Post-operative atrial fibrillation (PoAF) is among the most common complications of cardiac surgery and substantially increases morbidity and health care costs. Despite decades of surgical, anesthetic, and medical advances, rates of PoAF remain largely unchanged. Experiments and animal models suggest that peri-operative fish oil (omega-3 fatty acids) may reduce PoAF.(1) We recently reported in a large, multinational randomized trial that peri-operative fish oil did not reduce PoAF.(2) Yet, several other trials have evaluated this question, with mixed results. Most of these trials were small, and some were open label, i.e. neither double-blind nor placebo-controlled.
To compile all peer-reviewed evidence and evaluate reasons for potential heterogeneity, we conducted a meta-analysis, following PRISMA guidelines, of randomized trials of fish oil for preventing PoAF. We searched MEDLINE from earliest available indexing through Oct 2012, without language restrictions. Search terms were ("fatty acids, omega-3"[MeSH] or "eicosapentaenoic acid"[MeSH/tiab] or "docosahexaenoic acids"[MeSH/tiab] or "fish oils"[MeSH] or "omega-3"[tiab] or "n-3"[tiab] or "long chain n-3"[tiab] or "fish oil"[tiab]) and ("atrial fibrillation"[MeSH/tiab]) and (“clinical trial”[MeSH/tiab] or “cardiac surgical procedures”[MeSH/tiab]). Additional studies were identified through hand-searching citation lists and directly contacting experts. Studies were included if they were randomized trials of oral or intravenous fish oil administration that evaluated PoAF following cardiac surgery; trials with additional concomitant interventions, observational studies, and duplicate publications were excluded. Inclusion/exclusion decisions and data extraction were performed in duplicate by two investigators. Findings were pooled using inverse-variance weighted meta-analysis.(3) Fixedeffects models were prespecified based on large differences in sample sizes and results across studies, for which random-effects models could dramatically overweight small, imprecise studies. Prespecified potential sources of heterogeneity included placebo-control (yes/no) and type of surgery (valve surgery, yes/no).
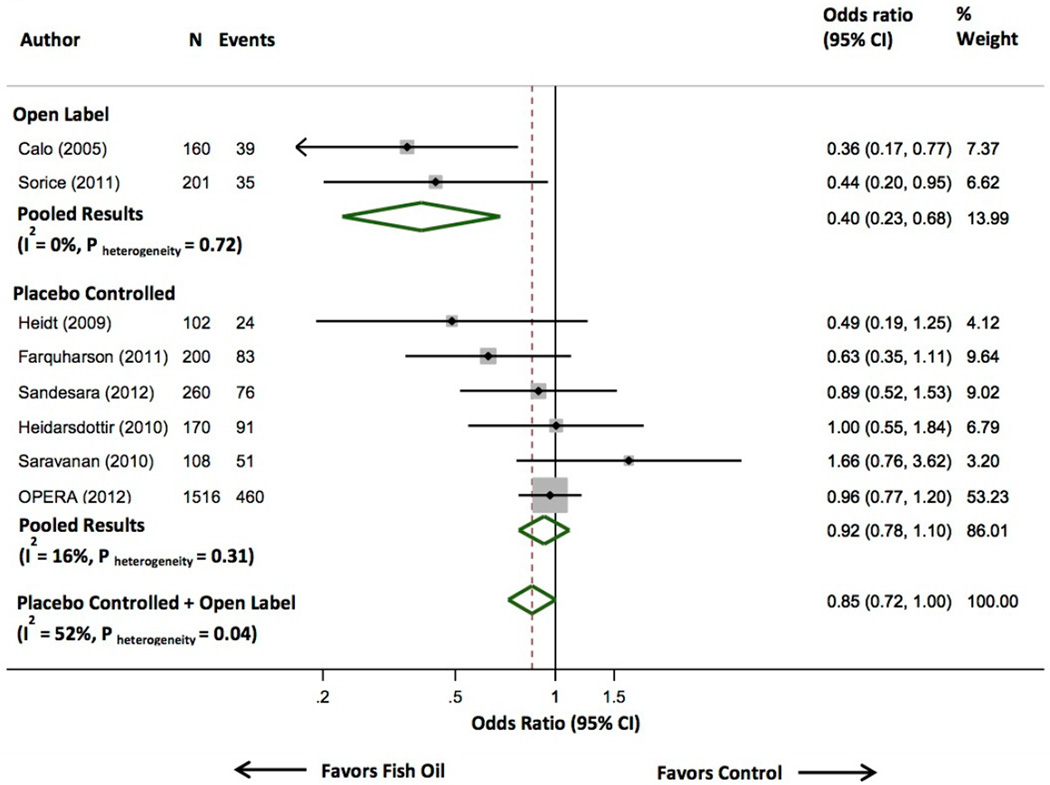
Of 83 identified abstracts, 8 full-text articles were retrieved for review. Eight randomized trials met inclusion criteria, including 2,687 subjects and 859 PoAF events (Figure). Heterogeneity was evident (I2=52%, Q-statistic=14.5, P-heterogeneity=0.04), principally owing to extreme results of two small, open-label (no placebo) studies. Presence or absence of placebo-control significantly modified the effect of fish oil on PoAF (P-interaction=0.028): benefits were seen in open-label, but not placebo-controlled, trials. Also, a preponderance of small trials with risk estimates below the pooled estimate suggested potential publication bias toward small positive trials. Little heterogeneity was evident among placebo-controlled trials (I2=16%, Q-statistic=5.9, P-heterogeneity=0.31), which both individually and together demonstrated no significant effect (pooled OR=0.92, 95%CI=0.78–1.10). In sensitivity analyses, we removed each trial individually from the pooled meta-analysis. Finding were similar; for example, removing the large OPERA trial, the pooled OR in the remaining placebo-controlled trials was 0.86 (95%CI=0.65–1.15; I2=28%, Q-statistic=5.6). We note that only two open-label trials were identified, so generalizability of these findings to other research questions should not be assumed. Yet, the variation in findings of small and especially open-label studies highlights the importance of large, adequately powered, placebo-controlled trials as well as appropriately performed meta-analyses such as the present report.
Figure. Randomized Controlled Trials of Peri-Operative Fish Oil Supplementation to Prevent Post-Operative Atrial Fibrillation.
Studies were pooled using inverse-variance weighted meta-analysis with fixed effects. Although the overall pooled result was of borderline statistical significance, substantial heterogeneity was evident (I2=52%, Q statistic=14.5), which was largely explained by whether trials were open label (top 2 studies) versus placebo-controlled (bottom 6 studies). The open-label studies suggested a benefit, but the double-blind, placebo-controlled trials confirmed no significant effect of fish oil on post-operative atrial fibrillation (OR=0.92, 95% CI=0.78–1.10), with little heterogeneity between studies (I2=16%, Q statistic=5.93). Sensitivity analyses using random effects meta-analysis showed similar findings for the overall pooled results (OR=0.76, 95% CI=0.57–1.03; I2=52%, Q statistic=14.5, P-heterogeneity = 0.04), results restricted to open-label trials (OR=0.40, 95% CI=0.23–0.68; I2=0%, Q statistic=0.13, P-heterogeneity=0.72), and results restricted to placebo-controlled trials (OR=0.91, 95% CI=0.73–1.13; I2=16%, Q statistic=5.93, P-heterogeneity=0.31).
In the large OPERA trial, subgroup analyses suggested a potential benefit of fish oil treatment in patients undergoing valve surgery (P-interaction=0.06).(2) We pooled these results with four other placebo-controlled trials that provided data stratified by type of cardiac surgery. In sum, data were available on 856 patients who underwent valve surgery and experienced 336 PoAF events, and 1,249 patients not undergoing valve surgery who experienced 358 PoAF events. Pooling all data, effects of fish oil on PoAF did not significantly differ according to valve surgery (P-interaction=0.94): the OR was 0.91 (95%CI=0.76–1.09) in patients undergoing valve surgery and 1.00 (95%CI=0.78–1.28) in patients not undergoing valve surgery. Dosing and duration of fish oil treatment were generally similar among trials, limiting ability to explore heterogeneity by these factors.
We evaluated pooled evidence for safety including numbers of patients with major bleeding, total mortality, and other reported serious adverse events. Fish oil was associated with less bleeding (N=165 events, data reported in 5 trials: OR=0.76, 95%CI=0.60–0.96; I2=34.1, Q-statistic= 6.1, P-heterogeneity=0.19), a nonsignificant trend toward lower mortality (N=32 events, data reported in 6 trials: OR=0.68, 95%CI=0.32–1.41; I2=0%, Q-statistic=1.98, P-heterogeneity= 0.58), and no difference in other reported serious adverse events (N=528 events, data reported in 6 trials: OR=1.0, 95%CI=0.81–1.25; I2=0%, Q-statistic=4.7, P-heterogeneity= 0.45) The unexpectedly lower bleeding risk could be due to chance. Conversely, this observation could plausibly relate to lower cardiopulmonary bypass-induced activation and loss of platelets and clotting factors;(4) further investigation of potential mechanisms is required. At the least, the observed lower bleeding risk counters concerns that anti-platelet effects of fish oil might increase blood loss during cardiac surgery. Overall, the findings indicate that peri-operative fish oil use was well-tolerated and safe, suggesting little need for its discontinuation in patients who are taking fish oil prior to cardiac surgery.
In sum, our meta-analysis provides convincing evidence that short-term fish oil use does not appreciably reduce PoAF, and indicates that heterogeneity in prior findings results from extreme results of small, open-label trials as well as potential publication bias. In addition, we found little evidence for differing efficacy according to type of cardiac surgery. There is also little evidence that intermediate-term (<1 year) fish oil use reduces recurrent arrhythmias in patients with established AF.(5) Fish oil may still prove useful in other clinical contexts, such as long-term use (years) for preventing the initial onset of AF among ambulatory elderly adults with hypertension or other risk factors. Such primary, rather than secondary, prevention approaches must be tested in large, appropriately powered, placebo-controlled clinical trials.
Acknowledgments
Funded by the National Heart, Lung, and Blood Institute, National Institutes of Health (RC2-HL101816).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011;58:2047–2067. doi: 10.1016/j.jacc.2011.06.063. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Marchioli R, Macchia A, et al. Fish oil and postoperative atrial fibrillation: the Omega-3 Fatty Acids for Prevention of Post-operative Atrial Fibrillation (OPERA) randomized trial. JAMA. 2012 doi: 10.1001/jama.2012.28733. Epub ahead of print Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 4.Sniecinski RM, Chandler WL. Activation of the hemostatic system during cardiopulmonary bypass. Anesth Analg. 2011;113:1319–1333. doi: 10.1213/ANE.0b013e3182354b7e. [DOI] [PubMed] [Google Scholar]
- 5.Kowey PR, Reiffel JA, Ellenbogen KA, Naccarelli GV, Pratt CM. Efficacy and safety of prescription omega-3 fatty acids for the prevention of recurrent symptomatic atrial fibrillation: a randomized controlled trial. JAMA. 2010;304:2363–2372. doi: 10.1001/jama.2010.1735. [DOI] [PubMed] [Google Scholar]