Abstract
Estimates of patients attending with conditions deemed non-urgent or inappropriate for accident and emergency services vary widely, from 6 to 80%. Previous research suggests that general practitioners (GPs) working in emergency departments can reduce referral rates, diagnostic testing, the proportion of patients who become emergency hospital admissions, and inappropriate attendances. However, little of this previous research is recent and new models of care for GPs working in emergency departments have now been developed, which remain to be evaluated. In this paper, we describe an integrated urgent care model, which was commissioned by NHS Hammersmith and Fulham in 2009 to manage the rising number of urgent attendances at local hospitals and its associated evaluation. The evaluation will include examining the effect of the system on outcomes such as utilization of diagnostic tests and effect on unplanned hospital admissions. If the new model of care is shown to be both clinically effective and cost-effective, the model and the proposed plan of evaluation will also be helpful to other areas that are considering the introduction of similar models of GP-led urgent care.
Introduction
Demand for urgent care in the UK continues to rise with increasing numbers of attendances at emergency departments, and the associated growth in unplanned hospital admissions and healthcare costs.1,2 With NHS budgets under severe pressure, using emergency services appropriately will be important in an era of financial austerity in healthcare.3,4
Estimates of patients attending with conditions deemed non-urgent or inappropriate for accident and emergency services vary widely, from 6 to 80%.5 Previous research suggests that general practitioners (GPs) working in emergency departments can reduce referral rates, diagnostic testing, the proportion of patients who become emergency hospital admissions, and inappropriate attendances.6–8 Furthermore, they can improve the efficiency of emergency departments by reducing the waiting time for emergency cases to receive care. Therefore, using GPs can be a cost-effective method of dealing with workload in emergency departments. However, little of this previous research is recent and new models of care for general practitioners working in emergency departments have now been developed, which remain to be evaluated.
In this paper, we describe an integrated urgent care model, which was commissioned by NHS Hammersmith and Fulham in 2009 to manage the rising number of urgent attendances at local hospitals.9 In August 2011, the Royal College of General Practitioners, in light of the soon to be formed clinical commissioning groups, published guidance on commissioning integrated urgent and emergency care. They identified the importance of examining pathways of care across systems.10
The model commissioned in Hammersmith and Fulham consisted of establishing two GP-led Urgent Care Centres. The centres were to be co-located with the emergency departments at Charing Cross and Hammersmith Hospitals, and were to provide general practice services. We describe our experience in developing an integrated model of care; some of the challenges in ensuring integration across the system; and a plan of analysis for the evaluation of the new service.
Background
The population of North West London is one of the most ethnically and socio-economically diverse in the UK. Ethnic minority groups comprise around 35% of the population, and pockets of deprivation co-exist alongside areas of affluence.11 The population is also highly mobile, with many residents who are not registered with a local general practice. These factors result in a high demand for care at local emergency departments.
The integrated model that was commissioned consisted of GPs who were responsible for triaging or streaming patients that walked through the doors of the urgent care centres. Patients attending either of the hospital sites automatically walked into the GP-led centre and reported to reception for registration. In this model, staff in the emergency department only saw patients who were referred by the GPs or nurses who worked at the centres or if patients arrived by ambulance.
Methods
Streaming guidelines were jointly developed between GPs and hospital specialists following consultation and preliminary piloting, leading to the implementation of the integrated urgent care model. Evaluation and subsequent analysis of the model will be undertaken by obtaining data from the clinical information systems mapped to the patient pathway. The following subheadings provide further description of methods to be used.
GP-led Streaming Model
Patients first report to reception and register. Following registration, the GP streamer sees the patient and makes a brief clinical decision, which takes approximately three minutes. Patients are then assigned to one of a number of clinical streams and are treated by either a doctor or nurse at the urgent care centre, or by a member of staff at the emergency department. Although streaming was usually undertaken by GPs, nurse practitioners sometimes undertook the role.
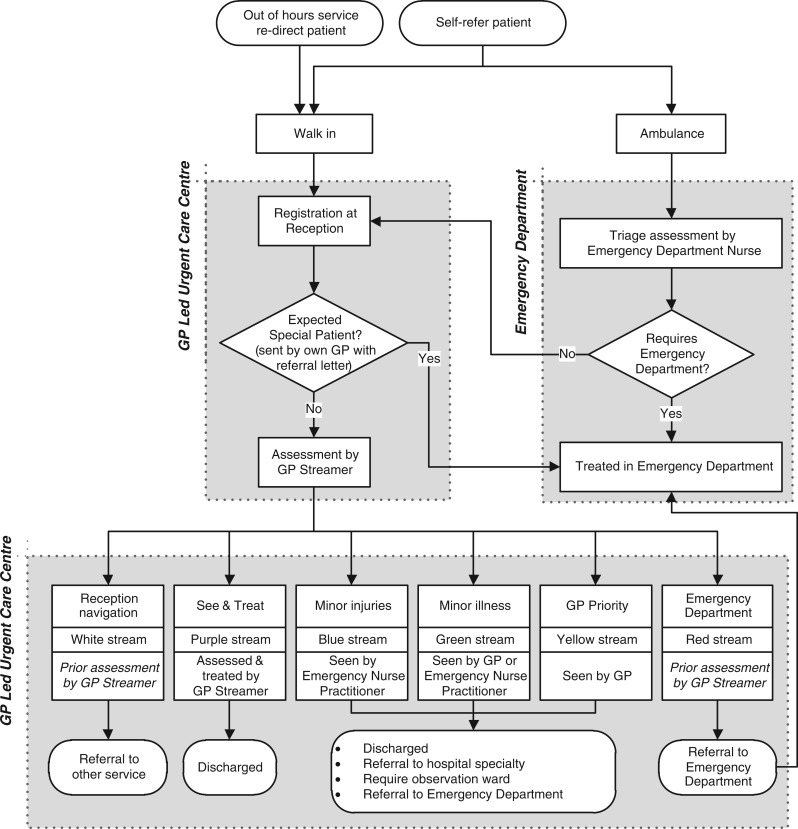
Figure 1 shows the patient pathway across the integrated model. Following assessment by the GP Streamer patients were directed to one of the following streams:
Emergency department (red stream)
Expected special patients are patients who arrive with a letter from their own GP, and are seen in the emergency department and are not seen by urgent care staff
GP priority case (yellow stream) – GP only
A minor injury (blue stream) – emergency nurse practitioner only
Minor illness (green stream) – GP or emergency nurse practitioner
Reception navigation (white stream) where patients were signposted to other services (such as an appointment with their own GP or referral to the Early Pregnancy Assessment Unit)
See and treat (purple stream) where treatment occurred at the point of streaming)
Did not wait (black stream) where patients did not wait to be seen.
Figure 1.
Patient pathway across the integrated GP-led model of care.
Streaming guidelines development
GPs who undertook streaming used jointly developed guidelines to ensure that patients were reviewed by the most appropriate clinician first time. The streaming guideline group consisted of two GPs, two emergency medicine consultants, and two accident and emergency nurse practitioners. The underlying principles followed by the guideline development group was to consider the type of patients that would normally walk through the door of the emergency department; the type of cases that GPs would be happy to see in the context of a normal surgery; and cases that were the exceptions to these rules and were not to be seen by GPs – that is, they were deemed an emergency and assigned to the red stream.
Although a formal algorithm was not used by the group, they did review evidence where available from the National Institute for Health & Clinical Excellence (NICE) and societies such as the British Thoracic Society to reach consensus on management of clinical conditions, for example chronic obstructive pulmonary disease. A key component of the group's discussion was to review any red flags in the history or examination, and agree the trigger points for measurement of physiological variables such as blood pressure, pulse rate, oxygen saturation and respiratory rate. Specialist advice and consensus on best practice was sought from emergency nurse practitioners, paediatricians, gynaecologists, and psychiatrists. The streaming guidelines were piloted in 200 clinical cases, 100 that were streamed by GPs and nurse practitioners. There were no adverse events recorded or any differences in how patients were managed by GPs and nurses.
Information system and flow of data
A key component of an integrated urgent care model is the underlying information systems to support the development of patient pathways. It is important that clinical data are available at the point of need. Further, data are required to fulfil the need for local and national performance metrics, such as the Department of Health's Accident and Emergency clinical quality data set that was introduced in April 2011.12
The Urgent Care Centres use the Adastra clinical patient management system.13 Adastra is a database system which is predominantly used by general practice out of hours services, and captures both patient administrative information and clinical data. The decision to use Adastra as the system of choice for the centres was because it would integrate with the out of hours GP services in the area. This is in contrast to the information database system used by the emergency departments at Charing Cross and Hammersmith Hospitals, which is Ascribe Symphony.14 Ascribe Symphony collects both administrative and clinical information, but is separate from the hospital's patient administrative system.
To date, the Adastra and Symphony databases do not share an interface that allows exchange of data. A key challenge in setting up the urgent care model has therefore been in integrating information systems.15 In the absence of integrated administrative and clinical data between the urgent care centre and the emergency department, a great deal of work has focussed on developing workaround processes to overcome such limitations. Patients who are identified as requiring care from an emergency department were immediately transferred to the emergency department for registration and management.
Information on the episode of care following urgent care centre attendance for patients registered with a GP in North West London is supplied in a discharge letter faxed over to their GP the next day, in the same way as done by the general practice out of hours service.
Evaluating the new model of care
The evaluation aims to answer the following questions:
Quality of care and health impact: Has the integrated care model as implemented resulted in improvements in the quality of care and in health outcomes for patients? Has there been a reduction in unscheduled hospital admissions? Has the model facilitated a more appropriate tailoring of clinical time and resources according to clinical need? Has the implementation of the integrated care model led to any other unintended consequences on the local health system including other primary care services?
Implementation: How has the new model of care been implemented? What elements of the model were more fully implemented than others? What were the factors that helped or blocked implementation?
Financial impact: What has been the cost of the model, both start-up and running costs? Has the model produced cost savings?
Patient experience: has the integrated care model as implemented resulted in a better patient experience of care?
Staff experience: What impact did the new model have on staff?
Initial analysis will focus on evaluating quality of care and health impact (objective 1). This will involve assessing:
Baseline demographic and clinical characteristics of patients attending the urgent care centres.
Trends in the total number of accident and emergency attendances at Hammersmith and Fulham Urgent Care Centres during the period January 2007 to December 2012.
Trends in the total number of accident and emergency hospital admissions at Hammersmith and Fulham Urgent Care Centres during the period January 2007 to December 2012.
Trends in the number of short stay hospital admissions at Hammersmith and Fulham Urgent Care Centres during the period January 2007 to December 2012.
Statistical analysis
Although randomised control trials are the ‘gold standard’ in the evaluation of health services, they are frequently not practical, ethical or politically acceptable in the evaluation of many health system or public health interventions. Hence, in this analysis, where possible, we will use an interrupted time series (ITS) design for the analysis of the quantitative data.16 An ITS is a regression model with an intervention at a given time point (see Figure 2). The intervention splits the regression into the two segments pre- and post-intervention, so that investigators can apply a segmented linear regression model. A policy effect is usually measured as the difference of outcome before and after the intervention. If the outcome has an underlying secular trend independent of the policy, standard statistical analysis will contribute the secular trend effect to the intervention, thus yielding an erroneously statistically significant effect of the policy. ITS analysis is not subject to this error, since it incorporates the secular trend of the outcome in the analysis. Where an ITS analysis is not possible, we will use a simpler ‘before and after’ design, combined with comparison with units in urban areas where the model of care has not changed.
Figure 2.
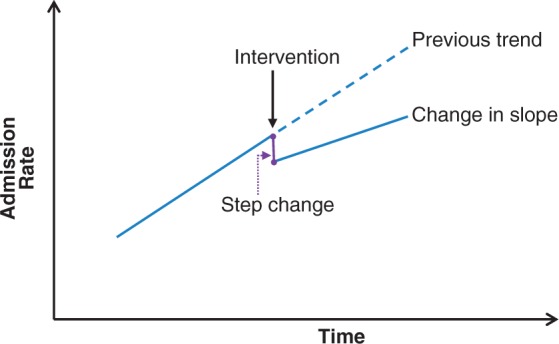
ITS design and regression analysis.
Discussion
As emergency department attendances continue to rise, there has been enormous interest among policy-makers to contain and reverse this trend by developing new models of care that avoid use of high cost hospital resources and diverting them to a more low cost primary care environment. Urgent care centres were implemented in the UK as part of this policy environment, without full evaluation, and proposed national evaluation has been hampered by access to data to identify the size of the effect, as well as wider organisational changes to the NHS. Quantifying the scope of substitution of one type of healthcare for another is difficult. However, previous research suggested that having GPs working in a hospital emergency department would lead to a more cost-effective method of substituting secondary care with primary care resources.7,17
A study in the Netherlands found that involving GPs during the day alongside staff at the accident and emergency department maintained the quality of care, and led to fewer examinations and led to greater patient satisfaction.18
Further, employing GPs in emergency departments to manage the primary care needs resulted in reduced rates of investigations, prescriptions and referrals. The study was set in a busy emergency department in London and did not consider patient outcome or satisfaction.7
Early studies in the 1990s used a modified version of the Sheffield or Nuffield Provincial Hospital criteria for classifying urgent care.19 The studies examined the medical records of patients and classified them according to the clinical management implied by their diagnosis. Patients with conditions which were not considered to require facilities above those available in general practice were labelled inappropriate. The high proportion of minor injuries among the inappropriate attendees when compared to users of out-of-hours primary care services suggested that they used the emergency department differently.
The streaming process used in the new model was initially counter intuitive for GPs, as it had to be a quick decision (approximately three minutes) to assess which stream a patient should be diverted to. GPs had been used to operating within a timeframe of a routine general practice consultation on average 10 minutes, and within this time frame making a definitive management plan.
Establishing any new service model involves implementing change management processes. In establishing the new health centres there were concerns that general practitioners would not have the full range of skills to manage many of the emergency department walk-in patients, and that evaluation of the model of care would provide information as to the quality and safety of care received. Furthermore, for many GPs, the urgent care centre presents a novel environment in dealing with patients.20 GPs in the UK normally have access to a full set of computerised medical records among their registered patients.21 The urgent care centre, along with emergency departments generally, only has access to clinical records if a patient has attended previously.
Any evaluation needs to consider the effect on staff working at the urgent care centre and the emergency department, and determine to what extent the change has influenced professional clinical practice and behaviours. The implications of these effects on patient outcomes remain to be seen.
Conclusion
We have developed a model of care which can potentially safely manage the vast majority of patients who walk into the two urgent care centres. Our next steps are to examine the effect of the system on outcomes such as utilisation of diagnostic tests and effect on unplanned hospital admissions, as well as on areas such as patient safety and quality of care. If the new model of care is shown to be both clinically effective and cost-effective, the model and the proposed plan of evaluation will also be helpful to other areas that are considering the introduction of similar models of GP-led urgent care.
DECLARATIONS
Competing interests
SG, FR, SI, JC and AM are employed by Imperial College London, which received funding to help evaluate the new model of care.
Funding
The new service model was funded by NHS Hammersmith & Fulham. The Department of Primary Care & Public Health at Imperial College received funding from the Imperial College NHS Trust to help evaluate the new model. Support for the evaluation was also received from the NIHR CLAHRC for NW London.
Guarantor
SG
Contributorship
SG, FR and AM conceived and wrote the article. All authors contributed to the critical revision of the paper and approved the final version.
Acknowledgements
We thank all the staff who have and currently work for Partnership for Health in setting up the services; and staff at Hammersmith and Charing Cross Emergency Departments for their help. We also thank Professor Chris Salisbury for his advice on the evaluation. Partnership for Health is a consortium of London Central and West Unscheduled Care Collaborative, Imperial College Healthcare NHS Trust and Central London Community Health Services.
Provenance
This article was submitted by the authors and peer reviewed by Sam Creavin
References
- 1. DOH. Accident and Emergency attendances Department of Health; 2011. See http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_077485 (last checked 8 April 2013)
- 2. Blunt I, Bardsley M, Dixon J. Trends in emergency admissions in England 2004–2009: is greater efficiency breeding inefficiency?, London: Nuffield Trust, 2010 [Google Scholar]
- 3. Majeed A. Primary care in Europe: entering the age of austerity. J Ambul Care Manage 2012; 35: 162–6 [DOI] [PubMed] [Google Scholar]
- 4. Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002; 324: 819–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murphy AW. ‘Inappropriate’ attenders at accident and emergency departments I: definition, incidence and reasons for attendance. Fam Prac 1998; 15: 23–32 [DOI] [PubMed] [Google Scholar]
- 6. Dale J, Green J, Reid F, Glucksman E. Primary care in the accident and emergency department. I. Prospective identification of patients. BMJ 1995; 311: 423–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dale J, Green J, Reid F, Glucksman E, Higgs R. Primary care in the accident and emergency department. II. Comparison of general practitioners and hospital doctors. BMJ 1995; 311: 427–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dale J, Lang H, Roberts JA, Green J, Glucksman E. Cost effectiveness of treating primary care patients in accident and emergency: a comparison between general practitioners, senior house officers, and registrars. BMJ 1996; 312: 1340–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. ICHN Trust. Hammersmith and Fulham Centres for Health, 2012. See http://www.imperial.nhs.uk/services/centreforhealth/index.htm (last checked 1 August 2012)
- 10. Agnelo F. Guidance for Commissioning Integrated Urgent and Emergency Care: ‘A Whole System Approach’, The RCGP Centre for Commissioning, London: Royal College of General Practitioners, 2011 [Google Scholar]
- 11. Harris M, Greaves F, Patterson S, et al. The North West London Integrated Care Pilot: innovative strategies to improve care coordination for older adults and people with diabetes. J Ambul Care Manage 2012; 35: 216–25 [DOI] [PubMed] [Google Scholar]
- 12. Department of Health. Accident and emergency provisional quality indicators. 2011. See http://www.dh.gov.uk/health/2011/08/accident-and-emergency-provisional-quality-indicators/ (last checked 8 April 2013)
- 13. Adastra AHC. Clinical patient management system, 2012. See http://www.advancedcomputersoftware.com/ahc/products/adastra-patient-management-system.php (last checked 8 April 2013)
- 14. Ascribe Symphony. Emergency departments and minor injuries, 2012. See http://www.ascribe.com/solutions-services/Pages/Ascribe-Symphony.aspx (last checked 8 April 2013)
- 15. Saboor SF, Ammenwerth E, Ammenwerth E. Categorizing communication errors in integrated hospital information systems. Methods Inf Med 2009; 48: 203–10 [DOI] [PubMed] [Google Scholar]
- 16. Pape UJ, Millet C, Lee JT, Car J, Majeed A. Disentangling secular trends and policy impacts in health studies: use of interrupted time series analysis. J R Soc Med 2013;106:124–129. [DOI] [PMC free article] [PubMed]
- 17. Roberts E, Mays N. Can primary care and community-based models of emergency care substitute for the hospital accident and emergency (A&E) department? Health Policy 1998; 44: 191–214 [DOI] [PubMed] [Google Scholar]
- 18. Boeke AJP. Effectiveness of GPs in accident and emergency departments. Br J Gen Pract 2010; 60: e378–e378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lowy A, Kohler B, Nicholl J. Attendance at accident and emergency departments: unnecessary or inappropriate? J Public Health 1994; 16: 134–40 [DOI] [PubMed] [Google Scholar]
- 20. Salisbury C, Chalder M, Scott TM, Pope C, Moore L. What is the role of walk-in centres in the NHS? BMJ 2002; 324: 399–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Majeed A, Molokhia M. Primary care in the United Kingdom. J Ambul Care Manage 2008; 31: 198–200 [DOI] [PubMed] [Google Scholar]