Abstract
It is currently impossible to predict the next pandemic influenza virus strain. We have thus established a library of influenza viruses of all hemagglutinin and neuraminidase subtypes and their genes. In this article, we examine the applicability of a rapid production model for the preparation of vaccines against emerging pandemic influenza viruses. This procedure utilizes the influenza virus library, cell culture-based vaccine production, and intranasal administration to induce a cross-protective immune response. First, an influenza virus reassortant from the library, A/duck/Hokkaido/Vac-3/2007 (H5N1), was passaged 22 times (P22) in Madin-Darby canine kidney (MDCK) cells. The P22 virus had a titer of >2 ×108 PFU/ml, which was 40 times that of the original strain, with 4 point mutations, which altered amino acids in the deduced protein sequences encoded by the PB2 and PA genes. We then produced a formalin-inactivated whole-virion vaccine from the MDCK cell-cultured A/duck/Hokkaido/Vac-3/2007 (H5N1) P22 virus. Intranasal immunization of mice with this vaccine protected them against challenges with lethal influenza viruses of homologous and heterologous subtypes. We further demonstrated that intranasal immunization with the vaccine induced cross-reactive neutralizing antibody responses against the homotypic H5N1 influenza virus and its antigenic variants and cross-reactive cell-mediated immune responses to the homologous virus, its variants within a subtype, and even an influenza virus of a different subtype. These results indicate that a rapid model for emergency vaccine production may be effective for producing the next generation of pandemic influenza virus vaccines.
INTRODUCTION
Before the 2009 H1N1 influenza pandemic occurred, it was widely thought that the next pandemic virus would be the avian H5N1 virus, because hundreds of people worldwide had been infected with the highly pathogenic H5N1 influenza virus since 1997, and 60% of them had died (1–3). However, no pandemic involving the highly pathogenic avian H5N1 influenza virus has occurred. This illustrates how difficult it is to predict which influenza virus strain will give rise to the next pandemic. The seasonal influenza vaccine is produced each year by using a chicken egg-based manufacturing process, which is tedious and time-consuming. This process, which starts with egg preparation and the choice of the seed strain, takes several months to produce an adequate supply of influenza vaccine (4). Therefore, the current vaccine production system would be inadequate to respond to an influenza pandemic, for which a novel rapid emergency vaccine-manufacturing process is required.
All of the genes of mammalian influenza viruses are derived from the avian influenza virus pool (3). In addition, avian influenza viruses are subjected to little immunological pressure in their natural hosts, water fowl. For these reasons, the antigenic sites of the virus are thought to be fairly well conserved in avian and pandemic viruses. Therefore, we hypothesized that all pandemic influenza viruses originate from an avian influenza virus gene pool and that these viruses express antigens that elicit protective immune reactions from host animals, including humans. The World Organization for Animal Health (OIE) Reference Laboratory for avian influenza at Hokkaido University has established an influenza virus library of all hemagglutinin (HA) and neuraminidase (NA) subtypes and their genes (5–10). The library includes influenza virus strains isolated from natural hosts; these strains have been used to prepare vaccines and have proved to be useful for raising the level of preparedness for future pandemics.
Most conventional influenza vaccines have been manufactured by the embryonated chicken egg-based process. However, the extended time required to produce egg-dependent vaccines might result in too few doses being available to counter a pandemic situation, such as occurred in 2009, or to stop a pandemic originating from a highly pathogenic avian virus, such as an H5N1 virus (11). An alternative to the egg-based process is viral propagation in mammalian cell lines, which also has been used to produce influenza vaccines (12–15). Several cell lines are currently approved for cell culture-based influenza production, and the use of Madin-Darby canine kidney (MDCK) cells and African green monkey Vero cells has been well documented (16–18).
Since a pandemic virus will not always be available from among existing library virus stocks, a cross-protective vaccine design that can use a stock virus with antigenic properties similar to those of the pandemic virus to generate a vaccine should be established. In animal models, intranasal immunization with an influenza virus split-virion vaccine with mucosal adjuvant [e.g., cholera toxin B, poly(I-C), or poly(γ-glutamic acid) nanoparticles] induces cross-protection and in vivo virus clearance against drift variants within a subtype and against different subtypes of virus (19–23). Furthermore, intranasal immunization of mice with formalin-inactivated intact virus alone (without adjuvant), but not with an ether-split vaccine alone, induces cross-protection against the homologous virus, intrasubtype variants, and influenza A viruses of different subtypes (24, 25).
Thus, to protect populations from the next influenza pandemic, a novel rapid emergency vaccine-manufacturing process is urgently needed. For this purpose, we propose a process involving the following steps. (i) Seed viruses for the emergency influenza vaccine that grow well in MDCK cells are made in advance from influenza virus strains in the virus library and stored. (ii) The genes of the stocked seed viruses are analyzed. (iii) When a pandemic occurs, the seed virus whose HA antigenicity most closely matches that of the pandemic virus is grown in MDCK cells and used to make a formalin-inactivated whole-virion vaccine. (iv) Individuals are immunized intranasally with the vaccine to protect them from the pandemic influenza virus. In the present study, we examined the feasibility of this approach to overcome shortages in the effective influenza vaccine supply in emergency pandemic situations, using a pathogenic H5N1 influenza virus reassortant strain from the influenza virus library.
MATERIALS AND METHODS
Cells.
MDCK cells, which were kindly provided by the Kanonji Institute, The Research Foundation for Microbial Diseases of Osaka University (Kanonji, Japan), were maintained in a serum-free medium, Opti-Pro SFM (Invitrogen, Carlsbad, CA) supplemented with 0.3 mg/ml l-glutamine and 8 μg/ml gentamicin. The cells were maintained at 37°C in 5% CO2 (26).
Virus strain.
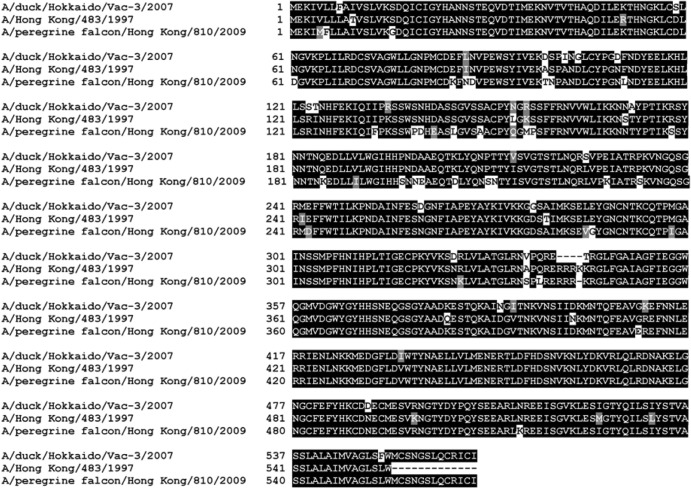
A low-pathogenicity influenza virus reassortant strain, A/duck/Hokkaido/Vac-3/2007 (Vac-3) (H5N1) (10), was stocked in an influenza virus library containing all HA and NA subtypes and their genes. The Vac-3 H5N1 strain was generated originally with A/duck/Hokkaido/101/04 (H5N3) as the HA and NS gene provider and A/duck/Hokkaido/262/04 (H6N1) as the PB2, PB1, PA, NP, NA, and M gene provider. The complete nucleotide sequences of the Vac-3 H5N1 strain are registered in GenBank (accession numbers AB355926 to AB355933). For mouse challenge experiments, mouse-adapted Vac-3 passaged 22 times (P22) (H5N1), mouse-adapted A/Brisbane/59/07 (BR/59/07) (H1N1), A/Hong Kong/483/1997 (HK/483/97) (H5N1, clade 0), which was isolated from a patient with a highly pathogenic avian influenza virus infection in 1997, and A/peregrine falcon/Hong Kong/810/2009 (PF/HK/810/09) (H5N1, clade 2.3.4.), which is a highly pathogenic avian influenza virus, were used (alignment of the deduced HA amino acid sequences of the H5N1 strains is shown in Fig. 1). A/Brisbane/59/2007 (BR/59/07) (H1N1) was kindly provided by Takato Odagiri (National Institute of Infectious Diseases, Tokyo, Japan). Both Vac-3 P22 and BR/59/07 were originally nonpathogenic to mice; therefore, mouse-adapted strains for challenge experiments were generated as follows. Mice were inoculated with virus (108 PFU in 40 μl phosphate-buffered saline [PBS]), and their lungs were harvested 3 days later. The lung tissue was homogenized in PBS using Multi-Beads Shocker (Yasui Kikai, Osaka, Japan) (one set of lungs per 1 ml PBS) and centrifuged (10,000 × g for 10 min), and the supernatants were harvested. Naive mice were inoculated with the supernatant (40 μl/mouse). These steps were repeated for a total of 10 inoculations. The mouse-adapted viruses were then grown once in MDCK cells, and the mouse 50% lethal dose (LD50) values for the viruses were assessed. Mouse-adapted Vac-3 P22 and mouse-adapted BR/59/07 were grown in MDCK cells, whereas HK/483/97 and PF/HK/810/09 production was in chicken eggs.
Fig 1.
Alignment of deduced HA amino acid sequences of the H5N1 strains used in this study. The alignment was based on published amino acid sequences (GenBank accession numbers BAF76006.1, AAF74330.1, and BAI39636.1). Black blocks, regions with identical amino acids; gray blocks, regions with similar amino acids; white blocks, regions with nonidentical nonsimilar amino acids. Dashes, absent or deleted amino acids.
Adaptation of the Vac-3 virus to MDCK cells.
Vac-3 was used to inoculate MDCK cells cultured at 35°C in minimal essential medium (MEM) supplemented with 0.3 mg/ml l-glutamine, 0.1% bovine serum albumin (BSA), 0.8 μg/ml crystal trypsin (Sigma, St. Louis, MO), and 8 μg/ml gentamicin. Three days after infection, the virus-containing supernatant was collected and was used to measure the virus titer and to inoculate fresh MDCK cells at a 1:1,000 dilution. After 22 passages, the virus-containing supernatant was collected and stored at −80°C. The stock virus, A/duck/Hokkaido/Vac-3/2007 P22 (Vac-3 P22), was used as a seed virus for an inactivated whole-virion influenza vaccine.
Virus growth assay.
Confluent MDCK cell monolayers in 6-cm petri dishes were infected with virus at a multiplicity of infection (MOI) of 0.001, in 800 μl of MEM with 0.1% BSA. After being washed with MEM without supplement, the infected cells were incubated at 35°C in 5 ml virus growth medium supplemented with 0.8 μg/ml crystal trypsin. The supernatant was collected at the times indicated in Fig. 2, and the virus titer in the supernatant was determined by plaque assay.
Fig 2.
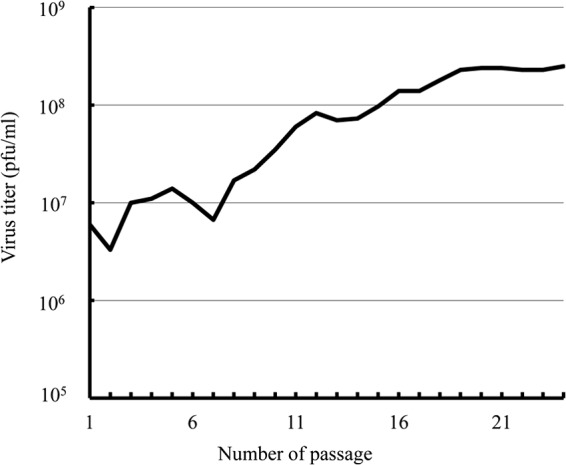
Enhanced replication of A/duck/Hokkaido/Vac-3/2007 (Vac-3) (H5N1) with repeated passage in MDCK cells. MDCK cells were inoculated at 35°C with Vac-3 in MEM supplemented with 0.3 mg/ml l-glutamine, 0.1% BSA, 0.8 μg/ml crystal trypsin, and 8 μg/ml gentamicin. Three days after infection, the virus-containing supernatant was collected and used for the inoculation of fresh MDCK cells at a 1:1,000 dilution, and the viral titer in the supernatant was measured by a virus plaque assay.
Plaque assay.
Viruses diluted 10-fold in 300 μl of MEM with 0.1% BSA were applied to confluent monolayers of MDCK cells in 6-well plates and incubated at 35°C for 1 h. Unbound viruses were removed, and the cells were washed with MEM. The cells were then overlaid with 2 ml virus growth medium containing 0.8% agarose (Sigma) and 0.8 μg/ml crystal trypsin (Sigma). After a 72-h incubation at 35°C, the cells were fixed with 10% formaldehyde and stained with 0.1% crystal violet solution.
Virus gene sequencing.
At two time points, i.e., after 2 passages and after 22 passages, the virus-containing supernatant was collected and the virus was purified by plaque cloning. This purification step was repeated 3 times at each time point. The virus-containing supernatants were collected, and the viral RNA was isolated using TRIzol reagent (Life Technologies, Carlsbad, CA) and reverse-transcribed with the Uni-12 primer (27), using a Superscript III reverse transcriptase kit (Life Technologies). The viral genes were then amplified by PCR with KOD-Plus DNA polymerase (Toyobo, Osaka, Japan), according to the manufacturer's protocol, using the universal primer set (27). The PCR products were purified with a QIAquick gel extraction kit (Qiagen, Venlo, Netherlands). The DNA template was sequenced using a BigDye direct cycle sequencing kit (Life Technologies), according to the manufacturer's protocol. The sequencing primers were designed according to the NCBI reference sequence, and samples were analyzed using an Applied Biosystems 3500 genetic analyzer (Life Technologies). The DNA sequences were completed and edited using the DNASIS Pro software package (Hitachi Solutions, Tokyo, Japan).
Vaccine preparation.
The seed virus, Vac-3 P22 (H5N1), was grown for vaccine production using a BelloCell cell culture system (CESCO Bioengineering, Taichung, Chinese Taipei). For cell attachment, a bottle was filled with 500 ml medium (10% fetal bovine serum [FBS] in MEM, with the glucose level adjusted to 3 g/liter) and inoculated with MDCK cells at 4 × 105 cells/ml. The bottle was then placed on a BelloStage console, with settings of an up/down speed of 2 mm/s and holding times of 30 s at the top and 0 s at the bottom for the first 3 h. The settings were then changed to an up/down speed of 1 mm/s and holding times of 10 s at the top and 30 s at the bottom, to allow sufficient aeration. The medium was completely replaced after the first 48 h and then either the medium was partially replaced or glucose concentrate was added as needed to maintain a glucose level of 2 g/liter for the MDCK cells. The cell density was measured periodically using a CVD nucleus staining kit (CESCO Bioengineering), by spotting samples taken from the bottle onto disks. Glucose concentrations were measured using a GlucCell meter (CESCO Bioengineering).
When the MDCK cell concentration reached about 2 × 107 to 3 × 107 cells/ml, the cultivation medium was completely aspirated and replaced with 500 ml of PBS. The bottles were placed on the BelloStage and washed for 5 min using the above-described settings for aeration, and then the PBS was completely aspirated and replaced with infection medium (MEM supplemented with 0.3 mg/ml l-glutamine, 8 μg/ml gentamicin, and 0.8 μg/ml crystal trypsin, with the glucose concentration adjusted to 3 g/liter). The cells were then infected at a MOI of 0.001 and incubated using the same settings for the BelloStage as for the cultivation.
Seventy-two hours after infection, the medium was collected and passed through a 0.22-μm filter (TPP, Trasadingen, Switzerland). The viruses in the medium were then concentrated and purified as follows. First, a tangential flow filtration ultrafiltration set (Millipore, Bedford, MA) was used for the primary concentration (100-fold), using a filter with a 50-kDa cutoff value. The viruses were further concentrated by two centrifugations through a discontinuous sucrose gradient (30% and 60% [wt/vol] sucrose in PBS) at 75,000 × g for 1.5 h at 4°C, in a Himac CP-80WX preparative ultracentrifuge (Hitachi, Japan). The purified viruses were recovered from the interface of the two sucrose layers, transferred to a 1- to 5-ml QuixSep microdialyzer cassette (Orange Scientific, Braine-l'Alleud, Belgium), and dialyzed against 2 liters of PBS at 4°C for 24 h.
After dialysis, the protein concentration was measured using a Pierce BCA protein assay kit (Thermo Scientific, Waltham, MA) and adjusted to 1 mg/ml, and the virus was inactivated by incubation with 0.02% formalin for 28 days at 4°C. Virus inactivation was confirmed by several blind passages on MDCK cells, followed by visually checking for plaque formation under a microscope. Finally, the formalin-inactivated vaccine was pressure-dialyzed against PBS using a QuixSep microdialyzer (Orange Scientific). For every batch (4 bottles) with a total volume of 2 liters of infection medium, we obtained 3 to 4 mg of total viral protein after concentration and sucrose gradient purification.
Seed viruses in suspension were inactivated by incubation with 0.2% formalin for 28 days at 4°C. Virus inactivation was confirmed by inoculation into MDCK cells, followed by checking for plaque formation. The formalin-inactivated virus suspension was diluted with PBS to a final concentration of 100 μg total virus protein per ml.
Vaccination and virus challenge.
BALB/c mice (6 weeks old, female; Japan SLC, Shizuoka, Japan) were anesthetized and inoculated intranasally (inoculation volume, 20 μl) with PBS or PBS containing Vac-3 P22 (H5N1) formalin-inactivated whole-virion vaccine (1, 3, or 10 μg), on days 0 and 21. To assess mouse mortality rates upon virus infection, the mice were inoculated intranasally, 14 days after the final immunization, with 40 μl of PBS containing one of the following: 100 × LD50 of mouse-adapted Vac-3 P22 (106 PFU), 100 × LD50 of HK/483/97 (H5N1, clade 0; 107.1 × 50% egg infective dose [EID50]), 100 × LD50 of PF/HK/810/09 (H5N1, clade 2.3.4; 103.5 × EID50), or 100 × LD50 of mouse-adapted BR/59/07 (H1N1; 107 PFU). The mortality status and weight loss of the mice were assessed daily for up to 14 days thereafter. To measure virus clearance in the lungs of the vaccine-immunized mice, the mice were inoculated intranasally, 14 days after the final immunization, with 20 μl of PBS containing 100 × LD50 of influenza virus. Three days later, the lungs were excised and homogenized using Multi-Beads Shocker (Yasui Kikai, Osaka, Japan), according to the manufacturer's protocol. The viral titer in the lung homogenate was estimated using a plaque assay. The institutional animal care and use committees of the Graduate School of Veterinary Medicine, Hokkaido University (approval number 11-0140), and the National Institute of Biomedical Innovation (approval number DS21-21) authorized this animal study, and all experiments were performed according to the guidelines of these committees.
Measurement of anti-influenza virus neutralizing antibody titers, IFN-γ ELISPOT assay, and preparation of effector and target cells for cytotoxic T-cell assays.
Neutralizing antibody titers in the mouse sera and bronchoalveolar lavage (BAL) fluids were determined by a micro-cytopathic effect neutralizing test (21, 24). The gamma interferon (IFN-γ) ELISPOT assay was performed as described previously (21, 28).
Effector cells for the cytotoxic assays were prepared as described previously (28), with some modifications. In brief, mice were immunized intranasally with formalin-inactivated whole-virion vaccine on days 0 and 21. On day 35, splenocytes from the vaccine-immunized mice (107 cells) were suspended in 5 ml of complete RPMI 1640 medium. Syngeneic mouse spleen mononuclear cells (MNCs) (5 × 106 cells per 100 μl of serum-free RPMI 1640 medium) were infected with 107 PFU of the influenza virus strain Vac-3 P22 or BR/59/07 for 1 h. After three washes with complete RPMI 1640 medium, the cells were suspended in 5 ml of complete RPMI 1640 medium. The cell suspensions were incubated for 3 h at 37°C in 5% CO2 and then were irradiated at 3,000 rad. The vaccine-immunized spleen cell suspension (3 × 107 cells in 15 ml of complete RPMI 1640 medium) and the influenza virus-infected feeder spleen cell suspension (1.5 × 107 cells in 15 ml of complete RPMI 1640 medium) were mixed in a 75-cm2 culture flask and cocultured for 6 days at 37°C in 5% CO2, to induce virus-specific cytotoxic T lymphocytes (CTLs) (effector cells). To prepare target cells, 5 × 106 P815 cells (JCRB Cell Bank, Ibaraki, Japan) were suspended in 1 ml of FBS-free RPMI 1640 medium and incubated for 1 h at 37°C in 5% CO2 with 5 × 107 PFU of Vac-3 P22 or BR/59/07. After a 1-h incubation, the cells were washed 3 times with complete RPMI 1640 medium. For cytotoxicity assays, the infected P815 cells were labeled with Na51CrO4 (PerkinElmer, Waltham, MA) as described previously (24). The target cells were suspended at 105 cells/ml in complete RPMI 1640 medium for use in the CTL assay. 51Cr-labeled target P815 cells were diluted to 105 cells per ml in complete RPMI 1640 medium, and 100 μl of the target cell suspension was added to each well of a 96-well, round-bottomed, microtiter plate. Effector cells, also in 100 μl of complete RPMI 1640 medium, were added at effector-to-target cell ratios of 50:1, 17:1, 5:1, and 1.7:1. Following a 4-h incubation at 37°C in 5% CO2, 100 μl of the supernatant was removed to determine the concentration of 51Cr released. All samples were counted in a TopCount NXT microplate scintillation and luminescence counter (PerkinElmer), and percent specific release was calculated as [(experimental release − spontaneous release)/(total release − spontaneous release)] × 100.
Statistical evaluations.
Fisher's exact test, performed using Statcel2 software (OMS, Tokyo, Japan), was used to evaluate the differences between groups in the mortality experiments. To analyze the data in the other experiments, nonparametric Student t tests were used. P values of <0.05 were considered significant.
RESULTS
Adaptation of an H5N1 influenza A virus strain from the influenza virus library for MDCK cells and mutations associated with the adaptation to MDCK cells.
We first adapted an influenza A virus reassortant strain, A/duck/Hokkaido/Vac-3/07 (Vac-3) (H5N1), from an influenza virus library containing all HA and NA subtypes for growth in MDCK cells by performing serial passages in those cells. The initial viral titers in the first and second passages were 6 × 106 PFU/ml and 3.3 × 106 PFU/ml, respectively (Fig. 2). After 8 passages, the viral titer had increased more than 5 times; after 16 passages, the titer was over 108 PFU/ml. After 22 passages, the viral titer remained the same, at 2.4 × 108 PFU/ml (Fig. 2).
To understand the molecular basis for the 40-fold increase in viral titers caused by adaptation to MDCK cells, twice-passaged virus (P2), in which the amino acids were all the same as in the original strain (data not shown), and 22-times-passaged virus (P22) Vac-3 were biologically cloned by virus plaque purification and sequenced. The sequences of all six P2 clones examined were the same as that of the original strain (data not shown). The sequences of all six P22 clones examined also matched each other, with acquired mutations mapping to the genes for the PB2 and PA proteins but not the HA protein (Fig. 3A). The P22 clone showed much greater growth than the P2 clone in MDCK cells (Fig. 3B); thus, the mutations might be associated with the enhanced viral growth in MDCK cells. Although amino acid changes at PB2 position 627 (from E to K) and PB2 position 701 (from D to N) are known to result in enhanced viral replication (29, 30), these amino acid changes were not found in P2 or P22.
Fig 3.
Viral mutation and enhanced viral replication with Vac-3 adaptation during repeated passage in MDCK cells. (A) After 2 passages and 22 passages, the virus-containing supernatant was collected and the virus was purified by infection of MDCK cells and isolation from the resulting plaques (P2, clones after 2 passages [n = 6 clones]; P22, clones after 22 passages [n = 6 clones]). The amino acid sequences of the clones were aligned, and discrepancies were assessed. (B) Confluent MDCK cells were inoculated with six P2 clones and six P22 clones in 6-cm petri dishes at a MOI of 0.001, and viral plaque assays were performed. ∗, P < 0.05 versus the group of P2 clones.
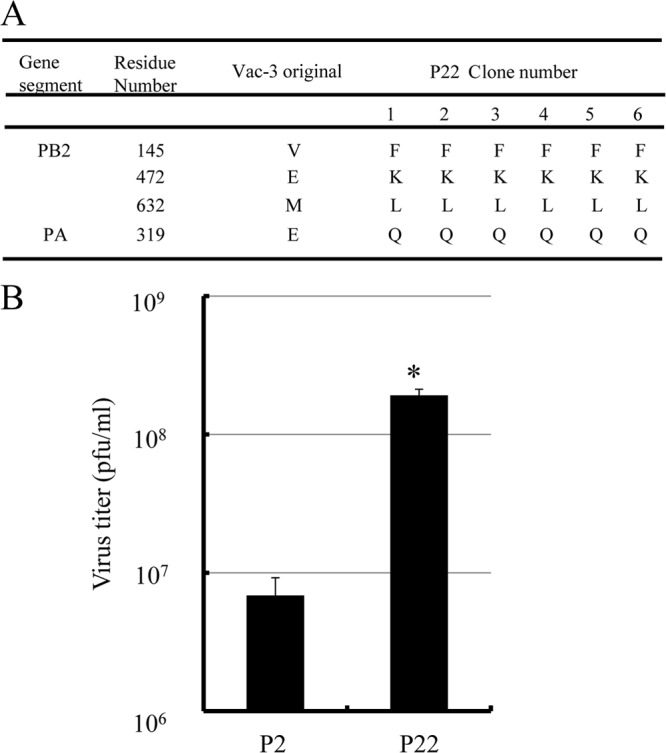
Cross-protection of mice immunized with inactivated whole-virion vaccine from MDCK cell-adapted A/duck/Hokkaido/Vac-3/07 P22 (Vac-3 P22) against challenges with influenza viruses of the same subtype.
We next produced a formalin-inactivated whole-virion influenza vaccine from the P22 strain of Vac-3 (Vac-3 P22) (H5N1) and determined whether the intranasal immunization of mice with this vaccine induced protection against the homotypic virus. Mice were intranasally inoculated twice with 20 μl of PBS or PBS containing the vaccine. We then examined the survival of the intranasally immunized mice after infection with 100 × LD50 of Vac-3 P22 or A/Hong Kong/483/1997 (HK/483/97) (H5N1, clade 0). All of the intranasally PBS-treated mice lost more than 20% of their body weight and died. In contrast, all of the mice intranasally immunized with 1, 3, or 10 μg of the vaccine lost less than 10% of their body weight after infection with either virus and survived (Fig. 4A and B).
Fig 4.
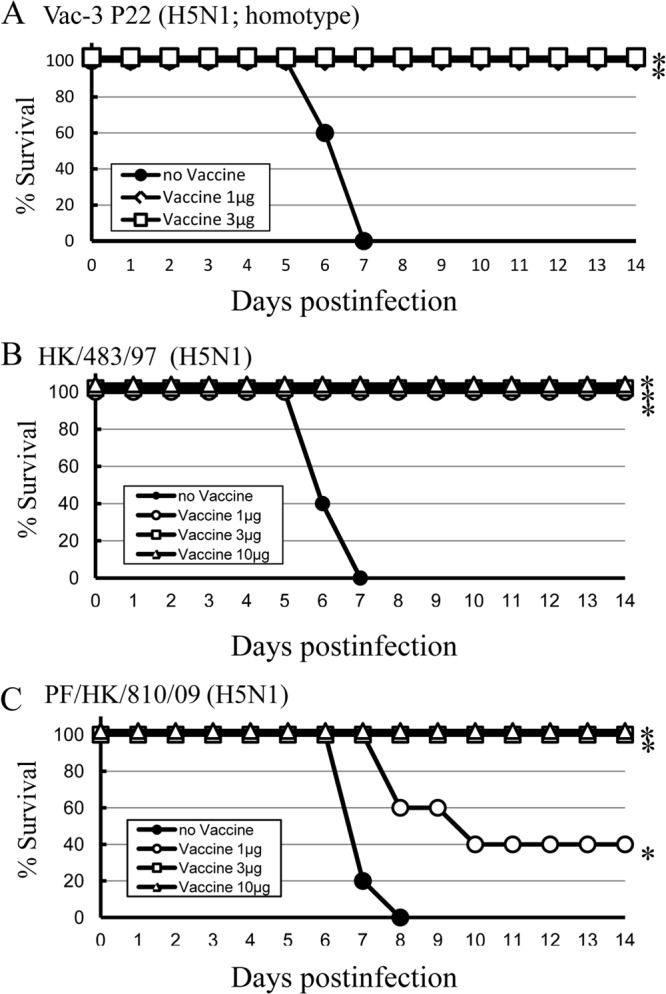
Cross-protection against variants within a subtype after intranasal immunization with vaccine from MDCK cell-adapted Vac-3 P22. Mice (5 per group) were inoculated intranasally twice with PBS (no Vaccine) or with 1, 3, or 10 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine). Fourteen days after the final immunization, the mice were infected with MDCK cell-adapted Vac-3 P22 (H5N1; 106 PFU) (A), A/Hong Kong/483/1997 (HK/483/97) (highly pathogenic, H5N1, clade 0; 107.1 × EID50) (B), or A/peregrine falcon/Hong Kong/810/2009 (PF/HK/810/09) (highly pathogenic, H5N1, clade 2.3.4; 103.5 × EID50) (C), and mortality status was assessed. ∗, P < 0.05 versus the group inoculated intranasally with PBS.
Next, we examined whether intranasal immunization of mice with the A/duck/Hokkaido/Vac-3/07 P22 formalin-inactivated whole-virion vaccine induced protection against A/peregrine falcon/Hong Kong/810/2009 (PF/HK/810/09) (H5N1, clade 2.3.4), an antigenic variant within the viral subtype. All of the mice intranasally immunized with 3 or 10 μg of the vaccine and 40% of the mice intranasally immunized with 1 μg of the vaccine lost less than 10% of their body weight after PF/HK/810/09 infection and survived (Fig. 4C).
We next determined the virus clearance against Vac-3 P22 (H5N1) and HK/483/97 (H5N1, clade 0) in mice intranasally immunized with the formalin-inactivated whole-virion vaccine. Intranasally immunized mice were infected with 100 × LD50 of the two virus strains 14 days after the final immunization. Three days after infection, the lungs of the infected mice were homogenized, and the viral titers in the lung homogenates were assessed. Intranasal immunization with 1, 3, or 10 μg of the vaccine significantly decreased the titers of both viruses (Fig. 5A and B). In addition, intranasal immunization with 3 or 10 μg of the vaccine significantly decreased the titers of PF/HK/810/09 (H5N1, clade 2.3.4) (Fig. 5C). Since Vac-3 P22 formalin-inactivated whole-virion vaccine induced cross-protection against PF/HK/810/09, which has the most varied HA in comparison with Vac-3 P22, these results suggest that the vaccine from MDCK cell-adapted Vac-3 P22 would be effective as a pandemic vaccine for H5N1 influenza virus.
Fig 5.
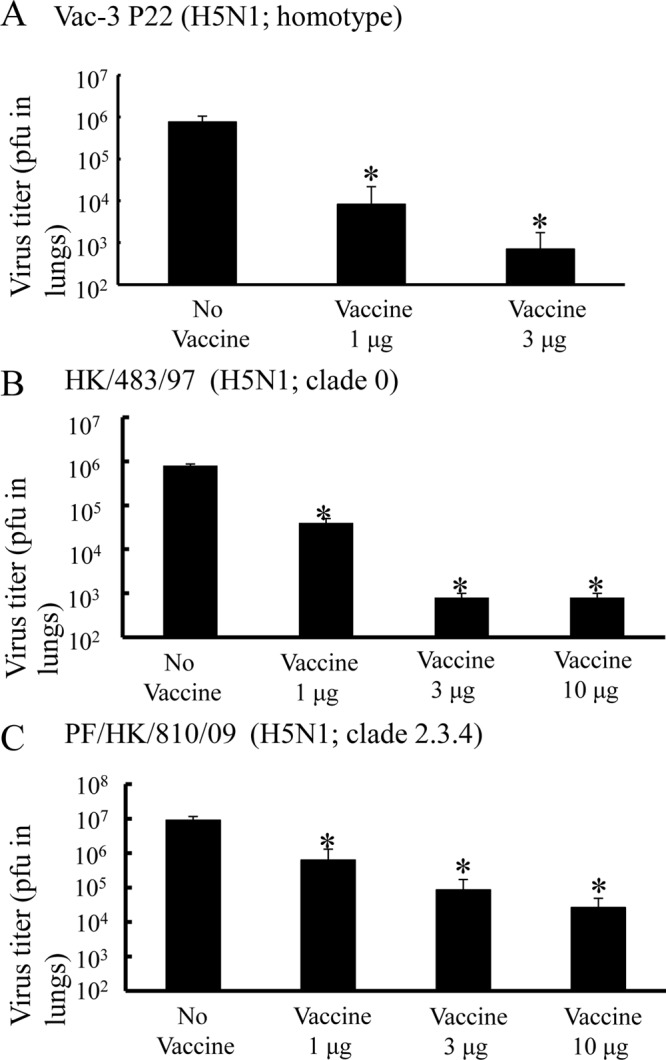
In vivo clearance of homotypic virus and drift variants within a subtype in immunized mice. Groups of mice (5 per group) were inoculated intranasally with PBS (No Vaccine) or with 1, 3, or 10 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine). Fourteen days after the final immunization, the mice were infected with MDCK cell-adapted Vac-3 P22 (H5N1; 106 PFU), HK/483/97 (H5N1, clade 0; 107.1 × EID50), or PF/HK/810/09 (H5N1, clade 2.3.4; 103.5 × EID50). Two days after infection, the lungs were harvested, and the PFU values for Vac-3 P22 (A), HK/483/97 (B), or PF/HK/810/09 (C) in the lung homogenates were determined. Bars, means ± standard deviations for 5 mice. ∗, P < 0.05 versus the group of mice inoculated intranasally with PBS.
Cross-protection of mice immunized with inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 against an influenza virus of a different subtype.
We next examined whether intranasal immunization of mice with the Vac-3 P22 formalin-inactivated whole-virion vaccine induced protection against an influenza virus of a different subtype. Mice were intranasally inoculated twice with 20 μl of PBS or PBS containing 3 μg of the vaccine, and their survival after infection with BR/59/07 (H1N1) was examined. All of the intranasally PBS-inoculated mice lost more than 20% of their body weight and died. In contrast, all of the mice intranasally immunized with the vaccine lost less than 10% of their body weight after BR/59/07 (H1N1) infection and survived (Fig. 6A). Furthermore, intranasal immunization with the vaccine significantly decreased the titers of BR/59/07 (H1N1) (Fig. 6B). Thus, intranasal immunization with the inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 induced cross-protection against a different subtype of the influenza virus.
Fig 6.
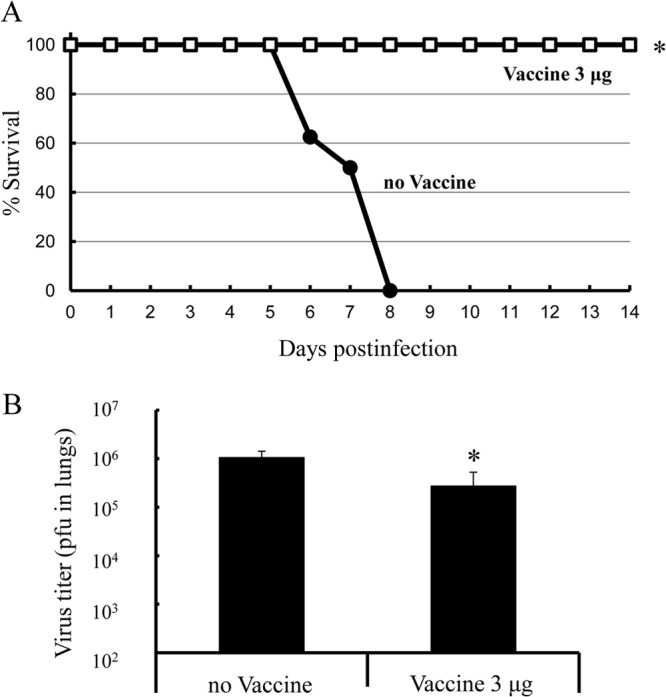
Cross-protection against and in vivo clearance of a different subtype of influenza virus in immunized mice. (A) Mice (5 per group) were inoculated intranasally twice with PBS (no Vaccine) or with 3 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine). Fourteen days after the final immunization, the mice were infected with 107 PFU of A/Brisbane/59/2007 (BR/59/07) (H1N1), and mortality status was assessed. (B) Mice (5 per group) were inoculated intranasally with PBS (no Vaccine) or 3 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine) and were infected with 107 PFU of BR/59/07, as described for panel A. Two days after infection, the lungs were harvested, and the numbers of PFU of BR/59/07 in the lung homogenates were assessed. Bars, means ± standard deviations for 5 mice. ∗, P < 0.05 versus the group of mice inoculated intranasally with PBS.
Cross-reactive neutralizing antibodies against several influenza viruses in mice intranasally immunized with the whole-virion vaccine from MDCK cell-adapted Vac-3 P22.
Several studies have demonstrated that intranasal immunization induces both humoral and cell-mediated immunity, suggesting that either or both of them might contribute to cross-protection. Therefore, we next examined how intranasal immunization with Vac-3 P22 formalin-inactivated whole-virion vaccine induced cross-protection. First, we determined the neutralizing antibody titers against several influenza virus strains in mice intranasally immunized with the Vac-3 P22 vaccine. Neutralizing antibodies for Vac-3 P22 (H5N1) and HK/483/97 (H5N1), but not for PF/HK/810/09 (H5N1) or BR/59/07 (H1N1), were detected in both BAL fluids and sera of immunized mice (Fig. 7). These results suggest that the vaccine induced a cross-protective humoral immune response to the homologous virus and to some of the antigenic variants within the influenza virus subtype but not to all variants within the subtype or to viruses of a different subtype.
Fig 7.
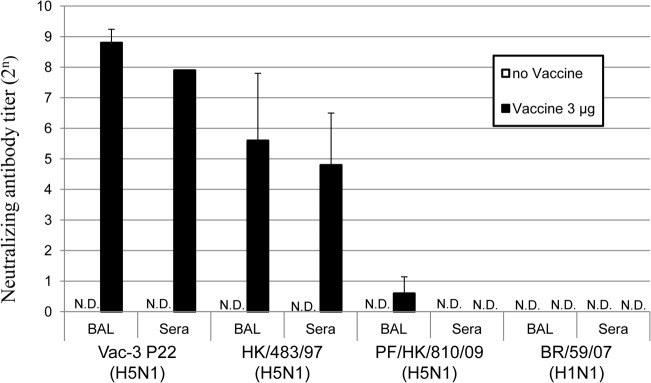
Cross-reactive anti-influenza neutralizing antibody titers in the BAL fluids and sera of immunized mice. Mice (50 per group) were inoculated intranasally twice with PBS (no Vaccine) or with 3 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine). Fourteen days after the final immunization, BAL fluid and serum samples were harvested. For BAL fluid, samples from 5 mice were pooled, pretreated with receptor-destroying enzyme, and concentrated. For serum, samples from 5 mice were pooled and pretreated with receptor-destroying enzyme. The neutralizing antibody titers for MDCK cell-adapted Vac-3 P22 (H5N1), HK/483/97 (H5N1), PF/HK/810/09 (H5N1), or BR/59/07 (H1N1) were then assessed. Bars, means ± standard deviations for 10 samples. N.D., not detected.
Cross-reactive cell-mediated immunity against several influenza viruses in mice intranasally immunized with whole-virion vaccine from MDCK cell-adapted Vac-3 P22.
We next determined whether a cross-protective cell-mediated immune response contributed to cross-protection against different subtypes of influenza virus, by performing IFN-γ ELISPOT assays. Interestingly, immunization with the Vac-3 P22 formalin-inactivated whole-virion vaccine resulted in equally greater numbers of IFN-γ spots in MNCs restimulated with UV-treated Vac-3 P22 (H5N1), PF/HK/810/09 (H5N1), and BR/59/07 (H1N1) (Fig. 8).
Fig 8.
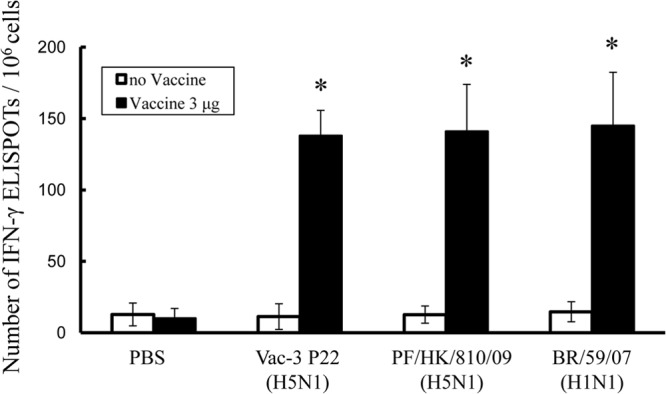
Cross-reactive influenza antigen-specific IFN-γ ELISPOT responses in the spleen MNCs of immunized mice. Mice (5 per group) were inoculated intranasally with PBS (no Vaccine) or with 3 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine). Fourteen days after the final immunization, MNCs were harvested and stimulated for 48 h with 106 PFU of MDCK cell-adapted Vac-3 P22 (H5N1), HK/483/97 (H5N1), PF/HK/810/09 (H5N1), or BR/59/07 (H1N1), which had been inactivated by pretreatment with 5,000 J/cm2 of UV radiation, in anti-IFN-γ monoclonal antibody-coated 96-well filtration plates. After stimulation, the plates were stained and the numbers of IFN-γ spots were determined. ∗, P < 0.01 versus the group of mice immunized with PBS.
Next, we assayed the cytotoxicity of CTLs against influenza virus-infected cells. As shown in Fig. 9, intranasal immunization with the Vac-3 P22 vaccine induced CTL activity not only for Vac-3 P22 (H5N1) but also for BR/59/07 (H1N1). The cross-reactive CTL activity against PF/HK/810/09 (H5N1) was not examined, because no facility was available to perform the CTL assay by using radioisotopic materials under the required biosafety level 3 conditions. However, since a cross-reactive cell-mediated immune response against a different subtype was shown clearly by the IFN-γ ELISPOT assay, it is likely that the CTLs are also cytotoxic against PF/HK/810/09 (H5N1).
Fig 9.
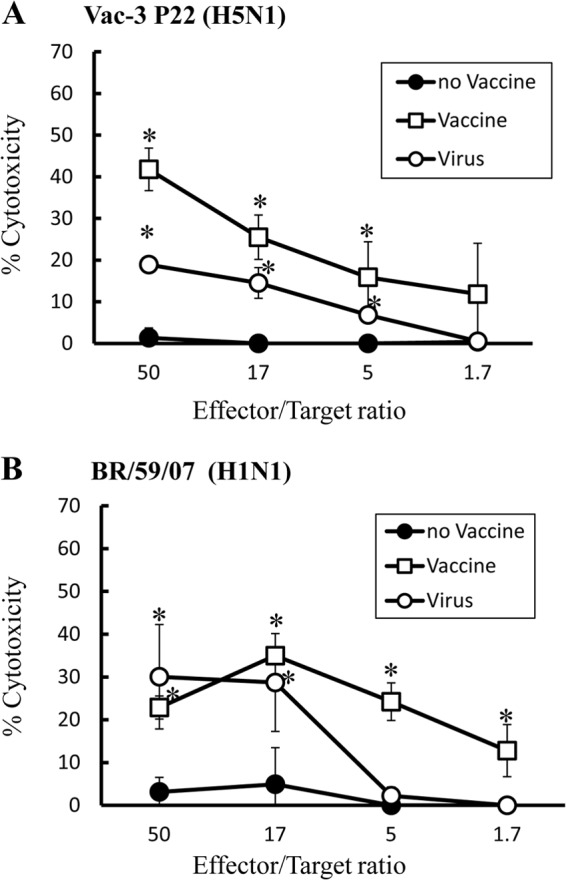
Cross-reactive anti-influenza CTL activity in immunized mice. Mice (5 per group) were inoculated intranasally with PBS (no Vaccine) or with 3 μg of formalin-inactivated whole-virion vaccine from MDCK cell-adapted Vac-3 P22 (Vaccine) or were infected intranasally with 103 PFU of Vac-3 P22 (Virus) twice. Fourteen days after the final immunization, spleen MNCs were restimulated with syngeneic mouse spleen cells infected with Vac-3 P22 (H5N1) (A) or BR/59/07 (H1N1) (B), to induce effector cells. 51Cr-labeled target cells infected with Vac-3 P22 or BR/59/07 and the effector cells, restimulated with the same virus as was used to infect the target cells, were added at the indicated effector-to-target cell ratios. Following a 4-h incubation at 37°C in 5% CO2, 100 μl of the supernatant was harvested to determine the concentration of 51Cr released. ∗, P < 0.01 versus the group of mice immunized with PBS.
DISCUSSION
In the present study, we have assessed whether our novel emergency vaccine-manufacturing process would be useful for preventing infection in the next influenza pandemic. We have demonstrated that our process, which uses an influenza virus library, cell culture-based vaccine production, and intranasal immunization to induce cross-protection, provides effective protection against homotypic and drift variants within a subtype of influenza virus infections. These results suggest that this vaccine-manufacturing process might be applied effectively for the next generation of pandemic influenza vaccines.
It is currently impossible to predict which influenza virus strains will cause the next pandemic. We previously proposed the use of avian influenza viruses as candidate vaccine strains when antigenically related and low-pathogenicity viruses from humans are not available (6, 7). Therefore, we have been establishing a library of nonpathogenic influenza A virus strains of different subtypes, without using reverse genetics technology (7). Furthermore, Itoh et al. demonstrated that a vaccine prepared from a nonpathogenic influenza virus strain from the influenza library conferred protective immunity against infection by a highly pathogenic avian influenza virus of the same subtype (6). In the present study, we demonstrated that a virus strain from the influenza library was modified to a high-titer vaccine virus by adaptation in MDCK cells and that intranasal immunization with the formalin-inactivated virus vaccine induced cross-protection against homotypic and heterotypic influenza virus infections.
Efficient influenza vaccine production requires a system that can produce a large amount of vaccine virus rapidly and safely. The cell-based method has several advantages over the current process using embryonated chicken eggs, including the following: (i) it enables faster and larger-scale vaccine production; (ii) it avoids the potential selection of variants adapted for chicken eggs, which alters virus antigenicity; (iii) egg-based production requires the selection of high-yield vaccine seed viruses; and (iv) egg-produced viruses may contain allergenic components of eggs (11, 12, 16, 31–34). Due to these advantages, the World Health Organization (WHO) has recommended that mammalian cell culture-based vaccines be established (35). Based on our present results, we propose that the preparation and storage of cell-adapted vaccine viruses from the influenza virus library would be useful for the rapid preparation of an emergency vaccine for an influenza pandemic. However, there are still several problems with the substantiation of faster and larger-scale production of a cell-adapted vaccine that need to be clarified in future studies. In addition, it is true that the virus selected for production in the event of a real pandemic might not behave like the current one. This is why many studies on the MDCK cell library strains are ongoing, to establish the cross-protection range for different strains within the same subtype or in different subtypes.
In the present study, MDCK cell-adapted Vac-3 passaged 22 times showed >30-times-greater viral growth in MDCK cells than that after two passages (when the amino acid sequence was identical to that of the original strain) (Fig. 3B). Four point mutations were associated with enhanced viral growth, i.e., three in PB2 (V145F, E472K, and M632L) and one in PA (E319Q). A major determinant of viral tropism is the influenza virus polymerase, since the polymerase, which is composed of the viral proteins PB1, PB2, and PA, assembles with viral RNA and nucleoprotein to mediate transcription and replication of the viral genome (36), suggesting that these mutations are associated with enhanced viral growth. Several studies have examined why the repeated passage of influenza viruses through cultured mammalian cells leads to increased viral growth. For example, the amino acid changes at PB2 position 627 (from E to K) (37–42) and PB2 position 701 (from D to N) (29, 30) in several highly pathogenic avian influenza viruses are important for enhancing viral replication in mammals. In addition, Murakami et al. (11) demonstrated that the amino acid change at HA2 position 117 (from N to Y) in human H1N1 influenza virus strain A/Puerto Rico/8/1934 is one of the factors responsible for the enhanced viral growth observed after repeated passage in Vero cells. However, the amino acid at PB2 position 627 was E and that at PB2 position 701 was D in both P2 and P22, indicating that the previously reported amino acid changes did not occur. Thus, the changes we observed in PB2 (V145F, E472K, and M632L) and PA (E319Q) might be novel mutations that promote viral growth in MDCK cells. We are now studying which changes are most responsible for enhanced growth.
Several studies have demonstrated that intranasal immunization with several forms of influenza vaccine induces cross-protection against drift variants within a subtype and against viruses of different subtypes (19–22, 24, 25, 43). Cross-protection with intranasal immunization has been shown to occur mainly through influenza virus-specific humoral immunity (i.e., anti-influenza neutralizing antibody secretion in serum and mucosa) and cell-mediated immunity (i.e., cytotoxic T-cell activity against influenza virus-infected cells). Intranasal immunization with gamma-radiation-inactivated whole-virion influenza vaccine induces influenza virus-specific cross-reactive humoral and cellular immunity (44, 45). On the other hand, formalin-inactivated whole-virion influenza vaccine induces cross-reactive humoral immunity but rarely cellular immunity (24, 45). Furthermore, cross-reactive neutralizing antibodies contribute to the cross-protection caused by intranasal immunization with formalin-inactivated whole-virion vaccine, and cross-reactive neutralization by intranasal immunization with a formalin-inactivated H1N1 influenza virus vaccine includes drift variants within the influenza virus subtype (24). However, Takada et al. demonstrated that formalin-inactivated H5N1 influenza whole-virion vaccine in intranasal immunization does not induce cross-protection against different influenza virus subtypes through cross-reactive neutralizing antibodies (25). In the present study, we have demonstrated that intranasal immunization with a formalin-inactivated H5N1 influenza virus vaccine induces cross-reactive humoral and cell-mediated immunity. While cross-reactive neutralizing antibody responses were observed for the homotypic H5N1 influenza virus and its drift variants but not a virus of a different subtype, cross-reactive cell-mediated immune responses were observed for all strains tested, including that of a different subtype. Therefore, formalin-inactivated influenza vaccine might induce cross-reactive cell-mediated immune responses that provide cross-protection against viruses of different subtypes. There are many responses other than the antiviral neutralization response associated with cross-protection, e.g., antibody-dependent cell cytotoxicity. It should be noted that cross-protection against the H1N1 virus is at least partially NA-mediated. Since no challenge with a virus carrying different HA and NA forms has been included, we must clearly limit the description of “cross-reactive” to H5N1 versus H1N1.
Our previous study (24) demonstrated that intranasal immunization with formalin-inactivated whole-virion influenza vaccine from human seasonal H1N1 influenza viruses did not induce cross-reactive cell-mediated immunity, and the reason why the formalin-inactivated H5N1 influenza virus whole-virion vaccine, but not the H1N1 influenza virus whole-virion vaccine, induced cross-reactive cell-mediated immune responses remains to be elucidated. It also is still unclear which formalin-inactivated virus strains can induce cross-reactive cell-mediated immune responses and whether an intranasal formalin-inactivated whole-virion vaccine can induce cross-protection against a virus of a different subtype via a humoral immune response in some cases.
Systemic immunization with formalin-inactivated whole-virion influenza vaccine derived from a pathogenic avian H5N1 influenza virus, but not from human H1N1 influenza viruses, induced CTL activity against the homotypic virus and a highly pathogenic influenza virus (46). Furthermore, Budimir et al. (47) reported that subcutaneous immunization with β-propiolactone and a formalin-inactivated whole-virion vaccine induced cross-protection against an influenza virus of a different subtype, in a CD8+ T-cell-dependent manner. In the present study, we confirmed that intranasal immunization, like subcutaneous immunization, with a formalin-inactivated whole-virion influenza vaccine induced cross-reactive cell-mediated immune responses against homotypic and heterotypic influenza viruses. However, whether the range and magnitude of the cross-reactive cell-mediated immune responses and cross-protection induced by intranasal immunization with a formalin-inactivated whole-virion vaccine are greater than those induced by subcutaneous immunization remains unknown. These procedures will be compared in future studies.
The ELISPOT assay suggests that the responses are T-cell mediated; however, which antigens play a role in the cross-reactive T-cell-mediated immune responses remains elusive. For future studies, we will consider using overlapping peptide libraries covering different viral proteins, which would give a better idea of how much of the T-cell response is directed against HA versus more-conserved internal proteins.
In the present study, we found that intranasal immunization with a formalin-inactivated whole-virion influenza vaccine induced cross-protection against the homotypic virus, drift variants within a virus subtype, and a virus of a different subtype. The cross-protection was due, at least in part, to cross-reactive neutralizing antibodies in the nasal cavity, lungs, and serum and to IFN-γ-secreting cells. Influenza virus vaccines for humans need to induce effective cross-protection with minimal side effects. A cold-adaptive live influenza vaccine for intranasal immunization (FluMist; MedImmune) is available clinically in the United States and Europe but not Japan. However, it is approved only for individuals 2 to 49 years of age and it can result in viral replication, leading to influenza-like syndromes (24). The formalin-inactivated whole-virion vaccine is licensed clinically only for intramuscular injection; the safety and side effects of intranasal immunization with formalin-inactivated whole-virion vaccine still need to be established. Nevertheless, since viral reactivation cannot occur with a formalin-inactivated whole-virion vaccine, this should be a good candidate for intranasal pandemic influenza vaccines for clinical use in the near future.
ACKNOWLEDGMENTS
We thank Yoshinobu Okuno, Toyokazu Ishikawa, and Yasuyuki Gomi (Kanonji Institute, The Research Foundation for Microbial Diseases of Osaka University) for providing the MDCK cells.
This study was partly supported by grants from the Japan Initiative for Global Research Network on Infectious Diseases (J-GRID), Japan Science and Technology Agency basic research programs, the Japanese Ministry of Health, Welfare, and Labor, and the Japanese Ministry of Education, Culture, Sports, and Science and by the Research Center for Zoonosis Control of Hokkaido University.
Footnotes
Published ahead of print 1 May 2013
REFERENCES
- 1. Doherty PC, Turner SJ, Webby RG, Thomas PG. 2006. Influenza and the challenge for immunology. Nat. Immunol. 7:449–455 [DOI] [PubMed] [Google Scholar]
- 2. Russell CJ, Webster RG. 2005. The genesis of a pandemic influenza virus. Cell 123:368–371 [DOI] [PubMed] [Google Scholar]
- 3. Wright PF, Neuman G, Kawaoka Y. 2007. Orthomyxoviruses, p 1691–1740 In Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE. (ed), Fields virology, 5th ed Lippincott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 4. Gerdil C. 2003. The annual production cycle for influenza vaccine. Vaccine 21:1776–1779 [DOI] [PubMed] [Google Scholar]
- 5. Isoda N, Sakoda Y, Kishida N, Soda K, Sakabe S, Sakamoto R, Imamura T, Sakaguchi M, Sasaki T, Kokumai N, Ohgitani T, Saijo K, Sawata A, Hagiwara J, Lin Z, Kida H. 2008. Potency of an inactivated avian influenza vaccine prepared from a non-pathogenic H5N1 reassortant virus generated between isolates from migratory ducks in Asia. Arch. Virol. 153:1685–1692 [DOI] [PubMed] [Google Scholar]
- 6. Itoh Y, Ozaki H, Tsuchiya H, Okamoto K, Torii R, Sakoda Y, Kawaoka Y, Ogasawara K, Kida H. 2008. A vaccine prepared from a non-pathogenic H5N1 avian influenza virus strain confers protective immunity against highly pathogenic avian influenza virus infection in cynomolgus macaques. Vaccine 26:562–572 [DOI] [PubMed] [Google Scholar]
- 7. Kida H, Sakoda Y. 2006. Library of influenza virus strains for vaccine and diagnostic use against highly pathogenic avian influenza and human pandemics. Dev. Biol. (Basel) 124:69–72 [PubMed] [Google Scholar]
- 8. Samad RA, Nomura N, Tsuda Y, Manzoor R, Kajihara M, Tomabechi D, Sasaki T, Kokumai N, Ohgitani T, Okamatsu M, Takada A, Sakoda Y, Kida H. 2011. A vaccine prepared from a non-pathogenic H5N1 influenza virus strain from the influenza virus library conferred protective immunity to chickens against the challenge with antigenically drifted highly pathogenic avian influenza virus. Jpn. J. Vet. Res. 59:23–29 [PubMed] [Google Scholar]
- 9. Soda K, Ozaki H, Sakoda Y, Isoda N, Haraguchi Y, Sakabe S, Kuboki N, Kishida N, Takada A, Kida H. 2008. Antigenic and genetic analysis of H5 influenza viruses isolated from water birds for the purpose of vaccine use. Arch. Virol. 153:2041–2048 [DOI] [PubMed] [Google Scholar]
- 10. Soda K, Sakoda Y, Isoda N, Kajihara M, Haraguchi Y, Shibuya H, Yoshida H, Sasaki T, Sakamoto R, Saijo K, Hagiwara J, Kida H. 2008. Development of vaccine strains of H5 and H7 influenza viruses. Jpn. J. Vet. Res. 55:93–98 [PubMed] [Google Scholar]
- 11. Murakami S, Horimoto T, Ito M, Takano R, Katsura H, Shimojima M, Kawaoka Y. 2012. Enhanced growth of influenza vaccine seed viruses in Vero cells mediated by broadening the optimal pH range for virus membrane fusion. J. Virol. 86:1405–1410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Genzel Y, Behrendt I, Konig S, Sann H, Reichl U. 2004. Metabolism of MDCK cells during cell growth and influenza virus production in large-scale microcarrier culture. Vaccine 22:2202–2208 [DOI] [PubMed] [Google Scholar]
- 13. Hu AY, Tseng YF, Weng TC, Liao CC, Wu J, Chou AH, Chao HJ, Gu A, Chen J, Lin SC, Hsiao CH, Wu SC, Chong P. 2011. Production of inactivated influenza H5N1 vaccines from MDCK cells in serum-free medium. PLoS One 6:e14578. 10.1371/journal.pone.0014578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hu AY, Weng TC, Tseng YF, Chen YS, Wu CH, Hsiao S, Chou AH, Chao HJ, Gu A, Wu SC, Chong P, Lee MS. 2008. Microcarrier-based MDCK cell culture system for the production of influenza H5N1 vaccines. Vaccine 26:5736–5740 [DOI] [PubMed] [Google Scholar]
- 15. Kistner O, Barrett PN, Mundt W, Reiter M, Schober-Bendixen S, Dorner F. 1998. Development of a mammalian cell (Vero) derived candidate influenza virus vaccine. Vaccine 16:960–968 [DOI] [PubMed] [Google Scholar]
- 16. Bernstein DI. 2010. Cell culture-derived influenza vaccines: has their time come? Clin. Infect. Dis. 51:1005–1006 [DOI] [PubMed] [Google Scholar]
- 17. Onions D, Egan W, Jarrett R, Novicki D, Gregersen JP. 2010. Validation of the safety of MDCK cells as a substrate for the production of a cell-derived influenza vaccine. Biologicals 38:544–551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hussain AI, Cordeiro M, Sevilla E, Liu J. 2010. Comparison of egg and high yielding MDCK cell-derived live attenuated influenza virus for commercial production of trivalent influenza vaccine: in vitro cell susceptibility and influenza virus replication kinetics in permissive and semi-permissive cells. Vaccine 28:3848–3855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ichinohe T, Watanabe I, Ito S, Fujii H, Moriyama M, Tamura S, Takahashi H, Sawa H, Chiba J, Kurata T, Sata T, Hasegawa H. 2005. Synthetic double-stranded RNA poly(I:C) combined with mucosal vaccine protects against influenza virus infection. J. Virol. 79:2910–2919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mizuno D, Ide-Kurihara M, Ichinomiya T, Kubo I, Kido H. 2006. Modified pulmonary surfactant is a potent adjuvant that stimulates the mucosal IgA production in response to the influenza virus antigen. J. Immunol. 176:1122–1130 [DOI] [PubMed] [Google Scholar]
- 21. Okamoto S, Matsuura M, Akagi T, Akashi M, Tanimoto T, Ishikawa T, Takahashi M, Yamanishi K, Mori Y. 2009. Poly(gamma-glutamic acid) nano-particles combined with mucosal influenza virus hemagglutinin vaccine protects against influenza virus infection in mice. Vaccine 27:5896–5905 [DOI] [PubMed] [Google Scholar]
- 22. Tamura S, Hasegawa H, Kurata T. 2010. Estimation of the effective doses of nasal-inactivated influenza vaccine in humans from mouse-model experiments. Jpn. J. Infect. Dis. 63:8–15 [PubMed] [Google Scholar]
- 23. Tamura SI, Samegai Y, Kurata H, Kikuta K, Nagamine T, Aizawa C, Kurata T. 1989. Enhancement of protective antibody responses by cholera toxin B subunit inoculated intranasally with influenza vaccine. Vaccine 7:257–262 [DOI] [PubMed] [Google Scholar]
- 24. Okamoto S, Matsuoka S, Takenaka N, Haredy AM, Tanimoto T, Gomi Y, Ishikawa T, Akagi T, Akashi M, Okuno Y, Mori Y, Yamanishi K. 2012. Intranasal immunization with a formalin-inactivated human influenza A virus whole-virion vaccine alone and intranasal immunization with a split-virion vaccine with mucosal adjuvants show similar levels of cross-protection. Clin. Vaccine Immunol. 19:979–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Takada A, Matsushita S, Ninomiya A, Kawaoka Y, Kida H. 2003. Intranasal immunization with formalin-inactivated virus vaccine induces a broad spectrum of heterosubtypic immunity against influenza A virus infection in mice. Vaccine 21:3212–3218 [DOI] [PubMed] [Google Scholar]
- 26. Yamada H, Moriishi E, Haredy AM, Takenaka N, Mori Y, Yamanishi K, Okamoto S. 2012. Influenza virus neuraminidase contributes to the dextran sulfate-dependent suppressive replication of some influenza A virus strains. Antiviral Res. 96:344–352 [DOI] [PubMed] [Google Scholar]
- 27. Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275–2289 [DOI] [PubMed] [Google Scholar]
- 28. Okamoto S, Yoshii H, Akagi T, Akashi M, Ishikawa T, Okuno Y, Takahashi M, Yamanishi K, Mori Y. 2007. Influenza hemagglutinin vaccine with poly(gamma-glutamic acid) nanoparticles enhances the protection against influenza virus infection through both humoral and cell-mediated immunity. Vaccine 25:8270–8278 [DOI] [PubMed] [Google Scholar]
- 29. de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, Qui PT, Cam BV, Ha do Q, Guan Y, Peiris JS, Chinh NT, Hien TT, Farrar J. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Thanh TT, van Doorn HR, de Jong MD. 2008. Human H5N1 influenza: current insight into pathogenesis. Int. J. Biochem. Cell Biol. 40:2671–2674 [DOI] [PubMed] [Google Scholar]
- 31. James JM, Zeiger RS, Lester MR, Fasano MB, Gern JE, Mansfield LE, Schwartz HJ, Sampson HA, Windom HH, Machtinger SB, Lensing S. 1998. Safe administration of influenza vaccine to patients with egg allergy. J. Pediatr. 133:624–628 [DOI] [PubMed] [Google Scholar]
- 32. Katz JM, Webster RG. 1992. Amino acid sequence identity between the HA1 of influenza A (H3N2) viruses grown in mammalian and primary chick kidney cells. J. Gen. Virol. 73:1159–1165 [DOI] [PubMed] [Google Scholar]
- 33. Minor PD. 2010. Vaccines against seasonal and pandemic influenza and the implications of changes in substrates for virus production. Clin. Infect. Dis. 50:560–565 [DOI] [PubMed] [Google Scholar]
- 34. Minor PD, Engelhardt OG, Wood JM, Robertson JS, Blayer S, Colegate T, Fabry L, Heldens JG, Kino Y, Kistner O, Kompier R, Makizumi K, Medema J, Mimori S, Ryan D, Schwartz R, Smith JS, Sugawara K, Trusheim H, Tsai TF, Krause R. 2009. Current challenges in implementing cell-derived influenza vaccines: implications for production and regulation, July 2007, NIBSC, Potters Bar, UK. Vaccine 27:2907–2913 [DOI] [PubMed] [Google Scholar]
- 35. Organ WH. 1995. Cell culture as a substrate for the production of influenza vaccines: memorandum from a WHO meeting. Bull. World Health Organ. 73:431–435 [PMC free article] [PubMed] [Google Scholar]
- 36. Neumann G, Kawaoka Y. 2006. Host range restriction and pathogenicity in the context of influenza pandemic. Emerg. Infect. Dis. 12:881–886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bogs J, Kalthoff D, Veits J, Pavlova S, Schwemmle M, Manz B, Mettenleiter TC, Stech J. 2011. Reversion of PB2-627E to -627K during replication of an H5N1 clade 2.2 virus in mammalian hosts depends on the origin of the nucleoprotein. J. Virol. 85:10691–10698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hatta M, Gao P, Halfmann P, Kawaoka Y. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293:1840–1842 [DOI] [PubMed] [Google Scholar]
- 39. Li Y, Shi J, Zhong G, Deng G, Tian G, Ge J, Zeng X, Song J, Zhao D, Liu L, Jiang Y, Guan Y, Bu Z, Chen H. 2010. Continued evolution of H5N1 influenza viruses in wild birds, domestic poultry, and humans in China from 2004 to 2009. J. Virol. 84:8389–8397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Maines TR, Lu XH, Erb SM, Edwards L, Guarner J, Greer PW, Nguyen DC, Szretter KJ, Chen LM, Thawatsupha P, Chittaganpitch M, Waicharoen S, Nguyen DT, Nguyen T, Nguyen HH, Kim JH, Hoang LT, Kang C, Phuong LS, Lim W, Zaki S, Donis RO, Cox NJ, Katz JM, Tumpey TM. 2005. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J. Virol. 79:11788–11800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Murakami S, Horimoto T, Mai le Q, Nidom CA, Chen H, Muramoto Y, Yamada S, Iwasa A, Iwatsuki-Horimoto K, Shimojima M, Iwata A, Kawaoka Y. 2008. Growth determinants for H5N1 influenza vaccine seed viruses in MDCK cells. J. Virol. 82:10502–10509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schat KA, Bingham J, Butler JM, Chen LM, Lowther S, Crowley TM, Moore RJ, Donis RO, Lowenthal JW. 2012. Role of position 627 of PB2 and the multibasic cleavage site of the hemagglutinin in the virulence of H5N1 avian influenza virus in chickens and ducks. PLoS One 7:e30960. 10.1371/journal.pone.0030960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kashima Y, Ikeda M, Itoh Y, Sakoda Y, Nagata T, Miyake T, Soda K, Ozaki H, Nakayama M, Shibuya H, Okamatsu M, Ishigaki H, Ishida H, Sawai T, Kawaoka Y, Kida H, Ogasawara K. 2009. Intranasal administration of a live non-pathogenic avian H5N1 influenza virus from a virus library confers protective immunity against H5N1 highly pathogenic avian influenza virus infection in mice: comparison of formulations and administration routes of vaccines. Vaccine 27:7402–7408 [DOI] [PubMed] [Google Scholar]
- 44. Furuya Y, Chan J, Regner M, Lobigs M, Koskinen A, Kok T, Manavis J, Li P, Mullbacher A, Alsharifi M. 2010. Cytotoxic T cells are the predominant players providing cross-protective immunity induced by γ-irradiated influenza A viruses. J. Virol. 84:4212–4221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Furuya Y, Regner M, Lobigs M, Koskinen A, Mullbacher A, Alsharifi M. 2010. Effect of inactivation method on the cross-protective immunity induced by whole ‘killed’ influenza A viruses and commercial vaccine preparations. J. Gen. Virol. 91:1450–1460 [DOI] [PubMed] [Google Scholar]
- 46. Sawai T, Itoh Y, Ozaki H, Isoda N, Okamoto K, Kashima Y, Kawaoka Y, Takeuchi Y, Kida H, Ogasawara K. 2008. Induction of cytotoxic T-lymphocyte and antibody responses against highly pathogenic avian influenza virus infection in mice by inoculation of apathogenic H5N1 influenza virus particles inactivated with formalin. Immunology 124:155–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Budimir N, Huckriede A, Meijerhof T, Boon L, Gostick E, Price DA, Wilschut J, de Haan A. 2012. Induction of heterosubtypic cross-protection against influenza by a whole inactivated virus vaccine: the role of viral membrane fusion activity. PLoS One 7:e30898. 10.1371/journal.pone.0030898 [DOI] [PMC free article] [PubMed] [Google Scholar]