Abstract
Atrial fibrillation occurs in 5-40% patients after coronary artery bypass graft surgery. Atrial fibrillation increases mortality and morbidity in the post-operative period. We sought to conduct a comprehensive review of literature focusing on pathophysiology, risk factors, prevention and treatment of post coronary artery bypass graft atrial fibrillation.
Keywords: AF, AF post CABG, atrial fibrillation post open heart, CABG
DEFINITION
Atrial fibrillation (AF) is a supraventricular tachyarrhythmia characterized by uncoordinated atrial activation with subsequent deterioration of mechanical function. Postoperative atrial fibrillation (POAF) is common after both cardiothoracic and noncardiothoracic surgery. AF has been reported in up to 5-40% of patients in the early postoperative period following coronary artery bypass graft (CABG),[1–3] in 37-50% after valve surgery,[4] 64% undergoing mitral valve replacement plus CABG, 49% undergoing aortic valve replacement (AVR) plus CABG and in 12% after cardiac transplantation.[5,6] POAF after cardiac surgery tends to occur within 2-4 days after the procedure with a peak incidence on postoperative day 2.[1] In a study by Aranki et al. on CABG patients, 70% and 94% patients developed POAF before the end of postoperative day 4 and 6, respectively.[7]
AF worsens a patient's hemodynamic status and increases the risk of congestive heart failure (CHF), embolic events and longer ICU stays. AF may also necessitate the use of atrioventricular nodal blocking and antiarrhythmics, which may increase the need for cardiac pacing. Stroke is a major complication seen in 2% of CABG patients, 37% of whom had preceding AF. Apart from a higher risk of stroke (OR 2.02), POAF after CABG was associated with greater in-hospital mortality (OR 1.7) and worse survival (74% vs. 87%) at long-term follow-up (4 - 5 years).[8] After controlling for a comprehensive array of risk factors associated with postcardiac surgery adverse outcomes, risk of long-term mortality in patients who developed new-onset POAF was 29% higher, for patients who underwent CABG.[9]
The impact of POAF on hospital resources is substantial and was estimated to lengthen hospital stay by 4.9 days, with an extra cost of $10,000 to $11,500 in hospital stay costs in the U.S.[7] Knowing that there are at least 640,000 open heart surgeries/ year in the U.S. according to the American Heart Association statistics in 2004 and assuming an incidence of 30% of POAF, the extra cost related to this postoperative complication could be estimated at a staggering $2 billion/year.[10]
PATHOPHYSIOLOGICAL MECHANISMS
The precise mechanism of post-CABG AF is still being investigated. The following pathophysiological factors play an important role: atrial factors (age-related structural changes such as atrial dilatation, hypertrophy, fibrosis and senile amyloidosis), postoperative inflammation (making the myocardium a tissue mosaic of differing refractory periods and conduction velocities susceptible to aberrant electrical activity, conduction and re-entry - the ‘anisotropic’ atrium,[11,12] pericarditis,[13] electrical remodeling (shortening of the effective refractory period),[14–16] autonomic imbalance (over activation of the sympathetic nervous system in response to stress, increased vagal tone,[17–20] atrial incision, perioperative ischemia,[21] alterations in atrial oxidative stress[1,22] increased expression of the gap-junctional protein connexin 40,[23] inflammatory mediators and leucocytosis after extracorporeal circulation.[24,25] Some theories proposed for AF in general are ‘Theory of Multiple Wavelets’[5,26–28] and ‘Theory of Unifocal/ Multifocal Impulse Formation and Re-entry’.[29–31] However, it is unclear if these theories hold good for post-CABG AF.
RISK FACTORS
Many risk factors have been investigated in the past; however, we will focus on those found consistently in multivariate analyses in major trials.
Preoperative
Advanced age;[7,32,33] male gender; genetic predisposition assessed by the interleukin-6 promoter gene variant,[34] history of CHF or AF; chronic obstructive pulmonary disease, chronic renal insufficiency, diabetes mellitus, rheumatic heart disease,[2,5,33,35] previous cardiac surgery, metabolic syndrome, obesity,[36–38] absence or withdrawal of beta-blocker or ACE inhibitor treatment, high pre-op Brain Natriuretic Peptide,[39] severe proximal right coronary artery stenosis,[40] mitral valve disease,[41] increased left atrial size,[42] decreased left ventricular ejection fraction, left atrial volume index ≥ 75 mL/m,[43] preoperative increase in P wave duration on surface (>116 ms) or on signal averaged (>140 ms) EKG[44–46] and blood transfusion before surgery.[44–47]
Age is consistently the independent factor most strongly associated with POAF. For every decade there is a 75% increase in the odds of developing POAF and based on age alone, anyone older than 70 years is considered to be at high risk for developing AF.[2] Age-associated changes in the atria such as dilatation, muscle atrophy, and decreased conduction may explain the strong association.
Concomitant valvular heart disease is also associated with postoperative atrial tachyarrhythmias. It is unclear whether this is because of the additional complexity of the required surgical procedure or the valvular disease itself. Neither the degree of ischemia nor the extent of coronary artery disease is a consistent predictor of postoperative atrial tachyarrhythmias.[3,48,49]
When beta-blocker was continued or started postoperatively, POAF risk was significantly reduced by 51–68%.[2] The use of adrenergic drugs is an independent risk factor for AF post-CABG.[50]
Intraoperative
Prolonged mechanical ventilation, atrial ischemia, hypokalemia,[51] hypomagnesemia.[52] There is conflicting data whether increased aortic cross-clamp and cardiopulmonary bypass time increase POAF.[7]
Postoperative
A substudy of the Atrial Fibrillation Suppression Trial II (AFIST) showed that patients who developed postoperative AF received 1.3 L more fluid than those without postoperative AF over 5 postoperative days.[53] Net fluid balance on postoperative day 2 was an independent predictor of post-CTS AF among amiodarone-naive patients (OR 6.4; 95% CI 1.4 to 29.1) which is noteworthy since most post-CTS AF occurs on this day.[54]
Characteristics that have not been identified consistently as independent risk factors include hypertension, left ventricular dysfunction, angina pectoris, and noncardiac illnesses.
PREVENTION
Beta-blocker
Since the autonomic nervous system plays a major role in the pathophysiology of post-CABG AF, beta blockers have been widely studied in its prevention. In one study beta-blockers had the greatest magnitude of effect across 28 trials (4,074 patients) with an odds ratio (OR) of 0.35, 95% CI 0.26-0.49.[55] In another meta-analysis of 24 trials limited to patients with ejection fraction >30% undergoing CABG, prophylactic beta-blockers were associated with protection against supraventricular tachycardia with an OR of 0.28, 95%CI 0.21-0.36.[56]
Sotalol
In a meta-analysis of 14 trials including 2,583 patients that compared beta-blocker or placebo, sotalol was found to be more effective in reducing POAF than beta-blocker or placebo. Therefore, it seems to offer significant additional protection over standard beta-blockers.[57]
Amiodarone
In a randomized trial including 124 patients undergoing a complex cardiac surgery, amiodarone administered orally at least 1 week preoperatively significantly reduced the incidence of POAF, from 53% in the placebo group to 25% in the treated group (P = 0.003). In the Amiodarone Reduction in Coronary Heart (ARCH) trial, postoperative intravenous administration of amiodarone was associated with a lower incidence of POAF (35%) compared with the placebo arm (47%) (P = 0.01).[58]
Atrial pacing
Prophylactic pacing has been investigated in a number of trials. Meta-analyses of these clinical trials have consistently shown that single- or dual-site atrial pacing significantly reduces the risk of new-onset POAF.[59,60] In a randomized trial, biatrial overdrive pacing in patients undergoing CABG was shown to be more effective in preventing POAF than single-site atrial pacing (12.5% vs. 36%).[61] However, this trial included a small number of patients and had significant limitations. Major adverse effect is potential proarrhythmic effect.
Calcium channel blockers
A recent meta-analysis showed that calcium-channel blockers reduce supra-ventricular tachyarrhythmia risk (OR 0.62; 95% CI 0.41-0.93).[62] However, in some studies, the perioperative use of these drugs was associated with an increased incidence of AV block and low output syndrome, due to their negative chronotropic and inotropic effect. In patients undergoing CABG, diltiazem reduced post-CABG AF incidence by 50–74% compared with placebo.[63]
Magnesium
A meta-analysis concluded that magnesium administration was effective for reducing POAF with a similar efficacy to common antiarrhythmic drugs.[64] Meta-analyses have shown magnesium to reduce POAF risk by 23-36%.[64,65] However, the studies included in these analyses included a small number of patients, and the design varied among the different studies, thus limiting the interpretation of the results.
Statins- The prospective randomized study Atorvastatin for Reduction of MYocardial Dysrhythmia After cardiac surgery (ARMYDA-3) has demonstrated that treatment with Atorvastatin 40 mg/day started 7 days before elective cardiac surgery under cardiopulmonary bypass and continued in the postoperative period significantly reduces the occurrence of POAF by 61%.[66] Statins have been shown to reduce inflammation in patients with coronary artery disease; and thus the theoretical benefit to decrease postoperative inflammation as a potential cause of POAF. When the theory examined was found to be useful in the prevention of POAF.
N-3 polyunsaturated fatty acids
In a randomized controlled trial of 160 patients undergoing elective CABG, PUFAs supplementation significantly reduced the incidence of POAF by 65% versus control, an effect similar to that obtained with beta-blockers, sotalol, or amiodarone (OR 0.35; 95% CI 0.16-0.76).[67] The modulation of cardiac connexin was probably the contributing mechanism to the antiarrhythmic effects of fish oil supplementation. Furthermore, in the general population, consumption of fish, inducing high plasma PUFA concentration, has been associated with a lower incidence of AF in a 12-year follow-up study.[68]
Anti-inflammatory agents
In a randomised controlled trial the authors concluded that nonsteroidal anti-inflammatory medications are effective in significantly reducing the incidence of AF after CABG. However, the risk versus benefit ratio of such prophylactic strategy remains uncertain, given their nephrotoxicity.[69] In another multicenter trial hydrocortisone proved beneficial in reducing the incidence of POAF in the first 84 hours.[70]
TREATMENT
Before initiating the treatment of AF, underlying medical comorbidities like electrolyte imbalance, hypoxia, COPD should be treated.[71] AF has been associated with physiological stress, drugs, pulmonary embolism, chronic lung disease, hyperthyroidism, caffeine, infectious processes, and various metabolic disturbances. AF has also been linked with obesity, and this phenomenon seems to be mediated by left atrial dilation
The treatment of post-CABG AF includes use of drugs and electrical cardioversion. Drugs can target to achieve rate control or rhythm control [Table 1]. According to a study conducted to study rate control versus rhythm control it was found that the latter is more beneficial because of a decreased time to cardioversion, prolonged maintenance of sinus rhythm, and decreased length of overall hospital stay.[72]
Table 1.
Dosage, advantages, and side effects of drugs used for treatment of POAF
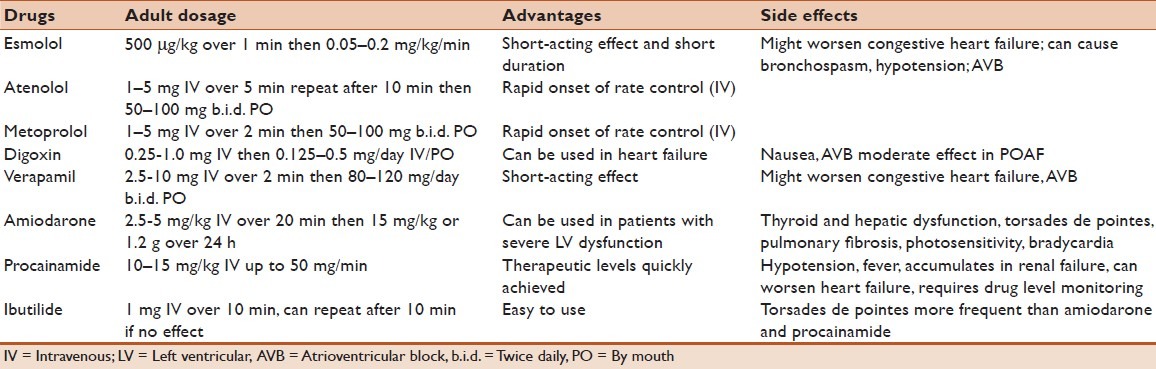
Short acting beta-blockers are the drug of choice,[71] especially in patients with ischemic heart disease. They should be used with care in patients with asthma, COPD, congestive cardiac failure and AV conduction block, in whom they are relatively contraindicated. Among calcium channel blockers, verapamil and diltiazem can be used. Digoxin is less effective when adrenergic tone is high but might be used in patients with congestive heart failure.[73] Amiodarone can also be used and is also known to improve hemodynamic status when used intravenously.[71,74] the risks and benefits of this treatment option, including the conversion rates.
Electrical Cardioversion- Indications for performing electrical cardioversion in patients with post-CABG AF are hemodynamic instability, myocardial ischemia, acute pump failure and elective restoration of normal sinus rhythm after a failed pharmacological attempt. Cardioversion can be associated with thromboembolism if POAF is present for more than 48 hours. The guidelines for anticoagulation in post surgical patients are not clear.[71]
Thromboembolism prevention: AF after CABG poses an increased risk of cerebrovascular accidents in the form of stroke;[75,76] however, using anticoagulants in the post operative period can lead to increased risk of bleeding and cardiac tamponade.[77] The risks might far outweigh the benefits especially in patients with advanced age, previous history of bleeding and uncontrolled hypertension.[61] Anticoagulants can be used for prolonged and/or frequent episodes of AF and is recommended by the American College of Chest Physicians in patients with history of stroke and transient ischemic attacks (30 days after the return of sinus rhythm).[78] Anticoagulation should be considered in patients 75 years or older and patients with risk factors for stroke, while antiplatelet agents may prove useful in younger patients, subgroups in whom anticoagulation is contraindicated, and in patients with low risk for stroke.[79]
CONCLUSIONS AND RECOMMENDATIONS
POAF is a burden to our health care system and increases ICU stay. We do have multiple modalities which range from the conservative medical approach to invasive biatrial pacing, so it would be worthwhile to be able to predict the occurrence of POAF. Many recent studies have tried to find predictors of POAF.[80,81] Developing a practical and simple AF score that can predict POAF is in order, and further research is required as to how to interpret these criteria and use them to utilize the available prevention and treatment modalities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med. 2001;135:1061–73. doi: 10.7326/0003-4819-135-12-200112180-00010. [DOI] [PubMed] [Google Scholar]
- 2.Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–9. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 3.Villareal RP, Hariharan R, Liu BC, Kar B, Lee VV, Elayda M, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol. 2004;43:742–8. doi: 10.1016/j.jacc.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 4.Asher CR, Miller DP, Grimm RA, Cosgrove DM, 3rd, Chung MK. Analysis of risk factors for development of atrial fibrillation early after cardiac valvular surgery. Am J Cardiol. 1998;82:892–5. doi: 10.1016/s0002-9149(98)00498-6. [DOI] [PubMed] [Google Scholar]
- 5.Creswell LL, Schuessler RB, Rosenbloom M, Cox JL. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg. 1993;56:539–49. doi: 10.1016/0003-4975(93)90894-n. [DOI] [PubMed] [Google Scholar]
- 6.Pavri BB, O’Nunain SS, Newell JB, Ruskin JN, William G. Prevalence and prognostic significance of atrial arrhythmias after orthotopic cardiac transplantation. J Am Coll Cardiol. 1995;25:1673–80. doi: 10.1016/0735-1097(95)00047-8. [DOI] [PubMed] [Google Scholar]
- 7.Aranki SF, Shaw DP, Adams DH, Rizzo RJ, Couper GS, Vander Vliet M, et al. Predictors of atrial fibrillation after coronary artery surgery.current trends and impact on hospital resources. Circulation. 1996;94:390–7. doi: 10.1161/01.cir.94.3.390. [DOI] [PubMed] [Google Scholar]
- 8.Blomstrom Lundqvist C. Post CABG atrial fibrillation: What are the incidence, predictors, treatment, and long-term outcome? In: Raviele A, editor. Venice, Italy: Springer; 2005. [Google Scholar]
- 9.Filardo G, Hamilton C, Hebeler RF, Jr, Hamman B, Grayburn P. New-onset postoperative atrial fibrillation after isolated coronary artery bypass graft surgery and long-term survival. Circ Cardiovasc Qual Outcomes. 2009;2:164–9. doi: 10.1161/CIRCOUTCOMES.108.816843. [DOI] [PubMed] [Google Scholar]
- 10.American heart association heart disease and stroke statistics— update at-A-glance. Circulation. 2007;115(5):e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 11.Ishii Y, Schuessler RB, Gaynor SL, Yamada K, Fu AS, Boineau JP, et al. Inflammation of atrium after cardiac surgery is associated with inhomogeneity of atrial conduction and atrial fibrillation. Circulation. 2005;111:2881–8. doi: 10.1161/CIRCULATIONAHA.104.475194. [DOI] [PubMed] [Google Scholar]
- 12.Tselentakis EV, Woodford E, Chandy J, Gaudette GR, Saltman AE. Inflammation effects on the electrical properties of atrial tissue and inducibility of postoperative atrial fibrillation. J Surg Res. 2006;135:68–75. doi: 10.1016/j.jss.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Willems S, Weiss C, Meinertz T. Tachyarrhythmias following coronary artery bypass graft surgery: Epidemiology, mechanisms, and current therapeutic strategies. Thorac Cardiovasc Surg. 1997;45:232–7. doi: 10.1055/s-2007-1013733. [DOI] [PubMed] [Google Scholar]
- 14.Zipes DP. Electrophysiological remodeling of the heart owing to rate. Circulation. 1997;95:1745–8. doi: 10.1161/01.cir.95.7.1745. [DOI] [PubMed] [Google Scholar]
- 15.Van Wagoner DR, Pond AL, Lamorgese M, Rossie SS, McCarthy PM, Nerbonne JM. Atrial L-type Ca2+ currents and human atrial fibrillation. Circ Res. 1999;85:428–36. doi: 10.1161/01.res.85.5.428. [DOI] [PubMed] [Google Scholar]
- 16.Nattel S. Ionic determinants of atrial fibrillation and Ca2+ channel abnormalities: Cause, consequence, or innocent bystander? Circ Res. 1999;85:473–6. doi: 10.1161/01.res.85.5.473. [DOI] [PubMed] [Google Scholar]
- 17.Schauerte P, Scherlag BJ, Patterson E, Scherlag MA, Matsudaria K, Nakagawa H, et al. Focal atrial fibrillation: Experimental evidence for a pathophysiologic role of the autonomic nervous system. J Cardiovasc Electrophysiol. 2001;12:592–9. doi: 10.1046/j.1540-8167.2001.00592.x. [DOI] [PubMed] [Google Scholar]
- 18.Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation. 2002;105:2753–9. doi: 10.1161/01.cir.0000018443.44005.d8. [DOI] [PubMed] [Google Scholar]
- 19.Zimmermann M, Kalusche D. Fluctuation in autonomic tone is a major determinant of sustained atrial arrhythmias in patients with focal ectopy originating from the pulmonary veins. J Cardiovasc Electrophysiol. 2001;12:285–91. doi: 10.1046/j.1540-8167.2001.00285.x. [DOI] [PubMed] [Google Scholar]
- 20.Dimmer C, Tavernier R, Gjorgov N, Van Nooten G, Clement DL, Jordaens L. Variations of autonomic tone preceding onset of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 1998;82:22–5. doi: 10.1016/s0002-9149(98)00231-8. [DOI] [PubMed] [Google Scholar]
- 21.Kanoupakis EM, Manios EG, Mavrakis HE, Kaleboubas MD, Parthenakis FI, Vardas PE. Relation of autonomic modulation to recurrence of atrial fibrillation following cardioversion. Am J Cardiol. 2000;86:954–8. doi: 10.1016/s0002-9149(00)01129-2. [DOI] [PubMed] [Google Scholar]
- 22.Carnes CA, Chung MK, Nakayama T, Nakayama H, Baliga RS, Piao S, et al. Ascorbate attenuates atrial pacing-induced peroxynitrite formation and electrical remodeling and decreases the incidence of postoperative atrial fibrillation. Circ Res. 2001;89:E32–8. doi: 10.1161/hh1801.097644. [DOI] [PubMed] [Google Scholar]
- 23.Dupont E, Ko Y, Rothery S, Coppen SR, Baghai M, Haw M, et al. The gap-junctional protein connexin40 is elevated in patients susceptible to postoperative atrial fibrillation. Circulation. 2001;103:842–9. doi: 10.1161/01.cir.103.6.842. [DOI] [PubMed] [Google Scholar]
- 24.Abdelhadi RH, Gurm HS, Van Wagoner DR, Chung MK. Relation of an exaggerated rise in white blood cells after coronary bypass or cardiac valve surgery to development of atrial fibrillation postoperatively. Am J Cardiol. 2004;93:1176–8. doi: 10.1016/j.amjcard.2004.01.053. [DOI] [PubMed] [Google Scholar]
- 25.Lamm G, Auer J, Weber T, Berent R, Ng C, Eber B. Postoperative white blood cell count predicts atrial fibrillation after cardiac surgery. J Cardiothorac Vasc Anesth. 2006;20:51–6. doi: 10.1053/j.jvca.2005.03.026. [DOI] [PubMed] [Google Scholar]
- 26.Moe GK, Abildskov JA. Observations on the ventricular dysrhythmia associated with atrial fibrillation in the dog heart. Circ Res. 1964;14:447–60. doi: 10.1161/01.res.14.5.447. [DOI] [PubMed] [Google Scholar]
- 27.Moe GK, Abildskov JA. Atrial fibrillation as a self-sustaining arrhythmia independent of focal discharge. Am Heart J. 1959;58:59–70. doi: 10.1016/0002-8703(59)90274-1. [DOI] [PubMed] [Google Scholar]
- 28.Cox JL. A perspective of postoperative atrial fibrillation in cardiac operations. Ann Thorac Surg. 1993;56:405–9. doi: 10.1016/0003-4975(93)90871-e. [DOI] [PubMed] [Google Scholar]
- 29.Jais P, Haissaguerre M, Shah DC, Chouairi S, Gencel L, Hocini M, et al. A focal source of atrial fibrillation treated by discrete radiofrequency ablation. Circulation. 1997;95:572–6. doi: 10.1161/01.cir.95.3.572. [DOI] [PubMed] [Google Scholar]
- 30.Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–66. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 31.Chen SA, Tai CT, Yu WC, Chen YJ, Tsai CF, Hsieh MH, et al. Right atrial focal atrial fibrillation: Electrophysiologic characteristics and radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 1999;10:328–35. doi: 10.1111/j.1540-8167.1999.tb00679.x. [DOI] [PubMed] [Google Scholar]
- 32.Almassi GH, Schowalter T, Nicolosi AC, Aggarwal A, Moritz TE, Henderson WG, et al. Atrial fibrillation after cardiac surgery: A major morbid event? Ann Surg. 1997;226:501–11. doi: 10.1097/00000658-199710000-00011. discussion 511-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathew JP, Parks R, Savino JS, Friedman AS, Koch C, Mangano DT, et al. Atrial fibrillation following coronary artery bypass graft surgery: Predictors, outcomes, and resource utilization. MultiCenter study of perioperative ischemia research group. JAMA. 1996;276:300–6. [PubMed] [Google Scholar]
- 34.Gaudino M, Andreotti F, Zamparelli R, Di Castelnuovo A, Nasso G, Burzotta F, et al. The -174G/C interleukin-6 polymorphism influences postoperative interleukin-6 levels and postoperative atrial fibrillation. is atrial fibrillation an inflammatory complication? Circulation. 2003;108(Suppl 1):II195–9. doi: 10.1161/01.cir.0000087441.48566.0d. [DOI] [PubMed] [Google Scholar]
- 35.Banach M, Rysz J, Drozdz JA, Okonski P, Misztal M, Barylski M, et al. Risk factors of atrial fibrillation following coronary artery bypass grafting: A preliminary report. Circ J. 2006;70:438–41. doi: 10.1253/circj.70.438. [DOI] [PubMed] [Google Scholar]
- 36.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort.the framingham heart study. JAMA. 1994;271:840–4. [PubMed] [Google Scholar]
- 37.Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Obesity and risk of new-onset atrial fibrillation after cardiac surgery. Circulation. 2005;112:3247–55. doi: 10.1161/CIRCULATIONAHA.105.553743. [DOI] [PubMed] [Google Scholar]
- 38.Echahidi N, Mohty D, Pibarot P, Despres JP, O’Hara G, Champagne J, et al. Obesity and metabolic syndrome are independent risk factors for atrial fibrillation after coronary artery bypass graft surgery. Circulation. 2007;116(Suppl 11):I213–9. doi: 10.1161/CIRCULATIONAHA.106.681304. [DOI] [PubMed] [Google Scholar]
- 39.Ata Y, Turk T, Ay D, Eris C, Demir M, Ari H, et al. Ability of B-type natriuretic peptide in predicting postoperative atrial fibrillation in patients undergoing coronary artery bypass grafting. Heart Surg Forum. 2009;12:E211–6. doi: 10.1532/HSF98.20091014. [DOI] [PubMed] [Google Scholar]
- 40.Mendes LA, Connelly GP, McKenney PA, Podrid PJ, Cupples LA, Shemin RJ, et al. Right coronary artery stenosis: An independent predictor of atrial fibrillation after coronary artery bypass surgery. J Am Coll Cardiol. 1995;25:198–202. doi: 10.1016/0735-1097(94)00329-o. [DOI] [PubMed] [Google Scholar]
- 41.Shen J, Lall S, Zheng V, Buckley P, Damiano RJ, Jr, Schuessler RB. The persistent problem of new-onset postoperative atrial fibrillation: A single-institution experience over two decades. J Thorac Cardiovasc Surg. 2011;141:559–70. doi: 10.1016/j.jtcvs.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manning WJ, Gelfand EV. Left atrial size and postoperative atrial fibrillation: The volume of evidence suggests it is time to break an old habit. J Am Coll Cardiol. 2006;48:787–9. doi: 10.1016/j.jacc.2006.05.036. [DOI] [PubMed] [Google Scholar]
- 43.Nattel S. New ideas about atrial fibrillation 50 years on. Nature. 2002;415:219–26. doi: 10.1038/415219a. [DOI] [PubMed] [Google Scholar]
- 44.Zaman AG, Archbold RA, Helft G, Paul EA, Curzen NP, Mills PG. Atrial fibrillation after coronary artery bypass surgery: A model for preoperative risk stratification. Circulation. 2000;101:1403–8. doi: 10.1161/01.cir.101.12.1403. [DOI] [PubMed] [Google Scholar]
- 45.Steinberg JS, Zelenkofske S, Wong SC, Gelernt M, Sciacca R, Menchavez E. Value of the P-wave signal-averaged ECG for predicting atrial fibrillation after cardiac surgery. Circulation. 1993;88:2618–22. doi: 10.1161/01.cir.88.6.2618. [DOI] [PubMed] [Google Scholar]
- 46.Buxton AE, Josephson ME. The role of P wave duration as a predictor of postoperative atrial arrhythmias. Chest. 1981;80:68–73. doi: 10.1378/chest.80.1.68. [DOI] [PubMed] [Google Scholar]
- 47.Koch CG, Li L, Van Wagoner DR, Duncan AI, Gillinov AM, Blackstone EH. Red cell transfusion is associated with an increased risk for postoperative atrial fibrillation. Ann Thorac Surg. 2006;82:1747–56. doi: 10.1016/j.athoracsur.2006.05.045. [DOI] [PubMed] [Google Scholar]
- 48.Hashimoto K, Ilstrup DM, Schaff HV. Influence of clinical and hemodynamic variables on risk of supraventricular tachycardia after coronary artery bypass. J Thorac Cardiovasc Surg. 1991;101:56–65. [PubMed] [Google Scholar]
- 49.Leitch JW, Thomson D, Baird DK, Harris PJ. The importance of age as a predictor of atrial fibrillation and flutter after coronary artery bypass grafting. J Thorac Cardiovasc Surg. 1990;100:338–42. [PubMed] [Google Scholar]
- 50.Salaria V, Mehta NJ, Abdul-Aziz S, Mohiuddin SM, Khan IA. Role of postoperative use of adrenergic drugs in occurrence of atrial fibrillation after cardiac surgery. Clin Cardiol. 2005;28:131–5. doi: 10.1002/clc.4960280306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wahr JA, Parks R, Boisvert D, Comunale M, Fabian J, Ramsay J, et al. Preoperative serum potassium levels and perioperative outcomes in cardiac surgery patients. multicenter study of perioperative ischemia research group. JAMA. 1999;281:2203–10. doi: 10.1001/jama.281.23.2203. [DOI] [PubMed] [Google Scholar]
- 52.England MR, Gordon G, Salem M, Chernow B. Magnesium administration and dysrhythmias after cardiac surgery.A placebo-controlled, double-blind, randomized trial. JAMA. 1992;268:2395–402. [PubMed] [Google Scholar]
- 53.White CM, Caron MF, Kalus JS, Rose H, Song J, Reddy P, et al. Intravenous plus oral amiodarone, atrial septal pacing, or both strategies to prevent post-cardiothoracic surgery atrial fibrillation: The atrial fibrillation suppression trial II (AFIST II) Circulation. 2003;108(Suppl 1):II200–6. doi: 10.1161/01.cir.0000087445.59819.6f. [DOI] [PubMed] [Google Scholar]
- 54.Giri S, White CM, Dunn AB, Felton K, Freeman-Bosco L, Reddy P, et al. Oral amiodarone for prevention of atrial fibrillation after open heart surgery, the atrial fibrillation suppression trial (AFIST): A randomised placebo-controlled trial. Lancet. 2001;357:830–6. doi: 10.1016/S0140-6736(00)04196-9. [DOI] [PubMed] [Google Scholar]
- 55.Crystal E, Garfinkle MS, Connolly SS, Ginger TT, Sleik K, Yusuf SS. Interventions for preventing post-operative atrial fibrillation in patients undergoing heart surgery. Cochrane Database Syst Rev. 2004:CD003611. doi: 10.1002/14651858.CD003611.pub2. [DOI] [PubMed] [Google Scholar]
- 56.Andrews TC, Reimold SC, Berlin JA, Antman EM. Prevention of supraventricular arrhythmias after coronary artery bypass surgery.A meta-analysis of randomized control trials. Circulation. 1991;84(5 Suppl):III236–44. [PubMed] [Google Scholar]
- 57.Burgess DC, Kilborn MJ, Keech AC. Interventions for prevention of post-operative atrial fibrillation and its complications after cardiac surgery: A meta-analysis. Eur Heart J. 2006;27:2846–57. doi: 10.1093/eurheartj/ehl272. [DOI] [PubMed] [Google Scholar]
- 58.Guarnieri T, Nolan S, Gottlieb SO, Dudek A, Lowry DR. Intravenous amiodarone for the prevention of atrial fibrillation after open heart surgery: The amiodarone reduction in coronary heart (ARCH) trial. J Am Coll Cardiol. 1999;34:343–7. doi: 10.1016/s0735-1097(99)00212-0. [DOI] [PubMed] [Google Scholar]
- 59.Crystal E, Connolly SJ, Sleik K, Ginger TJ, Yusuf S. Interventions on prevention of post-operative atrial fibrillation in patients undergoing heart surgery: A meta-analysis. Circulation. 2002;106:75–80. doi: 10.1161/01.cir.0000021113.44111.3e. [DOI] [PubMed] [Google Scholar]
- 60.Daoud EG, Snow R, Hummel JD, Kalbfleisch SJ, Weiss R, Augostini R. Temporary atrial epicardial pacing as prophylaxis against atrial fibrillation after heart surgery: A meta-analysis. J Cardiovasc Electrophysiol. 2003;14:127–32. doi: 10.1046/j.1540-8167.2003.02371.x. [DOI] [PubMed] [Google Scholar]
- 61.Fan K, Lee KL, Chiu CS, Lee JW, He GW, Cheung D, et al. Effects of biatrial pacing in prevention of postoperative atrial fibrillation after coronary artery bypass surgery. Circulation. 2000;102:755–60. doi: 10.1161/01.cir.102.7.755. [DOI] [PubMed] [Google Scholar]
- 62.Wijeysundera DN, Beattie WS, Rao V, Karski J. Calcium antagonists reduce cardiovascular complications after cardiac surgery: A meta-analysis. J Am Coll Cardiol. 2003;41:1496–505. doi: 10.1016/s0735-1097(03)00191-8. [DOI] [PubMed] [Google Scholar]
- 63.Dobrilovic N, Vadlamani L, Buchert B, Wright CB. Diltiazem prophylaxis reduces incidence of atrial fibrillation after coronary artery bypass grafting. J Cardiovasc Surg (Torino) 2005;46:457–61. [PubMed] [Google Scholar]
- 64.Miller S, Crystal E, Garfinkle M, Lau C, Lashevsky I, Connolly SJ. Effects of magnesium on atrial fibrillation after cardiac surgery: A meta-analysis. Heart. 2005;91:618–23. doi: 10.1136/hrt.2004.033811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shiga T, Wajima Z, Inoue T, Ogawa R. Magnesium prophylaxis for arrhythmias after cardiac surgery: A meta-analysis of randomized controlled trials. Am J Med. 2004;117:325–33. doi: 10.1016/j.amjmed.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 66.Patti G, Chello M, Candura D, Pasceri V, D’Ambrosio A, Covino E, et al. Randomized trial of atorvastatin for reduction of postoperative atrial fibrillation in patients undergoing cardiac surgery: Results of the ARMYDA-3 (atorvastatin for reduction of MYocardial dysrhythmia after cardiac surgery) study. Circulation. 2006;114:1455–61. doi: 10.1161/CIRCULATIONAHA.106.621763. [DOI] [PubMed] [Google Scholar]
- 67.Calo L, Bianconi L, Colivicchi F, Lamberti F, Loricchio ML, de Ruvo E, et al. N-3 fatty acids for the prevention of atrial fibrillation after coronary artery bypass surgery: A randomized, controlled trial. J Am Coll Cardiol. 2005;45:1723–8. doi: 10.1016/j.jacc.2005.02.079. [DOI] [PubMed] [Google Scholar]
- 68.Mozaffarian D, Psaty BM, Rimm EB, Lemaitre RN, Burke GL, Lyles MF, et al. Fish intake and risk of incident atrial fibrillation. Circulation. 2004;110:368–73. doi: 10.1161/01.CIR.0000138154.00779.A5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheruku KK, Ghani A, Ahmad F, Pappas P, Silverman PR, Zelinger A, et al. Efficacy of nonsteroidal anti-inflammatory medications for prevention of atrial fibrillation following coronary artery bypass graft surgery. Prev Cardiol. 2004;7:13–8. doi: 10.1111/j.1520-037x.2004.3117.x. [DOI] [PubMed] [Google Scholar]
- 70.Halonen J, Halonen P, Jarvinen O, Taskinen P, Auvinen T, Tarkka M, et al. Corticosteroids for the prevention of atrial fibrillation after cardiac surgery: A randomized controlled trial. JAMA. 2007;297:1562–7. doi: 10.1001/jama.297.14.1562. [DOI] [PubMed] [Google Scholar]
- 71.Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol. 2008;51:793–801. doi: 10.1016/j.jacc.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 72.Lee JK, Klein GJ, Krahn AD, Yee R, Zarnke K, Simpson C, et al. Rate-control versus conversion strategy in postoperative atrial fibrillation: Trial design and pilot study results. Card Electrophysiol Rev. 2003;7:178–84. doi: 10.1023/a:1027428003609. [DOI] [PubMed] [Google Scholar]
- 73.Zarowitz B, Gheorghiade M. Optimal heart rate control for patients with chronic atrial fibrillation: are pharmacologic choices truly changing? Am Heart J. 1992;123:1401–1403. doi: 10.1016/0002-8703(92)91058-9. [DOI] [PubMed] [Google Scholar]
- 74.Clemo HF, Wood MA, Gilligan DM, Ellenbogen KA. Intravenous amiodarone for acute heart rate control in the critically ill patient with atrial tachyarrhythmias. Am J Cardiol. 1998;81:594–8. doi: 10.1016/s0002-9149(97)00962-4. [DOI] [PubMed] [Google Scholar]
- 75.Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, et al. Stroke after cardiac surgery: A risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75:472–8. doi: 10.1016/s0003-4975(02)04370-9. [DOI] [PubMed] [Google Scholar]
- 76.Hogue CW, Jr, Murphy SF, Schechtman KB, Davila-Roman VG. Risk factors for early or delayed stroke after cardiac surgery. Circulation. 1999;100:642–7. doi: 10.1161/01.cir.100.6.642. [DOI] [PubMed] [Google Scholar]
- 77.Meurin P, Weber H, Renaud N, Larrazet F, Tabet JY, Demolis P, et al. Evolution of the postoperative pericardial effusion after day 15: The problem of the late tamponade. Chest. 2004;125:2182–7. doi: 10.1378/chest.125.6.2182. [DOI] [PubMed] [Google Scholar]
- 78.Epstein AE, Alexander JC, Gutterman DD, Maisel W, Wharton JM. American College of Chest Physicians. Anticoagulation: American college of chest physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest. 2005;128(2 Suppl):24S–7S. doi: 10.1378/chest.128.2_suppl.24s. [DOI] [PubMed] [Google Scholar]
- 79.Segal JB, McNamara RL, Miller MR, Kim N, Goodman SN, Powe NR, et al. Prevention of thromboembolism in atrial fibrillation.A meta-analysis of trials of anticoagulants and antiplatelet drugs. J Gen Intern Med. 2000;15:56–67. doi: 10.1046/j.1525-1497.2000.04329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rader F, Costantini O, Jarrett C, Gorodeski EZ, Lauer MS, Blackstone EH. Quantitative electrocardiography for predicting postoperative atrial fibrillation after cardiac surgery. J Electrocardiol. 2011;44:761–7. doi: 10.1016/j.jelectrocard.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Amar D, Shi W, Hogue CW, Jr, Zhang H, Passman RS, Thomas B, et al. Clinical prediction rule for atrial fibrillation after coronary artery bypass grafting. J Am Coll Cardiol. 2004;44:1248–53. doi: 10.1016/j.jacc.2004.05.078. [DOI] [PubMed] [Google Scholar]


