Abstract
Intraventricular hemorrhage with congenital cytomegalovirus (CMV) infection is rare and has been reported only in extremely premature infants or in association with thrombocytopenia. We report the first case of a full-term male infant with congenital CMV infection and intraventricular hemorrhage with a normal platelet count and coagulation profile. The infant also had a left subependymal cyst and bilateral occipital cysts without any other manifestations of CMV infection.
CASE REPORT
The mother of our patient was a 31-year-old woman (gravida 2, para 1) who was rubella and varicella immune, and all of her other serologic findings were negative. The parents were nonconsanguineous, and there was no family history of any bleeding disorder. Ultrasound examinations done at 12, 19, and 30 weeks of gestation showed normal fetal anatomy with a fetus appropriate for its gestational age.
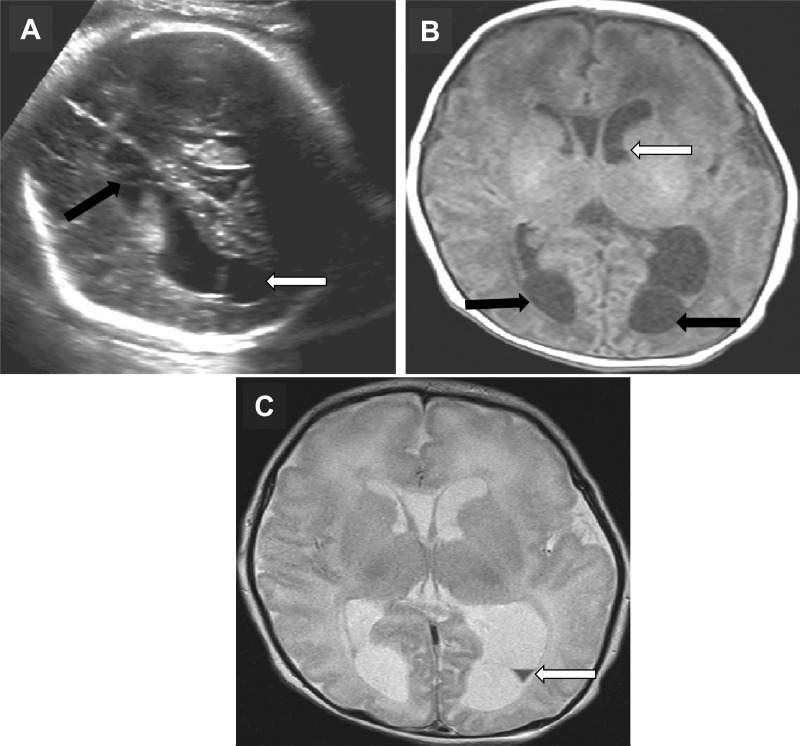
The pregnancy was uneventful until 38 weeks of gestation, when the mother felt that fetal movement had decreased. An ultrasound examination revealed asymmetric intracranial ventriculomegaly with the left lateral ventricle larger than the right and strands visible across both ventricles. The occipital horn of the right ventricle was also dilated, and there was echogenicity of the left choroid plexus suggestive of a blood clot (Fig. 1A). Fetal biometry was appropriate for the gestational age, the amniotic fluid index was normal, and the biophysical profile was 8/8.
Fig 1.
(A) Antenatal ultrasound at 38 weeks of gestation. Dilation of the occipital horn of both lateral ventricles, with the left lateral ventricle larger than the right (white arrow), is shown. Strands are visible in the ventricle. An echogenic left choroid and an adjacent inhomogeneous area suggestive of a blood clot (black arrow) are also visible. (B) Axial T1 MRI showing well-septated bilateral posterior occipital cysts (black arrows), a subependymal cyst anterior to the left caudothalamic groove (white arrow), and asymmetry of the anterior horns of the lateral ventricle. (C) Axial T2 MRI showing a collection of blood in the dependent area of the left lateral ventricle (white arrow) separated from the occipital cyst by a thin limiting membrane.
As an intraventricular hemorrhage was suspected, delivery was by cesarean section at 39 weeks of gestation with Apgar scores of 9 and 9 at 1 and 5 min, respectively. His birth weight was 2,790 g, his head circumference was 34 cm, and his length was 48 cm, all of which were appropriate for his gestational age. Except for mild hypotonia, the infant was normal upon examination.
Magnetic resonance imaging (MRI) done on day 2 of life showed a moderately dilated left lateral ventricle with a subependymal cyst at the left foramen of Munro extending along the caudothalamic notch, consistent with a previous intraventricular hemorrhage. There were bilateral occipital cysts compressing the occipital horns with a thin intervening septation (Fig. 1B). A small-volume intraventricular hemorrhage was visible in the dependent portion of the left lateral ventricle (Fig. 1C). Myelination was appropriate for a term infant, and magnetic resonance spectroscopy was noncontributory.
Given his history and neuroimaging findings, the infant was investigated for a bleeding disorder and bacterial and viral infections. Complete blood counts showed a platelet count of 190 × 109/liter (normal range, 150 × 109 to 400 × 109/liter) with normal hemoglobin and white cell counts. The partial thromboplastin time was 46.6 s, and the international normalized ratio was 1.4, both of which were within the normal range for a term infant. Bacterial cultures and tests for parvovirus B19-specific IgM and IgG and toxoplasma-specific IgM and IgG were negative. Both the rapid plasma reagin assay and a line immunoassay (Innogenetics, Ghent, Belgium) for syphilis were negative. Liver function test results were normal. The infant's cerebrospinal fluid (CSF) was negative for bacteria, herpes simplex viruses 1 and 2, enteroviruses, and varicella virus. Although a cytomegalovirus (CMV)-specific IgM test result was indeterminate, a CSF PCR assay and a urine culture done on the second day of life were positive for CMV. On ophthalmological examination, there was no evidence of chorioretinitis, and a hearing test result was normal. The infant was not treated for CMV, as there was no evidence of viral sepsis, hepatitis, pneumonitis, thrombocytopenia, chorioretinitis, or sensorineural deafness. By 1 week of age, the infant's tone had normalized, his head circumference was stable, and he was feeding normally. He was discharged home with neurologic, audiologic, and ophthalmologic follow-up.
CMV, a ubiquitous double-stranded DNA virus belonging to the herpesvirus family, is the most common cause of congenital infection, with a prevalence rate of 0.2 to 2.5% in all live newborns (1). In Canada, the reported prevalence rate is 0.4 to 1.7% (2). The fetus is infected by viral transmission via the placenta following an episode of viremia in the mother (1). Uncommonly, intrauterine infection can also take place by an ascending route through infected cervical secretions following rupture of fetal membranes (1). However, only 10% of infants with congenital infection are symptomatic at birth and can present with a myriad of clinical findings (1). Among these, central nervous system manifestations are prominent, with sensorineural deafness being the most common, but hypotonia, seizures, microcephaly, ventriculomegaly, intracranial calcifications, cerebellar and hippocampal hypoplasia, and cortical dysplasias such as pachygyria, polymicrogyria, and lissencephaly may also occur (1, 3–5). Intraventricular hemorrhage is rare with congenital CMV infection and has been reported either in very premature infants or in association with thrombocytopenia (6–8). McDonald et al. reported congenital CMV infection and intraventricular hemorrhage in a term female infant who also had severe thrombocytopenia (8). Nigro et al. reported a woman with primary CMV infection who underwent medical termination of pregnancy at 20 weeks of gestation with the fetus having dilation of the right occipital horn with a large left cerebral hemorrhage (6). Moinuddin et al. reported an infant at 35 weeks of gestation with congenital CMV who was diagnosed as having right parietal and temporal hemorrhages with ventriculomegaly on an antenatal MRI at 31 weeks of gestation (7). That infant was thrombocytopenic at birth. In their series of 11 patients with congenital CMV and brain abnormalities, Barkovich and Lindan described one infant with intraventricular hemorrhage (5). However, the gestational age and platelet counts are not reported. In the series by de Vries et al., one infant at 34 weeks of gestation had intraventricular hemorrhage and intraparenchymal hemorrhage but with severe thrombocytopenia (9). Unlike these previously reported cases, our patient was a term infant with congenital CMV infection and a normal platelet count who had both antenatal and postnatal evidence of intraventricular hemorrhage on neuroimaging. The other significant finding in our case was the presence of a left-side subependymal cyst and bilateral cysts adjacent to the occipital horns of the lateral ventricles. While subependymal cysts are well described in congenital CMV infections, occipital cysts are relatively uncommon but have been reported by other investigators (4, 5, 7, 9–11). In addition, the presence of multiple cysts in the absence of any other manifestations of CMV infection is also unusual (3, 9).
The mechanism of brain injury in congenital CMV is varied. Some investigators consider the virus to be neurotropic, causing direct injury to neurons, especially if the infection occurs early in gestation, when the germinal matrix is developing, resulting in cortical dysplasias and hypoplasia of the hippocampus and cerebellum (5). CMV, however, can also infect endothelial cells, causing a vasculitis that can also affect blood vessels of the central nervous system. This can manifest itself as thrombosis or hemorrhage in the absence of thrombocytopenia or as a coagulopathy (6, 12, 13). Intracranial and gastrointestinal hemorrhages with CMV infection in adults have been reported in the literature (13). A vasculitis may have been responsible for the intraventricular hemorrhage seen in our patient. The cause of periventricular cysts in congenital CMV infection is also poorly understood (7). Some investigators consider them to be secondary to a direct cytopathic effect of the virus, while others consider them to be due to intracerebral thrombosis or hemorrhage secondary to vasculitis (5, 7). The occipital cysts in our patient likely represent porencephalic pseudocysts secondary to ischemia or hemorrhage, as an antenatal ultrasound examination at 30 weeks did not show any evidence of cysts (7).
It is difficult to say at what gestational age the infant in our case became infected with CMV. The mother did not report any symptoms associated with CMV infection during pregnancy, such as fever, pharyngitis, fatigue, or myalgias. However, less than 25% of pregnant women with CMV infection report any symptoms suggestive of CMV infection (14). In addition, although the rate of transmission to the fetus is higher in primary infections, it is not possible to say whether the mother in our case had a primary or a recurrent infection, as serological testing for CMV during pregnancy is not part of regular antenatal care in North America (1, 14). It is likely, however, that infection occurred in the second trimester or later. Infections early in pregnancy are associated with cortical malformations and cerebellar hypoplasia, which were absent from our patient on MRI (4, 5).
In summary, to our knowledge, this is the first reported case of a term neonate with congenital CMV infection and intraventricular hemorrhage associated with a normal platelet count and coagulation profile. In addition, the infant had a subependymal cyst and bilateral porencephalic pseudocysts adjacent to the occipital horns of the lateral ventricles. Importantly, other than mild hypotonia, there was no evidence of systemic involvement, despite the infant's severe brain abnormalities. Intraventricular hemorrhage occurs in 3.5% of all term infants, sometimes without any obvious cause. As CMV infects 40,000 infants every year, it may be important to screen term infants who have intraventricular hemorrhage without a definite cause for congenital CMV infection (8). Importantly, the presence of multiple periventricular cysts should prompt investigations for congenital CMV infection even in the absence of any other disease manifestations.
ACKNOWLEDGMENT
We have no conflict of interest to declare.
Footnotes
Published ahead of print 15 May 2013
REFERENCES
- 1. Malm G, Engman ML. 2007. Congenital cytomegalovirus infections. Semin. Fetal Neonatal Med. 12(3):154–159 [DOI] [PubMed] [Google Scholar]
- 2. Vaudry W, Rosychuk RJ, Lee BE, Cheung PY, Pang X, Preiksaitis JK. 2010. Congenital cytomegalovirus infection in high-risk Canadian infants: report of a pilot screening study. Can. J. Infect. Dis. Med. Microbiol. 21:e12–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dogan Y, Yuksel A, Kalelioglu IH, Has R, Tatli B, Yildirim A. 2011. Intracranial ultrasound abnormalities and fetal cytomegalovirus infection: report of 8 cases and review of the literature. Fetal Diagn. Ther. 30:141–149 [DOI] [PubMed] [Google Scholar]
- 4. Manara R, Balao L, Baracchini C, Drigo P, D'Elia R, Ruga EM. 2011. Brain magnetic resonance findings in symptomatic congenital cytomegalovirus infection. Pediatr. Radiol. 41:962–970 [DOI] [PubMed] [Google Scholar]
- 5. Barkovich AJ, Lindan CE. 1994. Congenital cytomegalovirus infection of the brain: imaging analysis and embryologic considerations. AJNR Am. J. Neuroradiol. 15:703–715 [PMC free article] [PubMed] [Google Scholar]
- 6. Nigro G, La Torre R, Sali E, Auteri M, Mazzocco M, Maranghi L, Cosmi E. 2002. Intraventricular haemorrhage in a fetus with cerebral cytomegalovirus infection. Prenat. Diagn. 22:558–561 [DOI] [PubMed] [Google Scholar]
- 7. Moinuddin A, McKinstry RC, Martin KA, Neil JJ. 2003. Intracranial hemorrhage progressing to porencephaly as a result of congenitally acquired cytomegalovirus infection—an illustrative report. Prenat. Diagn. 23:797–800 [DOI] [PubMed] [Google Scholar]
- 8. McDonald JM, Raghuveer TS, D'Alessandro MP. 2001. Can congenital CMV infection lead to intracranial hemorrhage? J. Perinatol 21:402–404 [DOI] [PubMed] [Google Scholar]
- 9. de Vries LS, Gunardi H, Barth PG, Bok LA, Verboon-Maciolek MA, Groenendaal F. 2004. The spectrum of cranial ultrasound and magnetic resonance imaging abnormalities in congenital cytomegalovirus infection. Neuropediatrics 35:113–119 [DOI] [PubMed] [Google Scholar]
- 10. Boesch C, Issakainen J, Kewitz G, Kikinis R, Martin E, Boltshauser E. 1989. Magnetic resonance imaging of the brain in congenital cytomegalovirus infection. Pediatr. Radiol. 19:91–93 [DOI] [PubMed] [Google Scholar]
- 11. Malinger G, Lev D, Zahalka N, Ben Aroia Z, Watemberg N, Kidron D, Sira LB, Lerman-Sagie T. 2003. Fetal cytomegalovirus infection of the brain: the spectrum of sonographic findings. AJNR Am. J. Neuroradiol. 24:28–32 [PMC free article] [PubMed] [Google Scholar]
- 12. Persoons MCJ, Stals FS, Van dam Mieras MCE, Bruggeman CA. 1998. Multiple organ involvement during experimental cytomegalovirus infection is associated with disseminated vascular pathology. J. Pathol. 184:103–109 [DOI] [PubMed] [Google Scholar]
- 13. Golden MP, Hammer SM, Wanke CA, Albrecht MA. 1994. Cytomegalovirus vasculitis: case reports and review of the literature. Medicine 73:246–255 [PubMed] [Google Scholar]
- 14. Nigro G, Adler SP. 2011. Cytomegalovirus infections during pregnancy. Curr. Opin. Obstet. Gynecol. 23:123–128 [DOI] [PubMed] [Google Scholar]