
We conclude that there is a strong association between LR and patellar hypovascularity in this first analysis of Indian knees about 16 times the risk. There seems to be an increased need for LR (57%) during TKR probably due to more advanced osteoarthrosis and associated patellofemoral disorders. TBS is found to be an important imaging modality and patellar quantification enables objective documentation of patellar vascularity. Overall 38% knees post LR showed transient patellar ischemia which recovered by 8-10 weeks. Patients with pre-existing knee deformities needed LR more often. While other variables for TKR like fat pad excision, patellar resurfacement or patelloplasty were considered, the vascularity was not affected in cases of partial fat pad excision.Two-thirds of the knees with subtotal fat pad excision showed compromised vascularity. There was however no relationship of vascularity with patellar resurfacement or patelloplasty in our limited series,and we need to evaluate these findings in a larger cohort of patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Clayton ML, Thirupathi R. Patellar complications after total condylar arthroplasty. Clin Orthop Relat Res. 1982;170:152–5. [PubMed] [Google Scholar]
- 2.Brick GW, Scott RD. The patellofemoral component of total knee arthroplasty. ClinOrthopRelat Res. 1988;231:163–78. [PubMed] [Google Scholar]
- 3.Krompinger WJ, Fulkerson JP. Lateral retinacular release for intractable lateral retinacular pain. ClinOrthopRelatRes. 1983;179:191–3. [PubMed] [Google Scholar]
- 4.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis.A report of two hundred and twenty cases. J Bone Joint SurgAm. 1979;61:173–80. [PubMed] [Google Scholar]
- 5.InsallJN , Dethmers DA. Revision of total knee arthroplasty. Clin Orthop Relat Res. 1982;170:123–30. [PubMed] [Google Scholar]
- 6.Post WR, Teitge R, Amis A. Patellofemoralmalalignment: looking beyond the viewbox. Clin Sports Med. 2002;21:521–46. doi: 10.1016/s0278-5919(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 7.Grana WA, Hinkley B, Hollingsworth S. Arthroscopic evaluation and treatment of patellar malalignment. Clin Orthop Relat Res. 1984;186:122–8. [PubMed] [Google Scholar]
- 8.Metcalf RW. An arthroscopic method for lateral release of the subluxating or dislocating patella. Clin Orthop Relat Res. 1982;167:9–18. [PubMed] [Google Scholar]
- 9.Kayler DE, Lyttle D. Surgical interruption of patellar blood supply by total knee arthroplasty. ClinOrthopRelat Res. 1988;229:221–7. [PubMed] [Google Scholar]
- 10.Busch M, DeHaven K. Pitfalls of lateral retinacular release. Clin Sports Med. 1989;8:279–90. [PubMed] [Google Scholar]
- 11.Ogilvie-Harris DJ, Jackson RW. The arthroscopic treatment of chondromalacia patellae. J Bone Joint SurgBr. 1984;66:660–5. doi: 10.1302/0301-620X.66B5.6501358. [DOI] [PubMed] [Google Scholar]
- 12.Lazarus C. The arthroscopic treatment of chondromalacia patellae. In: Maisey MN, Britton KE, Gilday DL, editors. J Bone Joint SurgBr. London: Chapman and Hall; 1991. pp. 515–41. [Google Scholar]
- 13.Sharp PF, Gemmell HG. Practical Nuclear Medicine. Oxford: IRL Press; 1989. Data processing; pp. 62–3. [Google Scholar]
- 14.Murray IP, Ell PJ. Nuclear Medicine in Clinical Diagnosis and Treatment. Edinburgh: Churchill Livingstone; 1994. The computer and its application in nuclear medicine; p. 1309. [Google Scholar]
- 15.Ritter MA, Pierce MJ, Zhou H, Meding JB, Faris PM, Keating EM. Patellar complications (total knee arthroplasty).Effect of lateral release and thickness. ClinOrthopRelat Res. 1999;367:149–57. [PubMed] [Google Scholar]
- 16.Wetzner SM, Bezreh JS, Scott RD, Bierbaum BE, Newberg AH. Bone scanning in the assessment of patellar viability following knee replacement. ClinOrthopRelat Res. 1985;199:215–9. [PubMed] [Google Scholar]
- 17.Dye SF, Boll DA. Radionuclide imaging of the patellofemoral joint in young adults with anterior knee pain. Orthop Clin North Am. 1986;17:249–62. [PubMed] [Google Scholar]
- 18.Figgie HE, 3rd, Goldberg VM, Figgie MP, Inglis AE, Kelly M, Sobel M. The effect of alignment of the implant on fractures of the patella after condylar total knee arthroplasty. J Bone Joint Surg Am. 1989;71:1031–9. [PubMed] [Google Scholar]
- 19.Scuderi G, Schardf SC, Meltzer LP, Scott WN. The relationship of lateral releases to patellar viability in total knee arthroplasty. J Arthroplasty. 1987;2:209–14. doi: 10.1016/s0883-5403(87)80039-6. [DOI] [PubMed] [Google Scholar]
- 20.Scuderi G, Schardf SC, Meltzer L, Nisonson B, Scott WN. Evaluation of patellar viability and disruption of arterial circulation. Am J Sports Med. 1987;15:490–3. doi: 10.1177/036354658701500511. [DOI] [PubMed] [Google Scholar]
- 21.Scott RD, Turoff N, Ewald FC. Stress fracture of the patella following duopatellar total knee arthroplasty with patellar resurfacing. ClinOrthopRelat Res. 1982;170:147–51. [PubMed] [Google Scholar]
- 22.Ritter MA, Campbell ED. Postoperative patellar complications with or without lateral release during total knee arthroplasty. Clin Orthop Relat Res. 1987;219:163–8. [PubMed] [Google Scholar]
- 23.Ritter MA, Keating EM, Faris PM. Clinical, roentgenographic, and scintigraphic results after interupption of the superior lateral genicular artery during total knee arthroplasty. ClinOrthopRelat Res. 1989;248:145–51. [PubMed] [Google Scholar]
- 24.Gelfer Y, Pinkas L, Horne T, Halperin N, Alk D, Robinson D. Symptomatic transient patellar ischaemiafollowing total knee replacement as detected by scintigraphy.A prospective,randomized,double-blind study comparing the mid-vastus to the medial para-patellar approach. Knee. 2003;10:341–5. doi: 10.1016/s0968-0160(03)00026-7. [DOI] [PubMed] [Google Scholar]


