Abstract
Test (a) whether a dissonance-based eating disorder prevention program that reduces thin-ideal internalization mitigates the effects of risk factors for eating disorder onset and (b) whether the risk factors moderate the effects of this intervention on risk for eating disorder onset, to place the effects of this intervention within the context of established risk factors. Female adolescents (N=481) with body image concerns were randomized to the dissonance-based program, healthy weight control program, expressive writing control condition, or assessment-only control condition. Denial of costs of pursuing the thin-ideal was the most potent risk factor for eating disorder onset during the 3-year follow-up (OR=5.0). The dissonance program mitigated the effect of this risk factor. For participants who did not deny costs of pursuing the thin-ideal, emotional eating and externalizing symptoms increased risk for eating disorder onset. Negative affect attenuated the effects of each of the active interventions in this trial. Results imply that this brief prevention program offsets the risk conveyed by the most potent risk factor for eating disorder onset in this sample, implicate three vulnerability pathways to eating pathology involving thin-ideal pursuit, emotional eating, and externalizing symptoms, and suggest that negative affect mitigates the effects of eating disorder prevention programs.
Keywords: Body dissatisfaction, Eating disorders, Prevention, Risk factors, Moderators
Over 10% of young women experience an eating disorder, which are marked by functional impairment, health problems, health service utilization, and increased risk for obesity, psychiatric comorbidity, suicide, and mortality (Crow et al. 2009; Stice et al. 2009a; Wilson et al. 2003). Thus, numerous eating disorder prevention programs have been developed.
Mounting support has emerged for a dissonance-based eating disorder prevention program, wherein young women with body image concerns critique the thin-ideal espoused for women in verbal, written, and behavioral exercises, which theoretically produces cognitive dissonance that causes participants to reduce their endorsement of the thin-ideal. Reduced thin-ideal internalization putatively decreases body dissatisfaction, unhealthy weight control efforts, negative affect, and ultimately eating disorder symptoms. An efficacy trial, in which young women with body dissatisfaction were randomized to the dissonance program, healthy weight control program, expressive writing control condition, or assessment-only control condition, found that relative to assessment-only controls, dissonance participants showed greater reductions in thin-ideal internalization, body dissatisfaction, dieting, negative affect, and eating disorder symptoms at posttest and 6-month follow-up, and in thin-ideal internalization, dieting, and symptoms at 1-year follow-up (Stice et al. 2006). Compared to expressive writing controls, dissonance participants showed greater reductions in thin-ideal internalization, body dissatisfaction, dieting, negative affect, and symptoms at posttest, in body dissatisfaction, dieting, negative affect, and symptoms at 6-month follow-up, and in dieting at 1-year follow-up. Relative to healthy weight participants, dissonance participants showed greater reductions in thin-ideal internalization, body dissatisfaction, dieting, negative affect, and symptoms at posttest and in negative affect at 6-month and 1-year follow-ups. Obesity onset through 1-year follow-up period was lower for dissonance (3%) and healthy weight participants (1%) relative to expressive writing (9%) and assessment-only (12%) controls. Relative to assessment-only controls and sometimes expressive writing controls, dissonance participants showed greater decreases in thin-ideal internalization, body dissatisfaction, negative affect, symptoms, and functional impairment at 2-year follow-up and greater decreases in body dissatisfaction, negative affect, and functional impairment at 3-year follow-up (Stice et al. 2008b). Dissonance participants showed greater reductions in functional impairment by 3-year follow-up than healthy weight participants. Dissonance participants showed lower threshold/subthreshold eating disorders onset over 3-year follow-up than assessment-only controls (6% vs. 15%). Positive effects for the dissonance program have generally replicated in efficacy trials conducted by other teams (e. g., Becker et al. 2005; Mitchell et al. 2007).
An effectiveness trial found that when high school clinicians recruit high-risk participants and deliver this prevention program, dissonance participants showed greater reductions in thin-ideal internalization, body dissatisfaction, self-reported dieting, and eating disorder symptoms relative to educational brochure controls, with the latter effect persisting through 3-year follow-up (Stice et al. 2009b, 2011b). This program has also reduced eating disorder risk factors and symptoms in dissemination studies wherein college students deliver the intervention (e.g., Becker et al. 2006, 2008; Perez et al. 2010).
In support of the intervention theory for this prevention program, reductions in thin-ideal internalization appear to mediate the effects of the intervention on the outcomes (Seidel et al. 2009; Stice et al. 2007, 2011a). In support of the thesis that dissonance contributes to intervention effects, participants assigned to high-dissonance versions of this program show greater reductions in eating disorder symptoms than those assigned to low-dissonance versions of this program (Green et al. 2005; McMillan et al. 2011).
Although these studies provide encouraging evidence for this program, research has not evaluated the effects of this intervention on eating disorder onset relative to the effects of established eating disorder risk factors. This is one useful way to contextualize the effects of prevention programs relative to the risk processes that occur in youth at risk for eating disorders. Thus, the first aim of this report was to test whether the dissonance program offsets the risk conveyed by known risk factors. To address this aim, we used data from our large efficacy trial (Stice et al. 2006). As the dissonance program focuses primarily on reducing thin-ideal internalization, it logically follows that this program might reduce the impact of thin-ideal internalization on risk for future eating disorder onset. We used classification tree analyses (CTA) to address this aim because it is well suited to identifying non-linear interactions in predicting dichotomous outcomes (Kraemer et al. 2002).
Another way to investigate the effects of the dissonance program relative to the effects of eating disorder risk factors that operate for at-risk youth is to test whether these risk factors moderate the effects of this intervention. Thus, the second aim of this report was to contextualize the effects of the dissonance prevention program by testing whether established risk factors moderate intervention effects on risk for eating disorder onset. A past report that examined moderators of the effects of this program on continuous outcomes found that the intervention produced larger reductions in eating disorder symptoms for individuals with greater baseline thin-ideal internalization, body image distress, readiness to improve body satisfaction, and eating disorder symptoms (Stice et al. 2008a). However, no study has examined factors that moderate the effect of the dissonance prevention program on risk for eating disorder onset. Elucidation of factors that mitigate the program effects may identify subgroups that do not benefit from this prevention program and guide the development of potentially effective alternative interventions. Further, discovering factors that amplify the effects of this program may identify subgroups that should be targeted in dissemination efforts. CTA is well suited for testing whether risk factors moderate the effects of the dissonance program on eating disorder onset because it can detect non-linear interactions between dichotomous and continuous factors in predicting a dichotomous outcome.
We investigated several baseline risk factors drawn from the dual pathway model of eating pathology (Stice 2001). This model posits that pressure to be thin from family, friends, and the media, elevated body mass, and internalization of the thin-ideal contribute to body dissatisfaction and body image distress (Fig. 1a & b). This body dissatisfaction putatively contributes to unhealthy dietary restriction, negative affect, and emotional eating, thereby increasing risk for eating disorder onset. Prospective studies have found that body mass, perceived pressure to be thin, thin-ideal internalization, appearance overvaluation, body dissatisfaction, body image distress, self-reported dieting, negative affect, and emotional eating increase risk for eating disorder symptom escalation (e.g., Jacobi et al. 2004; Stice 2002).
Fig. 1.
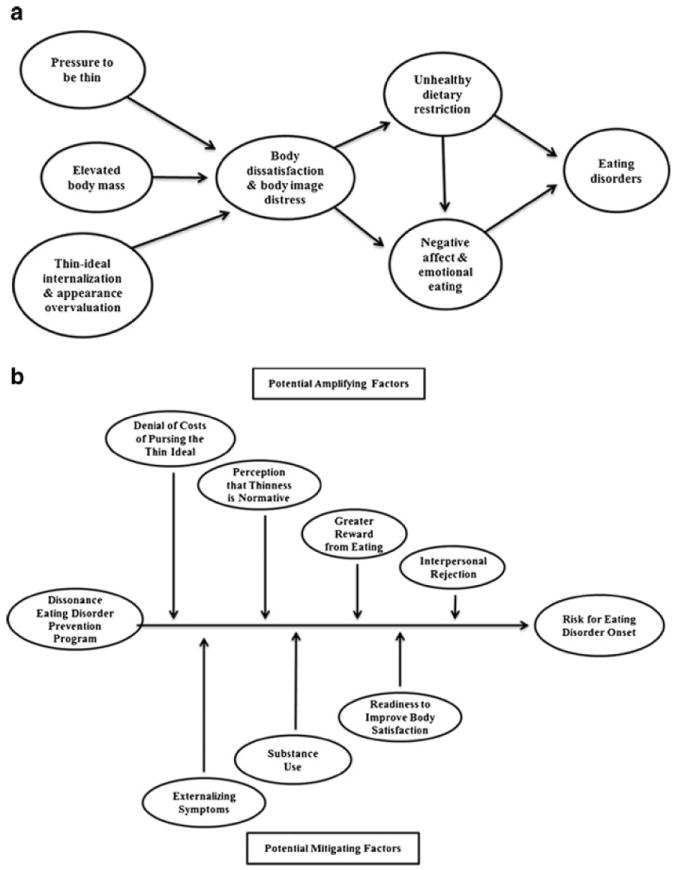
a Theoretical components of the dual-pathway model of eating pathology, b Moderators of intervention effects
We also investigated factors hypothesized to moderate program effects (Stice et al. 2008a). We theorized that denial of the costs of pursuing the thin-ideal and the perception that thinness is normative for women would attenuate intervention effects because these factors would render participants less likely to criticize the thin-ideal. Further, we theorized that greater subjective reward from eating and interpersonal rejection would mitigate intervention effects because they increase risk for eating disorder onset but are not directly targeted in the program. We also theorized that externalizing symptoms and substance use, which we consider proxy measures of impulsivity, increase risk for eating disorder onset, but are not directly addressed by the intervention and should therefore mitigate intervention effects. Finally, we hypothesized that readiness to improve body satisfaction should amplify intervention effects, as it should increase the odds that the participant engages fully in the intervention exercises.
Methods
Participants were 410 adolescent girls (M age =17.1, SD=1.6) with a mean body mass index (BMI=kg/m2) of 23.1 (SD= 4.2). The sample was 10% Asian/Pacific Islander, 5% Black, 19% Hispanic, 60% Caucasian, and 6% who specified other or mixed racial heritage. Highest reported parental education was 8% high school, 14% some college, 37% college graduate, and 41% advanced degree. The sample was fairly similar to adolescent girls from the Austin area enrolled in a large epidemiologic study (Stice et al. 2009a) in terms of BMI (M=22.8, SD=5.0), ethnicity (7% African American, 18% Hispanic, 65% Caucasian), and parental education (34% high school graduate or less; 25% some college; 26% college graduate; 15% graduate degree).
Participants were recruited from high schools and a university using direct mailings, fliers, and leaflets inviting females aged 14 and 19 to participate in a research project evaluating body acceptance interventions. Informed written consent was obtained from teens (and their parents if they were minors). For inclusion, students had to answer affirmatively when asked: “Do you have body image concerns?” during a phone screen. The sole exclusion criterion was meeting criteria for DSM-IV anorexia nervosa, bulimia nervosa, or binge eating disorder at baseline.
Participants were randomized to the dissonance intervention, healthy weight intervention, expressive-writing control intervention, or assessment-only control condition. The dissonance and healthy weight interventions consisted of three weekly 1-hour group sessions with 6–10 participants. Scripted treatment manuals were used. Advanced female graduate students served as the primary facilitators, with female undergraduate co-facilitators. The expressive writing condition, which consisted of three weekly 45-minute individual writing sessions, controlled for demand characteristics and expectancies, but not non-specific group factors.
Participants provided interview and survey data at pretest, posttest, and at 6-month, 1-year, 2-year, and 3-year follow-ups after posttest. Female assessors, blind to condition, attended 24 h of training. They had to demonstrate inter rater agreement (k>.80) with expert raters using 12 tape-recorded interviews. They also had to maintain inter rater kappa values of .80 or greater for a randomly selected 5% of the interviews that were re-conducted with independent assessors. Participants were paid for completing assessments. The local Institutional Review Board approved this project. Details regarding facilitator training and supervision, and participant flow are presented in Stice et al. (2008b).
Dissonance Intervention
Participants voluntarily engaged in verbal, written, and behavioral exercises in which they critiqued the thin-ideal during sessions and in homework activities. For example, they wrote an essay about the costs of pursuing the thin-ideal and engaged in a role-play in which they attempted to dissuade facilitators from pursuing the thin-ideal.
Healthy Weight Intervention
Participants were encouraged to make personalized small but lasting healthy changes to their diet and physical activity to achieve a healthier weight and improved body satisfaction. Motivational activities were used to promote behavior change.
Expressive Writing Control Intervention
Participants wrote about emotionally significant topics in three individual weekly 45-minute sessions (e.g., relationships or goals). They were told that research indicates that body dissatisfaction is linked to emotional issues and that expressive writing helps resolve these issues.
Assessment-Only Control Condition
Participants in this condition were referred to treatment if they met criteria for a DSM-IV eating disorder at any of the follow-up assessments (as were participants in all conditions).
Measures
Perceived Pressure to be Thin
The Perceived Sociocultural Pressure Scale assessed perceived pressure to be thin from family, friends, dating partners, and the media (Stice et al. 2002). Items were averaged for this scale and those described below. This 8-item scale has shown internal consistency (α=.88), 2-week test-retest reliability (r=.93), and predicted future onset of bulimic symptoms (Stice et al. 2002).
Thin-Ideal Internalization
The Ideal-Body Stereotype Scale-Revised assesses endorsement of the thin-ideal (Stice et al. 2006). This 8-item scale has shown internal consistency (α=.91), 2-week test-retest reliability (r=.80), and predicted bulimic symptom onset (Stice et al. 2006).
Appearance Overvaluation
Nine items from Beliefs About Appearance Scale (Spangler and Stice 2001) assessed agreement with beliefs about the perceived importance of appearance for relationships, achievement, self-view, and feelings. This scale possesses internal consistency (α=.95), 3-week test-retest reliability (r=.83), and predicted binge eating onset (Spangler and Stice 2001; Stice et al. 2002).
Denial of Costs of Pursuing Thin-Ideal
We created five items assessing denial of costs associated with pursuing the thin-ideal (sample items: One can never exercise too much in their effort to be thin and The risks associated with severe dieting are overrated). A pilot study (N=42) indicated that this scale possesses internal consistency (α=.82) and 1-week test-retest reliability (r=.87).
Body Dissatisfaction
Eight items from the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid et al. 1973) assessed satisfaction with various body regions. This scale has shown internal consistency (α=.94), 3-week test-retest reliability (r=.90), and predicted bulimic symptom onset (Stice et al. 2006).
Body Image Distress
Twelve items asking participants to rate their level of distress about their body image concerns were drawn from the Body Esteem Scale for Adolescents and Adults (Mendelson et al. 1996). A pilot study (N=42) indicated that this scale possessed internal consistency (α=.87) and 1-week test-retest reliability (r=.91).
Readiness to Improve Body Satisfaction
We generated four items assessing readiness to improve body satisfaction (e.g., I am committed to improving my body image). This scale showed internal consistency at pretest (α=.81).
Body Mass
The body mass index (BMI=Kg/M2) was used to reflect adiposity. Height was measured to the nearest millimeter using portable stadiometer and weight was measured to the nearest 0.1 kg using digital scales with participants wearing light clothing without shoes or coats.
Perceived Weight Norms
We generated four items assessing underestimation of weight norms. Participants were asked how many pounds they think the average woman weighs; what dress size she wears; the size of her waist circumference, and to circle the schematic figure that looks most like the average woman. This scale showed internal consistency (α=.81) and 1-week test-retest reliability (r=.96) in a pilot study (N=42).
Self-reported Dieting
The Dutch Restrained Eating Scale (van Strien et al. 1986) assesses the frequency of dieting behaviors. This scale has shown internal consistency (α=.95), 2-week test-retest reliability (r=.82), convergent validity with self-reported caloric intake, but not objectively measured caloric intake, and predicted bulimic symptom onset (Stice et al. 2008b; van Strien et al. 1986).
Negative Affect
Negative affect was assessed with the sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale-Revised (PANAS-X; Watson and Clark 1992). Participants reported the extent to which they had felt various negative emotions. This scale has shown internal consistency (α=.95), 3-week test-retest reliability (r=.78), convergent validity, and predicted bulimic symptom onset (Stice et al. 2006).
Emotional Eating
We adapted four items from the Eating Helps Manage Negative Affect scale (Hohlstein et al. 1998) to assess emotional eating (e.g., When I am feeling really upset, eating takes my mind off my problems). The original scale has shown internal consistency, convergent validity, and discriminate validity (Hohlstein et al. 1998). This adapted scale showed internal consistency at T1 (α=.92).
Reward from Eating
We generated eight items assessing reward from eating (e.g., Do you enjoy eating more than most people?). This scale showed internal consistency at T1 (α=.80).
Social Rejection
We adapted six items assessing acceptance, admiration, and affection from friends and romantic partners (reverse scored) from the Network of Relationships Inventory (Furman 1996) and generated three items assessing interpersonal rejection from romantic partners, friends, and peers (e.g., Did a serious dating partner break up with you?). This scale showed internal consistency at T1 (α=.70).
Externalizing Symptoms
We adapted 13 items from the Externalizing scale of the Child Behavior Checklist that inquired about delinquent behaviors (Achenbach and Edelbrock 1983). This adapted scale showed internal consistency (α=.89) and predicted future increases in substance abuse/dependence and depression (Chassin et al. 1999).
Substance Use
Substance use was assessed with nine items from a scale developed by Chassin et al. (1991). Youth reported the frequency and quantity of intake of beer/wine/wine coolers and hard liquor, frequency of heavy drinking (five or more drinks in a row), frequency and quantity of cigarette use, and frequency of marijuana, stimulants, downers, inhalants, and hallucinogen use during the past month. This scale showed internal consistency (α=.82) and 1-month test-retest reliability (r=.89) in this sample.
Eating Disorder Onset
The Eating Disorder Diagnostic Interview, a semi-structured interview adapted from the Eating Disorder Examination (Fairburn et al. 1995), assessed onset (incidence) of DSM-IV anorexia nervosa, bulimia nervosa, and binge eating disorder, or subthreshold variants of these disorders over the 3-year follow-up. For subthreshold anorexia nervosa we required a BMI of between 90% and 85% of that expected for age and gender (vs. less than 85% of that expected for age and gender for a full threshold diagnosis), report a definite fear of weight gain, and report that weight and shape were definitely aspects of self-evaluation. For subthreshold bulimia nervosa we required at least 6 uncontrollable binge eating episodes and 6 compensatory behavior episodes over a 3-month period (vs. 24 for a full threshold diagnosis), and that weight and shape were definitely aspects of self-evaluation. For subthreshold binge eating disorders we required at least 12 uncontrollable binge eating episodes/days over a 6-month period (vs. 48 for a full threshold diagnosis), fewer than 6 compensatory behavior episodes, report marked distress about binge eating, and that binge eating was characterized by three or more of the following; rapid eating, eating until uncomfortably full, eating large amounts when not physically hungry, eating alone because of embarrassment, feeling disgusted, depressed, or feeling guilty after overeating. Such subthreshold eating disorders would receive a diagnosis of eating disorder-not otherwise specified (ED-NOS) per DSM-IV criteria. Eating disorder diagnoses showed test-retest reliability (κ=.96) inter-rater agreement (κ=.86) in this sample.
Data Analytic Plan
Classification tree analysis (Breiman et al. 1984) provides a nonparametric alternative to linear and additive logistic models for dichotomous outcomes. Trees are fitted using a binary recursive partitioning approach that selects the optimal cut-point on the most potent risk factor for generating subgroups with differential risk for the outcome. This procedure is then repeated on the resulting subgroups until there are no remaining predictors that identify subgroups at significantly differential risk or the node sizes become too small. When different risk factors emerge for two branches from the same fork, it signifies an interaction. The Chi-Square Automatic Interaction Detection (CHAID) growing method was used and the minimum node size was set at 25 for the parent (i.e., initial) node and 10 for child (i.e., subsequent) nodes to minimize Type I error and influential outliers. A Bonferroni correction was used to maintain alpha at p=.05 for splitting nodes.
Three percent of participants did not provide data at posttest, 7% at the 6-month follow-up, 6% at the 1-year follow-up, 5% at the 2-year follow-up, and 6% at the 3-year follow-up. The number of completed assessments was not associated with intervention condition, demographic factors, or baseline risk factor scores (all ps>.05). We employed an intent-to-treat analysis by using maximum likelihood estimates to impute missing data with SPSS Missing Value analysis module, as it produces more accurate and efficient parameter estimates than listwise deletion or last-observation-carried-forward (Schafer and Graham 2002). We used all available data for the computed variables examined herein to impute missing data.
Results
To ensure that eating disorder onset occurred during follow-up, we excluded those who met criteria for subthreshold or threshold eating disorders at baseline; 71 participants (14%) had a baseline eating disorder and were omitted (2 met criteria for bulimia nervosa at baseline while the other 69 met criteria for subthreshold eating disorders). Presence of a subthreshold/threshold eating disorder at baseline was not related to intervention condition. A total of 36 participants (8.8%) developed an eating disorder over the 3-year follow-up (Stice et al. 2008b); 3 showed subthreshold anorexia nervosa onset, 1 showed bulimia nervosa onset, 23 showed subthreshold bulimia nervosa onset, 1 showed binge eating disorder onset, and 12 showed subthreshold binge eating disorder onset (4 experienced multiple disorders). Those who experienced an eating disorder onset reported significantly greater mental health care utilization at the 2- and 3-year follow-ups (an average of 11 times during follow-up) and significantly greater psychosocial impairment at 2- and 3-year follow-up than those who remained free of an eating disorder (Stice et al. 2008b). Table 1 shows the correlations between demographic factors and all measures for the 410 study participants that were followed over time. All correlations represent a small effect size.
Table 1.
Correlations between demographic characteristics and study measures
| Study Demographic Characteristics
|
|||
|---|---|---|---|
| Age | Minority Status | Parent Education | |
| Perceived pressure to be thin | .16 | .04 | .08 |
| Thin-ideal internalization | .20 | -.07 | .11 |
| Appearance overvaluation | .10 | -.03 | .07 |
| Denial of costs of pursuing thin ideal | −.24 | .10 | −.13 |
| Body dissatisfaction | −.09 | .01 | −.02 |
| Body image distress | .05 | −.02 | .06 |
| Readiness to improve body satisfaction | −.03 | .04 | −.03 |
| Body mass | .03 | .17 | .01 |
| Perceived weight norms | .24 | −.10 | .14 |
| Self-reported dieting | .03 | −.01 | .07 |
| Negative affect | −.08 | .01 | −.05 |
| Emotional eating | .14 | −.06 | .14 |
| Subjective reward from eating | .12 | .03 | −.01 |
| Social rejection | .14 | −.05 | −.02 |
| Externalizing symptoms | .01 | −.04 | .01 |
| Substance use | .12 | −.14 | .01 |
Pearson correlation coefficients are reported for participant age and parental education. Point-biserial correlation coefficients are reported for minority status
Classification Tree Analysis
We first estimated an unrestricted CTA model, in which the algorithm selected the strongest predictor of eating disorder onset from the entered baseline risk factors, demographic factors, and intervention condition. This was done to test whether assignment to intervention condition had stronger predictive effects than the risk factors or moderators. This CTA model produced a classification tree with four forks and six terminal nodes (Fig. 2). Denial of the costs of pursuing the thin-ideal emerged as the first and most potent predictor of eating disorder onset. Participants with scores in the upper 16% of the distribution showed a 4-fold increase in risk for eating disorder onset relative to adolescents with lower scores; eating disorder incidence was 23.5% for individuals with elevated denial scores versus 5.8% with lower denial scores (χ2 [1, N=410]= 22.14, adjusted p<.001; OR=4.95, 95% CI=2.41–10.17). Among participants with elevated denial scores, intervention condition emerged as the most potent predictor of eating disorder onset; the eating disorder incidence rate was 0.0% for participants in the dissonance condition versus 18.5% for participants in the healthy weight intervention or the expressive writing condition versus 50.0% for participants in the assessment-only condition (χ2 [2, N=68]= 14.79, adjusted p=.004; OR=6.32, 95% CI=2.16–18.54). In contrast, among participants with lower denial scores, emotional eating emerged as the most potent risk factor; eating disorder incidence was 15.9% for those with scores in the upper 18% of the distribution versus 3.6% for those with lower scores (χ2 [1, N=342]=14.10, adjusted p=.002; OR=5.08, 95% CI=2.01–12.08). Lastly, externalizing symptoms emerged as a risk factor, but only in the subset of participants with both low denial and low emotional eating scores: eating disorder incidence was 10.6% for those with elevated externalizing symptom scores versus 2.2% for those with lower scores (χ2 [1, N=279]=8.13, adjusted p=.013; OR=5.40, 95% CI=1.50–19.49).
Fig. 2.
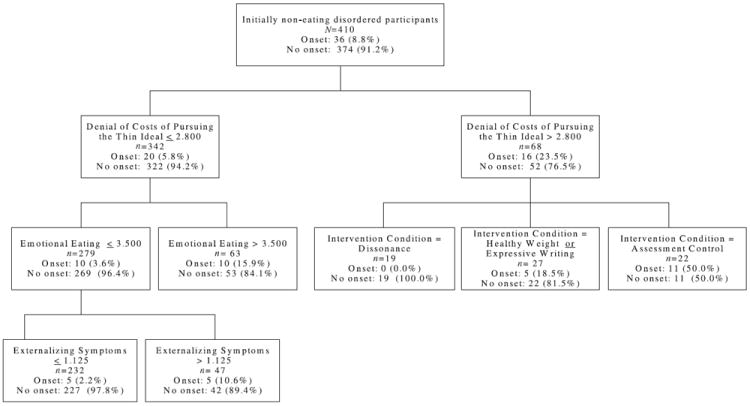
Decision rules for the classification tree predicting eating disorder onset with baseline risk factors and study condition. The empirically derived cut-points are shown with the sample size and the incidence for eating disorder onset during the study for each branch and node
Thus, the CTA with baseline factors and study condition revealed two 2-way interactions (high denial of costs of pursuing the thin-ideal X intervention condition; low denial of costs of pursuing the thin-ideal X emotional eating) and one 3-way interaction (low denial X low emotional eating X externalizing symptoms). These were all large effects, given the convention that odds ratios of 1.48, 2.48, and 4.28 reflect small, medium, and large effect sizes (Lipsey and Wilson 2001). The CTA resulted in a 91.2% accuracy rate in predicting eating disorder onset.
We knew a priori that it would be necessary to either manually enter the most potent risk factor for eating disorder onset or enter intervention condition on step one of a CTA model to provide an optimally sensitive test of whether the dissonance program mitigated the effects of the most potent risk factor for eating disorder onset and whether any factors moderated the effects of this intervention on eating disorder onset. Because the unrestricted CTA model selected a risk factor rather than intervention condition as the most potent single predictor of eating disorder onset, in the second CTA model we manually entered intervention condition on the first branch of the second CTA model before allowing the algorithm to select the next most potent risk factor that predicted eating disorder onset on the resulting branches. It should be noted that the algorithm still had to select the particular cut-point on the condition variable that identified groups at maximally differential risk for eating disorder onset.
The second CTA produced a classification tree with five forks and five terminal nodes (Fig. 3). Intervention condition split the sample between those in any active treatment group and those in the assessment-only control group; the eating disorder incidence rate was 6.7% for participants in any of the active intervention conditions versus 15.5% for participants in the assessment-only control condition (χ2 [1, N=410]=7.09, adjusted p=.054; OR=2.54, 95% CI=1.25–5.15). Among participants in the active intervention conditions, negative affect emerged as the strongest predictor of eating disorder onset. Participants with scores in the upper 10% of the distribution showed a 4-fold increase in risk for eating disorder onset relative to those with lower negative affect scores; eating disorder incidence was 20.7% for individuals with elevated negative affect scores versus 5.3% for those with lower negative affect scores (χ2 [1, N=313]=9.98, adjusted p=.014; OR= 4.68, 95% CI=1.66–13.21). Among active treatment participants with lower negative affect scores, emotional eating emerged as the most potent risk factor; eating disorder incidence was 9.0% for those with scores in the upper 54% of the emotional eating distribution versus 0.8% for those with lower scores (χ2 [1, N=284]=9.43, adjusted p=.019; OR=12.51, 95% CI=1.62–96.38). Among participants in the assessment-only control group, denial of the costs of pursuing the thin-ideal emerged as the strongest predictor of eating disorder onset. Youth with scores in the upper 16% of the distribution of denial showed a 10-fold increase in risk of eating disorder onset than adolescents with lower denial scores; incidence was 50.0% for participants with elevated denial scores versus 5.3% for participants lower denial scores (χ2 [1, N=97]=25.96, adjusted p<.001; OR=17.75, 95% CI=4.79–65.71). Last, appearance overvaluation emerged as a risk factor in the subset of adolescents in the assessment-only control group with low denial scores: Eating disorder incidence was 16.7% for those with elevated appearance overvaluation scores versus 0.0% for those with lower scores (χ2 [1, N=75]=8.98, adjusted p=.025; OR cannot be computed).
Fig. 3.
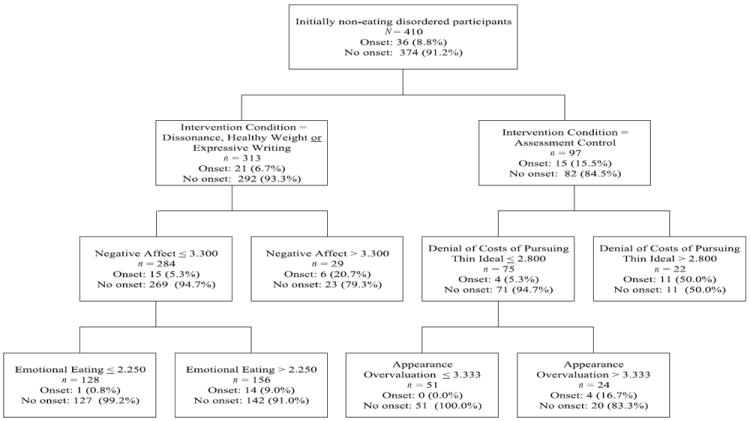
Decision rules for the classification tree predicting eating disorder onset with baseline risk factors and study condition entered as the first predictor. Empirically derived cut-points are shown with the sample size and the incidence during the study for each branch and node
Thus, the CTA model with condition entered as the first split revealed two 2-way interactions (active treatment condition X negative affect; assessment-only condition X denial of costs of pursuing the thin-ideal) and two 3-way interactions (active treatment condition X negative affect X emotional eating; assessment-only condition X denial of costs of pursuing the thin-ideal X appearance overvaluation). Findings in this second CTA model all reflected large effects. The CTA resulted in a 91.2% accuracy rate in predicting eating disorder onset.
Discussion
Denial of the costs of pursuing the thin-ideal emerged as the most potent risk factor for onset of eating disorders in this sample of young women at high risk for eating disorders by virtue of body dissatisfaction. Young women scoring in the upper 16% of this measure showed a 4-fold increase in risk for developing an eating disorder during the 3-year follow-up relative to the rest of the sample. This result converges with past evidence that thin-ideal internalization increases risk for future increases in eating pathology (Field et al. 1999; Wichstrom 2000). The fact that denial of costs of pursuing the thin-ideal emerged as a more potent predictor of eating disorder onset than intervention condition suggests that the former risk factor has a stronger effect than did the prevention programs. That denial of costs of pursuing the thin-ideal emerged as a more potent risk factor for eating disorder onset than related constructs (e.g., thin-ideal internalization and appearance overvaluation) or other widely studied risk factors (e.g., perceived pressure to be thin, self-reported dieting) implies that refusing to acknowledge the negative effects of pursuing an unrealistic beauty ideal may be a key vulnerability factor for the eating disorder onset and should be investigated in future etiologic and preventive studies.
With regard to the aim of identifying moderators of eating disorder prevention programs, results from the second CTA model, in which intervention condition was entered as the first branch, suggested that negative affect attenuated the effects of all three active interventions. Although this is partially due to the fact that the first split in this CTA model was between participants in any active intervention versus the assessment-only control condition, elevated negative affect increased the incidence of eating disorder onset from 5.2% to 20.0% for dissonance participants, from 5.4% to 12.5% for healthy weight participants, and from 5.3% to 27.3% for expressive writing participants. This suggests that negative affect may be a general moderator, rather than an intervention-specific moderator, perhaps because it reduces motivation to engage in prevention programs, regardless of intervention content. Clinically, this implies that it might be advisable to offer a prevention program that reduces affective disturbances for those who report negative affect before offering the dissonance program. Several prevention programs have been developed for this purpose (Stice et al. 2009c).
Of note, completing the healthy weight or expressive writing interventions reduced incidence of eating disorder onset for those who denied costs of pursuing the thin-ideal; the incidence was 18% for participants in these conditions versus 50% in the assessment-only control condition. Although the dissonance intervention was significantly more effective in reducing risk for eating disorder onset than these two alternative interventions, results imply that these other two interventions also significantly reduced risk for eating disorder onset relative to assessment-only controls. This pattern of findings suggests that initiating small, lasting changes to dietary intake and activity level, as well as expressing emotionally salient topics in writing may represent alternative methods of reducing risk for eating disorder onset. This pattern of findings may also suggest that non specific factors, such as participant expectations and demand characteristics inherent to randomized trials contribute to intervention effects of prevention programs, echoing results from other trials (McMillan et al. 2011).
Results from the unconstrained CTA model implicate three qualitatively distinct pathways to eating disorders onset in this high-risk sample, with results from the second restricted CTA model echoing this pattern of effects. Data suggest that the most potent vulnerability pathway to eating disorders involves pursuing the thin-ideal, with nearly 25% of individuals who deny the costs of pursuing this ideal showing onset of eating disorders, relative to less than 6% among individuals not denying these costs. Interestingly, results suggest that emotional eating was the next most prevalent vulnerability pathway to eating pathology in this sample. Among the subset of young women who did not deny the costs of pursuing the thin-ideal, the incidence of eating disorder onset was 16% for those with elevated emotional eating scores compared to less than 4% among those with lower emotional eating scores. This finding converges with prior evidence that emotional eating increases risk for onset of binge eating in non-high-risk samples (Smith et al. 2007; Stice et al. 2002). This finding provides support for the thesis that some individuals may initiate binge eating because it provides comfort or distraction from negative affect. Last, among youth not denying the costs of pursuing the thin-ideal or reporting emotional eating, externalizing symptoms emerged as the most potent risk factor: Eating disorder onset was 11% among those with elevated externalizing score, relative to only 2% for those endorsing fewer externalizing behaviors. Theoretically, these individuals are at elevated risk for eating disorder onset because this is a proxy measure of trait impulsivity (Wonderlich et al. 2004). Externalizing symptoms have predicted bulimic symptom onset (Wonderlich et al. 2004) and attention-deficit hyperactivity disorder predicts future escalation of eating disorder symptoms (Mikami et al. 2008).
Interestingly, the CTA model in which condition was entered as the first branch, negative affect emerged as a risk factor for eating disorder onset for participants assigned to any of the prevention interventions, and emotional eating emerged as a risk factor for adolescents who reported lower negative affect scores. This pattern of findings serves as a reminder that emotional eating may emerge as a risk factor for eating disorder onset even among individuals who do not report elevated negative affect.
In sum, results suggest three qualitatively distinct vulnerability pathways to eating disorder onset in this high-risk sample, characterized by pursuit of the thin-ideal, negative affect/emotional eating, and externalizing symptoms. A novel implication from these findings is that it may be possible to improve the overall yield of prevention efforts by offering a prevention program that reduces negative affect and emotional eating to individuals who endorse these risk factors and by offering a program that reduces externalizing symptoms for those reporting these behaviors. Future research should test whether such a tailored approach to prevention produces greater reductions in the lower incidence of eating disorder onset relative to using a single prevention program.
The limitations of this study should be noted. First, because only 36 out of the 410 initially eating disorder-free participants showed eating disorder onset during the 3-year follow-up (9%) and because CTA is an exploratory data analytic technique, it will be important to replicate findings. Second, it was not feasible to include measures of additional risk factors, due to respondent burden concerns. We might have observed different predictors and interactions among predictors if we had included additional risk factors (e.g., perfectionism). Third, it is possible that some of those participants who did not show eating disorder onset during the follow-up period may do so in the future, as certain eating disorders, such as binge eating disorder, shows initial onset in young adulthood (Wilson et al. 2003).
The present findings provide the first evidence that a brief eating disorder prevention program effectively reduces the risk conferred by a potent risk factor for future onset of eating disorders. The fact that the most potent risk factor was denial of the costs of pursuing the thin-ideal provides support for the intervention theory for the dissonance eating disorder prevention program. The CTA model suggested three pathways to eating disorder onset, characterized by pursuit of the thin-ideal, emotional eating/negative affect and externalizing symptoms. It may be possible to improve the overall yield of prevention efforts by expressly targeting each of these factors.
Acknowledgments
This study was supported by research grants (MH/DK6195 and MH70699) and a career award (MH01708) from the National Institutes of Health.
We thank project managers Erin Martinez, Emily Wade, and Kathryn Fisher; project research assistants Emily Burton, Cassie Goodin, and Natalie McKee; our undergraduate volunteers; the Austin Independent School District; and the participants who made this study possible.
References
- Achenbach TM, Edelbrock C. Manual for the child behavior checklist and revised child behavior profile. Burlington, VT: Queen City Printers; 1983. [Google Scholar]
- Becker CB, Smith L, Ciao AC. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–254. [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Peer-facilitated eating disorder prevention: A randomized effectiveness trial of cognitive dissonance and media advocacy. Journal of Counseling Psychology. 2006;53:550–555. [Google Scholar]
- Becker CB, Bull S, Schaumberg K, Cauble A, Franco A. Effectiveness of peer-led eating disorders prevention: A replication trial. Journal of Consulting and Clinical Psychology. 2008;76:347–354. doi: 10.1037/0022-006X.76.2.347. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees. Belmont, CA: Wadsworth; 1984. [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomatology among adolescent children of alcoholics. Journal of Abnormal Psychology. 1991;100:449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts S, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Crow S, Peterson C, Swanson S, Raymond N, Specker S, Eckert E, et al. Increased mortality in bulimia nervosa and other eating disorders. The American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Norman PA, Welch SL, O’Connor ME, Doll HA, Peveler RC. A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Archives of General Psychiatry. 1995;52:304–312. doi: 10.1001/archpsyc.1995.03950160054010. [DOI] [PubMed] [Google Scholar]
- Field A, Camargo C, Taylor C, Berkey C, Colditz G. Relation of peer and media influences to the development of purging behaviors among preadolescent and adolescent girls. Archives of Pediatric Adolescent Medicine. 1999;153:1184–1189. doi: 10.1001/archpedi.153.11.1184. [DOI] [PubMed] [Google Scholar]
- Furman W. The measurement of friendship perceptions: Conceptual and methodological issues. In: Bukowski WM, Newcomb AF, Hartup WW, editors. The company we keep. New York: Cambridge University Press; 1996. pp. 41–65. [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C, Pederson E. Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders. 2005;13:157–169. doi: 10.1080/10640260590918955. [DOI] [PubMed] [Google Scholar]
- Hohlstein LA, Smith GT, Atlas JG. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment. 1998;10:49–58. [Google Scholar]
- Jacobi C, Hayward C, Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Newbury Park, CA: Sage; 2001. [Google Scholar]
- McMillan W, Stice E, Rohde P. High- and low-level dissonance-based eating disorder prevention programs with young women with body image concerns: An experimental trial. Journal of Consulting and Clinical Psychology. 2011;79:129–134. doi: 10.1037/a0022143. [DOI] [PubMed] [Google Scholar]
- Mendelson B, White D, Mendelson M. Manual for the body-esteem scale for adolescents and adults. 1996 doi: 10.1207/S15327752JPA7601_6. Unpublished manual. [DOI] [PubMed] [Google Scholar]
- Mikami AY, Hinshaw SP, Patterson KA, Lee JC. Eating pathology among adolescent girls with attention-deficit/hyperactivity disorder. Journal of Abnormal Psychology. 2008;117:225–235. doi: 10.1037/0021-843X.117.1.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell KS, Mazzeo SE, Rausch SM, Cooke KL. Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. International Journal of Eating Disorders. 2007;40:120–128. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- Perez M, Becker C, Ramirez A. Transportability of an empirically supported dissonance-based prevention program for eating disorders. Body Image. 2010;7:179–186. doi: 10.1016/j.bodyim.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Seidel A, Presnell K, Rosenfield D. Mediators in the dissonance eating disorder prevention program. Behaviour Research and Therapy. 2009;47:645–653. doi: 10.1016/j.brat.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Smith G, Simmons J, Flory K, Agnes A, Hill K. Thinness and eating expectancies predict subsequent binge eating and purging behavior among adolescent girls. Journal of Abnormal Psychology. 2007;116:188–197. doi: 10.1037/0021-843X.116.1.188. [DOI] [PubMed] [Google Scholar]
- Spangler D, Stice E. Validation of the beliefs about appearance scale. Cognitive Therapy and Research. 2001;25:813–827. [Google Scholar]
- Stice E. A prospective test of the dual pathway model of bulimic pathology: Mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset: A prospective investigation. Health Psychology. 2002;21:131–138. [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Shaw H, O’Neil K. General and program-specific moderators of two eating disorder prevention programs. International Journal of Eating Disorders. 2008a;41:611–617. doi: 10.1002/eat.20524. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008b;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology. 2009a;118:587–597. doi: 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. Journal of Consulting and Clinical Psychology. 2009b;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009c;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Rohde P, Shaw H. Testing mediators hypothesized to account for the effects of a dissonance eating disorder prevention program over longer-term follow-up. Journal of Consulting and Clinical Psychology. 2011a doi: 10.1037/a0023321. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance-based eating disorder prevention program for female high school students: Long-term effects. Journal of Consulting and Clinical Psychology. 2011b;79:500–508. doi: 10.1037/a0024351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien T, Frijters JE, Van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch restrained eating scale. International Journal of Eating Disorders. 1986;5:747–75. [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality and Social Psychology. 1992;62:489–505. [Google Scholar]
- Wichstrom L. Psychological and behavioral factors unpredictive of disordered eating: A prospective study of the general adolescent population in Norway. International Journal of Eating Disorders. 2000;28:33–42. doi: 10.1002/(sici)1098-108x(200007)28:1<33::aid-eat5>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Becker CB, Heffernan K. Eating disorders. In: Mash EJ, Barkley RA, editors. Child psychopathology. 2. New York: Guilford; 2003. pp. 687–715. [Google Scholar]
- Wonderlich SA, Connolly KM, Stice E. Impulsivity as a risk factor for eating disordered behavior: Assessment implications with adolescents. International Journal of Eating Disorders. 2004;36:172–182. doi: 10.1002/eat.20033. [DOI] [PubMed] [Google Scholar]


