Abstract
We evaluated the ability of four commercial MIC testing systems (MicroScan, Vitek 2, Phoenix, and Etest) to detect vancomycin MIC values of ≤1 to ≥2 in 200 methicillin-resistant Staphylococcus aureus (MRSA) strains compared to the Clinical and Laboratory Standards Institute broth microdilution (BMD) reference methods. Compared to the BMD method, absolute agreement (0 ± dilution) was highest for the Phoenix system (66.2%) and the MicroScan turbidity method (61.8%), followed by the Vitek 2 system (54.3%). The Etest produced MIC values 1 to 2 dilutions higher than those produced by the BMD method (36.7% agreement). Of interest, the MicroScan system (prompt method) was more likely to overcall an MIC value of 1 mg/liter (74.1%), whereas the Phoenix (76%) and Vitek 2 (20%) systems had a tendency to undercall an MIC of 2 mg/liter. The ability to correctly identify vancomycin MIC values of 1 and 2 has clinical implications and requires further evaluation.
INTRODUCTION
The overall prevalence of methicillin-resistant Staphylococcus aureus (MRSA) continues to increase, with vancomycin (VAN) remaining the mainstay of therapy for serious infections (1–3). Over the last several years, there have been a number of studies that have demonstrated an association between vancomycin MICs of 1.5 or 2 mg/liter and failure of vancomycin therapy, even though these values lie within the Clinical and Laboratory Standards Institute's (CLSI's) and the FDA's acceptable vancomycin susceptibility range (≤2 mg/liter). The majority of these reports were derived from patients with MRSA-complicated bacteremia in whom a vancomycin MIC of 1.5 or 2 mg/liter was associated with persistent signs and symptoms of infection, including prolonged days of bacteremia, increased complications, increased lengths of hospital stay, and mortality (4–9). A recent observational study of 532 patients with MRSA and methicillin-susceptible Staphylococcus aureus (MSSA) bacteremia noted a significantly higher 30-day mortality rate associated with patients who had an isolate for which the MIC exceeded 1.5 mg/liter (by Etest methods). Of interest, this association did not seem to be related to vancomycin treatment, since patients who had MSSA bacteremia with an elevated vancomycin MIC and were treated with flucloxacillin had worse clinical outcomes than flucloxacillin-treated patients with MSSA bacteremia that had a lower vancomycin MIC value (P = 0.012) (10). In addition, a recent systematic review and meta-analysis of the literature regarding the relationship of vancomycin susceptibility and patient outcome concluded that vancomycin MIC values of 1.5 or 2 mg/liter were associated with greater treatment failure and mortality rates in patients with MRSA infections (11). Patients who have serious high-inoculum infections (i.e., infective endocarditis, medical device infections, etc.) with MRSA and for which the strain has been identified as heteroresistant vancomycin-intermediate S. aureus (hVISA) are also more likely to experience prolonged days of bacteremia, increased complications, multiple drug resistance, and relapse or recurrence of infection than those patients with susceptible strains (12–18). It has been demonstrated that some percentage of hVISA infections exist within the vancomycin susceptibility range and that the prevalence of these strains increases as the MIC reaches up to the breakpoint of 2 mg/liter (19–21). Taken together, these results suggest that in patients with serious, complicated, high-inoculum infections treated with vancomycin, the likelihood of treatment failure is greater when the S. aureus isolates demonstrate an MIC that exceeds 1 mg/liter.
The patient's exposure to vancomycin relative to the susceptibility of the organism to vancomycin is also a predictor of patient outcome. Based on in vitro, animal, and clinical data, it has been suggested that a specific vancomycin pharmacokinetic and pharmacodynamics (PK/PD) 24-hour area under the curve (AUC24)/MIC ratio target of ≥400 should be obtained in order to improve the outcomes of patients with severe staphylococcal infections, such as complicated bacteremia (3, 8). However, when the MIC is 2 mg/liter, obtaining this ratio is highly unlikely without exceeding vancomycin doses that would cause serious adverse events (22–24). Of interest, the inability to achieve this vancomycin PK/PD target when the MIC is 2 mg/liter is specifically mentioned in the recent vancomycin consensus guidelines and the Infectious Disease Society of America (IDSA) MRSA guidelines (25). Although the patient's clinical response to vancomycin therapy should be the primary consideration irrespective of the vancomycin MIC value, there has been increasing importance placed on vancomycin susceptibility for clinical decision making, especially when the patient's condition is worsening or not responding to therapy (3, 25–27).
Most investigations that evaluated the precision of automated susceptibility testing for vancomycin versus verified referenced MIC values used the essential agreement method (the MIC ± 1 log2 dilution). Based on the results of these studies, investigators have concluded that there are no major differences between automated systems for determining the vancomycin MIC value (28, 29).
However, several recent reports pointed out discrepancies in the ability of automated susceptibility testing methods to determine the vancomycin MIC for MRSA compared to the ability of the Etest or standard broth microdilution (BMD) methods (30, 31, 32). Based on the MRSA and vancomycin dosing and monitoring guidelines' emphasis on the importance of vancomycin susceptibility for clinical decision making, it is important to know the precision of automated MIC testing (3, 25). Therefore, our objective was to compare the ability of the currently available commercial automated BMD susceptibility testing methods (Vitek 2, MicroScan, and BD Phoenix) to identify vancomycin MIC values compared to standard reference BMD and Etest methods for MRSA.
MATERIALS AND METHODS
A collection of 200 clinical MRSA blood isolates was selected from an 1,800-isolate collection from nine U.S. medical centers (one from each consensus region) collected between 2002 and 2006, and 10 control strains with an MIC range of 0.25 to 8 mg/liter were utilized (33). Vancomycin MIC values were determined in two separate laboratories, in duplicate, using reference broth microdilution (frozen-form panels) and Etest methods. Frozen panels were prepared with 36 precise incremental dilutions ranging from 64 to 0.06 mg/liter, thus mimicking the Etest strip scale for comparison purposes. The CLSI standards for microdilution methods were followed throughout with quality control strains within published guidelines (34). Vancomycin susceptibility was determined with the Etest according to the manufacturer's instructions (bioMérieux, Durham, NC). A consensus MIC value was established for vancomycin using MIC values provided by the two reference laboratories. For example, for a 0.5-doubling-dilution difference, the higher MIC value was selected. If an MIC differed by a 1-dilution difference, the median value was selected as the consensus MIC. Meanwhile, the 10 control strains and 200 challenge strains were sent to the three outside clinical laboratories to determine the vancomycin MIC values by the three different automated testing systems. These included the BD Phoenix automated microbiology system (Franklin Lakes, NJ), the panel type PMIC/ID-107, the MicroScan WalkAway (Dade Behring, Deerfield, IL), the PC33 and the Vitek 2 (bioMérieux, Hazelwood, MO), and the AST-GP70. In order to evaluate the performance of the various automated BMD methods, the incremental reference scale MIC values were converted to the CLSI-referenced log2-based microdilutions. The Etest method results were compared to those of the incremental reference microdilution using the exact-dilution scale and with the MIC rounded up to the next dilution. The differences between the automated systems and the reference BMD method were calculated by the essential agreement method (MIC = 0 ± dilution and ± 1 log2 dilution), as previously described (35).
RESULTS
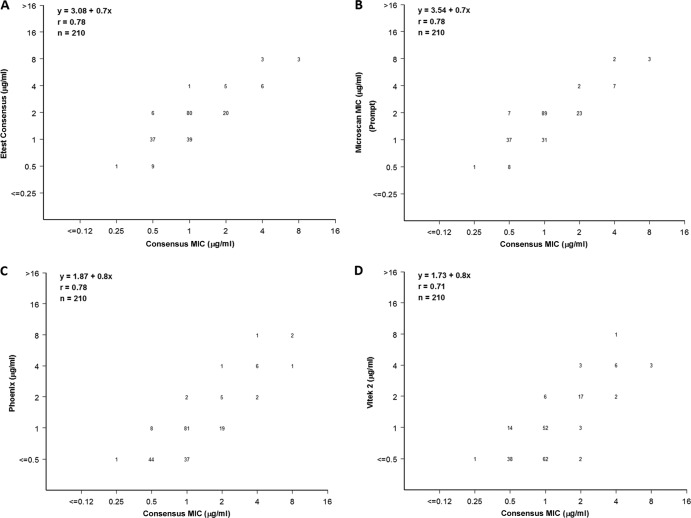
The reference laboratory consensus vancomycin MICs for the BMD and Etest methods ranged from 0.25 to 6 and 0.5 to 8 mg/liter, respectively. Comparing the MIC results between the two reference laboratories, out of the 210 strains evaluated, there were 9 (4.2%) strains that differed by ±1 log2 dilution, there was 1 strain (0.4%) that differed by 2 log2 dilutions, and there were no strains that differed by >2 log2 dilutions, resulting in very few instances where the consensus rule had to be applied. Overall, the Etest results tended to be higher than those of the broth microdilution values by 1 to 2 log2 dilutions for the two reference laboratories. The overall results for the BMD reference method, the Etest, and the commercial automated susceptibility testing methods are listed in Table 1. The results are presented as the log2 dilution variation from the reference BMD. Figure 1 shows scattergram plots of each method compared to the reference consensus vancomycin MIC. The MicroScan system has two methods for organism plate inoculation. Both the prompt and turbidity method results are listed in Table 1. All the methods displayed some variation compared to the reference BMD method. Agreement (±0 log2 dilution) was the highest for the Phoenix (66.2%) and the MicroScan turbidity method (61.8%), followed by the Vitek 2 system at 54.3%. The lowest agreement noted was for the MicroScan prompt method at 34.3%, followed by the Etest at 36.7%. A one-dilution overcall was highest for the MicroScan prompt method (62.4%), followed by the Etest at 60% and the MicroScan turbidity method at 36.2%. The Vitek 2 and the Phoenix systems were more likely to undercall the vancomycin MIC by 1 dilution at 32.3 and 26.7%, respectively. Of note, using a ±1 log2 dilution agreement scale, all of the automated systems provided 100% agreement, except for the Vitek 2 (99%), the MicroScan (prompt method, 96.7%), and the Etest (96.7%).
Table 1.
Comparison of BMD with the automated systems and Etest MIC results
| Consensus log2 MICs per BMD method | Susceptibility testing system (no. tested) | No. (%) of isolates with a log2 dilution variationa (compared to the reference BMD) of: |
||||
|---|---|---|---|---|---|---|
| −2 | −1 | 0 | +1 | +2 | ||
| 0.25 < MIC < 8 | MicroScan prompt (210) | — | — | 72 (34.3) | 131 (62.4) | 7 (3.3) |
| MicroScan turbidity (207) | — | 4 (1.9) | 128 (61.8) | 75 (36.2) | — | |
| Phoenix (210) | — | 56 (26.7) | 139 (66.2) | 15 (7.1) | — | |
| Vitek 2 (210) | 2 (1.0) | 68 (32.3) | 114 (54.3) | 26 (12.4) | — | |
| Etest (210) | 77 (36.7) | 126 (60.0) | 7 (3.3) | |||
| MIC = 0.5 | MicroScan prompt (52) | — | — | 8 (15.4) | 37 (71.1) | 7 (13.5) |
| MicroScan turbidity (51) | — | — | 15 (29.4) | 36 (70.6) | — | |
| Phoenix (52) | — | — | 44 (84.6) | 8 (15.4) | — | |
| Vitek 2 (52) | — | — | 38 (73.1) | 14 (26.9) | — | |
| Etest (210) | — | 9 (17.3) | 37 (71.1) | 6 (11.6) | — | |
| MIC = 1 | MicroScan prompt (120) | — | — | 31 (25.8) | 89 (74.1) | — |
| MicroScan turbidity (118) | — | 1 (0.8) | 82 (69.5) | 35 (29.7) | — | |
| Phoenix (120) | — | 37 (30.8) | 81 (67.5) | 2 (1.7) | — | |
| Vitek 2 (120) | — | 63 (52.5) | 50 (41.7) | 7 (5.8) | — | |
| Etest (210) | — | 40 (33.3) | 79 (65.9) | 1 (0.8) | — | |
| MIC = 2 | MicroScan prompt (25) | — | — | 23 (92.0) | 2 (8.0) | — |
| MicroScan turbidity (25) | — | 3 (12.0) | 21 (84.0) | 1 (4.0) | — | |
| Phoenix (25) | — | 19 (76.0) | 5 (20.0) | 1 (4.0) | — | |
| Vitek 2 (25) | 2 (8.0) | 3 (12.0) | 17 (68.0) | 3 (12.0) | — | |
| Etest (25) | — | — | 20 (80.0) | 5 (20.0) | — | |
—, no value found at this dilution.
Fig 1.
Scattergrams of the correlation between vancomycin MICs obtained by the broth microdilution method performed with frozen panels and the Etest (A), the MicroScan (B), the Phoenix (C), and the Vitek 2 (D) systems.
When examining the specific MIC values of 0.5, 1, and 2 mg/liter (Table 1), the MicroScan prompt and turbidity methods tended to overcall the MIC of 0.5 mg/liter by 1 dilution at 71.1 and 70.6%, respectively. The Phoenix and Vitek 2 systems overcalled by 1 dilution at 15.4 and 26.9%, respectively. At the vancomycin MIC of 1 mg/liter, the MicroScan prompt and turbidity methods overcalled by 74.1 and 29.7%, respectively. However, the Phoenix and Vitek 2 systems had a tendency to undercall by 30.8 and 52.5%, respectively. The Etest was 1 dilution higher (11.6%) and 1 dilution lower (17.3%) at an MIC of 0.5 mg/liter and 1 dilution higher (0.8%) and 1 dilution lower (33.3%) at an MIC of 1 mg/liter.
There was a total of 25 isolates that the reference laboratories identified with a vancomycin MIC value of 2 mg/liter (Table 1). All 25 strains were further evaluated by a modified population analysis as described elsewhere for hVISA (19). There were 19 (76%) that were found to be hVISA among these stains. For these 25 strains, the ±0 log2 dilution agreement was the highest with the MicroScan prompt and turbidity methods (92 and 84%, respectively) followed by the Etest (80%). The MicroScan turbidity method, however, undercalled 3 strains (12%), and all of them were hVISA with the propensity to fail vancomycin therapy (18). In contrast, neither the Etest nor the MicroScan prompt method undercalled any of the strains with vancomycin MICs of 2 mg/liter (Fig. 1). The most alarming result regarding the identification of an organism with a vancomycin MIC value of 2 mg/liter, especially in hVISA, was observed with the Phoenix system, with a ±0 log2 agreement of 20% (5 strains), and 19 isolates were undercalled (76%), including 18 hVISA strains. Finally, the Vitek 2 system had a ±0 log2 agreement of 68% (17 strains), but 5 strains (20%) were undercalled by 1 or 2 log2 dilutions, all of them being hVISA.
DISCUSSION
In patients with serious S. aureus infections, such as pneumonia and complicated bacteremia, including infective endocarditis, a vancomycin MIC of >1 mg/liter has been associated with poor patient outcomes (11). Although a vancomycin MIC value of 2 mg/liter should not be the only deciding factor for whether to change the therapy to alternative agents, it is an important consideration when assessing a patient's response to vancomycin therapy. In the recent IDSA MRSA guidelines, the management of persistent vancomycin treatment failures in adult patients is thoroughly discussed. Although declaring a treatment failure is a complex issue, it is recommended that an alternative therapy to vancomycin be considered when patients are persistently bacteremic or have a worsening clinical condition despite adequate debridement and removal of infection foci or if the vancomycin MIC is 2 mg/liter, especially in critically ill patients (25). Therefore, the ability to determine the vancomycin MIC with some degree of precision is important to clinical decision making. In addition, it has been reported that the proportion of hVISA is higher for isolates demonstrating an MIC value of 2 mg/liter (19–21). Since hVISA is associated with poor patient outcomes, including persistent infections, the ability to distinguish between MICs of 1 and 2 mg/liter is exceedingly important (18, 36). Our results only highlight the risk of automated systems missing vancomycin MICs of 2 mg/liter, especially when hVISA is involved. The therapeutic outcome of such results might be serious considering that clinicians might not change therapies for isolates with a vancomycin MIC of 1 mg/liter, as reported by the automated system (even though the actual MIC value may be 2 mg/liter), thus putting the patient at risk for failure especially if hVISA is present (18).
As with previous evaluations of automated susceptibility testing, we found that the current Phoenix, MicroScan, and Vitek 2 systems are relatively close in precision for vancomycin susceptibility testing when derived MIC values are within ±1 dilution (28, 29). Swenson et al. determined the vancomycin susceptibility of 129 S. aureus isolates using 6 commercial methods (including the Phoenix, Vitek 2, MicroScan, and Etest systems) and BMD. Using an essential agreement method with an accuracy of ±1 log2 dilution, the results were reported as 98.4% for the Phoenix system and 100% for the three other methods (28). Similarly, Kruzel et al. determined the vancomycin susceptibility of 161 blood isolates (with MIC values of ≤1 mg/liter) by broth microdilution methods, using both in-house-prepared and commercially prepared microtiter panels, and via automated systems such as the BD Phoenix, the Vitek 2, and the MicroScan. Using the same essential agreement method, the Vitek 2 and MicroScan systems demonstrated 96.3% agreement, whereas the Phoenix system had only 88.8% agreement. Only the Etest method varied significantly at 76.4% agreement (29).
Given the importance of identifying MRSA isolates with vancomycin MIC values that exceed 1 mg/liter, it would seem that accepting MIC values of ±1 log2 dilution would not be in the clinician's best interest for treating patients with serious MRSA infections. It is of interest that in the literature (18), vancomycin Etest values of ≥1.5 mg/liter have consistently been reported to predict poor outcomes in patients with MRSA bacteremia. Although the Etest has been demonstrated to read slightly higher than BMD methods, it may be the best conservative alternative for evaluating MRSA vancomycin MICs in patients with serious and life-threatening infections.
ACKNOWLEDGMENTS
This study was not supported by any external sources.
M.J.R. has served on the speaker bureaus of and as a consultant for and received grant support from Cubist, Cerexa, Forest, Clinical Therapeutics, the NIH, Theravance, Novartis, and Cepheid. H.S. has received research funding from BioFire, Inc. JMI Laboratories, Inc., received research and educational grants in 2009 to 2012 from the American Proficiency Institute (API), Anacor, Astellas, AstraZeneca, Bayer, Cempra, Cerexa, ContraFect, Cubist, Daiichi, Dipexium, Enanta, Furiex, GlaxoSmithKline, Johnson & Johnson (Ortho McNeil), LegoChem Biosciences Inc., Meiji Seika Kaisha, Merck, Nabriva, Novartis, Pfizer (Wyeth), Rempex, Rib-X Pharmaceuticals, Seachaid, Shionogi, The Medicines Co., Theravance, ThermoFisher, and some other corporations. Some JMI employees are advisors/consultants for Astellas, Cubist, Pfizer, Cempra, Cerexa-Forest, Johnson & Johnson, and Theravance. With regard to other speaker bureaus and stock options, we have no conflicts to declare. C.V., L.E.B., and A.W. have nothing to declare.
Footnotes
Published ahead of print 17 April 2013
REFERENCES
- 1. Styers D, Sheehan DJ, Hogan P, Sahm DF. 2006. Laboratory-based surveillance of current antimicrobial resistance patterns and trends among Staphylococcus aureus: 2005 status in the United States. Ann. Clin. Microbiol. Antimicrob. 5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pillar CM, Draghi DC, Sheehan DJ, Sahm DF. 2008. Prevalence of multidrug-resistant, methicillin-resistant Staphylococcus aureus in the United States: findings of the stratified analysis of the 2004 to 2005 LEADER Surveillance Programs. Diagn. Microbiol. Infect. Dis. 60:221–224 [DOI] [PubMed] [Google Scholar]
- 3. Rybak M, Lomaestro B, Rotschafer JC, Moellering R, Jr, Craig W, Billeter M, Dalovisio JR, Levine DP. 2009. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am. J. Health Syst. Pharm. 66:82–98 [DOI] [PubMed] [Google Scholar]
- 4. Lodise TP, Graves J, Evans A, Graffunder E, Helmecke M, Lomaestro BM, Stellrecht K. 2008. Relationship between vancomycin MIC and failure among patients with methicillin-resistant Staphylococcus aureus bacteremia treated with vancomycin. Antimicrob. Agents Chemother. 52:3315–3320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lodise TP, Miller CD, Graves J, Evans A, Graffunder E, Helmecke M, Stellrecht K. 2008. Predictors of high vancomycin MIC values among patients with methicillin-resistant Staphylococcus aureus bacteraemia. J. Antimicrob. Chemother. 62:1138–1141 [DOI] [PubMed] [Google Scholar]
- 6. Sakoulas G, Moise-Broder PA, Schentag J, Forrest A, Moellering RC, Jr, Eliopoulos GM. 2004. Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J. Clin. Microbiol. 42:2398–2402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Soriano A, Marco F, Martinez JA, Pisos E, Almela M, Dimova VP, Alamo D, Ortega M, Lopez J, Mensa J. 2008. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin. Infect. Dis. 46:193–200 [DOI] [PubMed] [Google Scholar]
- 8. Kullar R, Davis SL, Levine DP, Rybak MJ. 2011. Impact of vancomycin exposure on outcomes in patients with methicillin-resistant Staphylococcus aureus bacteremia: support for consensus guidelines suggested targets. Clin. Infect. Dis. 52:975–981 [DOI] [PubMed] [Google Scholar]
- 9. Neuner EA, Casabar E, Reichley R, McKinnon PS. 2010. Clinical, microbiologic, and genetic determinants of persistent methicillin-resistant Staphylococcus aureus bacteremia. Diagn. Microbiol. Infect. Dis. 67:228–233 [DOI] [PubMed] [Google Scholar]
- 10. Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O'Sullivan MV, Anderson TL, Roberts SA, Gao W, Christiansen KJ, Coombs GW, Johnson PD, Howden BP. 2011. Antibiotic choice may not explain poorer outcomes in patients with Staphylococcus aureus bacteremia and high vancomycin minimum inhibitory concentrations. J. Infect. Dis. 204:340–347 [DOI] [PubMed] [Google Scholar]
- 11. van Hal SJ, Lodise TP, Paterson DL. 2012. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin. Infect. Dis. 54:755–771 [DOI] [PubMed] [Google Scholar]
- 12. Moore MR, Perdreau-Remington F, Chambers HF. 2003. Vancomycin treatment failure associated with heterogeneous vancomycin-intermediate Staphylococcus aureus in a patient with endocarditis and in the rabbit model of endocarditis. Antimicrob. Agents Chemother. 47:1262–1266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maor Y, Hagin M, Belausov N, Keller N, Ben-David D, Rahav G. 2009. Clinical features of heteroresistant vancomycin-intermediate Staphylococcus aureus bacteremia versus those of methicillin-resistant S. aureus bacteremia. J. Infect. Dis. 199:619–624 [DOI] [PubMed] [Google Scholar]
- 14. Howden BP, Johnson PD, Ward PB, Stinear TP, Davies JK. 2006. Isolates with low-level vancomycin resistance associated with persistent methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob. Agents Chemother. 50:3039–3047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Howden BP, Ward PB, Charles PG, Korman TM, Fuller A, du Cros P, Grabsch EA, Roberts SA, Robson J, Read K, Bak N, Hurley J, Johnson PD, Morris AJ, Mayall BC, Grayson ML. 2004. Treatment outcomes for serious infections caused by methicillin-resistant Staphylococcus aureus with reduced vancomycin susceptibility. Clin. Infect. Dis. 38:521–528 [DOI] [PubMed] [Google Scholar]
- 16. Bae IG, Federspiel JJ, Miro JM, Woods CW, Park L, Rybak MJ, Rude TH, Bradley S, Bukovski S, de la Maria CG, Kanj SS, Korman TM, Marco F, Murdoch DR, Plesiat P, Rodriguez-Creixems M, Reinbott P, Steed L, Tattevin P, Tripodi MF, Newton KL, Corey GR, Fowler VG., Jr 2009. Heterogeneous vancomycin-intermediate susceptibility phenotype in bloodstream methicillin-resistant Staphylococcus aureus isolates from an international cohort of patients with infective endocarditis: prevalence, genotype, and clinical significance. J. Infect. Dis. 200:1355–1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Medves J, Godfrey C, Turner C, Paterson M, Harrison M, MacKenzie L, Durando P. 2010. Systematic review of practice guideline dissemination and implementation strategies for healthcare teams and team-based practice. Int. J. Evid. Based Healthc. 8:79–89 [DOI] [PubMed] [Google Scholar]
- 18. van Hal SJ, Paterson DL. 2011. Systematic review and meta-analysis of the significance of heterogeneous vancomycin-intermediate Staphylococcus aureus isolates. Antimicrob. Agents Chemother. 55:405–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rybak MJ, Leonard SN, Rossi KL, Cheung CM, Sader HS, Jones RN. 2008. Characterization of vancomycin-heteroresistant Staphylococcus aureus from the metropolitan area of Detroit, Michigan, over a 22-year period (1986 to 2007). J. Clin. Microbiol. 46:2950–2954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tenover FC, Moellering RC., Jr 2007. The rationale for revising the Clinical and Laboratory Standards Institute vancomycin minimal inhibitory concentration interpretive criteria for Staphylococcus aureus. Clin. Infect. Dis. 44:1208–1215 [DOI] [PubMed] [Google Scholar]
- 21. Sader HS, Jones RN, Rossi KL, Rybak MJ. 2009. Occurrence of vancomycin-tolerant and heterogeneous vancomycin-intermediate strains (hVISA) among Staphylococcus aureus causing bloodstream infections in nine U. S. A. hospitals. J. Antimicrob. Chemother. 64:1024–1028 [DOI] [PubMed] [Google Scholar]
- 22. Patel N, Pai MP, Rodvold KA, Lomaestro B, Drusano GL, Lodise TP. 2011. Vancomycin: we can't get there from here. Clin. Infect. Dis. 52:969–974 [DOI] [PubMed] [Google Scholar]
- 23. Lodise TP, Lomaestro B, Graves J, Drusano GL. 2008. Larger vancomycin doses (at least four grams per day) are associated with an increased incidence of nephrotoxicity. Antimicrob. Agents Chemother. 52:1330–1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mohr JF, Murray BE. 2007. Point: vancomycin is not obsolete for the treatment of infection caused by methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 44:1536–1542 [DOI] [PubMed] [Google Scholar]
- 25. Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, M JR, Talan DA, Chambers HF. 2011. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin. Infect. Dis. 52:285–292 [DOI] [PubMed] [Google Scholar]
- 26. Lubin AS, Snydman DR, Ruthazer R, Bide P, Golan Y. 2011. Predicting high vancomycin minimum inhibitory concentration in methicillin-resistant Staphylococcus aureus bloodstream infections. Clin. Infect. Dis. 52:997–1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deresinski S. 2012. Methicillin-resistant Staphylococcus aureus and vancomycin: minimum inhibitory concentration matters. Clin. Infect. Dis. 54:772–774 [DOI] [PubMed] [Google Scholar]
- 28. Swenson JM, Anderson KF, Lonsway DR, Thompson A, McAllister SK, Limbago BM, Carey RB, Tenover FC, Patel JB. 2009. Accuracy of commercial and reference susceptibility testing methods for detecting vancomycin-intermediate Staphylococcus aureus. J. Clin. Microbiol. 47:2013–2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kruzel MC, Lewis CT, Welsh KJ, Lewis EM, Dundas NE, Mohr JF, Armitige LY, Wanger A. 2011. Determination of vancomycin and daptomycin MICs by different testing methods for methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 49:2272–2273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hsu DI, Hidayat LK, Quist R, Hindler J, Karlsson A, Yusof A, Wong-Beringer A. 2008. Comparison of method-specific vancomycin minimum inhibitory concentration values and their predictability for treatment outcome of meticillin-resistant Staphylococcus aureus (MRSA) infections. Int. J. Antimicrob. Agents. 32:378–385 [DOI] [PubMed] [Google Scholar]
- 31. Bland CM, Porr WH, Davis KA, Mansell KB. 2010. Vancomycin MIC susceptibility testing of methicillin-susceptible and methicillin-resistant Staphylococcus aureus isolates: a comparison between Etest(R) and an automated testing method. South Med. J. 103:1124–1128 [DOI] [PubMed] [Google Scholar]
- 32. Liu Y, Cao B, Gu L, Liu K, Feng Z. 2012. Successful control of vancomycin-resistant Enterococcus faecium nosocomial outbreak in a teaching hospital in China. Am. J. Infect. Control. 40:568–571 [DOI] [PubMed] [Google Scholar]
- 33. Sader HS, Fey PD, Limaye AP, Madinger N, Pankey G, Rahal J, Rybak MJ, Snydman DR, Steed LL, Waites K, Jones RN. 2009. Evaluation of vancomycin and daptomycin potency trends (MIC creep) against methicillin-resistant Staphylococcus aureus isolates collected in nine U.S. medical centers from 2002 to 2006. Antimicrob. Agents Chemother. 53:4127–4132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Clincial and Laboratory Standards Institute 2010. Performance standards for antimicrobial susceptibility testing; 16th informational supplement. CLSI M100-S20. Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 35. Baker CN, Tenover FC. 1996. Evaluation of Alamar colorimetric broth microdilution susceptibility testing method for staphylococci and enterococci. J. Clin. Microbiol. 34:2654–2659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, M JR, Talan DA, Chambers HF, Infectious Diseases Society of America 2011. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 52:e18–e55. 10.1093/cid/ciq146 [DOI] [PubMed] [Google Scholar]