Abstract
Purpose
As mental illness stigma contributes to poor outcomes for schizophrenia in China, locating strategies to reduce public stigma is imperative. It is currently unknown whether diagnostic labeling and contact with different help-seeking sources increase or decrease public stigma in China. Further, it remains unresolved whether prior personal contact acts to reduce stigma in this context. Advancing understanding of these processes may facilitate stigma-reduction strategies.
Methods
We administered an experimental vignette randomly assigning one of four labeling conditions to respondents to assess social distance towards a psychotic vignette individual in a sample of 160 Northern, urban Chinese community respondents.
Results
As expected, respondents given a “non-psychiatric, indigenous label” + “lay help-seeking” condition endorsed the least social distance. Unexpectedly, the labeling condition with a “psychiatric diagnostic label” + “lay help-seeking” condition elicited the greatest social distance. Unlike Western studies, personal contact did not independently decrease community stigma. However, prior contact reduced social distance to a greater extent in the labeling condition with a “non-psychiatric, indigenous label” + “lay help-seeking” condition when compared with all other labeling conditions.
Conclusion
The results indicate that cultural idioms do provide some protection from stigma, but only among respondents who are already familiar with what mental illness is. Our finding that the condition that depicted untreated psychosis elicited the greatest amount of stigma, while the “treated psychosis” condition was viewed relatively benignly in China, suggests that improved access to mental health services in urban China has the potential to decrease public stigma via labeling mechanisms.
Keywords: Stigma, Culture, China, Schizophrenia, Attitudes
Introduction
Mental illness stigma in China
Community attitudes towards mental illness in Chinese societies—including Mainland China [1], Hong Kong [2], and Singapore [3]—have been described as particularly negative and severe [4, 5]. Comparative studies have indicated that respondents from Chinese groups endorse significantly greater negative stereotypes (e.g., unpredictability [6]) and pejorative attitudes (e.g., greater authoritarianism and social restrictiveness [7]) towards people with mental illness when compared with their Western counterparts [8–10]. Such negative attitudes give rise to discrimination that is commonly experienced by people with schizophrenia in China when their illness status is revealed [1]. These harmful conceptions might also lead to damaging internalization of stereotypes and a loss of self-esteem by people diagnosed with schizophrenia [2, 11–13] Cultural concerns of maintaining “face” further result in patients’ secrecy and poor treatment adherence [2]. Accordingly, mental illness stigma may at least partially contribute to the documented poor clinical and social outcomes of psychotic disorders in China [14].
A pressing issue thus is to locate strategies to successfully reduce public mental illness stigma in China. Given that mental illness “labeling” (i.e., via contact with psychiatric services) is a particularly salient mechanism by which stigma occurs [1], careful examination of these processes may yield important knowledge to decrease psychiatric stigma. The importance and complexity of this area is further highlighted by official efforts to rename schizophrenia with more benign diagnostic labels in Asian societies including Hong Kong [15] and Japan [16, 17] that have not achieved desired reductions in public stigma. The present study builds upon prior literature by investigating impacts upon community perceptions of stigma by varying both a commonly used indigenous label used to describe schizophrenia in China (“excessive thinking” [18, 19]) with a “schizophrenia” label and the source of that labeling (i.e., psychiatric vs. non-psychiatric). Further, the role of interpersonal contact with people with mental illness—which is acknowledged as one of the most effective means of countering stigma [20, 21]—is examined in relation to these labeling effects. Investigating this issue in China, where respondents may naturally utilize indigenous idioms to label schizophrenia, enables a novel test of whether prior contact consistently acts to decrease stigma towards symptomatic behavior, psychiatric labels, or both, or whether this association depends on ambient cultural circumstances. Advancing understanding of the labeling processes that ameliorate stigma may facilitate conceptualization and implementation of future stigma-reduction strategies in China.
Stigma and effects of diagnostic labeling
“Labeling”—or when people distinguish a human characteristic as significant and assign it a label—has been highlighted as a key mechanism in initiating stigma processes [22]. Goffman [23] proposed that stigma reduces the bearer from a whole person “to a tainted, discounted one” (p.3) via societal stereotypes that devalue an individual’s social identity in a particular context [24]. Accordingly, modified labeling theory [25] emphasizes that individuals as part of daily socialization internalize conceptions of what it means to be labeled with a psychiatric illness. These internalized notions consist of the extent to which community members believe that people with mental illness will be devalued and discriminated against. Since official labeling takes place through contact with psychiatric treatment and ensuing diagnosis, community perceptions of devaluation and discrimination become activated when individuals are labeled with mental illness. In addition to the stigma directly attributable to the patient’s disruptive behavior, effects from labeling have been found to add to community members’ rejecting social attitudes [26, 27]. Since the “schizophrenia” label elicits the most pejorative stereotypes, emotional responses, social distance, and pessimistic evaluations for recovery among all psychiatric conditions [28, 29], this label in particularly is likely to initiate negative stereotypes and subsequent rejecting responses.
In addition to the effects of diagnostic labeling, contact with different labeling sources (i.e., forms of help-seeking) appears to further modify potential stigma. Accordingly, entering mental health treatment (e.g., hospitalization in a psychiatric unit) for psychiatric difficulties has been perceived by community members as a more powerful “labeling event” than accessing other forms of treatment (e.g., Western general medical practitioner [30]). Labeling effects from treatment source might help account for individuals suffering from psychiatric difficulties preferring to access general medical practitioners for help rather than psychiatric sources [31, 32]. Although the effects of help-seeking source have yet to be established in China, the available evidence suggests that similar effects could be present. For example, Chinese Americans perceived greater community attitudes of shame when utilizing Western psychiatric services as opposed to traditional Chinese medical practitioners (i.e., those who use acupuncture, herbal medicine, or other physical treatments) to treat a mental disorder [33]. Further, Chinese Americans who reported depressive symptoms at a primary care clinic endorsed little stigma [34]. While consistent with modified labeling theory’s predictions that highlight the central role of psychiatric treatment contact in initiating stereotyping processes [25], key cultural dynamics within China may potentially allay the stigma associated with seeking psychiatric treatment. For example, stigma towards individuals exhibiting severe psychiatric symptoms but appropriately conforming to a “sick role” (i.e., seeking mental health care) might be ameliorated among Chinese by culturally driven preferences towards an increased adherence to social roles, obligations [35] and collective duties [36]. Thus, the comparative effects of diagnostic labeling, labeling source, and adherence to “role identities” [37] in shaping community attitudes towards mental illness have yet to be clarified within this context.
Indigenous explanations of schizophrenia as an alternative to diagnostic labels
An additional, but relatively unexamined, cultural process that might mitigate perceptions of stigma among Chinese groups are lay “explanatory models” or “indigenous idioms” of schizophrenia [38]. Indigenous idioms may reflect upon Western psychiatric classification of disease in complex ways. Frequently, indigenous idioms do not refer to psychiatric syndromes per se but instead to culturally formulated interpretations of illness [39]. While indigenous idioms reveal a pathway to viewing illness contextually, psychiatric nosology attempts to identify “basic” patterns of disorders in a manner that allows for these disorders to be examined independently and distinct from context [40] Yet, as cultural variation in the phenomenology of disorders has been acknowledged [41], cultural idioms might thus offer a way to contextualize and understand how specific diagnostic criteria might be interpreted and perceived within a specific cultural locale.
Accordingly, an individual’s understanding of and receptiveness towards mental illness can be shaped by these lay theories of mental illness, which consist of beliefs that are rooted in a society’s history, philosophy and culture [42, 43]. Specifically, in the Chinese context, a label of “excessive thinking” (xiang tai duo) or “an inability to let go of negative thoughts” might be applied to a person with schizophrenia symptoms, and this more benign label might positively influence community members’ levels of stigma and discrimination. “Excessive thinking” is considered one of the most commonly held causal beliefs of schizophrenia among Chinese groups. In one study conducted with relatives of schizophrenia patients in Mainland China, this idiom was endorsed by 25% of respondents to explain first psychiatric hospitalization [44]. Therefore, “excessive thinking” may be naturalistically used by Chinese community members as an indigenous label for psychotic symptomatology.
“Excessive thinking” shares similarities with the notion of “nerves” identified among North Americans (i.e., prone to worry over difficulties or being ill-tempered, hard to get along with, and possibly aggressive [45, 46]). Although unique indigenous terms may be used to describe behaviors associated with mental illness symptoms across different settings, they might share common functions across contexts. Specifically these concepts enable social group members to identify socially aberrant behavior while at the same time avoiding the classification of such behaviors as seriously deviant or psychopathological [19]. As such, these idioms may serve as a socially inclusive means of interpreting diverse (and commonly quite odd) behaviors that contrast with the exclusion associated with mental illness [45]. What provides these idioms’ normalizing power in their cultural setting is that behaviors associated with these idioms are perceived as occurring to varying degrees among all group members. Application of these idioms thus mitigates the strangeness of symptomatic behaviors and may diminish social rejection of individuals manifesting mental illness symptomatology but who have not yet received a formal psychiatric diagnosis [47].
Yet, “excessive thinking” also manifests several culturally specific characteristics. In a recent qualitative examination of this Chinese idiom, Yang and colleagues [19] found that in China, delusional thinking related to psychosis was often labeled and explained by using specific “expressive variants” of this excessive thinking construct. These variants consist of “inflexible and perseverative thinking” as well as “unwarranted suspicion of others” (see Table 1 for illustrations). The culturally specific features of the “excessive thinking” idiom among Chinese groups stems from its violation of the fundamental Chinese obligation to be restrained and moderate in one’s actions. But because “excessive thinking” is viewed as occurring across most individuals at least periodically, the use of these indigenous idioms of distress in Chinese groups allows for continued integration of mentally ill individuals into social groups. As described above, this practice is not unique to the Chinese context: the term nervios was identified among Mexican Americans to interpret schizophrenia-like symptoms along a continuum of normal behaviors [45]. Similarly, isamullatuq is used among Inuit Indians to describe the act of being “burdened down by thoughts” and serves as a culturally meaningful illness category for this group [48]. Yet, as detailed in Table 1, specific aspects of “excessive thinking” as formulated by lay conceptualizations may map onto particular features of schizophrenia symptomatology in Chinese groups because they share similar manifestations (i.e., “inflexible thinking” and “unwarranted suspicion”).
Table 1.
Illustrations of “expressive variants” of the excessive thinking idiom
| Type | Definition | Illustration |
|---|---|---|
| 1) Inflexible and perseverative thinking | ‘Taking things too much to heart’ captured the inflexible and perseverative quality of cognitions that typically accompanied delusional thinking | Because of buying the house for my Mom, [my wife] was [always] nagging. She said, “we took out all our savings and that was still not enough. We still had to borrow money, right?” She was then ruminating. Once thinking, she got herself into an insignificant problem and couldn’t get out. She couldn’t find her way out. She was then taking it too hard. I said, “Don’t be this way…” |
| 2) Unwarranted suspicion of others | Innocuous interpersonal events are mistakenly interpreted as having personal significance, illustrating how excessive thinking is commonly linked to paranoid psychosis | “[My neighbors] were doing construction at the back of the house. Hearing those banging noises, my wife became suspicious. They also owned a dog that would make noises sometimes. She thought that it barked on purpose… Sometimes we would joke about it with her…She thought that they did things on purpose [to irritate her]. In the beginning, we thought it was just her narrow-mindedness. Eventually, we realized that her frustration about the neighbor was growing more intense…” |
(Adapted from Yang et al. [19])
Endorsing the idiom of excessive thinking may plausibly ameliorate stigma among community members in the same manner as it initiates protective social effects for individuals with schizophrenia and their family members [47]. Chinese schizophrenia patients whose relatives attributed illness behaviors to excessive thinking showed fewer severe psychotic symptoms and re-hospitalizations over an 18-month period [18]. As Chinese individuals frequently utilize “excessive thinking” to explain aberrant behaviors, use of this idiom thus signals recognition of those exhibiting delusional thinking/behaviors as “full status” group members and provides a “social script” for accommodating behaviors. In a symbolic way, the utilization of this indigenous idiom by community members also conveys continued “moral status” or humanity [49], which allows communities to “hold onto” their members as one of their own. Therefore, the usage of this idiom may decrease mental health stigma in the community by legitimizing psychotic-like experiences and by shielding patients from the moral contamination and severe stigma that is associated with an official mental illness label [50].
Personal “contact” as a means of reducing stigma
Another critical process to consider in conjunction with labeling mechanisms is the effect of prior “personal contact”—or the disconfirmation of stigmatizing stereotypes via interaction with a person with mental illness—in reducing public stigma. Personal contact—unlike “impersonal” contact (i.e., merely observing people with mental illness in public)—has been found to consistently predict decreased stigma among community members [51] Personal contact has been heralded as the most promising strategy for reducing psychiatric stigma [21], with one review concluding that such contact tends to reduce stigmatizing views towards mental illness [52]. Unlike educational approaches alone, personal contact with people with mental illness has demonstrated lasting efficacy in decreasing stigmatizing attitudes [53]. In particular, social distance—or the unwillingness to engage in relationships of varying intimacy with a person [26]—has been found to decrease as personal contact increases [20, 54–59].
However, the majority of studies that demonstrate a link between interactive contact and reduced social distance towards people with mental illness have been conducted among Western groups [52]. While several studies among Chinese groups in Hong Kong report that increased personal contact led to less social distance and greater accepting attitudes of people with mental illness [60, 61], the evidence remains equivocal. For example, Callaghan and colleagues [62] found that previous personal contact with mental illness had no effect on decreasing psychiatric stigma among a sample of Chinese nursing students. One possible explanation for these inconsistent findings is that the severely marginalized status that people with mental illness occupy in Mainland China [1, 63] may provide few opportunities to interact with such individuals under conditions of equal status, thus undermining any beneficial effects that personal contact provides.
Another noteworthy, and unexamined, issue is whether the effects of personal contact remain constant even when alternative labels are utilized to describe individuals exhibiting psychiatric symptomatology. Prior personal contact is seen to result in positive perceptions towards the stigmatized individual that generalizes to more beneficial attitudes toward the stigmatized group as a whole [64]. Stigma might thus be seen to decrease towards both symptomatic behavior and the psychiatric label itself. However, this assumption has yet to be empirically tested. As indigenous idioms such as “excessive thinking” might plausibly be used to label schizophrenia within China, we make use of a novel opportunity to examine whether personal contact reduces stigma even when labels of symptomatology differ. As personal contact with a person with mental illness is seen to decrease stigma both towards the behaviors and label of schizophrenia, we would expect contact to decrease stigma among the schizophrenia labeling conditions to a greater extent when compared with an indigenous labeling condition.
Hypotheses
It is currently unknown whether a non-psychiatric diagnostic label and/or labeling source might act to mitigate or exacerbate the pre-existing severe stigma found among Chinese community groups. Replacing diagnostic labels and labeling sources with alternate but culturally indigenous labels might exert different effects among Chinese groups, who prize conformity towards social roles (i.e., a “patient” role) and fulfillment of collective obligations to a greater extent when compared with European-Americans [36]. This study seeks to investigate these important questions by examining whether varying the diagnostic label (“schizophrenia” vs. “excessive thinking”) and the labeling source (“psychiatrist” vs. “uncle”) of an individual exhibiting psychotic symptoms changes the degree of social distance endorsed among urban Chinese community respondents.
Although the effect of varying such labels among different cultural groups is not yet well understood, we offer the following hypotheses based on the substantial amount of literature to support such labeling effects in Western populations. First, based on our prior qualitative work in this area [19], we predict that both ‘excessive thinking’ and ‘mental illness’ labels will be endorsed by community respondents in their perceptions of psychotic symptomatology. Second, the use of a non-psychiatric diagnostic label (i.e., “excessive thinking”) and labeling source (i.e., “uncle”) to describe an individual manifesting psychotic symptomatology within a vignette will elicit the least social distance from community members when compared with psychiatric labeling conditions (i.e., “schizophrenia” and “psychiatrist”). Third, the condition utilizing both a psychiatric labeling source (i.e., “psychiatrist”) and a diagnostic label (i.e., “schizophrenia”) will result in greater social distance when compared with a ‘mixed’ condition of a non-psychiatric labeling source (i.e., “uncle”) when paired with a psychiatric diagnostic label (i.e., “schizophrenia”). Figure 1a provides an illustration of the main constructs identified in Hypotheses #2 and 3 and depicts how: (1) diagnostic label and treatment source interrelate to form one “Labeling” construct, which then impacts (2) social distance.
Fig. 1.
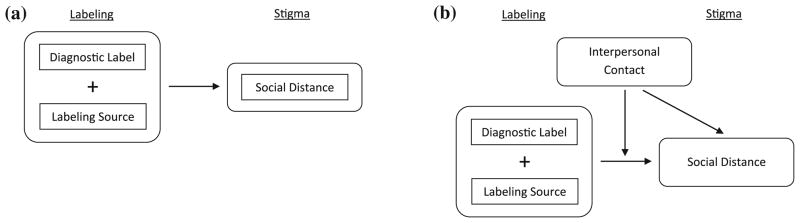
Illustrations of hypothesized relationships. a The combination of diagnostic label and labeling source elicits social distance, illustrating Hypotheses 2 and 3. b Personal contact has a direct effect on social distance and personal contact may differentially impact the way that diagnostic label and labeling source predicts social distance, illustrating Hypotheses 4 and 5
For our fourth hypothesis, based upon extensive literature among Western populations [52], personal contact is hypothesized to independently decrease community attitudes of social distance towards people with mental illness. Fifth, as personal contact is seen to decrease stigma both towards psychiatric behaviors and labels, contact will be expected to reduce stigma in the mental illness diagnostic labeling (“schizophrenia”) conditions, but not in the non-psychiatric diagnostic labeling (“excessive thinking”) condition. We thus test for an interaction between personal contact and labeling in the reduction of social distance. Figure 1b illustrates the main constructs identified in Hypotheses #4 and 5 and extends Fig. 1a by incorporating effects of “personal contact” upon social distance. Figure 1b depicts how: (1) personal contact may directly impact social distance (main effect) and how (2) personal contact might differentially impact labeling to influence social distance (interactive effect).
Method
Sample and procedures
The study sample consists of 160 adult (age 18 and older) urban community members ascertained in Beijing, China over a period of 3 months (June–August 2004). Respondents were administered an identical vignette describing a subject who was experiencing psychotic symptomatology. One of four labeling conditions was randomly assigned to each respondent (n = 40 respondents per condition). Three of these conditions varied the diagnostic label and labeling source; one condition left the vignette unlabeled (see “labeling conditions” below). Participants were then asked to respond to questions regarding the vignette character. Participants were identified by members of the Beijing Association of Family Members of the Mentally Ill, who administered the vignette questionnaire to residents in two separate “neighborhoods” (the smallest administrative unit in urban China). After obtaining the permission of the ‘neighborhood committee’, 80 adults were identified from different households from each ‘neighborhood’. The identified community members were administered the vignette questionnaires by trained interviewers; questionnaires were checked for valid completion before collection. The refusal rate for the identified individuals was less than 10%, largely because the survey was conducted with the approval of the local neighborhood committee. We do not claim our sample to be representative of the entire Chinese population; however, our sample is descriptive of an adult, urban, community sample in northern China.
Demographic characteristics
Questions assessing demographic characteristics of respondents were asked before presentation of the vignette. The variables assessed included gender, age, education, income, belief in any religion, children under 12 years old in the household, and prior personal contact with a person with mental illness (see “Measures”). Table 2 provides the sample’s mean demographic characteristics. Given the disproportionate amount of respondents who are female, we controlled for any potential effects of gender in all regression analyses.
Table 2.
Participant demographics (Total n = 160)
| Variable | n | % | Mean (SD) | Range |
|---|---|---|---|---|
| Gender | ||||
| Male | 25 | 15.6 | ||
| Female | 135 | 84.4 | ||
| Age (years) | 55.11 (13.04) | 18–85 | ||
| Education (years) | 7.49 (4.37) | 0–15 | ||
| Monthly income (RMBa) | 846.01 (539.03)b | 14–3,000 | ||
| Believe in any religion | ||||
| Yes | 12 | 7.5 | ||
| No | 148 | 92.5 | ||
| Has children under 12 years old | ||||
| Yes | 32 | 20 | ||
| No | 128 | 80 | ||
| Contact with person with mental illness | ||||
| Yes | 38 | 23.8 | ||
| No | 122 | 76.3 | ||
8.2765 RMB = 1 USD in 2004 when these data were collected
Per capita monthly income was 946.57 RMB in urban Beijing in 2004 [65]
Measures
Vignette
Participants were randomly assigned one of four vignette conditions describing a person exhibiting symptoms of schizophrenia that varied only in its labeling condition. The gender of the vignette subject was randomly varied. Description of these symptoms (including persecutory delusions, auditory hallucinations, and more than 6 months of impairment) were adapted from the vignette describing a person with schizophrenia used in the General Social Survey [29]. Statements describing characteristics congruent with “excessive thinking” (italicized below) were also embedded within the vignette. These statements describe behaviors that are consistent with how “excessive thinking” is perceived to be intertwined with the manifestation of schizophrenia symptoms. Following the description of the vignette subject, respondents were randomly assigned one of four labeling conditions (“no label”, “schizophrenia + psychiatrist”, “thinking too much + elder uncle”, and “schizophrenia + elder uncle”; see “labeling conditions” below). The “no label” condition was solely used to check the validity of the vignette in realistically depicting a person with “schizophrenia” or “excessive thinking”. The remaining three vignette conditions represented different labels and treatment sources reflecting how labeling conditions might naturalistically occur in China, which we then utilized to assess respondents’ social distance. The vignettes were professionally translated into Chinese and then independently back translated into English for comparison. Inconsistencies were resolved through discussion between the translators. Appropriate names were selected for male (“Jung”) and female (“Ahn”) vignette characters. For simplicity, the vignettes and dependent measures described below refer to a Chinese man. The vignette, labeling conditions, and questionnaires are provided below.
“Jung is a single, 23-year-old man. He completed high school and then started working. Up until about a year ago, he was steadily employed and self-supporting.
Jung has always been the kind of person who worries about others taking advantage of him. During the past few years, Jung became certain that people were spying on him and that they could hear what he was thinking. When he passes people talking on the street, he feels they are talking about him. He is convinced that he can hear voices talking about him from other rooms in his apartment building even though no one else can hear the voices. He constantly complains to others about people who he feels are out to hurt him, and gets very angry if people tell him his thoughts about this are wrong. Jung stopped working and retreated to his home, eventually spending most of his day alone in his room and refusing to talk to others. He has been living this way for 1 year.”
Independent variable
The independent variables are the diagnostic label and labeling source (italicized below), which were randomly assigned according to the following conditions:
No label provided
“Pure” psychiatric labeling condition: “A while ago, a family member brought Jung to see a psychiatrist for advice about his situation. The psychiatrist diagnosed Jung with the condition of schizophrenia.”
“Mixed” labeling condition: “A while ago, a family member brought Jung to see an elder uncle for advice about his situation. The uncle said that Jung was just like someone else he knew who had schizophrenia, and should see a psychiatrist right away.”
“Pure” non-psychiatric labeling condition: “A while ago, a family member brought Jung to see an elder uncle for advice about his situation. The uncle said that Jung was ‘taking things too hard’ and demonstrating excessive thinking.”
Dependent variables
To first evaluate the validity of the diagnostic label conditions, the following three items were administered to the “No label” group only: (1) “In your opinion, how likely is it that Jung has a mental illness?” (2) “In your opinion, how likely is it that Jung is demonstrating ‘excessive thinking’?” (3) “In your opinion, how likely is it that Jung has schizophrenia?” Separate questions were posed assessing “mental illness” and “schizophrenia” because the former encompasses a lay conception of “insanity” while the latter is a medical term that is more descriptive of specific symptomatology [42]. Respondents rated these items on a 4-point Likert scale: 1 = not at all likely, 2 = not very likely, 3 = somewhat likely, 4 = very likely.
A subset of five adapted items from a 19-item social distance measure previously used in China [60] was used to assess the main outcome. Social distance is one of the most commonly used outcomes to assess stigma towards persons with mental illness [66]. We did not seek to assess social distance in the “no label” condition because social distance might be attributable to one of many subjective interpretations that respondents had about the vignette character’s symptomatology. Hence, only respondents assigned to labeling conditions that depicted a fixed diagnostic label and a labeling source (i.e., conditions #2, 3 and 4) were administered the social distance measure. The five items used to assess social distance were: (1) “How willing are you to have someone like Jung as a neighbor?” (2) “How willing are you to allow a child of yours to marry Jung?” (3) “How willing are you to be close friends with someone like Jung?” (4) “How would you feel about introducing Jung to a young woman you are friendly with?” (5) “How would you feel about recommending someone like Jung for a job working for a friend of yours?” Respondents rated their agreement with these items on a 4-point Likert scale ranging from 1 = definitely willing, 2 = probably willing, 3 = probably unwilling, to 4 = definitely unwilling. Following prior literature, each item of the five-item scale was dichotomized (0 = “definitely willing” or “probably willing”, 1 = “probably unwilling” or “definitely unwilling” [29]); dichotomization is commonly used because being “willing” or “unwilling” to engage in certain relationships with the target individual is considered to be of utmost relevance. These five items were then summed to form a total score from 0 to 5 (with higher scores indicating greater social distance, Cronbach’s α = 0.80).
Personal contact
Prior to the administration of the vignette, respondents were asked, “Have you in your daily life had personal contact with a person with mental illness?” This item was designed to assess “personal” contact with people with mental illness and was coded dichotomously (yes/no). Single-item measures of personal contact have been found to significantly predict stigma in past research [51].
Covariates
As the independent variable (i.e., labeling condition) is randomly assigned to respondents, confounding of its effects on the outcome measures by other variables should be minimized. Examination of correlations confirms that there were no significant differences in sociodemographic variables (Table 2) between labeling conditions (all p values >0.05, results not shown). Also, there were no sociodemographic variables that significantly correlated with both personal contact and social distance. As a result, these sociodemographic variables (with the exception of gender, which we control for in regression analyses) are not considered further during analyses.
Analysis
To examine the validity of the labeling conditions, we examined the degree to which respondents from condition #1 agreed that labels were accurate in describing the vignette subject’s symptomatology. One sample t-tests against the test value of 2.5 (the midpoint score on each scale) were utilized to examine whether respondents agreed with each label. Paired-sample t-tests were then used to compare whether the respondents endorsed a label of “excessive thinking” more strongly than a label of “mental illness” or “schizophrenia”. Subsequently, correlational analyses were conducted to examine how respondents’ use of these different labels was associated with one another. We next examined the effects that labeling and personal contact had upon social distance. As we were not interested in assessing social distance among respondents in the “no label” vignette condition, they were excluded from these analyses. Accordingly, utilizing respondents from conditions #2–4, we conducted the following four multivariate regression models: (1) Model 1 assesses the effects of labeling condition upon social distance. (2) Model 2 assesses the effect of personal contact on social distance after controlling for labeling condition. (3) Model 3 examines the role of personal contact as an effect modifier of the labeling condition upon social distance (i.e., contact may reduce stigma more in one labeling condition when compared with other labeling conditions). We construct Model 3 by adding into the model the labeling condition, contact, and the interaction terms between the two (labeling × contact). As our purpose is to examine how social distance differs between these three naturally occurring labeling conditions, we utilize reference groups in the regression models to compare social distance between vignette conditions.
Results
Validity of labeling conditions
From vignette condition #1, respondents agreed with the suitability of all three labels for the vignette subject’s symptomatology. For the “mental illness”, “schizophrenia”, and “excessive thinking” labels, the mean scores were significantly higher than the midpoint of 2.5 as indicated by one-sampled t-tests (see Table 3). These results show that, on average, respondents endorsed the applicability of these labels to describe the vignette subject. Paired-sample t-tests also revealed trends for respondents to endorse the label of “excessive thinking” more strongly than a label of “mental illness” (see Table 3). Further, a Pearson correlation indicated that respondents who viewed the vignette subject as manifesting “mental illness” were also significantly more likely to endorse the label of “schizophrenia” (r = 0.55 [40], p <0.001). However, Pearson correlations also indicated that endorsement of the label of “excessive thinking” was not associated with utilization of the “mental illness” or “schizophrenia” labels (largest r = 0.09, all p values >0.10).
Table 3.
Validity of labeling conditions
| Label | Mean (SD) | Mean comparisons (t values)
|
||
|---|---|---|---|---|
| vs. 2.5a | vs. mental illnessb | vs. schizophreniab | ||
| Mental illness | 3.00 (0.64) | 4.93* | ||
| Schizophrenia | 3.02 (0.66) | 5.03* | ||
| Excessive thinking | 3.30 (0.69) | 7.36* | 1.96** | 1.92*** |
Degrees of freedom = 39
p value <0.001;
p value <0.06;
p value <0.07
One sample t-test
Paired-sample t-test
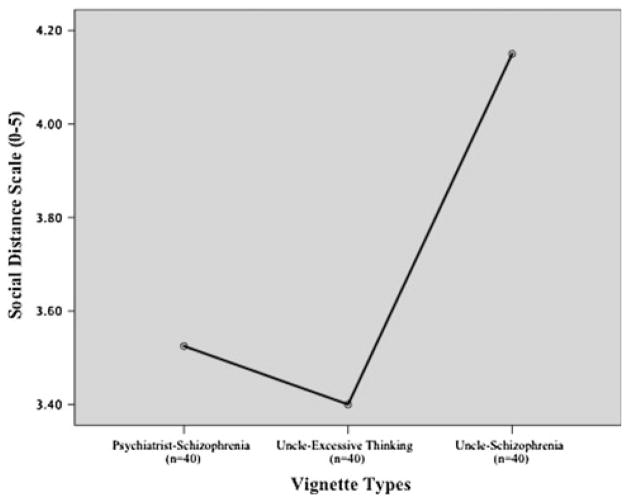
Labeling, contact, and social distance
We next utilized vignette conditions #2–4 to examine the effects of labeling and prior personal contact on social distance. As the sample is biased towards female respondents, we first entered gender into each regression model to control for any effects on social distance. Multivariate results in Table 4, Model 1, answer the question: Does the type of diagnostic label and labeling source affect respondents’ desire for social distance from the vignette subject? Dummy variables were assigned to each labeling condition to be tested in the regression models. Apriori predictions would indicate the ‘pure’ psychiatric condition (“schizophrenia” + “psychiatrist”) being assigned as the “reference” category, as we expected respondents from this group to exhibit the most social distance. However, Fig. 2 indicated that the ‘mixed’ psychiatric condition (“schizophrenia” + “uncle”) rather unexpectedly elicited the greatest mean social distance scores among all three conditions from respondents. Accordingly, we assigned this labeling condition as the reference category in order to measure the comparative decrease in social distance elicited by the remaining conditions.
Table 4.
Regression models predicting social distance
| Independent variable | Model 1
|
Model 2
|
Model 3
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | R2 | B | SE | R2 | B | SE | R2 | |
| Gender | −0.12 | 0.42 | 0.04 | −0.16 | 0.42 | 0.06 | −0.19 | 0.42 | 0.08 |
| Pure non-psychiatric | −0.75* | 0.36 | −0.77* | 0.36 | −0.43 | 0.40 | |||
| Pure psychiatric | −0.63** | 0.36 | −0.61** | 0.36 | −0.49 | 0.42 | |||
| Contact | −0.41 | 0.34 | 0.21 | 0.58 | |||||
| Contact × pure non-psychiatric | −1.51** | 0.86 | |||||||
| Contact × pure psychiatric | −0.51 | 0.80 | |||||||
Reference category is the “mixed” labeling condition (“schizophrenia + uncle”)
p value <0.05;
p value ≤ 0.09
Fig. 2.
Mean social distance score by Vignette conditions
Hypothesis 2 tested the effects of labeling condition upon social distance (Table 4, Model 1). Participants who were given the ‘pure’ non-psychiatric (“excessive thinking” + “uncle”) labeling condition scored significantly lower on the social distance scale than those who were given the ‘mixed’ labeling condition (“schizophrenia” + “uncle”) (B = −0.75, t = −2.1, df = 3, p <0.05). Contrary to Hypothesis 3, a trend existed in the direction opposite to our prediction; there was a trend finding that social distance was reduced among respondents who were given the “pure” psychiatric labeling condition (“schizophrenia” + “psychiatrist”) when compared with the “mixed” labeling condition (“schizophrenia” + “uncle”) (B = −0.63, t = −1.76, df = 3, p <0.09).
To test whether there were differences in the magnitude of these two effects, we imposed linear equality constraints as specified by Rindskopf [67]. This analysis revealed a trend that the magnitude of (“excessive thinking” + “uncle”) versus (“schizophrenia” + “uncle”) was greater than the magnitude of (“schizophrenia” + “psychiatrist”) versus (“Schizophrenia” + “Uncle”) (Hotelling’s T2[1, 120] = 3.14, p <0.10).
In order to test Hypothesis 4, our next question is whether respondents’ history of having personal contact with a person with mental illness independently affects their desire for social distance. After entering the fixed labeling conditions, we entered contact into a separate regression model (Table 4, Model 2). Examining the beta coefficient for contact indicated a negative, but non-significant, direct effect of contact on social distance scores.
Table 4, Model 3, addresses Hypothesis 5 by answering the question: Does the effect of the diagnostic label and labeling source differ between respondents who have had personal contact with a person with mental illness and those who have not? There was a trend finding for the interaction term for contact and the pure non-psychiatric condition (“excessive thinking + uncle”; B = −1.51, t = −1.76, df = 6, p = 0.081), while the interaction term for contact and the pure psychiatric condition (“schizophrenia + psychiatrist”) was not significant. Further, adding contact and the interaction terms to the labeling conditions in Model 1 reduced the beta coefficient of the pure non-psychiatric condition (“excessive thinking + uncle”) compared to the reference mixed condition (“schizophrenia + uncle”) by 42.6%, rendering it not significant. Thus, among those who had previous contact with a person with mental illness, only those exposed to the pure non-psychiatric condition (“excessive thinking + uncle”) exhibited the lowest mean social distance scores. Among those with no previous contact, this labeling condition did not appear to affect social distance. Stratification of the social distance scores in each labeling condition by personal contact in Fig. 3 portrays these findings graphically.
Fig. 3.
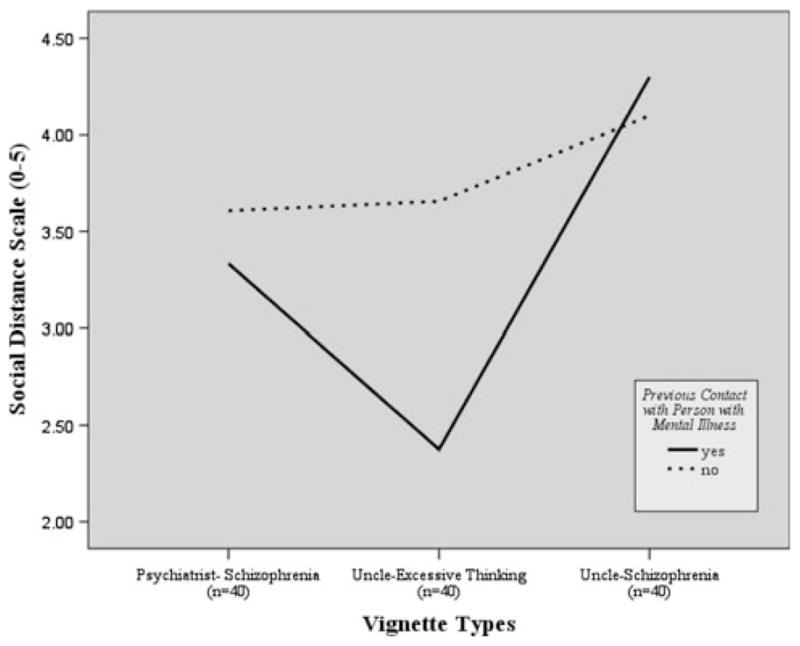
Stratification of social distance score by personal contact in each Vignette conditions
Discussion
The results are partially consistent with our hypotheses, or with what previous literature on labeling effects in Western populations might lead us to predict. Hypothesis 1 was supported, as respondents endorsed the application of “excessive thinking” and “mental illness” labels to the vignette individual’s psychotic symptomatology. That respondents tended to even more strongly agree that “excessive thinking” better described the presented symptomatology than the “mental illness” label further illustrated the validity of this indigenous idiom for describing schizophrenia symptomatology among urban, Chinese groups specifically. Further, community respondents’ use of the “excessive thinking” label appeared to refer to an indigenous interpretation of illness that was distinct from psychiatric conceptions of illness, as the correlation between use of “excessive thinking” and “mental illness/schizophrenia” labels was very low. Hypothesis 2 was partially confirmed, as respondents given the non-psychiatric diagnostic label and labeling source condition (“excessive thinking” + “uncle”) endorsed the least social distance among all three labeling conditions. However, analyses demonstrated that this condition somewhat unexpectedly elicited significantly less social distance from the “mixed” diagnostic label and labeling source condition (“schizophrenia” + “uncle”), but not the purely psychiatric labeling condition (“schizophrenia” + “psychiatrist”). Related to this finding, Hypothesis 3 yielded an unexpected result as respondents did not express the greatest social distance towards the condition that utilized both psychiatric labeling sources (“schizophrenia” + “psychiatrist”). Further, there was a trend for this “pure” psychiatric condition to result in reduced social distance when compared with the “mixed” labeling condition (“schizophrenia” + “uncle”). There was also suggestive evidence that the magnitude of the difference between the “mixed” labeling condition (“schizophrenia” + “uncle”) and “pure” non-psychiatric condition (“excessive thinking” + “uncle”) was greater than the magnitude between the “mixed” labeling condition (“schizophrenia” + “uncle”) and the “pure” psychiatric condition (“schizophrenia” + “psychiatrist”).
Contradicting Hypothesis 4 and findings among Western groups, prior personal contact with people with mental illness did not independently decrease community attitudes of social distance among respondents in our sample. In testing Hypothesis 5, contact did demonstrate a significant interaction with labeling condition in reducing social distancing attitudes. However, this interaction worked in the opposite manner framed by Western findings, as contact had no effect in reducing stigma in the diagnostic labeling (“schizophrenia”) conditions. Rather, analyses showed that those who received the “pure” non-psychiatric labeling condition (“excessive thinking” + “uncle”) and who had reported previous personal contact with individuals with mental illness endorsed reduced social distance compared with respondents who had no prior contact and received this same labeling condition. Subsequent analyses revealed that the reduction in social distance demonstrated between the “pure” non-psychiatric labeling condition (“excessive thinking” + “uncle”) and the “mixed” labeling condition (“schizophrenia” + “uncle”) was attributable to respondents within the “pure” non-psychiatric labeling condition who had prior contact endorsing less social distance than those who did not have previous contact.
Effects of diagnostic labeling in urban China
Our study demonstrated that the diagnostic label and source of labeling significantly influenced social distance towards mental illness in urban China even though the vignette character’s symptomatology remained constant across conditions. Although our primary hypothesis that the non-psychiatric diagnostic label of “excessive thinking” might be used to explain schizophrenia and contribute to decreased social distance was partially confirmed, the results from the remaining “mixed” and “pure” psychiatric conditions suggested different effects of labeling than what would be expected from Western findings. For example, our findings differ from earlier vignette studies [30, 33], which reported that the highest community levels of shame and stigma were directed towards individuals who contacted a psychiatrist for treatment as opposed to other healers for psychiatric symptoms. Our results instead indicated that the “mixed” labeling condition (“schizophrenia” + “uncle”) elicited the greatest amount of social distance. That this labeling condition in effect described someone with untreated psychosis—which combined with the severe stereotypes of dangerousness attributed to people with mental illness in China [8, 61]—might account for the elevated levels of social distance endorsed towards this labeling condition.
Alternatively, unique cultural dynamics in Chinese culture when compared with Western societies in regards to a family elder’s (i.e., uncle’s) role as a labeling source might have contributed to greater social distance [50, 68]. In Western societies, a psychiatrist is seen to more powerfully impact labeling and stigma than an elder family member because of ascribed authority and close affiliation with mental health institutions [30]. However, due to an emphasis on upholding hierarchical obligations as defined by one’s familial relationships in traditional China [50], family elders such as an uncle might hold a venerated position within their network. This respected position might result in even more highly ascribed authority than a psychiatrist and lead to increased associations of ‘moral contamination’ among observers. In any case, reduction in stigma did not take place as expected with use of non-psychiatric labeling sources; instead, the combination of a schizophrenia label in tandem with a non-professional help-seeking source paradoxically acted to increase stigma.
Further contrary to findings in Western populations, our results do not demonstrate greater stigmatizing effects when a vignette individual described with a psychiatric label contacts official psychiatric services when compared with non-psychiatric help sources [30]. In this case, schizophrenia that is treated by a psychiatrist was not seen as more stigmatizing than other labeling conditions in our sample, and there was even a trend finding that this “pure” psychiatric labeling condition resulted in less social distance than the “mixed” labeling condition (“schizophrenia” + “uncle”). This finding might be at least partially accounted for by the tendency for Chinese respondents to more likely identify themselves and others in terms of social roles than do American respondents [69]. Given the emphasis on collective duty and the Confucian desire to preserve social order in China [8], it is plausible that people with schizophrenia who prescribe to their “patient role” and adhere to treatment might be seen as more favorable than those who do not. This, in addition to stigma of untreated psychosis being seen as particularly negative [70], might have contributed to mitigating social distance towards people with schizophrenia who enter psychiatric treatment. More detailed differentiation of the mechanisms by which these labeling mechanisms function might be the focus of further empirical work.
Personal contact and labeling in reducing stigma
Personal contact where individuals have the opportunity to interact with people with mental illness, in contrast to “impersonal” contact, has been shown to be the most reliable means of reducing community stigma towards mental illness among Western groups. Retrospective “personal” contact alone was found to predict reduced stigma in a review of nine empirical studies conducted in Western settings [64]. Yet its efficacy among Chinese groups has yet to be conclusively determined. Increased prior personal contact with people with mental illness in our urban, northern Chinese sample did not independently reduce community attitudes of social distance. Our results are similar to a study of Chinese nurses’ attitudes, which were measured after assessing for retrospective personal contact (i.e., by reported family history of psychiatric illness) and prospective personal contact (i.e., after participating in psychiatric training [62]). Neither form of personal contact was found to result in more positive mental illness attitudes. A possible explanation for our non-significant findings could be that we did not explicitly account for the nature of personal contact that respondents experienced, as factors such as type of status (equal or not), degree of intimacy, whether contact was voluntary, perceived as pleasant, and viewed as cooperative or competitive are critical to determining its effect on stigmatizing attitudes [64]. Experiencing positive quality of contact (i.e., having equal status, one-on-one contact, and being placed in a cooperative situation) is optimal to changing stereotypes about a stigmatized group [71]. If personal contact took place in situations where people with mental illness were not afforded equal status (a common circumstance in China [63]), then stigma reduction is less likely to have occurred in these situations.
We further took advantage of a unique opportunity in China to examine whether personal contact reduced stigma towards symptomatic behavior, the psychiatric label itself, or when labels of symptomatology encompassed alternative labels (i.e. cultural idioms). In the “schizophrenia” labeling conditions, contact did not act to reduce social distance, thus implying that contact did not decrease stigma towards symptomatic behavior or the psychiatric label. Instead, a major, although unexpected, finding was that solely among those who received an indigenous label (i.e., “excessive thinking”) did experiencing personal contact diminish social distancing attitudes. Link et al.’s seminal work [26] demonstrated that the “set of pre-existing conceptions” that influence rejecting responses are critical to the emergence of the impacts of labeling. These “pre-existing beliefs” or stereotypes—which might be powerfully shaped by personal contact [52]—are then seen as highly salient to activating labeling effects. As contact does not significantly decrease stigma by itself among our sample, pre-existing mental illness attitudes thus remain negative even among individuals who have had personal contact with people with mental illness. In the alternative labeling condition, contact only decreases social distance because respondents know that the symptomatology being described is not indicative of mental illness, and thus does not merit a social distancing response. Hence, in the urban Chinese context, cultural idioms do provide some protection from stigma in the case of severe symptomatology, but only among respondents who are familiar with what mental illness is. The use of an alternative label in this instance was not found on its own to significantly reduce community stigma, which is not altogether unanticipated given that the severe symptomatology described in the vignette would be expected to independently elicit strong social distancing attitudes [26].
“Excessive thinking” as an idiom to reduce stigma towards schizophrenia
Our findings contribute further evidence to the durability of the cultural connection between excessive thinking and mental illness among urban Chinese community groups. Prior work has demonstrated that family members of Chinese individuals with schizophrenia frequently utilize this idiom to encapsulate disruptive symptomatology among ill relatives [72], resulting in positive effects such as reduced relapse and socially accommodating behaviors towards patients [18, 19] and reduced internalized stigma for relatives [47]. This study is the first to document that urban Chinese community members also endorse this elastic idiom in relation to psychiatric symptoms, which reduces stigmatizing attitudes among the subset of community members who have first-hand knowledge of mental illness towards those exhibiting symptomatic behaviors. “Excessive thinking” thus acts among Chinese groups in a comparable fashion to idioms identified in other groups—nervios among Mexicans [45] (similarly, nerves in other cultural groups), isamullatuq or “burdened down by thoughts” among Inuit Indians [48], and studiation madness or “excessive mental emphasis on any subject, especially when acquired through reading” in the Caribbean [73]. All of these idioms act as “culturally meaningful illness categories” which potentially preserve the moral status of those who demonstrate psychiatric symptoms that deviate from the norm [74].
With regards to community anti-stigma intervention in urban China, while use of the “excessive thinking” idiom itself was not sufficient on its own to de-stigmatize a person exhibiting severe psychotic symptoms, this idiom might be usefully integrated into traditional psycho-education campaigns to explicitly facilitate empathy of community members towards severely mentally ill persons. As indicated by our findings, community members are naturally inclined to incorporate such an idiom in their understanding of psychosis. Researchers have demonstrated that developing empathy for or assuming the perspective of a stigmatized other might diminish stigma by increasing understanding and compassion for that condition [75]. Stereotypes that delineate between sanity and insanity often exacerbate community members’ reactions to those with mental illness. The finding that urban Chinese individuals regard excessive thinking as occurring in varying degrees in all individuals [19] might provide a culturally sanctioned bridge between what is viewed as universally experienced and the status of “outcast” moral status that is assigned those officially labeled as mentally ill in China [50].
Moreover, although yet to be implemented within China, “community conversations” planned by health and community organizations to explore mental health and stigma [9] might usefully incorporate indigenous idioms such as “excessive thinking”. Use of these culturally congruent concepts of mental illness might better facilitate discussion of mental health issues such as the accurate interpretation of mental health problems and identification of when such problems become severe enough to require professional help [19]. As our findings suggest that respondents might be even more likely to view schizophrenia symptoms as “excessive thinking” than as mental illness, use of this idiom might enhance cultural sensitivity in discussing mental health problems. Such community-based approaches that integrated indigenous mental health constructs have led to improved awareness that mental illness is common and an increased willingness to talk about mental health problems [9]. Accordingly, use of indigenous idioms to construct shared understandings between community members and medical providers might act as a way to decrease stigma both via public education and community approaches.
Limitations
This study also has several limitations. First, we utilized social distance as our sole assessment of stigma. Although this measure is one of the most widely used assessments for stigma [66], incorporating other stigma constructs (e.g., stereotypes) may have allowed examination of potential mediators of social distance and a more diverse range of outcomes. Second, measuring respondents’ endorsement of “excessive thinking”, “mental illness”, and “schizophrenia” labels in the three vignette labeling conditions would have enabled assessment of respondents’ subjective interpretation of each labeling condition, and how these subjective endorsements might have further contributed to social distance. This important methodology might be used to strengthen future studies of labeling in China. However, when vignette labels were varied in the current study, differences in social distance emerged among respondents, thus giving us confidence that respondents’ perceptions of the vignette characters’ problems did change according to the label. A third study limitation includes the relatively small, geographically restricted (i.e., from Northern, urban China), and non-probability nature of our sample. Given that Chinese can differ by ethnicity, geography, urbanization, and westernization, our results are not generalizable to all of China. Also, the disproportionate amount of females in our sample further limits generalizability of our findings. However, these potential limitations are at least somewhat mitigated by the community-ascertained and therefore not self-selecting nature of our sample (other stigma studies in China have utilized volunteer student respondents [60, 62]), high response rate, and that survey samples typically tend to be proportionally more female than the general population [33]. Further, given that we controlled for any potential effects of gender during analyses, the disproportionate amount of females in our sample were shown not to influence our main findings. A fifth potential limitation is that we operationalized our personal contact construct with a single-item question rather than a multiple-item scale [76], which did not allow us to assess reliability of this item. However, this item did significantly predict decreased stigma within the “excessive thinking” labeling condition, even though it might not be as reliable as we ideally would like it to be. Finally, while we specifically assessed “personal” contact, which has on its own been shown to predict reduced stigma [64], our contact measure might also have assessed the “quality” of contact respondents had experienced with people with mental illness to further specify the nature of these interactions. Such an assessment should be included in future measures of personal contact in China.
Conclusion
This study provides valuable data obtained from a community sample in urban, Northern China regarding how personal contact and different labeling conditions impact attitudes towards mental illness. In Link et al.’s articulation of ‘Modified labeling theory’ [25], the multifaceted event of “contact with psychiatric services” was seen as the key event that initiated stigmatizing processes. Although a great deal of research has examined the specific impacts of the diagnostic label on stigma [9, 11, 15, 28, 31, 77–79], much work remains to clarify the effects of diagnostic label in relation to help-seeking source in determining stigma. Making use of a sample from urban China—and the proclivity of Chinese respondents to utilize indigenous idioms to label schizophrenia—enabled novel tests of these labeling effects that are not as easily studied in Western groups. One unexpected consequence of examining these labeling mechanisms that might be encouraging to global mental health advocates [80, 81] is that the condition depicting “untreated psychosis” elicited the greatest amount of stigma, while the “treated psychosis” condition was viewed relatively benignly in urban China. If replicated in more representative samples, these results suggest that formal psychiatric treatment of people with mental illness in China (the vast majority of whom are untreated; [80]) would not result in increased stigma for this group. We hope that this study will spur further research regarding how labeling processes within non-Western contexts such as China and other ethnic minority groups [82] both serve to increase and decrease stigma, thus unearthing further innovative means to counter the effects of this debilitating social dynamic and enabling consumers to achieve sustained remission and social recovery [83, 84].
Acknowledgments
The study was supported by National Institutes of Mental Health Grant K01 MH73034-01, which was awarded to the first author. This study was also supported, in part, by the Asian American Center on Disparities Research (National Institute of Mental Health grant P50MH073511). The authors thank Xiaoli Zhang for her assistance in creating the vignettes. We also wish to thank Ms. Nina Huynh for her assistance in formatting the manuscript.
Contributor Information
Lawrence H. Yang, Email: lhy2001@columbia.edu, Department of Epidemiology, Columbia University, 722 West 168th Street, Room 1610, New York, NY 10032, USA
Graciete Lo, Department of Psychology, Fordham University, 441 East Fordham Road, Dealy 226, Bronx, NY 10458, USA.
Ahtoy J. WonPat-Borja, Department of Epidemiology, Columbia University, 722 West 168th Street, Room 720E, New York, NY 10032, USA
Daisy R. Singla, Psychology Department, McGill University, Stewart Biology Building, 1205 Dr. Penfield Avenue #S3-20, Montreal, QC H3A 1B1, Canada
Bruce G. Link, Department of Epidemiology/Sociomedical Sciences, Columbia University, 722 West 168th Street, Room 1609, New York, NY 10032, USA
Michael R. Phillips, Suicide Research and Prevention Center and Research Methods Consulting Center, Shanghai Mental Health Center, Shanghai Jiaotong University School of Medicine, 3210 Humin Road, Shanghai 201108, People’s Republic of China. Emory University School of Medicine, Atlanta, USA
References
- 1.Phillips M, Pearson V, Li F, Xu M, Yang L. Stigma and expressed emotion: a study of people with schizophrenia and their family members in China. Br J Psychiatry. 2002;181(6):488–493. doi: 10.1192/bjp.181.6.488. [DOI] [PubMed] [Google Scholar]
- 2.Lee S, Lee M, Chiu M, Kleinman A. Experience of social stigma by people with schizophrenia in Hong Kong. Br J Psychiatry. 2005;186(2):153–157. doi: 10.1192/bjp.186.2.153. [DOI] [PubMed] [Google Scholar]
- 3.Lai Y, Hong C, Chee C. Stigma of mental illness. Singapore Med J. 2001;42(3):111–114. [PubMed] [Google Scholar]
- 4.Fogarty International Center. Stigma and global health: developing a research agenda. Fogarty International Center; Washington DC: 2001. [Google Scholar]
- 5.WonPat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-010-0319-7. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furnham A, Chan E. Lay theories of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2004;39(7):543–552. doi: 10.1007/s00127-004-0787-8. [DOI] [PubMed] [Google Scholar]
- 7.Shokoohi-Yekta M, Retish P. Attitudes of Chinese and American male students towards mental illness. Int J Soc Psychiatry. 1991;37(3):192–200. doi: 10.1177/002076409103700306. [DOI] [PubMed] [Google Scholar]
- 8.Yang L. Application of mental illness stigma theory to Chinese societies: synthesis and new direction. Singapore Med J. 2007;48(11):186–190. [PubMed] [Google Scholar]
- 9.Knifton L, Gervais M, Newbigging K, Mirza N, Quinn N, Wilson N, Hunkins-Hutchison E. Community conversation: addressing mental health stigma with ethnic minority communities. Soc Psychiatry Psychiatr Epidemiol. 2010;45(4):497–504. doi: 10.1007/s00127-009-0095-4. [DOI] [PubMed] [Google Scholar]
- 10.Yang LH, Wonpat-Borja AJ, Opler M, Corcoran C. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: An empirical question. Schizophr Res. 2010;120:42–48. doi: 10.1016/j.schres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chee C, Ng T, Kua E. Comparing the stigma of mental illness in a general hospital with a state mental hospital. Soc Psychiatry Psychiatr Epidemiol. 2005;40(8):648–653. doi: 10.1007/s00127-005-0932-z. [DOI] [PubMed] [Google Scholar]
- 12.Fung K, Tsang H, Chan F. Self-stigma, stages of change and psychosocial treatment adherence among Chinese people with schizophrenia: a path analysis. Soc Psychiatry Psychiatr Epidemiol. 2010;45(5):561–568. doi: 10.1007/s00127-009-0098-1. [DOI] [PubMed] [Google Scholar]
- 13.Lysaker PH, Tunze C, Yanos PT, Roe D, Ringer J, Rand K. Relationships between stereotyped beliefs about mental illness, discrimination experiences, and distressed mood over 1 year among persons with schizophrenia enrolled in rehabilitation. Soc Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-011-0396-2. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen A, Patel V, Thara R, Gureje O. Questioning an axiom: better prognosis for schizophrenia in the developing world? Schizophr Bull. 2007;34:229–244. doi: 10.1093/schbul/sbm105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung F, Chan JH. Can a less pejorative Chinese translation for schizophrenia reduce stigma? A study of adolescents’ attitudes toward people with schizophrenia. Psychiatry Clin Neurosci. 2004;58(5):507–515. doi: 10.1111/j.1440-1819.2004.01293.x. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y. Renaming the term schizophrenia in Japan. Lancet. 2002;360:879. doi: 10.1016/s0140-6736(02)09987-7. [DOI] [PubMed] [Google Scholar]
- 17.Griffiths K, Nakane Y, Christensen H, Yoshioka K, Jorm A, Nakane H. Stigma in response to mental disorders: a comparison of Australia and Japan. BMC Psychiatry. 2006 doi: 10.1186/1471-244X-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang L, Phillips M, Licht D, Hooley J. Causal attributions about schizophrenia in families in China: expressed emotion and patient relapse. J Abnorm Psychol. 2004;113(4):592–602. doi: 10.1037/0021-843X.113.4.592. [DOI] [PubMed] [Google Scholar]
- 19.Yang L, Phillips M, Lo G, Chou Y, Zhang X, Hopper K. “Excessive Thinking” as explanatory model for schizophrenia: impacts on stigma and “moral” status in Mainland China. Schizophr Bull. 2010;36:836–845. doi: 10.1093/schbul/sbn180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boyd J, Katz E, Link B, Phelan J. The relationship of multiple aspects of stigma and personal contact with someone hospitalized for mental illness, in a nationally representative sample. Soc Psychiatry Psychiatr Epidemiol. 2009;45(11):1063–1070. doi: 10.1007/s00127-009-0147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corrigan P, Penn D. Lessons from social psychology on discrediting psychiatric stigma. Am Psychol. 1999;54(9):765–776. doi: 10.1037//0003-066x.54.9.765. [DOI] [PubMed] [Google Scholar]
- 22.Link B, Phelan J. Conceptualizing stigma. Annu Rev Sociol. 2003;27:363–385. [Google Scholar]
- 23.Goffman E. Stigma: notes on the management of spoiled identity. Prentice-Hall; New Jersey: 1963. [Google Scholar]
- 24.Crocker J, Major B, Steele C. Social stigma: the psychology of marked relationships. In: Gilbert D, Fiske S, Lindzey G, editors. The handbook of social psychology. 4. Oxford University Press; New York: 1998. pp. 504–553. [Google Scholar]
- 25.Link B, Cullen F, Struening E, Shrout P, Dohrenwend B. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54(3):400–423. [Google Scholar]
- 26.Link B, Cullen F, Frank J, Wozniak J. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92(6):1461–1500. [Google Scholar]
- 27.Murrie D, Cornell D, McCoy W. Psychopathy, conduct disorder, and stigma: does diagnostic labeling influence juvenile probation officer recommendations? Law Hum Behav. 2005;29(3):323–342. doi: 10.1007/s10979-005-2415-x. [DOI] [PubMed] [Google Scholar]
- 28.Angermeyer M, Matschinger H. Public beliefs about schizophrenia and depression: similarities and differences. Soc Psychiatry Psychiatr Epidemiol. 2003;38(9):526–534. doi: 10.1007/s00127-003-0676-6. [DOI] [PubMed] [Google Scholar]
- 29.Link B, Phelan J, Bresnahan M, Stueve A, Pescosolido B. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89(9):1328–1333. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phillips D. Rejection: a possible consequence of seeking help for mental disorders. Am Sociol Rev. 1963;29:963–972. [Google Scholar]
- 31.Madianos M, Madianou D, Stefanis C. Help-seeking behaviour for psychiatric disorder from physicians or psychiatrists in Greece. Soc Psychiatry Psychiatr Epidemiol. 1993;28(6):285–291. doi: 10.1007/BF00795909. [DOI] [PubMed] [Google Scholar]
- 32.Mickus M, Colenda C, Hogan A. Knowledge of mental health benefits and preferences for type of mental health providers among the general public. Psychiatr Serv. 2000;51(2):199–202. doi: 10.1176/appi.ps.51.2.199. [DOI] [PubMed] [Google Scholar]
- 33.Yang L, Phelan J, Link B. Stigma and beliefs of efficacy towards traditional Chinese medicine and Western psychiatric treatment among Chinese-Americans. Cultur Divers Ethnic Minor Psychol. 2008;14(1):10–18. doi: 10.1037/1099-9809.14.1.10. [DOI] [PubMed] [Google Scholar]
- 34.Yeung A, Chang D, Gresham R, Jr, Nierenberg A, Fava M. Illness beliefs of depressed Chinese American patients in primary care. J Nerv Ment Dis. 2004;192(4):324–327. doi: 10.1097/01.nmd.0000120892.96624.00. [DOI] [PubMed] [Google Scholar]
- 35.Fuligni A, Yip T, Tseng V. The impact of family obligation on the daily activities and psychological well-being of Chinese American adolescents. Child Dev. 2002;73(1):302–314. doi: 10.1111/1467-8624.00407. [DOI] [PubMed] [Google Scholar]
- 36.Hong Y, Ip G, Chiu C, Morris M, Menon T. Cultural identity and dynamic construction of the self: Collective duties and individual rights in Chinese and American cultures. Soc Cogn. 2001;19(3):251–268. [Google Scholar]
- 37.Mead GH. Mind, self, and society, from the standpoint of a social behaviorist. University of Chicago Press; Chicago: 1934. [Google Scholar]
- 38.Kleinman A. Culture, illness. and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251–258. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 39.Mezzich JE, Kirmayer LJ, Kleinman A, Fabrega H, Parron DL, Good BJ, Lin KM, Manson SM. The place of culture in DSM-IV. J Nerv Ment Dis. 1999;187(8):457–464. doi: 10.1097/00005053-199908000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Kirmayer LJ. The fate of culture in DSM-IV. Transcult Psychiatr. 1998;35(3):339–342. [Google Scholar]
- 41.Lewis-Fernández R. The proposed DSM-IV trance and possession disorder category: Potential benefits and risks. Transcult Psychiatr Res Rev. 1992;29:301–318. [Google Scholar]
- 42.Lam CS, Tsang HWH, Corrigan PW, Lee Y-T, Angell B, Shi K. Chinese lay theory and mental illness stigma: implications for research and practices. J Rehabil. 2010;76:35–40. [Google Scholar]
- 43.Yang LH, Corsini-Munt S, Link B, Phelan JC. Beliefs in traditional Chinese medicine efficacy among Chinese Americans: implications for mental health service utilization. J Nerv Ment Dis. 2009;197(3):207–210. doi: 10.1097/NMD.0b013e3181999513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Phillips M, Li Y, Stroup T, Xin L. Causes of schizophrenia reported by patients’ family members in China. Br J Psychiatry. 2000;177(1):20–25. doi: 10.1192/bjp.177.1.20. [DOI] [PubMed] [Google Scholar]
- 45.Jenkins JH. Conceptions of schizophrenia as a problem of nerves: a cross-cultural comparison of Mexican-Americans and Anglo-Americans. Soc Sci Med. 1988;26(12):1233–1243. doi: 10.1016/0277-9536(88)90155-4. [DOI] [PubMed] [Google Scholar]
- 46.Low S. Culturally interpreted symptoms or culture-bound syndromes: a cross-cultural review of nerves. Soc Sci Med. 1985;21(2):187–196. doi: 10.1016/0277-9536(85)90088-7. [DOI] [PubMed] [Google Scholar]
- 47.Yang LH, Singla DR. Use of indigenous cultural idioms by Chinese immigrant relatives for psychosis: impacts on stigma and psychoeducational approaches. J Nerv Ment Dis. 2011;199(11):872–878. doi: 10.1097/NMD.0b013e3182349eb7. [DOI] [PubMed] [Google Scholar]
- 48.Kirmayer L, Fletcher C, Boothroyd L. Inuit attitudes toward deviant behavior: a vignette study. J Nerv Ment Dis. 1997;185(2):78–86. doi: 10.1097/00005053-199702000-00003. [DOI] [PubMed] [Google Scholar]
- 49.Yang L, Kleinman A, Link B, Phelan J, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64(7):1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 50.Yang L, Kleinman A. Face and the embodiment of stigma in China: the cases of schizophrenia and AIDS. Soc Sci Med. 2008;67(3):398–408. doi: 10.1016/j.socscimed.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Phelan JC, Link BG. Fear of people with mental illnesses the role of personal and impersonal contact and exposure to threat or harm. J Health Soc Behav. 2004;45:68–80. doi: 10.1177/002214650404500105. [DOI] [PubMed] [Google Scholar]
- 52.Couture S, Penn D. Interpersonal contact and the stigma of mental illness: a review of the literature. J Ment Health. 2003;12(3):291–305. [Google Scholar]
- 53.Reinke R, Corrigan P, Leonhard C, Lundin R, Kubiak M. Examining two aspects of contact on the stigma of mental illness. J Soc Clin Psychol. 2004;23(3):377–389. [Google Scholar]
- 54.Alexander L, Link B. The impact of contact on stigmatizing attitudes toward people with mental illness. J Ment Health. 2003;12(3):271–289. [Google Scholar]
- 55.Corrigan P, Edwards A, Green A, Diwan S, Penn D. Prejudice, social distance, and familiarity with mental illness. Schizophr Bull. 2001;27(2):219–225. doi: 10.1093/oxfordjournals.schbul.a006868. [DOI] [PubMed] [Google Scholar]
- 56.Corrigan P, Green A, Lundin R, Kubiak M, Penn D. Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv. 2001;52(7):953–958. doi: 10.1176/appi.ps.52.7.953. [DOI] [PubMed] [Google Scholar]
- 57.Ingamells S, Goodwin A, John C. The influence of psychiatric hospital and community residence labels on social rejection of the mentally ill. Br J Clin Psychol. 1996;35(3):359–368. doi: 10.1111/j.2044-8260.1996.tb01190.x. [DOI] [PubMed] [Google Scholar]
- 58.Read J, HarrÈ N. The role of biological and genetic causal beliefs in the stigmatisation of mental patients. J Ment Health. 2001;10(2):223–235. [Google Scholar]
- 59.Vezzoli R, Archiati L, Buizza C, Pasqualetti P, Rossi G, Pioli R. Attitude towards psychiatric patients: a pilot study in a northern Italian town. Eur Psychiatry. 2001;16(8):451–458. doi: 10.1016/s0924-9338(01)00606-x. [DOI] [PubMed] [Google Scholar]
- 60.Chung K, Chen E, Liu C. University students’ attitudes towards mental patients and psychiatric treatment. Int J Soc Psychiatry. 2001;47(2):63–72. doi: 10.1177/002076400104700206. [DOI] [PubMed] [Google Scholar]
- 61.Tsang H, Tam P, Chan F, Cheung W. Stigmatizing attitudes towards individuals with mental illness in Hong Kong: implications for their recovery. J Community Psychol. 2003;31(4):383–396. [Google Scholar]
- 62.Callaghan P, Shan C, Yu L, Ching L, Kwan T. Attitudes towards mental illness: testing the contact hypothesis among Chinese student nurses in Hong Kong. J Adv Nurs. 1997;26(1):33–40. doi: 10.1046/j.1365-2648.1997.1997026033.x. [DOI] [PubMed] [Google Scholar]
- 63.Lee S, Chiu M, Tsang A, Chui H, Kleinman A. Stigmatizing experience and structural discrimination associated with the treatment of schizophrenia in Hong Kong. Soc Sci Med. 2006;62(7):1685–1696. doi: 10.1016/j.socscimed.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 64.Desforges D, Lord C, Ramsey S, Mason J, Van Leeuwen M, West S, Lepper M. Effects of structured cooperative contact on changing negative attitudes toward stigmatized social groups. J Pers Soc Psychol. 1991;60(4):531–544. doi: 10.1037//0022-3514.60.4.531. [DOI] [PubMed] [Google Scholar]
- 65.US-China Business Council. USCBC snapshots: Beijing at a Glance. 2004 http://www.uschina.org/info/china-briefing-book/chops/beijing.html.
- 66.Link B, Yang L, Phelan J, Collins P. Measuring mental illness stigma. Schizophr Bull. 2004;30(3):511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- 67.Rindskopf D. Linear equality restrictions in regression and loglinear models. Psychol Bull. 1984;96(3):597–603. [Google Scholar]
- 68.Yang L, Pearson V. Understanding families in their own context: schizophrenia and structural family therapy in Beijing. J Fam Ther. 2002;24(3):233–257. [Google Scholar]
- 69.Ip G, Bond M. Culture, values, and the spontaneous self-concept. Asian J Psychol. 1995;1(1):30–36. [Google Scholar]
- 70.Melle I, Larsen T, Haahr U, Friis S, Johannessen J, Opjordsmoen S, Simonsen E, Rund B, Vaglum P, McGlashan T. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004;61(2):143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- 71.Desforges DM, Lord CG, Ramsey SL, Mason JA, Van Leeuwen MD, West SC, Lepper MR. Effects of structured cooperative contact on changing negative attitudes toward stigmatized social groups. J Pers Soc Psychol. 1991;60(4):531–544. doi: 10.1037//0022-3514.60.4.531. [DOI] [PubMed] [Google Scholar]
- 72.Yang L. Causal attributions, expressed emotion, and patient relapse: recent findings and application to Chinese societies. Hong Kong J Psychiatry. 2003;13(2):16–25. [Google Scholar]
- 73.Littlewood R. From vice to madness: the semantics of naturalistic and personalistic understandings in Trinidadian local medicine. Soc Sci Med. 1988;27(2):129–148. doi: 10.1016/0277-9536(88)90322-x. [DOI] [PubMed] [Google Scholar]
- 74.Jenkins J. Ethnopsychiatric interpretations of schizophrenic illness: the problem of nervios within Mexican-American families. Cult Med Psychiatry. 1988;12(3):301–329. doi: 10.1007/BF00051972. [DOI] [PubMed] [Google Scholar]
- 75.Batson C, Polycarpou M, Harmon-Jones E, Imhoff H, Mitchener E, Bednar L, Klein T, Highberger L. Empathy and attitudes: can feeling for a member of a stigmatized group improve feelings toward the group? J Pers Soc Psychol. 1997;72:105–118. doi: 10.1037//0022-3514.72.1.105. [DOI] [PubMed] [Google Scholar]
- 76.Holmes E, Corrigan P, Williams P, Canar J, Kubiak M. Changing attitudes about schizophrenia. Schizophr Bull. 1999;25(3):447–456. doi: 10.1093/oxfordjournals.schbul.a033392. [DOI] [PubMed] [Google Scholar]
- 77.González-Torres M, Oraa R, Aristegui M, Fernández-Rivas A, Guimon J. Stigma and discrimination towards people with schizophrenia and their family members. Soc Psychiatry Psychiatr Epidemiol. 2007;42(1):14–23. doi: 10.1007/s00127-006-0126-3. [DOI] [PubMed] [Google Scholar]
- 78.Mojtabai R. Mental illness stigma and willingness to seek mental health care in the European Union. Soc Psychiatry Psychiatr Epidemiol. 2010;45:705–712. doi: 10.1007/s00127-009-0109-2. [DOI] [PubMed] [Google Scholar]
- 79.Thompson A, Stuart H, Bland R, Arboleda-Florez J, Warner R, Dickson R. Attitudes about schizophrenia from the pilot site of the WPA worldwide campaign against the stigma of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2002;37(10):475–482. doi: 10.1007/s00127-002-0583-2. [DOI] [PubMed] [Google Scholar]
- 80.Phillips M, Zhang J, Shi Q, Song Z, Ding Z, Pang S, Li X, Zhang Y, Wang Z. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey. Lancet. 2009;373(9680):2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- 81.Yang L, Link B. Comparing diagnostic methods for mental disorders in China. Lancet. 2009;373:2002–2004. doi: 10.1016/S0140-6736(09)61091-6. [DOI] [PubMed] [Google Scholar]
- 82.Keyes KM, Martins SS, Hatzenbuehler ML, Blanco C, Bates LM, Hasin DS. Mental health service utilization for psychiatric disorders among Latinos living in the United States: the role of ethnic subgroup, ethnic identity, and language/social preferences. Soc Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-010-0323-y. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Opler M, Yang L, Caleo S, Alberti P. Statistical validation of the criteria for symptom remission in schizophrenia: preliminary findings. BMC Psychiatry. 2007;7:35. doi: 10.1186/1471-244X-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Link BG, Epperson M, Castille D, Yang LH. Arrest outcomes associated with outpatient committment in New York state. Psychiatr Serv. 2011;62:504–508. doi: 10.1176/ps.62.5.pss6205_0504. [DOI] [PMC free article] [PubMed] [Google Scholar]