Abstract
Background
The associations between breast tenderness during use of conjugated equine estrogen (CEE) therapy with or without medroxyprogesterone (MPA) therapy and subsequent breast cancer risk are unknown.
Methods
We analyzed data from the Women’s Health Initiative Estrogen plus Progestin (N = 16,608, 5.6 years intervention) and Estrogen-Alone (N = 10,739, 6.8 years intervention) clinical trials until trial close-out (Spring 2005). At baseline and annually, participants underwent mammography and clinical breast exam. Self-reported breast tenderness was assessed at baseline and 12 months. Invasive breast cancer was confirmed by medical record review.
Results
The risk of new-onset breast tenderness after 12 months was significantly higher among women assigned to active therapy than placebo (CEE alone vs. placebo risk ratio [RR] 2.15, 95% confidence interval [CI] 1.97–2.35; CEE + MPA vs. placebo RR 3.07, 95% CI 2.85–3.30). CEE + MPA doubled the risk of invasive breast cancer among women with baseline breast tenderness (hazard ratio [HR] 2.16, 95% CI 1.29–3.74), but had a smaller effect among women without baseline breast tenderness (HR 1.17; 95%CI 0.97–1.41). New-onset breast tenderness was associated with a higher risk of breast cancer among women assigned to CEE + MPA (HR 1.33, 95% CI 1.02–1.72, P=0.03), but not among women assigned to CEE alone (HR 0.98, 95% CI 0.62–1.53).
Conclusions
New-onset breast tenderness during use of CEE + MPA was associated with increased subsequent breast cancer risk. The association of CEE + MPA therapy with increased breast cancer risk was especially pronounced among women with baseline breast tenderness.
Keywords: breast tenderness, breast cancer, menopausal hormone therapy, conjugated equine estrogens, medroxyprogesterone acetate
Introduction
Breast tenderness is a common adverse effect of menopausal hormone therapy. Although studies vary in timing and methods of assessment of breast tenderness during menopausal hormone therapy, the incidence of breast tenderness in double-blind randomized controlled trials ranges from approximately 8% to 15% after initiation of conjugated equine estrogen therapy (CEE) alone [1,2], and from 9%–16% after initiation of CEE combined with medroxyprogesterone acetate (MPA) [3,2,4–6]. Little is known about the predictors of new-onset breast tenderness during use of CEE-containing therapy [7]. Traditional clinical teaching considers menopausal hormone therapy-associated breast tenderness to be an annoying adverse effect that may resolve with cessation[8] or alteration of menopausal hormone therapy dose or preparation[9,10], but little attention has been given to the biology underlying, or the potential clinical relevance of, menopausal hormone therapy-associated breast tenderness.
New-onset breast tenderness during CEE + MPA therapy may be a clinical correlate of increasing mammographic density, a strong breast cancer risk factor [11,12]. In a prior study, women reporting new-onset breast tenderness during therapy 12 months after initiation of CEE and MPA had greater increases in mammographic density compared to women without new-onset breast tenderness [2].
Previously, using data from the Women’s Health Initiative (WHI) Estrogen + Progestin Trial, we published results linking the new-onset of breast tenderness during CEE + MPA therapy with an increased risk of breast cancer over 5.6 years of follow-up [13]. We now report the results of our study regarding new-onset breast tenderness and subsequent breast cancer risk among women receiving CEE alone in the WHI Estrogen Alone Trial. The association between new-onset breast tenderness and breast cancer risk during therapy with CEE alone has not previously been examined. Because CEE + MPA and CEE alone have differential effects on breast cancer risk [14–17], and on mammographic density [18–20], it is possible that new-onset breast tenderness has differential associations with breast cancer risk among women taking CEE alone compared to women taking CEE + MPA.
The goals of this study were 1. To determine the association between new-onset breast tenderness and breast cancer risk among women taking CEE alone, and 2. To determine whether the association between new-onset breast tenderness and increased breast cancer risk in the CEE + MPA Trial persists over extended follow-up (until trial close-out with 180 additional breast cancer cases).
Methods
Design of the WHI Estrogen-Alone and Estrogen + Progestin Clinical Trials
Previous publications describe the eligibility criteria and recruitment methods [21,15,16]. For each of the two trials, postmenopausal women aged 50 to 79 years were recruited at 40 clinical centers between 1993 and 1998. The WHI Estrogen + Progestin Trial recruited 16,608 postmenopausal women without a previous hysterectomy [14]. The WHI Estrogen-Alone Trial recruited 10,739 postmenopausal women with previous hysterectomy [22]. Participation required cessation of any menopausal hormone therapy for 3 months before randomization [22,14]. Before enrollment, all participants underwent clinical breast examination and mammograms; abnormal findings required clearance prior to study enrollment [22,14]. Each institution obtained human subjects committee approval. Each participant provided written informed consent. The trials were registered at ClinicalTrials.gov (ClinicalTrials.gov Identifier NCT00000611.
In the Estrogen + Progestin Trial, participants were randomly assigned to receive conjugated equine estrogens 0.625mg + medroxyprogesterone acetate 2.5 mg daily (n = 8506) or placebo (n = 8102). In the Estrogen-Alone Trial, participants were randomly assigned to receive conjugated equine estrogens 0.625 mg daily (n = 5310) or placebo (n = 5429).
Clinical outcomes were assessed at 6-month intervals. Participants were required to undergo annual mammography and clinical breast examination for continued administration of study medication. Participants were clinically monitored regardless of medication adherence. The Estrogen + Progestin Trial intervention was stopped after a mean follow-up of 5.6 years because the incidence of breast cancer exceeded a predesignated stopping boundary, and a global index supported the finding that overall risks exceeded overall benefits [16]. The Estrogen-Alone Trial intervention was stopped after a mean follow-up of 6.8 years due to increased risk of stroke and low likelihood of cardioprotection [15]. Following cessation of intervention, annual mammography and participant follow-up continued on the same schedule until trial close-out (Spring 2005).
Assessment of invasive breast cancer
Breast cancer diagnoses were ascertained every 6 months by questionnaire, confirmed by local physician adjudication of medical records and pathology reports, and centrally adjudicated by trained coders using standards from the Surveillance, Epidemiology, and End Results system [14,23]. When study intervention ended (6.8 years for the Estrogen-Alone Trial, 5.2 years for the Estrogen + Progestin Trial), the numbers of invasive breast cancers centrally confirmed were 360 (206 among women assigned to CEE + MPA, 154 among women assigned placebo) in the Estrogen + Progestin Trial, and 239 (104 among women assigned to CEE, 135 among women assigned to placebo) for the Estrogen-Alone Trial. Between the end of study intervention and trial close-out (Spring 2005), the numbers of additional invasive breast cancers that were centrally confirmed were 153 (87 among women assigned to CEE + MPA, 66 among women assigned to placebo) in the Estrogen + Progestin Trial, and 27 (13 among women assigned to CEE, 14 among women assigned to placebo) for the Estrogen-Alone trial.
Assessment of breast tenderness
At baseline and at 12-month follow-up, breast tenderness was assessed using self-assessment questionnaires [24,25]. Degree of bother from breast tenderness during the past 4 weeks was rated with a 4-point Likert-type scale as: symptoms did not occur, symptom was mild (did not interfere with usual activities), symptom was moderate (interfered somewhat with usual activities), or symptom was severe (so bothersome that usual activities could not be pursued). We classified participants as having new-onset breast tenderness if they reported the absence of breast tenderness at baseline and the presence of breast tenderness (mild, moderate, or severe) at the first annual follow-up.
Other questionnaire-based measurements and anthropomorphic measurements
At baseline, participants were asked to fill standardized self-report questionnaires regarding breast cancer risk factors, medical and reproductive history, medication use (including previous menopausal hormone therapy use), prior breast biopsies, family medical history, previous hysterectomy and/or oophorectomy, cigarette smoking, alcohol intake, caffeine intake, menopausal vasomotor symptoms, race/ethnicity, education, income, and physical activity. Energy expenditure from recreational physical activity was estimated from the validated WHI Physical Activity Questionnaire [26–28].
Age at menopause was defined as the lowest of: 60 years, the age at which a woman had last had menstrual bleeding, the age at which a woman had undergone bilateral oophorectomy, or the age at which a woman had begun using postmenopausal hormone therapy [29]. Age at menopause was considered missing if ages at last menstrual bleeding, bilateral oophorectomy, and menopausal hormone therapy initiation were each unavailable. For women who had undergone hysterectomy without bilateral oophorectomy, age at menopause was defined as the lowest of: age 60, the age of onset of hot flashes or night sweats, the age at which she began taking menopausal hormone therapy, or the age at hysterectomy. Gail breast cancer risk score was calculated using baseline questionnaire information [30,31].
Using standardized protocols, baseline height and weight were directly measured for calculation of body mass index (BMI, weight in kilograms divided by height in meters squared).
Statistical analysis
All primary analyses were conducted on the intention-to-treat principle. Baseline characteristics were compared in women with and without new-onset breast tenderness at year 1 using χ2 tests of association, and adjusting for age and treatment assignment. We determined the relative risk of new-onset breast tenderness of any severity (mild, moderate, or severe) at 12-month follow-up by randomization assignment using generalized linear models with a log link function. We compared the magnitudes of associations between treatment assignment and risk of new-onset breast tenderness between the two trials using Chi-squared tests.
We used multivariate Cox proportional hazards models to examine the association between new-onset breast tenderness and invasive breast cancer. We included baseline breast tenderness (yes/no), breast tenderness at year 1 as a time-dependent binary covariate X(t), and a time-dependent interaction term. Survival time was defined as the number of days after randomization to the first diagnosis of breast cancer and was censored at the time of a woman’s last documented follow-up contact or death. Baseline hazard was stratified by age group (50–54, 55–59, 60–69, or 70–79 years-old) and randomization assignment in the WHI Dietary Modification Trial. We included the following variables based on biological plausibility and/or published studies: randomization assignment, age (linear), ethnicity (white, black, American Indian, Asian Pacific Islander, or unknown), alcohol consumption (nondrinker, ≤ 1 drink daily, or > 1 drink daily), cigarette smoking (never, past, or current), BMI (linear and quartiles), energy expenditure from physical activity (metabolic equivalent hours per week, including walking and mild, moderate, and strenuous physical activity, linear and quartiles), parity, age at first birth, breastfeeding (never, ≤1 year, > 1 year), time since menopause (<5 or 5–<10 or 10–<15 or ≥15 years), Gail model breast cancer risk (linear and quartiles), bilateral oophorectomy (yes/no), and menopausal hormone therapy use prior to trial participation (yes/no) [7,6,32–42,25,43–47].
Multiple imputation was used to avoid deletion of observations with missing covariate values. Cox regression models were then fit for each of five imputed datasets, and the resulting regression parameter estimates were averaged for statistical inference. Data were too sparse to allow reliable sensitivity analysis among the subgroup of women who were adherent to (took ≥ 80% of) therapy.
All statistical tests were 2-sided. P values less than 0.05 were considered statistically significant. Statistical analyses were performed using SAS/STAT 9.2 (SAS Institute, Inc).
Results
At baseline, mean age of participants was 63.6 years. Seventy-five percent of participants were White. Forty-five percent of participants had BMI greater than 30. Characteristics linked with the reporting of new-onset breast tenderness at 12-month follow-up in the Estrogen-Alone Trial are displayed in Table 1. In the CEE and placebo groups combined, characteristics that were statistically significantly associated with new-onset breast tenderness included older age, treatment assignment (CEE versus placebo), lower BMI, greater years since menopause, and past use of estrogen therapy (Table 1). Characteristics associated with new-onset breast tenderness in the combined treatment groups of the Estrogen + Progestin Trial have been previously reported and were similar [13].
Table 1.
Baseline Characteristics of Participants in the WHI CEE-alone Trial by Breast Tenderness Status at Year 1*
| Characteristic | No tenderness at year 1 (N=6218) | Tenderness at year 1 (N=1793) | P† |
|---|---|---|---|
| Age at screening, mean (SD), y | 63.9 (7.2) | 64.6(7.2) | <0.001 |
| Treatment assignment, No. (%) | <0.001 | ||
| CEE Placebo | 3463 (55.7) | 575 (32.1) | |
| CEE Active | 2755 (44.3) | 1218 (67.9) | |
| Ethnicity, No (%) | 0.06 | ||
| White | 4926 (79.2) | 1382 (77.1) | |
| Black | 794 (12.8) | 260 (14.5) | |
| Hispanic | 280 (4.5) | 88 (4.9) | |
| American Indian | 39 (0.6) | 10 (0.6) | |
| Asian/Pacific Islander | 97 (1.6) | 24 (1.3) | |
| Unknown | 82 (1.3) | 29 (1.6) | |
| Daily alcohol intake, No. (%) | 0.66 | ||
| Non drinker | 3086 (49.9) | 913 (51.1) | |
| ≤ 1 drink | 2509 (40.5) | 716 (40.1) | |
| > 1 drink | 595 (9.6) | 158 (8.8) | |
| Smoking status, No. (%) | 0.27 | ||
| Never | 3165 (51.4) | 919 (51.6) | |
| Past | 2369 (38.5) | 710 (39.9) | |
| Current | 623 (10.1) | 151 (8.5) | |
| Regular cups of coffee/day, No. (%) | 0.41 | ||
| None | 2280 (37.0) | 650 (36.5) | |
| 1 | 917 (14.9) | 266 (14.9) | |
| 2 | 1253 (20.3) | 393 (22.1) | |
| ≥ 3 | 1712 (27.8) | 472 (26.5) | |
| BMI (kg/m2), No. (%) | 0.03 | ||
| < 25 | 1399 (22.6) | 359 (20.2) | |
| 25–<30 | 2168 (35.0) | 626 (35.1) | |
| 30–<35 | 1482 (23.9) | 467 (26.2) | |
| 35–<40 | 745 (12.0) | 227 (12.7) | |
| ≥40 | 396 (6.4) | 102 (5.7) | |
| Quartiles of physical activity, MET h/wk, No. (%) | 0.07 | ||
| < 1.5 | 1458 (25.7) | 447 (27.2) | |
| 1.5 to 6.5 | 1517 (26.7) | 446 (27.1) | |
| 6.5 to 15.75 | 1390 (24.5) | 417 (25.4) | |
| ≥ 15.75 | 1311 (23.1) | 333 (20.3) | |
| Parity, No. (%) | 0.56 | ||
| Never pregnant/Never had term pregnancy | 567 (9.2) | 154 (8.6) | |
| 1 | 482 (7.8) | 129 (7.2) | |
| 2 | 1248 (20.2) | 377 (21.1) | |
| ≥3 | 3883 (62.8) | 1126 (63.0) | |
| Age at first birth, No, (%) | 0.90 | ||
| Never pregnant/never had term pregnancy | 567 (10.1) | 154 (9.7) | |
| < 20 years | 1327 (23.5) | 365 (23.1) | |
| 20 – 29 years | 3453 (61.2) | 984 (62.2) | |
| ≥ 30 years | 291 (5.2) | 80 (5.1) | |
| Age at menarche, No. (%) | 0.04 | ||
| <12 years | 1455 (23.5) | 387 (21.6) | |
| 12–13 years | 3281 (53.0) | 1012 (56.6) | |
| ≥14 years | 1458 (23.5) | 389 (21.8) | |
| Years since menopause, No. (%) | 0.01 | ||
| <5 | 354 (6.7) | 89 (5.8) | |
| 5–10 | 585 (11.1) | 122 (7.9) | |
| 11–14 | 847 (16.1) | 232 (15.0) | |
| ≥15 | 3474 (66.0) | 1101 (71.3) | |
| Prior benign breast disease, No. (%) | <0.001 | ||
| Never | 4589 (81.8) | 1263 (77.9) | |
| 1 biopsy | 755 (13.5) | 255 (15.7) | |
| 2+ biopsies | 264 (4.7) | 103 (6.4) | |
| Family history of female relative w/breast cancer, No. (%) | 980 (16.7) | 324 (19.3) | 0.01 |
| Bilateral oophorectomy, No. (%) | 2374 (41.1) | 701 (41.8) | 0.69 |
| Age when both ovaries removed, No. | 0.17 | ||
| < 40 years | 598(25.4) | 200 (28.8) | |
| 40–49 years | 1161 (49.4) | 323 (46.5) | |
| 50–54 years | 355 (15.1) | 95 (13.7) | |
| ≥ 55 years | 237 (10.1) | 76 (11.0) | |
| Age at hysterectomy, No. (%) | 0.14 | ||
| < 40 years | 2340 (37.9) | 694 (38.9) | |
| 40–49 years | 2691 (43.6) | 775 (43.4) | |
| 50–54 years | 648 (10.5) | 182 (10.2) | |
| ≥ 55 years | 500 (8.1) | 135 (7.6) | |
| Duration of breastfeeding, No. (%) | 0.52 | ||
| Never | 2893 (47.3) | 797 (45.3) | |
| ≤ 1 year | 2375 (38.8) | 703 (39.9) | |
| > 1 year | 850 (13.9) | 260 (14.8) | |
| Quartiles of 5-year Gail model risk scores, | 0.29 | ||
| No. (%) | |||
| < 1.1 | 1583 (25.5) | 442 (24.7) | |
| 1.1 to < 1.44 | 1574 (25.3) | 418 (23.3) | |
| 1.44 to < 1.91 | 1547 (24.9) | 453 (25.3) | |
| ≥ 1.91 | 1514 (24.3) | 480 (26.8) | |
| Pre-trial use of estrogen therapy, No. (%) | 0.01 | ||
| Never used | 3310 (53.2) | 951 (53.1) | |
| Past user | 2097 (33.7) | 657 (36.7) | |
| Current user | 810 (13.0) | 184 (10.3) | |
| Pre-trial use of estrogen + progesterone* therapy, No. (%) | 0.72 | ||
| Never used | 5944 (95.6) | 1715 (95.6) | |
| Past user | 243 (3.9) | 68 (3.8) | |
| Current user | 31 (0.5) | 10 (0.6) |
Of the 10739 WHI CEE-alone trial participants, information regarding baseline and year 1 breast tenderness was available for 9620 participants. Thus, this table excludes participants for whom information regarding breast tenderness was missing from the baseline visit (n=86), the year 1 visit (n=1014), and both (n=19).
Compares baseline characteristics of participants without vs with new-onset breast tenderness after adjustment for age and treatment assignment. Tests of association for age and treatment assignment are unadjusted.
Self-reported at screening interview
The prevalence of breast tenderness at baseline in the CEE-Alone Trial was 17.4% in women assigned to placebo and 16.8% in women assigned to CEE. The prevalence of breast tenderness at baseline in the CEE + MPA trial was 11.8 % in women assigned to placebo and 11.8 % in women assigned to CEE + MPA.
Women assigned to either of the active therapies were at higher risk of developing breast tenderness at Year 1 compared to women assigned to placebo, and the effect of CEE+MPA (relative risk [RR] 2.40; 95% confidence interval [95% CI] 2.26–2.54) was significantly larger (Phet <0.001) than the effect of CEE alone (RR 1.73; 95%CI 1.62–1.84) (Table 2). The increased risk of breast tenderness at year 1 with active therapy vs. placebo was significantly modified by baseline breast tenderness (P-interaction < 0.001). Again, the effects differed between active therapies (Phet < 0.001), where the risk of new-onset breast tenderness tripled for CEE+MPA (RR 3.07; 95%CI 2.85–3.30) and doubled for CEE (RR 2.15; 95%CI 1.97–2.35) compared to placebo. Among women experiencing breast tenderness at baseline, the risk of breast tenderness at Year 1 was approximately 25% higher for both active therapies compared to placebo.
Table 2.
Prevalence and Relative Risk of Breast Tenderness at the First Annual Follow-up Visit in the WHI Hormone Therapy Trials*
| CEE-Alone | CEE+MPA | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Subgroup | Active | Placebo | P-value‡ | Active | Placebo | P-Value | P-Het§ | ||||||||
| N | (%)** | N | (%) | RR† | (95% CI) | (%) | N | (%) | N | (%) | RR | (95% CI) | |||
|
| |||||||||||||||
| Active vs. placebo: All participants | 1771 | (36.9) | 1047 | (21.4) | 1.73 | (1.62, 1.84) | <0.001 | 3086 | (39.5) | 1230 | (16.5) | 2.40 | (2.26, 2.54) | <0.001 | < 0.001 |
|
| |||||||||||||||
| Breast tenderness at baseline | <0.001 | <0.001 | <0.001 | ||||||||||||
| No | 1218 | (30.7) | 575 | (14.2) | 2.15 | (1.97, 2.35) | 2477 | (36.1) | 770 | (11.8) | 3.07 | (2.85, 3.30) | |||
| Yes | 537 | (68.5) | 462 | (56.0) | 1.22 | (1.13, 1.32) | 589 | (65.8) | 448 | (52.2) | 1.26 | (1.17, 1.37) | |||
N = 8011 for Estrogen-Alone Trial and N = 13,423 for the Estrogen + Progestin Trial
Relative risk of breast tenderness at 12-month follow-up from a generalized linear model.
P-values for main effect of treatment (boldface) and for interaction between treatment assignment and baseline breast tenderness.
Test of whether estimated RR differs between WHI Hormone Therapy Trials.
Percent reporting breast tenderness at 12-month follow-up.
Published results of the WHI Hormone Trials have shown that the use of CEE + MPA increases the risk of invasive breast cancer, but use of CEE alone does not [14–17]. Subgroup analyses show that the effect of CEE + MPA was significantly modified by baseline breast tenderness (Pint = 0.03, Table 3), where CEE + MPA doubled the risk of invasive breast cancer among women with baseline breast tenderness (hazard ratio [HR] 2.16, 95% CI 1.29–3.74), but had a smaller effect among women without baseline breast tenderness (HR 1.17; 95%CI 0.97–1.41). Further stratification by prior hormone use (Pint = 0.04) showed that the impact of breast tenderness on the effect of CEE + MPA was especially pronounced among women with baseline breast tenderness who had not previously used menopausal hormone therapy (HR 2.29, 95% CI 1.21–4.56). Breast tenderness was only rarely moderate or severe in intensity, but the risk of breast cancer associated with CEE + MPA appeared to increase with severity of breast tenderness at baseline (Ptrend = 0.02). There was no conclusive evidence that breast tenderness at baseline modified the effect of CEE (Pint = 0.37), even when results were further stratified by prior menopausal hormone therapy use (Pint = 0.13) or by severity of baseline breast tenderness (Ptrend = 0.53).
Table 3.
Risk of Invasive Breast Cancer (Randomization through Close-Out according to baseline breast tenderness and prior menopausal hormone therapy in the WHI Hormone Trials
| Subgroup | CEE Trial | CEE+MPA Trial | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| CEE | Placebo | P† | CEE+MPA | Placebo | P | ||||||||||
| N | (%)‡ | N | (%) | HR* | (95% CI) | N | (%) | N | (%) | HR | (95% CI) | ||||
|
| |||||||||||||||
| Active vs. placebo: All participants | 117 | (0.28) | 149 | (0.35) | 0.81 | (0.63, 1.03) | 0.08 | 293 | (0.43 | 221 | (0.34) | 1.25 | (1.05, 1.49) | 0.01 | |
|
| |||||||||||||||
| Breast tenderness at baseline | 0.37 | 0.03 | |||||||||||||
| No | 91 | (0.26) | 125 | (0.35) | 0.75 | (0.57, 0.98) | 246 | (0.41) | 199 | (0.35) | 1.17 | (0.97, 1.41) | |||
| Yes | 24 | (0.34) | 23 | (0.31) | 1.00 | (0.56, 1.79) | 45 | (0.56) | 20 | (0.27) | 2.16 | (1.29, 3.74) | |||
| Breast tenderness at baseline by prior MHT§ | 0.13 | 0.04 | |||||||||||||
| No breast tenderness/No prior MHT | 42 | (0.23) | 75 | (0.42) | 0.56 | (0.38, 0.82) | 176 | (0.40) | 160 | (0.38) | 1.05 | (0.85, 1.30) | |||
| No breast tenderness/prior MHT | 49 | (0.29) | 50 | (0.29) | 1.02 | (0.69, 1.52) | 70 | (0.45) | 39 | (0.27) | 1.63 | (1.11, 2.44) | |||
| Breast tenderness/No prior MHT | 15 | (0.40) | 14 | (0.39) | 1.02 | (0.49, 2.15) | 31 | (0.55) | 13 | (0.24) | 2.29 | (1.21, 4.56) | |||
| Breast tenderness/prior MHT | 9 | (0.27) | 9 | (0.24) | 1.09 | (0.42, 2.80) | 14 | (0.58) | 7 | (0.32) | 1.80 | (0.74, 4.76) | |||
| Severity of Breast tenderness at baseline | 0.53 | 0.02 | |||||||||||||
| No breast tenderness | 91 | (0.26) | 125 | (0.35) | 0.75 | (0.57, 0.98) | 246 | (0.41) | 199 | (0.35) | 1.17 | (0.97, 1.41) | |||
| Mild tenderness | 20 | (0.36) | 18 | (0.30) | 1.14 | (0.60, 2.17) | 37 | (0.54) | 18 | (0.28) | 1.96 | (1.13, 3.54) | |||
| Moderate/severe tenderness | 4 | (0.27) | 5 | (0.37) | 0.64 | (0.16, 2.43) | 8 | (0.70) | 2 | (0.19) | 4.55 | (1.09, 30.82) | |||
Hazard ratio from Cox proportional hazards models stratified by age, WHI Dietary Modification Trial treatment assignment, and subgroup.
P-values for main effect of treatment (boldface) and for interaction between treatment assignment and subgroup.
Annualized percentage.
MHT = menopausal hormone therapy
Table 4 shows multivariable-adjusted associations between new-onset breast tenderness and the subsequent risk of invasive breast cancer. Before stratification by treatment assignment, new-onset breast tenderness was not statistically significantly associated with risk of breast cancer in the Estrogen-alone Trial or in the Estrogen + Progestin Trial. In the participants who were assigned to CEE + MPA, new-onset breast tenderness was associated with a statistically significantly increased breast cancer risk (hazard ratio 1.33, 95% confidence interval 1.02–1.72). In contrast, in the participants who were assigned to active therapy with CEE alone, new-onset breast tenderness was not statistically significantly associated with breast cancer risk (hazard ratio 0.98, 95% confidence interval 0.62–1.53).
Table 4.
Annualized Rates and Multivariable-Adjusted Risk of Invasive Breast Cancer Among women with and without New-Onset Breast Tenderness at 12-Month Follow-up in the WHI Estrogen-Alone and Estrogen + Progestin Trials
| HT Trial Arm | CEE Trial | CEE+MPA Trial | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Experienced new-onset breast tenderness | Did not experience new- onset breast tenderness | HR† | (95% CI) | P‡ | Experienced new-onset breast tenderness | Did not experience new- onset breast tenderness | HR | (95% CI) | P | ||||||
| Cases (N at risk) | (%)* | Cases (N at risk) | (%) | Cases (N at risk) | (%) | Cases (N at risk) | (%) | ||||||||
|
| |||||||||||||||
| All participants (Active and placebo) | 42 (1779) | (0.34) | 158 (6202) | (0.30) | 1.04 | (0.74, 1.48) | 0.81 | 116 (3231) | (0.51) | 301 (10149) | (0.35) | 1.22 | (0.97, 1.53) | 0.09 | |
|
| |||||||||||||||
| Active | 22 (1208) | (0.26) | 62 (2748) | (0.26) | 0.98 | (0.62, 1.53) | 0.92 | 93 (2471) | (0.53) | 141 (4380) | (0.37) | 1.33 | (1.02, 1.72) | 0.03 | |
| Placebo | 20 (571) | (0.50) | 96 (3454) | (0.34) | 1.15 | (0.70, 1.88) | 0.57 | 23 (760) | (0.43) | 160 (5769) | (0.34) | 1.07 | (0.70, 1.63) | 0.76 | |
Annualized rates
Hazard ratio from Cox proportional hazards models comparing risk of breast cancer among women with versus without new-onset breast tenderness. Cox proportional hazards models are adjusted for HT randomization assignment, age, ethnicity, alcohol consumption, smoking, body mass index (linear and quartiles), physical activity (linear and quartiles), parity, age at first birth, breast feeding, years of age at menopause, Gail model breast cancer risk (linear and quartiles), bilateral oophorectomy, menopausal hormone therapy use prior to trial participation. This table displays hazard ratios for women without baseline breast tenderness.
P-values for comparison of hazard ratios among women with new-onset breast tenderness and women without new-onset breast tenderness.
Kaplan-Meier curves illustrate the temporal patterns of associations between new-onset breast tenderness and breast cancer risk for the active therapy arms of both trials (Fig. 1). The curves for women on with new-onset breast tenderness and without new-onset breast tenderness during CEE + MPA use do not appear to converge.
Figure 1.
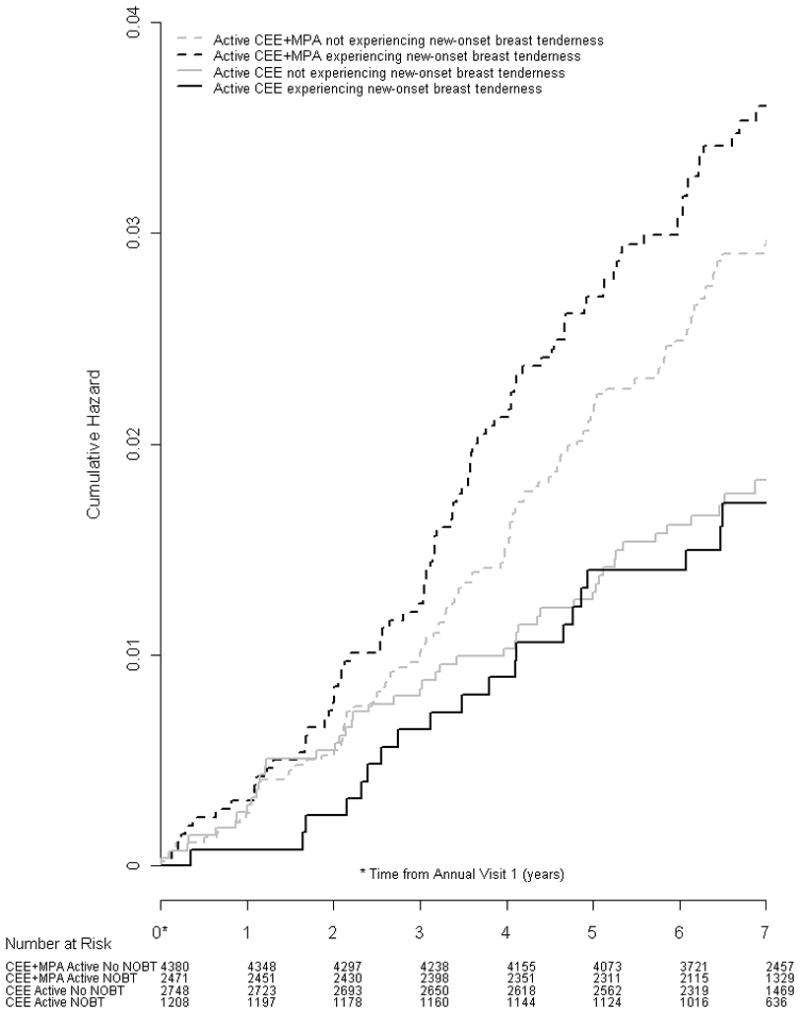
Cumulative hazard of breast cancer according to presence vs. absence of new-onset breast tenderness in the active therapy arms of the WHI CEE + MPA and CEE-Alone trials.
Discussion
The current study shows the potential relevance of breast tenderness symptoms prior to, and during administration of, menopausal hormone therapy. Among women with baseline breast tenderness, being assigned to CEE + MPA was associated with a doubling of the risk of invasive breast cancer compared to placebo. The increased risk of invasive breast cancer associated with use of CEE + MPA was attenuated among women without baseline breast tenderness. This effect modification could not be explained by prior menopausal hormone use, and appeared to increase with the severity of baseline breast tenderness. In contrast, the effect of CEE alone on breast cancer risk did not vary by the presence of breast tenderness before randomization.
Both CEE alone and CEE + MPA significantly increased risks of new-onset breast tenderness, but the effect of CEE + MPA was significantly greater than that of CEE alone. These results are intriguing, given similar effects of CEE alone and CEE + MPA on serum levels of estrone, estradiol, and sex hormone binding-globulin [48]. The development of new-onset breast tenderness after initiation of CEE + MPA, but not of CEE-alone, was associated with a statistically significantly higher subsequent risk of breast cancer.
The differential associations between new-onset breast tenderness and breast cancer risk among women assigned to active therapy in the CEE alone and CEE + MPA trials may be consistent with known differential effects of CEE and CEE + MPA on breast cancer risk, mammographic density, and breast tenderness. In the WHI, women assigned to CEE alone for a mean of 7.1 years had a 23% lower risk of breast cancer than women assigned to placebo at 10.7 years of follow-up (P = 0.02), whereas women assigned to CEE + MPA had a 24% (P < 0.001) higher risk of breast cancer than women assigned to placebo after a mean of 5.6 years of follow-up [15,17,14,16,49]. In addition, in prior studies from the Estrogen-Alone and Estrogen + Progestin Trials, mammographic breast cancer detection was not substantially compromised by use of CEE alone, but was comprised by use of CEE + MPA [22]. Moreover, the effects of CEE + MPA on mammographic density [20,18,19] and breast tenderness [2,25] are more pronounced than those of CEE alone.
An experience of breast tenderness could theoretically cause change in behavior, such as increased frequency of breast self-exam, or increased frequency of mammography, which could result in increased breast cancer diagnoses. We would have expected this change in behavior to similarly affect participants of both trials, and therefore this potential behavior change would not explain the differential associations of new-onset breast tenderness and breast cancer in the two trials.
Our study has several limitations. The occurrence of breast tenderness that resolved prior to the first annual visit would have led us to underestimate the incidence of breast tenderness. On the other hand, this ascertainment method probably mimics the way in which adverse effects are assessed in clinical settings. Also, discontinuation of CEE by some participants assigned to CEE may have led to an attenuation of the observed association of new-onset breast tenderness with breast cancer risk
Strengths of this study include the large number of participants, comprehensive assessment of breast cancer risk factors, rigorous ascertainment of breast cancer outcomes, blinding of participants and investigators to treatment assignment group, the requirement for annual mammography and clinical breast exam, the prospective blinded assessment of breast tenderness in the placebo and treatment groups, and longitudinal follow-up. To our knowledge, the WHI clinical trials were the largest and longest randomized controlled trials of menopausal hormone therapy ever performed.
In conclusion, among women assigned to CEE + MPA, but not among women assigned to CEE alone, the development of new-onset breast tenderness was associated with a significantly higher risk of breast cancer. The association of CEE + MPA therapy with increased breast cancer risk was especially pronounced among women with baseline breast tenderness. These findings highlight the complexity inherent in the use of surrogate risk markers to assess menopausal hormone therapy-associated breast cancer risk.
Acknowledgments
Funding
Dr. Crandall’s work was supported by the Eileen Ogle Award of the Iris Cantor-UCLA Women’s Health Center.
The WHI program is funded by National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services contracts N01WH22110, 24152, 32100-2, 32105-6, 32108-9, 32111-13, 32115, 32118-32119, 32122, 42107-26, 42129-32, and 44221.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all of the data and had final responsibility for the decision to submit for publication.
Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Joan McGowan, Leslie Ford, and Nancy Geller. Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Ross Prentice, Garnet Anderson, Andrea LaCroix, Charles L. Kooperberg; (Medical Research Labs, Highland Heights, KY) Evan Stein; (University of California at San Francisco, San Francisco, CA) Steven Cummings. Clinical Centers: (Albert Einstein College of Medicine, Bronx, NY) Sylvia Wassertheil- Smoller; (Baylor College of Medicine, Houston, TX) Haleh Sangi-Haghpeykar; (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (Brown University, Providence, RI) Charles B. Eaton; (Emory University, Atlanta, GA) Lawrence S. Phillips; (Fred Hutchinson Cancer Research Center, Seattle, WA) Shirley Beresford; (George Washington University Medical Center, Washington, DC) Lisa Martin; (Los Angeles Biomedical Research Institute at Harbor- UCLA Medical Center, Torrance, CA) Rowan Chlebowski; (Kaiser Permanente Center for Health Research, Portland, OR) Erin LeBlanc; (Kaiser Permanente Division of Research, Oakland, CA) Bette Caan; (Medical College of Wisconsin, Milwaukee, WI) Jane Morley Kotchen; (MedStar Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Northwestern University, Chicago/Evanston, IL) Linda Van Horn; (Rush Medical Center, Chicago, IL) Henry Black; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (State University of New York at Stony Brook, Stony Brook, NY) Dorothy Lane; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Alabama at Birmingham, Birmingham, AL) Cora E. Lewis; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of California at Davis, Sacramento, CA) John Robbins; (University of California at Irvine, CA) F. Allan Hubbell; (University of California at Los Angeles, Los Angeles, CA) Lauren Nathan; (University of California at San Diego, LaJolla/Chula Vista, CA) Robert D. Langer; (University of Cincinnati, Cincinnati, OH) Margery Gass; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Hawaii, Honolulu, HI) J. David Curb; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Massachusetts/Fallon Clinic, Worcester, MA) Judith Ockene; (University of Medicine and Dentistry of New Jersey, Newark, NJ) Norman Lasser; (University of Miami, Miami, FL) Mary Jo O’Sullivan; (University of Minnesota, Minneapolis, MN) Karen Margolis; (University of Nevada, Reno, NV) Robert Brunner; (University of North Carolina, Chapel Hill, NC) Gerardo Heiss; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (University of Tennessee Health Science Center, Memphis, TN) Karen C. Johnson; (University of Texas Health Science Center, San Antonio, TX) Robert Brzyski; (University of Wisconsin, Madison, WI) Gloria E. Sarto; (Wake Forest University School of Medicine, Winston-Salem, NC) Mara Vitolins; (Wayne State University School of Medicine/Hutzel Hospital, Detroit, MI) Michael S. Simon. Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker.
Footnotes
Author contributions
Conception and design: CC, AM
Collection and assembly of data: AA, JC, JM
Data analysis and interpretation: RC, AA, JC, GA, JM
Manuscript writing: all authors
Final approval of manuscript: all authors
Provision of study material of patients: JC
Conflicts of interest
CC: no conflicts of interest to declare
AA: no conflicts of interest to declare
JC: no conflicts of interest to declare
AM: consultant or advisory relationships: Novartis, Proctor and Gamble, Merck, Metagenics, Zymogenetic
stock ownership: Merck
honoraria: Wyeth, Novartis
research funding: Wyeth
JM: no conflicts of interest to declare
GA: expert testimony on behalf of Fred Hutchinson Cancer Research Center
RC: consultant or advisory relationships: Novartis, Pfizer, Astra Zeneca
Honoraria: Novartis, Astra Zeneca
Research funding: Amgen
Contributor Information
Carolyn J. Crandall, Email: ccrandall@mednet.ucla.edu.
Aaron K. Aragaki, Email: aaragaki@WHI.org.
Jane A. Cauley, Email: jcauley@edc.pitt.edu.
Anne McTiernan, Email: amctiern@fhcrc.org.
JoAnn E. Manson, Email: jmanson@rics.bwh.harvard.edu.
Garnet Anderson, Email: garnet@whi.org.
Rowan T. Chlebowski, Email: rowanchlebowski@gmail.com.
References
- 1.Brunner RL, Aragaki A, Barnabei V, Cochrane BB, Gass M, Hendrix S, Lane D, Ockene J, Woods NF, Yasmeen S, Stefanick M. Menopausal symptom experience before and after stopping estrogen therapy in the Women’s Health Initiative randomized, placebo-controlled trial. Menopause (New York, NY. 2010 doi: 10.1097/gme.0b013e3181d76953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crandall CJ, Karlamangla A, Huang MH, Ursin G, Guan M, Greendale GA. Association of new-onset breast discomfort with an increase in mammographic density during hormone therapy. Archives of internal medicine. 2006;166 (15):1578–1584. doi: 10.1001/archinte.166.15.1578. [DOI] [PubMed] [Google Scholar]
- 3.Utian WH, Shoupe D, Bachmann G, Pinkerton JV, Pickar JH. Relief of vasomotor symptoms and vaginal atrophy with lower doses of conjugated equine estrogens and medroxyprogesterone acetate. Fertil Steril. 2001;75(6):1065–1079. doi: 10.1016/s0015-0282(01)01791-5. S0015–0282(01)01791–5 [pii] [DOI] [PubMed] [Google Scholar]
- 4.Huber J, Palacios S, Berglund L, Hanggi W, Sathanandan SM, Christau S, Helmond F. Effects of tibolone and continuous combined hormone replacement therapy on bleeding rates, quality of life and tolerability in postmenopausal women. Bjog. 2002;109 (8):886–893. doi: 10.1111/j.1471-0528.2002.01338.x. [DOI] [PubMed] [Google Scholar]
- 5.Welton AJ, Vickers MR, Kim J, Ford D, Lawton BA, MacLennan AH, Meredith SK, Martin J, Meade TW. Health related quality of life after combined hormone replacement therapy: randomised controlled trial. BMJ (Clinical research ed. 2008;337:a1190. doi: 10.1136/bmj.a1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnabei VM, Cochrane BB, Aragaki AK, Nygaard I, Williams RS, McGovern PG, Young RL, Wells EC, O’Sullivan MJ, Chen B, Schenken R, Johnson SR. Menopausal symptoms and treatment-related effects of estrogen and progestin in the Women’s Health Initiative. Obstet Gynecol. 2005;105 (5 Pt 1):1063–1073. doi: 10.1097/01.AOG.0000158120.47542.18. [DOI] [PubMed] [Google Scholar]
- 7.Crandall CJ, Markovic D, Huang MH, Greendale GA. Predictors of breast discomfort among women initiating menopausal hormone therapy. Menopause. 2010;17(3):462–470. doi: 10.1097/gme.0b013e3181c29e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berek JS, Novak E. Berek & Novak’s gynecology. 14. Lippincott Williams & Wilkins; Philadelphia: 2007. [Google Scholar]
- 9.Speroff L, Fritz MA. Clinical gynecologic endocrinology and infertility. 7. Lippincott Williams & Wilkins; Philadelphia: 2005. [Google Scholar]
- 10.Strauss JF, Barbieri RL. Yen and Jaffe’s reproductive endocrinology: physiology, pathophysiology, and clinical management. 6. Saunders/Elsevier; Philadelphia, PA: 2009. [Google Scholar]
- 11.Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, Lockwood GA, Tritchler DL, Yaffe MJ. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995;87 (9):670–675. doi: 10.1093/jnci/87.9.670. [DOI] [PubMed] [Google Scholar]
- 12.Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, Hoover R, Haile R. Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995;87 (21):1622–1629. doi: 10.1093/jnci/87.21.1622. [DOI] [PubMed] [Google Scholar]
- 13.Crandall CJ, Aragaki AK, Chlebowski RT, McTiernan A, Anderson G, Hendrix SL, Cochrane BB, Kuller LH, Cauley JA. New-onset breast tenderness after initiation of estrogen plus progestin therapy and breast cancer risk. Archives of internal medicine. 2009;169(18):1684–1691. doi: 10.1001/archinternmed.2009.303. 169/18/1684 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, Rodabough RJ, Gilligan MA, Cyr MG, Thomson CA, Khandekar J, Petrovitch H, McTiernan A. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. Jama. 2003;289 (24):3243–3253. doi: 10.1001/jama.289.24.3243. [DOI] [PubMed] [Google Scholar]
- 15.Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, Chlebowski R, Curb D, Gass M, Hays J, Heiss G, Hendrix S, Howard BV, Hsia J, Hubbell A, Jackson R, Johnson KC, Judd H, Kotchen JM, Kuller L, LaCroix AZ, Lane D, Langer RD, Lasser N, Lewis CE, Manson J, Margolis K, Ockene J, O’Sullivan MJ, Phillips L, Prentice RL, Ritenbaugh C, Robbins J, Rossouw JE, Sarto G, Stefanick ML, Van Horn L, Wactawski-Wende J, Wallace R, Wassertheil-Smoller S. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. Jama. 2004;291 (14):1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 16.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. Jama. 2002;288 (3):321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 17.Stefanick ML, Anderson GL, Margolis KL, Hendrix SL, Rodabough RJ, Paskett ED, Lane DS, Hubbell FA, Assaf AR, Sarto GE, Schenken RS, Yasmeen S, Lessin L, Chlebowski RT. Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. Jama. 2006;295 (14):1647–1657. doi: 10.1001/jama.295.14.1647. [DOI] [PubMed] [Google Scholar]
- 18.McTiernan A, Chlebowski RT, Martin C, Peck JD, Aragaki A, Pisano ED, Wang CY, Johnson KC, Manson JE, Wallace RB, Vitolins MZ, Heiss G. Conjugated Equine Estrogen Influence on Mammographic Density in Postmenopausal Women in a Substudy of the Women’s Health Initiative Randomized Trial. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.21.7166. JCO.2008.21.7166 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McTiernan A, Martin CF, Peck JD, Aragaki AK, Chlebowski RT, Pisano ED, Wang CY, Brunner RL, Johnson KC, Manson JE, Lewis CE, Kotchen JM, Hulka BS. Estrogen-plus-progestin use and mammographic density in postmenopausal women: women’s health initiative randomized trial. J Natl Cancer Inst. 2005;97 (18):1366–1376. doi: 10.1093/jnci/dji279. [DOI] [PubMed] [Google Scholar]
- 20.Greendale GA, Reboussin BA, Slone S, Wasilauskas C, Pike MC, Ursin G. Postmenopausal hormone therapy and change in mammographic density. J Natl Cancer Inst. 2003;95 (1):30–37. doi: 10.1093/jnci/95.1.30. [DOI] [PubMed] [Google Scholar]
- 21.Design of the Women’s Health Initiative clinical trial and observational study. The Women’s Health Initiative Study Group. Controlled clinical trials. 1998;19 (1):61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 22.Chlebowski RT, Anderson G, Manson JE, Pettinger M, Yasmeen S, Lane D, Langer RD, Hubbell FA, McTiernan A, Hendrix S, Schenken R, Stefanick ML. Estrogen alone in postmenopausal women and breast cancer detection by means of mammography and breast biopsy. J Clin Oncol. 2010;28(16):2690–2697. doi: 10.1200/JCO.2009.24.8799. JCO.2009.24.8799 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, Johnson KC, Proulx-Burns L, Pastore L, Criqui M, Daugherty S. Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol. 2003;13(9 Suppl):S122–128. doi: 10.1016/s1047-2797(03)00048-6. S1047279703000486 [pii] [DOI] [PubMed] [Google Scholar]
- 24.Ganz PA, Day R, Ware JE, Jr, Redmond C, Fisher B. Base-line quality-of-life assessment in the National Surgical Adjuvant Breast and Bowel Project Breast Cancer Prevention Trial. J Natl Cancer Inst. 1995;87 (18):1372–1382. doi: 10.1093/jnci/87.18.1372. [DOI] [PubMed] [Google Scholar]
- 25.Greendale GA, Reboussin BA, Hogan P, Barnabei VM, Shumaker S, Johnson S, Barrett-Connor E. Symptom relief and side effects of postmenopausal hormones: results from the Postmenopausal Estrogen/Progestin Interventions Trial. Obstet Gynecol. 1998;92 (6):982–988. doi: 10.1016/s0029-7844(98)00305-6. [DOI] [PubMed] [Google Scholar]
- 26.Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, Siscovick DS. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–725. doi: 10.1056/NEJMoa021067. 347/10/716 [pii] [DOI] [PubMed] [Google Scholar]
- 27.Meyer AM, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the Women’s Health Initiative physical activity questionnaire. Med Sci Sports Exerc. 2009;41(3):530–538. doi: 10.1249/MSS.0b013e31818ace55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsia J, Wu L, Allen C, Oberman A, Lawson WE, Torrens J, Safford M, Limacher MC, Howard BV. Physical activity and diabetes risk in postmenopausal women. Am J Prev Med. 2005;28(1):19–25. doi: 10.1016/j.amepre.2004.09.012. S0749–3797(04)00252–1 [pii] [DOI] [PubMed] [Google Scholar]
- 29.Prentice RL, Manson JE, Langer RD, Anderson GL, Pettinger M, Jackson RD, Johnson KC, Kuller LH, Lane DS, Wactawski-Wende J, Brzyski R, Allison M, Ockene J, Sarto G, Rossouw JE. Benefits and risks of postmenopausal hormone therapy when it is initiated soon after menopause. Am J Epidemiol. 2009;170(1):12–23. doi: 10.1093/aje/kwp115. kwp115 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chlebowski RT, Anderson GL, Lane DS, Aragaki AK, Rohan T, Yasmeen S, Sarto G, Rosenberg CA, Hubbell FA. Predicting risk of breast cancer in postmenopausal women by hormone receptor status. J Natl Cancer Inst. 2007;99(22):1695–1705. doi: 10.1093/jnci/djm224. djm224 [pii] [DOI] [PubMed] [Google Scholar]
- 31.Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, Wieand HS. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst. 1999;91 (18):1541–1548. doi: 10.1093/jnci/91.18.1541. [DOI] [PubMed] [Google Scholar]
- 32.Bungay GT, Vessey MP, McPherson CK. Study of symptoms in middle life with special reference to the menopause. Br Med J. 1980;281 (6234):181–183. doi: 10.1136/bmj.281.6234.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davies EL, Gateley CA, Miers M, Mansel RE. The long-term course of mastalgia. Journal of the Royal Society of Medicine. 1998;91 (9):462–464. doi: 10.1177/014107689809100903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dennerstein L, Dudley EC, Hopper JL, Guthrie JR, Burger HG. A prospective population-based study of menopausal symptoms. Obstet Gynecol. 2000;96 (3):351–358. doi: 10.1016/s0029-7844(00)00930-3. [DOI] [PubMed] [Google Scholar]
- 35.Jensen J, Christiansen C. Effects of smoking on serum lipoproteins and bone mineral content during postmenopausal hormone replacement therapy. American journal of obstetrics and gynecology. 1988;159 (4):820–825. doi: 10.1016/s0002-9378(88)80144-3. [DOI] [PubMed] [Google Scholar]
- 36.Cassidenti DL, Vijod AG, Vijod MA, Stanczyk FZ, Lobo RA. Short-term effects of smoking on the pharmacokinetic profiles of micronized estradiol in postmenopausal women. American journal of obstetrics and gynecology. 1990;163 (6 Pt 1):1953–1960. doi: 10.1016/0002-9378(90)90780-b. [DOI] [PubMed] [Google Scholar]
- 37.Geisler J, Omsjo IH, Helle SI, Ekse D, Silsand T, Lonning PE. Plasma oestrogen fractions in postmenopausal women receiving hormone replacement therapy: influence of route of administration and cigarette smoking. J Endocrinol. 1999;162(2):265–270. doi: 10.1677/joe.0.1620265. JOE03234 [pii] [DOI] [PubMed] [Google Scholar]
- 38.Jensen J, Christiansen C, Rodbro P. Cigarette smoking, serum estrogens, and bone loss during hormone-replacement therapy early after menopause. N Engl J Med. 1985;313 (16):973–975. doi: 10.1056/NEJM198510173131602. [DOI] [PubMed] [Google Scholar]
- 39.McDivit AM, Greendale GA, Stanczyk FZ, Huang MH. Effects of alcohol and cigarette smoking on change in serum estrone levels in postmenopausal women randomly assigned to fixed doses of conjugated equine estrogens with or without a progestin. Menopause (New York, NY. 2008;15(2):382–385. doi: 10.1097/gme.0b013e3181407cb2. [DOI] [PubMed] [Google Scholar]
- 40.Carranza-Lira S, Garduno-Hernandez MP, Caisapanta DA, Aparicio H. Evaluation of mastodynia in postmenopausal women taking hormone therapy. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2005;89 (2):158–159. doi: 10.1016/j.ijgo.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 41.Ernster VL, Goodson WH, 3rd, Hunt TK, Petrakis NL, Sickles EA, Miike R. Vitamin E and benign breast “disease”: a double-blind, randomized clinical trial. Surgery. 1985;97 (4):490–494. [PubMed] [Google Scholar]
- 42.Girdler SS, O’Briant C, Steege J, Grewen K, Light KC. A comparison of the effect of estrogen with or without progesterone on mood and physical symptoms in postmenopausal women. Journal of women’s health & gender-based medicine. 1999;8 (5):637–646. doi: 10.1089/jwh.1.1999.8.637. [DOI] [PubMed] [Google Scholar]
- 43.McTiernan A, Tworoger SS, Ulrich CM, Yasui Y, Irwin ML, Rajan KB, Sorensen B, Rudolph RE, Bowen D, Stanczyk FZ, Potter JD, Schwartz RS. Effect of exercise on serum estrogens in postmenopausal women: a 12-month randomized clinical trial. Cancer Res. 2004;64 (8):2923–2928. doi: 10.1158/0008-5472.can-03-3393. [DOI] [PubMed] [Google Scholar]
- 44.Meyer EC, Sommers DK, Reitz CJ, Mentis H. Vitamin E and benign breast disease. Surgery. 1990;107 (5):549–551. [PubMed] [Google Scholar]
- 45.Yasui T, Uemura H, Umino Y, Takikawa M, Saito S, Kuwahara A, Matsuzaki T, Maegawa M, Furumoto H, Miura M, Irahara M. Serum estrogen level after hormone replacement therapy and body mass index in postmenopausal and bilaterally ovariectomized women. Maturitas. 2005;50(1):19–29. doi: 10.1016/j.maturitas.2004.03.013. S0378512204001197 [pii] [DOI] [PubMed] [Google Scholar]
- 46.American Cancer Society. Breast Cancer Racts & Figures 2009–2010. American Cancer Society, Inc; Atlanta, Georgia: 2009. [Google Scholar]
- 47.American Cancer Society. Cancer Facts & Figures 2010. Atlanta, Georgia: 2010. [Google Scholar]
- 48.Edlefsen KL, Jackson RD, Prentice RL, Janssen I, Rajkovic A, O’Sullivan MJ, Anderson G. The effects of postmenopausal hormone therapy on serum estrogen, progesterone, and sex hormone-binding globulin levels in healthy postmenopausal women. Menopause (New York, NY. 2010;17(3):622–629. doi: 10.1097/gme.0b013e3181cb49e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.LaCroix AZ, Chlebowski RT, Manson JE, Aragaki AK, Johnson KC, Martin L, Margolis KL, Stefanick ML, Brzyski R, Curb JD, Howard BV, Lewis CE, Wactawski-Wende J. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy: a randomized controlled trial. JAMA. 2011;305(13):1305–1314. doi: 10.1001/jama.2011.382. 305/13/1305 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]


